Professional Documents
Culture Documents
Implications For Managed Care and Specialty Pharmacy in Rheumatoid Arthritis
Uploaded by
Aline Leal CortesOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Implications For Managed Care and Specialty Pharmacy in Rheumatoid Arthritis
Uploaded by
Aline Leal CortesCopyright:
Available Formats
n reportS n
Implications for Managed Care and Specialty
Pharmacy in Rheumatoid Arthritis
William J. Cardarelli, PharmD
T
he European League Against Rheumatism (EULAR)
recently endorsed 3 overarching principles for the
Abstract
treatment of rheumatoid arthritis (RA).1 The prin-
Treatment of rheumatoid arthritis (RA) can
ciples state that rheumatologists are the specialists be very costly. Cost-effectiveness studies
who should primarily care for patients with RA, that the treat- provide insight into the value of treatment
ment of patients with RA should aim at the best care (based on from a number of perspectives (eg, soci-
a shared decision between the patient and the rheumatologist), etal, healthcare). In most cases, the indirect
and that RA is expensive with regard to medical costs and pro- costs of RA can offset the direct costs in 2
ways. Prevention of disease progression can
ductivity costs, both of which should be considered by the treat-
limit future costs, such as those related to
ing rheumatologist.1 The 2012 update of the 2008 American surgery and hospitalization. When disease
College of Rheumatology (ACR) recommendations for medica- progression is minimized, patients feel better
tion management of RA provides a written framework, based on and can have improved work productivity.
evidence, for handling the medication management of patients Disease control of RA has improved over
time, and this is attributed primarily to the
with RA, as outlined in the second article by Gibofsky in this
© Managed Care & introduction of more effective therapies.
supplement.2,3 This article will provide an overview of direct and
Healthcare Communications, LLC Despite the effectiveness of new therapies,
indirect costs associated with RA, with a focus on treatment- there are a number of barriers to optimal
related costs, the role of specialty pharmacy and managed care, treatment. Barriers include lack of education
and mechanisms to provide disease management that optimizes for patients and practitioners about RA, poor
economic outcomes. patient-provider communication, uncertainty
regarding which treatments to choose, cost,
and lack of adherence. Specialty pharmacy
Direct and Indirect Costs of RA
and disease therapy management programs
Significant patient, healthcare, and societal costs are associ- can assist patients by providing structure,
ated with RA. According to recent estimates, the per patient education, and mechanisms to improve treat-
annual direct medical cost of RA ranges from $2000 to $10,000. ment adherence and persistence to optimize
Estimates for indirect costs range from $1500 to $22,000.4,5 These therapy.
(Am J Manag Care. 2012;18:S315-S324)
costs depend on the cost estimates of the model, year of the
estimate, degree of inflation over time, severity of disease, and
treatment approach. To provide a degree of perspective, a study
conducted between 1993 and 1994 in a US group-model health
maintenance organization (HMO) compared resource utilization
and cost of care in 365 patients with RA with 10,101 patients
with osteoarthritis (OA).6 The average individual cost of arthri-
tis care was $2162 for RA and $543 for OA, a nearly 4-fold
greater cost for RA. In that study, the respective utilization of
various resources was compared, including prescription medica-
tion cost (62% vs 32% for RA and OA, respectively), ambulatory
care costs (21% vs 22%, respectively) and hospital visits (16% vs
46%, respectively). Despite the higher cost per patient for RA,
the total population cost was $703,053 for RA and $4,728,425
For author information and disclosures, see end of text.
for OA, suggesting that the HMO cost for RA was substantially
less (approximately 7-fold) than that for OA due to the relative
VOL. 18, No. 13 n The American Journal of Managed Care n S315
Reports
infrequency of RA.6 It is important to note that these data instruments (RA quality of life [QoL]), or combined with
are relatively old, and more expensive therapies have been mortality into a health utility, like the quality-adjusted life-
introduced for both diseases; therefore, if inflation were year (QALY).5 While mortality or cardiovascular events may
applied, the assumptions should be similar. not be tangible or measurable for most individual patients,
As suggested in the HMO study,6 medications account productivity and quality of life are important components of
for a large portion of the direct medical expenses associated indirect costs. Health benefits of RA treatment are expressed
with RA. Ambulatory care costs include primary care and in terms of pain, fatigue, and loss of function.5 Physical func-
specialist visits, urgent ambulatory care visits, joint imaging, tion may be monitored through the disability index of the
laboratory assessment, joint aspiration and injection, and Health Assessment Questionnaire (HAQ), and fatigue may
nerve conduction studies. Hospital care involves admission be measured using indices such as the Functional Assessment
for disease symptoms or adverse effects, admission for joint of Chronic Illness Therapy-Fatigue (FACIT-F). Fatigue
surgery (including joint replacement), emergency depart- occurs in about 90% of patients with RA. In a phase 3,
ment visits, physical therapy, and radiologic costs.6 Other placebo-controlled trial of golimumab, in patients who were
medical costs beyond treatment of joint disease in RA are inadequately responsive to methotrexate, HAQ (r = –0.62,
associated with extraarticular RA.7 Joyce and colleagues P <.01) and DAS28 score (r = –0.42, P <.01) were signifi-
sought to determine the attributable annual costs of cardio- cantly correlated with FACIT-F score.13 Fatigue was an inde-
vascular disease and depression coexistent with RA using a pendent predictor of physical function and disease activity,
healthcare claims database.7 Of 10,298 patients identified, and higher baseline FACIT-F scores (less fatigue) were more
8916 (86.6%) had RA alone, 608 (5.9%) had RA with car- likely associated with achieved remission at week 24 (P =
diovascular disease (CVD), 716 (7%) had RA with depres- .024). Golimumab was associated with improved FACIT-F
sion, and 58 (0.5%) had RA with depression and CVD. scores relative to placebo at week 12 (57.5% vs 42.8%, P
Adjusted mean total healthcare costs were highest in the RA <.001) and at week 24 (65.8% vs 40.3%, P <.001).13 These
plus CVD group ($14,145), followed by RA plus depression findings were confirmed with other TNF inhibitors.14,15 A
and CVD ($13,513), RA plus depression only ($12,225), recent systematic review and meta-analysis confirmed a
and RA alone ($11,404). The mean RA-related healthcare small, but significant, effect of any biologic agent in patients
costs were similar among groups ($6100-$6600), suggesting with an inadequate response to DMARDs or TNF inhibitors
that the extraarticular manifestations of RA are an impor- [effect size (ES), 0.45; 95% confidence interval [CI], 0.31-
tant component of the cost of healthcare.7 0.58]. An ES of less than 0.5 was considered small, 0.5 to
Cardiovascular complications associated with RA are an 0.8 was moderate, and greater than 0.8 was considered large.
