Professional Documents
Culture Documents
Bani 2006
Uploaded by
Nael NajeebCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bani 2006
Uploaded by
Nael NajeebCopyright:
Available Formats
A Method to Assess Posterior Urethral Valve Ablation
O. Bani Hani, K. Prelog and G. H. H. Smith*
From the Childrens Hospital at Westmead (Royal Alexandra Hospital for Children), Westmead, New South Wales, Australia
Purpose: There are few published reports addressing the assessment of posterior urethral valve ablation. This study was
performed to provide a ratio to measure successful treatment of posterior urethral valves.
Materials and Methods: A total of 35 patients with posterior urethral valves were treated by a single surgeon between 1995
and 2004. Of these patients 23 were younger than 1 year at diagnosis and were selected for this study. A urethral ratio was
calculated by dividing the posterior urethral diameter by the anterior urethral diameter. A total of 31 males undergoing
cystography for urinary tract infections were evaluated as normative controls. The urethral ratio was also measured and
calculated for these patients.
Results: Median patient age was 1.5 months. In 13 patients preoperative cystograms were available and in 20 patients
postoperative cystograms were available for review. Measurements were made of the posterior urethral and anterior urethral
diameters. Median preoperative ratio in 13 patients was 8.6. This ratio decreased postoperatively to 3.1 in 15 patients who
only required 1 ablation and 8.0 in 5 patients who required a second ablation. After a second ablation the ratio decreased to
3.1. The 5 cases requiring a second ablation were initially managed by cystoscopy and a flexible electrode. None of the patients
treated initially with a resectoscope required a second ablation. Urethral ratio was 2.6 in 31 normal males undergoing
cystogram for investigation of a urinary tract infection.
Conclusions: Calculating urethral ratio in patients with posterior urethral valves allows objective measurement of the
technical success of valve ablation.
Key Words: urethra, urethral obstruction, vesico-ureteral reflux, pediatrics
he management of PUVs remains controversial. Most MATERIALS AND METHODS
T authors now agree that valve ablation is the best
primary treatment.1–3 However, there are no clear
guidelines to assess the technical success of this therapy.
A total of 35 cases of PUVs were diagnosed and managed by
a single surgeon between 1995 and 2004. Patient identifica-
The indications for vesicostomy and high diversion are dis- tion and demographic information were collected prospec-
puted among authors.3 Most would agree that monitoring tively. Median patient age at diagnosis was 3.5 months
renal function, hydronephrosis, vesicoureteral reflux, uri- (range 1 to 130). Of the patients 23 were younger than 1 year
nary stream and bladder emptying is essential.4,5 However, at diagnosis, and this group was selected for the study.
these parameters often change slowly, during the course of Patients older than 1 year were excluded because this group
several months. The bladder is able to compensate for con- generally had a good prognosis and we were always able to
tinuing partial outlet obstruction. treat them with 1 valve ablation. In almost all cases cysto-
A pediatric urology specialist may treat 3 to 4 patients grams were done elsewhere and were not available for re-
with PUVs annually. However, a pediatric surgeon or urol- view.
ogist with a combined adult and pediatric practice may treat A total of 16 patients presented following prenatal diag-
only 1 patient every few years. To our knowledge there are nosis and 7 presented after a urinary tract infection. The
no data available to compare outcomes in patients treated by diagnosis was confirmed by VCUG. The standard manage-
these different groups of surgeons. ment plan was to perform valve ablation and then to repeat
How can the adequacy of valve ablation be assessed? the VCUG at 6 to 8 weeks postoperatively. Depending on the
Some authors recommend followup VCUG,6 while others clinical progress and VCUG appearance, a repeat ablation
recommend followup cystoscopy.7 In both instances postop- was performed.
erative assessment is based on qualitative factors and clin- We retrospectively collected data on the cystoscopic
ical judgment. Does the posterior urethra look less dilated? method of valve ablation from the operative reports. Sur-
Is the valve leaflet still visible? No quantitative guidelines geon preference was to use an 11Fr resectoscope with a
have been given. In this study we attempted to develop a Collins knife and a cutting diathermy current. When the
simple, objective, quantitative measurement of the success urethra was too small for this instrument a 9Fr cystoscope
of valve ablation. with a 2.4Fr flexible electrode was used.
