Professional Documents
Culture Documents
Jamapediatrics Zhu 2022 Oi 220016 1653493555.95451
Jamapediatrics Zhu 2022 Oi 220016 1653493555.95451
Uploaded by
Lucia NiculaeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jamapediatrics Zhu 2022 Oi 220016 1653493555.95451
Jamapediatrics Zhu 2022 Oi 220016 1653493555.95451
Uploaded by
Lucia NiculaeCopyright:
Available Formats
Research
JAMA Pediatrics | Original Investigation | CARING FOR THE CRITICALLY ILL PATIENT
Noninvasive High-Frequency Oscillatory Ventilation vs Nasal Continuous
Positive Airway Pressure vs Nasal Intermittent Positive Pressure
Ventilation as Postextubation Support for Preterm Neonates in China
A Randomized Clinical Trial
Xingwang Zhu, MD; HongBo Qi, MD; Zhichun Feng, MD; Yuan Shi, MD, PhD;
Daniele De Luca, MD, PhD; for the Nasal Oscillation Post-Extubation (NASONE) Study Group
Visual Abstract
IMPORTANCE Several respiratory support techniques are available to minimize the use of Supplemental content
invasive mechanical ventilation (IMV) in preterm neonates. It is unknown whether
noninvasive high-frequency oscillatory ventilation (NHFOV) is more efficacious than nasal
continuous positive airway pressure (NCPAP) or nasal intermittent positive pressure
ventilation (NIPPV) in preterm neonates after their first extubation.
OBJECTIVE To test the hypothesis that NHFOV is more efficacious than NCPAP or NIPPV
in reducing IMV after extubation and until neonatal intensive care unit discharge among
preterm neonates.
DESIGN, SETTING, AND PARTICIPANTS This multicenter, pathophysiology-based,
assessor-blinded, 3-group, randomized clinical trial was conducted in 69 tertiary referral
neonatal intensive care units in China, recruiting participants from December 1, 2017,
to May 31, 2021. Preterm neonates who were between the gestational age of 25 weeks
plus 0 days and 32 weeks plus 6 days and were ready to be extubated were randomized to
receive NCPAP, NIPPV or NHFOV. Data were analyzed on an intention-to-treat basis.
INTERVENTIONS The NCPAP, NIPPV, or NHFOV treatment was initiated after the first
extubation and lasted until discharge.
MAIN OUTCOMES AND MEASURES Primary outcomes were total duration of IMV, need for
reintubation, and ventilator-free days. These outcomes were chosen to describe the effect
of noninvasive ventilation strategy on the general need for IMV.
RESULTS A total of 1440 neonates (mean [SD] age at birth, 29.4 [1.8] weeks; 860 boys
[59.7%]) were included in the trial. Duration of IMV was longer in NIPPV (mean difference,
1.2; 95% CI, 0.01-2.3 days; P = .04) and NCPAP (mean difference, 1.5 days; 95% CI, 0.3-2.7
days; P = .01) compared with NHFOV. Neonates who were treated with NCPAP needed
reintubations more often than those who were treated with NIPPV (risk difference: 8.1%;
95% CI, 2.9%-13.3%; P = .003) and NHFOV (risk difference, 12.5%; 95% CI, 7.5%-17.4%;
P < .001). There were fewer ventilator-free days in neonates treated with NCPAP than in
those treated with NIPPV (median [25th-75th percentile] difference, −3 [−6 to −1] days;
P = .01). There were no differences between secondary efficacy or safety outcomes, except
for the use of postnatal corticosteroids (lower in NHFOV than in NCPAP group; risk difference,
7.3%; 95% CI, 2.6%-12%; P = .002), weekly weight gain (higher in NHFOV than in NCPAP
Author Affiliations: Author
group; mean difference, −0.9 g/d; 95% CI, −1.8 to 0 g/d; P = .04), and duration of study affiliations are listed at the end of this
intervention (shorter in NHFOV than in NIPPV group; median [25th-75th percentile] article.
difference, −1 [−3 to 0] days; P = .01). Group Information: Members of the
NASONE Study Group appear in
CONCLUSIONS AND RELEVANCE Results of this trial indicated that NHFOV, if used after Supplement 3.
extubation and until discharge, slightly reduced the duration of IMV in preterm neonates, Corresponding Author: Yuan Shi,
and both NHFOV and NIPPV resulted in a lower risk of reintubation than NCPAP. MD, PhD, Department of
Neonatology, Children's Hospital of
All 3 respiratory support techniques were equally safe for this patient population.
Chongqing Medical University,
TRIAL REGISTRATION ClinicalTrials.gov Identifier: NCT03181958 Ministry of Education Key Laboratory
of Child Development and Disorders,
Key Laboratory of Pediatrics in
Chongqing, China, No. 136,
Zhongshan 2nd Road, Yuzhong
JAMA Pediatr. 2022;176(6):551-559. doi:10.1001/jamapediatrics.2022.0710 District, Chongqing 401122, China
Published online April 25, 2022. (shiyuan@hospital.cqmu.edu.cn).
(Reprinted) 551
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 07/28/2023
Research Original Investigation NHFOV vs NCPAP vs NIPPV as Postextubation Support in Preterm Neonates
M
any preterm neonates eventually need invasive
m e c h a n i c a l ve nt i l at i o n ( I M V ) d u r i ng t h e i r Key Points
hospitalization.1,2 Invasive mechanical ventilation is
Question What is the best noninvasive ventilation mode to reduce
associated with bronchopulmonary dysplasia (BPD), later neu- postextubation invasive respiratory support in preterm neonates?
rological impairment, and rehospitalization during the first
Findings In this randomized clinical trial of 1440 preterm
year of life. 3-5 To minimize IMV, neonatal intensive care
neonates, noninvasive high-frequency oscillatory ventilation
units (NICUs) use nasal continuous positive airway pressure
(NHFOV) slightly reduced the duration of invasive ventilation.
(NCPAP) and various noninvasive ventilation modes. Both NHFOV and nasal intermittent positive pressure ventilation
Nasal continuous positive airway pressure is a commonly had a lower risk of reintubation than nasal continuous positive
established respiratory support used after extubation, airway pressure.
but many patients do not respond to NCPAP and need
Meaning Findings of this trial indicate that NHFOV and nasal
reintubation.6 Nasal intermittent positive pressure ventila- intermittent positive pressure ventilation in neonates provide a
tion (NIPPV) is a noninvasive ventilation mode that delivers small advantage of reduced need for invasive respiratory support
intermittent peak pressure on positive end-expiratory pres- when used from extubation and until discharge.
sure with a given inspiratory time and frequency.7 Use of
NIPPV reduces the need for IMV more effectively compared
with NCPAP, but does not substantially reduce BPD.8 More- screened the neonates daily for eligibility. Neonates who met
over, NIPPV in neonates is usually unsynchronized given that all of the following conditions were enrolled: (1) gestational age
synchronization is difficult to achieve because of leaks, high between 25 weeks plus 0 days and 32 weeks plus 6 days, (2)
respiratory rate, low tidal volume, and irregular breathing pat- received assistance from any IMV mode, (3) postconcep-
tern. Noninvasive high-frequency oscillatory ventilation tional age younger than 36 weeks, and (4) readiness for first-
(NHFOV) is an unconventional noninvasive ventilation mode time extubation (extubation readiness was described in the pro-
that applies a bias flow to generate a continuous distending tocol [Supplement 1]). Neonates were excluded if they had (1)
pressure with active oscillations that are superimposed on major congenital anomalies or chromosomal abnormalities;
spontaneous tidal breathing.9 Noninvasive high-frequency os- (2) neuromuscular diseases; (3) upper respiratory tract abnor-
cillatory ventilation may be beneficial because it allows a high malities; (4) surgical conditions; (5) grade IV intraventricular
mean airway pressure (Paw) to be reached, theoretically re- hemorrhage occurring before the first extubation; (6) birth
ducing gas trapping with the superimposed oscillations. More- weight of less than 600 g; or (7) suspected congenital lung
over, NHFOV is gaining popularity at least in some countries10 diseases, malformations, or pulmonary hypoplasia.
