Professional Documents
Culture Documents
Jurnal Metabol 1
Uploaded by
Ersalina NidiantiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jurnal Metabol 1
Uploaded by
Ersalina NidiantiCopyright:
Available Formats
RBMOnline - Vol 5. Suppl. 1. 73–86 Reproductive BioMedicine Online; www.rbmonline.
com/Article/697 on web 13 September 2002
Ovarian stimulation: from basic science to
clinical application
Michael Ludwig1,3, Ricardo E Felberbaum1, Klaus Diedrich1, Bruno Lunenfeld2
1Division of Reproductive Medicine and Gynecologic Endocrinology, Department of Gynecology and Obstetrics,
University Clinic, Ratzeburger Allee 160, 23538 Lübeck, Germany
2Faculty of Life Sciences, Bar–Ilan University, Ramat Gan, 52900 Israel
3Correspondence: Tel: +49 451 5002158; Fax: +49 451 5059334; e-mail: Ludwig_M@t-online.de
Abstract
Treatment for infertility, including ovarian stimulation, was first introduced almost 100 years ago. At this time, radiation
therapy became an established treatment, and it was only some decades later that the problem of radiation-induced cancer
emerged. Non-human gonadotrophins, such as pregnant mare serum gonadotrophin (PMSG), and human pituitary
gonadotrophins (HPG), were commonly used for hormonal stimulation procedures. However, use of PMSG led to antibody
formation, and it was therefore only useful for the first treatment cycle. HPG produced good results, but its use came to an
end in the late 1980s when it was linked to the development of Creutzfeldt–Jakob disease. The first hormonal product from
human menopausal urine to be used was human menopausal gonadotrophin (HMG), followed later by purified preparations
of this product. All of these preparations contained a high percentage of unknown urinary proteins, which interfered with
batch-to-batch consistency. This changed with the introduction of recombinant gonadotrophins, produced from an
immortalized/standardized mammalian cell line (CHO). More recent developments include the introduction of long-acting
gonadotrophin formulations. The development of gonadotrophin-releasing hormone (GnRH) analogues and more recently
the use of GnRH antagonists has helped to improve ovarian stimulation protocols by optimizing their efficacy, and making
them easier to administer.
Keywords: FSH, GnRH antagonist, gonadotrophin formulation, LH, recombinant gonadotrophin, urinary gonadotrophin
Introduction in infertile women has been driven by the need to make these
products effective, safe, pure and consistent, thereby reducing
Infertility is not an entity of our century – it is as old as treatment variability.
mankind. The Bible tells the story of several infertile women
(Figure 1) (Lunenfeld, 1995). At that time, however, fertility Some of the leading scientists and clinicians who have
was believed to be a gift from God, which could be given and contributed to this history over the past 100 years are shown in
taken away, depending on what people did or did not do. Figure 2.
Nowadays there is an ongoing discussion as to whether the
prevalence of infertility is increasing. Statistics from around Ovarian and pituitary irradiation for
1900, from Australia, have estimated the prevalence of the treatment of infertility
infertility in married couples to be 11% (Cummins, 1999), a
similar figure to that observed today (Snick et al., 1997). In the early 1900s, it was proposed that irradiation of the
ovaries might be a useful treatment for infertility by
As knowledge on the aetiology of infertility has increased over stimulating ovarian function (Halberstaedter, 1905). In
the years, treatment options have changed, and a number of addition, beneficial effects of Roentgen irradiation of the
different assisted reproductive techniques are now available. pituitary were reported (Beclere, 1926). As a result, the
The success of these techniques depends on many factors, techniques of ovarian and pituitary irradiation became widely
including the age of the patient, the patient’s medical history, established as treatments for infertile women in the USA
and the ovarian stimulation regimen used. For IVF and (Rubin, 1926; Mazer and Greenberg, 1943; Kaplan, 1948).
intracytoplasmic sperm injection (ICSI), laboratory This resulted in a statement by Rita Finkler, in 1949, that:
conditions, the number of embryos replaced and the skill of the ‘Irradiations of the ovarian and pituitary regions for the relief
embryologist also have to be considered. of functional sterility, in the female is a universally accepted
therapeutic procedure’ (Finkler, 1949).
The history of the use of gonadotrophins in the treatment of
infertility extends from early attempts at their extraction from The benefits of radiation therapy compared with endocrine
animals, human cadavers and human urine, to the production therapy were demonstrated in a study of 130 patients who
of recombinant products from CHO cells. During the last 15 underwent irradiation of the ovaries and pituitary at a dose of
years, the development of gonadotrophin-releasing hormone 200 ~kV. Such treatment was reported to require shorter
(GnRH) analogues has helped to improve ovarian stimulation treatment regimens, to be less expensive, and to be easier to
protocols by optimizing their efficacy, and making them easier administer than endocrine therapy (Finkler, 1949). The
for doctors to administer and more comfortable for patients to cumulative pregnancy rates after a 2-week course of radiation
receive. All along, the development of gonadotrophins for use therapy are shown in Figure 3. It was concluded that the 73
Reprinted from Vol. 5, Suppl. 1 (2002) pp. 73 86. S3
Ovarian stimulation: from basic science to clinical application - M Ludwig et al.
Figure 1. Infertility in the bible. Abraham was married to
Sarah. Sarah, however, was unable to become pregnant, and
therefore she gave her maid Hagar to Abraham instead;
perhaps the first surrogate mother. Hagar became pregnant
with Ishmael. Sarah subsequently became pregnant herself –
as written in the Bible, due to the will of God – and gave birth
to Isaac. Isaac, after other wives, married Rebecca, who
initially was infertile. Only after Isaac had asked God for
fertility in his marriage, did God take away her infertility from
Rebecca and she gave birth to twins, Esau and Jacob. Rachel,
Jacob’s wife, was infertile, too, due to the will of God, since
God wanted to punish Jacob, who loved Rachel more than
Leah, his other wife. Finally, however, after Leah had given
birth to several sons, God made Rachel fertile and she gave
birth to Joseph. Before that, due to her infertility, she, just like
Sarah, gave her maid Bilha to Jacob and Bilha gave birth to Figure 2. Some of the pioneers who pushed the development
two sons (Genesis 16–30) (adapted from Lunenfeld, 1995). of gonadotrophins forward, either by clarifying the
physiological background or by the development of innovative
preparations. Selmar Aschheim (a), Bernhard Aschner (b),
Gerhard Bettendorf (c), Pietro Donini (d), Bruno Lunenfeld
cumulative conception rates were independent of the treatment
(e), Carl Axel Gemzell (f), Philip Edward Smith (g) and
administered, being 34.2% among patients receiving hormonal
Bernhard Zondek (h). All of the pictures, with the exception of
therapy and 35.2% among those receiving radiation therapy. In
(e), were reprinted with kind permission of Springer Verlag
patients suffering from secondary amenorrhoea, menstrual
[from: G. Bettendorf (1995) Zur Geschichte der
bleeding was re-established in 40.6% of those receiving
Endokrinologie und Reproduktionsmedizin. Springer Verlag,
hormonal therapy and 46.4% of those receiving radiation
pp. 12, 15, 37, 117, 174, 539, 632].
therapy (Finkler, 1949). However, we now know that the
stimulatory effect of irradiation may have been due to
increased blood flow and hyperaemia. The price of radiation
therapy did not emerge until some 45 years later, around 1985, function of higher centres in the brain. This hypothesis was
when the National Institute of Health (NIH) and others based on his observations in men and women with head trauma
reported that many patients who had received this kind of that lesions between the hypothalamus and the pituitary lead to
therapy had developed ovarian cancer (Ron et al., 1994). hypopituitarism and gonadal atrophy (Aschner, 1912).
Therefore, he was the first to propose a hypothalamic–pituitary
Early understanding of the interaction for gonadotrophic action.
hypothalamic–pituitary–ovarian axis In 1926, Smith and Engle demonstrated that immature male or
The pituitary was already known in Ancient Greece. They female animals that were hypophysectomized failed to mature
called it hypophysis, or ‘something which grows at the bottom sexually. They also showed that daily transplants of anterior
of the brain’. Later on, the physician Galen proposed, that the pituitary gland tissue from mice, rats, cats, rabbits and guinea
hypophysis is a kind of trashcan, where metabolites from the pigs into immature male and female mice and rats rapidly
brain are collected. He therefore called this structure glandula induced precocious sexual maturity and superovulation
pituitaria, because he thought that the trash was brought to the (Smith, 1926; Smith and Engle, 1927). In the same year, the
nose as pituita, nose mucus. Only in the seventeenth century pioneering experiments by Zondek showed that ovarian
did it became clear that under normal conditions, there is no function is regulated by the pituitary: the implantation of
flow of any fluid from the brain to the nose, and that the anterior pituitary glands of adult cows, bulls and humans into
pituitary must have another function. immature animals was shown to evoke the rapid development
of sexual puberty (Zondek, 1926).
Work by Crowe et al. in 1910 showed that partial ablation of
the pituitary gland leads to atrophy of the genital organs in It was again Zondek, only 4 years later, who proposed the
adult dogs, and to the persistence of infantilism and sexual secretion of two hormones by the pituitary:
inadequacy in puppies (Crowe et al., 1910). Two years later, ‘Follikelreifungshormon’ or Prolan A, and
74 Aschner postulated that pituitary function depends on the ‘Luteinisierungshormon’ or Prolan B (Zondek, 1930) (Figure
S4 Reprinted from Vol. 5, Suppl. 1 (2002) pp. 73 86.
Ovarian stimulation: from basic science to clinical application - M Ludwig et al.
