Professional Documents
Culture Documents
Jurnal 1 Terapi Bedah - H
Uploaded by
Yusuf DiansyahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jurnal 1 Terapi Bedah - H
Uploaded by
Yusuf DiansyahCopyright:
Available Formats
ISSN(Online): XXXXXX
ISSN (Print): XXXXXX
International Journal of Innovative Research in Dental Sciences
Vol. 4, Issue 3, May-June 2019
Epulis Fissuratum in Total Denture Wearers
Clinical Case Report
Dr. FZ.GHAZZAR, Dr. A.HATIM, Dr. K.MRHAR, Pr. S.BELLEMKHANNATE
(1)(2)(3): Prosthodontist in the Removable Prosthesis Service C.C.T.D Casablanca, Head of the Removable Prosthesis
Service C.C.T.D. Faculty of Dentistry, University Hassan II Casablanca, Morocco
ABSTRACT: Patients with a removable prosthesis may develop various mucosal pathologies, when
this prosthesis based on the depressible tissues of the fibromucosa overlying the maxillary and
mandibular jaw bone is poorly adapted.
Inflammatory fibrous hyperplasia, otherwise known as epulis fissuratum, is the most common
reactive mucosal disorder and is directly correlated to prosthesis wear. [5]
It is a reactive lesion of the oral mucosa caused by trauma to chronic trauma due to poorly fitting
prostheses [1, 2]
The size of the lesion varies from a few millimeters to a massive extension involving the entire
vestibule.
It is usually asymptomatic but sometimes severe inflammation and ulceration can occur, causing pain
and discomfort.
Surgical excision of the lesion and rehabilitation of the prosthesis are the treatment of choice.
This article presents, through clinical cases, the therapeutic approaches of different prosthetic
hyperplasias, secondary to the wearing of poorly adapted prostheses, for conventional prosthetic
rehabilitation.
KEYWORDS: Epulis fissuratum, ill fitting denture, inflammatory hyperplasia.
I. INTRODUCTION
The epulis fissuratum or fibrous prosthetic hyperplasia is a circumscribed pseudo-tumoral
hyperplastic lesion, sitting in the vestibule. It is a reaction lesion to poorly adapted prostheses
which appear in patients who have been fitted for a very long time. Chronic irritation is due to
prostheses whose edges are too sharp or too bulky. The lesions are presented as single or multiple
hyperplastic proliferations, of greater or lesser volume, elongated in the gingivo-labial or gingivo-
Copyright to IJIRDS 542
ISSN(Online): XXXXXX
ISSN (Print): XXXXXX
International Journal of Innovative Research in Dental Sciences
Vol. 4, Issue 3, May-June 2019
jugal groove. The hyperplastic folds are floating, somehow firm and their proliferation may hinder
retention and prosthetic stability.
The chronic nature of the process means that the discomfort is often not an important feature, and
that the patient can continue to wear the defective prosthesis until the size of the hyperplasias
increases, and before the patient becomes report the lesion. In addition, the epulis fissuratum may be
associated with painful ulcerations at the base of the folds.
This pseudo-tumoral formation is frequent in the elderly with a female predominance, and develops
most often at the edges of the mandibular prostheses.
Treatment of the epulis includes surgical removal and pathological examination, followed by
relining of the patient's existing prosthesis with delayed-setting resin.
Case Report:
A 61-year-old female patient, consulting at the Casablanca Dental Consultation and Treatment
Center in the Prosthodontic Department, complaining of prosthetic instability and severe pain
exacerbated by the wearing of the prosthesis.
During the interrogation, the patient reports having been fitted with a total bimaxillary prosthesis
for 6 years, and the appearance of a small mass of soft tissue at the level of the lower arch which has
developed to the current size on a 12-month period with increased pain during chewing.
The endobuccal examination revealed the presence of multiple hyperplastic tissue folds at the
mandibular vestibule floor, the lesion is firm non-haemorrhagic floating with ulcerated appearance.
[Figure 1]
- The examination of the old prostheses reveals a medium prosthetic hygiene, an unstable
mandibular prosthesis and thin and sharp edges compared to the hyperplasia.
Following this examination, a surgical and prosthetic treatment plan was proposed to the patient.
