Professional Documents
Culture Documents
Survival Analysis of Treatment Defaulters
Uploaded by
Dr. Meghana NarendranOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Survival Analysis of Treatment Defaulters
Uploaded by
Dr. Meghana NarendranCopyright:
Available Formats
Original Article
Survival Analysis of Treatment Defaulters among Tuberculosis
Patients in Government Medical College and Hospital,
Aurangabad
Downloaded from http://journals.lww.com/ijcm by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AW
Apeksha Premnath Paunikar, Hrishikesh Arvindrao Khadilkar, Mohan Kondiba Doibale, Avinash R. Lamb1
Departments of Community Medicine and 1TB and Chest, Government Medical College and Hospital, Aurangabad, Maharashtra, India
nYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8K2+Ya6H515kE= on 07/11/2023
Abstract
Context: Tuberculosis (TB) patients who do not complete treatment pose a potential public health risk through disease reactivation,
increased transmission, and development of drug resistance. Aims: (1) To determine the duration TB patients stay in the treatment
before defaulting. (2) Factors associated with defaulters who had been treated in Government Medical College and Hospital (GMCH),
Aurangabad. Setting and Design: The study was conducted at TB Unit of GMCH, Aurangabad, and community. This was a retrospective
cohort study. Materials and Methods: Based on record review of 440 bacteriological‑confirmed TB patients enrolled in the TB Unit of GMCH,
Aurangabad, in 2015 from January 1, to December 31, we collected information on potential risk factors of all confirmed cases by primary and
secondary data. For survival analysis, outcome of interest was treatment defaulter. Kaplan–Meier curves, log‑rank test, and Cox‑proportional
hazard regression analysis were used to model outcome of interest. Statistical Analysis Used: Statistical analysis is performed using SPSS
version 17. Results: Out of total 440 TB patients registered, 13 patients got defaulted in 2015. Overall mean time of default was 279 days,
with 276 days for males against 279 days for females. Many patients interrupted treatment during continuation phase. Treatment defaulters
had an association with gender, category at the initiation of treatment, HIV status, smoking, and alcohol consumption. Conclusion: Targeted
intervention with the goal toward adherence in persons abusing smoking and alcohol is recommended. Necessary actions need to be initiated
in the program to strengthen the follow‑up of patients and to bring behavioral changes by proper counseling.
Keywords: Cox proportional hazard, log‑rank, survival analysis, treatment defaulters
Introduction treatment was interrupted for 2 consecutive months or
more.[4]
Tuberculosis (TB) is an infectious disease which continues
to be the leading cause of death. According to the Global TB Many studies have been conducted on TB; however, very
Report 2017, released by the WHO, India has topped list of few studies that focus specifically on survival analysis of TB
seven countries accounting for 64% of over 10 million new patients are present till date. Survival analysis is generally
TB cases worldwide in 2016. An estimated 1.7 million people defined as a set of methods for analyzing data where the
died from TB in 2016.[1] outcome variable is the time until the occurrence of an event of
interest. In survival analysis, subjects are usually followed over
India accounts for one‑fourth of the global TB burden. In 2015,
a specified time period, and the focus is on the time at which
an estimated 28 lakh cases occurred and 4.8 lakh people died
due to TB.[2]
Address for correspondence: Dr. Hrishikesh Arvindrao Khadilkar,
TB patients who do not complete treatment pose a Department of Community Medicine, Government Medical College,
Aurangabad ‑ 431 001, Maharashtra, India.
potential public health risk. Although DOTS coverage and E‑mail: hak4049@gmail.com
health workers involvement in TB prevention and control
activities is improving, patients still are failing to complete
their treatment.[3] Defaulter is defined as a patient whose This is an open access journal, and articles are distributed under the terms of the Creative
Commons Attribution‑NonCommercial‑ShareAlike 4.0 License, which allows others to
remix, tweak, and build upon the work non‑commercially, as long as appropriate credit
Access this article online is given and the new creations are licensed under the identical terms.
Quick Response Code: For reprints contact: reprints@medknow.com
Website:
www.ijcm.org.in
How to cite this article: Paunikar AP, Khadilkar HA, Doibale MK,
Lamb AR. Survival analysis of treatment defaulters among tuberculosis
patients in government medical college and hospital, Aurangabad. Indian J
DOI:
10.4103/ijcm.IJCM_292_18
Community Med 2019;44:44-7.
