Professional Documents
Culture Documents
GI Disorders Problems in Elimiation Absorption Digestion
Uploaded by
Mikee Paningbatan0 ratings0% found this document useful (0 votes)
6 views4 pagesOriginal Title
GI Disorders Problems in Elimiation Absorption Digestion(1)
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
6 views4 pagesGI Disorders Problems in Elimiation Absorption Digestion
Uploaded by
Mikee PaningbatanCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 4
Disturbances in Digestion Endoscopy and MRI or CT
Identifies the source and cause of bleeding
Gastrointestinal bleeding Stool test- for occult blood
A bleeding symptom either in upper of lower GI
Maybe obvious in emesis or stool or occult or Nursing Diagnosis
hidden Fluid volume deficit related to blood loss
Altered Nutrition: Less than body
TYPES OF GI BLEEDING (LOCATION) requirement related to nausea, vomiting and
Upper GI bleeding diarrhea
• bleeding in the upper gastrointestinal tract
arising from the esophagus, stomach or EMERGENCY INTERVENTION
duodenum. Patient remains on NPO
• Coffee ground or black IV lines and oxygen therapy
Lower GI Bleeding Administer vasopressin and blood replacement
Bleeding occurs in the colon, rectum, or anus because severe bleeding is life threatening and to
presents hematochezia or melena treat shock
Intra arterial vasopressin- to slow or stop
Pathophysiology and Etiology bleeding from diverticulum
Trauma in the GI tract Surgical if indicated.
Erosions or ulcers
Ruptured of an enlarged vein such as varicosity Nasogastric tube Intubation
(esophageal or gastric varices An NG tube should be in place for most patients
Inflammation such as esophagitis (cause by with acute or upper GI bleeding
acid), gastritis, 2-3 L of tap water lavage and if the aspirate
Inflammatory bowel disease (ulcerative colitis continues to be bloody, this indicate that the
and Crohn’s patient is in active bleeding that requires
Alcohol and drugs ( aspirin, NSAIDS and emergent intervention
cortecosteroids)
Diverticular disease Nursing Interventions
Hemorrhoids or fissures Attaining Normal Fluid Volume
Maintain NG tube and NPO status to rest GI
Clinical Manifestations tract and evaluate bleeding
Characteristic of blood Monitor I and O to evaluate fluid status and
Bright red: vomited from high esophagus hydration
(hematemesis), rectum or distal colon Monitor VS
Mixed with dark red: higher up in colon and Administer IV fluids,
small intestine, mixed with stool Assess signs of shock such as hypotension,
Coffee Ground: esophagus, stomach, and tachycardia, tachypnea (increase RR), decrease
duodenum urine output, change in mental status.
Melena (black tarry stool) excessive blood in the
stomach Attaining Balance Nutritional Status
Weigh daily to monitor caloric status’
Signs and Symptoms of Bleeding TPN, to promote hydration and nutrition while
Massive bleeding on NPO restriction
Acute, bright red hematemesis or large amount Begin liquids if patient is no longer on NPO,
of black tarry stool then DAT. DAT should be high in calorie, high
Rapid pulse, hypotension, hypovolemia and CHON. Frequent small feedings if indicated.,
shock
Subacute bleeding Patient Education
Intermittent/alternate melena or coffee ground Instruct the patient to report signs of GI
emesis bleeding such as melena, emesis that is bright
Weakness, dizziness red or coffee ground color, rectal bleeding,
Chronic Bleeding weakness, fatigue and SOB
Intermittent appearance of blood Evaluation
Increased weakness, paleness or SOB Fluid volume is maintained, hypovolemic shock
Occult blood is prevented
Patient verbalized no signs of bleeding
Diagnostic Evaluation/test/Assessment Nutritional and body weight status is maintained
History
Change in bowel pattern, Complications
Presence of pain or tenderness Hemorrhage, Shock, Death
Recent intake of food and what kind(red beef),
Alcohol consumption and medications taken GASTRITIS
(aspirin or steroids, NSAIDS) Inflammation of the gastric or stomach mucosa
CBC It affects both sexes but more common in older
Low hemoglobin, high hematocrit, low platelet adults
High PT( 10-12 sec )and aPTT( 30-45sec); NV
TYPES OF GASTRITIS with fluid and blood) and to undergo superficial
ACUTE erosion which will result to hemorrhage.
lasting several hours to few days In chronic gastritis, persistent and repeated
insults lead to chronic inflammation that leads to
Causes
severe form of acute gastritis is caused by atrophy or thinning of the gastric tissue.