The treatment consisted of the following steps:
- Motivation for prosthetic hygiene and mucosal hygiene,
- Plastic surgery followed by an anatomopathological examination of the operative specimen which
confirmed the epulidian nature of the tumor. [Figure 2]
-Realization of a tissue conditioning conventional bimaxillary prosthesis.
-After cicatrization realization of new prostheses respecting the norms. [Figure ¾]
Copyright to IJIRDS 543
ISSN(Online): XXXXXX
ISSN (Print): XXXXXX
International Journal of Innovative Research in Dental Sciences
Vol. 4, Issue 3, May-June 2019
Figure 1: Presence of multiple hyperplastic
Figure 2: Ablation of mucous replies
Figure 3: Result after 15 days
Copyright to IJIRDS 544
ISSN(Online): XXXXXX
ISSN (Print): XXXXXX
International Journal of Innovative Research in Dental Sciences
Vol. 4, Issue 3, May-June 2019
Figure 4: Result after 1 month
II. DISCUSSION
Epulis fissuratum is a common lesion in patients with old and inadequate removable prostheses
due to bone resorption associated with aging. This leads to repeated suction and suction motions
causing mucosal effusion, generating Fibrous hyperplasias in the form of bulges or leaflets.These
oral lesions related to the wearing of a removable prosthesis are most often observed in the carriers
of Complete Removable Prostheses (PAC) than Partial Movable Prostheses (PAP) [2], probably
because of the maximum mucosal recovery. [3] The prosthetic base acts as an insulator, a chemical,
mechanical and microbial irritant.
Ulcerations in areas with over-extension [1] are the most frequently found lesions. [4] They appear
after a point or chronic irritation of the mucosa caused by the wearing of a poorly adapted prosthesis.
In fact, the epulis fissuratum is more common in women, probably because they wear their
prostheses longer than men, for aesthetic reasons including [3,14] more postmenopausal mucosal
atrophy would generate a field favorable to the development of such lesions. [15]
The epulis fissuratum may assume the appearance of a sessile outgrowth with simple or multiple
benign proliferations. Most often, there are two layers, one extending below the prosthesis and the
other extending over the polished outer surface of the prosthesis. This lesion is most often covered
with an intact mucosa, soft or firm and not hemorrhagic, but it can sometimes be ulcerated. The
locations are most often located at the vestibule or anterior pelvic-lingual groove.
Hyperplasia is characterized by an absence of symptomatology often making consultation late; the
circumstances of consultation are due in general to the appearance of functional disorders.
Copyright to IJIRDS 545
ISSN(Online): XXXXXX
ISSN (Print): XXXXXX
International Journal of Innovative Research in Dental Sciences
Vol. 4, Issue 3, May-June 2019
Histologically, epulis fissuratum is hyperplastic fibrous connective tissue. The epithelium above
the latter is often hyperkeratotic.
The management of this type of pathologies induced by the removable prosthesis comprises several
phases. The conditioning of the oral cavity appears as the preliminary sequence of a coherent
prosthetic treatment. The indication of pre-prosthetic surgery, with or without tissue conditioning and
rehabilitation of existing prostheses, can restore histological and physiological behavior to the oral
mucosa.
The treatment of hyperplasia can be non-surgical set in tissue condition or by surgical removal.
In the early stages of mucosal hyperplasia, when minimal and soft tissue conditioning is often
sufficient to reduce or eliminate this lesion.
Nevertheless, pre-prosthetic surgery is essential whenever these hyperplasias are important, fibrous
and old and when the conditioning in tissue condition brings no improvement.
Surgical excision should be systematically accompanied by a histopathological examination of the
operative specimen to confirm the diagnosis and eliminate any malignancy.
Rectification of defective prostheses; as well from the point of view of adaptation of the intrados
and edges, as at the occlusal level; allows to obtain a stable prosthesis whose limits are precise, if
these old prostheses are unusable, they will serve as transitional prostheses before making the final
prostheses, to carry out simultaneously the restoration of tissue condition and functional and aesthetic
rehabilitation.