Cumulative pregnancy rate
Months
Figure 3. Effect of a 2-week course of radiation therapy on ovaries and the pituitary in cases of ‘functional infertility’, i.e.
infertility due to abnormal hormonal values or abnormal bleeding patterns without a male factor. Eighty rads was delivered into
each ovary and into the pituitary gland. Shown are cumulative pregnancy rates in a group of 54 patients. Seventeen of these
patients were ‘endocrine resistant’, i.e. they did not get pregnant after combined PMSG/HCG treatment. In another series, the
authors showed a cumulative pregnancy rate of 47%; in 28 amenorrhoeic patients they were able to re-establish menses in 46.4%
(Finkler, 1949).
4). This hypothesis was proved only a year later with the
extraction of two different hormones from the pituitary, one of
which acted as a follicle stimulating factor and one as a
luteinizing factor (Fevold et al., 1931).
The third gonadotrophin, human chorionic gonadotrophin
(HCG), was first described in 1943, when it was shown to be
secreted from trophoblastic cells. Zondek and Aschheim, after
administration of urine from pregnant individuals, showed the
development of follicular cysts and hemorrhagic follicles in
the mouse – the first pregnancy test (Zondek and Aschheim,
1927). Such changes are nowadays commonly seen in ovarian
hyperstimulation syndrome (OHSS).
The link between the hypothalamus and the pituitary was
finally proposed by Guillemin in 1967, when he suggested that
an LH-releasing factor, now termed GnRH, controlled the
release of gonadotrophins from the pituitary for follicular
maturation (Guillemin, 1967). The race between two different
laboratories to elucidate the structure of this GnRH finally
ended in June 1971, with a report by Andrew Schally and
colleagues at the annual meeting of the Endocrine Society in
San Francisco of the decapeptide structure of GnRH (Schally
et al., 1971). The group had analysed 240 μg of the compound,
amalgamated from 160,000 pig pituitaries.
The next steps in the learning process were the discoveries that
the GnRH gene is located on chromosome 8, and that GnRH is
produced from a pre-hormone known as Pre-Pro-GnRH
(Wetsel et al., 1991, 1995). GnRH was also shown to be
rapidly metabolized, with a half-life of <5 min, and to be
mediated by a transmembrane receptor, which stimulates the
release of LH and FSH. This receptor was shown to be a
Figure 4. The original figure (Zondek, 1930) showing the calcium-mobilizing, seven transmembrane domain receptor
proposed connection between pituitary and ovaries, as well as that is coupled to phospholipase Cβ though G proteins (Yen,
the action of Prolan A (‘Follikelreifungshormon’) and Prolan B 1999).
(‘Luteinisierungshormon’). The graph shows the action of
Prolan A on the secondary follicle, resulting in maturation to It was Knobil who contributed with his pioneering work to the
the Graafian follicle. After ‘Follikelsprung’ (ovulation), a discovery of the interaction between the hypothalamus and
corpus luteum results, which, following the idea of Professor pituitary by GnRH. Circhoral LH pulses were assumed to be
Zondek, is under the influence of Prolan B. Furthermore, the the consequence of pulsatile GnRH secretion by the
action of follicular hormones on the endometrium is shown in hypothalamus. This gave rise to the idea, that an oscillator or
its different phases (‘Proliferationsphase’ and signal generator in the central nervous system, the so-called
‘Sekretionsphase’). Figure reprinted with kind permission of GnRH pulse generator, must exist (Knobil, 1974, 1980). He
Springer Verlag. also showed, that continuous administration of GnRH results 75
Reprinted from Vol. 5, Suppl. 1 (2002) pp. 73 86. S5
Ovarian stimulation: from basic science to clinical application - M Ludwig et al.
Figure 5. Production of urinary gonadotrophins. Shown is
the collection of pooled urine from postmenopausal
women (a), the collection in large tanks (b), and the
manual processing of a Kaolin filter after centrifugation
(c). All pictures reprinted with kind permission of Serono
International S.A., Geneva, Switzerland.
b
in pituitary suppression. Pulsatile GnRH administration was Patients who did not get pregnant after the first or second
necessary to produce an adequate pituitary response and LH treatment cycle using PMSG became insensitive to it, and this
secretion (Knobil, 1980, 1988; Wildt et al., 1986). Thus, marked the end of the PMSG era (Ostergaard, 1942; Zondek and
GnRH can either stimulate or inhibit gonadotrophin secretion, Sulman, 1942). Interestingly, PMSG was still used in Eastern
depending on its mode of administration (Plant et al., 1978; Germany until 1973 (Groot-Wassink and Blawert, 1973).
Wildt et al., 1981).
Human pituitary gonadotrophins
Introduction of pregnant mare (HPG)
serum gonadotrophin (PMSG)
In, 1958, another source of gonadotrophins was discovered:
In 1930, Cole and Hart showed that pregnant mare serum the pituitary glands from human cadavers. The gonadotrophins
gonadotrophin (PMSG), produced in the endometrial cups of extracted from this source were termed human pituitary
pregnant mares, has potent gonadotrophic activity (Cole and gonadotrophin (HPG) (Gemzell et al., 1958; Bettendorf,
Hart, 1930). Thus in 1937, PMSG was extracted for use in 1963). HPG was shown to induce ovarian stimulation in
anovulatory women. However, this extract produced hypophysectomized individuals (Bettendorf, 1963), and was
inconsistent results and adverse effects. In 1941, the concept of used extensively for the induction of ovulation until 1988.
the two-step protocol was introduced: ovarian stimulation
using gonadotrophins and the induction of ovulation using At this time, HPG was withdrawn from the market because of
HCG. Mazer and Ravetz used PMSG in this protocol in the discovery of 12 cases of Creutzfeldt–Jakob disease that
amenorrhoeic women with good results: 23 severely were thought to be linked to the use of this product (Dumble
amenorrhoeic women received either PMSG or a pituitary and Klein, 1992). Interestingly, however, these cases of
extract from pigs and sheep for follicle stimulation, and HCG Creutzfeldt–Jakob disease did not occur in patients who
for the induction of ovulation. Menstruation was induced in 19 received pharmaceutically produced products but in patients
of the patients, some of whom had not menstruated for years. who received government-produced products: from the
These results suggested the presence of a pituitary factor that Pituitary Agency in Australia, the Pituitary Agency in the UK,
stimulated mature follicle development (Mazer, 1946). and the Pituitary Agency of France. HPG was withdrawn from
the market after that, and another period of gonadotrophins
In 1942, however, a number of research groups described the came to its end (Cochius et al., 1990).
development of ‘antihormones’ in women who were treated
76 with PMSG. This was essentially an antigen–antibody reaction.
S6 Reprinted from Vol. 5, Suppl. 1 (2002) pp. 73 86.
Ovarian stimulation: from basic science to clinical application - M Ludwig et al.
Figure 6. Purification of human postmenopausal urine to retrieve HMG. First, the urine is passed through a column containing
kaolin. This produces a solution containing urinary FSH, LH and 95% urinary proteins (a). Polyvalent antibodies to HCG are then
bound into the kaolin column, which holds back the urinary LH but allows urinary FSH to pass through. The result is a mixture
of urinary FSH and 95% urinary proteins (b). The final step involves the introduction of a monoclonal anti-FSH antibody into a
Sepharose column, followed by the elution of bound FSH from the column (c).
basis on the future of gonadotrophins, as well as on the
Human menopausal gonadotrophin standardization of these new products. In the summer of 1953,
(HMG) several scientists met in Geneva, Switzerland, to define basic
Human menopausal gonadotrophin (HMG) was developed at and clinical goals for gonadotrophic research. Some of the
around the same time as HPG. This gonadotrophin is present members of this first meeting of the ‘Gonadotrophin Club’ (G-
in the urine of postmenopausal women (Figure 5), and was Club) were Rudi Borth, Bruno Lunenfeld, Hubert de
extracted using a technique developed by a Serono chemist in Watteville, Egon Diczfalusy, Jim Brown, John Loraine, and
1949 (Donini et al., 1964), in which kaolin is used to absorb A.C. Crooke. The participants agreed to develop specific assay
glycoproteins from the urine (Figure 6). The gonadotrophin procedures, bioassay standards and purification methods, that
thus produced was shown to have about 5% biological activity would lead to the development of a gonadotrophic preparation
and to consist of 95% urinary proteins. Administration of this for therapeutic purposes. It was also their work to first define
gonadotrophin in an animal model resulted in an increase in the term ‘human menopausal gonadotrophin’ (HMG) for the
the size of the ovaries and uteri, therefore proving its newly made preparation. The second meeting of the G-Club
effectiveness in ovarian stimulation (Borth et al., 1954). was held in Birmingham, where the main topic was the
chemical and biological properties of gonadotrophins
In 1953, HMG was successfully used to stimulate the ovaries extracted from human fluids.
of hypophysectomized rats (Borth et al., 1954), and in 1959,
its use in humans was shown to cause dramatic changes in In 1959 another G-Club meeting led to the agreement that a
steroid excretion, and in the endometrium and vaginal reference batch of gonadotrophin was needed, to standardize
epithelium (Lunenfeld et al., 1960). The first live births treatment with gonadotrophins. In 1960, this resulted in the
following the administration of HMG to humans were reported decision that a batch of 50 g Pergonal® (human menopausal
in 1962 (Lunenfeld et al., 1962). gonadotrophin; Serono International S.A.), lot 23, should be
the reference preparation. Four years of discussion followed
At around this time, the threshold hypothesis was developed: and an international collaborative study was organized to
this suggested that an enlargement of the FSH window would calibrate the FSH and LH activities in this batch. Eventually,
lead to an increase in the number of developing follicles in the in 1964, the Second International Reference Preparation-HMG
early follicular phase (Lunenfeld et al., 1961). This hypothesis was established.
was picked up in later years and elegantly described as
’threshold therapy’. The hypothesis also led to the development
of different ovarian stimulation procedures (Figure 7).
As a result of these rapid developments in this field, in the
mid-1950s the G-Club formed, to discuss on an international 77
Reprinted from Vol. 5, Suppl. 1 (2002) pp. 73 86. S7
Ovarian stimulation: from basic science to clinical application - M Ludwig et al.