important contributor to mortality in RA.8 An ideal therapy When TNF inhibitors plus DMARDs were compared with
would increase life expectancy and quality of life. In a recent placebo plus DMARDs, the ES was smaller (ES, 0.36; 95%
analysis of mortality with non-biologic disease-modifying CI, 0.21-0.51). When biotherapies (anti-TNF, rituximab, or
antirheumatic drugs (DMARDs) and tumor necrosis factor abatacept) plus DMARDs were compared with DMARDs
(TNF) inhibitors, rituximab, and other biologics, mortal- plus placebo for an inadequate response to DMARDs, the
ity per 1000 patient years adjusted for age, sex, treatment, ES was similar (ES, 0.38; 95% CI, 0.3-0.46). When abata-
and comorbid conditions was improved with TNF inhibitors cept, golimumab, or rituximab were given with DMARDs
relative to DMARDs (hazard ratio [HR], 0.65; P = .0004). and compared with placebo plus DMARDs for an inade-
Mortality associated with rituximab (HR, 0.81; P = .34) and quate response to TNF inhibitors, the ES was moderate (ES,
other biologics (HR, 0.84; P = .42) was similar to that asso- 0.57; 95% CI, 0.27-0.86).15 Thus, fatigue was minimized by
ciated with DMARDs. Across the population, each 1-point improved disease activity attained with aggressive treatment.
increase in the disease activity score in 28 joints (DAS28) Improvement in disease activity and fatigue can lead to
was associated with a 15% higher death rate (HR, 1.15; P functional improvement, which could improve work produc-
= .002). Increased prednisone use was also associated with tivity. Work disability associated with RA has been estima
higher mortality (HR per 5 mg/day increment of prednisone ted to be 3 times as expensive as the direct medical costs of
dose, 1.2; P = .003).9 The reduction in cardiovascular events managing the disease.5 Factors associated with work disabil-
with TNF inhibitors relative to DMARDs was demonstrated ity include the ability to retain employment, absenteeism,
in some,10,11 but not all, recent studies.12 early retirement, and reduced work performance. Significant
Health-related quality of life is measurable through a irreversible work disability usually occurs within 5 years of
number of general (Short Form-36) and disease-specific disease onset; however, by 1 year, about 20% of patients
S316 n www.ajmc.com n december 2012
Implications for Managed Care and Specialty Pharmacy in Rheumatoid Arthritis
are no longer engaged in full-time work, and this number initiation of treatment.21-23 Rather than provide an exhaus-
increases to about 50% by 15 years. The average disability tive review of all pharmacoeconomic studies for every avail-
costs are estimated at $10,000 per year. These estimates are able agent, this section will present select studies that focus
variable and depend on the type of output of the company on representative approaches to treatment, as suggested in
and the salary of the individual. Step activity is a measure the 2012 ACR treatment recommendations.2 The second
of functional capacity in RA. A recent study of etanercept article by Gibofsky in this supplement can be used to assess
demonstrated that step activity could be improved along differences among available treatments.3
with improvements in HAQ and DAS28 disease activity, A recent meta-analysis examined the impact of early
but this was only observed early in the disease (<5 years in treatment on radiographic progression in RA.24 Compared
duration), before irreversible joint damage occurred.16 A with early treatment initiation, delayed treatment initiation
number of studies have demonstrated improvement in work was associated with a –0.19 standardized mean difference
productivity with TNF inhibitor therapy compared with (95% CI, –0.34 to –0.04), which corresponded to a 33%
DMARD therapy in early RA.17-19 In 1 of those studies, etan- reduction (95% CI, –50% to –16%) in long-term progres-
ercept plus methotrexate improved work attendance by an sion (Figure 1). Patients with more aggressive disease dem-
estimated 22 to 37 days per patient, compared with metho- onstrated a greater benefit from DMARD initiation (P =
trexate alone. The associated cost of productivity gained, .04).24 A recent analysis compared the cost-effectiveness of
converted to US dollars, was approximately $2500 to $4000 6 DMARD-based approaches to early treatment, including
per person. When presenteeism (reduced work performance monotherapy, step-up combination, parallel combination,
on the job) was included, the estimate increased to $4700.17 intensive step-up combination, step-down combination, and
Thus, from a societal perspective, effective treatment of RA a steroid plus monotherapy (Table).25 Step-down combina-
could improve work productivity. From an employer per- tion therapy exceeded monotherapy, step-up, parallel, and
spective, a study evaluated direct and indirect costs of RA in steroid combinations, because it was less costly and more
patients compared with matched controls.20 The estimated effective, and thus dominated the other strategies with the
annual cost for a disabled patient with RA was $17,822, 3 exception of the intensive strategy. Comparing the remain-
times that of the average matched disabled control ($6131). ing strategy (intensive DMARD combination) to step-down
Disability was more common among employees with RA treatment, the estimated incremental cost-effectiveness
(44%) than other matched controls (22%). Work loss costs ratio (ICER) was £27,392. The authors assumed that deci-
for patients with RA, including disability and absentee- sion makers adopt a threshold of £20,000 (approximately
ism, were 1.6 times that of matched controls.20 Caution US$29,000) per QALY, thus the value of each strategy can
should be used when interpreting these data. A limitation be expressed in monetary terms; using QALY to determine
of modeling cost-effectiveness in RA is that extrapolation of a net benefit, the best strategy would be that with the great-
long-term benefits is often made with little or no long-term est net benefit. In this case, step-down combination therapy
data. If there were a way to determine which patients would (£258k) had the greatest net benefit and could be considered
have severe progressive disease or which medication would the most cost-effective.25
yield the best response in an individual patient, then the Another study compared sequential monotherapy, step-
cost-effectiveness numbers would improve substantially. As up combination, monotherapy with prednisone, and com-
research continues, we may find that early biologic interven- bination therapy with infliximab.26 Figure 2 demonstrates
tion may induce durable drug-free remission, which would the 2-year costs in 2008 euros (1 euro equals approximately
also improve the cost-effectiveness of these biologics. US$1.25) of these regimens using 3 different pharmaco-
economic models. The models show that infliximab had a
Treatment-Related Costs larger increase in QALYs, but that cost-effectiveness was
Costs of treatment include the cost of medication, tests only improved with work productivity in the human capital
for monitoring the effects (disease response) or adverse method. The friction method only accounts for productivity
effects of the drug, and administration costs (if applicable).5 losses up to 6 months, and assumes an employee is replaced
A number of studies have demonstrated that, over time, or back to work at that point. The human capital method
disease activity has improved in populations with RA. The accounts for sustained productivity. Thus, depending on
improvement in disease activity and increased attainment of the model, high-cost items could be cost-effective as long as
remission has been attributed to the introduction of newer cost utility is improved and work productivity is associated
therapies, an improved approach to treatment, and earlier with an improvement in QALYs.26 Thus, it appears that
VOL. 18, No. 13 n The American Journal of Managed Care n S317
Reports
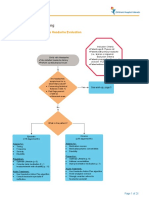
n Figure 1. Representation of DMARD Initiation by Study Type24
worse worse RCT RCT
start stop
Enrollment
X-ray Delayed
damage Delayed DMARD
DMARD
Early Early
DMARD DMARD
0 0
Time
Time
Delay period
Relative delay period
(= RCT duration)
A B
Representation of delayed disease-modifying antirheumatic drug (DMARD) initiation by study type. A, In cohort studies of patients with early rheumatoid
arthritis, long-term radiographic progression is contrasted between subsets with early versus delayed initiation of DMARD therapy. B, In a randomized
controlled trial (RCT), effective DMARD regimens are compared with placebo or a less-effective DMARD regimen. At the end of the RCT period, blinding
is removed and patients are free to receive any DMARD. In follow-up studies of these RCTs, delayed DMARD initiation is conceptualized as a relative
delay to effective DMARD therapy in the comparator arm compared with the active treatment arm. Studies that did not receive comparable DMARDs
during the follow-up period were excluded so that long-term radiographic progression could be compared with respect to the initial therapeutic strategy.
