Professional Documents
Culture Documents
Case 10 Fever PDF
Uploaded by
Sue HuangOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case 10 Fever PDF
Uploaded by
Sue HuangCopyright:
Available Formats
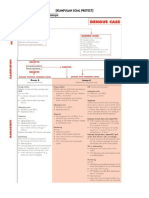
Case 10
6-MONTH-OLD WITH A FEVER - HOLLY
Author: Christopher White, M.D., Medical College of Georgia Case Objectives 1. Meningitis must be considered in the differential diagnosis of any febrile infant, regardless of the presence or absence of meningeal signs. 2. The only reliable way to rule out meningitis in a febrile infant less than 12 months of age is with a lumbar puncture. 3. Urinary tract infections should be considered in the differential diagnosis of any febrile infant with a non-focal History and Physical Examination. 4. The only reliable method of diagnosing a urinary tract infection in an infant is a urine culture from a catheterized specimen (urine cultures obtained from bag specimens are unreliable). 5. Empiric antibiotic therapy for an infant or young child with an uncomplicated urinary tract infection should cover predominantly enteric gram-negative bacilli, particularly E. coli. Infants with severe symptoms should receive parenteral antibiotics. 6. All infants with a urinary tract infection need to have an evaluation of their genitourinary tract. This consists of an abdominal and pelvic ultrasound, and a voiding cystourethrogram (VCUG). Summary of Clinical Scenario: 6 month old Holly has had a fever for 2 days, is fussy and not eating. Her review of symptoms is negative. There are no focal findings on physical exam, including negative Kernigs Brudzinkis signs. Elevated WBC with left shift suggests bacterial infection but normal chest X-ray rules out pneumonia and normal CSF rules out meningitis. Leukocytes and nitrite in the urine strongly suggests a bacterial UTI.
Fever for two days Fussy
Key Findings from History
Poor appetite Absence of coryza/cough Absence of vomiting/diarrhea
Non-focal PE
Key Findings from Physical Exam
(-) Kernigs and Brudzinskis signs Tachycardia Tachypnea
URI Gastroenteritis
Differential Diagnosis
Otitis media Meningitis UTI Pneumonia
Elevated WBC
Key Findings from Testing
Normal CSF Leukocytes/nitrite in urine, Normal CXR
Final Diagnosis
UTI with pyelonephritis
Case Highlights: Students learn to narrow the diagnosis for fever using targeted questions to the mother, and by using lab and imaging studies. They learn about the Yale Infant Observation Scale, and how to perform and interpret maneuvers to elicit Kernig's and Brudzinki's signs. The case teaches how to interpret Holly's CBC and dipstick urinalysis, leading to a diagnosis of UTI. Students then learn guidelines for admitting a child with a UTI, and which antibiotics to prescribe for treating the acute symptoms and providing later prophylaxis. Information on tests for renal scarring is also provided. Multimedia features include: image of dipstick and its interpretation, voiding cystourethrogram.
Key Teaching Points
Knowledge:
Definitions for Fever Conditions Fever - 100.5F, or 38.0C. Bacteremia - presence of viable bacteria in circulating blood. Septicemia - systemic disease caused by multiplication of microorganisms in the circulating blood. Fever Without Source (FWS) - fever with no apparent focus of infection after careful Hx and PE. Fever of Unknown Origin is a fever of at least two weeks duration with failure to reach a diagnosis after one week of evaluation. Occult bacteremia (OB) - pathogenic bacterial species in blood cx from child not suspected of having a bacterial infection based on history, physical examination, and screening laboratory tests, including chest X-ray, lumbar puncture, and urinalysis. OB occurs in febrile infants birth to 3 yo. Serious bacterial Illness (SBI) - bacteremia, bacterial meningitis, bacterial enteritis, pneumonia, sepatientic arthritis, osteomyelitis, and cellulitis.
