Professional Documents
Culture Documents
Heart Rate Variability For The Prediction of Treatment Response in Major Depressive Disorder
Uploaded by
Eden DingOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Heart Rate Variability For The Prediction of Treatment Response in Major Depressive Disorder
Uploaded by
Eden DingCopyright:
Available Formats
MINI REVIEW
published: 30 June 2020
doi: 10.3389/fpsyt.2020.00607
Heart Rate Variability for the
Prediction of Treatment Response
in Major Depressive Disorder
Kwan Woo Choi 1 and Hong Jin Jeon 2*
1 Department of Psychiatry, Korea University College of Medicine, Seoul, South Korea, 2 Department of Psychiatry,
Depression Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, South Korea
Major depressive disorder (MDD) is one of the disabling diseases in the world-wide, and
known to increase cardiac morbidity and mortality. Therefore, previous studies related
heart rate variability (HRV) have been conducted to evaluate and diagnose MDD, and to
predict treatment outcomes in patient with MDD. We reviewed extensively on the previous
peer-reviewed publications associated with this issue, using Pub-Med. In this review
article, we introduce the basic concept of HRV and HRV measures, and present several
Edited by:
J. John Mann, important findings associated with diagnosis and treatment prediction in MDD with using
Columbia University, United States HRV parameters. Furthermore, we discuss the possible underlying mechanism of this
Reviewed by: phenomenon, and suggest several considerations for the future research.
Gianna Sepede,
University of Studies G. d' Annunzio Keywords: heart rate variability, major depressive disorder, antidepressant treatment, treatment, diagnosis
Chieti and Pescara, Italy
Alessandro Del Debbio,
Azienda USL Toscana Nord Ovest,
Italy INTRODUCTION
*Correspondence:
Hong Jin Jeon
Major depressive disorder (MDD) is one of the most disabling conditions, featured by depressive
jeonhj@skku.edu episodes lasting at least two weeks, over changes in mood, cognition, and vegetative symptoms (1).
However, because MDD is a heterogenous condition, and patients with MDD exhibit multiple
Specialty section: variable symptoms, which make the correct diagnosis difficult (2). Furthermore, although
This article was submitted to antidepressant medication has been considered as the first-line treatment for MDD, only 50% of
Mood and Anxiety Disorders, patients are non-responsive to initial treatment, and it is difficult to predict future responsiveness of
a section of the journal MDD at the time of beginning treatment (3). Therefore, it is necessary to develop a more reliable
Frontiers in Psychiatry method to diagnose MDD and predict treatment responsivity in MDD patients.
Received: 17 April 2020 Numerous research findings have proven that major depressive disorder (MDD) is strongly
Accepted: 11 June 2020 associated with elevated risk for the development and progression of cardiovascular diseases (4–13).
Published: 30 June 2020
Autonomic nervous system (ANS) dysfunction is considered one of the pathways linking MDD and
Citation: negative CVD outcomes (14). Heart rate variability (HRV), levels of variability of the heart beat-to-
Choi KW and Jeon HJ (2020) Heart beat interval over time, has been known to provide an index of ANS functioning including the
Rate Variability for the Prediction of
sympathetic and parasympathetic system (15). In this brief review, we aim to describe a clinical
Treatment Response in Major
Depressive Disorder.
overview of the HRV parameters, methodologic issues, and HRV research which found an
Front. Psychiatry 11:607. association between HRV parameters and MDD diagnosis, and between baseline HRV
doi: 10.3389/fpsyt.2020.00607 parameters and MDD treatment responsivity.
Frontiers in Psychiatry | www.frontiersin.org 1 June 2020 | Volume 11 | Article 607
Choi and Jeon HRV for Treatment Prediction in MDD
MATERIALS AND METHODS HEART RATE VARIABILITY PARAMETERS
We performed a brief review of major publication on the HRV is defined as fluctuation of the heart beat interval over time
diagnosis for MDD with using HRV use, and predictive value of (16). Since the heart is dually innervated by the sympathetic and
HRV parameters for treatment response, especially in patients parasympathetic branches of the autonomous nervous system
with MDD. A structured literature search was conducted from the (ANS), subtle moment-to-moment changes in heart rate (HR) are
PubMed data base until March 2020 (with no publication data qualitative indicators of ANS function (17). According to the
limitations) (Arksey and O’Malley, 2005). Search terms and reliable international guidelines, HRV parameters could be
databases were determined in consultation with a health science divided into two domains; frequency domain (spectral analysis)
librarian at Korea University and Samsung Medical Center. and time domain (non-spectral analysis) (Table 1) (15, 18).
Relevant articles which were identified using the following
keywords: “heart rate variability” and “major depressive Time Domain Measures
disorder” and “diagnosis”; “heart rate variability” and “major Time domain HRV features are calculated with simple
depressive disorder” and “treatment”; “heart rate variability” and mathematical methods to measure the amount of variability
“major depressive disorder” and “treatment response”; “heart present in a specific time period in a continuous ECG signal
rate variability” and “depression” and “remission”. The retrieved (19). These parameters are based on the time series of R to R
title and abstracts were investigated for relevance for two interval (RRI) from the ECG signals. The standard deviation of
reviewers (Kwan Woo Choi [KWC], and Hong Jin Jeon [HJJ]) average normal to normal (NN) intervals (SDNN), the root
using the following inclusion criteria: 1) the study focused on mean square of successive differences (RMSSD), and the
heart rate variability as the main outcome; 2) the study mainly percentage of absolute differences in successive NN values
focused on the diagnosis or treatment response of major greater than 50ms (pNN50) are widely utilized as time-domain
depressive disorder (MDD); 3) the population of the study HRV indicators. SDNN is known to reflect both sympathetic and
targeted adult people, who are older than 18 years old; 4) the parasympathetic functioning, whereas RMSSD and pNN50 are
article is written in English. In reviewing abstracts, citations were related to parasympathetic functioning (20–22).
excluded from the review using the following criteria: 1) the study
does not deal with specific HRV parameters; 2) the study was not Frequency Domain Measures
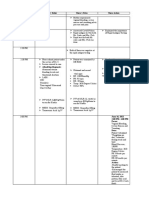
written in English. The initial database search returned 155 Frequency domain provides an assessment of vagal modulation of
database citations. 155 abstracts were selected to review for the RRI, extracted from the ECG. Frequency domain is mostly
inclusion in the scoping review and 27citations qualified for full commonly acquired by fast Fourier transformation to separate RRI
paper review. Following full paper review, seven articles were into characteristic very low frequency (VLF, 0.003–0.04 Hz), low
excluded as they did not meet inclusion criteria. The final set of 13 frequency (LF, 0.04–0.15 Hz), and high frequency (HF, 0.15–0.4
studies included (Figure 1). Hz) band (20). Spectral measures are acquired over different time
intervals (approximately 2.5 to 15 min), depending on the
frequency being analyzed (20). According to previous studies, LF
is influenced by both sympathetic and parasympathetic activities,
and HF is affected by mostly parasympathetic activities (23, 24). LF/
HF ratio is ratio of LF and HF, and it implicates the sympathetic
predominance compared to parasympathetic activities (21, 22).
TABLE 1 | A brief description of the most relevant measures of heart rate
variability.