Figure 7. Step-up (a), step-down (b) and sequential protocol
(c) (Lunenfeld, 1963; Fauser et al., 1993; Hugues et al., 1996).
Whilst the step-up protocol (a) seems to be ideal for patients
suffering from polycystic ovarian syndrome, since it helps to
avoid multifollicular development, others have described, for
the same cohort of patients, the step-down protocol (b) as the
ideal approach. Each of the three protocols has been proven to
c work and may have its benefits as well as drawbacks.
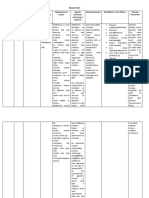
Table 1. WHO classification scheme for cases of ovarian
Ovarian hyperstimulation hyperstimulation syndrome (OHSS) (World Health
syndrome: the problem of Organization, 1973). This historical scheme has been
gonadotrophin administration modified several times, but it remains the one used in most
studies for classification of this entity.
Soon after HMG preparations were first used in ovarian
stimulation procedures, the first cases of OHSS were reported Grade Findings Treatment
in the literature (Mozes et al., 1965). As a result, the World
Health Organisation proposed a classification and I Variable ovarian No treatment
management scheme for cases of OHSS (Table 1) (Melmed et enlargement necessary
al., 1969). Even now, OHSS is the most important Sometimes ovarian Report additional
complication of ovarian stimulation. It can itself lead to further cysts symptoms to the physician
complications (Ludwig et al., 1999b, 2000), and may be life Increased urine
threatening (Cluroe and Synek, 1995). hormones
II Abdominal Careful medical
LH and FSH in ovarian stimulation distension observation
protocols: the two-cell theory Nausea Symptomatic treatment
Vomiting
The two-cell two-gonadotrophin theory was proposed in 1966 Diarrhoea
(Ryan and Petro, 1966; Ryan, 1979). Essentially, this states III Large ovarian Hospitalization and
that LH binds to receptors on the thecal cells, stimulating the cysts prompt medical treatment
production of androgens. These diffuse to the granulosa cells, Ascites Correction of altered fluid
where they are then transformed into oestrogens by the and electrolyte balance
aromatase produced by the granulosa cells, stimulated by FSH. Sometimes
hydrothorax
With respect to LH, it is now well known that there is a certain Haemoconcentration
threshold concentration of this gonadotrophin below which may appear
78 oocyte maturation will not occur. This situation is observed in
S8 Reprinted from Vol. 5, Suppl. 1 (2002) pp. 73 86.
Ovarian stimulation: from basic science to clinical application - M Ludwig et al.
Table 2. Results of a meta-analysis of eight prospective, randomized trials comparing urinary FSH and
HMG in IVF treatments. Included were ovarian stimulation protocols with and without the use of GnRH
agonists. Data according to Daya et al. (1995).
Analysis per Gonadotrophin Clinical Absolute Odds ratio P-value
used pregnancy (%) treatment effect (95% CI)
in favour of
FSH (%)
Cycle start FSH 63/285 (22.1) 8.5 1.71 (1.12–2.62) 0.009
HMG 45/332 (13.6)
Oocyte retrieval FSH 63/268 (23.5) 8.0 1.69 (1.10–2.59) 0.016
HMG 45/291 (15.5)
Embryo transfer FSH 63/254 (24.8) 8.3 1.70 (1.10–2.62) 0.018
HMG 45/273 (16.5)
women with WHO I ovarian insufficiency, such patients HP]; Metrodin HP®, Serono International S.A., Geneva,
showing little or no gonadotrophic activity. In these patients, Switzerland) (le Cotonnec et al., 1993; Howles et al., 1994).
oestrogen production and endometrial growth occur only with
the administration of exogenous LH, as demonstrated in a Several prospective, randomized studies were then performed
prospective randomized study (The European Recombinant to determine the efficacy of highly purified FSH for ovarian
Human LH Study Group, (1998). stimulation. A meta-analysis of eight of these studies clearly
showed that purified FSH was more effective in this respect
However, there is now overwhelming evidence to show that than HMG, increasing the pregnancy rate by approximately
inappropriately high concentrations of LH also have a 1.7 fold (Table 2) (Daya et al., 1995).The use of FSH either
detrimental effect on fertility: high concentrations of LH alone or following contraceptive pills and/or in combination
appear to have a direct effect on the follicles, leading to with GnRH analogues became the gold standard for patients
premature luteinization, follicular atresia and poor-quality with PCOD receiving assisted reproductive treatment.
oocytes. These, in turn, result in higher abortion and lower However, a major problem with the production of highly
ongoing pregnancy rates (Stanger and Yovich, 1985; Ludwig purified FSH was the need for large quantities of urine from
et al., 1999a). postmenopausal women. When production of urinary
gonadotrophins began, there were three urine collecting
Purification of HMG centres, with about 600 donors who produced 120,000 l of
urine annually: one in the Netherlands, one in Spain, and one
As long ago as 1973, the World Health Organization (WHO) in Italy. At the start of the 1990s it was estimated that 120 ×
(Figure 8) stated that: ‘The ratio of FSH to LH varies in 106 million litres of urine would be needed to satisfy the
different HMG and HPG preparations, but the available worldwide demand for pure FSH, and this would require the
evidence indicates, that preparations with ratios of 0.1–10.0 services of about 600,000 donors. Clearly, a different source of
are acceptable therapeutic agents provided, that a sufficient pure FSH was needed (Rodgers et al., 1994; Giudice et al.,
total dosage of FSH is administered to the patient’ (WHO, 2001).
1973). A preparation with such high variation (Rodgers et al.,
1994) is not ideal for clinical use. Furthermore, HCG is This increased need was due to the increasing number of
sometimes added to HMG in order to increase the LH content indications. In the early 1960s HMG was used as replacement
and achieve the labelled activity of 75 IU per ampoule. HCG therapy in WHO I patients, in the late 1960s, HMG was used
has been detected in all available HMG products, irrespective as regulation therapy in WHO II patients who did not respond
of their declared purity (Stokman et al., 1993). Since the half- or who did not conceive following three cycles with
life of HCG is significantly longer than that of LH, the variable clomiphene citrate, from the mid-1970s it was increasingly
amounts of HCG added may contribute to the batch-to-batch used for ovarian stimulation for IVF in infertile patients with
variations. tubal pathology, and in the 1990s there was an exponential
increase when it was used for ICSI in cases of severe male
In view of the detrimental effect of high LH concentrations on factor infertility. In fact, the first IVF pregnancy, in 1975, was
fertility, attempts were made to minimize LH activity in the result of HMG stimulation, although it ended as an ectopic
preparations of HMG. This was achieved by extracting the LH pregnancy (Steptoe and Edwards, 1976). Louise Brown was
using a polyvalent antibody to HCG in a kaolin column, then born following natural cycle IVF in 1978 (Steptoe and
leaving a solution containing only FSH and urinary proteins Edwards, 1978). By 2–3 years later, babies had been born in
(Donini et al., 1966; Eshkol and Lunenfeld, 1967). Serono Australia and France, then in USA in 1982.
Laboratories further refined this purification technique by
introducing monoclonal anti-FSH antibodies into the kaolin Development of recombinant
column and eluting FSH from the column by breaking the
antigen–antibody complex. This process increased the FSH
gonadotrophins
concentration in the gonadotrophin preparation from 100 to The production of gonadotrophins by recombinant genetic
10,000 IU/mg protein (urinary FSH highly purified [uFSH- engineering technology was finally made possible by the
79
Reprinted from Vol. 5, Suppl. 1 (2002) pp. 73 86. S9
Ovarian stimulation: from basic science to clinical application - M Ludwig et al.
Figure 8. The title page of the WHO paper on ‘Agents
stimulating gonadal function in the human’. The members of
the scientific board (reproduced with kind permission of the
WHO).
isolation of the human genes coding for the common alpha
subunit and the specific beta subunits. This led to the
preparation of appropriate vectors, which were transfected into Figure 9. A modern bioreactor for the production of follitropin
a suitable immortalized mammalian cell line namely, the alpha (Gonal F®). Picture reprinted with kind permission of
Chinese hamster ovary (CHO) cell line. A cell line Serono International S.A., Geneva, Switzerland.
characterized by a high and stable level of FSH expression was
isolated from the transfected cells: CHO DUKI with two
plasmids (follitropin alpha; Gonal F®, Serono International are using mathematical statistical models for the calculation of
S.A., Geneva, Switzerland) and CHO KI with one plasmid costs, they are a helpful tool under these circumstances.
(follitropin beta; Puregon®, Organon, Oss, The Netherlands).
These cell lines were used to establish a master cell bank, In one UK study, a decision-analytic model was used to
which now serves as the source of working cell banks (WCB). compare the results achieved with the recombinant human
Thus, a continuous supply of recombinant human FSH with FSH follitropin beta and those achieved with urinary FSH and
guaranteed consistency from WCB to WCB is now available HMG. The cost of one IVF cycle was £5135 for recombinant
(Howles, 1996). A modern bioreactor used in the manufacture human FSH, £4806 for urinary FSH, and £4202 for HMG. For
of recombinant human FSH (follitropin alpha) is shown in one ongoing pregnancy, the costs were in favour of
Figure 9. recombinant human FSH (£8992 versus £10,834 for urinary
FSH and £9472 for HMG (Sykes et al., 2001). Another UK
The advantages of using recombinant human FSH include the study used a Markovian decision framework and Monte Carlo
availability of unlimited quantities of the hormone, guaranteed simulation to compare the costs of treatment with the
quality of the source of the product and the final product, recombinant human FSH follitropin alpha and urinary FSH. In
batch-to-batch consistency, and the availability of a highly this study, the cost per successful pregnancy was significantly
pure preparation that is not contaminated with unknown lower for recombinant human FSH (£5906) than for urinary
urinary proteins (Hugues, 2001; Risquez, 2001). Furthermore, FSH (£6060) (Daya et al., 2001). Similarly, a Markov model
a recent meta-analysis has shown that recombinant human analysis performed in the United States gave costs per
FSH is superior to urinary FSH (Table 3) (Daya, 2002). successful pregnancy of $40,688 for recombinant human FSH
(follitropin alpha) and $47,096 for urinary FSH (Silverberg et
Recent cost-effectiveness analyses have also shown that the al., 2002a,b).
higher costs of recombinant human FSH compared with
urinary FSH are outweighed by the higher success rates Following the successful production of recombinant human
80 achieved with the former preparation. Even if all these studies FSH, similar technology was used to produce other
S10 Reprinted from Vol. 5, Suppl. 1 (2002) pp. 73 86.