Tissue conditioning is a prerequisite for the development of a complete prosthesis. It uses, among
other things, a delayed-setting resin filling the intrados of a prosthesis of use or transition. This step
of the prosthetic treatment is intended to place the patient favorable to the development of a new
prosthesis, improving the histological, anatomical and physiological structures of the tissues in
contact with the prosthesis.
The delayed-setting resins consist of [5]:
a powder consisting of micro-beads of polyethylmethacrylate and polyethylene methyl
methacrylate of different diameters;
a liquid mixture of ethyl alcohol and plasticizers comprising different types of phthalates.
These resins once applied at the intrados of the prosthesis after mixing, they spread slowly and
mold accurately to the tissue reliefs. The gel obtained acts in the viscoelastic phase as a cushion
Copyright to IJIRDS 546
ISSN(Online): XXXXXX
ISSN (Print): XXXXXX
International Journal of Innovative Research in Dental Sciences
Vol. 4, Issue 3, May-June 2019
cushion between the prosthetic intrados and the mucosa reducing the trauma on the inflammatory
tissues.
The material loses its elastic properties, becomes granular. This transformation is caused by the
escape of the alcoholic esters to the salivary medium while the saliva enters the resin. The retard resin
becomes rough, aggressive towards the underlying tissues. This requires frequent renewal until the
tissues and surfaces of altered supports are improved.
New prostheses are made after healing, respecting a physiological distribution of the functional
pressures applied over the entire mucosal bearing surface in the realization of fingerprints and final
bases. The design of the prostheses must respect the different degrees of tissue resilience and other
factors of respect for the mucosal load capacity, by producing well-adapted, well-balanced and non-
traumatogenic prostheses, making it possible to restore all the physiological functions.
III. CONCLUSION
Although the wearing of a removable prosthesis provides an undeniable improvement in the quality
of life of the patient, the wearing of a poorly adapted prosthesis may be responsible for mucosal
lesions sometimes very debilitating.
REFERENCES
[1] Kafas P, Upile T, Stavrianos C, Angouridakis N, Jerjes W. Mucogingival overgrowth in a
geriatric patient. Dermatol Online J. 2010;16:7.
[2] Canger EM, Celenk P, Kayipmaz S. Denture-related hyperplasia: A clinical study of a Turkish
population group. Braz Dent J. 2009;20:243–8.
[3] Bhasker RM, Davenport JC, Thomson JM. 5th ed. UK: Willy-Blackwell; 2001. Prosthetic
treatment of the edentulous patients.
[4] Espinoza I, Rojas R, Aranda W, Gamonal J. Prevalance of oral mucosal lesions in elderly people
in Santiago Chile. J Oral Pathol Med. 2003;32:571–5.
[5] Firoosmand LM, Almeide JD, Cabral LA. Study of denture-induced fibrous hyperplasia cases
diagnosed from 1979-2001. Quintessence Int. 2005;36:825–9.
[6] Omal PM, Mathew SA. Denture-induced extensive fibrous inflammatory hyperplasia (Epulis
fissuratum) Kerala Dent J. 2010;3:154–5.
Copyright to IJIRDS 547
ISSN(Online): XXXXXX
ISSN (Print): XXXXXX
International Journal of Innovative Research in Dental Sciences
Vol. 4, Issue 3, May-June 2019
[7] Naveen Kumar J, Bhaskaran M. denture induced fibrous hyperplasia. Treatment with carbon
dioxide laser and a two year follow-up. Indian J Dent Res. 2007;18:135–7.
[8] Bhusal D, Joshi S. Comprehensive complete denture rehabilitation, a way to achieve recovery
of abused tissue: A case report. J Nepal Dent Assoc. 2010;11:59–6.
[9] Jainkittivong A, Aneksuk V, Langlais RP. Oral mucosal lesions in denture wearers.
Gerodontology 2010 ;27 :26-32.
[10] . Mikkonen M, Nyyssonen V, Paunio I et al. Prevalence of oral mucosal lesions associated with
wearing removable dentures in Finnish adults. Community Dent Oral Epidemiol 1984 ;12 :191-
194.
[11] . Coelho CM, Sousa YT, Dare AM. Denture-related oral mucosal lesions in a brazilian school of
dentistry. J Oral Rehabil 2004 ;31 :135-139.