Parameters Description
Time domain
SDNN SD of the normal to normal intervals
RMSSD Square root of the mean squared difference between
successive RRs
NN50 The numbers of successive RR intervals that differ by more
than 50ms
pNN50 The percentage of NN50
Frequency domain
HF Power band encompassing 0.15–0.4 Hz range
LF Power band encompassing 0.04–0.15 Hz range
VLF Power band encompassing 0.003–0.04 Hz range
LF/HF The ratio between LF and HF
FIGURE 1 | Flow chart of review selection process.
HF, high frequency; LF, low frequency; VLF, very low frequency.
Frontiers in Psychiatry | www.frontiersin.org 2 June 2020 | Volume 11 | Article 607
Choi and Jeon HRV for Treatment Prediction in MDD
HRV FOR THE DIAGNOSIS OF MDD (38, 44). Further studies will be needed to evaluate the
relationship between HF and MDD.
MDD is assoicated with the increased risk of cardiovascular
morbidity and mortality (4, 5), and also known to be associated Low pNN50
with reduced HRV (25, 26). For these reasons, there have been The pNN50 is known to be associated with HF, which reflects the
numerous studies to find the neurobiological biomarkers of activity level of the parasympathetic nervous system (15, 28).
MDD related to HRV parameters (Table 2). There have been several reports which showed reduced pNN50
in patients with MDD compared to HCs (28, 32, 33). Especially,
Increased LF/HF Ratio Ha et al. showed that reduced in pNN50 in the medication-naïve,
Consistently, there have been many reports which showed an and newly diagnosed with elderly MDD patients who were older
increased LF/HF ratio in patients with MDD compared to HCs than 60 years old (33). Choi et al. also revealed a lower value of
(25–28). According to the previous meta-analysis by Kemp et al. pNN50 compared to HCs at the stress phase, and recovery
which compared 673 depressed patients and 407 healthy controls phase (28).
(HCs) with using 18 articles (25), depressed patients without
cardiovascular disease showed reduced time domain HRV, HF
HRV, and increased LF/HF ratio than HCs. Udupa et al. also
found that 40 patients with MDD showed a more increased LF/ BASELINE HRV PARAMETERS FOR THE
HF ratio than 40 age matched HCs (27). More recently, Choi PREDICTION OF TREATMENT RESPONSE
et al. found that patients with MDD showed an elevated LF/HF IN MDD
ratio especially after the stress induction compared HCs (28).
The LF/HF ratio is associated with sympathetic predominance Antidepressants have been utilized as a front-line treatment of
(34), which could be related to the increased sympathetic MDD, whereas only one-third to one-half MDD patients who
modulation or disrupted ANS modulation in MDD. take a complete initial course of antidepressants achieve
remission (45, 46). Whereas there are consistent findings that
Low HF tricyclic antidepressants reduce HRV, it is controversial whether
As well as LF/HF ratio, decreased HF has also been one of the selective serotonin reuptake inhibitors (SSRIs) alters HRV (25,
consistent HRV parameters which were significantly associated 47). Although there have been studies which found increases in
with MDD (25, 29, 30, 35, 36). In one meta-analysis, patients HRV or stability after successful antidepressant treatment in
with MDD had lower resting levels of HRV than HCs (25). patients with MDD (48, 49), there has been paucity of research
According the large-scale prospective Netherland Study of which found specific baseline HRV parameters, which could
Depression and Anxiety (NESDA), Licht et al. also showed predict treatment responsivity in patients with MDD. Table 3
that remitted and current MDD patients had a lower HF summarizes previous HRV findings associated with MDD.
compared to HCs, although they concluded the association Previously, in response to the emotional stimulus, baseline
appeared to be mainly associated with the effect of changes in LF and LF/HF ratio were positively associated with
antidepressants (36). Rottenberg et al. also found significantly the decrease level in MDD symptoms during fluoxetine
reduced HF in patients with MDD, however the overall effect size treatment (50). More recently, Jain et al. found that baseline
was relatively small according to their meta-analysis (29). In VLF was negatively correlated with symptom improvement in
reviewing previous reports, HF could be particularly related with depression (51). Shapiro et al. showed that remitters in MDD
anxious depression. Reduction in HF might have significant had significantly more increased HF, and decreased LF than non-
relations with anxiety according to neurovisceral integration remitters during yoga treatment (52). Choi et al. found that delta
(NVI) model studies (37, 38). Moreover, various anxiety LF/HF ratio (Stress phase–Rest phase), and delta pNN50 (Stress
disorders were associated with reduced HRV (39, 40). Some
investigators found that low HF in MDD is driven or exacerbated
TABLE 3 | Heart rate variability for the prediction of better or worse treatment
by co-occurring anxiety (26, 31, 41, 42). HF is associated with the response in MDD.
parasympathetic tone (43, 44). Relatively high HF is known to
reflect adaptive functioning, and neural activity in the prefrontal HRV measures Related studies
cortex related to emotional, cognitive, and autonomic regulation Baseline LF, LF/HF response to the Fraguas et al. (50) (Fluoxetine
emotional stimuli treatment)
TABLE 2 | Heart rate variability for the diagnosis of major depressive disorder. Baseline VLF Jain et al. (51)
Higher HF, and Lower LF Shapiro et al., (52) (Yoga
Reduced HRV Kemp et al. (25), Kemp and Quintana, 2013 treatment)
Increased LF/HF Udupa et al. (27), Kemp et al. (25), Kemp et al. (26), Choi Higher Delta (Stress–Rest phase) LF/HF Choi et al. (28)
ratio et al. (28) ratio, pNN50
Lower HF Rottenberg (29, 30), Licht et al. (31), Kemp et al. (25) Higher baseline HF Kircanski et al. (31) (Anxious
Lower pNN50 Wang et al. (32), Ha et al. (33), Choi et al. (28) depression)
HF, high frequency; pNN50, the percentage of absolute differences in successive NN HF, high frequency; LF, low frequency; VLF, very low frequency; pNN50, the percentage of
values greater than 50 ms. absolute differences in successive NN values greater than 50 ms.
Frontiers in Psychiatry | www.frontiersin.org 3 June 2020 | Volume 11 | Article 607
Choi and Jeon HRV for Treatment Prediction in MDD
phase–Rest phase) were significantly positively associated with associated with altered cardiac function in MDD patients,
treatment response (after 12 weeks) in patients with MDD (28). specifically for treatment non-responders.
Regarding types of MDD, Kircanski et al. recently showed that
patients with higher HRV, or HF had better treatment outcomes
especially in anxious depression (31). However, in non-anxious
depression, patients with lower HRV had better outcomes (31).
METHODOLOGIC CONSIDERATION
Their study implicates that there might be subtype-specific Although HRV is a non-invasive, pain free, economic and simple
treatment biomarkers in patients with MDD. A similar study. technique and one of the easily accessible modalities measuring
attempted to differentiate treatment response group from non- ANS profiles (18), it is important to consider several important
response group using EEG and HRV (53). However, the potential confounding factors for the future research.
researchers did not predict treatment responsivity in
depression using HRV parameters, while they could predict Time of Measurement
treatment outcome in MDD only using the EEG parameter Due to circadian variation in autonomic cardiac function and
(53). Despite focusing on PTSD diagnosis other than MDD, HRV (64, 65), it should be recommended to evaluate HRV
Minassian et al. showed that high LF/HF ratio (>6.7) before parameters at about the same time of the day. Furthermore,
deployment was significantly associated with post-deployment participants should be recommended to have a normal sleep
post-traumatic stress disorder (PTSD) in active-duty routine, no intense physical training, and no alcohol the day
marines (54). before the measurement (66–70).