Shaded circles indicate DMARD initiation.
Reprinted with permission of Oxford University Press from Finckh A, Liang MH, van Herckenrode CM, de Pablo P. Arthritis Rheum. 2006;55(6):864-872.
aggressive treatment of early RA, compared with mono- cost-effective at a willingness to pay threshold of $50,000
therapy regimens, is cost-effective using step-down combi- per QALY. When patients who failed to respond to metho-
nation therapy or combination with a TNF inhibitor due to trexate combination therapy or sequential DMARD admin-
enhanced efficacy, improvements in QALY, and improved istration were compared with those who received additional
productivity. These results confirm other published find- DMARD sequencing or a biologic alone or in combination
ings.27-29 The lowest direct cost would be from DMARD with a DMARD, 14 of 35 (40%) comparisons had ICERs
optimization,27-29 but biologics as monotherapy are also con- below the $100,000 threshold. Median ICERs per QALY
sidered cost-effective, with ICERs ranging from $50,000 to were $81,000 (range, $63,000-$383,000) for adalimumab,
$100,000 (Figure 3).28 Consequently, biologics in combina- $79,000 (range, $60,000-$175,000) for adalimumab plus
tion with DMARDs for early RA have mostly proved not methotrexate, $127,000 (range, $45,000-$612,000) for etan-
to be-cost-effective, due to ICERs greater than $100,000 ercept, $75,000 (range, $72,000-$134,000) for etanercept
in 6 of 7 (85.7%) studies.28 Figure 3 also demonstrates that plus methotrexate, and $133,000 (range, $80,000-$378,000)
when initial therapy fails, biologics after DMARD failure for infliximab plus methotrexate.30 When biologics were
had ICERs less than $100,000 in 14 of 18 studies (77.8%), evaluated after TNF inhibitor failure in 4 studies, ritux-
and biologics after TNF inhibitor failure had ICERs less imab and abatacept had ICER values less than $50,000 per
than $100,000 in 4 out of 4 studies (100%).28 A separate QALY, and abatacept and etanercept had ICER values less
systematic review of biologics for DMARD failure evaluated than $100,000 in 2 of the studies (Figure 3). Thus, biologic
several scenarios using 2009 Canadian dollars ($1 Cana- agents have the potential to be cost-effective, especially
dian equals approximately US$1.01).30 When methotrexate when used in combination with DMARDs for DMARD fail-
monotherapy failed, methotrexate monotherapy was com- ure, and are cost-effective for TNF inhibitor failure, particu-
pared with biologic combination with methotrexate, and larly when rituximab or abatacept are used.28
all 20 comparisons found ICER values ranging from $6000
to $92,000, suggesting cost-effectiveness at a willingness to Role of Managed Care and Specialty Pharmacy
pay threshold of $100,000 per QALY. Seven of 12 (58.3%) Given the data on efficacy of pharmaceuticals in RA,
of these comparisons conducted from a societal perspective managed care organizations have been left with a difficult
and 2 of 8 (25%) from a payer perspective found the therapy decision regarding the most effective allocation of agents for
S318 n www.ajmc.com n december 2012
Implications for Managed Care and Specialty Pharmacy in Rheumatoid Arthritis
n Table. Cost-Effectiveness Results of Initial Non-Biologic Therapy for Early RA25
ICER
(compared with Incremental Net Benefit Net Benefit
Strategya Cost QALY monotherapy) Analysisb (£20,000) Rank
Monotherapy £55,996 13.73 — Dominated £218,604 3
Step-up combination £50,791 11.91 £2852 Dominated £187,409 5
Parallel combination £55,573 13.42 £1356 Dominated £212,827 4
Intensive step-up £61,046 15.77 £2482 £27,392 £254,354 2
combination
Step-down £48,849 15.32 Cost saving Reference £257,551 1
combination strategy
Steroid plus £57,468 11.79 Dominated Dominated £178,332 6
monotherapy
DMARD indicates disease-modifying antirheumatic drug; ICER, incremental cost-effectiveness ratio; QALY, quality-adjusted life-year; RA, rheumatoid
arthritis.
a
Monotherapy = DMARD monotherapy; step-up combination = patients begin with DMARD monotherapy, and a second DMARD is added if an
inadequate response is observed (within first 6 months); parallel combination = 2 or more DMARDs given in combination at the same time; intensive
step-up combination = patients begin with a DMARD parallel combination strategy, and rapid dose increases are made when an inadequate response
is observed (within first 6 months); step-down combination = initial parallel combination followed by downward dose titration and withdrawal; steroid
plus monotherapy = glucocorticoids routinely used alongside a DMARD monotherapy regimen. The other combination strategies use steroids on an
“as needed” basis.
b
Incremental comparisons are against the next-best, nondominated treatment strategy.
Reprinted with permission from Tosh JC, Wailoo AJ, Scott DL, Deighton CM. J Rheumatol. 2011;38(8):1593-1600.
optimal disease management. Historically, specialty items important factors in adherence to RA treatment were the
like the biologics were covered under the medical benefit. relationship between the patient and the provider, and the
Under the medical benefit, where agents were primarily belief that the medication was necessary.35 In another study,
given in the physician’s office, it was difficult to track agent factors important in filling the initial DMARD prescription
selection and sequence, as it was done for adjudicated claims included communication with, and trust in, the rheuma-
through a pharmacy benefit management (PBM) company.31 tologist, and perceptions about the medication, such as per-
However, costs for specialty drugs have been increasing ceived adverse effects. Factors associated with subsequent
while those for traditional medications remain static, and adherence included experience with the medication (eg,
the market for RA medications is expected to increase.32,33 In development of adverse effects), ability to fit the medication
an effort to control selection and sequence of agents, PBM schedule into daily life, and level of engagement in decision
companies acquired or contracted with specialty pharma- making.36 The final factor determining adherence appears to
cies to manage administration of high-cost medications. By be the medication itself. One recent study identified differ-
managing these medications as part of the pharmacy benefit, ences in adherence and discontinuation between anakinra,
specialty pharmacies ensure safe handling, restrict drug dis- infliximab, and etanercept.37 The proportion of days covered
tribution, and can contract with pharmaceutical companies (goal ≥0.8) was 0.36 for anakinra, 0.57 for etanercept, and
to get better acquisition rates and pass the savings along to 0.64 for infliximab, with respective adherence rates of 11%,
the payers and patients compared with physician offices and 32%, and 43%, and discontinuation rates of 76%, 41%, and
clinics.31 An important factor in treatment adherence, and 41%.37 These data highlight the importance of the relation-
hence efficacy of an agent, is the amount of cost-sharing a ship between a patient and their provider, the need for edu-
patient has to bear. A recent study indicated that for patients cation, and the importance of agent selection in ensuring
with RA or multiple sclerosis (MS), out-of-pocket (OOP) that the benefit of RA therapy is optimized.
expenses of more than $100 for TNF inhibitors (RA OOP Specialty pharmacies manage utilization, monitor
$0-$100, 4.7% abandonment; RA OOP >$100, 10.5%- patients, and ensure adherence to reduce the potential for
26.4% abandonment; P <.001), or $200 for MS medications adverse effects or suboptimal treatment. Specialty pharma-
(MS OOP $0-$200, 5.3%-10.6% abandonment; RA OOP cies are able to provide these services by obtaining prior
>$200, 25.8%-28.5%; P <.001 compared with $0-$100) authorization for patients, ensuring step-up therapy by docu-
were associated with increased risk of prescription aban- menting patients who have not responded to prior therapy
donment.34 A systematic review identified that the 2 most before receiving approval for more expensive agents, provid-
VOL. 18, No. 13 n The American Journal of Managed Care n S319
Reports
n Figure 2. Two-Year Costs and QALYs Depending on Type of Analysis26
Societal perspective, friction cost method
€30,000
€25,000 Healthcare perspective
€20,000
Total costs
€15,000
Societal perspective, human capital method
€10,000
Sequential monotherapy
Step-up combination
€5000
Initial combination with prednisone
Initial combination with infliximab
€0
1.25 1.30 1.35 1.40 1.45
QALYs, according to EQ5D-UK
EQ5D-UK indicates British EuroQol; QALY, quality-adjusted life-year.
