Professional Documents
Culture Documents
Respiratory Disorders
Uploaded by
Julie EstebanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Respiratory Disorders
Uploaded by
Julie EstebanCopyright:
Available Formats
Chapter 40
Nursing Care of a Family When a
Child Has a Respiratory Disorder
Upper Respiratory Tract Disorders #1
❖Choanal atresia
❖Acute nasopharyngitis
o Assessment
o Therapeutic management
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Upper Respiratory Tract Disorders #2
❖Pharyngitis
o Viral pharyngitis
o Streptococcal pharyngitis
o Retropharyngeal abscess
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Upper Respiratory Tract Disorders #3
❖Epistaxis
❖Sinusitis
❖Laryngitis
❖Congenital laryngomalacia/tracheomalacia
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Upper Respiratory Tract Disorders #4
❖ Laryngotracheobronchitis (Croup)
o Assessment
o Therapeutic management
❖Epiglottitis
o Assessment
o Therapeutic management
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Upper Respiratory Tract Disorders #5
❖Aspiration
❖Bronchial obstruction
o Assessment
o Therapeutic management
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Lower Respiratory Tract Disorders #1
❖Influenza
❖Bronchitis
❖Bronchiolitis
o Respiratory syncytial virus
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Lower Respiratory Tract Disorders #2
❖Asthma
o Mechanism of disease
o Assessment
▪ History
▪ Physical assessment
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Lower Respiratory Tract Disorders #3
❖Asthma—(cont.)
o Pulmonary function studies
▪ Peak expiratory flow rate monitoring
o Therapeutic management
o Allergy triggers
❖Status asthmaticus: failure to respond to first-line
therapy.
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Lower Respiratory Tract Disorders #4
❖Pneumonia
o Pneumococcal pneumonia
o Chlamydial pneumonia
o Viral pneumonia
o Mycoplasmal pneumonia
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Lower Respiratory Tract Disorders #5
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Lower Respiratory Tract Disorders #6
❖Atelectasis
o Primary atelectasis
o Secondary atelectasis
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Pneumothorax
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Lower Respiratory Tract Disorders #7
❖Pneumothorax
❖Bronchopulmonary dysplasia
❖Tuberculosis
o Assessment
o Therapeutic management
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Lower Respiratory Tract Disorders #8
❖Cystic fibrosis
o Pancreas involvement
o Lung involvement
o Sweat gland involvement
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Lower Respiratory Tract Disorders #9
❖Cystic fibrosis—(cont.)
o Assessment
▪ Sweat testing
▪ Duodenal analysis
▪ Stool analysis
▪ Pulmonary testing
o Therapeutic management
Copyright © 2018 Wolters Kluwer · All Rights Reserved
2020 National Health Goals Related to
Respiratory Illness in Children #1
❖Reduce hospitalizations for asthma in children under
5 years of age from a baseline of 41.4 out of 10,000
children to a target level of 18.1 out of 10,000
children.
❖Reduce invasive pneumococcal infections in children
under 5 years from 20.3 out of 100,000 children to
12.0 out of 100,000 children.
Copyright © 2018 Wolters Kluwer · All Rights Reserved
2020 National Health Goals Related to
Respiratory Illness in Children #2
❖Reduce the number of courses of antibiotics
prescribed solely for the common cold from 1,728
out of 100,000 children to 864 out of 100,000
children.
❖Increase the proportion of children 6 months to 2
years of age who are immunized yearly against
seasonal influenza from 25% to 80%.
Copyright © 2018 Wolters Kluwer · All Rights Reserved
2020 National Health Goals Related to
Respiratory Illness in Children #3
❖Increase the proportion of children 2 to 4 years of
age who are immunized yearly against seasonal
influenza from 23% to 80%.
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Nursing Process: Respiratory Disorder
❖Assessment
❖Nursing diagnosis
❖Outcome identification and planning
❖Implementation
❖Outcome evaluation
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Assessing Respiratory Illness #1
❖Physical assessment
o Cough
▪ Paroxysmal coughing
o Rate and depth of respirations
o Retractions
o Restlessness
o Cyanosis
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Sites of Respiratory Retractions
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Assessing Respiratory Illness #2
❖Physical assessment—(cont.)