ingestion of strong acid or alkali that may (Grossman and Porth, 2014)
cause the mucosa to become gangrene or
possible for perforation. Scarring can occur Clinical Manifestations
which results to Pyloric stenosis (narrowing or
tightening) or obstruction Acute Gastritis- rapid onset of symptoms that last
AG maybe develop in acute illnesses or major from a few hours to a few days
traumatic injuries (Burns, severe infection, Hiccups
hepatic,kidney or respiratory failure and major Anorexia
surgery also known as Stress Related Gastritis Epigastric pain (rapid onset
Dyspepsia (Indigestion)
CLASSIFICATION OF ACUTE GASTRITIS
Nausea and vomiting
Based on pathologic manifestations present in the gastric
mucosa (Wehbi, et al.,2104) Melena (black, tarry stools,) hematemesis
(blood in vomitus), hematochezia (bright red,
Erosive Acute Gastritis bloody stools)- Erosive gastritis ,Possible sign of
most often cause by local irritants such as shock
aspirin and other NSAIDS (Naproxen, Voltaren,
Ibuprofen), alcohol consumption and gastric Chronic Gastritis
radiation therapy (Grossman, & Porth, 2014,
Belching
Wehbi, et al.,2104NIDDK, 2015)
Early satiety Anorexia
Non-Erosive Acute Gastritis Intolerance to fatty and spicy foods
most often caused by an infection with Nausea and vomiting
Helicobacter Pylori (H. Pylori) (Wehbi, et Pyrosis/heartburn (Burning sensation in the
al.,2104) stomach and esophagus that moves up into the
70% of individauls in US and other mouth after eating
industrialized countries are infected with H.
Sour taste in mouth
Pylori (CDC, 2016)
Epigastric pain relieves by eating
CHRONIC Systemic: Fatigue and anemia
results from repeated exposure to irritating
agents or recurrent episodes of acute gastritis Diagnostic Test
Upper Endoscopy and histologic examination
Causes confirms the diagnosis. This visualized
H. Pylori infection is the most common cause
inflammatory changes lesions or erosion and can
(Marcus and Greenwald, 2014). Chronic H.
Pylori gastritis is implicated in the development determine H.Pylori by biopsy
ofPUD, gastric adeno carcinoma, and gastric Other non invasive test that can detect H. Pylori
mucosa associated with lymphoid tissue is through serologic testing for antibodies
lymphoma (Chin, et al.,2015) against H Pylori antigen, stool antigen test ,
Chemical gastric injury (Gastropathy)- long Urea breath test
term use of NSAIDS and aspirin CBC- to assess anemia as a result of hemorrhage
Autoimmune disease- Hashimoto thyroiditis,
Addison’s disease, Grave’s disease are also be
associated with Chronic Gastritis (Grossman and NURSING INTERVENTIONS
Porth, 2014; Marcus and Greenwald, 2014) Independent
Promoting Optimal Nutrition
PATHOPHYSIOLOGY No foods of fluids by mouth for a few days-
until acute symptoms subside to allow gastric
Gastritis is characterized by Disruption of the mucosa to heal. (Erosive)
mucosal barrier that normally protects the Monitor I and O and electrolytes (Na, K,
stomach from digestive juices (Hcl and pepsin) Chloride) if in IVF every 24 hrs. to detect any
are irritating agents (Aspirin, NSAID and H. imbalances and signs of DHN (minimum oral
Pylori) comes in contact with the gastric mucosa fluid intake of 1.5 L/day
that resulted to inflammation. Assess for signs of hemorrhagic gastritis such as
In Acute gastritis, the inflammation is usually hematemesis, tachycardia and hypotension. All
transient and self-limiting in nature. stools should examine for the presence of occult
Inflammation causes the gastric mucosa to bleeding.
become edematous and hyperemic (congested Monitor VS and notify the primary provider or
the attending physician.
