Professional Documents
Culture Documents
Glucose 6 Phosphate Def
Uploaded by
Joey MaravillasOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Glucose 6 Phosphate Def
Uploaded by
Joey MaravillasCopyright:
Available Formats
Case Studies
An Unexpected Emergency Request for
Glucose-6-Phosphate Dehydrogenase Testing
in a 9-Year-Old African American Boy
Peter Platteborze, PhD,1* Renee Matos, MD,2 Vinod Gidvany-Diaz, MD,2 Kelly Wilhelms, PhD1
Downloaded from https://academic.oup.com/labmed/article/46/2/150/2505057 by guest on 06 April 2023
Lab Med Spring 2015;46:150-152
DOI: 10.1309/LMEEC680QNEHQGIF
CLINICAL HISTORY
Patient: 9-year-old African American male. Previous Medical History: Unknown.
Chief Complaint: Recently diagnosed with acute lymphoblastic Family History: Largely unknown, but no apparent chronic diseases.
leukemia (ALL) after investigation into a large anterior mediastinal
mass causing airway compression. Physical Examination Findings: Three weeks of progressively
worsening lymphadenopathy, coughing, night sweats, mild
History of Present Illness: The day before the unexpected urgent hepatosplenomegaly, and breathing difficulty when supine. The
glucose-6-phosphate dehydrogenase (G6PD) request, the patient was patient arrived at the medical center for airway management and had
diagnosed with an aggressive form of leukemia and a significant tumor a temperature of 36.1°C; blood pressure, 120/87 mmHg; pulse, 115
mass causing airway compression. A computed tomography (CT) scan bpm; respiratory rate, 22 breaths per minute, with labored breathing
indicated potential renal involvement. Based on this information and the but normal O2 saturation while upright and awake, in room air.
size of the mass, the patient was referred for immediate chemotherapy.
However, there was a concern that he could develop tumor lysis Principle Laboratory Findings: Table 1.
syndrome (TLS) during treatment. To avoid this condition, the pediatric
intensive care unit (ICU) sought to pretreat the child with rasburicase, Keywords: deficiency, glucose-6-phosphate dehydrogenase,
which led to the emergency G6PD request. leukemia, rasburicase, tumor lysis syndrome, uric acid
Questions
1. What are the most striking clinical and laboratory
findings for this patient?
2. Is there a legitimate concern that this patient could
develop tumor lysis syndrome (TLS)?
Abbreviations: 3. What are some treatment options for TLS?
ALL, acute lymphoblastic leukemia; G6PD, glucose-6-phosphate
dehydrogenase; CT, computed tomography; TLS, tumor lysis syndrome; 4. What could occur if this patient were deficient in
ICU, intensive-care unit; UA, uric acid; FDA, United States Food and
glucose-6-phosphate dehydrogenase (G6PD) after
Drug Administration; RBC, red blood cells; NADPH, nicotinamide
adenine dinucleotide phosphate; NA, not applicable; BUN, blood urea receiving rasburicase?
nitrogen.
5. Is it likely this patient has a G6PD deficiency?
Departments of 1Pathology and Area Laboratory Services and
2
Pediatrics, Brooke Army Medical Center, San Antonio, TX
6. What types of laboratory tests are helpful in confirming
*To whom correspondence should be addressed. a diagnosis of G6PD deficiency?