Reprinted with permission from van den Hout WB, Goekoop-Ruiterman YP, Allaart CF, et al. Arthritis Rheum. 2009;61(3):291-299.
ing patient and provider training, determining quantity lim- tion between physicians and patients is lacking, and the role
its so that reauthorization is needed, determining dosing lim- of the primary care physician in optimizing care is uncer-
its, establishing length of therapy limits, selecting alternative tain. The focus group also identified that interdisciplinary
agents, and providing case management services.31 The next care could improve outcomes, but is often lacking, and that
section highlights some disease management programs in patient education is inadequate. In regard to the need for
RA that have successfully improved patient outcomes. adequate resources, the main need was for a team approach
across multiple disciplines.38 Thus, special attention to
Optimizing Clinical and Economic Outcomes With patients with RA and a multidisciplinary approach may be
Disease Therapy Management useful in improving outcomes.
A focus group study completed recently in Quebec, Can- A randomized trial evaluated an intensive treat-to-target
ada, sought to evaluate barriers to optimal care of patients outpatient approach for RA versus routine care. This trial
with RA.38 Barriers were divided into 4 categories: prior to was called the TICORA (TIght COntrol for Rheumatoid
primary care contact, speed of referral to a specialist, barriers Arthritis) study.39 The intensive therapy group met with a
to treatment, and inadequate resources. In the initial stage, rheumatologist monthly and had their disease activity cal-
there was a lack of awareness in the general population about culated at each visit. Disease activity was determined to be
RA, and patient demographics (eg, sex, age, socioeconomic high, moderate, or low. At each visit, swollen joints were
status) can affect access to care. Once a patient is seen, pri- injected with triamcinolone, unless previously injected in
mary care physicians may not differentiate the symptoms of the last 3 months, and DMARD therapy was escalated as
RA from other inflammatory processes, and delay referral needed according to an established protocol. In the rou-
to a specialist. Patient demographic factors may also affect tine care group, patients were seen every 3 months by their
referral to a specialist. There are also access issues, which rheumatologist with no formal composite measure of disease
are barriers to being seen by rheumatologists. Results dem- activity or plan of care. The improvement in disease activity
onstrated that during treatment, primary care physicians are was evident within 3 months in the intensive therapy group
not comfortable initiating definitive therapy, communica- (P <.0001). At the 18-month follow-up, EULAR remission
S320 n www.ajmc.com n december 2012
Implications for Managed Care and Specialty Pharmacy in Rheumatoid Arthritis
n Figure 3. Published Incremental Cost-Effectiveness Ratios28,29
Indication 50,000 100,000 Etanercept
Adalimumab
DMARDs in Infliximab
early RA Abatacept
Rituximab
DMARD
Biologics as
monotherapy TNF inhibitor,
in early RA unspecified
Biologics in
combination
therapy (+MTX)
in early RA
Biologics after
DMARD failure
Biologics after
TNF inhibitor
failure
10,000 100,000 1,000,000
Incremental cost-effectiveness ratio
in US$ per QALY gained (log scale)
DMARD indicates disease-modifying antirheumatic drug; ICER, incremental cost-effectiveness ratio; MTX, methotrexate; QALY, quality-adjusted life-
year; RA, rheumatoid arthritis; TNF, tumor necrosis factor.
Data points represent reported ICERs of the drugs investigated. Values to the left of the vertical lines at $50,000 and $100,000 are commonly consid-
ered to be cost-effective. Comparing ICERs between trials is inappropriate.
Reprinted with permission of BMJ Publishing Group Ltd from Schoels M, Wong J, Scott DL, et al. Ann Rheum Dis. 2010;69(6):995-1003; and with per-
mission of Oxford University Press from Fautrel B. Rheumatology (Oxford). 2012;51(suppl 4):iv21-iv26.
was achieved in 65% of patients in the intensive therapy care in the Netherlands. The nurse provided information
group and 16% of those in the routine care group (OR, 9.7; about RA, prescribed medical equipment in consultation
95% CI, 3.9-23.9; P <.0001), and ACR 20% improvement with a rheumatologist, and referred patients to other health-
(91% vs 64%; OR, 5.7; 95% CI, 1.9-16.7; P <.0001), ACR care professionals such as occupational therapists, physical
50% improvement (84% vs 40%; OR, 6.1; 95% CI, 2.5- therapists, and social workers when needed for a period of
14.9; P <.0001) and ACR 70% improvement (71% vs 18%; 12 weeks. The inpatient team and the day patient team
OR, 11; 95% CI, 4.5-27; P <.0001) were similarly improved, consisted of nurses, a rheumatologist, an occupational thera-
respectively. The intensive therapy group also benefited pist, a physical therapist, and a social worker. The team met
from less erosion score progression (median, 0.5; interquar- weekly to discuss treatment goals and modalities. Patients
tile range [IQR], 0-3.375 vs median 3; IQR, 0.5-8.5; P = also received written materials and an hour-long educational
.002), but no difference in joint space narrowing (median session on RA. Inpatients and day patients received 9 treat-
3.25; IQR, 1.125-7.5 vs median 4.5; IQR, 1.5-9; P = .331) ment days. Inpatients stayed overnight for 12 consecutive
was noted in comparison with the rountine care group. Total days with 3 nontreatment days. Day patients stayed 3 days
direct costs (hospital inpatient and outpatient, medication, per week for 6 hours and had 1.5 hours of rest for 3 weeks.
travel, healthcare professional visits, and diagnostic test) in After the intervention period, all patients were followed as
2000-2001 £, were £1427 for intensive care and £1590 for outpatients. In all 3 groups, functional status, quality of life,
routine care, indicating a cost savings with the intensive health utility, and disease activity improved significantly
therapy regimen.39 over time (P <.05). There was no significant difference
Studies have also evaluated a team approach to RA.40-42 among the groups over time. Patient satisfaction with the
One study40 examined patients randomized to a clinical nurse specialist care was significantly lower (P <.001) than
nurse specialist, inpatient team care, or day patient team the other groups.40 An economic analysis was presented in
VOL. 18, No. 13 n The American Journal of Managed Care n S321
Reports
a second publication.41 Based on similar outcomes in the (P <.001 vs DTM program cohorts). In the quality-of-life
effectiveness of treatment on quality of life and utility instru- assessment, the cohort included only 9.4% of patients in
ments, and that other healthcare and non-healthcare costs the DTM program groups, and the DTM program and non-
were similar over the 2-year follow-up, the only differences DTM program groups were not compared. Baseline and
observed were with the initial cost of care. The cost of ini- 6-month SF-12 scores improved (P = .048), but productiv-
tial treatment was €200 for the nurse, €5000 for the inpatient ity loss worsened from baseline (12.9% vs 28.3%, P = .045).