Demographic Factors: Age, Gender,
POSSIBLE IMPLICATION Alcohol Use, Smoking and Body Weight
According to the previous research, HRV decreases with aging
Disrupted autonomic function may be regarded as a serious (71), or HRV parameters changes with a trend toward a decrease
pathophysiological candidate for elevated risk of cardiovascular in autonomous cardiac function (72, 73). HRV parameters are also
mortality in patients with MDD. Thayer and Lane suggested a known to have different profiles between male and female
neurovisceral integration (NVI) model in the context of population (71, 72, 74). In the recent meta-analysis, Koenig and
emotional regulation (55). According to the NVI model, Thayer showed that females had a significantly lower mean RR
decreased activation of the central autonomic network (CAN) interval, lower SDNN, lower LF power, lower LF/HF ratio and
may affect the decreased level of HRV. CAN is known to be the greater HF power, which implied more increased parasympathetic
constellation of brain areas responsible for the neurobiological activity than males (74). Alcohol use is also associated with altered
and physiological regulation of affect and attendant behaviors. HRV parameters (69, 70). According to the meta-analytic study by
According to the NVI modes, the CAN modulates the Quintana et al., alcohol dependence patients showed reduced
neuroendocrine, visceromotor, and even behavioral systems HRV compared to nondependent controls (69). On the
(37, 56). Furthermore, the CAN has connection with the contrary, the researchers found that habitual, and moderate
sinoatrial node of the heart via the stellate ganglion through alcohol drinkers showed increased levels of HF compared to
vagus nerve (57). Therefore, HRV is a widely utilized biomarkers nonhabitual drinkers in their other original study (70). It might
of CAN regulatory functioning and considered an informative be associated with a J-shaped curve that moderate alcohol use is
indicator of brain–body integration, and concomitant health or related to a protective effect compared to alcohol dependence or
pathological states (58, 59). CAN is known to consist with the abstinence (69, 70). Smoking is also associated with reduced HRV
anterior cingulate cortex, insular cortex, ventromedial prefrontal levels according to previous studies (75, 76). Recent studies also
cortex, and the various subcortical structures such as amygdala, reported that even e-cigarette use decreased HF component, and
hypothalamus, periaqueductal gray matter, parabrachial plexus, increased LF and LF/HF ratio compared to controls (77, 78).
and etc. (55–57). Both direct and indirect links between frontal Weight, height, and waist-to-hip ratio are also considered as
cortex and autonomic motor circuits have been known to be potential confounding factors (79). Yi et al. recently showed that
responsible for both the sympathetic and parasympathetic effects waist-to-hip ratio was more strongly correlated with HRV indices
on the heart (21, 37, 56). Previous brain imaging studies found and more likely predict reduced HRV compared to body mass
that brain regions such as right superior prefrontal, right index (BMI), and percentage of body fat mass. However, although
dorsolateral prefrontal, right dorsolateral prefrontal and left the previous study indicated no correlation between HRV and
rostral anterior cingulate cortices showed significantly BMI (80), BMI should be considered as one of the confounding
functional decrease concomitantly with decreased HRV (37, factors since it is still controversial (79, 81). Therefore, above-
60–62). According to the Thayer and Lane, prefrontal top- mentioned demographic factors should be considered to conduct
down inhibitory and regulatory processes might influence on future research related to HRV.
subcortical emotion regulation centers (37). MDD can be related
to the prefrontal hypoactivation and the loss of inhibitory neural Antidepressant Medication
functioning with poor affective information processing and Previous studies suggest HRV alterations related to
regulation (21, 37, 55, 56, 63). Prefrontal hypoactivity might be antidepressant medication. According to 2010 Kemp et al.’s
Frontiers in Psychiatry | www.frontiersin.org 4 June 2020 | Volume 11 | Article 607
Choi and Jeon HRV for Treatment Prediction in MDD
meta-analysis, they showed that tricyclic antidepressant (TCA) AUTHOR CONTRIBUTIONS
decreased HRV whereas SSRI nefazedone, and mirtazapine did
not have any significant effect on HRV (25). On the contrary, KC and HJ: Writing and reviewing the whole manuscript.
their large-scale longitudinal study showed that SSRI, and
serotonin and norepinephrine reuptake inhibitors decreased
HRV parameters (82). More recently, without TCA and
clozapine, there were no significant effect on HRV parameters
ACKNOWLEDGMENTS
associated with SSRI treatment (83). Futures studies will be This research was supported by the Original Technology
needed to clarify relationships between specific treatment Research Program for Brain Science through the National
regimen and HRV parameters. Research Foundation of Korea (NRF) funded by the Ministry
of Education, Science and Technology (No. NRF-2016M3
C7A1947307; PI HJ), and by the Bio & Medical Technology
CONCLUSION Development Program of the NRF funded by the Korean
government, MSIT (No. NRF-2017M3A9F1027323; PI HJ). This
In conclusion, there have been several attempts to diagnose research was also supported by Healthcare AI Convergence
MDD, and to predict treatment responsiveness in patients with Research & Development Program through the National IT
MDD with using baseline HRV parameters. We should consider Industry Promotion Agency of Korea (NIPA) funded by the
methodological issues and potential confounding factors to Ministry of Science and ICT(No. S1601-20-1041). This work
examine relationships between MDD and HRV parameters. was supported and funded by Korea University (No. K1922891;
Furthermore, it will be needed to have larger sample size, KWC). The NRF of Korea, NIPA and Korea University had no
prospective and longitudinal study design, and related other further role in study design; collection, analysis, and interpretation
regimen such as neuroimaging, inflammatory markers, and so of data; writing of the report; or in the decision to submit the
on for the more refined future research. study for publication.
REFERENCES 12. Penninx BW, Beekman AT, Honig A, Deeg DJ, Schoevers RA, van Eijk JT,
et al. Depression and cardiac mortality: results from a community-based
1. American Psychiatric Association. Diagnostic and Statistical Manual of longitudinal study. Arch Gen Psychiatry (2001) 58:221–7. doi: 10.1001/
Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association archpsyc.58.3.221
(2013). 13. Zellweger MJ, Osterwalder RH, Langewitz W, Pfisterer ME. Coronary artery
2. Baldessarini RJ, Forte A, Selle V, Sim K, Tondo L, Undurraga J, et al. disease and depression. Eur Heart J (2004) 25:3–9. doi: 10.1016/j.ehj.2003.09.009
Morbidity in Depressive Disorders. Psychother Psychosom (2017) 86:65–72. 14. Stapelberg NJ, Hamilton-Craig I, Neumann DL, Shum DH, McConnell H.
doi: 10.1159/000448661 Mind and heart: heart rate variability in major depressive disorder and
3. Cleare A, Pariante CM, Young AH, Anderson IM, Christmas D, Cowen PJ, coronary heart disease - a review and recommendations. Aust N Z J
et al. Evidence-based guidelines for treating depressive disorders with Psychiatry (2012) 46:946–57. doi: 10.1177/0004867412444624
antidepressants: A revision of the 2008 British Association for 15. Malik M. Heart rate variability. Standards of measurement, physiological
Psychopharmacology guidelines. J Psychopharmacol (2015) 29:459–525. interpretation, and clinical use. Task Force of the European Society of
doi: 10.1177/0269881115581093 C a r d io l og y a n d th e N o r th Am e ri c a n S oc i et y o f P a c i n g a n d
4. Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for Electrophysiology. Eur Heart J (1996) 17:354–81.
mortality in patients with coronary heart disease: a meta-analysis. Psychosom 16. Roy-Byrne PP, Stang P, Wittchen HU, Ustun B, Walters EE, Kessler RC.