In most cases VCUG images were stored in the hospital
picture archiving and communications system. The preoper-
ative and postoperative x-rays of 3 patients were performed
Submitted for publication September 29, 2005.
* Correspondence: Department of Urology, Childrens Hospital at elsewhere and could not be traced. In 13 patients preopera-
Westmead, Westmead, New South Wales, 2145, Australia. tive and postoperative images were available for review, and
0022-5347/06/1761-0303/0 303 Vol. 176, 303-305, July 2006
THE JOURNAL OF UROLOGY® Printed in U.S.A.
Copyright © 2006 by AMERICAN UROLOGICAL ASSOCIATION DOI:10.1016/S0022-5347(06)00562-3
304 METHOD TO ASSESS POSTERIOR URETHRAL VALVE ABLATION
FIG. 1. Preoperative urethral measurement in patient with PUV FIG. 3. Urethral measurement in control patient
in 7 patients only postoperative images were available for
ablation was 8.6 (range 4 to 14.7). A catheter was left in-
review, giving a total of 20 patients with postoperative im-
dwelling in 4 of these patients.
ages available for the study.
Postoperative films were available in 20 patients and the
We defined UR as the diameter of the posterior urethra
median UR was 3.4 (range 1.9 to 15.5). The postoperative
divided by the diameter of the anterior urethra measured
group was divided into patients requiring only 1 valve abla-
during the voiding phase on an oblique film (figs. 1 and 2).
tion and those requiring a second ablation. In the 15 pa-
The diameter of the posterior urethra was measured trans-
tients requiring 1 ablation the ratio decreased to 3.1 (range
versely at a point halfway between the bladder neck and the
1.9 to 4) postoperatively. In the 5 patients requiring a second
distal end of the membranous urethra. The diameter of the
ablation the ratio decreased to 8.0 (range 5 to 15.5) after the
anterior urethra was measured as a transverse diameter at
first ablation and to 3.1 (2.9 to 6.4) after the second ablation
the point of the maximum distention in the bulbar urethra.
(fig. 4). A catheter was left indwelling in 2 of the 5 patients
We aimed to measure these diameters on a voiding film
requiring a second ablation.
without a catheter. Both measurements were taken on the
We judged an arbitrary UR value of 3.5 to be represen-
same film.
tative of adequate valve ablation and relief of obstruction. To
If several films were available, measurements were made
demonstrate reproducibility of the ratio, 15 measurements
on the image where the anterior urethra was most dis-
were taken by the first and third authors (OBH, GHHS) and
tended. The measurements were made separately by 2 au-
compared. There was agreement on satisfactory or unsatis-
thors (OBH, KP) and then a consensus was reached. To show
factory valve ablation in 11 patients and disagreement in 4
reproducibility, another set of 15 measurements was made
(see table). All of the films where disagreement occurred
by the first and third authors (OBH, GHHS) and compared.
revealed a catheter in the urethra on voiding, which compli-
As a control group, the same urethral ratio was calculated for
cated the measurement.
31 age matched males who had a normal VCUG as part of the
A pediatric resectoscope was used in 8 of 21 cases for the
evaluation for suspected urinary tract pathology (fig. 3).
initial ablation, and the remaining 13 were managed by
cystoscope and flexible electrode. All of the patients requir-
RESULTS ing a second ablation were treated initially with the cysto-
Median age for the controls was 4 months (range 1 to 11), scope and flexible electrode.
and median UR was 2.6 (1.3 to 5.5). Median age for the study
group was 1.5 months (range 1 to 12). Preoperative films
were available in 13 patients and the median UR before
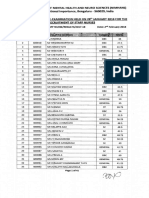
FIG. 4. Change in urethral ratio with ablation and repeat ablation.
Paired t test comparing ratio of preoperative group to that of post-
operative group revealed mean UR in 12 patients with paired films
decreased from 9.7 to 5.1 (p ⬍0.01) after first procedure. After
FIG. 2. Postoperative urethral measurement in patient with treated second procedure mean ratio in 5 patients with paired films de-
PUV. creased from 8.7 to 3.8 (p ⬍0.02).
METHOD TO ASSESS POSTERIOR URETHRAL VALVE ABLATION 305
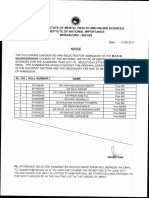
No. GHHS
lieved that this procedure was too invasive in infants who
were often unwell and had impaired renal function.