o Clubbing of fingers
o Adventitious sounds
o Chest diameter
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Clubbing of Fingers
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Assessing Respiratory Illness #3
❖Laboratory tests
o Blood gas analysis
▪ Pulse oximetry
▪ Nasopharyngeal culture
▪ Sputum analysis
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Assessing Respiratory Illness #4
❖Diagnostic procedures
o Chest radiography
o Bronchoscopy
o Pulmonary function studies
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Nursing Diagnoses
❖Activity intolerance
❖Fatigue
❖Fear
❖Impaired gas exchange
❖Impaired social interaction
❖Ineffective breathing pattern
❖Deficient knowledge
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Quality & Safety Education for Nurses
(QSEN)
❖Patient-Centered Care
❖Teamwork & Collaboration
❖Evidence-Based Practice
❖Quality Improvement
❖Safety
❖Informatics
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Therapeutic Techniques #1
❖Humidification
❖Inhalation devices
❖Coughing
❖Mucus-clearing devices
❖Chest physiotherapy
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Use of a Nebulizer
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Use of a Flutter Device
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Positions for Bronchial Drainage
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Therapeutic Techniques #2
❖Therapy to improve oxygenation
o Oxygen administration
o Pharmacologic therapy
▪ Metered-dose inhalers
o Incentive spirometry
o Breathing techniques
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Therapeutic Techniques #3
❖Therapy to improve oxygenation—(cont.)
o Endotracheal intubation
o Tracheostomy
▪ Suctioning technique
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Therapeutic Techniques #4
❖ Therapy to improve oxygenation—(cont.)
o Assisted ventilation
❖ Lung transplantation
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Question #1
When assessing a child for cyanosis, which is
important for the nurse to remember?
A. Cyanosis is an early indicator of respiratory distress.
B. The degree of cyanosis is not an accurate indicator of the
degree of hypoxia.
C. Cyanosis is caused by a decrease in the depth of respirations.
D. Cyanosis will be present if the child has had a large loss of
blood volume.
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Answer to Question #1
B. The degree of cyanosis is not an accurate indicator
of the degree of hypoxia.
Rationale: If the hemoglobin is low (decreased number of
RBCs), there may not be much cyanosis as the red blood
cells, which when not completely oxygenated, are what gives
the blood the dark color. Cyanosis is present with a PO2 of
less than 40 mmHg, which is usually a later sign in
respiratory distress.
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Question #2
Which is the primary nursing responsibility when a 4-
year-old child with a tracheostomy tube eats?
A. Prevent aspiration of food or fluids into the tube.
B. Limit ingestion of too much fluid.
C. Foster smooth passage of foods through the tube opening.
D. Prevent dyspnea from eating too rapidly.
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Answer to Question #2
A. Prevent aspiration of food or fluids into the tube.
Rationale: Because preschoolers are not necessarily neat
eaters, protecting the tube from food entering it is
important.
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Question #3
A child is to use an incentive spirometer four times
daily. Which statement suggests that the child
understands the purpose and correct technique of the
procedure?
A.“To do this right, I take in a very deep breath.”
B.“Using this will help me cough less.”
C.“The harder I blow out, the better I am doing.”
D.“This will make more room for my heart in my chest.”
Copyright © 2018 Wolters Kluwer · All Rights Reserved
Answer to Question #3
A. “To do this right, I take in a very deep breath.”
Rationale: The purpose of incentive spirometry is to make
the child take a deep breath to aerate the lungs better.