Med (2004) 66:802–13. doi: 10.1097/01.psy.0000146332.53619.b2 Lifetime panic-depression comorbidity in the National Comorbidity Survey.
5. Nicholson A, Kuper H, Hemingway H. Depression as an aetiologic and Association with symptoms, impairment, course and help-seeking. Br J
prognostic factor in coronary heart disease: a meta-analysis of 6362 events Psychiatry (2000) 176:229–35. doi: 10.1192/bjp.176.3.229
among 146 538 participants in 54 observational studies. Eur Heart J (2006) 17. Bilchick KC, Berger RD. Heart rate variability. J Cardiovasc Electrophysiol
27:2763–74. doi: 10.1093/eurheartj/ehl338 (2006) 17:691–4. doi: 10.1111/j.1540-8167.2006.00501.x
6. Barefoot JC, Schroll M. Symptoms of depression, acute myocardial infarction, 18. Laborde S, Mosley E, Thayer JF. Heart Rate Variability and Cardiac Vagal
and total mortality in a community sample. Circulation (1996) 93:1976–80. Tone in Psychophysiological Research - Recommendations for Experiment
doi: 10.1161/01.cir.93.11.1976 Planning, Data Analysis, and Data Reporting. Front Psychol (2017) 8:213.
7. Carney RM, Blumenthal JA, Catellier D, Freedland KE, Berkman LF, Watkins LL, doi: 10.3389/fpsyg.2017.00213
et al. Depression as a risk factor for mortality after acute myocardial infarction. Am 19. Sgoifo A, Carnevali L, Alfonso Mde L, Amore M. Autonomic dysfunction and
J Cardiol (2003) 92:1277–81. doi: 10.1016/j.amjcard.2003.08.007 heart rate variability in depression. Stress (2015) 18:343–52. doi: 10.3109/
8. Frasure-Smith N, Lesperance F, Talajic M. Depression and 18-month 10253890.2015.1045868
prognosis after myocardial infarction. Circulation (1995) 91:999–1005. 20. Kidwell M, Ellenbroek BA. Heart and soul: heart rate variability and major
doi: 10.1161/01.cir.91.4.999 depression. Behav Pharmacol (2018) 29:152–64. doi: 10.1097/
9. Freedland KE, Rich MW, Skala JA, Carney RM, Davila-Roman VG, Jaffe AS. FBP.0000000000000387
Prevalence of depression in hospitalized patients with congestive heart failure. 21. Thayer JF, Yamamoto SS, Brosschot JF. The relationship of autonomic
Psychosom Med (2003) 65:119–28. doi: 10.1097/01.psy.0000038938.67401.85 imbalance, heart rate variability and cardiovascular disease risk factors. Int J
10. Glassman AH. Depression and cardiovascular comorbidity. Dialogues Clin Cardiol (2010) 141:122–31. doi: 10.1016/j.ijcard.2009.09.543
Neurosci (2007) 9:9–17. 22. Kuang D, Yang R, Chen X, Lao G, Wu F, Huang X, et al. Depression
11. Lett HS, Blumenthal JA, Babyak MA, Sherwood A, Strauman T, Robins C, recognition according to heart rate variability using Bayesian Networks.
et al. Depression as a risk factor for coronary artery disease: evidence, J Psychiatr Res (2017) 95:282–7. doi: 10.1016/j.jpsychires.2017.09.012
mechanisms, and treatment. Psychosom Med (2004) 66:305–15. 23. Akselrod S, Gordon D, Ubel FA, Shannon DC, Berger AC, Cohen RJ. Power
doi: 10.1097/01.psy.0000126207.43307.c0 spectrum analysis of heart rate fluctuation: a quantitative probe of beat-to-
Frontiers in Psychiatry | www.frontiersin.org 5 June 2020 | Volume 11 | Article 607
Choi and Jeon HRV for Treatment Prediction in MDD
beat cardiovascular control. Science (1981) 213:220–2. doi: 10.1126/ 43. Berntson GG, Bigger JTJr., Eckberg DL, Grossman P, Kaufmann PG, Malik M,
science.6166045 et al. Heart rate variability: origins, methods, and interpretive caveats.
24. Billman GE. The LF/HF ratio does not accurately measure cardiac sympatho- Psychophysiology (1997) 34:623–48. doi: 10.1111/j.1469-8986.1997.tb02140.x
vagal balance. Front Physiol (2013) 4:26. doi: 10.3389/fphys.2013.00026 44. Porges SW. Orienting in a defensive world: mammalian modifications of our
25. Kemp AH, Quintana DS, Gray MA, Felmingham KL, Brown K, Gatt JM. evolutionary heritage. A Polyvagal Theory. Psychophysiology (1995) 32:301–
Impact of depression and antidepressant treatment on heart rate variability: a 18. doi: 10.1111/j.1469-8986.1995.tb01213.x
review and meta-analysis. Biol Psychiatry (2010) 67:1067–74. doi: 10.1016/ 45. Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, et al.
j.biopsych.2009.12.012 Evaluation of outcomes with citalopram for depression using measurement-
26. Kemp AH, Quintana DS, Felmingham KL, Matthews S, Jelinek HF. based care in STAR*D: implications for clinical practice. Am J Psychiatry
Depression, comorbid anxiety disorders, and heart rate variability in (2006) 163:28–40. doi: 10.1176/appi.ajp.163.1.28
physically healthy, unmedicated patients: implications for cardiovascular 46. Saveanu R, Etkin A, Duchemin AM, Goldstein-Piekarski A, Gyurak A,
risk. PloS One (2012) 7:e30777. doi: 10.1371/journal.pone.0030777 Debattista C, et al. The international Study to Predict Optimized Treatment
27. Udupa K, Sathyaprabha TN, Thirthalli J, Kishore KR, Lavekar GS, Raju TR, in Depression (iSPOT-D): outcomes from the acute phase of antidepressant
et al. Alteration of cardiac autonomic functions in patients with major treatment. J Psychiatr Res (2015) 61:1–12. doi: 10.1016/j.jpsychires.
depression: a study using heart rate variability measures. J Affect Disord 2014.12.018
(2007) 100:137–41. doi: 10.1016/j.jad.2006.10.007 47. Licht CM, de Geus EJ, van Dyck R, Penninx BW. Longitudinal evidence for
28. Choi KW, Jang EH, Kim AY, Fava M, Mischoulon D, Papakostas GI, et al. unfavorable effects of antidepressants on heart rate variability. Biol Psychiatry
Heart rate variability for treatment response between patients with major (2010) 68:861–8. doi: 10.1016/j.biopsych.2010.06.032
depressive disorder versus panic disorder: A 12-week follow-up study. J Affect 48. Balogh S, Fitzpatrick DF, Hendricks SE, Paige SR. Increases in heart rate
Disord (2019) 246:157–65. doi: 10.1016/j.jad.2018.12.048 variability with successful treatment in patients with major depressive
29. Rottenberg J. Cardiac vagal control in depression: a critical analysis. Biol disorder. Psychopharmacol Bull (1993) 29:201–6.
