100% found this document useful (6 votes)
37K views10 pagesHistory Taking Format
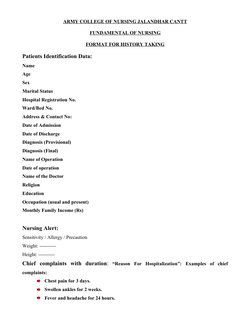
This document provides a format for taking a patient's medical history. It includes sections for collecting the patient's identification data, chief complaints, history of present illness, past medical history, surgical history, family history, environmental history, physical examination findings, diagnostic evaluations, medications, nursing care plan, and nurses' notes. The goal is to gather comprehensive information about the patient's health to inform their diagnosis and treatment.
Uploaded by
Muskaan DeepCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
100% found this document useful (6 votes)
37K views10 pagesHistory Taking Format
This document provides a format for taking a patient's medical history. It includes sections for collecting the patient's identification data, chief complaints, history of present illness, past medical history, surgical history, family history, environmental history, physical examination findings, diagnostic evaluations, medications, nursing care plan, and nurses' notes. The goal is to gather comprehensive information about the patient's health to inform their diagnosis and treatment.
Uploaded by
Muskaan DeepCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
- Patient Identification and Nursing Alert: Covers identification data for patients and essential nursing alerts related to patient history taking.
- Medical Histories Overview: Details the process of gathering relevant information on the patient's present and past medical history, including illness history.
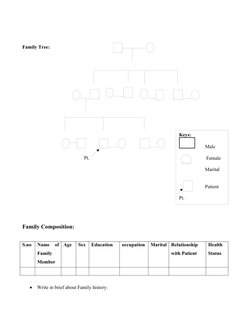
- Family History and Composition: Describes how to record and visualize family health history and its composition for medical purposes.
- Environmental History and Personal Habits: Focuses on acquiring information about the patient's living environment and their personal habits impacting health.
- General Examination: Provides guidelines for assessing the patient's general appearance, vital signs, and other health indicators.
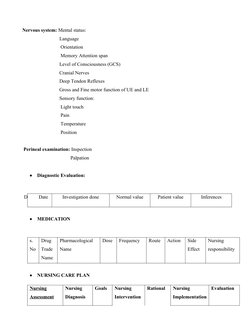
- Detailed Physical Examination: Outlines the specific examination steps for each part of the body during a physical exam.
- Diagnostic Evaluation and Nursing Care: Explains diagnostic evaluation processes and the planning of nursing care based on patient assessment.
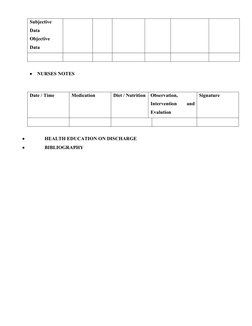
- Nursing Notes and Additional Information: Includes areas for nursing notes, health education guidance, and bibliography references.