Ovarian stimulation: from basic science to clinical application - M Ludwig et al.
Table 3. Results of a meta-analysis comparing recombinant FSH and urinary FSH in
ovarian stimulation for IVF cycles (data according to Daya, 2002). Follitropin alpha:
Gonal F®, Follitropin beta: Puregon®.
Type of procedure and Common odds ratio Risk difference (%)
follitropin used (95% confidence interval) (95% confidence interval)
IVF
Follitropin alpha 1.37 (1.05–1.79) 5.4 (0.8–10.1)
Follitropin beta 1.19 (0.95–1.49) 3.5 (–1.0–7.9)
ICSI
Follitropin alpha 1.04 (0.73–1.47) 0.8 (–6.7–8.3)
Follitropin beta No data available No data available
IVF or ICSI
Overall total 1.21 (1.04–1.42)
Table 4. Milestones in the development of recombinant human gonadotrophins (data modified
according to Howles, 1996).
1972 First recombinant DNA molecules generated at Stanford University, CA, USA
1979 Human insulin was cloned in bacterial cells
1979 Human chorionic gonadotrophin α-subunit cloned
1983 Amino acid sequence of human β-FSH subunit established
1985 Human β-FSH gene cloned, and biologically active FSH was expressed in
mouse fibroblast cells
1988 Human FSH expressed in continuous mammalian cell line (CHO)
1989–1990 Serono established a master cell bank and working cell bank, from which all
cells originate, which produce recombinant human FSH (Gonal F®)
1990 First batch of recombinant human FSH made for clinical studies
1992 First pregnancy using recombinant human FSH following an IVF cycle in
Switzerland and Belgium
1995 Gonal F® is the first pharmaceutical to be granted European-wide marketing
approval by the European Medicines Evaluation Agency
1996 Puregon® is registered in Europe
1997 First pregnancy following use of only recombinant gonadotrophins
(recombinant human FSH, LH and HCG) in a woman suffering from WHO I
amenorrhoea (Agrawal et al., 1997)
2000 European registration of recombinant human LH (Luveris®)
2001 European registration of recombinant human HCG (Ovidrel®/Ovitrelle®)
Luveris® = recombinant human LH; Ovitrelle® = recombinant HCG.
recombinant human gonadotrophins, and both recombinant days, when pituitary LH secretion has been suppressed, the
human LH and recombinant human HCG are now available on patient receives gonadotrophins until the follicles reach an
the market. Milestones in the development of the recombinant appropriate size and HCG can be given to induce ovulation.
human gonadotrophins are shown in Table 4. This protocol has now been used as the stimulation protocol of
choice for nearly two decades. In Germany, for example, it is
Use of GnRH analogues in ovarian used in 65% of all IVF cycles.
stimulation procedures GnRH antagonists have also been developed in parallel with
For many years, premature LH surges leading to poor-quality the GnRH agonists. At first, the former had the disadvantage
oocytes and embryos, and low implantation and pregnancy of stimulating histamine release, with the consequent problems
rates, were a common complication of ovarian stimulation. In of allergic reactions. In, 1999, however, cetrorelix
1983, however, a GnRH agonist, buserelin, was used for the (Cetrotide®, Serono International S.A., Geneva, Switzerland)
first time to suppress endogenous LH surges according to a was introduced to the market originally by ASTA Medica
treatment protocol termed the ’long GnRH agonist protocol’ (Frankfurt, Germany), and this was followed a year later by
(Porter et al., 1984). This protocol involves the administration ganirelix (Orgalutran®, Antagon®, Organon, Oss, The
of a GnRH agonist starting on either the early follicular or the Netherlands). Neither of these GnRH antagonists significantly
mid-luteal phase of the preceding menstrual cycle. After 14 stimulates histamine release. They are both administered once 81
Reprinted from Vol. 5, Suppl. 1 (2002) pp. 73 86. S11
Ovarian stimulation: from basic science to clinical application - M Ludwig et al.
Figure 10. Ovarian stimulation using GnRH
antagonists. Shown are the multiple-dose (a) and the
single-dose (b) protocols. In the standardized
multiple dose protocol, gonadotrophin administration
starts on day 2 or 3 following spontaneous menstrual
bleeding. The GnRH antagonist is given starting on
day 6 of ovarian stimulation (0.25 cetrorelix or
ganirelix). It is administered up to and including the
day of HCG. In the single dose protocol (b) the
GnRH antagonist is given only once (3 mg
cetrorelix), on day 7 of ovarian stimulation, i.e. day 8
of the cycle. This will protect against a premature LH
b surge for about 96 h.
daily at a dose of 0.25 mg (Figure 10). Cetrorelix is also Novel delivery systems
available as a 3 mg dose, allowing a single administration
during the mid-follicular phase which guarantees pituitary Follitropin alpha is available as a multidose presentation, one
suppression for 96 h (Chillik and Acosta, 2001; Howles, ampoule containing the equivalent of fourteen 75 IU doses of
2002). recombinant human FSH. Once reconstituted, this
gonadotrophin solution can be stored at room temperature for
The major advantages of using GnRH antagonists rather than up to 28 days (Munafo et al., 2001).
GnRH agonists for ovarian stimulation are discussed
extensively in other publications in this supplement (Ludwig et In the last 2 years, sophisticated injection methods have been
al., 2002). Briefly, these include a shorter duration of developed. The autoinjecting Puregon Pen® (follitropin beta
treatment, no flare-up effect and hence no risk of cyst administered by a pen device, Organon, Oss, The
formation, no depletion of sex steroids and the consequent side Netherlands), for example, allows the dose administered to be
effects, a shorter period of ovarian stimulation and hence the altered in 25 IU increments, enabling the adjustment of the
administration of a lower cumulative dose of gonadotrophins, required dose. The pen device for administering follitropin
and a lower risk of OHSS. However, several studies have also beta developed from a device used for long-term delivery of
investigated the possibility of a lower pregnancy rate with insulin to diabetic patients, and is a welcome addition to the
GnRH antagonists (Olivennes et al., 2000; Albano et al., 2000; tools available to physicians treating infertility (Voortman et
The European Orgalutran Study Group et al., 2000). al., 1999). Both follitropin beta administered by a pen device
and the multidose presentation of follitropin alpha allow the
Further prospective, randomized studies are needed to injection of a very low volume of gonadotrophin, which
determine whether there are actually any differences between increases patient comfort during treatment.
the different GnRH antagonists or between GnRH agonists or
antagonists (Ludwig et al., 2001). New recombinant human FSH
formulation: follitropin alpha filled by mass
Recent advances in ovarian
stimulation A new presentation of recombinant human FSH has recently
been developed by Serono S.A. This presentation, known as
With the advent of recombinant human gonadotrophins, Gonal F® filled by mass (FbM) (follitropin alpha FbM;
ovarian stimulation procedures have become safer and more Serono International S.A., Geneva, Switzerland), differs from
convenient for the patient than ever before. In particular, conventional follitropin alpha in that the product is filled by
gonadotrophins can now be administered by subcutaneous protein content (mass in micrograms) rather than by biological
injection, which makes self-administration a viable option. activity. It is claimed that follitropin alpha FbM is produced
Patients can therefore administer their own treatment at home,
82 making it simpler, cheaper and more convenient.
using an improved manufacturing process, which employs
physico-chemical techniques rather than an in-vivo bioassay to
S12 Reprinted from Vol. 5, Suppl. 1 (2002) pp. 73 86.
Ovarian stimulation: from basic science to clinical application - M Ludwig et al.
measure the amount (mass) of FSH protein added to each vial known relationship between isoform profile and activity, this
during filling (Driebergen et al., 2002). means that the calculated weight of FSH protein consistently
delivers the same biological activity. In recognition of this fact,
The biological activity of FSH derives from the sequence of vials of follitropin alpha FbM are labelled by mass (and by
amino acids in its α- and β-chains, and from the specific biological activity), and a SE-HPLC assay is used to test the
pattern of glycosylation. Different isoforms of FSH exist due strength/potency of this product (Driebergen et al., 2002).
to different patterns of glycosylation of the parent molecule.