No. OBH, KP Satisfactory Unsatisfactory
Reviewing our data, we believed that a ratio of 3.5 rep-
Satisfactory 3 4 resented an acceptable result postoperatively. This estimate
Unsatisfactory 0 8
meant that 4 of 31 controls had a UR greater than 3.5 and 1
patient with PUV had a UR of more than 3.5 after we had
completed what we considered a successful ablation. Fur-
This group of 20 patients was followed for a median of ther studies will be needed to adjust the UR considered
27.5 months (range 6 to 97). One patient required a renal acceptable after treatment, and to confirm these findings.
transplant and 1 is receiving dialysis.
CONCLUSIONS
DISCUSSION Urethral ratio is a simple measurement that allows quanti-
tative assessment of valve ablation. It allows preoperative
Shopfner and Hutch studied the normal urethra on VCUG
and postoperative VCUGs from different facilities to be com-
and described its radiological and anatomical features.8 Po-
pared. Perhaps with further data it can become a validated
pek et al looked at the histological and pathological changes
method of assessing satisfactory valve ablation.
in the urethra with development and with obstruction.9
Both groups hypothesized that the posterior urethra has the
capacity to stretch with increased voiding pressure due to its
unique histological and anatomical configuration, in con- Abbreviations and Acronyms
trast to the anterior urethral segment. There is variability of PUV ⫽ posterior urethral valve
urethral measurement depending on the stage of voiding, UR ⫽ urethral ratio
voided volume and position of the penis. VCUG ⫽ voiding cystourethrogram
Ideally, a catheter should not be left in the urethra on
voiding films. In reality some patients do not void without a REFERENCES
catheter, and a film showing the urethra with a catheter in
place is better than no film at all. An indwelling catheter will 1. Cromie, W. J., Cain, M. P., Bellinger, M. F., Betti, J. A. and
tend to decrease the urethral ratio by decompressing the Scott, J.: Urethral valve incision using a modified venous
posterior urethra and opening the anterior urethra. valvulotome. J Urol, 151: 1053, 1994
Endoscopic valve ablation is the preferred treatment for 2. Hulbert, W. C. and Duckett, J. W.: Current views on posterior
urethral valves. Pediatr Ann, 17: 31, 1988
posterior urethral valves. The aim of the procedure is to
3. Smith, G. H., Canning, D. A., Schulman, S. L., Snyder, H. M.,
relieve infravesical obstruction. Duckett and Snow observed III and Duckett, J. W.: The long-term outcome of posterior
that approximately 20% to 30% of patients require a second urethral valves treated with primary valve ablation and
procedure to achieve satisfactory valve ablation.10 They observation. J Urol, 155: 1730, 1996
stated that it was preferable to undercut rather than to 4. Edmond, T. and Gonzales, J.: Posterior urethral valves and
overcut, to avoid the risk of urethral stricture or inconti- other urethral anomalies. In: Campbell’s Urology, 6th ed.
nence. Our incidence of repeat valve ablation was slightly Edited by P. C. Walsh, R. F. Gittes, A. D. Perlmutter and
higher than that of Duckett and Snow. All patients who T. A. Stamey. Philadelphia: W. B. Saunders Co., chapt. 49,
required a second ablation were younger than 1 month, and pp. 1872–1892, 1992
were initially treated with cystoscopy and flexible electrode 5. Duckett, J. W., Jr.: Current management of posterior urethral
valves. Urol Clin North Am, 1: 471, 1974
ablation.
6. Eklof, O. and Ringertz, H.: Pre- and postoperative urographic
Some authors recommend routine cystoscopic followup findings in posterior urethral valves. Pediatr Radiol, 4: 43,
after valve ablation.7 This procedure has the advantage of 1975
allowing assessment of the valve ablation and further ther- 7. Imaji, R. and Dewan, P. A.: The clinical and radiological find-
apy if needed. However, it has the disadvantage of being ings in boys with endoscopically severe congenital posterior
more expensive and more invasive than repeat VCUG. Most urethral obstruction. BJU Int, 88: 263, 2001
authors accept that repeat VCUG at 6 weeks after valve 8. Shopfner, C. E. and Hutch, J. A.: The normal urethrogram.
ablation is the best method of assessing surgical outcome.4 Radiol Clin North Am, 6: 1659, 1968
We have demonstrated that urethral ratio can be measured 9. Popek, E. J., Tyson, R. W., Miller, G. J. and Caldwell, S. A.:
and that a decrease in this ratio appears to correlate with Prostate development in prune belly syndrome (PBS) and
posterior urethral valves (PUV): etiology of PBS—lower
our clinical assessment of a satisfactory valve ablation.
urinary tract obstruction or primary mesenchymal defect?