team care, and €4100 for the day patient care. Thus, the HAQ-DI scores improved from baseline by 0.08 points (P
societal costs were significantly lower with the nurse special- <.001), including improvements in dressing, grooming,
ist.41 This is consistent with how most patients are managed arising, grip, and reach. At month 6, 72.2% rated the pro-
today, as outpatients, but also highlights the importance of a gram as very helpful in managing their health.
team approach to care. Overall, this study provides promise for improving treat-
A national pharmacy benefit manager evaluated a dis- ment adherence and, potentially, patient outcomes in RA. It
ease therapy management (DTM) program for RA as an is important to note that this study was observational and that
enhanced offering for patients receiving specialty pharmacy the QOL measures were not specific to the studied groups. In
services.42 Core consultation topics for the DTM program addition, the data were not limited to the first use of inject-
were pathophysiology of RA, laboratory values pertain- able medication, and it is uncertain how “late” in the disease
ing to RA and its treatment, optimization of medication patients were at enrollment, and consequently how much ben-
therapy, adherence, symptom management, pain manage- efit they stood to gain, if any. Future studies should evaluate
ment, stress management, importance of a balanced diet, how QOL and productivity are impacted directly by a DTM
importance of exercise, importance of patient-provider program when therapies are initiated at the optimal time based
communication, appropriate use of assistive devices, home on available treatment recommendations, and what effect it
safety, and additional resources, including financial assis- has on disease outcome (ie, radiographic progression).2
tance. Patients with an RA diagnosis and a pharmacy claim
for RA who were continuously enrolled in the plan for 4 Conclusion
months before enrollment and 8 months after identifica- Rheumatoid arthritis is associated with significant treat-
tion were stratified into 3 groups, DTM program (n = 340), ment costs; however, in most situations, treatment is cost-
specialty pharmacy (n = 244), and community pharmacy effective when delivered in a structured and timely manner.
(n = 244), in observational fashion. Patients in the DTM Cost-effectiveness primarily stems from prevention of dis-
program were further categorized as intent-to-treat (ITT) ease progression and improved work productivity associated
(all 340 patients in the DTM program) and completers with disease control. Disease control limits the potential
(n = 244). The primary end point was proportion of days costs associated with surgery and hospitalization, and also
covered (PDC), a marker of persistence and adherence to has the potential to make patients more productive mem-
treatment, over the 8-month post-identification period. bers of society. Barriers to the success of treatment include
Patient-reported outcomes (short form [SF]-12, Work Pro- lack of education for patients and practitioners about RA,
ductivity Activity Impairment [WPAI], and Health Assess- access to specialists, communication, uncertainty regard-
ment Questionnaire-Disability Index [HAQ-DI]) were ing which treatments to choose, cost, and lack of treat-
also collected in 371 patients who completed the 0- and ment adherence. Specialty pharmacy and DTM programs
6-month consultations regardless of enrollment group or can assist patients by providing structure, education, and
requirements. Among specialty pharmacy patients, 14% mechanisms to improve patient adherence in order to opti-
enrolled in the DTM program. Mean PDC was 0.81 for mize therapy.
specialty pharmacy, 0.83 for the DTM program ITT group,
Author affiliation: Atrius Health, Harvard Vanguard Medical Associates,
0.89 for the DTM program completers group (P <.001 vs
Watertown, MA.
specialty pharmacy), and 0.6 for community pharmacy (P Funding source: This activity is supported by an educational grant from
<.001 for both DTM program cohorts). In addition, 10.7% Bristol-Myers Squibb.
of patients in the DTM program completer group, 20.3% Author disclosure: Dr Cardarelli has no relevant financial relationships
with commercial interests to disclose.
of those in the DTM program ITT group, 22.1% of those
Authorship information: Acquisition of data; analysis and interpretation
in the specialty pharmacy group (P <.001 vs DTM pro- of data; drafting of the manuscript; critical revision of the manuscript for
gram completers), and 40.6% of those in the community important intellectual content; statistical analysis; and supervision.
pharmacy group discontinued injectable biologic agents Address correspondence to: E-mail: william_cardarelli@vmed.org.
S322 n www.ajmc.com n december 2012
Implications for Managed Care and Specialty Pharmacy in Rheumatoid Arthritis
toid arthritis treated with adalimumab. J Occup Environ Med.
References 2010;52(6):618-621.
19. Kavanaugh AF, Emery P, van Vollenhoven R, et al.
1. Smolen JS, Landewé R, Breedveld FC, et al. EULAR recom- Comparisons of work productivity and patient-reported out-
mendations for the management of rheumatoid arthritis with comes through 78 weeks among OPTIMA study arms 2, 4 and 5.
synthetic and biological disease-modifying antirheumatic drugs. Ann Rheum Dis. 2012;71(suppl 3):362.
Ann Rheum Dis. 2010;69(6):964-975.
20. Birnbaum HG, Barton M, Greenberg PE, et al. Direct and
2. Singh JA, Furst DE, Bharat A, et al. 2012 update of the 2008 indirect costs of rheumatoid arthritis to an employer. J Occup
American College of Rheumatology recommendations for the Environ Med. 2000;42(6):588-596.
use of disease-modifying antirheumatic drugs and biologic 21. González-Alvaro I, Descalzo MA, Carmona L. Trends toward
agents in the treatment of rheumatoid arthritis. Arthritis Care an improved disease state in rheumatoid arthritis over time:
Res (Hoboken). 2012;64(5):625-639. influence of new therapies and changes in management
3. Gibofsky A. Comparative effectiveness of current treatments approach: analysis of the EMECAR cohort. Arthritis Res Ther.
for rheumatoid arthritis. Am J Manag Care. 2012;18:S303-S314. 2008;10(6):R138
4. Fautrel B, Clarke AE, Guillemin F, et al. Costs of rheuma- 22. Aga AB, Lie E, Fagerli KM, Uhlig T, Kvien TK, Haavardsholm
toid arthritis: new estimates from the human capital method EA. Trends in baseline disease activity, response and remission
and comparison to the willingness-to-pay method. Med Decis rates in rheumatoid arthritis (RA) during the last decade: results
Making. 2007;27(7):138-150. from the NOR-DMARD Register. Ann Rheum Dis. 2012;71(suppl
5. Bansback N, Marra CA, Finckh A, Anis A. The economics 3):329.
of treatment in early rheumatoid arthritis. Best Prac Res Clin 23. Andersson ML, Forslind K, Söderlin M, Hafström I.