Received: 21‑09‑18, Accepted: 31-01-19
44 © 2019 Indian Journal of Community Medicine | Published by Wolters Kluwer - Medknow
Paunikar, et al.: Survival analysis of treatment defaulters among TB patients
the event of interest occurs. However, the difficulty commonly Kaplan–Meier curves, log‑rank test, and Cox‑proportional
encountered is only some individuals’ experience the event, hazard regression analysis were used to display the probability
and subsequently, survival times will be unknown for subset of treatment defaulter over time for each risk factor. SPSS
of the study group. This phenomenon is called censoring.[4] For version 17 was used for statistically significant.
example, a patient has not experienced the relevant outcome
by the time of close of the study or patient lost to follow‑up Results
during the study or patient experiences different event.
Downloaded from http://journals.lww.com/ijcm by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AW
A total of 440 bacteriological‑confirmed TB patients who
Duration of treatment is important in deciding survival initiated treatment, 249 (56.59%) were male patients, and
of patients.[5] Further, improving treatment outcomes and 191 (43.41%) were female patients. At the initiation of
designing effective interventions require understanding of treatment, 365 (82.95%) were of Category I, 74 (16.82%) of
factors that prevent people from adhering and those that help
nYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8K2+Ya6H515kE= on 07/11/2023
Category II, and 1 (0.23%) patient of Category III. More than
in treatment completion.[6,7] half (57.27%) were classified as smear‑positive PTB, 12.05%
Hence, the present study was designed to determine the duration were smear‑negative PTB, and 30.68% were EPTB cases.
TB patients stay in treatment before defaulting and factors 416 (94.55%) TB patients were from urban area and 24 (5.45%)
associated with defaulters who had been treated in Government from rural area. 432 (98.18%) were HIV negative while 8 (1.82%)
Medical College and Hospital (GMCH), Aurangabad. patients were HIV positive. 135 (30.68%) were smokers and
305 (69.32%) nonsmokers. 147 (33.41%) were consuming
alcohol and the rest 293 (66.59%) were nondrinkers [Table 1].
Materials and Methods
Out of total 440, 13 (2.95%) patients were defaulters. Out
The retrospective cohort study was carried out at GMCH,
of 13 defaulted patients, 12 (92.31%) were males and
Aurangabad, for all the 440 TB cases registered in TB Unit
1 (7.69%) female. Twelve patients got defaulted during
of the hospital from January 1, 2015, to December 31, 2015.
continuation phase. Overall, the mean time of default was
This included smear‑positive pulmonary TB (PTB) patients,
279 days and was 276 days for males against 279 days for
smear‑negative PTB patients, and extra‑PTB (EPTB) patients.
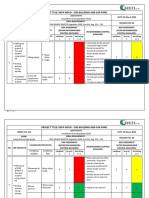
females [Table 2 and Figure 1], with significance on log‑rank
The study protocol was approved by the ethics committee.
test (P < 0.05) [Table 3]. Hazard ratio (HR): 0.114 showed
Informed consent was taken from the participants before
inclusion.
Smear‑positive pulmonary case was defined as a patient with Table 1: Demographic and clinical characteristics of
one or more initial sputum smear examination (acid‑fast tuberculosis patients initiating tuberculosis treatment
bacilli [AFB+]) or one sputum examination AFB+ and at Government Medical College and Hospital,
radiographic abnormalities consistent with active PTB as Aurangabad (n=440)
determined by a clinician. Smear‑negative pulmonary case Variable Frequency (%)
defined as patient with at least two sputum smear examinations Sex
negative for AFB and radiographic abnormalities consistent Male 249 (56.59)
with active PTB with no response to a course of broad‑spectrum Female 191 (43.41)
antibiotics. EPTB case was defined as a patient with TB of Category (patient history)
organs other than the lungs. I 365 (82.95)
Secondary data were abstracted from TB treatment registers II 74 (16.82)
in GMCH, Aurangabad. These included demographic III 1 (0.23)
Types of TB
data (age, sex, residence) and treatment data (treatment
Smear‑positive PTB 252 (57.27)
observer, category, i.e. Category I and Category II, patient
Smear‑negative PTB 53 (12.05)
types, i.e. new, relapse, failure, treatment after default,
EPTB 135 (30.68)
transfer status, HIV status, treatment regimen, sputum smear
Address of patients
microscopy results, date of start and end of treatment, and
Urban 416 (94.55)
treatment outcome). Rural 24 (5.45)
To obtain primary data, TB patients were interviewed using HIV test/result
a questionnaire by visiting their residence with the help of Negative 432 (98.18)
community health workers who had been trained to collect Positive 8 (1.82)
the relevant information from the patient. The information Smoking status
was collected on alcohol, smoking habits, and other relevant Yes 135 (30.68)
information about the patient. No 305 (9.32)
Alcohol consumption
For the survival analysis, the outcome of interest was treatment Yes 147 (33.41)
defaulter. For the purpose of our analysis, only the times for No 293 (66.59)
patients who were defaulted were taken as event. TB: Tuberculosis, PTB: Pulmonary TB, EPTB: Extra‑PTB
Indian Journal of Community Medicine ¦ Volume 44 ¦ Issue 1 ¦ January-March 2019 45
Paunikar, et al.: Survival analysis of treatment defaulters among TB patients
that probability of defaulting was less by 89% in females than 238 and 280 days, respectively. Log‑rank test (P > 0.05) was
males at any given time [Table 4]. not significant [Table 3]. HR: 0.250 indicated that probability
of defaulting was 75% less in HIV‑negative defaulter patients
Of the total, 5 (38.46%) from Category I and 8 (61.54%) from
as compared to HIV positive [Table 4].