150 Lab Medicine Spring 2015 | Volume 46, Number 2 www.labmedicine.com
Case Studies
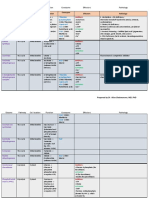
Table 1. Laboratory Findings on Admission for
Possible Answers the Patient, a 9-Year-Old African American Boy
Resulting Reference
1. On admission, the patient exhibited several mildly Test Value Interval Units
abnormal laboratory findings, among which were Chemistry
significantly elevated lactate dehydrogenase, uric acid (UA), Albumin 4.2 3.8-5.4 g/dL
and white blood cell count (Table 1). The hyperuricemia of Anion gap 21a 5-14 NA
BUN 14 8-23 mg/dL
the patient prompted the health care providers to administer
Calcium 10.2 8.8-10.8 mg/dL
Downloaded from https://academic.oup.com/labmed/article/46/2/150/2505057 by guest on 06 April 2023
chemotherapy immediately, to address the aggressive Chloride 95a 96-108 mmol/L
leukemia and to restore normal pulmonary function. CO2 18a 22-32 Mmol/L
Creatinine 0.5a 0.7-1.2 mg/dL
2. This patient is at high risk to develop potentially life- G6PD 13.0 7.0-20.5 U/g Hb
threatening TLS, a rare condition that often occurs after Glucose 64a 74-109 mg/dL
Lactate dehydrogenase 1152a 120-300 U/L
chemotherapeutic treatment1,2 of various malignant Phosphorus 3.3 3.0-5.4 mg/dL
neoplasms, especially high-grade lymphomas and Potassium 3.8 3.3-4.5 mmol/L
ALL.3 As its name implies, rapid tumor cell lysis often Sodium 134 133-145 mmol/L
results in elevated levels of UA and significant electrolyte Uric acid 8.6a 3.4-7.0 mg/dL
Hematology
imbalances (ie, potassium, phosphate, and calcium)
White blood cells 21.7a 4.5-13.5 ×103
that can result in crystal deposition in renal tubules and
NA, not applicable; BUN, blood urea nitrogen; G6PD, glucose-6-phosphate
culminate in acute renal failure.1,4 Once chemotherapy dehydrogenase.
a
Abnormal result.
began, we observed shifts in plasma calcium,
phosphorus, and UA levels, consistent with cellular lysis.
product allantoin but also produces hydrogen peroxide,
3. An effective clinical management strategy is to preclude
which can cause severe hemolysis and methemoglobinemia
TLS by concurrently administering intravenous fluids and
in patients with G6PD deficiency.6,7
hypouricemic drugs,5 which increase glomerular flow
and reduce the risk of crystal formation. Historically, the 5. G6PD deficiency is the most common type of enzyme
drug of choice was allopurinol, a competitive inhibitor of deficiency in humans, with an estimated 400 million
xanthine oxidase. In 2002, the United States Food and people affected worldwide. G6PD deficiency is an X-linked
Drug Administration (FDA) approved the use of rasburicase, inherited disorder most commonly affecting persons of
a recombinant urate oxidase that compensates for the African, Southeast Asian, and Mediterranean ethnicity.8,9
inability of the human body to express this enzyme.6 Use of The disease is usually more severe in individuals who
rasburicase in patients yields significantly faster reduction are homozygous for the deficiency. In the United States,
in uricemia and more efficient kidney function than use of African American males are most commonly affected, with
allopurinol in comparable patients.4 In our patient, judicious a prevalence of approximately 10% in that population.10
use of rasburicase resulted in the rapid reduction of UA Because our patient is male and African American, he had
levels and the avoidance of TLS. an increased likelihood of G6PD deficiency.
4. Rasburicase is contraindicated in patients with G6PD 6. Appropriate tests to screen for G6PD deficiency involve
deficiency because administration of this drug could cause assessing the endogenous RBC activity of the patient;
death.6 G6PD catalyzes the first step in the pentose- qualitative and quantitative laboratory tests are available for
phosphate pathway and is critical for red blood cells (RBCs) this purpose. The former test type is much more commonly
to generate the reduced form of nicotinamide adenine used; it is based on an ultraviolet fluorescence spot test.
dinucleotide phosphate (NADPH). Individuals with G6PD However, colloquially, these qualitative tests have been
deficiency are unable to produce sufficient NADPH to shown to lack sufficient sensitivity to identify many of the
maintain normal levels of reduced glutathione, making their moderate G6PD deficiencies in males or heterozygotic
RBCs highly susceptible to oxidative damage from certain females. Recently, a 62-year-old African American man with
drugs, ketoacidosis, infections, and ingestion of fava beans. leukemia was misdiagnosed as not having G6PD deficiency
Rasburicase reduces UA to the much more water-soluble due to the results of a spot test;6 after being administered
www.labmedicine.com Spring 2015 | Volume 46, Number 2 Lab Medicine 151
Case Studies
rasburicase, he developed fatal methemoglobinemia. In our
patient, a quantitative assay unequivocally showed that he
did not display G6PD deficiency.
Dedication
We are grateful to have worked with Joseph Andris, BS. To
all who knew him he was a divine inspiration and gallantly
Downloaded from https://academic.oup.com/labmed/article/46/2/150/2505057 by guest on 06 April 2023
remained an optimist until recently succumbing to the
scourge of cancer. LM
References
1. Davidson MB, Thakkar S, Hix JK, Bhandarkar ND, Wong A,
Schreiber MJ. Pathophysiology, clinical consequences, and
treatment of tumor lysis syndrome. Am J Med. 2004;116:546-554.