Avoid NSAIDS and alcohol
Dependent Nursing Interventions Antacids, H2 blockers, PPI (NIDDK, 2015)
Diet Antibiotics- Metronidazole (Flagyl),
Ice chips followed by clear liquids after Amoxixillin, Clarithromicin, Tetracycline
symptoms subsides then solid foods as ordered. Bismuth salts (rare)
Advise Non-irritating food. high-fiber foods,
Metronidazole (Flagyl)
such as whole grains, fruits, vegetables, and
beans. low-fat foods, such as fish, lean meats, MA: Antibacterial & anti protozoal that assist in
and vegetables. Foods with low acidity, eradicating H. Pylori in gastric mucosa. It may
including vegetables and beans. cause anorexia and metallic taste
IV fluids if symptom persist just to maintain NC: Give with meals to decrease GI upset.
hydration if bleeding persist. If IV 3L/day Avoid alcohol, it increases blood thinning
NG tube intubation effects of warfarin
Administer antacids. H2 receptors blockers,
PPI, Antibiotics Amoxixillin,
MA: Eradicated H pylori bacteria in gastric
Pharmacological Therapy mucosa
ANTACIDS NC: Should not be used in patients with
Neutralized gastric acid by increasing the in pH hypersensitivity to penicillin
the GI tract. Provide symptomatic relief but do
not heal esophageal lesions.
Ex: Aluminum hydroxide (Amphogel),
Clarithromicin,
Aluminum hydroxide and Magnesium hydroxide
(Maalox); Milk of magnesia MA: Eradicated H pylori bacteria in gastric
Antacids containing both aluminum and mucosa
magnesium hydroxide balance the constipating NC: may cause GI upset, headache and altered
effects of ALUMINUM with the LAXATIVE taste, Can cause drug-drug interaction
effects of MAGNESIUM
Tetracycline
Nursing Responsibilities MA: Eradicated H pylori bacteria in gastric
shake the suspension or chewable tablets chew mucosa
them thoroughly and drink half glass of water to NC: may cause photosensitivity reaction, advise
promote passage to the stomach the patient to use sunscreen
Give antacids at least 1 hour from enteric coated May cause GI upset
tablets Caution in renal or hepatic impairment
Avoid intake of milk and dairy products that
Histamine 2 receptor antagonist/H2 blockers reduce effectiveness
Inhibit or decrease acid production by blocking Do not take iron supplements, multivitamins,
action of histamine on histamine receptors of calcium supplements, antacids, or laxatives
parietal cells of the stomach within 2 hours before or after taking
Ex: Cimetidine (Tagamet), Famotidine (Pepcid), tetracycline. These products can
Ranitidine (Zantac) make tetracycline less effective in treating your
infection.
PROTON PUMP INHIBITORS
Block gastric acid secretions by inhibiting acid Bismuth salts (rare)
pump in gastric parietal cells
Treat erosive esophagitis and GERD MA: suppresses H. Pylori in the gastric mucosa
Doudenal ulcer, Active gastric ulcer and assist in healing of ulcers
Eradicate H. Pylori infection NC: should be taken on an empty stomach. And
Ex: Esomeprazole (Nexium), Lanzoprazole, maygiven with antibiotics to eradicate the H
Omeprazole, Pantoprazole, Rabeprazole Pylori
NURSING RESPONSIBILITY RELIEVES PAIN
Swallow the capsules whole and not to chew or Assess the level of pain
crush them Analgesics as ordered.
Administer 1 hour before meal
Avoid gastric irritants like alcohol, smoking,
Heath Teachings
aspirin, caffeine, NSAIDS
Avoid taking NSAIDS and Aspirin
For CHRONIC GASTRITIS Avoid or refrain from alcohol and food until
Modify the diet. Avoid carbonated and caffeine, symptoms subside
irritating foods Avoid carbonated and caffeine drinks. Caffeine
Rest is a CNS stimulant that increase gastric activity
Reduce stress and pepsin secretion
Avoid smoking because nicotine reduces
secretion of pancreatic bicarbonate which
inhibits neutralization of gastric acid in the
duodenum (Lu et al., 2014)
Enforce to the patient the importance of
completing medication regimen as prescribed to
eradicate H. Pylori infection
Teach family members to how to administer
vitamin B 12 injection or make arrangement to
the primary provider in order to receive injection
. In gastritis or PUD, there is malabsorption of
Vitamin B 12
Emphasized the follow up appointments with
primary provider.