It could be argued that a better assessment of PUV ab- Pediatr Pathol, 11: 1, 1991
lation could be made with preoperative and postoperative 10. Duckett, J. W. and Snow, B. W.: Disorders of the urethra and
urodynamic studies. To perform urodynamic studies in in- penis. In: Campbell’s Urology, 5th ed. Edited by M. F.
fants, it is necessary to insert a suprapubic catheter to avoid Campbell and P. C. Walsh. Philadelphia: W. B. Saunders
interfering with urethral resistance during voiding. We be- Co., chapt. 48, pp. 2000 –2030, 1986
You might also like
- Better Orchiopexy and High Ligation 2016Document4 pagesBetter Orchiopexy and High Ligation 2016Richard QiuNo ratings yet
- Conventional Versus Laparoscopic Surgery For Acute AppendicitisDocument4 pagesConventional Versus Laparoscopic Surgery For Acute AppendicitisAna Luiza MatosNo ratings yet
- VVF RepairDocument4 pagesVVF RepairAdil KhurshidNo ratings yet
- Redo Psarp.Document4 pagesRedo Psarp.Siti Ruh Azizah100% (1)
- Three-Port vs Four-Port Laparoscopic Cholecystectomy: A Randomized TrialDocument4 pagesThree-Port vs Four-Port Laparoscopic Cholecystectomy: A Randomized TrialmenishefNo ratings yet
- Tau 06 03 510Document7 pagesTau 06 03 510Eko NoviantiNo ratings yet
- Endourology and Stone Diseases: Original ArticlesDocument5 pagesEndourology and Stone Diseases: Original ArticlesTatik HandayaniNo ratings yet
- Early Vaginal Replacement in Cloacal Malformation: Shilpa Sharma & Devendra K. GuptaDocument9 pagesEarly Vaginal Replacement in Cloacal Malformation: Shilpa Sharma & Devendra K. GuptaRohit GuptaNo ratings yet
- Laparoscopic Appendectomy For Complicated Appendicitis - An Evaluation of Postoperative Factors.Document5 pagesLaparoscopic Appendectomy For Complicated Appendicitis - An Evaluation of Postoperative Factors.Juan Carlos SantamariaNo ratings yet
- Lich GregoirDocument5 pagesLich GregoirIoannis ValioulisNo ratings yet
- Recurrence Rate of Endometriomas Following A Laparoscopic CystectomyDocument5 pagesRecurrence Rate of Endometriomas Following A Laparoscopic CystectomyPutri Tamara DasantosNo ratings yet
- Boaris FlapDocument6 pagesBoaris FlapNihal S KiranNo ratings yet
- Laparoscopic Appendectomy PostoperativeDocument6 pagesLaparoscopic Appendectomy PostoperativeDamal An NasherNo ratings yet
- Poh 2011Document8 pagesPoh 2011DH SiriruiNo ratings yet
- Complicated AppendicitisDocument4 pagesComplicated AppendicitisMedardo ApoloNo ratings yet
- Wrap Plication of Megaureter Around Normal-Sized Ureter For Complete Duplex System ReimplantationsDocument5 pagesWrap Plication of Megaureter Around Normal-Sized Ureter For Complete Duplex System ReimplantationsDirga Rasyidin LNo ratings yet
- Pemeriksaan IVPDocument41 pagesPemeriksaan IVPChandra Noor SatriyoNo ratings yet
- Risk of Failure in Pediatric Ventriculoperitoneal Shunts Placed After Abdominal SurgeryDocument31 pagesRisk of Failure in Pediatric Ventriculoperitoneal Shunts Placed After Abdominal SurgeryWielda VeramitaNo ratings yet
- Ultrasound Abdominal Alternative Peritoneal Lavage: J. Chambers & PilbrowDocument8 pagesUltrasound Abdominal Alternative Peritoneal Lavage: J. Chambers & PilbrowZuni TriyantiNo ratings yet
- Role of US and IVU in evaluating hematuriaDocument8 pagesRole of US and IVU in evaluating hematuriaalda aldaNo ratings yet