Category 2 got defaulted and no one defaulted in Category 3.
Survival curves showed in [Figure 2]. Log‑rank test showed Regarding smoking status, 8 (61.54%) were smokers
significant difference (P < 0.001) [Table 3]. The value of HR: and 5 (38.46%) nonsmokers with a mean survival time
Downloaded from http://journals.lww.com/ijcm by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AW
276.033 for Category I and HR: 2003.025 for Category II of 254 and 283 days, respectively. Log‑rank test was
indicated that Category II had far more chance of defaulting significant (P < 0.05) [Table 3]. HR: 0.266 indicates that
nonsmokers have 74% less chance of defaulting than smokers
than Category I with no default in Category III [Table 5].
with significance at 5% probability level.
Out of 13, 1 (7.69%) HIV‑positive and 12 (92.31%)
nYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8K2+Ya6H515kE= on 07/11/2023
In concern with alcohol status, 6 (46.15%) were drinkers and
HIV‑negative patients defaulted with mean duration of defaulter
7 (53.85%) nondrinkers with a mean survival time of 273
and 279 days, respectively [Figure 3]. Log‑rank test was not
Table 2: Survival analysis of defaulters according to significant (P > 0.05) [Table 3]. HR: 0.602 indicated that
gender nondrinkers have 40% less risk of defaulting as compared to
drinkers [Table 4].
Meana
Estimate SE 95% CI
Discussion
Upper bound Lower bound
Very few studies on survival analysis of defaulter patients
Male 275.704 3.021 269.784 281.625
among TB have been carried out till recently. In our study, we
Female 278.663 1.333 276.050 281.276
found that 13 (2.95%) patients got defaulted while the rate of
Overall 279.225 2.010 275.285 283.165
a
Estimation is limited to the largest survival time if it is censored.
default was 13.5% in Ethiopian study.[3]
CI: Confidence interval, SE: Standard error In our study, 92.31% of defaulters were documented during
continuation phase. This may be due to less vigilant follow‑up
Table 3: Descriptive statistics of survival data of of patients during continuation phase as compared to intensive
defaulters (SPSS output of Kaplan-Meier estimator) phase. This is similar the findings of Ajagbe et al.,[4] which had
Covariates Log rank df Significant
Sex
Male 6.350 1 0.012
Female
Category
I 15.685 2 0.000
II
III
HIV status
HIV positive 2.053 1 0.152
HIV negative
Smoking
Yes 6.220 1 0.013
No
Alcohol
Yes 0.851 1 0.356
Figure 1: Kaplan–Meier estimate for survival probability based on gender
No of patients
Table 4: SPSS output for covariates with survival time (Cox regression analysis) for gender, HIV status, smoking, and
alcohol
B SE Wald df Significant Exp (B) 95.0% CI for Exp (B)
Lower Upper
Gender −2.174 1.042 4.356 1 0.037 0.114 0.015 0.876
HIV status −1.385 1.045 1.756 1 0.185 0.250 0.032 1.942
Smoking −1.323 0.570 5.387 1 0.020 0.266 0.087 0.814
Alcohol −0.508 0.557 0.833 1 0.361 0.602 0.202 1.791
SE: Standard error, CI: Confidence interval
46 Indian Journal of Community Medicine ¦ Volume 44 ¦ Issue 1 ¦ January-March 2019
Paunikar, et al.: Survival analysis of treatment defaulters among TB patients
Downloaded from http://journals.lww.com/ijcm by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AW
nYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8K2+Ya6H515kE= on 07/11/2023
Figure 2: Kaplan–Meier estimate for survival probability based on three Figure 3: Kaplan–Meier estimate for survival probability based on alcohol
categories at the initiation of treatment status
Table 5: SPSS output for covariates with survival association with gender, category at initiation of treatment,
time (Cox regression analysis) in relation to category at HIV status, smokers, and alcohol consumption. Hence,
start of treatment enhanced patient pretreatment counseling and constant
motivation specifically to males, Category II, HIV positive,
B SE Wald df Significant Exp (B)
smokers, and alcoholic TB patients during follow‑ups
Treat cat at 11.465 2 0.003
start
to complete treatment without interruption are needed.