You might also like
- Esophageal Varices, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandEsophageal Varices, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- GI BleedDocument28 pagesGI BleedAnn Lan100% (1)
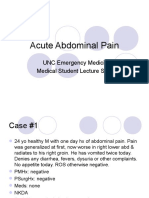
- Emergency Medicine: Acute AbdomenDocument33 pagesEmergency Medicine: Acute AbdomenPrashant MishraNo ratings yet
- Portal Vein Thrombosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandPortal Vein Thrombosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- The Gastrointestinal System: Anatomy, Symptoms and Common Presenting ComplaintsDocument84 pagesThe Gastrointestinal System: Anatomy, Symptoms and Common Presenting ComplaintsAlshare NisreenNo ratings yet
- GI Bleeding Team Work - 2nd EditionDocument9 pagesGI Bleeding Team Work - 2nd EditionUsman Ali AkbarNo ratings yet
- Vomiting of Blood, (Hematemesis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandVomiting of Blood, (Hematemesis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Abdominal PainDocument26 pagesAbdominal Painsammy_d6No ratings yet
- Acute AbdomenDocument25 pagesAcute AbdomenAli TahirNo ratings yet
- PBL 1Document7 pagesPBL 1Skyla Fiesta100% (1)
- PancreatitisDocument12 pagesPancreatitisjhodane100% (4)
- Signs N Symptoms of GEHDocument83 pagesSigns N Symptoms of GEHDdh2812No ratings yet
- PancreatitisDocument12 pagesPancreatitisapi-3797941100% (2)
- NCMB 316 Cu10 LgitDocument49 pagesNCMB 316 Cu10 LgitMaica LectanaNo ratings yet
- PancreatitisDocument12 pagesPancreatitismardsz100% (5)
- GI Signs and SymptomsDocument40 pagesGI Signs and SymptomsJohnny BeeNo ratings yet
- UgumDocument50 pagesUgumhailu henockNo ratings yet
- ICD 10.0: K29 Condition/Disease: Gastritis Description:: SymptomDocument3 pagesICD 10.0: K29 Condition/Disease: Gastritis Description:: SymptomvicndubNo ratings yet
- Acute AbdomenDocument60 pagesAcute AbdomenAnish DhamiNo ratings yet
- CP Upper Gastrointestinal / Esophageal BleedingDocument5 pagesCP Upper Gastrointestinal / Esophageal Bleedingeyecatcher_0013532No ratings yet
- CP Upper Gastrointestinal / Esophageal BleedingDocument5 pagesCP Upper Gastrointestinal / Esophageal Bleedingeyecatcher_0013532No ratings yet
- Abdominalpain 130214101728 Phpapp01Document78 pagesAbdominalpain 130214101728 Phpapp01Riddhisundar SamantaNo ratings yet
- Ashley Esdaile MSIII Byron Baptist MSIII Mike Pothen MS IIIDocument77 pagesAshley Esdaile MSIII Byron Baptist MSIII Mike Pothen MS IIISutapa PawarNo ratings yet
- Acute Abdomen Diagnosis and ManagementDocument54 pagesAcute Abdomen Diagnosis and ManagementChaichon PochaiNo ratings yet
- CME Upper GI BleedDocument46 pagesCME Upper GI Bleedfarah fadzilNo ratings yet
- Acute GastrointestinalDocument4 pagesAcute GastrointestinalJhexy Rhay BayagenNo ratings yet
- Acute AbdomenDocument19 pagesAcute Abdomenmazin89No ratings yet
- Acute AbdomenDocument47 pagesAcute AbdomenDani LeeNo ratings yet
- Signs N Symptoms of GEHDocument96 pagesSigns N Symptoms of GEHfatimah marwahNo ratings yet
- Renal Colic: Prepared By: Regine Anne B. PanganibanDocument19 pagesRenal Colic: Prepared By: Regine Anne B. PanganibanRej PanganibanNo ratings yet
- The Acute AbdomenDocument30 pagesThe Acute Abdomenmary2001pkNo ratings yet
- Upper Gi BleedingDocument37 pagesUpper Gi Bleedingfathima AlfasNo ratings yet
- Gi Case Study (Sep Batch)Document45 pagesGi Case Study (Sep Batch)MOHANTA, deviprasadNo ratings yet
- Abdominal Pain Causes and Exam FindingsDocument171 pagesAbdominal Pain Causes and Exam FindingsNaveen ChandanNo ratings yet