Psychol (2007) 74:200–11. doi: 10.1016/j.biopsycho.2005.08.010 49. Glassman AH, Bigger JT, Gaffney M, Van Zyl LT. Heart rate variability in
30. Rottenberg J, Wilhelm FH, Gross JJ, Gotlib IH. Respiratory sinus arrhythmia acute coronary syndrome patients with major depression: influence of
as a predictor of outcome in major depressive disorder. J Affect Disord (2002) sertraline and mood improvement. Arch Gen Psychiatry (2007) 64:1025–31.
71:265–72. doi: 10.1016/s0165-0327(01)00406-2 doi: 10.1001/archpsyc.64.9.1025
31. Kircanski K, Williams LM, Gotlib IH. Heart rate variability as a biomarker of 50. Fraguas RJr., Marci C, Fava M, Iosifescu DV, Bankier B, Loh R, et al.
anxious depression response to antidepressant medication. Depress Anxiety Autonomic reactivity to induced emotion as potential predictor of response
(2019) 36:63–71. doi: 10.1002/da.22843 to antidepressant treatment. Psychiatry Res (2007) 151:169–72. doi: 10.1016/
32. Wang Y, Zhao X, O’Neil A, Turner A, Liu X, Berk M. Altered cardiac j.psychres.2006.08.008
autonomic nervous function in depression. BMC Psychiatry (2013) 13:187. 51. Jain FA, Cook IA, Leuchter AF, Hunter AM, Davydov DM, Ottaviani C, et al.
doi: 10.1186/1471-244X-13-187 Heart rate variability and treatment outcome in major depression: a pilot study. Int
33. Ha JH, Park S, Yoon D, Kim B. Short-term heart rate variability in older J Psychophysiol (2014) 93:204–10. doi: 10.1016/j.ijpsycho.2014.04.006
patients with newly diagnosed depression. Psychiatry Res (2015) 226:484–8. 52. Shapiro D, Cook IA, Davydov DM, Ottaviani C, Leuchter AF, Abrams M.
doi: 10.1016/j.psychres.2015.02.005 Yoga as a complementary treatment of depression: effects of traits and moods
34. Reyes del Paso GA, Langewitz W, Mulder LJ, van Roon A, Duschek S. The on treatment outcome. Evid Based Complement Alternat Med (2007) 4:493–
utility of low frequency heart rate variability as an index of sympathetic 502. doi: 10.1093/ecam/nel114
cardiac tone: a review with emphasis on a reanalysis of previous studies. 53. Pawlowski MA, Gazea M, Wollweber B, Dresler M, Holsboer F, Keck ME,
Psychophysiology (2013) 50:477–87. doi: 10.1111/psyp.12027 et al. Heart rate variability and cordance in rapid eye movement sleep as
35. Rottenberg J, Salomon K, Gross JJ, Gotlib IH. Vagal withdrawal to a sad film biomarkers of depression and treatment response. J Psychiatr Res (2017)
predicts subsequent recovery from depression. Psychophysiology (2005) 92:64–73. doi: 10.1016/j.jpsychires.2017.03.026
42:277–81. doi: 10.1111/j.1469-8986.2005.00289.x 54. Minassian A, Maihofer AX, Baker DG, Nievergelt CM, Geyer MA, Risbrough
36. Licht CM, de Geus EJ, Zitman FG, Hoogendijk WJ, van Dyck R, Penninx BW. VB, et al. Association of Predeployment Heart Rate Variability With Risk of
Association between major depressive disorder and heart rate variability in the Postdeployment Posttraumatic Stress Disorder in Active-Duty Marines.
Netherlands Study of Depression and Anxiety (NESDA). Arch Gen Psychiatry JAMA Psychiatry (2015) 72:979–86. doi: 10.1001/jamapsychiatry.2015.0922
(2008) 65:1358–67. doi: 10.1001/archpsyc.65.12.1358 55. Thayer JF. Lane RD. A model of neurovisceral integration in emotion
37. Thayer JF, Lane RD. Claude Bernard and the heart-brain connection: further regulation and dysregulation. J Affect Disord (2000) 61:201–16. doi:
elaboration of a model of neurovisceral integration. Neurosci Biobehav Rev 10.1016/S0165-0327(00)00338-4
(2009) 33:81–8. doi: 10.1016/j.neubiorev.2008.08.004 56. Smith R, Thayer JF, Khalsa SS, Lane RD. The hierarchical basis of
38. Thayer JF, Ahs F, Fredrikson M, Sollers JJ. 3rd, Wager TD. A meta-analysis of neurovisceral integration. Neurosci Biobehav Rev (2017) 75:274–96.
heart rate variability and neuroimaging studies: implications for heart rate doi: 10.1016/j.neubiorev.2017.02.003
variability as a marker of stress and health. Neurosci Biobehav Rev (2012) 57. Benarroch EE. The central autonomic network: functional organization,
36:747–56. doi: 10.1016/j.neubiorev.2011.11.009 dysfunction, and perspective. Mayo Clin Proc (1993) 68:988–1001. doi:
39. Licht CM, de Geus EJ, van Dyck R, Penninx BW. Association between anxiety 10.1016/S0025-6196(12)62272-1
disorders and heart rate variability in The Netherlands Study of Depression 58. Beissner F, Meissner K, Bar KJ, Napadow V. The autonomic brain: an
and Anxiety (NESDA). Psychosom Med (2009) 71:508–18. doi: 10.1097/ activation likelihood estimation meta-analysis for central processing of
PSY.0b013e3181a292a6 autonomic function. J Neurosci (2013) 33:10503–11. doi: 10.1523/
40. Chalmers JA, Quintana DS, Abbott MJ, Kemp AH. Anxiety Disorders are JNEUROSCI.1103-13.2013
Associated with Reduced Heart Rate Variability: A Meta-Analysis. Front 59. McCraty R, Shaffer F. Heart Rate Variability: New Perspectives on
Psychiatry (2014) 5:80. doi: 10.3389/fpsyt.2014.00080 Physiological Mechanisms, Assessment of Self-regulatory Capacity, and
41. Chang HA, Chang CC, Tzeng NS, Kuo TB, Lu RB, Huang SY. Generalized Health risk. Glob Adv Health Med (2015) 4:46–61. doi: 10.7453/
anxiety disorder, comorbid major depression and heart rate variability: a case- gahmj.2014.073
control study in taiwan. Psychiatry Invest (2013) 10:326–35. doi: 10.4306/ 60. Gianaros PJ, Van Der Veen FM, Jennings JR. Regional cerebral blood flow
pi.2013.10.4.326 correlates with heart period and high-frequency heart period variability
42. Watkins LL, Grossman P, Krishnan R, Blumenthal JA. Anxiety reduces during working-memory tasks: Implications for the cortical and subcortical
baroreflex cardiac control in older adults with major depression. Psychosom regulation of cardiac autonomic activity. Psychophysiology (2004) 41:521–30.