because of its advantages, such as no need for synchroniza- Race and ethnicity data were not collected. All of the par-
tion, efficiency in carbon dioxide removal, easy alveolar re- ticipants were Chinese newborns.
cruitment, and noninvasive interface.11
Nasal continuous positive airway pressure is the current Randomization and Blinding
standard of care for preterm neonates early in life (that is, be- Between December 1, 2017, and May 31, 2021, neonates were
fore surfactant administration, if any).12,13 Although NCPAP, randomized to receive NCPAP, NIPPV, or NHFOV when extu-
NIPPV, and NHFOV are alternative strategies to ventilate pa- bation was deemed imminent (within 1 hour of the planned
tients later during the NICU stay, it is unclear which ventila- extubation); they were randomized to a study group after the
tion mode should be preferred; thus, a multigroup design is decision to extubate (Figure). Simple centralized randomiza-
appropriate. We conducted a multicenter, pathophysiology- tion was done according to a software-generated random num-
based, assessor-blinded, 3-group, randomized clinical trial ber sequence that was posted on a dedicated and secured
with parallel design to test the hypothesis that NHFOV is website. The website generated the randomization, but the se-
more efficacious than NCPAP or NIPPV in reducing the need quence was concealed from investigators at each of the par-
for IMV after extubation and until NICU discharge among ticipating sites. Neonates who were randomized to 1 group
preterm neonates. could not cross over to the others during the study. In case of
reintubation, when the neonate was reextubated, the same
treatment was provided and managed according to the trial
protocol.14
Methods Because of the nature of the intervention, blinding of the
Study Design and Eligibility Criteria clinicians was impossible and blinding of the neonates made
The trial protocol14 (Supplement 1) was approved by the eth- no sense. However, the outcome assessors were blinded be-
ics committee of the Third Affiliated Hospital of Chongqing cause the outcome data were recorded by investigators who
Military Medical University. Written informed consent was were not working in the NICU and who reviewed patient files
obtained from parents or guardians antenatally or on NICU ad- while blinded for the allocated treatment. An assessor was
mission, and data were treated according to all relevant local nominated for each participating NICU.
regulations. We followed the Consolidated Standards of
Reporting Trials (CONSORT) reporting guideline.15 Devices and Interfaces
A total of 69 tertiary referral NICUs in China participated We used either variable- or continuous-flow devices to pro-
in this randomized clinical trial. Attending neonatologists vide NCPAP. Given that neonatal ventilators rarely offer this
552 JAMA Pediatrics June 2022 Volume 176, Number 6 (Reprinted) jamapediatrics.com
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 07/28/2023
NHFOV vs NCPAP vs NIPPV as Postextubation Support in Preterm Neonates Original Investigation Research
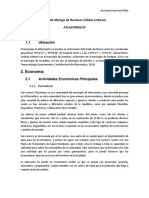
Figure. CONSORT Diagram
1974 Assessed for eligibility
481 Excluded
80 Met at least 1 exclusion criterion
315 Parent(s) refused to participate
86 Hospital transfer before randomization
1493 Randomized
501 Allocated to NCPAP and received 495 Allocated to NIPPV and received 497 Allocated to NHFOV and received
the allocated intervention the allocated intervention the allocated intervention
NCPAP indicates nasal continuous
21 Discontinued NCPAP 15 Discontinued NIPPV 17 Discontinued NHFOV positive airway pressure; NIPPV, nasal
intermittent positive pressure
ventilation; NHFOV, noninvasive
480 Analyzed 480 Analyzed 480 Analyzed
high-frequency oscillatory
ventilation.
option, NIPPV was unsynchronized. Noninvasive high- For all groups, if the maximal parameters were not enough
frequency oscillatory ventilation was provided only with pis- to maintain preductal saturation between 90% and 95%, the
ton or membrane oscillators that were able to produce active FiO2 was gradually increased up to 0.40. Parameters were
expiration. The complete list of devices allowed in the study managed and weaned as described in the trial protocol. A dedi-
is described in the trial protocol (Supplement 1). The NCPAP, cated training program was deployed to disseminate this
NIPPV, and NHFOV were administered through the same management policy to all participating NICUs.14
short binasal prongs because these prongs are more com-
monly used in the participating NICUs and have good me- Cointerventions and Concurrent Monitoring
chanical characteristics.16-18 Prong size was chosen as the best Routine medical care and nursing were not changed solely for
fitting according to the diameter of the nares (the largest ones study purposes apart from the trial intervention. Nonpharma-
that fit the nares without blanching the surrounding tissues) cologic sedation with pacifiers and 33% glucose solutions were
and the manufacturer’s recommendations. Particular care provided when needed; no other sedation was allowed. Vital
(eg, pacifiers and positioning) was taken to reduce leaks. parameters monitoring and point-of-care ultrasonography
were performed, and blood gases were measured in arterial-
Ventilatory Management ized capillary samples or using transcutaneous devices.14 All
Neonates who were randomized to NCPAP were given an ini- other typical NICU procedures and treatments were provided
tial pressure of 5 cm H2O, which can be increased to 8 cm H2O according to shared best clinical practices.
according to oxygenation. Neonates who were randomized to
NIPPV were initially treated with the following parameters: (1) Outcomes
positive end-expiratory pressure of 4 cm H2O, which can be The primary outcomes were (1) total duration of IMV during the
increased to 8 cm H2O according to oxygenation; (2) peak in- NICU stay, (2) need for reintubation (criteria for reintubation
spiratory pressure of 15 cm H2O, which can be increased to 25 were fixed), and (3) ventilator-free days, as defined in the pub-
cm H2O according to chest expansion and PaCO2 levels; (3) fre- lished protocol.14 These 3 primary outcomes were chosen to
quency of 30 breaths per minute, which can be increased to describe the general need for IMV from different points of view.
50 breaths per minute according to chest expansion and PaCO2 Secondary outcomes were represented by several effi-
levels; and (4) inspiratory time set between 0.45 and 0.5 sec- cacy and safety end points, as detailed in the protocol. Nasal
onds according to pressure waveform and leaks evaluation. injury was evaluated with a dedicated score.21 We also ana-
Neonates who were randomized to NHFOV received starting lyzed the duration of the study intervention and supplemen-
treatments with the following parameters: (1) Paw of 10 cm H2O tal oxygen.