[12] Kivovics P, Jahn M, Borbély J et al. Frequency and location of traumatic ulcerations following
placement of complete dentures. Int J Prosthodont 2007;20(4) :397-401.
[13] Mandali G, Sener ID, Turker SB et al. Factors affecting the distribution and prevalence of oral
mucosal lesions in complete denture wearers. Gerodontol 2011 ;28 :97-103.
[14] Correa L, Frigerio ML, Sousa SC et al. Oral lesions in elderly population : a biopsy survey
using 2250 histopathological records. Gerontology 2006 ;23 :48-54.
[15] Freitas JB, Gomez RS, De Abreu MH et al. Relationship between the use of full dentures and
mucosal alterations among elderly brazilians. J Oral Rehabil 2008 ;35 :370-374.
[16] Coelho CMP, Zucoloto S, Lopez RA. Denture induced fibrous inflammatory hyperplasia : a
retrospective study in a school of dentistry. Int J Prosthodont 2000 ;13 :148-151.
[17] Bellato L , Martinelli-Klay CP, Martinelli et al. Alveolar ridge keratosis – a retrospective
clinicopathological study. Head Face Med 2013 ;9(1) :12
Copyright to IJIRDS 548
You might also like
- Peri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentFrom EverandPeri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentNo ratings yet
- Kumar AM Et Al PJMS Vol 13 No 2 2014 PP 31 - 35Document6 pagesKumar AM Et Al PJMS Vol 13 No 2 2014 PP 31 - 35egarochmawatiNo ratings yet
- Focal Fibrous Hyperplasia: A Clinical and Histological InsightDocument3 pagesFocal Fibrous Hyperplasia: A Clinical and Histological InsightIJAR JOURNALNo ratings yet
- DentHypotheses7267-3698345 101623Document4 pagesDentHypotheses7267-3698345 101623Aliyah SaraswatiNo ratings yet
- Mucositis PeriDocument9 pagesMucositis PerianonimoNo ratings yet
- Ijos 201375 ADocument4 pagesIjos 201375 AIsmail YusufNo ratings yet
- 9685 40464 1 PBDocument3 pages9685 40464 1 PBTri Sakti Sunda RomdhoniNo ratings yet
- Journal of Periodontology - 2018 - Heitz Mayfield - Peri Implant MucositisDocument10 pagesJournal of Periodontology - 2018 - Heitz Mayfield - Peri Implant MucositisFrancisca Cardenas OñateNo ratings yet
- Berglundh 2018 Peri Implant Diseases and ConditionsDocument6 pagesBerglundh 2018 Peri Implant Diseases and ConditionsPatricia CastellanosNo ratings yet
- Peripheral Cemento-Ossifying Fibroma - A Case Report With A Glimpse On The Differential DiagnosisDocument5 pagesPeripheral Cemento-Ossifying Fibroma - A Case Report With A Glimpse On The Differential DiagnosisnjmdrNo ratings yet
- Epulis PathologyDocument5 pagesEpulis PathologyStefany FanyNo ratings yet
- 3 RdarticleDocument5 pages3 RdarticleAmira Pradsnya ParamitaNo ratings yet
- Maxillary Gingiva Case Report on Peripheral Ossifying FibromaDocument5 pagesMaxillary Gingiva Case Report on Peripheral Ossifying Fibromaanugraha GanendraNo ratings yet
- IndianJDentSci9134-1297591 033615Document4 pagesIndianJDentSci9134-1297591 033615Fransiski HoNo ratings yet
- Crid2014 842578Document5 pagesCrid2014 842578GouravSoniNo ratings yet
- Gingival Enlargement A ReviewDocument12 pagesGingival Enlargement A ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Perio 2000 VOL-76 Treatment of Pathologic Peri-Implant Pocket PDFDocument11 pagesPerio 2000 VOL-76 Treatment of Pathologic Peri-Implant Pocket PDFchandanaNo ratings yet
- Jurnal 3 Terapi BedahDocument7 pagesJurnal 3 Terapi BedahYusuf DiansyahNo ratings yet