Sialic acid residues play a major role in protecting the Clinical experience with follitropin alpha
molecule against rapid metabolic clearance in vivo. For this FbM
reason FSH isoforms show differences in in-vivo bioactivity
which are related to differences in isolelectric point (pI). In a multicentre, prospective, randomized, comparative trial,
Isoforms with a pI around 3.5 are 100–200 times more potent 456 women undergoing IVF were treated with either
in the in-vivo bioassay than isoforms with a pI of 5.5–6.0. follitropin alpha FbM (220 patients) or follitropin alpha (223
Current preparations of recombinant human FSH contain a patients) according to a long luteal protocol for an average of
mix of the different isoforms. 9.7 ± 1.8 and 10.2 ± 1.8 days respectively. The average number
of ampoules of follitropin alpha used was significantly lower
It is well recognized in the biopharmaceutical industry that the (26.1 ± 10.3) for patients treated with the FbM formulation
use of an in-vivo bioassay to determine the biopotency of a than for those treated with the standard formulation (29.3 ±
drug has many disadvantages: it requires the use of many 11.9; P < 0.01). The oestradiol concentration on the day of
animals, typically 120–180 to obtain a single test result, and it HCG administration was significantly higher in the follitropin
is imprecise, inaccurate and not environmentally friendly. The alpha FbM group than in the group receiving conventional
coefficient of variation for an in-vivo bioassay is typically follitropin alpha (7792 ± 4911 versus 6642 ± 4219 pmol/l; P <
around 10%, which cannot compare to the performance of 0.01), and the number of retrieved oocytes (11.9 ± 6.3 versus
physico–chemical analytical techniques such as size exclusion 10.8 ± 6.8; P = 0.052) was greater. Consequently, the total
high-performance liquid chromatography (SE-HPLC), for number of embryos obtained was also higher in the follitropin
which the coefficient of variation is typically 2–3%. The new alpha FbM group (6.5 ± 4.0 versus 5.7 ± 3.7; P < 0.05). The
manufacturing process for follitropin alpha FbM involves the researchers concluded that improvements in the manufacturing
use of two physico-chemical techniques to ensure the process for recombinant human human FSH were responsible
consistency of the preparations – glycan mapping and for this increase in quality of the product (Abuzeid et al., 2001;
isoelectric focusing. A highly precise SE-HPLC assay is used Neuspillier et al., 2002). This was confirmed by another
to quantify accurately the drug substance content in the prospective, randomized, double-blind study. In this study
product. follitropin alpha, coming from four bulk lots of r-hFSH, was
filled to eight batches, one batch filled by the conventional
The glycan mapping method provides a fingerprint of the bioassay and one filled by mass, so that two batches came from
glycan species of r-hFSH and an estimation of the degree of each bulk lot. The results showed more consistency and less
sialylation of the oligosaccharide chains. After release from between-batch variation using the follitropin alpha FbM as
the protein by hydrazinolysis, the intact glycan species are compared with the conventional follitropin alpha (Hugues et
labelled with a fluorescent derivative. Each glycan molecule is al., 2002).
labelled with a single molecule of dye reagent. The response
coefficient is therefore the same for all the glycan species. The Long-acting recombinant human FSH
glycan species are then separated according to charge by anion
exchange chromatography, and detected by fluorimetry. Under Two different ways of developing long-acting gonadotrophin
these conditions, the glycan species are eluted as a function of preparations are currently under investigation. Such
their charge, which is related to the number of sialic acids they preparations should enable gonadotrophins to be injected only
carry. The results are expressed as the relative percentage of once or twice during a stimulation cycle rather than daily, as is
the glycan species grouped as a function of their charge. A currently the case.
hypothetical charge number Z has been defined as the sum of
the percent areas under the curve in the neutral, mono-, di-, tri- The results achieved with a long-acting FSH molecule in an
and tetra-sialylated glycan regions multiplied by their international, multicentre trial were published recently
corresponding charge (Hermentin et al., 1996). (Bouloux et al., 2001). This molecule consisted of the original
FSH α subunit and a hybrid β-subunit and was synthesized by
Isoelectric focusing (IEF) of r-hFSH is performed in a suitable Organon (Oss, The Netherlands). The latter was made from the
gel matrix across a pH range of 3.5–7 and visualized by original FSH molecule and the c-terminal peptide (CTP) from
Coomassie Brilliant Blue staining. The gel is then scanned and HCG. The idea for this design came from the observation that
the pI values as well as band intensities of the sample isoforms CTP is the main distinguishing feature between LH and HCG,
are compared with those obtained for the Reference House and may therefore be responsible for the prolonged half-life of
Standard. It can therefore be concluded that the drug substance HCG. Indeed, this newly designed FSH molecule is reported to
produced by the commercial manufacturing process is highly have a half-life in animals and in-vivo bioactivity that are two
consistent in isoform distribution. times greater than those of natural FSH (Bouloux et al., 2001).
When the molecule was administered to 13
Use of these techniques enables the consistency of the hypogonadotrophic males, no drug-related adverse events
manufactured product to be guaranteed in terms of both were observed, although symptoms of mild local tolerance
glycosylation pattern and isoform profile. Because of the symptoms occurred in 39% of the subjects. These symptoms 83
Reprinted from Vol. 5, Suppl. 1 (2002) pp. 73 86. S13
Ovarian stimulation: from basic science to clinical application - M Ludwig et al.
lasted for more than 24 h in 31% of subjects. No antibodies to Agrawal R, West C, Conway GS et al. 1997 Pregnancy after
either component of the FSH molecule were observed, and the treatment with three recombinant gonadotropins. Lancet 349,
elimination half-life was reported to be 94.7 ± 26.2 h, which is 29–30.
Albano C, Felberbaum RE, Smitz J et al. 2000 Controlled ovarian
2–3 times longer than that of natural FSH (Bouloux et al.,
stimulation with HMG: results of a prospective randomized phase
2001). The data from female patients have not yet been III European study comparing the LHRH-antagonist Cetrorelix
published. (Cetrotide) and the LHRH-agonist Buserelin. Human
Reproduction 15, 526–531.
Serono International S.A. is also developing a novel, long- Aschner B 1912 Ueber die Beziehung zwischen Hypophysis und
acting formulation of recombinant human FSH (Dr Steve Genitale. Archives of Gynecology 97, 200–227.
Arkinstall, Serono International S.A., personal Beclere A 1926 [Article title unavailable]. Paris Medical 13, 97.
communication). The new formulation is based on Alkermes’ Bettendorf G 1963 Human hypophyseal gonadotropin in
hypophysectomized women. International Journal of Fertility 8,
ProLease injectable sustained-release drug delivery
799.
technology, which involves the encapsulation of a drug into Borth R, Lunenfeld B, de Watteville H 1954 Activité gonadotrope
small polymeric microspheres. These degrade slowly and d’un extrait d’urines de femmes en menopause. Experientia 10,
release the encapsulated drug at a controlled rate following 266–270.
subcutaneous or intramuscular injection. The new formulation Bouloux PM, Handelsman DJ, Jockenhovel F et al. 2001 First
is designed to offer patients the alternative of a single injection human exposure to FSH-CTP in hypogonadotrophic hypogonadal
rather than multiple daily injections. Data on this formulation males. Human Reproduction 16, 1592–1597.
have yet to be published. Chillik C, Acosta A 2001 The role of LHRH agonists and
antagonists. Reproductive BioMedicine Online 2, 120–128.
Cluroe AD, Synek BJ 1995 A fatal case of ovarian hyperstimulation
Non-peptide molecules syndrome with cerebral infarction. Pathology 27, 344–346.
Cochius JI, Burns RJ, Blumbergs PC et al. 1990 Creutzfeldt–Jakob
As knowledge about the activating sites of gonadotrophins and disease in a recipient of human pituitary-derived gonadotrophin.
GnRH analogues has increased, it has become possible to Australia and New Zealand Journal of Medicine 20, 592–593.
create small, non-peptide molecules that induce signal Cole HH, Hart GH 1930 The potency of blood serum of mares in
transduction without binding to the extracellular domains of progressive stages of pregnancy in effecting the sexual maturity
membrane proteins. Such molecules will ultimately be of the immature rat. American Journal of Physiology 93, 57–68.
converted into highly potent orally active therapeutic Crowe SJ, Cushing H, Homans J 1910 Experimental
hypophysectomy. Bulletin of the Johns Hopkins Hospital 21,
preparations, and will replace the dimeric glycoprotein
127–167.
hormones or will act as antagonists. A number of these Cummins J 1999 Evolutionary forces behind human infertility.
molecules are already being actively tested. It is therefore Nature 397, 557–558.
feasible that the future of ovarian stimulation will be a simple Daya S 2002 Updated meta-analysis of recombinant follicle-
treatment schedule composed of different tablets, which have stimulating hormone (FSH) versus urinary FSH for ovarian
to be taken at certain time points during the ovarian stimulation in assisted reproduction. Fertility and Sterility 77,
stimulation cycle. 711–714.
Daya S, Gunby J, Hughes EG et al. 1995 Follicle-stimulating
hormone versus human menopausal gonadotropin for in vitro
The future of ovarian stimulation fertilization cycles: a meta-analysis. Fertility and Sterility 64,
347–354.
Over the next 5–10 years, it is envisaged that more Daya S, Ledger W, Auray JP et al. 2001 Cost-effectiveness
sophisticated use of GnRH antagonists will lead to their modelling of recombinant FSH versus urinary FSH in assisted
widespread use in ovarian stimulation protocols. The reproduction techniques in the UK. Human Reproduction 16,
gonadotrophin of choice will be recombinant human FSH, 2563–2569.
since it guarantees a consistent structure and biological Donini P, Puzzuoli D, Montezemolo R 1964 Purification of
activity. Where necessary, LH can be added to the protocol by gonadotropin from human menopausal urine. Acta
Endocrinologica 45, 329.
the administration of recombinant LH, and ovulation will be
Donini P, Puzzuoli D, D’Alessio C et al. 1966 Purification and
induced using recombinant HCG. Also, fixed combinations of separation of follicle-stimulating hormone (FSH) and luteinizing
recombinant LH and recombinant human FSH may be an hormone (LH) from human postmenopausal gonadotrophin
attractive option. (HMG). Acta Endocrinologica 52, 169–185.
Driebergen R, Bassett R, Baer G et al. 2002 Improvements in
Technology has come a long way since the era of animal-, quantification of recombinant human FSH activity: SE-HPLC
human pituitary- and urinary-derived hormones, and it seems versus the in-vivo rat bioassay. Human Reproduction (Abstract
clear that new pharmaceutical products will offer the safest book) 17, 163.
Dumble LJ, Klein RD 1992 Creutzfeldt–Jakob legacy for Australian
option for ovarian stimulation during assisted reproductive
women treated with human pituitary gonadotropins. Lancet 340,
techniques. 847–848.