Treat cat at 5.621 131.462 0.002 1 0.966 276.033
Education on behavior change of patients is essential.
start (1) Targeted intervention aimed at assuring adherence in
Treat cat at 7.602 131.461 0.003 1 0.954 2003.025 persons abusing smoking and alcohol is also recommended.
start (2) Necessary actions need to be initiated in the TB control
SE: Standard error program to strengthen the follow‑up of patients with TB
from start to completion of treatment based on the factors
shown 70% patients interrupted treatment during continuation associated with defaulters.
phase.
Financial support and sponsorship
In the present study, we found significant difference in survival Nil.
curves of male and female in contrast to the findings of Ajagbe
et al.,[4].in which no significant difference was found. Conflicts of interest
There are no conflicts of interest.
In this study, there was more chance of defaulting in Category
II than Category I with no default in Category III which is
similar to the findings of the study in South India which stated References
that survival probabilities of Category II patients are less than 1. World Health Organization. Global TB Report 2017. Geneva: WHO;
2017.
Category I and III.[5] 2. TB India 2017, RNTCP Annual Status Report, Central TB Division,
Nirman Bhavan, New Delhi: Directorate General Services of Health
In our study, although HIV negative defaulted late as compared
Services, Ministry of Health and Family Welfare; 2017.
to HIV positive, difference was not significant on log‑rank 3. Akessa GM, Tadesse M, Abebe G. Survival analysis of loss to
test (P > 0.05). On the other hand, being HIV‑positive appeared follow‑up treatment among tuberculosis patients at Jimma University
to be associated with defaulter in univariate but not in the Specialized Hospital, Jimma, Southwest Ethiopia. Int J Stat Mech
2015;7:923025. [doi: 10.1155/2015/923025].
multivariate analysis in the study of Ethiopia.[3]
4. Ajagbe OB, Kabair Z, O’Connor T. Survival analysis of adult
In Ajagbe et al.,[4] smokers and alcohol drinkers had hazard of tuberculosis disease. PLoS One 2014;9:e112838.
5. Vasantha M, Gopi PG, Subramani R. Survival of tuberculosis patients
1.8 and were associated with shorter survival time of defaulters treated under dots in a rural tuberculosis unit (TU), South India. Indian
which is similar to the present findings of the study with HR J Tuberc 2008;55:64‑9.
of 0.266 and 0.602 for smoking and alcohol, respectively, 6. Muture BN, Keraka MN, Kimuu PK, Kabiru EW, Ombeka VO, Oguya F,
indicating that the nonsmokers have 74% less chance of et al. Factors associated with default from treatment among tuberculosis
patients in Nairobi Province, Kenya: A case control study. BMC Public
defaulting and nondrinkers have 40% less risk of defaulting. Health 2011;11:696.
7. Senbeta A, Weldegerima G, Romha G. Survival analysis and
Conclusion associated risk factors of tuberculosis in‑hospital patients’ death in
Hawassa city and at Yirgalem town health centers. World J Med Sci
The present study showed treatment defaulters had an 2014;11:382‑8.
Indian Journal of Community Medicine ¦ Volume 44 ¦ Issue 1 ¦ January-March 2019 47
You might also like
- Clinical Synopsis of COVID-19: Evolving and ChallengingFrom EverandClinical Synopsis of COVID-19: Evolving and ChallengingHemanshu PrabhakarNo ratings yet
- LHQW Korea ChinaDocument7 pagesLHQW Korea ChinaFebie DevinaNo ratings yet
- 1 s2.0 S2213422020302766 MainDocument7 pages1 s2.0 S2213422020302766 MainJOSIAH JEFFERSON CABRERANo ratings yet
- TB 2Document12 pagesTB 2ikNo ratings yet
- 2021 - Factors Affecting Outcome of Longer Regimen Multidrug-Resistant Tuberculosis Treatment in West Java Indonesia A Retrospective Cohort StudyDocument13 pages2021 - Factors Affecting Outcome of Longer Regimen Multidrug-Resistant Tuberculosis Treatment in West Java Indonesia A Retrospective Cohort StudyNurul RifqianiNo ratings yet
- Comparison of The Efficacy and Safety of 2 Different Antiretroviral Regimens in Tertiary Care Hospital: A Retrospective Observational StudyDocument5 pagesComparison of The Efficacy and Safety of 2 Different Antiretroviral Regimens in Tertiary Care Hospital: A Retrospective Observational StudyNarendranath SNo ratings yet