- Peri-Implant MucositisDocument10 pagesPeri-Implant MucositisCarlos Armijos SNo ratings yet
- Management of Fibrous Epulis Case ReportDocument10 pagesManagement of Fibrous Epulis Case ReportTrianita DivaNo ratings yet
- Jurnal Resesi Gingiva 2Document7 pagesJurnal Resesi Gingiva 2Muhammad KholisNo ratings yet
- Chipalia 2014 Articulocompleto PDFDocument11 pagesChipalia 2014 Articulocompleto PDFLeid ArizaNo ratings yet
- Rare Herniation of Buccal Fat Pad into Oral Cavity After Tooth ExtractionDocument4 pagesRare Herniation of Buccal Fat Pad into Oral Cavity After Tooth ExtractionQuang BuiNo ratings yet
- Berglundh Et Al-2018-Journal of Clinical PeriodontologyDocument6 pagesBerglundh Et Al-2018-Journal of Clinical PeriodontologyCristian CulcitchiNo ratings yet
- Berglundh Et Al (2018) - Peri Implant Diseases and Conditions - Consensus Report of Workgroup 4 - 1Document9 pagesBerglundh Et Al (2018) - Peri Implant Diseases and Conditions - Consensus Report of Workgroup 4 - 1FelipeOyarceSalazarNo ratings yet
- Radicular Cyst: A Case Report: Harshitha KR, Varsha VK, Deepa. CDocument3 pagesRadicular Cyst: A Case Report: Harshitha KR, Varsha VK, Deepa. CEzza RiezaNo ratings yet
- Renvert Et Al (2018) - Peri Implant Health, Peri Implant Mucositis, and Peri Implantitis - Case Definitions and Diagnostic Considerations - 1Document9 pagesRenvert Et Al (2018) - Peri Implant Health, Peri Implant Mucositis, and Peri Implantitis - Case Definitions and Diagnostic Considerations - 1FelipeOyarceSalazarNo ratings yet
- Long Term Follow-Up of Oral Submucous Fibrosis Grade IV Case With A Versatile Nasolabial FlapA Case ReportDocument3 pagesLong Term Follow-Up of Oral Submucous Fibrosis Grade IV Case With A Versatile Nasolabial FlapA Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Ing 4Document7 pagesIng 4Ajeng Saskia PutriNo ratings yet
- PERIIMPLANTITIS RESUMEN Berglundh - Et - Al-2018-Journal - of - Clinical - PeriodontologyDocument12 pagesPERIIMPLANTITIS RESUMEN Berglundh - Et - Al-2018-Journal - of - Clinical - PeriodontologyDaniela RojasNo ratings yet
- The Periodontal Abscess: A Review: IOSR Journal of Dental and Medical Sciences November 2015Document7 pagesThe Periodontal Abscess: A Review: IOSR Journal of Dental and Medical Sciences November 2015Ameria Briliana ShoumiNo ratings yet
- Reusing Dental Implants?: An Experimental Study For Detecting The Success Rates of Re-OsseointegrationDocument7 pagesReusing Dental Implants?: An Experimental Study For Detecting The Success Rates of Re-OsseointegrationSatya AsatyaNo ratings yet
- Multiple Pulp Polyps Associated With Deciduous TeethDocument4 pagesMultiple Pulp Polyps Associated With Deciduous TeethJea Ayu YogatamaNo ratings yet
- Shira's Technique, An Alternative For The Enucleation of Cervicofacial CystsDocument4 pagesShira's Technique, An Alternative For The Enucleation of Cervicofacial CystsManuel Alejandro LinaresNo ratings yet
- ChirurgieDocument5 pagesChirurgiePatricia RalucaNo ratings yet
- ArticlefibromapublishedDocument6 pagesArticlefibromapublishedSiti firdha BimariskaNo ratings yet
- Radicular Cyst With Primary Mandibular Molar A RarDocument5 pagesRadicular Cyst With Primary Mandibular Molar A RargarciadeluisaNo ratings yet
- Schwarz Et Al (2018) - Peri Implantitis - 1Document23 pagesSchwarz Et Al (2018) - Peri Implantitis - 1FelipeOyarceSalazarNo ratings yet