Eshkol A, Lunenfeld B 1967 Purification and separation of follicle
References stimulating hormone (FSH) and luteinizing hormone (LH) from
human menopausal gonadotrophin (HMG). Acta Endocrinologica
Abuzeid MI, Kelly E, Loumaye E et al. 2001 A new formulation of 54, 919–927.
Gonal-F (r-hFSH) filled by mass delivers more and better oocytes Fauser BC, Donderwinkel P, Schoot DC 1993 The step-down
and embryos with a lower cumulative dose when compared with principle in gonadotrophin treatment and the role of GnRH
the current follitropin alfa preparation in ovarian stimulation for analogues. Baillieres Clinical Obstetrics and Gynaecology 7,
ART. Preliminary data. Middle East Fertility Society Journal 6, 309–330.
O33. Fevold HL, Hisaw FL, Leonard SL 1931 The gonad stimulating and
84
S14 Reprinted from Vol. 5, Suppl. 1 (2002) pp. 73 86.
Ovarian stimulation: from basic science to clinical application - M Ludwig et al.
the luteinizing hormones of the anterior lobe of the pituitary. ovarian hyperstimulation syndrome and health of children born.
American Journal of Physiology 109, 655–665. Reproductive BioMedicine Online 5 (suppl. 1), 61–67.
Finkler RS 1949 Evaluation of hormonal and radiation therapy in, Ludwig M, Tölg R, Richardt G et al. 1999b Myocardial infarction
190 cases of functional sterility and secondary amenorrhea. associated with ovarian hyperstimulation syndrome. JAMA 282,
Preliminary report. American Journal of Obstetrics and 632–633.
Gynecology 58, 559–564. Lunenfeld B 1963 Treatment of anovulation by human
Gemzell CA, Diszfalusy E, Tillinger, G 1958 Clinical effect of gonadotropins. International Journal of Obstetrics and
human pituitary follicle stimulating hormone. Journal of Clinical Gynecology 1, 153.
Endocrinology and Metabolism 18, 138–148. Lunenfeld B 1995 Infertility throughout the ages. In: AT Alberda, RA
Giudice E, Crisci C, Altarocca V, O’Brien M 2001 Characterization Gan, HM Vemer (eds) Proceedings of a symposium held in Oss,
of a partially purified human menopausal gonadotropin The Netherlands, 1993. Parthenon Publishing Group, New York,
preparation. Journal of Clinical Research 4, 27–34. London, pp. 55–71.
Groot-Wassink K, Blawert H 1973 Vergleichende Untersuchungen Lunenfeld B, Menzi A, Volet B 1960 Clinical effects of human post-
zur Ovulationsauslösung mit Follistiman und Pergonal. menopausal gonadotrophin. In: F Fuchs (ed.) Advance Abstracts
Zentralblatt for Gynakologie 9, 1019–1024. of Short Communications. First International Congress of
Guillemin R 1967 Chemistry and physiology of hypothalamic Endocrinology, Copenhagen, p. 587.
releasing factors for gonadotrophins. International Journal of Lunenfeld B, Rabau E, Rumney G, Winkelsberg G 1961 The
Fertility 12, 359–367. responsiveness of the human ovary to gonadotrophin. (Hypophsis
Halberstaedter L 1905 [Article title unavailable]. Berlin Klinische III). Proceedings of Third World Congress Gynecology and
Wochenschrift 42, 64. Obstetrics, Vienna 1, 220.
Hermentin P, Witzel R, Kanzy E-J et al. 1996 The hpothetical N- Lunenfeld B, Sulimovici S, Rabau E, Eshkol A 1962 L’induction de
glycan charge: a number that characterizes protein glycosylation. l’ovulation dans les amenorrheas hypophysaires par un traitement
Glycobiology 6, 217–230. combine de gonadotrophins urinaires menopausiques et de
Howles CM 1996 Genetic engineering of human FSH (Gonal-F). gonadotrophins chorioniques. Comptes Rendus de la Société
Human Reproduction Update 2, 172–191. Française de Gynecologie 32, 346.
Howles CM 2002 The place of gonadotrophin-releasing hormone Mazer C 1946 Diagnosis and Treatment of Menstrual Disorders and
antagonists in reproductive medicine. Reproductive BioMedicine Sterility. Paul B. Hoeber, New York.
Online 4, 64–71. Mazer C, Greenberg R 1943 Low dosage irradiation in the treatment
Howles C, Loumaye E, Giroud D, Luyet G 1994 Multiple follicular of amenorrhea. American Journal of Obstetrics and Gynecology
development and ovarian steroidogenesis following subcutaneous 46, 648–652.
administration of a highly purified urinary FSH preparation in Melmed H, Mashiach S, Insler V et al. 1969 The response of the
pituitary desensitized women undergoing IVF: a multicentre hyposensitive ovary to massive stimulation with human
European phase III study. Human Reproduction 9, 424–430. gonadotrophins. Journal of Obstetrics and Gynaecology of the
Hugues JN 2001 Recombinant human follicle-stimulating hormone: a British Commonwealth 76, 437–443.
scientific step to clinical improvement. Reproductive BioMedicine Mozes M, Bogokowsky H, Antebi E et al. 1965 Thromboembolic
Online 2, 54–64. phenomena after ovarian stimulation with human gonadotrophins.
Hugues JN, Cedrin-Durnerin I, Avril C et al. 1996 Sequential step-up Lancet 2, 1213–1215.
and step-down dose regimen: an alternative method for ovulation Munafo A, Bilham W, Trinchard-Lugan I, Buraglio M 2001
induction with follicle-stimulating hormone in polycystic ovarian Comparative bioavailability and safety of a single dose and a
syndrome. Human Reproduction 11, 2581–2584. multiple dose formulation of recombinant human follicle
Hugues JN, Barlow DH, Rosenwaks Z et al. 2002 A new filled-by- stimulating hormone (Gonal-F). Journal of Clinical Research 4,
mass manufacturing process for Gonal F delivers a more 12–26.
consistent clinical response. Human Reproduction (Abstract Neuspillier N, Kelly E, Denton G et al. 2002 Technical
book) 17, 88. improvements in the Gonal F (filled by mass) manufacturing
Kaplan I 1948 The use of high voltage roentgentherapy in the process yield improved clinical results. Human Reproduction
treatment of amenorrhea and sterility in women. American (Abstract book) 17, 71–72.
Journal of Roentgenology 59, 3703–3779. Olivennes F, Belaisch-Allart J, Emperaire JC et al. 2000 A
Knobil E 1974 On the control of gonadotropin secretion in the rhesus prospective randomized controlled study in IVF-ET with a single
monkey. Recent Progress in Hormone Research 30, 1–46. dose of a LH-RH antagonist (Cetrorelix) or a depot formula of a
Knobil E 1980 The neuroendocrine control of the menstrual cycle. LH-RH agonist (Triptorelin). Fertility and Sterility 73, 314–320.
Recent Progress in Hormone Research 36, 53–88. Ostergaard E 1942 Antigonadotrophic Substances. Munksgaard,
Knobil E 1988 The neuroendocrine control of ovulation. Human Copenhagen, Denmark.
Reproduction 3, 469–472. Plant TM, Nakai Y, Belchetz P et al. 1978 The sites of action of
le Cotonnec JY, Porchet HC, Beltrami V, Howles C 1993 estradiol and phentolamine in the inhibition of the pulsatile,
Comparative pharmacokinetics of two urinary human follicle circhoral discharges of LH in the rhesus monkey (Macaca
stimulating hormone preparations in healthy female and male mulatta). Endocrinology 102, 1015–1018.
volunteers. Human Reproduction 8, 1604–1611. Porter RN, Smith W, Craft IL et al. 1984 Induction of ovulation for
Ludwig M, Felberbaum RE, Diedrich K 2000 Deep vein thrombosis in-vitro fertilisation using buserelin and gonadotropins. Lancet 2,
during administration of HMG for ovarian stimulation. Archives 1284–1285.
of Gynecology and Obstetrics 263, 139–141. Risquez F 2001 Induction of follicular growth and ovulation with
Ludwig M, Finas DF, Al-Hasani S et al. 1999a Oocyte quality and urinary and recombinant gonadotrophins. Reproductive
treatment outcome in intracytoplasmic sperm injection cycles of BioMedicine Online 3, 54–72.
polycystic ovarian syndrome patients. Human Reproduction 14, Rodgers M, McLoughlin J, Peers N et al. 1994 Accumulation of
354–358. human chorionic gonadotrophin in the serum of patients during
Ludwig M, Katalinic A, Diedrich K 2001 Use of GnRH antagonists in-vitro fertilization treatment cycles with Pergonal. Human
in ovarian stimulation for ART compared to the long protocol: a Reproduction 9, 638–642.
meta-analysis. Archives of Gynecology and Obstetrics 265, Ron E, Boice JD Jr, Hamburger S, Stovall M 1994 Mortality
175–182. following radiation treatment for infertility of hormonal origin or
Ludwig M, Katalinic A, Felberbaum RE, Diedrich K 2002 Safety amenorrhoea. International Journal of Epidemiology 23,
aspects of GnRH antagonists in ovarian stimulation procedures: 1165–1173.
85
Reprinted from Vol. 5, Suppl. 1 (2002) pp. 73 86. S15
Ovarian stimulation: from basic science to clinical application - M Ludwig et al.
Rubin IC 1926 Sterility associated with habitual amenorrhea relieved 2000 Treatment with the gonadotrophin-releasing hormone
by X ray therapy. American Journal of Obstetrics and antagonist ganirelix in women undergoing ovarian stimulation
Gynecology 12, 76–82. with recombinant follicle stimulating hormone is effective, safe
Ryan KJ 1979 Granulosa–theca cell interaction in ovaria. Journal of and convenient: results of a controlled, randomized, multicentre
Steroid Biochemistry 11, 799–800. trial. Human Reproduction 15, 1490–1498.