- 6 - Iype2014Document7 pages6 - Iype2014Muhammad SyaifullahNo ratings yet
- Medi 99 E23649Document6 pagesMedi 99 E23649kornelis aribowoNo ratings yet
- Early Initiation of ARV Therapy Among TB-HIV Patients in Indonesia Prolongs Survival Rates!Document6 pagesEarly Initiation of ARV Therapy Among TB-HIV Patients in Indonesia Prolongs Survival Rates!Eka CintyaNo ratings yet
- Early Initiation of ARV Therapy Among TB-HIV Patients in Indonesia Prolongs Survival Rates!Document9 pagesEarly Initiation of ARV Therapy Among TB-HIV Patients in Indonesia Prolongs Survival Rates!Ayu DinafebrianiNo ratings yet
- 1 s2.0 S120197121400037X MainDocument5 pages1 s2.0 S120197121400037X MainAisyNo ratings yet
- 1 s2.0 S0422763815301023 MainDocument4 pages1 s2.0 S0422763815301023 MainEghar EverydayishellNo ratings yet
- Nejmoa 2104535Document12 pagesNejmoa 2104535niken maretasariNo ratings yet
- The Efficacy of Daily Chlorhexidine Bathing For Preventing Healthcare-Associated Infections in Adult Intensive Care UnitsDocument12 pagesThe Efficacy of Daily Chlorhexidine Bathing For Preventing Healthcare-Associated Infections in Adult Intensive Care UnitsKanameMizumiNo ratings yet
- International Journal of Infectious DiseasesDocument5 pagesInternational Journal of Infectious DiseasesNovita maraNo ratings yet
- Safety of Cupping Therapy in Studies Conducted in Twenty One Century: A Review of LiteratureDocument12 pagesSafety of Cupping Therapy in Studies Conducted in Twenty One Century: A Review of LiteratureMona HassanNo ratings yet
- Treatment Seeking Behavior and Factors Associated With Its Delay Among Newly Diagnosed Pulmonary Tuberculosis Patients in Bhopal, Madhya PradeshDocument6 pagesTreatment Seeking Behavior and Factors Associated With Its Delay Among Newly Diagnosed Pulmonary Tuberculosis Patients in Bhopal, Madhya PradeshAdvanced Research PublicationsNo ratings yet
- Bao Et AlDocument7 pagesBao Et Alkang.asep008No ratings yet
- Ofx 137Document7 pagesOfx 137Sheila Alcalde RNo ratings yet
- Apjtd 03 03 227Document5 pagesApjtd 03 03 227Yoggi Nurr HiddayattNo ratings yet
- 16 RaDocument10 pages16 RaNitish TankNo ratings yet
- Template Article UpdateDocument11 pagesTemplate Article UpdateAnggun SasmitaNo ratings yet
- J Clin Tuberc Other Mycobact Dis: SciencedirectDocument4 pagesJ Clin Tuberc Other Mycobact Dis: SciencedirectHelenaNo ratings yet
- Pone 0142607 PDFDocument9 pagesPone 0142607 PDFNurul Muqarribah Pratiwi IshaqNo ratings yet
- Assessment of Factors Influencing Tuberculosis Diagnostic and Treatment Delays Among Patients at Two Tertiary Hospitals in Ishaka, BushenyiDocument11 pagesAssessment of Factors Influencing Tuberculosis Diagnostic and Treatment Delays Among Patients at Two Tertiary Hospitals in Ishaka, BushenyiKIU PUBLICATION AND EXTENSIONNo ratings yet
- 1 s2.0 S2210803316300781 MainDocument8 pages1 s2.0 S2210803316300781 MainGilang Aji P. EmonNo ratings yet
- 19 37 3 PBDocument6 pages19 37 3 PBWidia Ade SeptianaNo ratings yet
- Pone 0198080Document15 pagesPone 0198080kornelis aribowoNo ratings yet
- Pone 0150849Document12 pagesPone 0150849yeremia imanuelNo ratings yet
- Penelitian AbstraktifDocument9 pagesPenelitian AbstraktifYondi Piter PapulungNo ratings yet
- Effect of Isoniazid Preventive Therapy On PulmonaryDocument5 pagesEffect of Isoniazid Preventive Therapy On Pulmonaryketut suryanaNo ratings yet
- Arsad Et AlDocument10 pagesArsad Et Alkang.asep008No ratings yet
- Dosis FlowDocument6 pagesDosis FlowArhaMozaNo ratings yet
- Mortality in HIV and TB-NaidooDocument13 pagesMortality in HIV and TB-Naidoodani catriaNo ratings yet
- Health Related Quality of Life Among TB Patients Q PDFDocument8 pagesHealth Related Quality of Life Among TB Patients Q PDFAmna SaifullahNo ratings yet
- Factors Influencing Quality of Life Among People Living With HIV in Coastal South IndiaDocument7 pagesFactors Influencing Quality of Life Among People Living With HIV in Coastal South IndiadrpklalNo ratings yet