and titrated within the 5- to 16-cm H2O range according to
the open lung strategy, similar to invasive high-frequency os- Statistical Analysis
cillatory ventilation targeting a fraction of inspired oxygen A prospective, cohort, nonrandomized pilot study compar-
(FiO2) of 25% to 30%19; (2) inspiratory time of 50%, which was ing postextubation NIPPV and NHFOV in preterm neonates
kept unchanged18; (3) frequency of 10 Hz and titrated within provided data on the duration of IMV.22 This previous study
the 8- to 15-Hz range; and (4) amplitude of 25 cm H2O and ti- showed a decrease in IMV duration of approximately 30%
trated within 25- to 50-cm H2O range. Frequency and ampli- for patients who received NHFOVvs NIPPV, although this
tude were titrated according to PaCO2 levels, rather than on the report was included only in an abstract.22 A randomized trial
magnitude of chest oscillations, because carbon dioxide clear- of NIPPV vs NCPAP showed a similar 30% reduction in IMV
ance also occurs in the upper airway dead space.20 duration.23 Because these previous trials did not have the
jamapediatrics.com (Reprinted) JAMA Pediatrics June 2022 Volume 176, Number 6 553
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 07/28/2023
Research Original Investigation NHFOV vs NCPAP vs NIPPV as Postextubation Support in Preterm Neonates
Table 1. Baseline Characteristics of the Study Population
No. (%)
Characteristic NCPAP group (n = 480) NIPPV group (n = 480) NHFOV group (n = 480)
Gestational age at birth, mean (SD), wk 29.5 (1.7) 29.4 (1.8) 29.4 (1.8)
Neonates between
25 wk + 0 d and 27 wk + 6 d 63 (13.1) 75 (15.6) 80 (16.7)
28 wk + 0 d and 29 wk + 6 d 166 (34.6) 182 (37.9) 152 (31.7)
30 wk + 0 d and 32 wk + 6 d 251 (52.3) 223 (46.5) 248 (51.6)
Birth weight, mean (SD), g 1341 (318.0) 1334 (366.0) 1317 (353.0)
Neonates with birth weight <1000 g 67 (14.0) 82 (17.1) 93 (19.4)
Abbreviations: CRIB II, Clinical Risk
Female sex 208 (43.3) 188 (39.2) 184 (38.3) Index for Babies II; FiO2, fraction of
Male sex 272 (56.7) 292 (60.8) 296 (61.7) inspired oxygen; NCPAP, nasal
SGA neonates 45 (9.4) 42 (8.8) 36 (7.5) continuous positive airway pressure;
NHFOV, noninvasive high-frequency
Twins 132 (27.5) 145 (30.2) 148 (30.8)
oscillatory ventilation; NIPPV, nasal
Cesarean delivery 259 (53.9) 256 (53.3) 260 (54.1) intermittent positive pressure
Prenatal corticosteroid prophylaxisa 207 (43.1) 235 (48.9) 218 (45.4) ventilation; OI, oxygenation index;
CRIB II score, mean (SD)b 5.2 (3.0) 5.2 (3.3) 5.4 (3.2) Paw, mean airway pressure;
5-min Apgar score, median 9 (8-9) 9 (8-9) 9 (8-9) SGA, small for gestational age.
(25th-75th percentile) a
Prenatal corticosteroid was
Surfactant replacementc 408 (85.0) 417 (86.9) 404 (84.1) considered if complete (two 12-mg
Early-onset sepsis 13 (2.7) 13 (2.7) 11 (2.3) doses of betamethasone, 24 hours
apart from each other).
Postnatal age at first extubation, 3 (2-6) 4 (2-7) 3 (2-7)
b
median (25th-75th percentile), d CRIB-II, pH, and OI
Before extubation, mean (SD) (OI = [FiO2 × Paw] × 100/PaO2)
OIb 3.5 (4.1) 3.6 (2.2) 3.8 (2.7) were dimensionless variables.
c
pHb 7.37 (0.10) 7.36 (0.35) 7.35 (0.29) Surfactant replacement was always
performed by intubation-
PaCO2, mm Hg 37.9 (10.6) 37.8 (10.4) 38.7 (10.4)
surfactant-extubation technique.
same design as the present trial, we were cautious and parents or guardians withdrew their consent for participa-
aimed at a difference of 20% in the reduction of IMV dura- tion; these patients received routine clinical care, and their trial
tion. Considering a mean (SD) IMV duration of 10 (8.5) days, data were destroyed.14 As a result, 1440 neonates were ana-
which was derived from the aforementioned studies, α = .05 lyzed (Figure). These neonates had a mean (SD) age at birth of
(with a Bonferroni correction for multiple comparisons of 29.4 (1.8) weeks and included 580 girls (40.3%) and 860 boys
0.017), and β = 95%, we enrolled 480 neonates in each (59.7%). The 3 groups (NCPAP, NIPPV, and NHFOV) were bal-
group with a 1:1:1 ratio. Thus, a total of at least 1440 neo- anced in terms of basic characteristics (Table 1). The interim
nates had to be enrolled. An interim analysis was previewed analysis did not reveal any safety problem. The trial was com-
at greater than 50% enrollment (and was realized after the pleted without any particular adverse event, need for discon-
trial protocol publication), analyzing safety data and quality tinuation, or protocol modification. eTable 1 in Supplement 2
indicators. describes the devices used in the trial.
Outcomes were analyzed on an intention-to-treat basis.
We calculated a risk difference (with 95% CI) for dichoto- Primary Outcomes
mous outcomes and mean (with 95% CI) or median (25th- The total duration of IMV was different between the study
75th percentile, using Hodges-Lehmann) differences for con- groups. Duration of IMV was longer in the NIPPV (mean dif-
tinuous outcomes between the study groups. We conducted ference, 1.2; 95% CI, 0.01-2.3 days; P = .04) and NCPAP (mean
χ2 tests to compare dichotomous outcomes and parametric difference, 1.5 days; 95% CI, 0.3-2.7 days; P = .01) groups than
(using 1-way analysis of variance, followed by Sidak post hoc in the NHFOV group, whereas no significant difference was ob-
test if needed) or nonparametric tests (Mann-Whitney test, served between the NIPPV and NCPAP groups (Table 2). The
followed by Conover-Iman post hoc test if needed) as appro- frequency rates of reintubation and reintubation within 48
priate to compare continuous outcomes. Reintubations over- hours from extubation were different between the study groups
time were also analyzed with Kaplan-Meier curves and con- and significantly higher in the NCPAP group vs the NHFOV
trasted with a log-rank test. Two-sided P < .05 was considered group (risk difference, 12.5%; 95% CI, 7.5%-17.4%; P < .001) and
to be statistically significant. Analyses were performed with vs the NIPPV group (risk difference: 8.1%; 95% CI, 2.9%-
SPSS, version 16 (IBM). 13.3%; P = .003), although no difference was observed be-
tween the NIPPV and NHFOV groups (Table 2). These results
were confirmed by Kaplan-Meier analysis, whose curves were
significantly different (eFigure in Supplement 2).
Results The reasons for reintubation were similar between the
A total of 1493 neonates underwent randomization. The allo- study groups (eTable 2 in Supplement 2). Ventilator-free days
cated treatment was interrupted in 53 neonates because their differed between the study groups and were significantly fewer
554 JAMA Pediatrics June 2022 Volume 176, Number 6 (Reprinted) jamapediatrics.com
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 07/28/2023
NHFOV vs NCPAP vs NIPPV as Postextubation Support in Preterm Neonates Original Investigation Research
Table 2. Primary Outcome Results
No. (%) NCPAP vs NIPPV NCPAP vs NHFOV NIPPV vs NHFOV
NCPAP group NIPPV group NHFOV group Post hoc Post hoc Post hoc
Outcome (n = 480) (n = 480) (n = 480) Difference P value Difference P value Difference P value
Total duration 7.8 (7.2) 7.3 (9.2) 6.2 (5.7) Mean .75 Mean (95% CI): .01 Mean .04
of IMV, (95% CI): 0.44 1.5 (0.3 to 2.7) (95% CI): 1.2
mean (SD), d (−0.7 to 1.6) (0.01 to 2.3)
Reintubations, % 123 (25.6) 84 (17.5) 63 (13.1) Risk (95% CI): .003 Risk (95% CI): <.001 Risk (95% CI): .07
8.1 (2.9 to 12.5 (7.5 to 4.4 (0.2 to
13.3) 17.4) 8.9)
Reintubations 97 (20.2) 55 (11.4) 43 (8.9) Risk (95% CI): <.001 Risk (95% CI): <.001 Risk (95% CI): .20
within 48 h, % 8.7 (4.1 to 11.2 (6.8 to 2.5 (−1.3 to
13.3) 15.7) 6.4)
Ventilator-free days, 32 (20 to 45) 35 (21 to 52) 34 (17 to 52) Median .01 Median .62 Median .08
median (25th-75th (25th-75th (25th-75th (25th-75th
percentile) percentile): −3 percentile): −2 percentile): 1
(−6 to −1) (−3 to 2) (0 to 5)
Abbreviations: IMV, invasive mechanical ventilation; NCPAP, nasal continuous positive airway pressure; NHFOV, noninvasive high-frequency oscillatory ventilation;
NIPPV, nasal intermittent positive pressure ventilation.