Rheumatol. 2009;23(1):83-92. Comparison between patients included in the BARFOT Study
6. Lanes SF, Lanza LL, Radensky PW, et al. Resource utiliza- 1992-1999 and 2000-2006 – a five year follow-up. Ann Rheum
tion and cost of care for rheumatoid arthritis and osteoarthritis Dis. 2012;71(suppl 3):104.
in a managed care setting: the importance of drug and surgery 24. Finckh A, Liang MH, van Herckenrode CM, de Pablo P.
costs. Arthritis Rheum. 1997;40(8):1475-1481. Long-term impact of early treatment on radiographic progres-
7. Joyce AT, Smith P, Khandker R, Melin JM, Singh A. Hidden sion in rheumatoid arthritis: a meta-analysis. Arthritis Rheum.
cost of rheumatoid arthritis (RA): estimating cost of cormorbid 2006;55(6):864-872.
cardiovascular disease and depression among patients with RA. 25. Tosh JC, Wailoo AJ, Scott DL, Deighton CM. Cost-
J Rheumatol. 2009;36(4):743-752. effectiveness of combination nonbiologic disease-modifying
antirheumatic drug strategies in patients with early rheumatoid
8. McInnes IB, Schett G. The pathogensis of rheumatoid arthritis.
arthritis. J Rheumatol. 2011;38(8):1593-1600.
N Engl J Med. 2011;365(23):2205-2219.
26. van den Hout WB, Goekoop-Ruiterman YP, Allaart CF, et
9. Listing J, Pattloch D, Kekow J, et al. Successful control of
al. Cost-utility analysis of treatment strategies in patients with
disease activity and treatment with biologics increase the life
recent-onset rheumatoid arthritis. Arthritis Rheum. 2009;61(3):
expectancy in rheumatoid arthritis patients. Ann Rheum Dis.
291-299.
2012;71(suppl 3):69.
27. Verhoeven AC, Bibo JC, Boers M, Engel GL, van der Linden
10. van Sijl AM, Visman IM, Peters MF, et al. TNF-blocking thera- S; COBRA Trial Group. Cost-effectiveness and cost-utility of
py reduces cardiovascular disease and risk factors in rheumatoid combination therapy in early rheumatoid arthritis: random-
arthritis. Ann Rheum Dis. 2012;71(suppl 3):358. ized comparison of combined step-down prednisolone,
11. Burmester G, Emery P, Signorovitch J, et al. The effect of methotrexate and sulphasalazine with sulphasalazine alone.
adalimumab on risk of major adverse cardiovascular events in Combinatietherapie Bij Reumatoïde Artritis. Br J Rheumatol.
rheumatoid arthritis: a meta-analysis of randomized trials. Ann 1998;37(10):1102-1109.
Rheum Dis. 2012;71(suppl 3):359. 28. Schoels M, Wong J, Scott DL, et al. Economic aspects of
12. Ljung L, Rantapää-Dahlqvist S, Askling J, Jacobsson L. The treatment options in rheumatoid arthritis: a systematic literature
risk of acute coronary syndromes in RA in relation to TNF inhibi- review informing the EULAR recommendations for the manage-
tors and risk in the general population: a national cohort study. ment of rheumatoid arthritis. Ann Rheum Dis. 2010;69(6):995-
Ann Rheum Dis. 2012;71(suppl 3):518. 1003.
13. Westhovens R, Weinblatt ME, Han C, et al. Fatigue is an 29. Fautrel B. Economic benefits of optimizing anchor therapy
independent variable predicting physical function and DAS-28 for rheumatoid arthritis. Rheumatology (Oxford). 2012;51(suppl
remission for patients with rheumatoid arthritis treated with 4):iv21-iv26.
intravenously administered golimumab: results from phase 3, 30. van der Velde G, Pham B, Machado M, et al. Cost-
placebo controlled clinical trial. Ann Rheum Dis. 2012;71(suppl effectiveness of biologic response modifiers compared to dis-
3):665. ease-modifying antirheumatic drugs for rheumatoid arthritis: a
14. Bilgici A, Uzuner B, Kuru A, Bedir A. The efficacy of anti- systematic review. Arthritis Care Res (Hoboken). 2011;63(1):65-
tumor necrosis factor therapy and the factors which contribute 78.
to fatigue in rheumatoid arthritis. Ann Rheum Dis. 2012;71(suppl 31. Shane R. Management of chronic disease in the 21st centu-
3):663. ry: the emerging role of specialty pharmacies. Am J Health Syst
15. Chauffier K, Salliot C, Berenbaum F, Sellam J. Effect of bio- Pharm. 2007;64(22)2382-2385.
therapies on fatigue in rheumatoid arthritis: a systematic review 32. Costs for traditional meds static while specialty drug costs
of the literature and meta-analysis. Rheumatology (Oxford). soar. Manag Care. 2012;21(6):47.
2012;51(1):60-68. 33. Specialty drugs to spark the next round of increases. Manag
16. Willeke P, Winter C, Schotte H, et al. Etanercept increases Care. 2012;21(7):53.
step activity in patients with active rheumatoid arthritis and 34. Gleason PP, Starner CI, Gunderson BW, Schafer JA, Sarran
short disease duration. Ann Rheum Dis. 2012;71(suppl 3):665. HS. Association of prescription abandonment with cost share
17. Anis A, Zhang W, Emery P, et al. The effect of etanercept for high-cost specialty pharmacy medications. J Manag Care
on work productivity in patients with early active rheumatoid Pharm. 2009;15(8):648-658.
arthritis: results for the COMET study. Rheumatology (Oxford). 35. Pasma A, van’t Spijker A, van Busschbach J, Hazes M, Luime
2009;48(10):1283-1289. J. Factors associated with adherence to pharmaceutical treat-
18. Herenius MM, Hoving JL, Sluiter JK, et al. Improvement in ment for rheumatoid arthritis: a systematic review. Ann Rheum
work ability, quality of life, and fatigue in patients with rheuma- Dis. 2012;71(suppl 3):658.
VOL. 18, No. 13 n The American Journal of Managed Care n S323
Reports
36. Pasma A, Luime J, Hazes M, van Busschbach J, van’t Spijker 40. Tijhuis GJ, Zwinderman AH, Hazes JM, Van Den Hout WB,
A. Reasons to adhere to DMARD therapy in patients recently Breedveld FC, Vliet Vlieland TP. A randomized comparison of
diagnosed with rheumatoid arthritis, arthritis psoriatica or poly- care provided by a clinical nurse specialist, an inpatient team,
arthritis: a qualitative report. Ann Rheum Dis. 2012;71(suppl 3): and a day patient team in rheumatoid arthritis. Arthritis Rheum.
658. 2002;47(5):525-531.
37. Li P, Blum MA, Von Feldt J, Hennessy S, Doshi JA. 41. van den Hout WB, Tijhuis GJ, Hazes JMW, Breedveld FC,
Adherence, discontinuation, and switching of biologic therapies Vliet Vlieland TP. Cost effectiveness and cost utility analysis of
in Medicaid enrollees with rheumatoid arthritis. Value Health. multidisciplinary care in patients with rheumatoid arthritis: a
2010;13(6):805-812. randomised comparison of clinical nurse specialist care, inpa-
38. Bernatsky S, Feldman D, De Civita M, et al. Optimal care tient team care, and day patient team care. Ann Rheum Dis.
for rheumatoid arthritis: a focus group study. Clin Rheumatol. 2003;62(4):308-315.
2010;29(6):645-657. 42. Stockl KM, Shin JS, Lew HC, et al. Outcomes of a rheuma-
39. Grigor C, Capell H, Stirling A, et al. Effect of treatment toid arthritis disease therapy management program focusing on
strategy on tight control for rheumatoid arthritis (the TICORA medication adherence. J Manag Care Pharm. 2010;16(8):593-604.
study): a single-blind randomised controlled trial. Lancet.
