Professional Documents
Culture Documents
CKD PDF
Uploaded by
aparajitaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CKD PDF
Uploaded by
aparajitaCopyright:
Available Formats
Chronic kidney disease
Strategies for management
Lifestyle and pharmacological strategies to
preserve kidney function and improve outcomes
Intervention strategies
Interventions include non-pharmacological strategies,such as diet
and lifestyle modifications, and pharmacological strategies
Diet and lifestyle For disease progression For cardiovascular risk For other comorbidities Renal replacement
Pharmacological strategies
Timing of implementation
All strategies have a window of optimal effect based on a patient’s stage of kidney function decline
Plant dominant, low-protein diet
Nutrient-focused intervention (low sodium, phosphate, and potassium)
Physical activity
Smoking cessation
Weight reduction*
Renin–angiotensin–aldosterone system blockade Unnecessary weight loss in
SGLT2 inhibitors advanced chronic kidney disease
should be avoided, unless
For individuals with Non-steroidal mineralocorticoid receptor antagonists* absolutely required
diabetic kidney disease
Tolvaptan for polycystic kidney disease
Rituximab* For primary membranous nephropathy
Steroids for IgA nephropathy
Lipid-lowering agents
Blood-pressure lowering agents
Glucose-lowering agents
Sodium and volume management
Potassium binders
Acidosis management
Symptom management
Infection prevention
Dialysis
Transplantation
eGFR 120 60 30 10 0
Increasing Loss of residual
Hyperfiltration Albuminuria Declining GFR
uraemia kidney function
eGFR=estimated glomerular filtration rate (mL/min per 1·73 m2)
Read the full Seminar on chronic kidney disease at thelancet.com/clinic
The best science for better lives
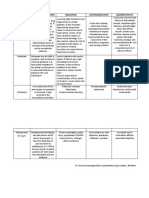
Interventions in more detail
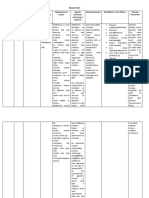
Diet and lifestyle strategies Targeting
Intervention Pros Cons CKD CVD Uraemia
Plant dominant, Patient-centered, inexpensive, improves Risk of hyperkalaemia and protein-energy wasting
low-protein diet metabolic parameters, mitigates acidosis; might
slow CKD progression and attenuate uraemia
Nutrient-focussed Traditional familiarity in clinical practice including Excessive dietary potassium restriction can
intervention potassium and phosphorus control deprive patients from intake of healthy diet
Physical activity Numerous clear health benefits including Excessive physical activity can lead to
slower decline in kidney function and rhabdomyolsis, which can cause acute kidney injury
improving cardiovascular profile
Smoking cessation Current and former smoking associated with None
greater risk of incident CKD and cardiovascular risk
Weight reduction Improves cardiometabolic health, might mitigate In dialysis-dependent patients, weight loss can be
glomerular hyperfiltration and slow decline in be associated with poor outcome (obesity paradox)
kidney function, and might improve albuminuria
Pharmacological strategies Targeting
Intervention Pros Cons CKD CVD Uraemia
Renin–angiotensin– Slows CKD progression with clearest benefit in Risk of hyperkalaemia and acute kidney injury
aldosterone system people with substantial albuminuria
blockade
SGLT2 inhibitors Slows and prevents cardiovascular events Higher risk of genital fungal infection and
regardless of diabetes as the cause of CKD nondiabetic ketoacidosis. Cannot be currently