Table 3. Secondary Efficacy Outcomes
No. (%) NCPAP vs NIPPV NCPAP vs NHFOV NIPPV vs NHFOV
NIPPV
NCPAP group group NHFOV group Post hoc Post hoc Post hoc
Outcome (n = 480) (n = 480) (n = 480) Difference P value Difference P value Difference P value
BPD 184 (38.3) 182 (37.9) 163 (34) Risk (95% CI): .89 Risk (95% CI): .16 Risk (95% CI): .20
0.4 (−5.7 to 6.5) 4.3 (−1.7 to 3.9 (−2.1 to 10)
10.4)
Moderate-to-severe 75 (15.6) 66 (13.8) 52 (10.8) Risk (95% CI): .38 Risk (95% CI): .09 Risk (95% CI): .39
BPDa 4.5 (−5.4 to 8.9 (−1.3 to 4.4 (−5.6 to
14.3) 18.7) 14.2)
Postnatal 98 (20.4) 77 (16.0) 63 (13.1) Risk (95% CI): .08 Risk (95% CI): .002 Risk (95% CI): .20
corticosteroidsb 4.4 (−0.5 to 9.2) 7.3 (2.6 to 12) 2.9 (−1.6 to 7.4)
In-hospital mortality 5 (1.0) 4 (0.8) 8 (1.7) Risk (95% CI): .74 Risk (95% CI): .40 Risk (95% CI): .25
0.2 (−1.2 to 1.7) −0.7 (−1 to 2.3) −0.9 (−0.7 to
2.5)
BPD/mortalityc 189 (39.4) 186 (38.8) 171 (35.6) Risk (95% CI): .84 Risk (95% CI): .23 Risk (95% CI): .32
0.6 (−5.5 to 6.8) 3.8 (−2.4 to 9.8) 3.2 (−3.0 to 9.2)
Duration of allocated 12 (6 to 12 (6 to 10 (5 to 18) Median .29 Median .10 Median .01
intervention, median 20) 22) (25th-75th (25th-75th (25th-75th
(25th-75th percentile): −1 percentile): 1 percentile): −1
percentile), dd (−2 to 1) (0 to 2) (−3 to 0)
Duration of 25 (14 to 24 (12 to 22 (11 to 37) Median .78 Median .10 Median .18
supplemental oxygen, 39) 37) (25th-75th (25th-75th (25th-75th
median (25th-75th percentile): 1 percentile): 3 percentile): 2
percentile), d (−2 to 2) (0 to 4) (−1 to 4)
Abbreviations: BPD, bronchopulmonary dysplasia; NCPAP, nasal continuous administration is known to be harmful. Use of postnatal corticosteroids and
positive airway pressure; NHFOV, noninvasive high-frequency oscillatory the diagnosis of BPD were reported among survivors and until hospital
ventilation; NIPPV, nasal intermittent positive pressure ventilation. discharge.
a c
Severity of BPD was classified according to the 2001 definition from the BPD/mortality was the composite end point represented by BPD development
National Institute of Child Health and Human Development. or in-hospital mortality.
b d
Postnatal corticosteroids were given after the study intervention (ie, after Duration of allocated intervention was the duration of treatment with NCPAP,
extubation) and always after the first week of age, as earlier corticosteroid NIPPV, or NHFOV.
in the NCPAP group than in the NIPPV group (median [25th- P = .002), whereas the duration of the study intervention
75th percentile] difference, −3 [−6 to −1] days; P = .01) (Table 2). was shorter in the NHFOV group than in the NIPPV group
In addition, NHFOV provided better oxygenation after extu- (median [25th-75th percentile] difference, −1 [−3 to 0] days;
bation (eTable 3 in Supplement 2). P = .01) (Table 3).
Similarly, the study groups did not differ significantly in
Secondary Outcomes secondary safety outcomes, except for weekly weight gain,
Secondary efficacy outcomes did not differ significantly which was higher in neonates who were treated with NHFOV
between the study groups, except for postnatal corticoste- than those who received NCPAP (mean difference, −0.9 g/d;
roids and the duration of study intervention. Postnatal corti- 95% CI, −1.8 to 0 g/d; P = .04) (Table 4). Secondary extrapul-
costeroids were used less in the NHFOV group than in the monary outcomes were also similar among the 3 groups
NCPAP group (risk difference, 7.3%; 95% CI, 2.6%-12%; (eTable 4 in Supplement 2).
jamapediatrics.com (Reprinted) JAMA Pediatrics June 2022 Volume 176, Number 6 555
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 07/28/2023
Research Original Investigation NHFOV vs NCPAP vs NIPPV as Postextubation Support in Preterm Neonates
Table 4. Secondary Safety Outcomes
Mean (SD) NCPAP vs NIPPV NCPAP vs NHFOV NIPPV vs NHFOV
NHFOV
NCPAP group NIPPV group group Post hoc Post hoc Post hoc
Outcome (n = 480) (n = 480) (n = 480) Differencea P value Differencea P value Differencea P value
Air leaks, 4 (0.8) 9 (1.9) 3 (0.6) Risk (95% CI): .16 Risk (95% CI): 0.2 .70 Risk (95% CI): .08
No. (%)b −1.1 (−0.5 to 2.8) (−1.1 to 1.6) 1.3 (−0.2 to
2.9)
Weekly weight 12 (4) 12 (6) 13 (5) Mean (95% CI): .81 Mean (95% CI): .04 Mean (95% CI): .25
gain, g/d −0.3 (−1.2 to 0.6) −0.9 (−1.8 to 0) −0.6 (−1.5 to
0.3)
Apnea (No./wk) 5 (4) 4 (4) 4 (4) Mean (95% CI): .29 Mean (95% CI): .13 Mean (95% CI): .97
0.5 (−0.2 to 1.2) 0.6 (−0.1 to 1.3) 0.1 (−0.6 to
0.9)
Nasal injury 0 (0-1) 0 0 (0-1) Median .61 Median .40 Median .17
score, median (25th-75th (25th-75th (25th-75th
(25th-75th percentile): 0 percentile): 0 percentile): 0
percentile), dc
Grade III-IV nasal 17 (3.5) 17 (3.5) 23 (4.8) Risk (95% CI): 0 >.99 Risk (95% CI): .33 Risk (95% CI): .33
injury, No. (%) (−2.4 to 2.4) −1.2 (−1.3 to 3.9) −1.2 (−1.3 to
3.9)
PIPP scored 7.5 (1.9) 7.6 (2.0) 7.4 (2.0) Risk (95% CI): .38 Risk (95% CI): 0.1 .63 Risk (95% CI): .19
−0.1 (−0.4 to 0.2) (−0.2 to 0.4) 0.2 (−0.1 to
0.5)
Abbreviations: NCPAP, nasal continuous positive airway pressure; median score and as number of grade III-IV lesions.
NHFOV, noninvasive high-frequency oscillatory ventilation; NIPPV, nasal d
PIPP score was calculated in the first 48 hours from the study intervention.
intermittent positive pressure ventilation; PIPP, Premature Infant Pain Profile. Both nasal skin injury and PIPP score were dimensionless values.
a
All outcomes were considered among survivors and until hospital discharge. Data were not available for 90 infants in the CPAP (continuous positive airway
b
Air leaks were considered if they occurred after the study intervention. pressure) group, 90 infants in the NIPPV group, and 143 infants in the NHFOV
c
group.