Copyright © 2018 Wolters Kluwer · All Rights Reserved
You might also like
- Ms Flash CardsDocument15 pagesMs Flash CardsMia MalazoNo ratings yet
- Assessing Childbearing WomenDocument27 pagesAssessing Childbearing WomenJoan Diana100% (1)
- Chap 20Document17 pagesChap 20Joanna Mie EstrososNo ratings yet
- Nursing Care of A Family With A High-Risk Newborn Nursing Care of A Family With A High-Risk NewbornDocument27 pagesNursing Care of A Family With A High-Risk Newborn Nursing Care of A Family With A High-Risk NewbornJoanna Mie Estrosos100% (1)
- Ch10Document38 pagesCh10Bridget Shienne DaculaNo ratings yet
- Ch18 Nursing Care of A Family With A NewbornDocument109 pagesCh18 Nursing Care of A Family With A NewbornKathleen Ang100% (1)
- Enjoying Pure Wellness: Discovering and Maximizing the Benefits of IV Nutritional and Regenerational TherapyFrom EverandEnjoying Pure Wellness: Discovering and Maximizing the Benefits of IV Nutritional and Regenerational TherapyRating: 5 out of 5 stars5/5 (1)
- Case Study PedsDocument11 pagesCase Study PedsGenesis Bicera100% (1)
- Nursing Care of A Family During A Surgical Intervention For Birth Nursing Care of A Family During A Surgical Intervention For BirthDocument30 pagesNursing Care of A Family During A Surgical Intervention For Birth Nursing Care of A Family During A Surgical Intervention For BirthJoanna Mie EstrososNo ratings yet
- Chapter61 Management of Patients With Neurologic DysfunctionDocument49 pagesChapter61 Management of Patients With Neurologic DysfunctionAhmed 123No ratings yet
- Drugs Acting On Lower RespiratoryDocument45 pagesDrugs Acting On Lower RespiratoryHannah Lorraine Gamayon100% (1)
- Nursing Care of A Family When A Child Has A Long-Term or Terminal Illness Nursing Care of A Family When A Child Has A Long-Term or Terminal IllnessDocument31 pagesNursing Care of A Family When A Child Has A Long-Term or Terminal Illness Nursing Care of A Family When A Child Has A Long-Term or Terminal IllnessJoanna Mie EstrososNo ratings yet
- Management of Patients With Chest and Lower Respiratory Tract DisordersDocument42 pagesManagement of Patients With Chest and Lower Respiratory Tract DisordersRegine Faye OnalNo ratings yet
- Nursing Care of A Family When A Child Has A Malignancy Nursing Care of A Family When A Child Has A MalignancyDocument32 pagesNursing Care of A Family When A Child Has A Malignancy Nursing Care of A Family When A Child Has A Malignancymanuzon.billarlangmail.comNo ratings yet
- Assessing Female Genitalia, Anus, and RectumDocument27 pagesAssessing Female Genitalia, Anus, and RectumCrestyl Faye R. CagatanNo ratings yet
- AbdomenDocument43 pagesAbdomenEmmanuel CuevasNo ratings yet
- Chapter 12Document91 pagesChapter 12Moxie MacadoNo ratings yet
- Assessing Newborns and InfantsDocument16 pagesAssessing Newborns and InfantsCrestyl Faye R. CagatanNo ratings yet
- Assessment of Respiratory Function Chpt.20Document32 pagesAssessment of Respiratory Function Chpt.20Maricar RosasNo ratings yet
- Chapter37 Assessment and Management of Patients With Allergic DisordersDocument40 pagesChapter37 Assessment and Management of Patients With Allergic Disordersjericho dinglasanNo ratings yet
- Assessing Children and AdolescentsDocument25 pagesAssessing Children and AdolescentsCrestyl Faye R. CagatanNo ratings yet
- Assessments CH 13 NutritionDocument23 pagesAssessments CH 13 NutritionIman HusainatNo ratings yet
- Pulling It All Together: Integrated Head-to-Toe AssessmentDocument20 pagesPulling It All Together: Integrated Head-to-Toe AssessmentCrestyl Faye R. CagatanNo ratings yet
- Chapter15Document49 pagesChapter15AikoSnowNo ratings yet
- Ch09Document32 pagesCh09Bridget Shienne DaculaNo ratings yet
- Chapter 20 Respiratory Assessment.Document35 pagesChapter 20 Respiratory Assessment.shrbaNo ratings yet
- Chapter - 40 WabsnDocument45 pagesChapter - 40 WabsnMichelle DislaNo ratings yet
- Gi DisordersDocument53 pagesGi DisordersJulie EstebanNo ratings yet
- Nursing Care of A Family With An Infant Nursing Care of A Family With An InfantDocument38 pagesNursing Care of A Family With An Infant Nursing Care of A Family With An InfantRj SantiagoNo ratings yet
- Nursing Care of The Child With An Alteration in Gas Exchange/Respiratory DisorderDocument30 pagesNursing Care of The Child With An Alteration in Gas Exchange/Respiratory DisorderGlory MimiNo ratings yet