Skills:
History and Physical Exam: Meningeal Signs ("meningismus") - physical findings after meningeal irritation from inflammation, tumor or hemorrhage. Basis for tests is to see if patient rejects any
movement that stretches spinal nerves, which pass through the irritated subarachnoid space. 1. Neck Stiffness ("nuchal rigidity") - involuntary resistance to neck flexion. Clinician flexes patient's neck forward. In severe cases, increased extensor tone of neck and spine leads to hyperextension of entire spine, or "opisthotonus." 2. Kernig's Sign - Flex patient's hips and extend knees, and see if patient resists knee extension from this position. (+) Kernig's sign when patient resists extension. 3. Brudzinski's Sign - flex supine patient's neck, and see if patient flexes both hips and knees. (+) Brudzinski's if patient retracts legs toward the chest. (Reference: McGee, S. Evidence-Based Physical Diagnosis. Philadelphia, Pennsylvania: W.B. Saunders Company. 2001: 303-304.) Differential Diagnosis: UTI - consider in patients two months two years with unexplained fever, non-focal Hx and PE. Consider degree of toxicity, dehydration, and ability to retain oral intake. In this case UTI likely since UA abnormal, elevated WBC, and absence of physical findings suggesting other causes. Based on high WBC and fever, she may have an upper UTI (pyelonephritis). Gastroenteritis - Viral or bacterial gastroenteritis may cause high fever, but would expect to see vomiting and/or diarrhea by 2nd day of illness. URI - Infants with viral URI may present with a high fever, but diagnosis unlikely because no cough, congestion or coryza. AOM - ruled out by PE. Meningitis - Must consider in any febrile infant, regardless of presence or absence of meningeal signs. The only reliable way to R/O meningitis in febrile infant <12 mos old is with LP. In this case, meningitis is possible, need to R/O by LP as normal CSF rules out this diagnosis. Pneumonia - Most infants with pneumonia have cough and/or tachypnea, but fever may be only presenting sx. Even though chest exam normal, still consider pneumonia. However, pneumonia very unlikely with normal CXR. URI - Viral URI unlikely due to the negative history and PE, and elevated WBC. Studies: Diagnostic Tests 1. CXR - Bacterial pneumonia is possible in any ill-appearing infant with a fever for several days, even in the absence of respiratory symptoms or abnormal pulmonary findings. Most clinicians would consider getting obtaining a CXR in this setting. 2. CBC A total WBC > 15,000 cells/mm3 with a "left shift" suggests a possible serious bacterial infection, although the predictive value of this finding is low. Most viral infections have normal WBC and differential. 3. UA Positive nitrate, leukocyte esterase, and blood strongly suggest bacterial UTI. Urine specimens obtained by bags have high rate of contamination. Therefore, get catheterized sample when need to R/O UTI in child who is not toilettrained. (+) Nitrite in UA highly specific for bacteruria (few false positives). A negative nitrite has very poor sensitivity (lots of false negatives) for bacteruria or infection. (+) leukocyte esterase detects esterases released from broken-down leukocytes. (+) test usually indicates presence of WBCs in urine (pyuria), but it can be seen in a variety of conditions besides UTI. Thus, (+) leukocyte insufficient to make UTI diagnosis.
4. Lumbar Puncture Indications - examine spinal fluid for suspected infection or malignancy, instill intrathecal chemo, measure opening pressure. Some perform LPs in any febrile young infant (<6 mos old) who has no obvious focus of infection. Others only perform when infant is toxicappearing, or laboratory studies suggesting serious bacterial infection (i.e., WBC > 15,000 with a "left shift," or temperature >40 with no obvious other focus for infection). General rule - if going to treat any febrile young infant with parenteral antibiotics for a "presumed" bacterial infection, LP should be done. Contraindications/Cautions 1. Increased intracranial pressure - before LP, look for evidence of high ICP (papilledema, retinal hemorrhage). 2. Bleeding diathesis - platelet count should be >50,000 before LP. 3. Overlying skin infection 4. Unstable patients (Reference: Harriet Lane, 16th Ed.) 5. Voiding cysturethrogram (VCUG). Recommended for all infants after their first UTI. "Backwash" of urine from bladder into ureter or kidney due to incompetent ureterovesical junction. Most VUR cases mild and resolve spontaneously. In up to 50% of patients < 1 yo with UTI. Patients with VUR have increased risk recurrent UTIs, so often placed on prophylactic abx until reflux has resolved or been surgically corrected. Potential complication - renal scarring due to high pressures during voiding and repeated episodes pyelonephritis. Diagnosis Vesicoureteral reflux (VUR) 6. Abdominal ultrasound Necessary to perform on all infants after their first UTI. Provides information about renal structure and dilations in the collecting system.