- Case Report On Maxillary Labial FrenectomyDocument9 pagesCase Report On Maxillary Labial Frenectomyviolita chresnaNo ratings yet
- Clinical Case Reports - 2016 - Ronco - A Novel Suturing Approach For Tissue Displacement Within Minimally InvasiveDocument7 pagesClinical Case Reports - 2016 - Ronco - A Novel Suturing Approach For Tissue Displacement Within Minimally InvasiveÄpriolia SuNo ratings yet
- Ams 5 108Document4 pagesAms 5 108Alice EmailsNo ratings yet
- Report on Two Cases of Gingival Epulis LesionsDocument5 pagesReport on Two Cases of Gingival Epulis LesionsAnandNo ratings yet
- Frenectomy As A Multidisciplinary Prostho-Perio Management Approach For Partial Denture-A Case ReportDocument6 pagesFrenectomy As A Multidisciplinary Prostho-Perio Management Approach For Partial Denture-A Case ReportMidda SosmedNo ratings yet
- Esthetic and Functional Reconstruction of Large Mandibular Defects Using Free Fibula Flap and Implant-Retained Prosthetics - A Case Series With Long-Term Follow-UpDocument7 pagesEsthetic and Functional Reconstruction of Large Mandibular Defects Using Free Fibula Flap and Implant-Retained Prosthetics - A Case Series With Long-Term Follow-UppankajNo ratings yet
- Residual CystDocument4 pagesResidual Cyst053 Sava Al RiskyNo ratings yet
- Exostosis MandibularDocument6 pagesExostosis MandibularCOne Gomez LinarteNo ratings yet
- Dentigerous Cyst With An Impacted Canine in The Maxillary Sinus: A Rare Entity!Document3 pagesDentigerous Cyst With An Impacted Canine in The Maxillary Sinus: A Rare Entity!PaTt Tyy RodríguezNo ratings yet
- Abscesses of The Periodontium Article-PDF-bansi M Bhusari Rizwan M Sanadi Jayant R Ambulgeka-558Document4 pagesAbscesses of The Periodontium Article-PDF-bansi M Bhusari Rizwan M Sanadi Jayant R Ambulgeka-558Ferdinan PasaribuNo ratings yet
- Peripheral Ossifying Fibroma - A Case ReportDocument5 pagesPeripheral Ossifying Fibroma - A Case ReportIJAR JOURNALNo ratings yet
- Case DefinitionsDocument9 pagesCase DefinitionsCarlos Armijos SNo ratings yet
- 10863-Article Text-52091-1-10-20220425Document11 pages10863-Article Text-52091-1-10-20220425Aira Grace PadillaNo ratings yet
- MainDocument7 pagesMainPaula Francisca Moraga HidalgoNo ratings yet
- Large Unusual Fibroepithelial Polyp Case ReportDocument4 pagesLarge Unusual Fibroepithelial Polyp Case ReportmuharrimahNo ratings yet
- Paradental Cyst ArticleDocument6 pagesParadental Cyst Articlerohit singhaiNo ratings yet
- Adenomatoid Odontogenic Tumour of Maxilla A Case ReportDocument6 pagesAdenomatoid Odontogenic Tumour of Maxilla A Case ReportAthenaeum Scientific PublishersNo ratings yet
- Ojst 2017110914371416Document6 pagesOjst 2017110914371416Santa ChrisNo ratings yet
- OsteomaDocument4 pagesOsteomaAnjungAdelNo ratings yet
- Maintaining Dental Implants to Prevent InfectionDocument9 pagesMaintaining Dental Implants to Prevent Infectionالعمري العمريNo ratings yet
- ROOT COVERAGE WITH PERIOSTEUM PEDICLE GRAFT - A NOVEL APPROACH DR Vineet VinayakDocument3 pagesROOT COVERAGE WITH PERIOSTEUM PEDICLE GRAFT - A NOVEL APPROACH DR Vineet VinayakDr Vineet VinayakNo ratings yet