2. Cairo MS, Coiffier B, Reiter A, Younes A, TLS Expert Panel.
Recommendations for the evaluation of risk and prophylaxis of
tumour lysis syndrome (TLS) in adults and children with malignant
diseases: an expert TLS panel consensus. B J Haematol.
2010;149:578-586.
3. Wilson FP, Berns JS. Tumor lysis syndrome: new challenges and
recent advances. Adv Chronic Kidney Dis. 2014;21:18-26.
4. Sonbol MB, Yadav H, Vaidya R, Rana V, Witzig TE.
Methemoglobinemia and hemolysis in a patient with G6PD deficiency
treated with rasburicase. Am J Hematol. 2013;88:152-154.
5. Coiffier B, Altman A, Pui CH, Younes A, Cairo MS. Guidelines for
the management of pediatric and adult tumor lysis syndrome: an
evidence-based review. J Clin Oncol. 2008;26:2767-2778.
6. Bucklin MH, Groth CM. Mortality following rasburicase-induced
methemoglobinemia. Ann Pharmacother. 2013;47:1353-1358.
7. Arese P, Gallo V, Pantaleo A, Turrini F. Life and death of glucose-
6-phosphate dehydrogenase (G6PD) deficient erythrocytes–role
of redox stress and band 3 modifications. Tranfus Med Hemother.
2012;39:328-334.
8. Youngster I, Arcavi L, Schechmaster R, et al. Medications and
glucose-6-phosphate dehydrogenase deficiency: an evidence based
review. Drug Saf. 2010;33:713-726.
9. Elyassi AR, Rowshan HH. Perioperative management of the glucose-
6-phosphate dehydrogenase deficient patient: a review of the
literature. Anesth Prog. 2009;56:86-91.
10. Frank JE. Diagnosis and management of G6PD deficiency. Am Fam
Physician. 2005;72:1277-1282.
To read this article online, scan
the QR code, http://labmed.
ascpjournals.org/content/46/2/157.
full.pdf+html
152 Lab Medicine Spring 2015 | Volume 46, Number 2 www.labmedicine.com
You might also like
- Asidosis Laktat 2Document10 pagesAsidosis Laktat 2MizanMaulanaNo ratings yet
- Hypercalcemia, Acute Kidney Injury, and Esophageal LymphadenopathyDocument3 pagesHypercalcemia, Acute Kidney Injury, and Esophageal Lymphadenopathysar9203No ratings yet
- 2005 26 96-104 Jennifer M. Pearce and Richard H. Sills: Consultation With The Specialist: Childhood LeukemiaDocument11 pages2005 26 96-104 Jennifer M. Pearce and Richard H. Sills: Consultation With The Specialist: Childhood LeukemiaNathalie Soler BarreraNo ratings yet
- Chong 2018Document2 pagesChong 2018keisy MarquezNo ratings yet
- Clin Lab ElectrolytesDocument5 pagesClin Lab ElectrolytesPsyryst AlladoNo ratings yet
- Carrick 2018Document7 pagesCarrick 2018Edwin AlvarezNo ratings yet
- Glucogenosis CovidDocument5 pagesGlucogenosis CovidPaola Andrea MontoyaNo ratings yet
- Clinical Management of Hyperkalemia: ReviewDocument19 pagesClinical Management of Hyperkalemia: ReviewRawan KhateebNo ratings yet
- Nad Karni 2014Document2 pagesNad Karni 2014pedrotuliorochaNo ratings yet
- Laprosy Research Paper (Ahmed Tanjimul Islam)Document7 pagesLaprosy Research Paper (Ahmed Tanjimul Islam)AHMED TANJIMUL ISLAMNo ratings yet
- PKD BiochemistryDocument7 pagesPKD BiochemistryHyun Jae WonNo ratings yet
- CASE STUDY 11 411 5 and 12 2 12 3Document6 pagesCASE STUDY 11 411 5 and 12 2 12 3Florenz JoyNo ratings yet
- Management of G6PD Defecient PatientDocument6 pagesManagement of G6PD Defecient PatientRajesh T EapenNo ratings yet
- B2 PDFDocument9 pagesB2 PDFDr. Arvind YadavNo ratings yet