Management:
UTI Abx Tx If patient does not appear ill but has (+) urine cx, start IV or po abx. Empiric abx for an infant or young child with uncomplicated UTI should cover predominantly enteric gram-negative bacilli, particularly E. coli. Infants with severe symptoms should receive IV abx. If patient with suspected UTI is toxic, dehydrated, or unable to retain oral intake, initiate abx and consider hospitalization. If patient not responsive to abx after 2 days, reevaluate and repeat urine cx. All patients with UTI should complete a 7- to 14-day abx course orally. After 7- to 14-day course of abx, patients with UTI should be on abx until the imaging studies completed. Other Studies - all infants with UTI need eval of GU tract, which includes abdominal and pelvic U/S, and voiding cystourethrogram (VCUG). Indications for Inpatient Tx Toxic appearance, dehydration, or inability to retain oral intake. Evidence of: clinical urosepsis, bacteremia. Antibiotics for Pyelonephritis IV Antibiotics
In a child who has not been on prophylactic abx, most likely cause of an initial episode of pyelonephritis is E. coli, with the remainder of cases caused by other enteric gram-negative organisms or enterococci. Ampicillin and gentamicin are still the antibiotics of choice for IV treatment of UTI. Ceftriaxone has excellent coverage against most gram-negative bacilli (except Pseudomonas aeruginosa and enterococci), and has excellent safety profile in children. Ciprofloxacin can be used, but expensive and potential adverse reactions in children, particularly damage to articular cartilage, especially the knee (usually not permanent). Should not be routinely used in children <16 yo. PO Antibiotics after D/C for Pyelonephritis Trimethoprim/Sulfamethoxazole (TMP/SMZ) good choice because it's inexpensive, well tolerated, and requires only twice-daily dosing. Rare problems include serious skin reactions. Ampicillin/clavulanate (Augmentin) okay, but much more expensive than TMP/SMZ. Nitrofurantoin recommended for lower UTI, not pyelonephritis. Sulfisoxazole should not be used because of resistance. Followup for pyelonephritis 1. 2. 3. 4. Voiding Cystourethrogram (VCUG) Abdominal Ultrasound Urinalysis for any febrile incidents without clear focus Periodic radionuclide cystogram to follow vesicoureteral reflux (VUR)
Web links: CDC sites on the National Immunization Program and adverse event report system National Network for Immunization Information Web site (current info on vaccines) Immunization Action Coalition Web site CDC's The Pink Book (Epidemiology and Prevention of Vaccine-Preventable Diseases) The CDC's Vaccine Adverse Event Reporting System Article on using the Yale Infant Observation Scale Article on meningitis and how to use Kernig's and Brudzinski's maneuvers to diagnose the disease AAP practice guideline diagnosing and treating the initial UTI in febrile infants and young children A Web site that explains voiding cystourethrogram as you might describe it to a parent (Cincinnati Children's Hospital Medical Center) AAP parent handout on UTIs in children
Back to Top Copyright 2011 iInTIME. All Rights Reserved.