Med (1999) 61:334–40. doi: 10.1097/00006842-199905000-00012 doi: 10.1111/1469-8986.2004.00179.x
Frontiers in Psychiatry | www.frontiersin.org 6 June 2020 | Volume 11 | Article 607
Choi and Jeon HRV for Treatment Prediction in MDD
61. Lane RD. Neural substrates of implicit and explicit emotional processes: a 75. Sjoberg N, Saint DA. A single 4 mg dose of nicotine decreases heart rate
unifying framework for psychosomatic medicine. Psychosom Med (2008) variability in healthy nonsmokers: implications for smoking cessation
70:214–31. doi: 10.1097/PSY.0b013e3181647e44 programs. Nicotine Tob Res (2011) 13:369–72. doi: 10.1093/ntr/ntr004
62. Lane RD, McRae K, Reiman EM, Chen K, Ahern GL, Thayer JF. Neural 76. Hayano J, Yamada M, Sakakibara Y, Fujinami T, Yokoyama K, Watanabe Y,
correlates of heart rate variability during emotion. Neuroimage (2009) 44:213– et al. Short- and long-term effects of cigarette smoking on heart rate
22. doi: 10.1016/j.neuroimage.2008.07.056 variability. Am J Cardiol (1990) 65:84–8. doi: 10.1016/0002-9149(90)90030-5
63. Beauchaine TP, Thayer JF. Heart rate variability as a transdiagnostic 77. Moheimani RS, Bhetraratana M, Peters KM, Yang BK, Yin F, Gornbein J, et al.
biomarker of psychopathology. Int J Psychophysiol (2015) 98:338–50. Sympathomimetic Effects of Acute E-Cigarette Use: Role of Nicotine and
doi: 10.1016/j.ijpsycho.2015.08.004 Non-Nicotine Constituents. J Am Heart Assoc (2017) 6(9):e006579.
64. van Eekelen AP, Houtveen JH, Kerkhof GA. Circadian variation in cardiac doi: 10.1161/JAHA.117.006579
autonomic activity: reactivity measurements to different types of stressors. 78. Moheimani RS, Bhetraratana M, Yin F, Peters KM, Gornbein J, Araujo JA,
Chronobiol Int (2004) 21:107–29. doi: 10.1081/cbi-120027983 et al. Increased Cardiac Sympathetic Activity and Oxidative Stress in Habitual
65. Massin MM, Maeyns K, Withofs N, Ravet F, Gerard P. Circadian rhythm of Electronic Cigarette Users: Implications for Cardiovascular Risk. JAMA
heart rate and heart rate variability. Arch Dis Child (2000) 83:179–82. Cardiol (2017) 2:278–84. doi: 10.1001/jamacardio.2016.5303
doi: 10.1136/adc.83.2.179 79. Yi SH, Lee K, Shin DG, Kim JS, Kim HC. Differential association of adiposity
66. Stein PK, Pu Y. Heart rate variability, sleep and sleep disorders. Sleep Med Rev measures with heart rate variability measures in Koreans. Yonsei Med J (2013)
(2012) 16:47–66. doi: 10.1016/j.smrv.2011.02.005 54:55–61. doi: 10.3349/ymj.2013.54.1.55
67. Stanley J, Peake JM, Buchheit M. Cardiac parasympathetic reactivation 80. Antelmi I, de Paula RS, Shinzato AR, Peres CA, Mansur AJ, Grupi CJ.
following exercise: implications for training prescription. Sports Med (2013) Influence of age, gender, body mass index, and functional capacity on heart
43:1259–77. doi: 10.1007/s40279-013-0083-4 rate variability in a cohort of subjects without heart disease. Am J Cardiol
68. Quintana DS, Heathers JA. Considerations in the assessment of heart rate (2004) 93:381–5. doi: 10.1016/j.amjcard.2003.09.065
variability in biobehavioral research. Front Psychol (2014) 5:805. 81. Gulgun M, Fidanci MK. Body mass index may be an influential factor in heart rate
doi: 10.3389/fpsyg.2014.00805 variability. Rev Port Cardiol (2015) 34:789. doi: 10.1016/j.repc.2015.03.029
69. Quintana DS, McGregor IS, Guastella AJ, Malhi GS, Kemp AH. A meta- 82. Kemp AH, Brunoni AR, Santos IS, Nunes MA, Dantas EM, Carvalho de
analysis on the impact of alcohol dependence on short-term resting-state Figueiredo R, et al. Effects of depression, anxiety, comorbidity, and
heart rate variability: implications for cardiovascular risk. Alcohol Clin Exp Res antidepressants on resting-state heart rate and its variability: an ELSA-
(2013) 37 Suppl 1:E23–9. doi: 10.1111/j.1530-0277.2012.01913.x Brasil cohort baseline study. Am J Psychiatry (2014) 171:1328–34.
70. Quintana DS, Guastella AJ, McGregor IS, Hickie IB, Kemp AH. Moderate doi: 10.1176/appi.ajp.2014.13121605
alcohol intake is related to increased heart rate variability in young adults: 83. Alvares GA, Quintana DS, Hickie IB, Guastella AJ. Autonomic nervous
implications for health and well-being. Psychophysiology (2013) 50:1202–8. system dysfunction in psychiatric disorders and the impact of psychotropic
doi: 10.1111/psyp.12134 medications: a systematic review and meta-analysis. J Psychiatry Neurosci
71. Umetani K, Singer DH, McCraty R, Atkinson M. Twenty-four hour time domain (2016) 41:89–104. doi: 10.1503/jpn.140217
heart rate variability and heart rate: relations to age and gender over nine decades.
J Am Coll Cardiol (1998) 31:593–601. doi: 10.1016/s0735-1097(97)00554-8 Conflict of Interest: The authors declare that the research was conducted in the
72. Kuo TB, Lin T, Yang CC, Li CL, Chen CF, Chou P. Effect of aging on gender absence of any commercial or financial relationships that could be construed as a
differences in neural control of heart rate. Am J Physiol (1999) 277:H2233–9. potential conflict of interest.
doi: 10.1152/ajpheart.1999.277.6.H2233
73. Fukusaki C, Kawakubo K, Yamamoto Y. Assessment of the primary effect of Copyright © 2020 Choi and Jeon. This is an open-access article distributed under the
aging on heart rate variability in humans. Clin Auton Res (2000) 10:123–30. terms of the Creative Commons Attribution License (CC BY). The use, distribution or
doi: 10.1007/bf02278016 reproduction in other forums is permitted, provided the original author(s) and the
74. Koenig J, Thayer JF. Sex differences in healthy human heart rate variability: A copyright owner(s) are credited and that the original publication in this journal is
meta-analysis. Neurosci Biobehav Rev (2016) 64:288–310. doi: 10.1016/ cited, in accordance with accepted academic practice. No use, distribution or
j.neubiorev.2016.03.007 reproduction is permitted which does not comply with these terms.