- Role of Transabdominal Ultrasound in Evaluating Patients With Acute Urinary Retention (Aur) Due To Benign Prostatic Hyperplasia (BPH)Document3 pagesRole of Transabdominal Ultrasound in Evaluating Patients With Acute Urinary Retention (Aur) Due To Benign Prostatic Hyperplasia (BPH)Yuni AngrianiNo ratings yet
- Jurnal 3Document3 pagesJurnal 3Ega Gumilang SugiartoNo ratings yet
- Ma 07004Document5 pagesMa 07004Lilik PrasajaNo ratings yet
- Undescended TestisDocument3 pagesUndescended TestisIoannis ValioulisNo ratings yet
- Original Research: Flexible Ureteroscopic Lithotripsy For The Treatment of Upper Urinary Tract Calculi in InfantsDocument7 pagesOriginal Research: Flexible Ureteroscopic Lithotripsy For The Treatment of Upper Urinary Tract Calculi in InfantsFusarina MumpuniNo ratings yet
- Primary Total Shoulder Arthroplasty Performed Entirely Thru The Rotator Interval - Technique and Minimum Two-Year OutcomesDocument10 pagesPrimary Total Shoulder Arthroplasty Performed Entirely Thru The Rotator Interval - Technique and Minimum Two-Year OutcomesmotohumeresNo ratings yet
- Isj-10132 CSDocument9 pagesIsj-10132 CSdavidgalcantaraNo ratings yet
- Pi Is 0022534715050119Document2 pagesPi Is 0022534715050119xtm69846No ratings yet
- Hep 20506Document7 pagesHep 20506Christos ChristidisNo ratings yet
- Ovarian Remnant Syndrome: 27 Cases of Pelvic Pain from Ovarian Tissue Remaining After Bilateral Salpingo-OophorectomyDocument3 pagesOvarian Remnant Syndrome: 27 Cases of Pelvic Pain from Ovarian Tissue Remaining After Bilateral Salpingo-OophorectomyFlaviu TabaranNo ratings yet
- Bess Is Sow 2014Document2 pagesBess Is Sow 2014Alfredo ChoquetNo ratings yet
- Complete Penile DisassemblyDocument2 pagesComplete Penile DisassemblyGunduz AgaNo ratings yet
- Posterior Sagittal Anorectoplasty in Anorectal MalformationsDocument5 pagesPosterior Sagittal Anorectoplasty in Anorectal MalformationsmustikaarumNo ratings yet
- Percutaneous Nephrolithotomy : Randomized Comparison of Large Bore, Small Bore and TubelessDocument6 pagesPercutaneous Nephrolithotomy : Randomized Comparison of Large Bore, Small Bore and TubelessAmir Akram MasihNo ratings yet
- Emergency Department Ultrasound in The Evaluation of Blunt Abdominal TraumaDocument5 pagesEmergency Department Ultrasound in The Evaluation of Blunt Abdominal TraumaesmoesNo ratings yet
- Liver Abscess: Catheter Drainage V/s Needle AspirationDocument6 pagesLiver Abscess: Catheter Drainage V/s Needle AspirationMishel Rodriguez GuzmanNo ratings yet
- Focusedassessment Withsonographyfor Trauma:Methods, Accuracy, and IndicationsDocument13 pagesFocusedassessment Withsonographyfor Trauma:Methods, Accuracy, and IndicationsOtto Guillermo SontayNo ratings yet
- Deep Venous Thrombosis After Total Joint ArthroplastyDocument7 pagesDeep Venous Thrombosis After Total Joint ArthroplastyJesse CusterNo ratings yet
- Prosthetic Repair of Acutely Incarcerated Groin Hernias: A Prospective Clinical Observational Cohort StudyDocument6 pagesProsthetic Repair of Acutely Incarcerated Groin Hernias: A Prospective Clinical Observational Cohort Studynh2411No ratings yet
- Yu 2013Document4 pagesYu 2013raissametasariNo ratings yet
- Striktur UretraDocument4 pagesStriktur UretramariamunsriNo ratings yet
- Modified Ureteral Orthotopic Reimplantation Method For Managing Infant Primary Obstructive Megaureter. 2016. ESTUDIO CLINICODocument5 pagesModified Ureteral Orthotopic Reimplantation Method For Managing Infant Primary Obstructive Megaureter. 2016. ESTUDIO CLINICOPaz MoncayoNo ratings yet