- Virtual Medical Library Homepage Quick ReferenceDocument4 pagesVirtual Medical Library Homepage Quick ReferenceAhmed HusseinNo ratings yet
- Week2 LgitDocument49 pagesWeek2 LgitriverabeanicoNo ratings yet
- Acute Gastrointestinal Bleeding GuideDocument47 pagesAcute Gastrointestinal Bleeding GuideJohn Clements Galiza100% (1)
- Medical Surgical Nursing Study GiudeDocument5 pagesMedical Surgical Nursing Study GiudeRexson Alcantara DalanginNo ratings yet
- Cholecystitis: A Case Presentation of Group 1&2Document73 pagesCholecystitis: A Case Presentation of Group 1&2MARIA STEPHANY DELA CRUZ100% (1)
- Acute and Chronic DiarrheaDocument38 pagesAcute and Chronic DiarrheaAriba AsifNo ratings yet
- Management of Patients With Gastro-Intestinal DisordersDocument84 pagesManagement of Patients With Gastro-Intestinal DisordersY. Beatrice AbigailNo ratings yet
- Upper Gastrointestinal Haemorrhage: S5 Unit 2006 Mbbs Batch Trivandrum Medical CollegeDocument194 pagesUpper Gastrointestinal Haemorrhage: S5 Unit 2006 Mbbs Batch Trivandrum Medical CollegeSrini VasanNo ratings yet
- Small Bowel ObstructionDocument38 pagesSmall Bowel ObstructionRUSSELL CILOTNo ratings yet
- Quiz BukasDocument3 pagesQuiz BukasDYRAH GRACE COPAUSNo ratings yet
- Gastrointestinal SurgeryDocument12 pagesGastrointestinal SurgeryHafsa AliNo ratings yet
- Acute Abdomen: Part I: Intestinal Obstruction/Bowel Infarction/ Constipation (And How To Assess and Initiate Management)Document63 pagesAcute Abdomen: Part I: Intestinal Obstruction/Bowel Infarction/ Constipation (And How To Assess and Initiate Management)Rumana IslamNo ratings yet
- Prepared by Inzar Yasin Ammar LabibDocument47 pagesPrepared by Inzar Yasin Ammar LabibdiaNo ratings yet
- Upper Gastrointestinal - Esophageal BleedingDocument15 pagesUpper Gastrointestinal - Esophageal Bleedingmardsz100% (9)
- Acute and Chronic DiarrhoeaDocument20 pagesAcute and Chronic DiarrhoeaVipul Nagnesia100% (2)
- Powerpoint: ComplicationsDocument50 pagesPowerpoint: Complicationsj.doe.hex_8750% (2)
- Lecture On Conjugated HyperbilirubinaemiaDocument38 pagesLecture On Conjugated HyperbilirubinaemiaIgwe SolomonNo ratings yet
- Hematemesis Melena (Upper Gi Bleeding)Document134 pagesHematemesis Melena (Upper Gi Bleeding)Mardoni Efrijon100% (1)
- Renal DisordersDocument60 pagesRenal DisordersENJELAH RAIKA NEYRANo ratings yet
- Department of Surgery: Case Presentation Intestinal ObstructionDocument46 pagesDepartment of Surgery: Case Presentation Intestinal Obstructionhadil ayeshNo ratings yet
- 401 TransesDocument6 pages401 TransesMYLENE GRACE ELARCOSANo ratings yet
- Assessing & Managing Urinary Tract DisordersDocument5 pagesAssessing & Managing Urinary Tract DisordersAlyssa Nicole CajayonNo ratings yet
- Renal Disorders 1Document73 pagesRenal Disorders 1Kyla PamaNo ratings yet
- Acute Abdominal Pain MS LectureDocument63 pagesAcute Abdominal Pain MS LectureRovanNo ratings yet
- Enc=Encoded=x00dbw9zvazhqrkomzztloljfr Fp0iikmmtestise8xoyj4rwomnikeop1wzsgqvmqfw95nhq==Document20 pagesEnc=Encoded=x00dbw9zvazhqrkomzztloljfr Fp0iikmmtestise8xoyj4rwomnikeop1wzsgqvmqfw95nhq==Mikee PaningbatanNo ratings yet
- Newly Revise Emergency Nursing 1Document65 pagesNewly Revise Emergency Nursing 1Mikee PaningbatanNo ratings yet
- Chapter 7 Nursing EthicsDocument66 pagesChapter 7 Nursing EthicsMikee PaningbatanNo ratings yet
- COMMON TERMS IN GI TREATMENT MODALITIES Part 1Document11 pagesCOMMON TERMS IN GI TREATMENT MODALITIES Part 1Mikee PaningbatanNo ratings yet