Frontiers in Psychiatry | www.frontiersin.org 7 June 2020 | Volume 11 | Article 607
You might also like
- Heart Rate Variability For Treatment Response Between Patients With Major Depressive Disorder Versus Panic Disorder A 12-Week Follow-Up StudyDocument9 pagesHeart Rate Variability For Treatment Response Between Patients With Major Depressive Disorder Versus Panic Disorder A 12-Week Follow-Up StudyEden DingNo ratings yet
- Zhang 2020Document10 pagesZhang 2020Isa GuzmánNo ratings yet
- Journal of Psychiatric Research 141 (2021) 167-175Document9 pagesJournal of Psychiatric Research 141 (2021) 167-175DavidNo ratings yet
- 1 s2.0 S2213158219303511 MainDocument8 pages1 s2.0 S2213158219303511 MainGilbert SihombingNo ratings yet
- University of Groningen: 10.1016/j.jad.2012.07.036Document8 pagesUniversity of Groningen: 10.1016/j.jad.2012.07.036bellaNo ratings yet
- Fneur 11 00028Document6 pagesFneur 11 00028Farimah AbbaspourNo ratings yet
- 02 Attention-Based CNN and LSTM For Short-Term Detection of Mood DisordersDocument29 pages02 Attention-Based CNN and LSTM For Short-Term Detection of Mood DisordersTauqeer AhmedNo ratings yet
- 2018 - NATURE - Automatic Detection of Major Depressive Disorder Using Electrodermal ActivityDocument9 pages2018 - NATURE - Automatic Detection of Major Depressive Disorder Using Electrodermal ActivityPriya KumariNo ratings yet
- Factors Affecting Post-StrokeDocument12 pagesFactors Affecting Post-StrokeSitti Rosdiana YahyaNo ratings yet
- Neurological Soft Signs: A Further Step in The Diagnosis of Bipolar-I DisorderDocument6 pagesNeurological Soft Signs: A Further Step in The Diagnosis of Bipolar-I DisorderMonica TeletinNo ratings yet
- Jiwa 3Document15 pagesJiwa 3Tri WidiantoNo ratings yet
- ADHD and BPD Treatment with MethylphenidateDocument11 pagesADHD and BPD Treatment with MethylphenidatePaula TrindadeNo ratings yet
- Fneur 10 01411Document14 pagesFneur 10 01411Kandi IssayaNo ratings yet
- Anhedonia and Reward Circuit Connectivity Distinguish Nonresponders From Responders To Dorsomedial Prefrontal Repetitive Transcranial Magnetic Stimulation in Major DepressionDocument10 pagesAnhedonia and Reward Circuit Connectivity Distinguish Nonresponders From Responders To Dorsomedial Prefrontal Repetitive Transcranial Magnetic Stimulation in Major DepressionKhory Aurora BertyNo ratings yet
- Cognitive Functioning As Predictor and Marker of Response To - 2022 - General HoDocument14 pagesCognitive Functioning As Predictor and Marker of Response To - 2022 - General Hojingwen2002No ratings yet
- A Systematic Review and Meta Analysis On The Effects ofDocument15 pagesA Systematic Review and Meta Analysis On The Effects ofAlan EhrichNo ratings yet
- Latest findings on brain imaging in borderline personality disorderDocument10 pagesLatest findings on brain imaging in borderline personality disorderme13No ratings yet
- Assessing Mood Symptoms Through Heartbeat Dynamics A - 2017 - Journal of PsychiDocument10 pagesAssessing Mood Symptoms Through Heartbeat Dynamics A - 2017 - Journal of PsychiEden DingNo ratings yet
- Zjrms in - Press in - Press 962841 PDFDocument6 pagesZjrms in - Press in - Press 962841 PDFnelaNo ratings yet
- 2018 Article 113Document6 pages2018 Article 113Fernanda NascimentoNo ratings yet
- Factors Associated With Post-Stroke Depression and Fatigue: Lesion Location and Coping StylesDocument8 pagesFactors Associated With Post-Stroke Depression and Fatigue: Lesion Location and Coping StylesnurhayanaNo ratings yet
- Applsci 12 01409Document14 pagesApplsci 12 01409Antonio FernandezNo ratings yet
- Toc CBTDocument9 pagesToc CBTRaquel IsahíNo ratings yet
- Arnaldi 2017Document10 pagesArnaldi 2017Jaime AguilarNo ratings yet
- 10.1002@acn3.51102Document12 pages10.1002@acn3.51102chemistpl420No ratings yet
- 10 1016@j Ijcard 2016 06 057Document6 pages10 1016@j Ijcard 2016 06 057AlejandraNo ratings yet
- Lange 2017Document8 pagesLange 2017Rodrigo AdryNo ratings yet
- S2211034821001711Document9 pagesS2211034821001711loloasbNo ratings yet
- Journal of A Ffective Disorders: Research PaperDocument7 pagesJournal of A Ffective Disorders: Research PaperLast ChildNo ratings yet
- Comparing Mindfulness Based Cognitive THDocument5 pagesComparing Mindfulness Based Cognitive THolgasacristan316No ratings yet
- AwalDocument5 pagesAwal0625Adinda Salsa AmiraNo ratings yet
- 17 J.jpsychores.2019.109908Document7 pages17 J.jpsychores.2019.109908Stardya RuntuwarowNo ratings yet
- Post-Stroke Mood and Emotional Disturbances: Pharmacological Therapy Based On MechanismsDocument12 pagesPost-Stroke Mood and Emotional Disturbances: Pharmacological Therapy Based On MechanismsScribdMeUpNo ratings yet
- TDCS and MS (Fatigue Depens On The Test)Document13 pagesTDCS and MS (Fatigue Depens On The Test)Silvia OliverNo ratings yet
- Zhou 2020Document8 pagesZhou 2020Rosalía PattyNo ratings yet
- Mania Associated With Antidepressant Treatment: Comprehensive Meta-Analytic ReviewDocument12 pagesMania Associated With Antidepressant Treatment: Comprehensive Meta-Analytic ReviewFiqih IbrahimNo ratings yet
- Abbass 2021Document9 pagesAbbass 2021Nerdi FlandersNo ratings yet
- PNES ClinicalApproachesDocument19 pagesPNES ClinicalApproachesClaudiaNo ratings yet
- Anxiete Et Depression Chez Les Patients Hospitalises en CardiologieDocument6 pagesAnxiete Et Depression Chez Les Patients Hospitalises en CardiologieIJAR JOURNALNo ratings yet
- A Multi-Method Assessment of Attentional Processes in Chronic, Treatment-Resistant Depression Mira Cladder-Micus A, E, - , Janna N. VrijsDocument9 pagesA Multi-Method Assessment of Attentional Processes in Chronic, Treatment-Resistant Depression Mira Cladder-Micus A, E, - , Janna N. VrijsIsabelaValeria Idrovo-LuqueNo ratings yet
- Jamapsychiatry Lundberg 2022 Oi 220078 1675180162.82637Document9 pagesJamapsychiatry Lundberg 2022 Oi 220078 1675180162.82637Pedro IborraNo ratings yet
- Association of Post Stroke Depression With Social Factors, Insomnia, and Neurological Status in Chinese Elderly PopulationDocument7 pagesAssociation of Post Stroke Depression With Social Factors, Insomnia, and Neurological Status in Chinese Elderly Populationsri mulyaniNo ratings yet
- Mp201672a MolekularDocument9 pagesMp201672a MolekularNadia OktarinaNo ratings yet
- Depresión, PronosticoDocument17 pagesDepresión, PronosticoEduardNo ratings yet
- Medicine: Pharmacological and Psychotherapeutic Interventions For Management of Poststroke DepressionDocument5 pagesMedicine: Pharmacological and Psychotherapeutic Interventions For Management of Poststroke DepressionaditNo ratings yet