You might also like
- Guide to Pediatric Urology and Surgery in Clinical PracticeFrom EverandGuide to Pediatric Urology and Surgery in Clinical PracticeNo ratings yet
- 8 Day Urinary Tract InfectionDocument9 pages8 Day Urinary Tract InfectionShreyash HaritwalNo ratings yet
- Pediatric Urinary Tract Infection: Practice EssentialsDocument14 pagesPediatric Urinary Tract Infection: Practice EssentialsPutu Arimarta Irianta HerosNo ratings yet
- Pediatric Urinary Tract InfectionDocument29 pagesPediatric Urinary Tract InfectionFenty IswarNo ratings yet
- Study of Clinical Etiological and Radiological Profile of UTI CasesDocument8 pagesStudy of Clinical Etiological and Radiological Profile of UTI CasesDebabrata MohapatraNo ratings yet
- Pelvic MassesDocument15 pagesPelvic MassesJulia kwapeNo ratings yet
- Journal Reading UTIDocument25 pagesJournal Reading UTIBourbon ZeroNo ratings yet
- 299-Article Text-633-1-10-20200912Document5 pages299-Article Text-633-1-10-20200912daily of sinta fuNo ratings yet
- 4 PART 2 Nursing Management of Newborn at Risk 2nd Semester 1Document20 pages4 PART 2 Nursing Management of Newborn at Risk 2nd Semester 1ammarNo ratings yet
- Current Approach To The Diagnosis and Emergency Department Management of Appendicitis in ChildrenDocument6 pagesCurrent Approach To The Diagnosis and Emergency Department Management of Appendicitis in ChildrenmaithamNo ratings yet
- Clinical Overview IvuDocument45 pagesClinical Overview IvularevalomunozNo ratings yet
- Uti 1Document75 pagesUti 1Muwanga faizoNo ratings yet
- Necrotizing EnterocolitisDocument7 pagesNecrotizing EnterocolitisWardah AlAkrahNo ratings yet
- Clinical Therapy of UTI in Children Under The Age of Five Varies WidelyDocument21 pagesClinical Therapy of UTI in Children Under The Age of Five Varies WidelyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Urinary Tract InfectionDocument30 pagesUrinary Tract InfectionMedita PrasetyoNo ratings yet
- 3 Common Pediatric Surgery ContinuedDocument5 pages3 Common Pediatric Surgery ContinuedMohamed Al-zichrawyNo ratings yet
- Acute Abdominal Pain InInfants and ChildrenDocument14 pagesAcute Abdominal Pain InInfants and Childrenemergency.fumcNo ratings yet
- Soal Dan Pembahasan Pretest IRDocument16 pagesSoal Dan Pembahasan Pretest IRSummer SnowNo ratings yet
- Virology CaseDocument6 pagesVirology CaseGus AbellaNo ratings yet
- Urinary Tract Infection in ChildrenDocument17 pagesUrinary Tract Infection in Childrendeladestianiaji2490No ratings yet
- JHACH UTI Clinical PathwayDocument13 pagesJHACH UTI Clinical PathwayRyeowook RyeNo ratings yet
- Neonatal SepsisDocument5 pagesNeonatal SepsisLeana SiñelNo ratings yet
- Urinary Tract Infection in Children - ClinicalKeyDocument60 pagesUrinary Tract Infection in Children - ClinicalKeylarevalomunozNo ratings yet
- Appendicitis CaseDocument8 pagesAppendicitis CaseStarr NewmanNo ratings yet
- Obstetrics Patient M.L. 26/F Date Admitted: December 17, 2018 Date Discharged: December 19, 2018 Informant: Patient Reliability: 80%Document6 pagesObstetrics Patient M.L. 26/F Date Admitted: December 17, 2018 Date Discharged: December 19, 2018 Informant: Patient Reliability: 80%Justin LamNo ratings yet
- Neonatal Sepsis 1219225703095484 9Document50 pagesNeonatal Sepsis 1219225703095484 9Ali FalihNo ratings yet