initiated if starting eGFR <25 mL/min/1.73m2
Non-steroidal Reduction in risk of adverse renal and Higher risk of hyperkalaemia; yet to be
mineralocorticoid receptor cardiovascular outcomes in type 2 diabetes evaluated in non-diabetic kidney disease
antagonists
Tolvaptan for polycystic Slows rate of kidney growth and glomerular Higher risk of dehydration and hypernatremia
kidney disease filtration rate decline in autosomal dominant if not responsive to thirst; risk of liver damage
polycystic kidney disease
Rituximab for primary Increases likelihood of long-term remission Little randomised controlled trial data directly
membranous nephropathy comparing with alkylating agents
Steroids for IgA Extensive clinical experience Mixed results in clinical trials, increased risk of
nephropathy adverse events, especially serious infection
Lipid-lowering agents Reduces vascular events in people with No clear benefit for initiating treatment
CKD, well tolerated in people on dialysis therapy
Blood pressure-lowering Reduces cardiovascular and might reduce Greater risk of adverse events, including acute
agents adverse renal outcomes kidney injury, as kidney function declines
Glucose-lowering agents SGLT2-inhibitors and GLP-1 receptor Risk of hypoglycemia and other
agonists reduce adverse cardiovascular treatment related adverse events with
events in type 2 diabetes intensive glucose-lowering therapy
Acidosis management May slow progression of CKD NaHCO3 administration may worsen
pharmacological strategies sodium and fluid retention
Potassium binders Reduces risk of hyperkalaemia associated cardiac No data on patient-level outcomes or
events and might enable use of renin–angiotensin– progression of kidney disease
aldosterone pathway modulators
Sodium and volume Well established clinical experience Effect on CKD progression uncertain
management
Symptom management Important priority for patients with more Unknown to affect risk of CKD
unpleasant symptoms progression or need for dialysis
Infection prevention Many infectious events can cause acute kidney Direct kidney involvement not
injury, faster CKD progression, or both certain, such as in COVID-19
Renal repacement strategies Targeting
Intervention Pros Cons CKD CVD Uraemia
Dialysis Provides effective therapy for uraemia, fluid Conventional dialysis therapy can be
overload, hyperkalaemia, and acidosis; associated with unpleasant symptoms, such
incremental transition to dialysis is preferred as muscle cramps and post-dialysis fatigue
Kidney transplant The most effective renal replacement therapy if Associated immunosuppression increases
there is a well functioning allograft risk of opportunistic infection and cancer
CKD=chronic kidney disease; CVD=cardiovascular disease
Read the full Seminar on chronic kidney disease at thelancet.com/clinic
The best science for better lives
You might also like
- Chronic Kidney Disease StagesDocument62 pagesChronic Kidney Disease StagesBryant Munoz100% (3)
- Important Complications of Chronic Kidney Disease PDFDocument4 pagesImportant Complications of Chronic Kidney Disease PDFDrBishnu Prasad MahalaNo ratings yet
- Name of Drug Content Class and Mechanism of Action (MOA) Indication/s Contraindication/s Side Effects (Pere System) Nursing ConsiderationsDocument8 pagesName of Drug Content Class and Mechanism of Action (MOA) Indication/s Contraindication/s Side Effects (Pere System) Nursing ConsiderationsJustin John NavarroNo ratings yet