Nasal injury was evaluated with a dedicated score21 and reported both as
did not reach statistical significance. These differences in the
Discussion use of invasive support may seem small (approximately 1-1.5
fewer days of IMV, and approximately −12% of reintubations),
To our knowledge, this was the first large trial in preterm neo- but every additional day of IMV27 and each reintubation28 has
nates that compared NCPAP, NIPPV, and NHFOV as respira- been associated with adverse outcomes, although these data
tory support after extubation until NICU discharge without any were produced in younger preterm populations.
change of ventilatory policy. Neonates who were supported The critical level of IMV duration that significantly in-
with NHFOV had a slightly shorter duration of IMV than those creases the risk of adverse respiratory outcome remains un-
supported with NIPPV and NCPAP. Moreover, NHFOV and clear given that this threshold may be longer4 than the ben-
NIPPV resulted in lower risk of reintubation compared with efit provided by NHFOV. The less frequent early reintubations
NCPAP, whereas there were significantly more ventilator- and the better postextubation gas exchange that were ob-
free days with NIPPV than NCPAP. served with NHFOV suggest that NHFOV might reduce extu-
These results are novel and may help in choosing the re- bation failure primarily because of the respiratory disorder
spiratory support strategy for preterm neonates after extuba- while the reasons for reintubations are similar across the 3
tion until their NICU discharge. This area is complex, and groups. This finding may be explained by the interaction be-
many strategies are possible; therefore, a multigroup study de- tween worsening respiratory failure requiring reintubation
sign was suitable to allow a quicker and more effective and some factors, such as lower gestational age and greater
investigation.24 We believe the findings expand the current respiratory severity before extubation, that need to be inves-
knowledge, particularly on NHFOV, which was previously tigated in subgroup analyses.
investigated only in retrospective studies25,26 and small trials; Reducing IMV could be helpful in decreasing BPD preva-
these past studies suggested the possible benefits of NHFOV, lence. Invasive mechanical ventilation is a proinflammatory
as also reported in a recent meta-analysis.9 trigger that contributes to BPD development,29 whereas rein-
We found that NHFOV had some advantages over NCPAP tubation is associated with the occurrence of ventilator-
and NIPPV in that it reduced the use of invasive respiratory sup- associated pneumonia, which also increases BPD risk.30 None-
port as globally evaluated by the primary outcomes. With theless, BPD is a complex multifactorial, pathobiological
NHFOV, IMV duration decreased by approximately 20% com- process and can be diagnosed in preterm infants who have
pared with NCPAP and by approximately 15% compared with never been treated with invasive ventilation.31 Thus, we did
NIPPV. Consistently, reintubations in NHFOV-treated neo- not find any difference in BPD prevalence between the 3
nates were significantly less frequent than in neonates who re- groups, but we did find less need for postnatal corticoste-
ceived NCPAP. Reintubations and ventilator-free days also roids in the NHFOV group. These observations must be inter-
tended to favor NHFOV over NIPPV, although these results preted cautiously and warrant future explanatory trials or
556 JAMA Pediatrics June 2022 Volume 176, Number 6 (Reprinted) jamapediatrics.com
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 07/28/2023
NHFOV vs NCPAP vs NIPPV as Postextubation Support in Preterm Neonates Original Investigation Research
subgroup analyses.32 Such studies should examine whether safe, and comfort with these modes was similar across the
NHFOV is the best choice for neonates with evolving BPD as- study groups. This finding is important for NHFOV because it
sociated with lung inflammation that is induced or aggra- was the most recent technique and was based on high Paw, and
vated by IMV. As for other complex syndromes,33 it is un- amplitude could theoretically have resulted in air leaks, na-
likely that one solution would fit all, and NHFOV could be sal trauma, or discomfort. Thus, the findings were consistent
useful for a more personalized approach for these patients after with those of a recent cross-sectional study that reported
adequate training is provided. Together with the reduced NHFOV provided good patient comfort, which was not ad-
duration of study intervention in the NHFOV group, this is- versely affected by increasing Paw.38 These results were also
sue requires dedicated studies with pharmacoeconomic consistent with those of previously published smaller trials in-
analysis to ascertain whether wide implementation of NHFOV vestigating the use of NHFOV for shorter times.9
is suitable. These findings should be compared with those of trials ex-
The trial design was based on pathophysiological prin- amining postextubation NHFOV.39-41 In a smaller trial involv-
ciples to guide respiratory support, and the results may be ex- ing a more mature population, NHFOV did not reduce reintu-
plained in the context of the ventilatory strategy. In the NHFOV bations, but a pattern of less feeding intolerance was reported.39
group, Paw was started at the optimal level for the postsur- In the present trial, NHFOV was not used according to a patho-
factant phase.19 We kept a 2- to 3-cm H2O difference in initial physiologically driven strategy; thus, NIPPV and NHFOV were
Paw between the study groups, and Paw was further titrated set at the same Paw, and NHFOV provided only small
to provide better alveolar recruitment with NIPPV and NHFOV amplitudes.39 Chen et al40 found fewer reintubations in a
than with NCPAP. Other parameters were managed according patient population whose age was similar to the population in
to bench and physiological data to optimize carbon dioxide the trial by Seth et al39 but who had mixed severity because
clearance, which, during NHFOV, seemed to occur not only in the population also included infants who were recovering from
the alveoli.20,34 It was difficult to distinguish between the prop- acute respiratory distress syndrome.40 The benefit of NHFOV
erties of the examined ventilation modes and the different was more evident in smaller and sicker infants.40 In a small
ventilatory settings given that these settings were purposely single-center trial with a design and population that were analo-
decided based on the mechanical properties of the ventila- gous to those in the present trial, Li et al41 reported results that
tory mode. It would have been difficult to increase the NCPAP were similar to our findings. In addition, a meta-analysis of
level without any superimposed ventilation because doing so trials of NHFOV as the primary respiratory support in neo-
might theoretically induce gas trapping.11 Previous trials have nates with respiratory distress syndrome showed fewer intu-
compared ventilatory techniques at equal Paw but, unsurpris- bations compared with NCPAP.42 These observations suggest
ingly, have not reported any advantage because similar low- that an NHFOV strategy that is based on higher Paw might
pressure levels provided similar alveolar recruitment.9 This reduce IMV, particularly in neonates with younger gesta-
situation is a main problem as it prevents the full realization tional age or who are recovering from more severe respira-
of the potential of NIPPV and NHFOV.35 Conversely, data have tory failure. These results could be different if NHFOV were
shown that noninvasive respiratory support with high Paw of- applied with other interfaces and pressures or if devices that
ten prevents reintubation but have suggested that neonates did not provide active oscillations were used. These issues
treated with high NCPAP rather than with a noninvasive ven- require further specific studies to clarify the best way to
tilation technique often need an alternate mode of noninva- apply NHFOV.
sive support.36,37 These data support the findings of the pre-
sent trial, but the small outcome differences and similar Strengths and Limitations
maximum Paw between NIPPV and NHFOV groups suggest that This study has some strengths. The trial used a large popula-
increasing Paw is the crucial point. It remains unclear whether tion and rigorous design, including physiologically targeted
applying NIPPV with higher pressure is safer and more suit- ventilatory management that tried to mimic, whenever pos-
able than using NHFOV and how to address the need for syn- sible, the high-quality design of pharmacological trials. More-
chronization during NIPPV. over, the trial received national public funding43 and was
We chose the 3 primary outcomes to describe the global conducted with advice from a large network of international
burden of care associated with IMV. Although the interven- experts who received specific training and shared basic clini-
tions in the trial can directly change the need for reintuba- cal practices.