- Urinecollectionmethodsin Children:: Which Is The Best?Document7 pagesUrinecollectionmethodsin Children:: Which Is The Best?endah dwi cahyaniNo ratings yet
- AppendicitisDocument14 pagesAppendicitisMary Joy BunuanNo ratings yet
- M.D Pediatrics PH.D Pediatric Special Need and Nutrition Consultant Mansoura National Hospital Insurance H Fever H and Egyptian Liver HDocument49 pagesM.D Pediatrics PH.D Pediatric Special Need and Nutrition Consultant Mansoura National Hospital Insurance H Fever H and Egyptian Liver HMona MostafaNo ratings yet
- Module 14 Pediatric TB ENGLISHDocument85 pagesModule 14 Pediatric TB ENGLISHDellNo ratings yet
- Case ManagementDocument11 pagesCase ManagementGabrielle CatalanNo ratings yet
- Pediatric (S) 2023 Final 7th SemDocument226 pagesPediatric (S) 2023 Final 7th SemSyed NoorNo ratings yet
- 393 FullDocument10 pages393 FullMateen ShukriNo ratings yet
- Aafp Uti GuidelinesDocument10 pagesAafp Uti GuidelinesCess Lagera YbanezNo ratings yet
- Case PressDocument9 pagesCase PresskerbyannmNo ratings yet
- Pediatric Appendicitis Clinical Presentation - History, Physical ExaminationDocument5 pagesPediatric Appendicitis Clinical Presentation - History, Physical ExaminationBayu Surya DanaNo ratings yet
- Referat UtiDocument20 pagesReferat UtiYeni Rosa SitohangNo ratings yet
- 18-Month-Old Boy With Abdominal Pain and Rectal Bleeding BackgroundDocument5 pages18-Month-Old Boy With Abdominal Pain and Rectal Bleeding Backgroundcamille nina jane navarroNo ratings yet
- Typhoid Fever With Acute Pancreatitis in A Five-Year-Old ChildDocument2 pagesTyphoid Fever With Acute Pancreatitis in A Five-Year-Old Childnurma alkindiNo ratings yet
- PPT-Acute PyeloDocument117 pagesPPT-Acute PyeloJudy UrciaNo ratings yet
- Urinary Tract Infection: Mentor DR - SaralaDocument53 pagesUrinary Tract Infection: Mentor DR - SaralaMimi Suhaini SudinNo ratings yet
- Journal Reading AnakDocument19 pagesJournal Reading AnakPutra Priambodo WibowoNo ratings yet
- Neonatal SepsisDocument5 pagesNeonatal SepsisBhawna PandhuNo ratings yet
- Sepsis NeonatorumDocument3 pagesSepsis NeonatorumKim TranateNo ratings yet
- Diseases, Syndromes & Health Events Under SurveillanceDocument61 pagesDiseases, Syndromes & Health Events Under SurveillanceGina BoligaoNo ratings yet
- Gi QodDocument67 pagesGi QodAmmar AlnajjarNo ratings yet
- Absceso Hepático NeonatalDocument6 pagesAbsceso Hepático NeonatalNabila Peña ZapataNo ratings yet
- Urinary Tract Infections in Neonates With Unexplained Pathological Indirect Hyperbilirubinemia: Prevalence and SignificanceDocument5 pagesUrinary Tract Infections in Neonates With Unexplained Pathological Indirect Hyperbilirubinemia: Prevalence and SignificancePutri YingNo ratings yet
- Infection Urinaire 2019Document11 pagesInfection Urinaire 2019KhaoulapediatreNo ratings yet
- Pediatrics Nursing DisordersDocument9 pagesPediatrics Nursing DisordersAli IgnacioNo ratings yet
- Comparison Between Small and Large Bowel Intussusception in ChildrenDocument3 pagesComparison Between Small and Large Bowel Intussusception in ChildrenParamartha KesumaNo ratings yet
- Patient Scenario, Chapter 45, Nursing Care of A Family When A Child Has A Gastrointestinal DisorderDocument93 pagesPatient Scenario, Chapter 45, Nursing Care of A Family When A Child Has A Gastrointestinal DisorderDay MedsNo ratings yet