- Cancer Reports - 2022 - Boskabadi - Ifosfamide Induced Acute Kidney Injury in A Patient With Leiomyosarcoma A Case ReportDocument6 pagesCancer Reports - 2022 - Boskabadi - Ifosfamide Induced Acute Kidney Injury in A Patient With Leiomyosarcoma A Case ReportFreddy Shanner Chávez VásquezNo ratings yet
- Case Study For Colon CancerDocument2 pagesCase Study For Colon Cancerrhimineecat7150% (2)
- Artigo - Gitelman Syndrome ÍntegraDocument2 pagesArtigo - Gitelman Syndrome Íntegrasalvianolucas5No ratings yet
- Recurrent Nephrolithiasis in A 9-Year-Old Child: (University of North Carolina, Chapel Hill, NC)Document4 pagesRecurrent Nephrolithiasis in A 9-Year-Old Child: (University of North Carolina, Chapel Hill, NC)Shaysta KhanNo ratings yet
- CA A Cancer J Clinicians - 2018 - Zagzag - Hypercalcemia and Cancer Differential Diagnosis and TreatmentDocument10 pagesCA A Cancer J Clinicians - 2018 - Zagzag - Hypercalcemia and Cancer Differential Diagnosis and TreatmentWilliam Perero RodríguezNo ratings yet
- Referensi Nilai KritisDocument9 pagesReferensi Nilai KritisFaiz AchmadNo ratings yet
- J May Ocp 202006014Document19 pagesJ May Ocp 202006014Edwin Medicina DE UrgenciaNo ratings yet
- Ariceta, 2021Document13 pagesAriceta, 2021ValentinaNo ratings yet
- Nephrolithiasis in A 9 Year OldDocument4 pagesNephrolithiasis in A 9 Year OldJasmin Kae SistosoNo ratings yet
- Uric AcidDocument5 pagesUric AcidDr Alamzeb JadoonNo ratings yet
- ZH 800906003455Document8 pagesZH 800906003455Dung TranNo ratings yet
- Use of Conivaptan To Allow Aggressive Hydration To Prevent Tumor Lysis Syndrome in A Pediatric Patient With Large-Cell Lymphoma and SIADHDocument5 pagesUse of Conivaptan To Allow Aggressive Hydration To Prevent Tumor Lysis Syndrome in A Pediatric Patient With Large-Cell Lymphoma and SIADHmaryNo ratings yet
- Mahmud (2007) Coma With Diffuse White Matter Hemorrhages PDFDocument9 pagesMahmud (2007) Coma With Diffuse White Matter Hemorrhages PDFFelicia HarsonoNo ratings yet
- A Curious Case of QuadriplegiaDocument4 pagesA Curious Case of QuadriplegiaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Prevalence and Potential Risk Factors of Hypokalemia in Pediatric Patients With Diabetic KetoacidosisDocument2 pagesPrevalence and Potential Risk Factors of Hypokalemia in Pediatric Patients With Diabetic KetoacidosisAti Rahmi PurwandariNo ratings yet
- DKA ManagementDocument7 pagesDKA ManagementbababrijeshNo ratings yet
- 2482 8791 1 PBDocument2 pages2482 8791 1 PBMuhammad Irvan AvandiNo ratings yet
- Sulodexide For Kidney Protection in Type 2 Diabetes PatientsDocument8 pagesSulodexide For Kidney Protection in Type 2 Diabetes PatientsFerdinand YuzonNo ratings yet
- Diabetes y Quistes RenalesDocument11 pagesDiabetes y Quistes RenalesJairo StragaNo ratings yet
- JIFCC Lab Tests Interpretation 2018Document8 pagesJIFCC Lab Tests Interpretation 2018Abdul SattarNo ratings yet
- Hyperkalemia in Heart Failure Foe or FriendDocument10 pagesHyperkalemia in Heart Failure Foe or FriendRESIDENTES MEDICINA INTERNANo ratings yet
- A Model for Gene Therapy: Gene Replacement in the Treatment of Sickle Cell Anemia and ThalassemiaFrom EverandA Model for Gene Therapy: Gene Replacement in the Treatment of Sickle Cell Anemia and ThalassemiaNo ratings yet