- Nursing Leadership and Management NotesDocument20 pagesNursing Leadership and Management NotesMikee Paningbatan100% (1)
- Kolej Matrikulasi Pulau Pinang Kementerian Pelajaran Malaysia 13200 Kepala BatasDocument9 pagesKolej Matrikulasi Pulau Pinang Kementerian Pelajaran Malaysia 13200 Kepala Bataskelisa157100% (2)
- Application of CFD To Debottleneck Production SepaDocument14 pagesApplication of CFD To Debottleneck Production SepaFernando AmoresNo ratings yet
- Commercial Kitchen Equipment CalculatorDocument16 pagesCommercial Kitchen Equipment CalculatorMohammad pharabiaNo ratings yet
- W 2HotlineContacts2019 - 0 2 PDFDocument3 pagesW 2HotlineContacts2019 - 0 2 PDFNathan Townsend Levy100% (1)
- Report On MinesDocument7 pagesReport On MinesYhaneNo ratings yet
- Phil. Crocodile-WPS OfficeDocument19 pagesPhil. Crocodile-WPS OfficeQUEENIE JAM ABENOJANo ratings yet
- Parts List of Engine Assy Ofdz-00536Document1 pageParts List of Engine Assy Ofdz-00536CwsNo ratings yet
- Master Gardener Home Vegetable Guide: Chapter 1 - Gardening BasicsDocument30 pagesMaster Gardener Home Vegetable Guide: Chapter 1 - Gardening BasicsAmr M. SaidNo ratings yet
- Activity 2EE56L FINALDocument6 pagesActivity 2EE56L FINALLUAÑA ALMARTNo ratings yet
- FREE BioGeometry Emitter PhotoDocument5 pagesFREE BioGeometry Emitter PhotoNisha Joshi75% (8)
- Company Profile ASIA ONE - 2022Document15 pagesCompany Profile ASIA ONE - 2022Nur SiswantoNo ratings yet
- Constructors in JavaDocument5 pagesConstructors in JavaAnonymous GqTzzkOfNo ratings yet
- Dynamic Bearing Capacity of Shallow FoundationDocument31 pagesDynamic Bearing Capacity of Shallow FoundationLingeswarran NumbikannuNo ratings yet
- Contractor base list in UsaDocument8 pagesContractor base list in Usamytech206No ratings yet
- Heat and Mass Chapter 2Document49 pagesHeat and Mass Chapter 2Mvelo PhungulaNo ratings yet
- CMG STARS Guide PDFDocument1,136 pagesCMG STARS Guide PDFAastha91% (11)
- VKS INFRA DPR Submission for NHAI Bihar ProjectDocument1 pageVKS INFRA DPR Submission for NHAI Bihar ProjectamirNo ratings yet
- Cost and Cost ClassificationDocument35 pagesCost and Cost ClassificationSusmita AcharyaNo ratings yet
- PTR 326 Theoretical Lecture 1Document14 pagesPTR 326 Theoretical Lecture 1muhammedariwanNo ratings yet
- Spartan-3E FPGA Starter Kit Board User Guide: UG230 (v1.2) January 20, 2011Document120 pagesSpartan-3E FPGA Starter Kit Board User Guide: UG230 (v1.2) January 20, 2011Alex XanderNo ratings yet
- CA ruling on fertilizer disputeDocument16 pagesCA ruling on fertilizer disputeRuby Anna TorresNo ratings yet
- Input Interfaces - Locate LPN LockDocument22 pagesInput Interfaces - Locate LPN LockSatyanarayana NekkantiNo ratings yet
- "Employee Payroll Management System": Miss - Priyanka Abhaynath YadavDocument31 pages"Employee Payroll Management System": Miss - Priyanka Abhaynath Yadavhabeb TubeNo ratings yet
- Mana Paribhsha RSBKDocument31 pagesMana Paribhsha RSBKlohiyakankshaNo ratings yet
- CP306 Example 01 OKDocument5 pagesCP306 Example 01 OKManish MahadevwalaNo ratings yet
- ECT ModelDocument12 pagesECT Modelhii_bhartiNo ratings yet
- Case Study of Haleeb FoodDocument18 pagesCase Study of Haleeb Foodjazi_4u86% (22)
- Future Developments in Management AccountingDocument4 pagesFuture Developments in Management AccountingAmar narayanNo ratings yet
- Giáo trình TACN Đồ họa 1 - 2021 - chính thứcDocument57 pagesGiáo trình TACN Đồ họa 1 - 2021 - chính thứcHeo BiểnNo ratings yet
- MEL - Math 10C Item Writing - MC & NR ReviewDocument71 pagesMEL - Math 10C Item Writing - MC & NR ReviewMya TseNo ratings yet