tion, they may only indirectly affect the total duration of IMV This study also has some limitations. The blinding pro-
because this duration may be influenced by several factors. cess was imperfect because of the type of intervention. We ad-
However, we reduced this influence because the extubation dressed this limitation by using prespecified outcome defini-
and reintubation criteria were dictated, and the same inter- tions and blinding the assessors, although this solution did not
vention was maintained during the trial.14 completely eliminate the problem. We did not provide higher
We did not find significant differences in other second- NCPAP levels because of the risk of gas trapping. Moreover,
ary efficacy outcomes. However, these outcomes included European guidelines do not recommend these higher levels,13
complex multifactorial end points, such as BPD and mortal- and they are not the standard of care in Chinese NICUs. Syn-
ity, which may be influenced by many concurrent factors and chronized NIPPV might have led to better results, but synchro-
for which the trial was likely underpowered. Secondary safety nization during noninvasive ventilation is unavailable in most
outcome analysis showed that the 3 techniques were equally neonatal ventilators; thus, synchronization remains to be
jamapediatrics.com (Reprinted) JAMA Pediatrics June 2022 Volume 176, Number 6 557
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 07/28/2023
Research Original Investigation NHFOV vs NCPAP vs NIPPV as Postextubation Support in Preterm Neonates
studied in dedicated trials using specific devices. It is un- neonates who received more common corticosteroid prophy-
known to what extent these results can be generalized to popu- laxis. The former information can be obtained by planned
lations with different genetic backgrounds. This trial should subgroup analyses of the data set, and the latter will need dedi-
be considered a pragmatic trial that recruited neonates who cated trials in different settings.
might have been reintubated for several reasons; explana-
tory trials may be conducted in subgroups identified from the
findings of this trial. For instance, we enrolled a population of
very preterm neonates who received relatively uncommon
Conclusions
prenatal corticosteroids. Very small neonates were excluded This randomized clinical trial found that NHFOV, if used
from the study because their resuscitation depended on par- after extubation and until the NICU discharge, slightly re-
ents’ wishes and resuscitation was not constantly provided in duced the duration of IMV in preterm neonates, whereas both
Chinese NICUs. It remains to be determined whether the re- NHFOV and NIPPV had a lower risk of reintubation than NCPAP.
sults would be the same at younger gestational age or among These 3 respiratory support techniques were equally safe.
ARTICLE INFORMATION approval of the manuscript; and decision to submit (NIPPV) versus nasal continuous positive airway
Accepted for Publication: January 12, 2022. the manuscript for publication. pressure (NCPAP) for preterm neonates after
Group Information: NASONE Study Group extubation. Cochrane Database Syst Rev. 2017;2(2):
Published Online: April 25, 2022. CD003212. doi:10.1002/14651858.CD003212.pub3
doi:10.1001/jamapediatrics.2022.0710 members and centers are listed in Supplement 3.
Data Sharing Statement: See Supplement 4. 9. De Luca D, Centorrino R. Nasal high-frequency
Author Affiliations: Children's Hospital of ventilation. Clin Perinatol. 2021;48(4):761-782.
Chongqing Medical University, Ministry of Additional Contributions: We thank the families of doi:10.1016/j.clp.2021.07.006
Education Key Laboratory of Child Development all infants who participated in the study and the
and Disorders, Key Laboratory of Pediatrics, staff members who cared for them. 10. Fischer HS, Bohlin K, Bührer C, et al.
Chongqing, China (Zhu, Shi); First Affiliated Nasal high-frequency oscillation ventilation in
Hospital of Chongqing Medical University, REFERENCES neonates: a survey in five European countries.
Chongqing, China (Qi); Affiliated BaYi Children’s Eur J Pediatr. 2015;174(4):465-471. doi:10.1007/
1. Stefanescu BM, Murphy WP, Hansell BJ, s00431-014-2419-y
Hospital, People's Liberation Army General Fuloria M, Morgan TM, Aschner JL. A randomized,
Hospital, Beijing, China (Feng); Division of controlled trial comparing two different continuous 11. De Luca D, Dell’Orto V. Non-invasive
Pediatrics and Neonatal Critical Care, Assistance positive airway pressure systems for the successful high-frequency oscillatory ventilation in neonates:
Publique–Hôpitaux de Paris, Paris-Saclay University extubation of extremely low birth weight infants. review of physiology, biology and clinical data. Arch
Hospitals, Medical Centre A. Béclère, Paris, France Pediatrics. 2003;112(5):1031-1038. doi:10.1542/peds. Dis Child Fetal Neonatal Ed. 2016;101(6):F565-F570.
(De Luca); Physiopathology and Therapeutic 112.5.1031 doi:10.1136/archdischild-2016-310664
Innovation, Institut National de la Santé et de la 12. Polin RA, Carlo WA; Committee on Fetus and
Recherche Médicale U999 Unit, Paris Saclay 2. Barrington KJ, Bull D, Finer NN. Randomized trial
of nasal synchronized intermittent mandatory Newborn; American Academy of Pediatrics.
University, Paris, France (De Luca). Surfactant replacement therapy for preterm and
ventilation compared with continuous positive
Author Contributions: Prof Shi had full access to all airway pressure after extubation of very low birth term neonates with respiratory distress. Pediatrics.
of the data in the study and takes responsibility for weight infants. Pediatrics. 2001;107(4):638-641. 2014;133(1):156-163. doi:10.1542/peds.2013-3443
the integrity of the data and the accuracy of the doi:10.1542/peds.107.4.638 13. Sweet DG, Carnielli V, Greisen G, et al.
data analysis. Drs Zhu, Qi, and Feng contributed European consensus guidelines on the
equally as co–first authors. Profs Shi and De Luca 3. Chien YH, Tsao PN, Chou HC, Tang JR, Tsou KI.
Rehospitalization of extremely-low-birth-weight management of respiratory distress syndrome -
contributed equally as co–last authors. 2019 update. Neonatology. 2019;115(4):432-450.
Concept and design: Zhu, Shi, De Luca. infants in first 2 years of life. Early Hum Dev. 2002;
66(1):33-40. doi:10.1016/S0378-3782(01)00233-X doi:10.1159/000499361
Acquisition, analysis, or interpretation of data:
Zhu, Qi, Feng, Shi. 4. Jensen EA, DeMauro SB, Kornhauser M, Aghai ZH, 14. Shi Y, De Luca D; NASal OscillatioN
Drafting of the manuscript: Zhu, Shi, De Luca. Greenspan JS, Dysart KC. Effects of multiple ventilation post-Extubation (NASONE) study group.
Critical revision of the manuscript for important courses and duration of mechanical ventilation on Continuous positive airway pressure (CPAP) vs
intellectual content: All authors. respiratory outcomes in extremely low-birth-weight noninvasive positive pressure ventilation (NIPPV)
Statistical analysis: Zhu, Shi. infants. JAMA Pediatr. 2015;169(11):1011-1017. vs noninvasive high frequency oscillation
Obtained funding: Shi. doi:10.1001/jamapediatrics.2015.2401 ventilation (NHFOV) as post-extubation support in
Administrative, technical, or material support: preterm neonates: protocol for an
5. Vliegenthart RJS, Onland W, assessor-blinded, multicenter, randomized
Zhu, Shi. van Wassenaer-Leemhuis AG, De Jaegere APM,
Supervision: Qi, Feng, Shi, De Luca. controlled trial. BMC Pediatr. 2019;19(1):256.