- 360 1442 2 PBDocument8 pages360 1442 2 PBEghar EverydayishellNo ratings yet
- Pone 0194087 PDFDocument15 pagesPone 0194087 PDFInekeNo ratings yet
- Development and Validation of A Nomogram Using On Admission Routine Laboratory Parameters To Predict In-Hospital Survival of Patients With COVID-19Document23 pagesDevelopment and Validation of A Nomogram Using On Admission Routine Laboratory Parameters To Predict In-Hospital Survival of Patients With COVID-19dariusNo ratings yet
- Electrohomoeopathy Medicine in Covid19 A Multicenter Clinical ObservationalDocument4 pagesElectrohomoeopathy Medicine in Covid19 A Multicenter Clinical Observationaluraigal9728No ratings yet
- Treatment OutcomesDocument7 pagesTreatment OutcomestarisafidiaNo ratings yet
- Global Treatment Outcomes of Extensively Drug-Resistant Tuberculosis in Adults - A Systematic Review and Meta-AnalysisDocument13 pagesGlobal Treatment Outcomes of Extensively Drug-Resistant Tuberculosis in Adults - A Systematic Review and Meta-AnalysisEghar EverydayishellNo ratings yet
- JurnalDocument7 pagesJurnalRahmi SilviyaniNo ratings yet
- AAP - Guideline Adoption PneumoniaDocument15 pagesAAP - Guideline Adoption PneumoniaSonia FitrianiNo ratings yet
- 576-Article Text-5306-3-10-20210430Document5 pages576-Article Text-5306-3-10-20210430Sudartoshanan DartoNo ratings yet
- 1 s2.0 S2589537023000573 MainDocument11 pages1 s2.0 S2589537023000573 MainSadia MacavilcaNo ratings yet
- Cigarette Smoking and Health-Promoting Behaviours Among Tuberculosis Patients in Rural AreasDocument9 pagesCigarette Smoking and Health-Promoting Behaviours Among Tuberculosis Patients in Rural AreasMaria FulgensiaNo ratings yet
- 10 5588@ijtld 14 0963Document8 pages10 5588@ijtld 14 0963Oscar Rosero VasconesNo ratings yet
- A Study of Nutritional Assessment of Newly Diagnos PDFDocument7 pagesA Study of Nutritional Assessment of Newly Diagnos PDFKaushik SahaNo ratings yet
- Factor Associated With Unfavourable Treatment Outcome Among Adult Tuberculosis Patients in Agra: A Cross-Sectional StudyDocument7 pagesFactor Associated With Unfavourable Treatment Outcome Among Adult Tuberculosis Patients in Agra: A Cross-Sectional StudyIJAR JOURNALNo ratings yet
- Covid 19 Patients' Clinical Characteristics, Discharge Rate, and Fatality Rate of Meta AnalysisDocument7 pagesCovid 19 Patients' Clinical Characteristics, Discharge Rate, and Fatality Rate of Meta AnalysisDelfina RubioNo ratings yet
- Servikal TBDocument15 pagesServikal TBnur wahidaNo ratings yet
- Evaluation of Tuberculosis Control Programs in Indonesian Community Health Centers Using Systemic ApproachDocument7 pagesEvaluation of Tuberculosis Control Programs in Indonesian Community Health Centers Using Systemic ApproachYoseph 'schatzi' DmcNo ratings yet
- 1 s2.0 S2173511517301550 MainDocument6 pages1 s2.0 S2173511517301550 MainHermenegildo chitumbaNo ratings yet
- HIV Publication - DR DigvijayDocument7 pagesHIV Publication - DR DigvijayDigvijay ChavanNo ratings yet
- Evaluation Factors Contributing To The Treatment Default by Tuberculosis Patients at ART Clinic in Ishaka Adventist Hospital, Bushenyi District, Uganda.Document15 pagesEvaluation Factors Contributing To The Treatment Default by Tuberculosis Patients at ART Clinic in Ishaka Adventist Hospital, Bushenyi District, Uganda.KIU PUBLICATION AND EXTENSIONNo ratings yet
- ProkalsitoninDocument9 pagesProkalsitoninAndhika HamdanyNo ratings yet
- MainDocument6 pagesMainkornelis aribowoNo ratings yet
- Understanding The Gaps in DR TB Care Casc - 2020 - Journal of Clinical TuberculoDocument16 pagesUnderstanding The Gaps in DR TB Care Casc - 2020 - Journal of Clinical TuberculoKarina ChristantoNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument4 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- 22 Ref Doc VH202 White Paper PART2 Draft05Document6 pages22 Ref Doc VH202 White Paper PART2 Draft05Gaelle BaudouinNo ratings yet
- Neonatal Antiepileptic Medication Treatment Patterns A Decade of ChangeDocument8 pagesNeonatal Antiepileptic Medication Treatment Patterns A Decade of ChangeEduardo Rios DuboisNo ratings yet