2004;364(9430):263-269.
S324 n www.ajmc.com n december 2012
You might also like
- Clinical Updates in Rheumatoid Arthritis: New Strategies to Target Remission and Individualize Comprehensive CareFrom EverandClinical Updates in Rheumatoid Arthritis: New Strategies to Target Remission and Individualize Comprehensive CareNo ratings yet
- The Journal of Rheumatology Volume 38, No. 8Document4 pagesThe Journal of Rheumatology Volume 38, No. 8Jeff LapianNo ratings yet
- Treat to Target Approach for Rheumatoid Arthritis RemissionDocument18 pagesTreat to Target Approach for Rheumatoid Arthritis RemissionYoaAguilarCastilloNo ratings yet
- Reference 333Document123 pagesReference 333sabrinaNo ratings yet
- 1 s2.0 S1556086415317809 MainDocument7 pages1 s2.0 S1556086415317809 MainBegoña MartinezNo ratings yet
- Role of pharmacists in reducing healthcare costsDocument8 pagesRole of pharmacists in reducing healthcare costsAnsar MushtaqNo ratings yet
- AJMC - 10 - 2016 - Najafzadeh (Final)Document14 pagesAJMC - 10 - 2016 - Najafzadeh (Final)Praphatsorn ChaphakdeeNo ratings yet
- Aujesky 2005Document2 pagesAujesky 2005Devanti EkaNo ratings yet
- Contrato Riesgos Compartidos PDFDocument4 pagesContrato Riesgos Compartidos PDFSergio TerrasaNo ratings yet
- Eco 3Document12 pagesEco 3Walaa KhasawnehNo ratings yet
- 10 1177@0897190020903573Document13 pages10 1177@0897190020903573JorgeAlejandroSanchezDelgadoNo ratings yet
- Evidence-Based Medical Treatment of Peripheral Arterial Disease: A Rapid ReviewDocument14 pagesEvidence-Based Medical Treatment of Peripheral Arterial Disease: A Rapid ReviewLeo OoNo ratings yet
- Smith Et Al-2017-Arthritis Care & ResearchDocument9 pagesSmith Et Al-2017-Arthritis Care & ResearchFerryGoNo ratings yet
- Cea AmlodipineDocument6 pagesCea AmlodipineM UlfahNo ratings yet
- The Active Comparator, New User Study Design in Pharmacoepidemiology: Historical Foundations and Contemporary ApplicationDocument8 pagesThe Active Comparator, New User Study Design in Pharmacoepidemiology: Historical Foundations and Contemporary ApplicationDici RachmandaNo ratings yet
- Hepb y RTX PDFDocument3 pagesHepb y RTX PDFYeli VeMeNo ratings yet
- Issue 09 Treat To Target enDocument3 pagesIssue 09 Treat To Target enArja' WaasNo ratings yet
- Non-Inflammatory Pain in Inflammatory ArthritisDocument6 pagesNon-Inflammatory Pain in Inflammatory Arthritisyoelpurnama1991No ratings yet
- Economic Issues and Medication Non-Adherence in Inflammatory ArthritisDocument10 pagesEconomic Issues and Medication Non-Adherence in Inflammatory ArthritisVirgo WNo ratings yet
- Rheumatoid Arthritis Assessment and TreatmentDocument9 pagesRheumatoid Arthritis Assessment and TreatmentPerry MárquezNo ratings yet
- Cost-Effectiveness and Clinical Effectiveness of The Risk Factor Management Clinic in Atrial FibrillationDocument12 pagesCost-Effectiveness and Clinical Effectiveness of The Risk Factor Management Clinic in Atrial FibrillationsarahNo ratings yet
- Migrain in The WorldDocument5 pagesMigrain in The WorldveNo ratings yet
- 2016 JBMR - Local, National, and Service Component Cost VariationsDocument8 pages2016 JBMR - Local, National, and Service Component Cost VariationsAlessandra Aparecida PalacioNo ratings yet
- LeprosyDocument20 pagesLeprosyHafiz Sulistio UtomoNo ratings yet
- Medication Adherence and Its Related Factors Among Patients With Coronary Artery DiseaseDocument3 pagesMedication Adherence and Its Related Factors Among Patients With Coronary Artery DiseaseInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- ArticleDocument11 pagesArticlejesica_loNo ratings yet
- Cost Effectiveness and Resource AllocationDocument7 pagesCost Effectiveness and Resource AllocationSarah AmeliaNo ratings yet
- Caso Clinico 1Document10 pagesCaso Clinico 1Rosa ArrascueNo ratings yet
- 19 03 PDFDocument2 pages19 03 PDFT h o r y n R a m o sNo ratings yet
- NR Endo 201421Document6 pagesNR Endo 201421Lucia VillacrizNo ratings yet
- TTT Intention in OA MiglioreDocument4 pagesTTT Intention in OA MiglioreDuilio GuzzardoNo ratings yet
- General Principles of Management of Rheumatoid ArthritisDocument19 pagesGeneral Principles of Management of Rheumatoid ArthritisSakinah Ginna RNo ratings yet
- Medication Adherence in Patients After Percutaneous Coronary Intervention Due To Acute Myocardial Infarction: From Research To Clinical ImplicationsDocument8 pagesMedication Adherence in Patients After Percutaneous Coronary Intervention Due To Acute Myocardial Infarction: From Research To Clinical ImplicationsCeGa EliNo ratings yet
- Cost and Effectiveness of Biologics For Rheumatoid Arthritis in A Commercially Insured PopulationDocument11 pagesCost and Effectiveness of Biologics For Rheumatoid Arthritis in A Commercially Insured PopulationAjeng DwiNo ratings yet
- PSY21 COST EFFECTIVENESS ANALYSIS OF EMICIZUMAB FOR THE TREATME - 2019 - Value IDocument1 pagePSY21 COST EFFECTIVENESS ANALYSIS OF EMICIZUMAB FOR THE TREATME - 2019 - Value IMichael John AguilarNo ratings yet
- Managing Res InfectionsDocument24 pagesManaging Res InfectionsDivya RamuNo ratings yet
- Cea Hipertensi 8Document7 pagesCea Hipertensi 8ani rahayuNo ratings yet
- The Health and Work Questionnaire HWQ An InstrumenDocument124 pagesThe Health and Work Questionnaire HWQ An InstrumenLorraine VillanuevaNo ratings yet
- Table II: JA A DDocument3 pagesTable II: JA A DEduardoAndrésRamírezNo ratings yet
- American Heart Journal Plus: Cardiology Research and PracticeDocument6 pagesAmerican Heart Journal Plus: Cardiology Research and Practice18ME045No ratings yet
- PPI-Induced Nephrotoxicity Risk Factors and ManagementDocument12 pagesPPI-Induced Nephrotoxicity Risk Factors and ManagementSergio Herrero BermejoNo ratings yet
- Exercício em Pacientes Com CâncerDocument20 pagesExercício em Pacientes Com CâncerDrDermeval Reis JuniorNo ratings yet
- The Effect of Text Message Reminders On Medication.8Document7 pagesThe Effect of Text Message Reminders On Medication.8amar prasadNo ratings yet
- Rheumatoid Factor Testing: Policy Number: CMP - 049 Effective Date: January 1, 2018Document6 pagesRheumatoid Factor Testing: Policy Number: CMP - 049 Effective Date: January 1, 2018Ocef GrahastamaNo ratings yet