Aarnoudse-Moens CSH, van Kaam AH. doi:10.1186/s12887-019-1625-1
Other - instruction on the used technique: De Luca. Restricted ventilation associated with reduced
Conflict of Interest Disclosures: Prof De Luca neurodevelopmental impairment in preterm 15. Schulz KF, Altman DG, Moher D; CONSORT
reported receiving grants, personal fees, and infants. Neonatology. 2017;112(2):172-179. doi:10. Group. CONSORT 2010 statement: updated
nonfinancial support from Vyaire Medical Inc; 1159/000471841 guidelines for reporting parallel group randomised
personal fees from Getinge; and personal fees from trials. Trials. 2010;11:32. doi:10.1186/1745-6215-11-32
6. Meneses J, Bhandari V, Alves JG, Herrmann D.
Philips outside the submitted work. No other Noninvasive ventilation for respiratory distress 16. De Paoli AG, Davis PG, Faber B, Morley CJ.
disclosures were reported. syndrome: a randomized controlled trial. Pediatrics. Devices and pressure sources for administration of
Funding/Support: The trial was funded by grant 2011;127(2):300-307. doi:10.1542/peds.2010-0922 nasal continuous positive airway pressure (NCPAP)
cstc2016shms-ztzx13001 from the Scientific in preterm neonates. Cochrane Database Syst Rev.
7. Owen LS, Manley BJ. Nasal intermittent positive 2008;1(1):CD002977.
Research Projects Unit of Chongqing Medical pressure ventilation in preterm infants: equipment,
University. evidence, and synchronization. Semin Fetal 17. De Luca D, Carnielli VP, Conti G, Piastra M.
Role of the Funder/Sponsor: The funder had no Neonatal Med. 2016;21(3):146-153. doi:10.1016/j. Noninvasive high frequency oscillatory ventilation
role in the design and conduct of the study; siny.2016.01.003 through nasal prongs: bench evaluation of efficacy
collection, management, analysis, and and mechanics. Intensive Care Med. 2010;36(12):
8. Lemyre B, Davis PG, De Paoli AG, Kirpalani H. 2094-2100. doi:10.1007/s00134-010-2054-7
interpretation of the data; preparation, review, or Nasal intermittent positive pressure ventilation
558 JAMA Pediatrics June 2022 Volume 176, Number 6 (Reprinted) jamapediatrics.com
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 07/28/2023
NHFOV vs NCPAP vs NIPPV as Postextubation Support in Preterm Neonates Original Investigation Research
18. De Luca D, Piastra M, Pietrini D, Conti G. Effect a retrospective chart review. Am J Perinatol. 2020. simple trials neglecting complex respiratory
of amplitude and inspiratory time in a bench model doi:10.1055/s-0040-1718738 physiology. J Perinatol. 2017;37(9):1065-1066.
of non-invasive HFOV through nasal prongs. Pediatr 27. Walsh MC, Morris BH, Wrage LA, et al; National doi:10.1038/jp.2017.84
Pulmonol. 2012;47(10):1012-1018. doi:10.1002/ Institutes of Child Health and Human Development 36. Binmanee A, El Helou S, Shivananda S, Fusch C,
ppul.22511 Neonatal Research Network. Extremely low Mukerji A. Use of high noninvasive respiratory
19. De Jaegere A, van Veenendaal MB, Michiels A, birthweight neonates with protracted ventilation: support pressures in preterm neonates:
van Kaam AH. Lung recruitment using oxygenation mortality and 18-month neurodevelopmental a single-center experience. J Matern Fetal Neonatal
during open lung high-frequency ventilation in outcomes. J Pediatr. 2005;146(6):798-804. Med. 2017;30(23):2838-2843. doi:10.1080/
preterm infants. Am J Respir Crit Care Med. 2006; doi:10.1016/j.jpeds.2005.01.047 14767058.2016.1265931
174(6):639-645. doi:10.1164/rccm.200603-351OC 28. Shalish W, Kanbar L, Kovacs L, et al. The impact 37. Ahmad HA, Deekonda V, Patel W, Thabane L,
20. Mukerji A, Finelli M, Belik J. Nasal of time interval between extubation and Shah PS, Mukerji A. Comparison of high CPAP
high-frequency oscillation for lung carbon dioxide reintubation on death or bronchopulmonary versus NIPPV in preterm neonates: a retrospective
clearance in the newborn. Neonatology. 2013;103 dysplasia in extremely preterm infants. J Pediatr. cohort study. Am J Perinatol. 2021. doi:10.1055/s-
(3):161-165. doi:10.1159/000345613 2019;205:70-76.e2. doi:10.1016/j.jpeds.2018.09.062 0041-1727159
21. Fischer C, Bertelle V, Hohlfeld J, Forcada-Guex M, 29. De Luca D, Shankar-Aguilera S, Centorrino R, 38. Centorrino R, Loi B, De Luca D. Extremely
Stadelmann-Diaw C, Tolsa JF. Nasal trauma due to Fortas F, Yousef N, Carnielli VP. Less invasive preterm infants experienced good comfort with
continuous positive airway pressure in neonates. surfactant administration: a word of caution. Lancet various nasal respiratory support techniques
Arch Dis Child Fetal Neonatal Ed. 2010;95(6): Child Adolesc Health. 2020;4(4):331-340. doi:10. delivered with masks. Acta Paediatr. 2021;110(10):
F447-F451. doi:10.1136/adc.2009.179416 1016/S2352-4642(19)30405-5 2753-2755. doi:10.1111/apa.15907
22. Dell’Orto V, Centorrino R, Shankar-Aguilera S, 30. Dell’Orto V, Raschetti R, Centorrino R, et al. 39. Seth S, Saha B, Saha AK, Mukherjee S, Hazra A.
et al. Noninvasive high frequency oscillatory Short- and long-term respiratory outcomes in Nasal HFOV versus nasal IPPV as a post-extubation
ventilation versus noninvasive intermittent positive neonates with ventilator-associated pneumonia. respiratory support in preterm infants—a randomised
pressure ventilation for preterm babies developing Pediatr Pulmonol. 2019;54(12):1982-1988. doi:10. controlled trial. Eur J Pediatr. 2021;180(10):3151-3160.
BPD: a pilot study. Abstract presented at: the 2018 1002/ppul.24487 doi:10.1007/s00431-021-04084-1
Pediatric Academic Societies Meeting; May 5-8, 31. Nobile S, Marchionni P, Gidiucci C, et al; 40. Chen L, Wang L, Ma J, Feng Z, Li J, Shi Y.
Toronto, Canada. Accessed March 21, 2022. https:// Marche Neonatal Network. Oxygen saturation/FIO2 Nasal high-frequency oscillatory ventilation in
www.xcdsystem.com/pas/program/2018/index. ratio at 36 weeks’ PMA in 1005 preterm infants: preterm infants with respiratory distress syndrome
cfm?pgid=156 effect of gestational age and early respiratory and ARDS after extubation: a randomized
23. Ramanathan R, Sekar KC, Rasmussen M, disease patterns. Pediatr Pulmonol. 2019;54(5): controlled trial. Chest. 2019;155(4):740-748.