- Interest of Trans-Obturator Tape (Tot) in Stress Urinary Incontinence :series of 173 Women and 1 ManDocument5 pagesInterest of Trans-Obturator Tape (Tot) in Stress Urinary Incontinence :series of 173 Women and 1 ManIJAR JOURNALNo ratings yet
- Diagnostic Value of Combined Static Excretory MR Urogr - 2015 - Journal of AdvanDocument9 pagesDiagnostic Value of Combined Static Excretory MR Urogr - 2015 - Journal of AdvanSuresh SeerviNo ratings yet
- JurnlDocument29 pagesJurnlBarbie Nurdilia RNo ratings yet
- Bloomberg 1989 (Advantages of Paramedian Approach)Document5 pagesBloomberg 1989 (Advantages of Paramedian Approach)Olivia LimNo ratings yet
- Whitaker Test PDFDocument4 pagesWhitaker Test PDFKahn GenghisNo ratings yet
- Pi Is 0022534714035575Document2 pagesPi Is 0022534714035575Andri Feisal NasutionNo ratings yet
- Testiculo No PalpableDocument6 pagesTesticulo No PalpableisabellaNo ratings yet
- Bariatric SurgeryDocument4 pagesBariatric SurgeryCla AlsterNo ratings yet
- 1 s2.0 S0022480423002895 MainDocument7 pages1 s2.0 S0022480423002895 Mainlucabarbato23No ratings yet
- Sonographic Whirlpool Sign in Ovarian Torsion: S. Boopathy Vijayaraghavan, MD, DMRDDocument7 pagesSonographic Whirlpool Sign in Ovarian Torsion: S. Boopathy Vijayaraghavan, MD, DMRDjohnalanNo ratings yet
- Groin Hernia: VZI, But It May Well Be That A Long Follow-UpDocument3 pagesGroin Hernia: VZI, But It May Well Be That A Long Follow-UpAnas YahyaNo ratings yet
- Batchala 2021Document6 pagesBatchala 2021qrscentralNo ratings yet
- bien chung nieu mổ lấy thaiDocument4 pagesbien chung nieu mổ lấy thaiMint For MomsNo ratings yet
- Utd 04524 Clinical - Article KunduzDocument5 pagesUtd 04524 Clinical - Article Kunduzzenatihanen123No ratings yet
- Laparoscopic Orchidopexy: Current Surgical Opinion.: AbstractDocument6 pagesLaparoscopic Orchidopexy: Current Surgical Opinion.: AbstractGemiNo ratings yet
- Transcutaneous Laryngeal UltrasoundDocument8 pagesTranscutaneous Laryngeal UltrasoundKennie RamirezNo ratings yet
- Esophageal Preservation and Replacement in ChildrenFrom EverandEsophageal Preservation and Replacement in ChildrenAshwin PimpalwarNo ratings yet
- Contrast-Enhanced Ultrasound Imaging of Hepatic NeoplasmsFrom EverandContrast-Enhanced Ultrasound Imaging of Hepatic NeoplasmsWen-Ping WangNo ratings yet
- On Bed ListDocument2 pagesOn Bed ListNael NajeebNo ratings yet
- Online Seat Allocation INI-CETDocument2 pagesOnline Seat Allocation INI-CETNael NajeebNo ratings yet
- Results StaffNurse 28 01 2018 BW - 2Document41 pagesResults StaffNurse 28 01 2018 BW - 2Nael NajeebNo ratings yet
- MCHDocument1 pageMCHNael NajeebNo ratings yet
- Compendium of New and Emerging Health TechnologiesDocument54 pagesCompendium of New and Emerging Health TechnologiesDian NovitaNo ratings yet
- BridgewaterPureAlpha CaseStudy MPIDocument9 pagesBridgewaterPureAlpha CaseStudy MPIMichael Guan100% (2)
- Impact of NPA on Profitability of Nifty Index BanksDocument9 pagesImpact of NPA on Profitability of Nifty Index Banksmohammed salmanNo ratings yet
- Enterprise Resource Planning ERPDocument16 pagesEnterprise Resource Planning ERPsaifNo ratings yet
- CLASIFICACION RESUMEN Caton - Et - Al-2018-Journal - of - Clinical - PeriodontologyDocument12 pagesCLASIFICACION RESUMEN Caton - Et - Al-2018-Journal - of - Clinical - PeriodontologyDaniela RojasNo ratings yet