- Estado Hiperglucémico Hiperosmolar: Una Forma Poco Frecuente de Inicio de La Diabetes Mellitus Tipo 1 en La InfanciaDocument2 pagesEstado Hiperglucémico Hiperosmolar: Una Forma Poco Frecuente de Inicio de La Diabetes Mellitus Tipo 1 en La InfanciaGabriel Davila CNo ratings yet
- Dickvet What Diagnosis April 2014Document6 pagesDickvet What Diagnosis April 2014VioletNo ratings yet
- I-131 Radiation-Induced Myelosuppression in Differentiated Thyroid Cancer TherapyDocument8 pagesI-131 Radiation-Induced Myelosuppression in Differentiated Thyroid Cancer TherapyRizqi AmaliaNo ratings yet
- HIgado GrasoDocument6 pagesHIgado GrasoWilson Suarez VenturaNo ratings yet
- Alcohol Abuse-Related Severe Acute Pancreatitis With Rhabdomyolysis ComplicationsDocument4 pagesAlcohol Abuse-Related Severe Acute Pancreatitis With Rhabdomyolysis ComplicationsMihai SebastianNo ratings yet
- 555-Article Text-4693-2-10-20201212Document7 pages555-Article Text-4693-2-10-20201212bboyhelyNo ratings yet
- Na Hypo MyxedemaDocument4 pagesNa Hypo Myxedemaanderson roberto oliveira de sousaNo ratings yet
- Hypocalcemia Pada Beta Thalassemia PDFDocument3 pagesHypocalcemia Pada Beta Thalassemia PDFYohana Elisabeth GultomNo ratings yet
- Acute Tumor Lysis SyndromeDocument3 pagesAcute Tumor Lysis SyndromeVincent SnansenNo ratings yet
- 2021 - Elbokl - Severe Caffeine Intoxication Treated With HemodialysisDocument4 pages2021 - Elbokl - Severe Caffeine Intoxication Treated With Hemodialysisamanda lssNo ratings yet
- Hyperkalemia CKDDocument23 pagesHyperkalemia CKDHend MahranNo ratings yet
- Elevated Liver Biochemistries in Hospitalized Chinese Patients With Severe COVID-19: Systematic Review and Meta-AnalysisDocument22 pagesElevated Liver Biochemistries in Hospitalized Chinese Patients With Severe COVID-19: Systematic Review and Meta-AnalysisPedro Luz da RosaNo ratings yet
- KDIGO Gitelman Conf ReportDocument10 pagesKDIGO Gitelman Conf Reportfelix tanzilNo ratings yet
- Hiperkalemia en ERDocument8 pagesHiperkalemia en ERmjbb1310No ratings yet
- Hyperkalemia Management in The Emergency Department: An Expert Panel ConsensusDocument8 pagesHyperkalemia Management in The Emergency Department: An Expert Panel ConsensusDaniel HeSaNo ratings yet
- Babesiosis As A Rare Cause of Fever in The Immunocompromised Patient: A Case ReportDocument5 pagesBabesiosis As A Rare Cause of Fever in The Immunocompromised Patient: A Case ReportDaniel Alfredo Galindo ChoqueNo ratings yet
- Case 1 CKDocument4 pagesCase 1 CKmcpaulfreemanNo ratings yet
- Lipodistrofia FamiliarDocument4 pagesLipodistrofia FamiliarKaren Magalí CruzNo ratings yet
- Diagnosis and Management of Bartter SyndromeDocument12 pagesDiagnosis and Management of Bartter SyndromeMercedes Monserrath Garcia MorenoNo ratings yet
- Oxidative Dna Damage in Patients With Type 2 Diabetes MellitusDocument7 pagesOxidative Dna Damage in Patients With Type 2 Diabetes MellitusmuniraliiNo ratings yet
- Clinchem 1565Document4 pagesClinchem 1565ghfkhgfjhfgNo ratings yet
- Renal CaseDocument3 pagesRenal CaseAndy BiersackNo ratings yet
- Case Studies: Recurrent Fever, Chills, and Malaise in A 53-Year-Old ManDocument2 pagesCase Studies: Recurrent Fever, Chills, and Malaise in A 53-Year-Old Mansreeja maragoniNo ratings yet
- Chem 1223Document5 pagesChem 1223Ramil LucasNo ratings yet