Bhatia J, Soll RF. Nasal intermittent positive 637-643. doi:10.1002/ppul.24265 doi:10.1016/j.chest.2019.01.014
pressure ventilation after surfactant treatment for 32. Thorpe KE, Zwarenstein M, Oxman AD, et al. 41. Li Y, Wei Q, Zhao D, et al. Non-invasive
respiratory distress syndrome in preterm infants A pragmatic-explanatory continuum indicator high-frequency oscillatory ventilation in preterm
<30 weeks’ gestation: a randomized, controlled summary (PRECIS): a tool to help trial designers. infants after extubation: a randomized, controlled
trial. J Perinatol. 2012;32(5):336-343. doi:10.1038/ J Clin Epidemiol. 2009;62(5):464-475. doi:10.1016/ trial. J Int Med Res. 2021;49(2):300060520984915.
jp.2012.1 j.jclinepi.2008.12.011 doi:10.1177/0300060520984915
24. Parmar MK, Carpenter J, Sydes MR. 33. De Luca D, Harrison DA, Peters MJ. ‘Lumping or 42. Li J, Chen L, Shi Y. Nasal high-frequency
More multiarm randomised trials of superiority are splitting’ in paediatric acute respiratory distress oscillatory ventilation versus nasal continuous
needed. Lancet. 2014;384(9940):283-284. syndrome (PARDS). Intensive Care Med. 2018;44 positive airway pressure as primary respiratory
doi:10.1016/S0140-6736(14)61122-3 (9):1548-1550. doi:10.1007/s00134-018-5323-5 support strategies for respiratory distress
25. Mukerji A, Singh B, Helou SE, et al. Use of 34. Gaertner VD, Waldmann AD, Davis PG, et al. syndrome in preterm infants: a systematic review
noninvasive high-frequency ventilation in the Transmission of oscillatory volumes into the and meta-analysis. Eur J Pediatr. 2022;181(1):215-223.
neonatal intensive care unit: a retrospective review. preterm lung during noninvasive high-frequency doi:10.1007/s00431-021-04190-0
Am J Perinatol. 2015;30(2):171-176. doi:10.1055/s- ventilation. Am J Respir Crit Care Med. 2021;203(8): 43. Shankar-Aguilera S, Taveira M, De Luca D.
0034-1381317 998-1005. doi:10.1164/rccm.202007-2701OC Neonatal ventilation trials need specific funding.
26. Ali YAH, Seshia MM, Ali E, Alvaro R. 35. De Luca D. Noninvasive high-frequency Lancet Respir Med. 2014;2(11):867-869. doi:10.
Noninvasive high-frequency oscillatory ventilation: ventilation and the errors from the past: designing 1016/S2213-2600(14)70194-8
jamapediatrics.com (Reprinted) JAMA Pediatrics June 2022 Volume 176, Number 6 559
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 07/28/2023
You might also like
- 基于流式细胞术的可测量残留... 白血病预后意义的前瞻性研究 霍娅Document8 pages基于流式细胞术的可测量残留... 白血病预后意义的前瞻性研究 霍娅liu guidiNo ratings yet
- 儿童急性T淋巴细胞白血病的诊疗进展 唐文豪Document5 pages儿童急性T淋巴细胞白血病的诊疗进展 唐文豪liu guidiNo ratings yet
- 淋巴瘤诊疗规范 (2018年版)Document22 pages淋巴瘤诊疗规范 (2018年版)liu guidiNo ratings yet
- Netrin-1 Induces The Anti-ApoptoticDocument14 pagesNetrin-1 Induces The Anti-Apoptoticliu guidiNo ratings yet
- 肿瘤患儿中性粒细胞缺乏伴发热的抗感染治疗 许凤玲Document5 pages肿瘤患儿中性粒细胞缺乏伴发热的抗感染治疗 许凤玲liu guidiNo ratings yet
- 儿童朗格汉斯细胞组织细胞增... 发病机制及靶向治疗研究进展 周婵Document4 pages儿童朗格汉斯细胞组织细胞增... 发病机制及靶向治疗研究进展 周婵liu guidiNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- Plan de SeguridadDocument34 pagesPlan de SeguridadAlexitoh AleNo ratings yet
- ZH Folia PMTDocument1 pageZH Folia PMTIago CorreiaNo ratings yet
- Limitaciones Del EstudioDocument21 pagesLimitaciones Del EstudioElena Reyzabal EreñoNo ratings yet
- Código Sustantivo DEL Trabajo: Ximena Alexandra Andrade Gonzalez 2023Document38 pagesCódigo Sustantivo DEL Trabajo: Ximena Alexandra Andrade Gonzalez 2023Ximena GonzalezNo ratings yet
- Sound Level Measurement December 2020Document3 pagesSound Level Measurement December 2020rio alfarisiNo ratings yet
- SEMINARIO #02 - OPERATORIA DENTAL II - I Unidad - 2021Document23 pagesSEMINARIO #02 - OPERATORIA DENTAL II - I Unidad - 2021AngelicaNo ratings yet
- Ejercicios para Evaluaciones y Actividades RESUELTODocument3 pagesEjercicios para Evaluaciones y Actividades RESUELTOCamilo ChauxNo ratings yet
- Solución Caso Practico MariaDocument31 pagesSolución Caso Practico MariapsicologiapmvictimascotaNo ratings yet
- Ergo Silla de RuedasDocument7 pagesErgo Silla de RuedasNatalia RinconNo ratings yet
- Learning ACT: An Acceptance & Commitment Therapy Skills-Training Manual For TherapistsDocument4 pagesLearning ACT: An Acceptance & Commitment Therapy Skills-Training Manual For TherapistsPedro GuimarãesNo ratings yet
- Learning Disability: Sed Prof 224Document38 pagesLearning Disability: Sed Prof 224LJ Agpoon ReyesNo ratings yet
- IMNCIDocument84 pagesIMNCIAyenew100% (1)
- Practica AINESDocument5 pagesPractica AINESErwin Hernández GarcíaNo ratings yet
- PIEX TI (Abner Rodrigues Figueira)Document7 pagesPIEX TI (Abner Rodrigues Figueira)AbnerrffNo ratings yet
- 9 Nurse AssessmentDocument14 pages9 Nurse AssessmentHielda MariyanaNo ratings yet
- Protocolos de Seguridad ExpDocument16 pagesProtocolos de Seguridad ExpQueritáw Xzxz'No ratings yet
- Atlacomulco Plan de Manejo de ResiduosDocument10 pagesAtlacomulco Plan de Manejo de ResiduosAna Karen Guerrero PlataNo ratings yet
- Administração de Medicamentos Via Endovenosa - Sou EnfermagemDocument7 pagesAdministração de Medicamentos Via Endovenosa - Sou EnfermagemImerson Alberto AlfaneNo ratings yet
- Hernias Internas. Claves DiagnósticasDocument20 pagesHernias Internas. Claves DiagnósticasResidentes Cirugia HGQNo ratings yet
- Proyecto de ReciclajeDocument12 pagesProyecto de ReciclajeMarisela TomalaNo ratings yet
- SOP For Waste & Scarp Management: 1. PurposeDocument5 pagesSOP For Waste & Scarp Management: 1. Purposemrugeshj83% (6)
- Fragmentos y Definiciones. PMLDocument8 pagesFragmentos y Definiciones. PMLMarisol MaimoNo ratings yet
- Riesgos 20211117 192311 147Document21 pagesRiesgos 20211117 192311 147yomiraNo ratings yet
- TSI - Clasificacion - Documentacion - MGH 2022Document54 pagesTSI - Clasificacion - Documentacion - MGH 2022ese pescaNo ratings yet
- Indian Api Industry - Reaching The Full Potential: AprilDocument88 pagesIndian Api Industry - Reaching The Full Potential: AprilStevin GeorgeNo ratings yet
- Comite Paritario en FaenasDocument10 pagesComite Paritario en FaenasJuan Mejia Aburto100% (2)
- Reglamento de Seguridad MineraDocument12 pagesReglamento de Seguridad MineraCarlos NuñezNo ratings yet
- Plan de BienestarDocument10 pagesPlan de BienestarMaria Margarita Alvarez OrtizNo ratings yet
- Trabajo de ÉticaDocument4 pagesTrabajo de ÉticaBENJAMIN ANTONIO BARRIOS PLAZANo ratings yet
- IPDC PPTDocument12 pagesIPDC PPTDhruv VaghasiyaNo ratings yet