- Prescription AssignmentDocument6 pagesPrescription AssignmentChiela Alcantara BagnesNo ratings yet
- Characteristics of Young Language LearnersDocument16 pagesCharacteristics of Young Language Learnersfatihgun007No ratings yet
- Growth of Luxury Market & Products in IndiaDocument60 pagesGrowth of Luxury Market & Products in IndiaMohammed Yunus100% (2)
- Slevin 1986Document9 pagesSlevin 1986YuliaNo ratings yet
- Synthesis: Turn Learnings into Opportunities for DesignDocument12 pagesSynthesis: Turn Learnings into Opportunities for DesignLuisana MartínNo ratings yet
- G8DLL Q2W6 LC32-34Document17 pagesG8DLL Q2W6 LC32-34Joemard FranciscoNo ratings yet
- Sri Sri Ramakrishna Kathamrita - Volume 5Document289 pagesSri Sri Ramakrishna Kathamrita - Volume 5Estudante da VedantaNo ratings yet
- An Introduction To Identification & Intervention For Children With Sensory Processing DifficultiesDocument92 pagesAn Introduction To Identification & Intervention For Children With Sensory Processing DifficultiesFrancisca CondutoNo ratings yet
- Education and Social ChangeDocument13 pagesEducation and Social ChangeBert M DronaNo ratings yet
- Iowa Board of Regents Settlement Agreement 3Document108 pagesIowa Board of Regents Settlement Agreement 3kcrgdotcomNo ratings yet
- Recommended Curriculum: Seven (7) Types of CurriculumDocument1 pageRecommended Curriculum: Seven (7) Types of CurriculummoyesaNo ratings yet
- Access NCERT Solutions For Class 6 Chapter 14 - UpDocument5 pagesAccess NCERT Solutions For Class 6 Chapter 14 - UpKamjith PadinjareveeduNo ratings yet
- Apiaceae (Umbelliferae) : The Carrot FamilyDocument1 pageApiaceae (Umbelliferae) : The Carrot FamilyHamid AwanNo ratings yet
- CV Zahrotun NisaDocument2 pagesCV Zahrotun NisaZahro ShaziaNo ratings yet
- Letter of Undertaking for Cargo ReleaseDocument1 pageLetter of Undertaking for Cargo ReleaseSitiJamilahAlimanNo ratings yet
- 10 Steps For Avoiding Teacher BurnoutDocument3 pages10 Steps For Avoiding Teacher BurnoutSarah DeNo ratings yet
- Differentiation Between Complex Tic and Eyelid Myoclonia With Absences: Pediatric Case Report and Brief Review of The LiteratureDocument5 pagesDifferentiation Between Complex Tic and Eyelid Myoclonia With Absences: Pediatric Case Report and Brief Review of The LiteratureAperito InternationalNo ratings yet
- Role of education in curbing child labourDocument11 pagesRole of education in curbing child labourA.n. Surya100% (2)
- Economy Shipping Case AnswersDocument72 pagesEconomy Shipping Case Answersreduay67% (3)
- CARAVAL - Opening ExtractDocument29 pagesCARAVAL - Opening ExtractHodder Stoughton100% (1)
- WNL Slum Golf The Sport That Stormed The Streets of Mumbai UppDocument5 pagesWNL Slum Golf The Sport That Stormed The Streets of Mumbai UppStephen McKennaNo ratings yet
- A Beautiful Day in The Neighborhood Activity GuideDocument13 pagesA Beautiful Day in The Neighborhood Activity GuideQuirk Books100% (8)
- Afsm 2011Document4 pagesAfsm 2011Rakshit SehgalNo ratings yet
- Jadwal Pemeliharaan Alat Medik ICUDocument28 pagesJadwal Pemeliharaan Alat Medik ICUsarifahaniNo ratings yet
- SHS General Mathematics Q2 M7Document16 pagesSHS General Mathematics Q2 M7Abegail PanangNo ratings yet
- Human Resource Management Practices andDocument12 pagesHuman Resource Management Practices andMoathNo ratings yet