- Uremia (End-Stage Renal Disease)Document4 pagesUremia (End-Stage Renal Disease)nathalieNo ratings yet
- Gouty Arthritis: Nama: Adibah Nur M. No. Korona: 03 Nama Medis: Malocclusion Nama Korona: Dentistry No. Absen: 22Document2 pagesGouty Arthritis: Nama: Adibah Nur M. No. Korona: 03 Nama Medis: Malocclusion Nama Korona: Dentistry No. Absen: 22almiraNo ratings yet
- Patient Reported Endpoints ForDocument11 pagesPatient Reported Endpoints FortisepNo ratings yet
- 2022 ITECritiqueDocument80 pages2022 ITECritiqueJon LetkoNo ratings yet
- Estey 2020Document73 pagesEstey 2020drToikNo ratings yet
- Makalah KesehatanDocument9 pagesMakalah KesehatanNini RahmiNo ratings yet
- Cost-Effectiveness of Alcohol Use Treatments in Patients With Alcohol-Related CirrhosisDocument9 pagesCost-Effectiveness of Alcohol Use Treatments in Patients With Alcohol-Related CirrhosisTIARA AMELIANo ratings yet
- 1 s2.0 S1098301510688778 MainDocument2 pages1 s2.0 S1098301510688778 MainPeter SalimNo ratings yet
- Perioperative Management GuidelineDocument10 pagesPerioperative Management Guidelineblue diamondNo ratings yet
- Economic Impact of Illness: COI AnalysisDocument49 pagesEconomic Impact of Illness: COI AnalysisNumeratorNo ratings yet
- Chan (2018)Document16 pagesChan (2018)Aprilla Ayu WulandariNo ratings yet
- 2022.7 Incident and recurrent herpes zoster for first line bDMARD and tsDMARD users in seropositive rheumatoid arthritis patientsDocument10 pages2022.7 Incident and recurrent herpes zoster for first line bDMARD and tsDMARD users in seropositive rheumatoid arthritis patientsindream81No ratings yet
- Assessing Fatigue in The ESRD Patient: A Step Forward: Related Article, P. 327Document3 pagesAssessing Fatigue in The ESRD Patient: A Step Forward: Related Article, P. 327Rina FebriantiNo ratings yet
- Clinical Practice Guidelines and Quality of Care For Older Patients With Multiple Comorbid DiseasesDocument9 pagesClinical Practice Guidelines and Quality of Care For Older Patients With Multiple Comorbid DiseasesBiblioteca Centro Médico De Mar del PlataNo ratings yet
- Healthcare SpendingDocument20 pagesHealthcare Spendingmikeb92556No ratings yet
- Eectiveness Tolerability and Safety of Tofacitinib inDocument14 pagesEectiveness Tolerability and Safety of Tofacitinib indanny gomezNo ratings yet
- Practical Research 2 PDFDocument60 pagesPractical Research 2 PDFSargeant Oxford100% (1)
- Epi PediaDocument1 pageEpi Pediag3nj1No ratings yet
- ReviewerDocument24 pagesReviewerMaria Lourdes ReyesNo ratings yet
- Thesis Risk AssessmentDocument9 pagesThesis Risk Assessmentoxylhkxff100% (2)
- Manual Therapy Interventions For Carpal Tunnel Syndrome A ReviewDocument10 pagesManual Therapy Interventions For Carpal Tunnel Syndrome A ReviewlathifatulNo ratings yet
- 1090 Syllabus 1 1090 Syllabus 1Document6 pages1090 Syllabus 1 1090 Syllabus 1jhgNo ratings yet
- Taking Tylenol During Pregnancy May Raise Autism, ADHD RiskDocument3 pagesTaking Tylenol During Pregnancy May Raise Autism, ADHD RiskJun KedNo ratings yet
- ICPR 5 1 WebDocument96 pagesICPR 5 1 WebAndreea-Luciana UrzicăNo ratings yet
- Ovary Female Reproductive SystemDocument1 pageOvary Female Reproductive SystemtheodorastanerNo ratings yet
- Codex Standard For Wheat and Durum WheatDocument3 pagesCodex Standard For Wheat and Durum WheatCiprian CorneaNo ratings yet
- (Schuler, 2016) Shattering World AssumptionDocument8 pages(Schuler, 2016) Shattering World AssumptionJudith Velasco RodríguezNo ratings yet
- Spanish Dissertation TopicsDocument8 pagesSpanish Dissertation TopicsWritingPaperServicesToledo100% (1)
- CPCWHS3001 - Learner Guide V1.0Document20 pagesCPCWHS3001 - Learner Guide V1.0sharma SoniaNo ratings yet
- Effects of Job Stress On Employees PerformanceDocument9 pagesEffects of Job Stress On Employees PerformanceKungurirai MagushaNo ratings yet
- How Do You Assess Biopure's Potential in The Human Market? The Animal Market? Human MarketDocument8 pagesHow Do You Assess Biopure's Potential in The Human Market? The Animal Market? Human MarketYilei RenNo ratings yet
- ROLE OF SPIRITUALITY IN ATTAINING WELLBEING - Final Version After Changes PDFDocument24 pagesROLE OF SPIRITUALITY IN ATTAINING WELLBEING - Final Version After Changes PDFKiran Kumar SalagameNo ratings yet
- Ebola - Reading ExerciseDocument4 pagesEbola - Reading ExercisePriscila PereiraNo ratings yet
- Thesis Statement On Young MarriageDocument8 pagesThesis Statement On Young Marriagebser9zca100% (2)
- Module 12.1Document17 pagesModule 12.1robelyn veranoNo ratings yet
- Blessing in Disguise EssayDocument8 pagesBlessing in Disguise Essayafabfoilz100% (2)
- 2015 Traumatic Pulmonary Pseudocysts After Blunt Chest TraumaDocument6 pages2015 Traumatic Pulmonary Pseudocysts After Blunt Chest TraumaLexotanyl LexiNo ratings yet
- Headache Clinical PathwayDocument25 pagesHeadache Clinical PathwayKoushik Mazumder ShuvoNo ratings yet
- SearchDocument216 pagesSearchTina LocklearNo ratings yet
- The Hold Me Tight Workbook - Dr. Sue JohnsonDocument187 pagesThe Hold Me Tight Workbook - Dr. Sue JohnsonMoh100% (8)
- PTE AcademicDocument104 pagesPTE AcademicAna FajardoNo ratings yet
- NegOr Q4 EAPP Module8 v2Document20 pagesNegOr Q4 EAPP Module8 v2XYZA LopezNo ratings yet
- CHCCCS025 Support Relationships With Carers and Families EKDocument67 pagesCHCCCS025 Support Relationships With Carers and Families EKIkhsan Misbahuddin75% (8)
- Diet guide for managing hyperuricemia and high cholesterolDocument6 pagesDiet guide for managing hyperuricemia and high cholesterolAmelito LajaraNo ratings yet
- Menstruation, Religion and Society: Aru BhartiyaDocument5 pagesMenstruation, Religion and Society: Aru BhartiyaDilpreet KharbandaNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (14)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (327)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Daniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisFrom EverandDaniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisRating: 3.5 out of 5 stars3.5/5 (130)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)