- Chapter 4Document31 pagesChapter 4Livan MartellNo ratings yet
- Shock and Multiple Organ Dysfunction SyndromeDocument34 pagesShock and Multiple Organ Dysfunction SyndromeRegine Faye OnalNo ratings yet
- Critical Thinking in Health AssessmentDocument38 pagesCritical Thinking in Health AssessmentMoxie MacadoNo ratings yet
- Assessment and Management of Patients With Breast Disorders Assessment and Management of Patients With Breast DisordersDocument36 pagesAssessment and Management of Patients With Breast Disorders Assessment and Management of Patients With Breast DisordersMozart OlarioNo ratings yet
- Nursing Care of The Child With An Infectious or Communicable Disorder Nursing Care of The Child With An Infectious or Communicable DisorderDocument32 pagesNursing Care of The Child With An Infectious or Communicable Disorder Nursing Care of The Child With An Infectious or Communicable DisorderMichelle DislaNo ratings yet
- Chapter62 1Document34 pagesChapter62 1Mozart OlarioNo ratings yet
- Assessment of Hematologic Function and Treatment Modalities Assessment of Hematologic Function and Treatment ModalitiesDocument26 pagesAssessment of Hematologic Function and Treatment Modalities Assessment of Hematologic Function and Treatment ModalitiesEdelweiss Marie CayetanoNo ratings yet
- Ch01Document19 pagesCh01Bridget Shienne DaculaNo ratings yet
- Chapter171Document36 pagesChapter171Chris Deniel BaldozaNo ratings yet
- Ch04Document31 pagesCh04Moxie MacadoNo ratings yet
- Pneumonia Thesis TopicsDocument8 pagesPneumonia Thesis Topicsdwt29yrp100% (2)
- Critical Thinking in Health AssessmentDocument27 pagesCritical Thinking in Health AssessmentLivan MartellNo ratings yet
- Chapter 66 - Management of Patients With Neurologic DysfunctionDocument54 pagesChapter 66 - Management of Patients With Neurologic DysfunctionFeliciaDorgham100% (2)
- Ch09Document94 pagesCh09Moxie MacadoNo ratings yet
- Study GuideDocument46 pagesStudy GuideAkia Cayasan BayaNo ratings yet
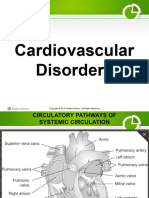
- 3 Cardiovascular DisordersDocument123 pages3 Cardiovascular Disordersbautil.jameelNo ratings yet
- O2 ModalitiesDocument49 pagesO2 ModalitiesVyklyn Testa0% (1)
- Metabolic Disorders PowerpointDocument48 pagesMetabolic Disorders PowerpointJamesNo ratings yet
- Chapter151.2Document43 pagesChapter151.2Chris Deniel BaldozaNo ratings yet
- Ch01Document24 pagesCh01Sheena EspañolNo ratings yet
- Dissertation On PneumoniaDocument7 pagesDissertation On PneumoniaCustomWrittenPaperLittleRock100% (1)
- 4gastrointestinal DisorderDocument48 pages4gastrointestinal DisorderIzelwyn DaguioNo ratings yet
- Pediatrics-2006 BronchiolitisDocument22 pagesPediatrics-2006 BronchiolitisOscar Echeverría OrellanaNo ratings yet
- Staying Healthy in Childcare - Gov Handbook - 4th EditionDocument138 pagesStaying Healthy in Childcare - Gov Handbook - 4th EditionSarah Williamson PhippsNo ratings yet
- Airway Obstruction - Types, Causes, and SymptomsDocument6 pagesAirway Obstruction - Types, Causes, and SymptomsGilbertLiem100% (1)
- Airway Management and Common ConditionsDocument34 pagesAirway Management and Common Conditionsrigo montejoNo ratings yet
- Infectious Pediatric Pneumonia: Author: Roberta D. Hood, HBSC, MD, CCFP Date Created: December 2011Document137 pagesInfectious Pediatric Pneumonia: Author: Roberta D. Hood, HBSC, MD, CCFP Date Created: December 2011Kartika Rezky100% (1)
- Respiratory Disorders Prat IDocument50 pagesRespiratory Disorders Prat Izainahalqahtani3No ratings yet
- Chapter - 030.bridge To NCLEX Review Question AnswersDocument7 pagesChapter - 030.bridge To NCLEX Review Question AnswersJackie JuddNo ratings yet
- Summary of Brian Tyson, George Fareed & Mathew Crawford's Overcoming the COVID DarknessFrom EverandSummary of Brian Tyson, George Fareed & Mathew Crawford's Overcoming the COVID DarknessNo ratings yet
- Matrix of Comments and SuggestionsDocument1 pageMatrix of Comments and SuggestionsJulie EstebanNo ratings yet
- NursingDocument1 pageNursingJulie EstebanNo ratings yet
- Final Term - 2nd Sem MCN PPT NotesDocument42 pagesFinal Term - 2nd Sem MCN PPT NotesJulie EstebanNo ratings yet
- Gi DisordersDocument53 pagesGi DisordersJulie EstebanNo ratings yet