- Bilateral Ectopic Third Molars in Maxillary Sinus Associated With Dentigerous Cyst Identified With Ophthalmic, Nasal and Maxillary Complication: A Rare Case ReportDocument4 pagesBilateral Ectopic Third Molars in Maxillary Sinus Associated With Dentigerous Cyst Identified With Ophthalmic, Nasal and Maxillary Complication: A Rare Case ReporttasbetulNo ratings yet
- Conservative Composite Resin Restoration For Proximal Caries - Two Case ReportsDocument8 pagesConservative Composite Resin Restoration For Proximal Caries - Two Case Reportsmin moongNo ratings yet
- 82984-Article Text-200031-1-10-20121112Document3 pages82984-Article Text-200031-1-10-20121112Yusuf DiansyahNo ratings yet
- Interpretation of Panoramic RadiographsDocument6 pagesInterpretation of Panoramic RadiographsYusuf DiansyahNo ratings yet
- Jurnal 3 Terapi BedahDocument7 pagesJurnal 3 Terapi BedahYusuf DiansyahNo ratings yet
- Bilateral Maxillary Second Molar Tooth Microdontia: A Case of Very Rare Tooth AnomalyDocument3 pagesBilateral Maxillary Second Molar Tooth Microdontia: A Case of Very Rare Tooth AnomalyYusuf DiansyahNo ratings yet
- Oral Mucosal Lesions Associated With The Wearing of Removable DenturesDocument17 pagesOral Mucosal Lesions Associated With The Wearing of Removable DenturesnybabyNo ratings yet
- Month:: Sunday Saturday Tuesday Wednesday Thursday Friday MondayDocument1 pageMonth:: Sunday Saturday Tuesday Wednesday Thursday Friday MondayYusuf DiansyahNo ratings yet
- Digital Prosthetic Workflow During COVID-19 Pandemic To LimitDocument4 pagesDigital Prosthetic Workflow During COVID-19 Pandemic To LimitalphaniaNo ratings yet
- Jama Grennan 2019 PG 190004 PDFDocument1 pageJama Grennan 2019 PG 190004 PDFKanesti KamajayaNo ratings yet
- Retention in Conventional Fixed Partial Dentures: A Review: Key MessageDocument6 pagesRetention in Conventional Fixed Partial Dentures: A Review: Key MessagePuskesmas Losarang100% (1)
- Tingkatan Respon TiongkokDocument6 pagesTingkatan Respon TiongkokYusuf DiansyahNo ratings yet
- Complete Dentures - Part 2Document7 pagesComplete Dentures - Part 2Lee MulderNo ratings yet
- How the longevity of fixed dental prostheses depends on the cement functionDocument12 pagesHow the longevity of fixed dental prostheses depends on the cement functionYusuf DiansyahNo ratings yet
- Complete Dentures An Update On Clinical Assessment PDFDocument8 pagesComplete Dentures An Update On Clinical Assessment PDFandres schlosserNo ratings yet
- Writing Sample 2Document9 pagesWriting Sample 2api-582848179No ratings yet
- Orthop J Sports Med 2021 9 7 23259671211013394Document6 pagesOrthop J Sports Med 2021 9 7 23259671211013394Fernando SousaNo ratings yet
- THIBARMY Best Damn NATTY LIFTSDocument11 pagesTHIBARMY Best Damn NATTY LIFTSÒó Reverse100% (3)
- Dialysis Notes 1Document3 pagesDialysis Notes 1SarahSigrid87% (23)
- Beliefs About Obsessional Thoughts InventoryDocument21 pagesBeliefs About Obsessional Thoughts InventoryMarta CerdáNo ratings yet
- Prolonged Fasting - How Is It PosiblerDocument17 pagesProlonged Fasting - How Is It PosiblersaturninojonesNo ratings yet
- Importance of Sustainable Development GoalsDocument2 pagesImportance of Sustainable Development GoalsDyas FerNo ratings yet
- PAN India Empanelled Hospital List - OICDocument423 pagesPAN India Empanelled Hospital List - OICBHARAT BHUSHANNo ratings yet
- AP Psychology Review in 40 CharactersDocument83 pagesAP Psychology Review in 40 CharactersKitty chenNo ratings yet