- Water Resources EngineeringDocument22 pagesWater Resources EngineeringBethel Princess Flores100% (1)
- Outreach Service in Selected Local in Lagos NigeriaDocument48 pagesOutreach Service in Selected Local in Lagos NigeriaDOYINSOLA ADENUGANo ratings yet
- Safe - Work - Method - Statement - Roof - Truss - Installation V1.0Document8 pagesSafe - Work - Method - Statement - Roof - Truss - Installation V1.0hurairamughal666No ratings yet
- High-Risk Pregnancy CareDocument34 pagesHigh-Risk Pregnancy CareShaufyqyn EzaniNo ratings yet
- Ansi Asse Z359.15 2014 PDFDocument48 pagesAnsi Asse Z359.15 2014 PDFrengenier2750% (2)
- Insanity Workout DVDDocument2 pagesInsanity Workout DVDshopzillahouse001No ratings yet
- Summary Report For:: 29-1131.00 - VeterinariansDocument6 pagesSummary Report For:: 29-1131.00 - Veterinariansapi-266289406No ratings yet
- Adult Friends Diaper (Thought Process)Document2 pagesAdult Friends Diaper (Thought Process)Rohan HiremathNo ratings yet
- Video Games BenefitsDocument8 pagesVideo Games BenefitsAbdussalam100% (2)
- Child Labor and Health: A Systematic Literature Review of The Impacts of Child Labor On Child 'S Health in Low-And Middle-Income CountriesDocument9 pagesChild Labor and Health: A Systematic Literature Review of The Impacts of Child Labor On Child 'S Health in Low-And Middle-Income CountriesNabila IsnaniNo ratings yet
- Vendor ManualDocument19 pagesVendor Manualvinurules20No ratings yet
- School of Distance Education (University of Calicut) : Model Project For BA Political Science ProgrammeDocument32 pagesSchool of Distance Education (University of Calicut) : Model Project For BA Political Science Programmejitendra panigrahiNo ratings yet
- Brick Work JSA HSE ProfessionalsDocument1 pageBrick Work JSA HSE ProfessionalsStansilous Tatenda NyagomoNo ratings yet
- Medic Shoes - Clinic Report - 25/10/2020Document49 pagesMedic Shoes - Clinic Report - 25/10/2020יפה גולןNo ratings yet
- Sulit 013 (B) : Berdasarkan Gambar Yang Diberi, Berikan Jawapan Yang Lengkap. Tulis Jawapan Kamu Di Tempat Yang DisediakanDocument7 pagesSulit 013 (B) : Berdasarkan Gambar Yang Diberi, Berikan Jawapan Yang Lengkap. Tulis Jawapan Kamu Di Tempat Yang DisediakanMar OmarNo ratings yet
- ResearchDocument26 pagesResearchJhen de Vera83% (12)
- Brukner and Khans Clinical Sports Medicine Injuries, Volume 1 - MedicineDocument7 pagesBrukner and Khans Clinical Sports Medicine Injuries, Volume 1 - Medicinezaferyha17% (6)
- Clinical Case Presentation - Score - SheetDocument1 pageClinical Case Presentation - Score - SheetHema LaughsalotNo ratings yet
- Irr FinalDocument7 pagesIrr Finalapi-612103161No ratings yet
- What Is Alcohol2012AAlisherMDPhDDocument58 pagesWhat Is Alcohol2012AAlisherMDPhDAlisher AgzamovNo ratings yet
- 013 HIRARC Installation of Hoisting BeamDocument8 pages013 HIRARC Installation of Hoisting Beambdiey100% (1)
- Consenso Chileno de Técnicas de Kinesiología Respiratoria en PediatríaDocument15 pagesConsenso Chileno de Técnicas de Kinesiología Respiratoria en PediatríaRobert CerdaNo ratings yet
- Physical Assessment of The GentialiaDocument48 pagesPhysical Assessment of The GentialiaWilliam Lim100% (2)
- Natural Hygiene MagazineDocument33 pagesNatural Hygiene MagazineColm Rooney100% (1)
- Sickle Cell AnaemiaDocument8 pagesSickle Cell AnaemiaBhargav DesaiNo ratings yet
- BookOfSuicide1 201Document103 pagesBookOfSuicide1 201DEShifNo ratings yet
- Occupational Hazards in Dentistry: Acta Scientific DENTAL SCIENCES (ISSN: 2581-4893)Document7 pagesOccupational Hazards in Dentistry: Acta Scientific DENTAL SCIENCES (ISSN: 2581-4893)nioh envisNo ratings yet
- Mpulungu Trust Summary ProfileDocument4 pagesMpulungu Trust Summary ProfileViktor Dmitri KanyozeNo ratings yet
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsFrom EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsRating: 4.5 out of 5 stars4.5/5 (39)
- Summary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisFrom EverandSummary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (5)
- An Autobiography of Trauma: A Healing JourneyFrom EverandAn Autobiography of Trauma: A Healing JourneyRating: 5 out of 5 stars5/5 (2)