- Coenzyme CofactorDocument13 pagesCoenzyme CofactorGabriel RamosNo ratings yet
- 11-01 Amino Acids - Nitrogen DisposalDocument53 pages11-01 Amino Acids - Nitrogen DisposalFrankenstein MelancholyNo ratings yet
- Fatty Acid BiosynthesisDocument7 pagesFatty Acid BiosynthesisJeremiah Eyo AmanamNo ratings yet
- Beckers World of Cell Chapter 2 Questions and AnswersDocument30 pagesBeckers World of Cell Chapter 2 Questions and AnswersiremsenakNo ratings yet
- Pentose Phosphate PathwayDocument2 pagesPentose Phosphate PathwayGianneCarloGomedNo ratings yet
- Photosynthesis: Multiple ChoiceDocument23 pagesPhotosynthesis: Multiple ChoiceValentina RumhizhaNo ratings yet
- Angelo BanaresDocument11 pagesAngelo BanaresNathan Russel PangilinanNo ratings yet
- List of AbbreviationsDocument3 pagesList of Abbreviationsjuwita latiefahNo ratings yet
- The Performance of A Cyanobacterial Biomass-Based Microbial Fuel Cell (MFC)Document30 pagesThe Performance of A Cyanobacterial Biomass-Based Microbial Fuel Cell (MFC)Muhamad SuharNo ratings yet
- J Parenter Enteral Nutr - 2015 - Frank - Thiamin in Clinical PracticeDocument18 pagesJ Parenter Enteral Nutr - 2015 - Frank - Thiamin in Clinical Practicejuhh tavaresNo ratings yet
- Dark ReactionDocument13 pagesDark ReactionAnazAsharafANo ratings yet
- BCHEM 254 Metabolism of Nutrients II-Lecture 1 20180121-1Document140 pagesBCHEM 254 Metabolism of Nutrients II-Lecture 1 20180121-1Nicholas BoampongNo ratings yet
- Biology - XI - Photosynthesis in Higher Plants - MCQs 1Document105 pagesBiology - XI - Photosynthesis in Higher Plants - MCQs 1SDO BSNL NALAGARHNo ratings yet
- NRF 2 ChapterDocument29 pagesNRF 2 Chaptercychiu1215No ratings yet
- Laboratory Memory 2Document13 pagesLaboratory Memory 2Candela Sierra MoralesNo ratings yet
- Important EnzymesDocument15 pagesImportant EnzymesErin HillNo ratings yet
- Biology National MDCAT FLP # 1Document22 pagesBiology National MDCAT FLP # 1Salam FatimaNo ratings yet
- AOAC 2020.08 Lactose Concentration in Milk, Milk Products and Dairy Ingredients by Megazyme Test KitDocument7 pagesAOAC 2020.08 Lactose Concentration in Milk, Milk Products and Dairy Ingredients by Megazyme Test KitdcardonasterNo ratings yet
- Metabolism Complete Notes #KigogoDocument145 pagesMetabolism Complete Notes #KigogoHesbone AneneNo ratings yet
- Vitamins As Coenzymes CofactorsDocument5 pagesVitamins As Coenzymes CofactorssharenNo ratings yet
- Module Trial STPM Biology Term 1 2022 Set 2Document9 pagesModule Trial STPM Biology Term 1 2022 Set 2RuoQi LeeNo ratings yet
- Brahmastra 19 02 2023Document53 pagesBrahmastra 19 02 2023Vaibhav Kumar SinghNo ratings yet
- Biochemistry 1001 Reviewand Viva Voce Qand ADocument13 pagesBiochemistry 1001 Reviewand Viva Voce Qand AKhadija BukhadNo ratings yet
- Bio 212 Physiology 2021Document17 pagesBio 212 Physiology 2021Bello AjetayoNo ratings yet
- Ch. 14Document153 pagesCh. 14sgarcia2156No ratings yet
- 02.determinants of Crop YieldDocument49 pages02.determinants of Crop YieldGAMUCHIRAI MUGADZANo ratings yet
- BotanyDocument6 pagesBotanyCyrill Mae MagallonNo ratings yet
- g6pd Group 5 A2Document39 pagesg6pd Group 5 A2Kristian CadaNo ratings yet
- Biochemistry A Short Course 3rd Edition Ebook PDF VersionDocument61 pagesBiochemistry A Short Course 3rd Edition Ebook PDF Versionramona.evans546100% (45)