Ryan KJ, Petro Z 1966 Steroid biosynthesis by human ovarian The European Recombinant Human LH Study Group 1998
granulosa and theca cells. Journal of Clinical Endocrinology Recombinant human luteinizing hormone (LH) to support
Metabolism 26, 46–51. recombinant human follicle-stimulating hormone (FSH)-induced
Schally AV, Nair RM, Redding TW, Arimura A 1971 Isolation of the follicular development in LH- and FSH-deficient anovulatory
luteinizing hormone and follicle-stimulating hormone-releasing women: a dose-finding study. The European Recombinant Human
hormone from porcine hypothalami. Journal of Biological LH Study Group. Journal of Clinical Endocrinology and
Chemistry 246, 7230–7236. Metabolism 83, 1507–1514.
Silverberg K, Daya S, Auray JP et al. 2002a Analysis of the cost Voortman G, van de Post J, Schoemaker RC, van Geerven JMA 1999
effectiveness of recombinant versus urinary follicle-stimulating Bioequivalence of subcutaneous injections of recombinant human
hormone in in vitro fertilization/intracytoplasmic sperm injection follicle stimulating hormone (Puregon(R)) by Pen-injector and
programs in the United States. Fertility and Sterility 77, 107–113. syringe. Human Reproduction 14, 1698–1702.
Silverberg K, Schertz J, Falk B, Beresniak A 2002b Impact of urinary Wetsel WC, Liposits Z, Seidah NG, Collins S 1995 Expression of
FSH price: a cost-effectiveness analysis of recombinant and candidate pro-GnRH processing enzymes in rat hypothalamus
urinary FSH in assisted reproduction techniques in the USA. and an immortalized hypothalamic neuronal cell line.
Reproductive BioMedicine Online 5, 265–269. Neuroendocrinology 62, 166–177.
Smith PE 1926 Hastening of development of female genital system Wetsel WC, Mellon PL, Weiner RI, Negro-Vilar A 1991 Metabolism
by daily hemoplastic pituitary transplants. Proceedings of the of pro-luteinizing hormone-releasing hormone in immortalized
Society for Experimental Biology and Medicine 24, 1311–1333. hypothalamic neurons. Endocrinology 129, 1584–1595.
Smith PE, Engle ET 1927 Experimental evidence of the role of World Health Organization 1973 Agents stimulatins gonadal function
anterior pituitary in development and regulation of gonads. in human. World Health Organization Technical Report Series,
American Journal of Anatomy 40, 159. pp. 514–520.
Snick HK, Snick TS, Evers JL, Collins JA 1997 The spontaneous Wildt L, Hausler A, Marshall G et al. 1981 Frequency and amplitude
pregnancy prognosis in untreated subfertile couples: the of gonadotropin-releasing hormone stimulation and gonadotropin
Walcheren primary care study. Human Reproduction 12, secretion in the rhesus monkey. Endocrinology 109, 376–385.
1582–1588. Wildt L, Diedrich K, van der Ven HH et al. 1986 Ovarian
Stanger JD, Yovich JL 1985 Reduced in vitro fertlization of human hyperstimulation for in-vitro fertilization controlled by GnRH
oocytes from patients with raised basal luteinizing hormone agonist administered in combination with human menopausal
levels during the follicular phase. British Journal of Obstetrics gonadotrophins. Human Reproduction 1, 15–19.
and Gynaecology 92, 385–393. Yen SSC 1999 Neuroendocrinology of reproduction. In: SSC Yen,
Steptoe PC, Edwards RG 1976 Reimplantation of a human embryo RB Jaffe, RL Barbieri (eds) Reproductive Endocrinology.
with subsequent tubal pregnancy. Lancet 1, 880–882. Saunders, Philadelphia, London, Toronto, Montreal, Sydney,
Steptoe PC, Edwards RG 1978 Birth after the reimplantation of a Tokyo, pp. 30–80.
human embryo. Lancet 2, 366. Zondek B 1926 Ueber die Funktion des Ovariums. Zeitschrift für
Stokman PG, De Leeuw R, van den Wijngaard HA et al. 1993 Geburtshilfe und Gynäkologie 90, 327.
Human chorionic gonadotropin in commercial human Zondek B 1930 Ueber die Hormone des Hypophysenvorderlappens.
menopausal gonadotropin preparations. Fertility and Sterility 60, Klinische Wochenschrift 9.
175–178. Zondek B, Aschheim S 1927 Das Hormon des
Sykes D, Out HJ, Palmer SJ, van Loon J 2001 The cost-effectiveness Hypophysenvorderlappens: Testobjekt zum Nachweis des
of IVF in the UK: a comparison of three gonadotrophin Hormons. Klinische Wochenschrift 6, 248–254.
treatments. Human Reproduction 16, 2557–2562. Zondek B, Sulman F 1942 The Antigonadotropic Factor. Williams
The European Orgalutran Study Group, Mannaerts BMJL, Borm G Wilkinsm Baltimore.
86
S16 Reprinted from Vol. 5, Suppl. 1 (2002) pp. 73 86.
You might also like
- Castor Oil Packs For Abdominal Adhesions ScarringDocument10 pagesCastor Oil Packs For Abdominal Adhesions ScarringWandarh Rh100% (1)
- Progestogens in Obstetrics and Gynecology 2015th Edition (PRG)Document213 pagesProgestogens in Obstetrics and Gynecology 2015th Edition (PRG)amenu_bizuneh100% (4)
- Cape Biology 2019 PDFDocument11 pagesCape Biology 2019 PDFFelecia Hutchins100% (1)
- Tuesday, October 19, 2004 2:30 P.M.: Supported By: NICHDDocument2 pagesTuesday, October 19, 2004 2:30 P.M.: Supported By: NICHDFerry DimyatiNo ratings yet
- 1 s2.0 S0301211503002112 MainDocument4 pages1 s2.0 S0301211503002112 MainDr. Eser AĞARNo ratings yet
- PIIS00150282990060Document4 pagesPIIS00150282990060lilou.magnaboscoNo ratings yet
- Uterine Fibroid ThermometryDocument7 pagesUterine Fibroid ThermometryEva YeungNo ratings yet
- Mild Ovarian Stimulation For IVFDocument17 pagesMild Ovarian Stimulation For IVFanyka2No ratings yet
- The Use of Acupuncture With in Vitro Fertilization: Is There A Point?Document10 pagesThe Use of Acupuncture With in Vitro Fertilization: Is There A Point?lu salviaNo ratings yet
- The Use of Medicinal Herbs in Gynecological and Pregnancy Related Disorders by Jordanian Women A Review of Folkloric Practice Vs Evidence BasedDocument19 pagesThe Use of Medicinal Herbs in Gynecological and Pregnancy Related Disorders by Jordanian Women A Review of Folkloric Practice Vs Evidence BasedAisy AndroidTVNo ratings yet
- Total Fasting The of Obesity: TreatmentDocument5 pagesTotal Fasting The of Obesity: TreatmentCarlos RiscoNo ratings yet
- Total Fasting The of Obesity: TreatmentDocument5 pagesTotal Fasting The of Obesity: TreatmentCarlos RiscoNo ratings yet
- V15n2a04 15Document1 pageV15n2a04 15Lalo Hernández cruzNo ratings yet
- Nuribjh 4541 PDFDocument10 pagesNuribjh 4541 PDFLucky SeptianisNo ratings yet
- Acupuncture As Adjunct Therapy For in Vitro Fertilization: Advisor: Paul Magarelli, MD, PHD, FacogDocument10 pagesAcupuncture As Adjunct Therapy For in Vitro Fertilization: Advisor: Paul Magarelli, MD, PHD, FacogDoctora SantanaNo ratings yet
- Jurnal Bo, MissabDocument4 pagesJurnal Bo, MissabDewi Ajeng RahmawatiNo ratings yet
- Incidence of Epidural Hematoma, Infection, and Neurologic Injury in Obstetric Patients With Epidural Analgesia/AnesthesiaDocument6 pagesIncidence of Epidural Hematoma, Infection, and Neurologic Injury in Obstetric Patients With Epidural Analgesia/Anesthesiarian00019No ratings yet
- Pregnancy Rate After Emergency Contraception With Single-Dose Oral Levonorgestrel in Japanese WomenDocument7 pagesPregnancy Rate After Emergency Contraception With Single-Dose Oral Levonorgestrel in Japanese WomenAnugerahIndahMarethaNo ratings yet
- Severe PsoriasisDocument4 pagesSevere PsoriasisAdelin Luthfiana FajrinNo ratings yet
- Application of Ultrasonography in Female Infertility: A Comprehensive ReviewDocument11 pagesApplication of Ultrasonography in Female Infertility: A Comprehensive ReviewNur Fitryanti Lubis100% (1)
- Mariott I 2010Document2 pagesMariott I 2010Susana RocheNo ratings yet
- Al-Hamdani2017 2Document9 pagesAl-Hamdani2017 2namratahans786No ratings yet
- A New Rapid and Effective Method For Treatment ofDocument6 pagesA New Rapid and Effective Method For Treatment ofVictoria TsoyNo ratings yet
- Therapy of Bovine Endometritis With Prostaglandin F: A Meta-AnalysisDocument15 pagesTherapy of Bovine Endometritis With Prostaglandin F: A Meta-AnalysisIndah frysay marbunNo ratings yet
- Piis1472648310001264 PDFDocument8 pagesPiis1472648310001264 PDFRahma Evasari LubisNo ratings yet