- Kuliah 5. Kasus 1 Dan 2 (GGK)Document94 pagesKuliah 5. Kasus 1 Dan 2 (GGK)yudiNo ratings yet
- GGK PKMRS PugerDocument12 pagesGGK PKMRS Pugersyamsul arifinNo ratings yet
- CHRONIC KIDNEY DISEASE Pelatihan Perawat HD 2021Document33 pagesCHRONIC KIDNEY DISEASE Pelatihan Perawat HD 2021Yudha WirawanNo ratings yet
- Management of Diabetic Kidney Disease Updated 0Document1 pageManagement of Diabetic Kidney Disease Updated 0Jia-PeiWuNo ratings yet
- CKD Du 22Document76 pagesCKD Du 22PUTROSM DARSONONo ratings yet
- Antidiabetic Drug 1 190517142411Document17 pagesAntidiabetic Drug 1 190517142411salehaNo ratings yet
- CKD CmeDocument45 pagesCKD Cmeizatul farhanahNo ratings yet
- Chronic Kidney Disease: Chronic Kidney Disease (CKD) Is Defined As Abnormalities in Kidney Structure orDocument11 pagesChronic Kidney Disease: Chronic Kidney Disease (CKD) Is Defined As Abnormalities in Kidney Structure orAnangNo ratings yet
- 5 D4 Pemberian Diet Pada CKDDocument29 pages5 D4 Pemberian Diet Pada CKDPinny Rilenda L NgaraNo ratings yet
- 2023 - Trà - Ptico KDIGODocument1 page2023 - Trà - Ptico KDIGOIngrid OrduzNo ratings yet
- Takeaways For Clinicians From The KDIGO 2020 Clinical Practice Guideline For Diabetes Management in CKDDocument1 pageTakeaways For Clinicians From The KDIGO 2020 Clinical Practice Guideline For Diabetes Management in CKDLabontu IustinaNo ratings yet
- Diabetes ManagementDocument44 pagesDiabetes ManagementRahaf AlhubailNo ratings yet
- Gagal Ginjal Kronik FarmakoDocument28 pagesGagal Ginjal Kronik FarmakoIkhza Yasyifa RusydaNo ratings yet
- Prinsip Terapi Pada GG Ginjal Dan Hepar - DR Tri Murti Andayani, SP - FrsDocument58 pagesPrinsip Terapi Pada GG Ginjal Dan Hepar - DR Tri Murti Andayani, SP - FrsJinan RanasaninahNo ratings yet
- PCPOnePage 1side EnglishDocument1 pagePCPOnePage 1side EnglishfazilahbajuriNo ratings yet
- CKD CHCRTDocument28 pagesCKD CHCRTNurhidayati KeriyunNo ratings yet
- Chronic Kidney Disease Bhakti MuliaDocument24 pagesChronic Kidney Disease Bhakti MuliaCOVID RSHJNo ratings yet
- Aki and CKD Therapy 2021Document46 pagesAki and CKD Therapy 2021Alfathri YunediNo ratings yet
- 1.acute Kidney InjuryDocument3 pages1.acute Kidney InjuryIan CruzNo ratings yet
- Chronic Kidney Disease: Diagnosis and TherapyDocument21 pagesChronic Kidney Disease: Diagnosis and TherapyLindsNo ratings yet
- CKD Dan DM (Modul 4)Document6 pagesCKD Dan DM (Modul 4)Nurul AwaliahNo ratings yet
- Prevention Strategy of Chronic Kidney Disease Progression inDocument30 pagesPrevention Strategy of Chronic Kidney Disease Progression inAndi Rahmat HidayatNo ratings yet
- Overview of Antidiabetic Drugs: Insulin Hyperglycemic Diabetes MellitusDocument14 pagesOverview of Antidiabetic Drugs: Insulin Hyperglycemic Diabetes Mellitus4760rkNo ratings yet
- DPlanDocument2 pagesDPlanErin Trisha Kristel GaspanNo ratings yet
- RosuvastatinDocument2 pagesRosuvastatinShaira Richelle OmagapNo ratings yet
- CKD SheetDocument4 pagesCKD SheetMomy SutanNo ratings yet
- Glycaemic Control and Blood Glucose Lowering AgentDocument23 pagesGlycaemic Control and Blood Glucose Lowering AgentIrsa SevenfoldismNo ratings yet
- Drug Study #1Document7 pagesDrug Study #1Sarah Kaye BañoNo ratings yet
- Drug Study 2Document5 pagesDrug Study 2Bani Ann Dela CruzNo ratings yet