- Feel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveFrom EverandFeel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveRating: 4 out of 5 stars4/5 (250)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)
- Summary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDFrom EverandSummary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDRating: 4.5 out of 5 stars4.5/5 (167)
- My Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesFrom EverandMy Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesRating: 5 out of 5 stars5/5 (70)
- Rewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryFrom EverandRewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryRating: 4.5 out of 5 stars4.5/5 (158)
- Redefining Anxiety: What It Is, What It Isn't, and How to Get Your Life BackFrom EverandRedefining Anxiety: What It Is, What It Isn't, and How to Get Your Life BackRating: 4.5 out of 5 stars4.5/5 (153)
- The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeFrom EverandThe Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeRating: 4.5 out of 5 stars4.5/5 (141)
- The Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeFrom EverandThe Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeRating: 4.5 out of 5 stars4.5/5 (49)
- The Worry Trick: How Your Brain Tricks You into Expecting the Worst and What You Can Do About ItFrom EverandThe Worry Trick: How Your Brain Tricks You into Expecting the Worst and What You Can Do About ItRating: 4.5 out of 5 stars4.5/5 (107)
- The Autoimmune Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against YouFrom EverandThe Autoimmune Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against YouNo ratings yet
- Don't Panic: Taking Control of Anxiety AttacksFrom EverandDon't Panic: Taking Control of Anxiety AttacksRating: 4 out of 5 stars4/5 (12)
- Binaural Beats: Activation of pineal gland – Stress reduction – Meditation – Brainwave entrainment – Deep relaxationFrom EverandBinaural Beats: Activation of pineal gland – Stress reduction – Meditation – Brainwave entrainment – Deep relaxationRating: 5 out of 5 stars5/5 (9)
- Breaking the Chains of Transgenerational Trauma: My Journey from Surviving to ThrivingFrom EverandBreaking the Chains of Transgenerational Trauma: My Journey from Surviving to ThrivingRating: 4.5 out of 5 stars4.5/5 (30)
- Feeling Great: The Revolutionary New Treatment for Depression and AnxietyFrom EverandFeeling Great: The Revolutionary New Treatment for Depression and AnxietyNo ratings yet
- Somatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionFrom EverandSomatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionNo ratings yet
- Happiness Hypothesis, The, by Jonathan Haidt - Book SummaryFrom EverandHappiness Hypothesis, The, by Jonathan Haidt - Book SummaryRating: 4.5 out of 5 stars4.5/5 (95)
- Vagus Nerve: A Complete Self Help Guide to Stimulate and Activate Vagal Tone — A Self Healing Exercises to Reduce Chronic Illness, PTSD, Anxiety, Inflammation, Depression, Trauma, and AngerFrom EverandVagus Nerve: A Complete Self Help Guide to Stimulate and Activate Vagal Tone — A Self Healing Exercises to Reduce Chronic Illness, PTSD, Anxiety, Inflammation, Depression, Trauma, and AngerRating: 4.5 out of 5 stars4.5/5 (16)
- Winning the War in Your Mind: Change Your Thinking, Change Your LifeFrom EverandWinning the War in Your Mind: Change Your Thinking, Change Your LifeRating: 5 out of 5 stars5/5 (561)
- Emotional Detox for Anxiety: 7 Steps to Release Anxiety and Energize JoyFrom EverandEmotional Detox for Anxiety: 7 Steps to Release Anxiety and Energize JoyRating: 5 out of 5 stars5/5 (6)
- The Anatomy of Loneliness: How to Find Your Way Back to ConnectionFrom EverandThe Anatomy of Loneliness: How to Find Your Way Back to ConnectionRating: 4.5 out of 5 stars4.5/5 (163)
- Overcoming Unwanted Intrusive Thoughts: A CBT-Based Guide to Getting Over Frightening, Obsessive, or Disturbing ThoughtsFrom EverandOvercoming Unwanted Intrusive Thoughts: A CBT-Based Guide to Getting Over Frightening, Obsessive, or Disturbing ThoughtsRating: 4.5 out of 5 stars4.5/5 (48)