- Incidence of Epidural Hematoma, Infection, and Neurologic Injury in Obstetric Patients With Epidural Analgesia/AnesthesiaDocument6 pagesIncidence of Epidural Hematoma, Infection, and Neurologic Injury in Obstetric Patients With Epidural Analgesia/AnesthesiaBig TexNo ratings yet
- Endo Study 2013Document0 pagesEndo Study 2013Agent Orange LegacyNo ratings yet
- Testosterone For The Treatment of Mammary and Prostate Cancers: Historical Perspectives and New DirectionsDocument17 pagesTestosterone For The Treatment of Mammary and Prostate Cancers: Historical Perspectives and New DirectionsClyde R.OrtegaNo ratings yet
- Male Reproductive Health and Environmental XenoestrogensDocument63 pagesMale Reproductive Health and Environmental XenoestrogensJamesNo ratings yet
- Pregnancy Rate After Emergency Contraception With Single-Dose Oral Levonorgestrel in Japanese WomenDocument7 pagesPregnancy Rate After Emergency Contraception With Single-Dose Oral Levonorgestrel in Japanese WomenAnugerahIndahMarethaNo ratings yet
- 15 Obstetric Anesthesia and Analgesia: Effects On The Fetus and NewbornDocument38 pages15 Obstetric Anesthesia and Analgesia: Effects On The Fetus and NewbornJenny MendozaNo ratings yet
- For A Post-Tubal Sterilization Syndrome?: Is There Any EvidenceDocument8 pagesFor A Post-Tubal Sterilization Syndrome?: Is There Any EvidenceSiva Deepthi SomuNo ratings yet
- Atrofia EndometrialDocument5 pagesAtrofia EndometrialFelipe ValenciaNo ratings yet
- Outpatient Management of Severe Ovarian Hyperstimulation Syndrome (OHSS) With Placement of Pigtail CatheterDocument7 pagesOutpatient Management of Severe Ovarian Hyperstimulation Syndrome (OHSS) With Placement of Pigtail CatheterDwi PurwantiNo ratings yet
- 45 Full PDFDocument4 pages45 Full PDFvilla88No ratings yet
- Del 484Document9 pagesDel 484tria nurdianaNo ratings yet
- Acupuncture For Uterine FibroidsDocument17 pagesAcupuncture For Uterine FibroidsTomas MascaroNo ratings yet
- Disruptores EndocrinosDocument16 pagesDisruptores EndocrinospalomitadanceNo ratings yet
- Bromelain, The Enzyme Complex of PineappleDocument13 pagesBromelain, The Enzyme Complex of PineappleEllisaTanNo ratings yet
- FOGSI FOCUS PTL-tocolyticDocument2 pagesFOGSI FOCUS PTL-tocolyticAnjali SharmaNo ratings yet
- CLINICS Botelho Et Al 2014Document8 pagesCLINICS Botelho Et Al 2014deboratomeNo ratings yet
- Enfermedad de Creutzfeldt-Jakob Iatrogénica Secundaria A Hormonas Hipofisiarias Cadavéricas.Document3 pagesEnfermedad de Creutzfeldt-Jakob Iatrogénica Secundaria A Hormonas Hipofisiarias Cadavéricas.JuanCk7No ratings yet
- Ajacm 2009 4 (1) Acup Improve EndometrDocument7 pagesAjacm 2009 4 (1) Acup Improve EndometrdirkvandeweyerNo ratings yet
- Enck2009 BiofeedbackDocument9 pagesEnck2009 BiofeedbackDuti YuriszkahNo ratings yet
- Principles and Practice of Controlled Ovarian Stimulation in ARTDocument418 pagesPrinciples and Practice of Controlled Ovarian Stimulation in ARTAnca Negreanu100% (1)
- 17-Alpha-Hydroprogesterone Caproate and Cervical ChangesDocument1 page17-Alpha-Hydroprogesterone Caproate and Cervical Changesari naNo ratings yet
- Nonhuman Primates A Vital ModelDocument14 pagesNonhuman Primates A Vital ModelLídia SilveiraNo ratings yet
- Case 3-1996Document6 pagesCase 3-1996K. O.No ratings yet
- PHRS DevelopmentOfThePillDocument2 pagesPHRS DevelopmentOfThePillsallyfrankenwarteNo ratings yet
- PII002822438690167XDocument11 pagesPII002822438690167XChristian VieryNo ratings yet
- Supported By: None.: AbstractsDocument1 pageSupported By: None.: AbstractsFerry DimyatiNo ratings yet
- The Effect of The "Laying On of Hands" On Transplanted Breast Cancer in MiceDocument12 pagesThe Effect of The "Laying On of Hands" On Transplanted Breast Cancer in MiceIvan Roca100% (2)
- 1479 6805 Joe 21 0449Document12 pages1479 6805 Joe 21 0449Salim MichaelNo ratings yet
- Lathyrism India Curative Treatment Jacoby 1946Document2 pagesLathyrism India Curative Treatment Jacoby 1946ennescribeNo ratings yet
- Daniel Scott, Fatima Elsayed, Joseph Wright, Inaki Moya, Grace CookDocument28 pagesDaniel Scott, Fatima Elsayed, Joseph Wright, Inaki Moya, Grace CookINAKI MOYANo ratings yet
- Hum. Reprod. 2009 Scarpellini 2703 8Document6 pagesHum. Reprod. 2009 Scarpellini 2703 8MitarXNo ratings yet
- Contraindications To Regional Anaesthesia in Obstetrics: A Survey of German PracticeDocument9 pagesContraindications To Regional Anaesthesia in Obstetrics: A Survey of German PracticeSyane TitaleyNo ratings yet
- Ibuprofen BookDocument259 pagesIbuprofen BookbabithyNo ratings yet
- Introduction to Clinical Reproductive EndocrinologyFrom EverandIntroduction to Clinical Reproductive EndocrinologyRating: 1 out of 5 stars1/5 (1)
- Antenatal CorticosteroidsDocument17 pagesAntenatal CorticosteroidsRolando DiazNo ratings yet
- Kuliah ADENOMYOSISDocument38 pagesKuliah ADENOMYOSISmarajuuNo ratings yet
- Oogonium) - Oogonia Are Diploid (2n) Stem Cells That Divide Mitotically To Produce Millions ofDocument2 pagesOogonium) - Oogonia Are Diploid (2n) Stem Cells That Divide Mitotically To Produce Millions ofstriata100% (1)
- WWW Bibliotecapleyades Net Sociopolitica Mindcontrol2 ApDocument11 pagesWWW Bibliotecapleyades Net Sociopolitica Mindcontrol2 Apapi-2317816750% (1)
- The Female Reproductive System Is Designed To Carry Out Several FunctionsDocument2 pagesThe Female Reproductive System Is Designed To Carry Out Several FunctionsArdie MingayNo ratings yet
- Ovarian CystsDocument16 pagesOvarian CystsKevin BaniwalNo ratings yet
- Bio12 c10 10 7Document8 pagesBio12 c10 10 7Eric McMullenNo ratings yet
- Fs p1 Prep Sept 2015 QP EngDocument15 pagesFs p1 Prep Sept 2015 QP Engapi-202349222No ratings yet
- TTTTTTTT VCHDocument22 pagesTTTTTTTT VCHkeltu123royNo ratings yet
- Drug Study #1Document7 pagesDrug Study #1Sarah Kaye BañoNo ratings yet
- OB/Gyn Clinical PearlsDocument4 pagesOB/Gyn Clinical PearlsD50% (4)
- Ob Review QuestionsDocument31 pagesOb Review QuestionsRandyNo ratings yet
- The Flo Guide To Glowing SkinDocument7 pagesThe Flo Guide To Glowing SkinDelphoneNo ratings yet
- Tog 12665Document13 pagesTog 12665saeed hasan saeed100% (1)
- Endocrinology NotesDocument24 pagesEndocrinology NotesEmily Dong100% (1)
- Human Reproduction Male Reproductive System: (Continued)Document11 pagesHuman Reproduction Male Reproductive System: (Continued)Meeta DeviNo ratings yet
- Infertility NirwenDocument55 pagesInfertility Nirwenpok yeahNo ratings yet
- Anatomy of The Female Pelvis FinalDocument209 pagesAnatomy of The Female Pelvis FinalMignot Aniley86% (14)
- Recombinant Human Luteinizing Hormone To Trigger Ovulation Randomized Controlled Dose Finding Pilot Study in Ovulation InductionDocument13 pagesRecombinant Human Luteinizing Hormone To Trigger Ovulation Randomized Controlled Dose Finding Pilot Study in Ovulation InductionDevansh ShethNo ratings yet
- UTS Module Version 2-1Document82 pagesUTS Module Version 2-1Shakira ChuNo ratings yet
- Reproductive System Old FormatDocument4 pagesReproductive System Old FormatRobie SanaoNo ratings yet
- Menstrual Cycle: G10 BiologyDocument17 pagesMenstrual Cycle: G10 BiologyCharlize Andrea DiestaNo ratings yet
- The Wisdom of Menopause by Christiane Northrup: The Physical Foundation of The Change (Excerpt)Document42 pagesThe Wisdom of Menopause by Christiane Northrup: The Physical Foundation of The Change (Excerpt)Random House Publishing Group91% (11)
- Menstrual CycleDocument46 pagesMenstrual CycleManilyn PenafloridaNo ratings yet
- Fontbonne 2020Document7 pagesFontbonne 2020ALAN RODRIGO ROJAS COVARRUBIASNo ratings yet
- Your Past Menstrual Cycles Will Work As A Guide For EstimatingDocument3 pagesYour Past Menstrual Cycles Will Work As A Guide For EstimatingBjtan TanNo ratings yet
- Physiology of MenstruationDocument6 pagesPhysiology of MenstruationgmindalanoNo ratings yet
- Hormones and Menstrual CycleDocument5 pagesHormones and Menstrual CycleJei TorresNo ratings yet
- % Chapter 4: Hormonal Control of Reproductive CycleDocument22 pages% Chapter 4: Hormonal Control of Reproductive CycleK CNo ratings yet
- Canine InfertilityDocument21 pagesCanine InfertilitygnpobsNo ratings yet