- Ratio of MBDNF To proBDNF For Differential Diagnosis of Major Depressive Disorder and Bipolar DepressionDocument10 pagesRatio of MBDNF To proBDNF For Differential Diagnosis of Major Depressive Disorder and Bipolar DepressionJackyDanielsNo ratings yet
- Seeing Gray When Feeling Blue? Depression Can Be Measured in The Eye of The DiseasedDocument4 pagesSeeing Gray When Feeling Blue? Depression Can Be Measured in The Eye of The DiseasedguttersniperNo ratings yet
- Relationship of DepressionDocument12 pagesRelationship of DepressionFlorin TudoseNo ratings yet
- Rebt Vs CT Vs Med in DepressionDocument19 pagesRebt Vs CT Vs Med in DepressionPaula StroianNo ratings yet
- Evidence-Based Guideline: Treatment of Painful Diabetic NeuropathyDocument11 pagesEvidence-Based Guideline: Treatment of Painful Diabetic NeuropathyTriNo ratings yet
- Depresia CazDocument19 pagesDepresia CazBetu SasuNo ratings yet
- Music Therapy PDFDocument8 pagesMusic Therapy PDFRamo123No ratings yet
- Estatinas y DepresiónDocument16 pagesEstatinas y DepresiónCarmen Garcia OliverNo ratings yet
- Predictors of Long-Term Improvement Following Cognitive Remediation in A Sample With Elevated Depressive SymptomsDocument11 pagesPredictors of Long-Term Improvement Following Cognitive Remediation in A Sample With Elevated Depressive SymptomsNerea Montero GarcíaNo ratings yet
- Versão Final Depressão ExecutivasDocument15 pagesVersão Final Depressão ExecutivasGeorgiana PrisoschiNo ratings yet
- Validation of The Hospital Anxiety and Depression Scale in Patients With Acute Low Back PainDocument10 pagesValidation of The Hospital Anxiety and Depression Scale in Patients With Acute Low Back PainJihanMukhtarNo ratings yet
- Riedel - 2011 - Clinical Predictors of Response and Remission in Inpatients With Depressive SyndromesDocument13 pagesRiedel - 2011 - Clinical Predictors of Response and Remission in Inpatients With Depressive SyndromesRicardo DíazNo ratings yet
- Predictors of manic switch in bipolar depressionDocument78 pagesPredictors of manic switch in bipolar depressionSheryl ElitaNo ratings yet
- Case Study-Ectopic PNDocument55 pagesCase Study-Ectopic PNArbie Jacinto100% (2)
- Case of Hymen Imperforata in Adolescents: Ade Triansyah, Muh Ardi Munir, Daniel SarangaDocument6 pagesCase of Hymen Imperforata in Adolescents: Ade Triansyah, Muh Ardi Munir, Daniel Sarangafabiola umbohNo ratings yet
- Canadian Syncope Risk ScoreDocument4 pagesCanadian Syncope Risk ScoreRisky WijayaNo ratings yet
- Nurse's Notes on Patient Admitted for Abnormal Uterine BleedingDocument6 pagesNurse's Notes on Patient Admitted for Abnormal Uterine BleedingAina De LeonNo ratings yet
- Magdy El-Masry Prof. of Cardiology Tanta UniversityDocument55 pagesMagdy El-Masry Prof. of Cardiology Tanta UniversityPrabJot SinGhNo ratings yet
- Ultrasound Clinic Lab Report for Mr. ArvindDocument4 pagesUltrasound Clinic Lab Report for Mr. ArvindsuganthiaravindNo ratings yet
- 10 1017@S0022215112000102Document8 pages10 1017@S0022215112000102irfana efendiNo ratings yet
- Gary Earle ResumeDocument2 pagesGary Earle Resumeapi-310096159No ratings yet
- Group 6 - Emergency, Medicine and Trauma Service PolicyDocument26 pagesGroup 6 - Emergency, Medicine and Trauma Service PolicyDAYANG NURHAIZA AWANG NORAWINo ratings yet
- Treating Social Anxiety DisorderDocument6 pagesTreating Social Anxiety DisorderIago SalvadorNo ratings yet
- Admission FormDocument1 pageAdmission FormYasin AhmedNo ratings yet
- Textbook of Removable ProsthodonticsDocument249 pagesTextbook of Removable ProsthodonticsskcaswuiNo ratings yet
- Igims DirectoryDocument28 pagesIgims DirectoryRavi ManiyarNo ratings yet
- Respiratory Rate AssessmentDocument2 pagesRespiratory Rate AssessmentChubs RiegoNo ratings yet
- IV Admixture CalculationsDocument20 pagesIV Admixture CalculationsudinNo ratings yet
- Wolfe - Understanding and Treating Anxiety Disorders An Integrative Approach To Healing The Wounded Self (2005)Document300 pagesWolfe - Understanding and Treating Anxiety Disorders An Integrative Approach To Healing The Wounded Self (2005)Ruxandra Pop100% (5)
- Acute Complicated Urinary Tract Infection (Including Pyelonephritis) in Adults - UpToDateDocument39 pagesAcute Complicated Urinary Tract Infection (Including Pyelonephritis) in Adults - UpToDateLaís FialhoNo ratings yet
- Case Presentation Thalamic Infarct LatestDocument48 pagesCase Presentation Thalamic Infarct LatestDoneva Lyn MedinaNo ratings yet
- Practical Prescriber PDFDocument515 pagesPractical Prescriber PDFGandhi Lanka100% (2)
- TranscriptDocument13 pagesTranscriptKetheesaran Lingam100% (3)
- Technology Act, 2000, The Legislations Governing The Sale of Drugs in IndiaDocument15 pagesTechnology Act, 2000, The Legislations Governing The Sale of Drugs in IndiaKritiKrishna100% (1)
- Rai Work Experience SheetDocument2 pagesRai Work Experience Sheetmark langcayNo ratings yet
- World Health Organization Dimensions of Adherence.9Document7 pagesWorld Health Organization Dimensions of Adherence.9Lucky Radja PonoNo ratings yet
- Mark Fredderick R. Abejo RN, MAN: Fundamentals of Nursing BulletsDocument4 pagesMark Fredderick R. Abejo RN, MAN: Fundamentals of Nursing BulletsDan Hernandez100% (1)
- HysterosalpingographyDocument20 pagesHysterosalpingographyAshvanee Kumar SharmaNo ratings yet
- Diabetic Foot Care Center:: One Stop Service For The Management of Diabetic Foot ProblemsDocument29 pagesDiabetic Foot Care Center:: One Stop Service For The Management of Diabetic Foot ProblemsscribdNo ratings yet
- DapusDocument4 pagesDapusRiza ZaharaNo ratings yet
- Wrist Fractures Recovery GuideDocument5 pagesWrist Fractures Recovery Guideat tNo ratings yet
- MCFARLANE - 2016 - ARD - EULAR-recommendations - FibromyalgiaDocument11 pagesMCFARLANE - 2016 - ARD - EULAR-recommendations - FibromyalgiaTata2666No ratings yet
- Keeping Healthy: Key ConceptsDocument11 pagesKeeping Healthy: Key ConceptsMrs S Baker100% (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (18)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (403)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosFrom Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosRating: 4.5 out of 5 stars4.5/5 (207)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Algorithms to Live By: The Computer Science of Human DecisionsFrom EverandAlgorithms to Live By: The Computer Science of Human DecisionsRating: 4.5 out of 5 stars4.5/5 (722)
- Summary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (11)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Secure Love: Create a Relationship That Lasts a LifetimeFrom EverandSecure Love: Create a Relationship That Lasts a LifetimeRating: 5 out of 5 stars5/5 (18)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)