- Unit 06: Drugs Acting On The Gastrointestinal SystemDocument9 pagesUnit 06: Drugs Acting On The Gastrointestinal SystemDental LecturesMMQNo ratings yet
- Buku CKD ManagementDocument27 pagesBuku CKD ManagementPutri Atthariq IlmiNo ratings yet
- Management of Chronic Kidney Disease: Patient Population: ObjectivesDocument27 pagesManagement of Chronic Kidney Disease: Patient Population: ObjectivesNadya SaptarinaNo ratings yet
- Diabetes Mellitus: Geriatrics Evaluation & ManagementDocument4 pagesDiabetes Mellitus: Geriatrics Evaluation & ManagementAngeles SlzrNo ratings yet
- CKD, Mbbs LectureDocument25 pagesCKD, Mbbs LectureElvis obajeNo ratings yet
- Preventif CKD FinalDocument43 pagesPreventif CKD Finaltika.dyahmustikaNo ratings yet
- Microvascular Complications and Foot Care - Standards of Medical Care in Diabetes22020Document17 pagesMicrovascular Complications and Foot Care - Standards of Medical Care in Diabetes22020Walter Lopez TaboadaNo ratings yet
- 0006F PDFDocument13 pages0006F PDFreioctabianoNo ratings yet
- Leveraging GLP-1 Receptor Agonist Options To Advance Glycemic and Extraglycemic Goals in Type 2 DiabetesDocument34 pagesLeveraging GLP-1 Receptor Agonist Options To Advance Glycemic and Extraglycemic Goals in Type 2 DiabetesMagdy GabrNo ratings yet
- Renal Nutrition (For Non-Renal Dietitians)Document41 pagesRenal Nutrition (For Non-Renal Dietitians)Vaidehi UlaganathanNo ratings yet
- Diabetic Gastroparesis: Pathophysiology, Evaluation and ManagementDocument10 pagesDiabetic Gastroparesis: Pathophysiology, Evaluation and ManagementboomNo ratings yet
- DefisniDocument41 pagesDefisniAzizah MNo ratings yet
- Clinical Case Aki Presentation EportfolioDocument32 pagesClinical Case Aki Presentation Eportfolioapi-463444835No ratings yet
- dm2 Non-InsulinDocument38 pagesdm2 Non-Insulinapi-649066372No ratings yet
- Evaluation of Proteinuria Overview - Epocrates OnlineDocument4 pagesEvaluation of Proteinuria Overview - Epocrates Onlinerey_fremyNo ratings yet
- Drugs Mechanism of Action Indication Contraindication Adverse EffectsDocument2 pagesDrugs Mechanism of Action Indication Contraindication Adverse Effectsisprikitik3No ratings yet
- Trade/Generic Name Classification Action of Medication Dosage/Route/ Frequency Indications For Use (Patient Specific)Document16 pagesTrade/Generic Name Classification Action of Medication Dosage/Route/ Frequency Indications For Use (Patient Specific)lightzapNo ratings yet
- Oral Manifestations of Chronic Kidney Disease-An OverviewDocument4 pagesOral Manifestations of Chronic Kidney Disease-An OverviewrinakartikaNo ratings yet
- Att CKD Oct04Document24 pagesAtt CKD Oct04A9 El-EbidiNo ratings yet
- Mini Case Study RuliuDocument26 pagesMini Case Study Ruliuapi-300681452No ratings yet
- CKDDocument35 pagesCKDgailNo ratings yet
- Medication: Expected Pharmacological Action Therapeutic UseDocument1 pageMedication: Expected Pharmacological Action Therapeutic UseMike EveretteNo ratings yet
- Tatalaksana Diabetes Pada Pelayanan PrimerDocument49 pagesTatalaksana Diabetes Pada Pelayanan PrimerEvri LiaNo ratings yet
- Jurnal CKD FaizDocument12 pagesJurnal CKD FaizToxic idNo ratings yet
- Reviewer Pharmacology FinalsDocument12 pagesReviewer Pharmacology FinalsCherry BoticarioNo ratings yet
- Drug StudyDocument9 pagesDrug StudyComia AltheiaNo ratings yet
- Chronic Kidney DiseaseDocument5 pagesChronic Kidney DiseaseXtelle Casipit0% (1)