- NutritionDocument5 pagesNutritionk,srikanthNo ratings yet
- Ps DM - Ogl 365-Module 6 PaperDocument3 pagesPs DM - Ogl 365-Module 6 Paperapi-573130450No ratings yet
- COVID vaccination certificate for Indian teenDocument1 pageCOVID vaccination certificate for Indian teenShubham TiwariNo ratings yet
- Cure Disease: Charred Skeever Hide Felsaad Tern Feathers Hawk Feathers Mudcrab Chitin Vampire DustDocument5 pagesCure Disease: Charred Skeever Hide Felsaad Tern Feathers Hawk Feathers Mudcrab Chitin Vampire DustFarsiko Risma YandiNo ratings yet
- [Journal of Autism and Childhood Schizophrenia vol. 49 iss. 6] Ng, Rowena_ Heinrich, Kimberley_ Hodges, Elise K. - Brief Report_ Neuropsychological Testing and Informant-Ratings of Children with Autism Spectrum Disorder, Atten - libgen.liDocument8 pages[Journal of Autism and Childhood Schizophrenia vol. 49 iss. 6] Ng, Rowena_ Heinrich, Kimberley_ Hodges, Elise K. - Brief Report_ Neuropsychological Testing and Informant-Ratings of Children with Autism Spectrum Disorder, Atten - libgen.ligustavNo ratings yet
- Gelofusine Solutionforinfusion MandatoryinformationDocument3 pagesGelofusine Solutionforinfusion Mandatoryinformationhanen.aymanNo ratings yet
- Nur3116 Social Determinants of Health PaperDocument6 pagesNur3116 Social Determinants of Health Paperapi-578141969No ratings yet
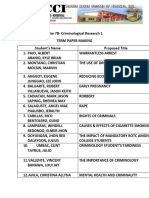
- Term Paper TitlesDocument6 pagesTerm Paper TitlesGOOD BATA WAY BITOKNo ratings yet
- La Fortuna Nhs GPB 2022Document50 pagesLa Fortuna Nhs GPB 2022Jesselly ValesNo ratings yet
- Maxillary LandmarksDocument30 pagesMaxillary LandmarksRajsandeep Singh86% (14)
- Occupational Therapy Practice Framework: Domain and Process Fourth Edition (2020)Document87 pagesOccupational Therapy Practice Framework: Domain and Process Fourth Edition (2020)Susana Ahumada100% (1)
- Physio 2.05 Bloodphysiology2 HemostasisDocument9 pagesPhysio 2.05 Bloodphysiology2 HemostasisSimon Peter Familara100% (1)
- Jeenspsu 17Document13 pagesJeenspsu 17GokulVijayGopal G10No ratings yet
- Intelligent ConstructionDocument4 pagesIntelligent ConstructionRikesh SapkotaNo ratings yet
- NuRS 115 ResearchDocument15 pagesNuRS 115 ResearchD-Babygirl BlessedShorty DonnaNo ratings yet
- Talent Management SystemDocument22 pagesTalent Management SystemDeepa Yadav100% (1)
- Output-Poi PNP Swat Post Training ProgramDocument4 pagesOutput-Poi PNP Swat Post Training ProgramSJ SalazarNo ratings yet
- 6.11 Bullying ReadyDocument41 pages6.11 Bullying ReadyAstraX EducationNo ratings yet
- Oral Surgery Maxill - Anesthesia TechniquesDocument4 pagesOral Surgery Maxill - Anesthesia TechniquesSaif AyedNo ratings yet
- Digital Citizenship vs. Global CitizenshipDocument20 pagesDigital Citizenship vs. Global CitizenshipMacasinag Jamie Anne M.No ratings yet
- Project On-Law of Torts Topic - NegligenceDocument10 pagesProject On-Law of Torts Topic - NegligenceSoumya Shefali ChandrakarNo ratings yet





















































































![[Journal of Autism and Childhood Schizophrenia vol. 49 iss. 6] Ng, Rowena_ Heinrich, Kimberley_ Hodges, Elise K. - Brief Report_ Neuropsychological Testing and Informant-Ratings of Children with Autism Spectrum Disorder, Atten - libgen.li](https://imgv2-2-f.scribdassets.com/img/document/596448205/149x198/c66e65b0ff/1710588633?v=1)