- All Peads SEQsDocument14 pagesAll Peads SEQsShifa AminNo ratings yet
- Neonatal Necrotizing Enterocolitis: Clinical Challenges, Pathophysiology and ManagementDocument10 pagesNeonatal Necrotizing Enterocolitis: Clinical Challenges, Pathophysiology and ManagementFahmi SyarifNo ratings yet
- An Antenatal Appearance of Megacystis-Microcolon-Intestinal Hypoperistalsis SyndromeDocument8 pagesAn Antenatal Appearance of Megacystis-Microcolon-Intestinal Hypoperistalsis SyndromeserubimNo ratings yet
- Neonatal Bacterial InfectionDocument8 pagesNeonatal Bacterial InfectionNuurNo ratings yet
- Kırşehir Ahi Evran Üniversitesi Sağlık Bilimleri Enstitüsü: Neonatal Sepsis & MeningitisDocument40 pagesKırşehir Ahi Evran Üniversitesi Sağlık Bilimleri Enstitüsü: Neonatal Sepsis & MeningitisAli FalihNo ratings yet
- UTI GuidelinesDocument7 pagesUTI GuidelinesstarkNo ratings yet
- NIH Public Access: Author ManuscriptDocument12 pagesNIH Public Access: Author ManuscriptadipurnamiNo ratings yet
- GIS-K-25 Acute Appendicitis Appendiceal Mass / AbscessDocument24 pagesGIS-K-25 Acute Appendicitis Appendiceal Mass / AbscessYasmine Fitrina SiregarNo ratings yet
- All India Quota Medical Seats (MBBS) With AIPMT 2015 Score PDFDocument5 pagesAll India Quota Medical Seats (MBBS) With AIPMT 2015 Score PDFjuhiNo ratings yet
- Cardiovascular Pharmacology: DR Muhamad Ali Sheikh Abdul Kader MD (Usm) MRCP (Uk) Cardiologist, Penang HospitalDocument63 pagesCardiovascular Pharmacology: DR Muhamad Ali Sheikh Abdul Kader MD (Usm) MRCP (Uk) Cardiologist, Penang HospitalCvt RasulNo ratings yet
- Sample UploadDocument14 pagesSample Uploadparsley_ly100% (6)
- CO2 & SelexolDocument18 pagesCO2 & Selexolmihaileditoiu2010No ratings yet
- Case Diagnosis For RomanDocument4 pagesCase Diagnosis For RomanChris Marie JuntillaNo ratings yet
- File3 PDFDocument119 pagesFile3 PDFikkemijnnaam0% (1)
- Aircraft Noise Management: Graduation Project Defense For The Diploma of Air Traffic Management EngineerDocument46 pagesAircraft Noise Management: Graduation Project Defense For The Diploma of Air Traffic Management Engineerchouchou chamaNo ratings yet
- Operator's Manual: SE Series Slab ScissorsDocument52 pagesOperator's Manual: SE Series Slab ScissorsthuanNo ratings yet
- Energies: Numerical Simulations On The Application of A Closed-Loop Lake Water Heat Pump System in The Lake Soyang, KoreaDocument16 pagesEnergies: Numerical Simulations On The Application of A Closed-Loop Lake Water Heat Pump System in The Lake Soyang, KoreaMvikeli DlaminiNo ratings yet
- Retrenchment in Malaysia Employers Right PDFDocument8 pagesRetrenchment in Malaysia Employers Right PDFJeifan-Ira DizonNo ratings yet
- Level 9 - Unit 34Document7 pagesLevel 9 - Unit 34Javier RiquelmeNo ratings yet
- ECO-321 Development Economics: Instructor Name: Syeda Nida RazaDocument10 pagesECO-321 Development Economics: Instructor Name: Syeda Nida RazaLaiba MalikNo ratings yet
- Task 2: Health Services Survey: School Community 1. What Are The Health Services Provided?Document1 pageTask 2: Health Services Survey: School Community 1. What Are The Health Services Provided?Bernadeth BaiganNo ratings yet
- Chem Sba 2019-2020Document36 pagesChem Sba 2019-2020Amma MissigherNo ratings yet
- Datasheet Cofraplus 60Document2 pagesDatasheet Cofraplus 60Žarko JanjićNo ratings yet
- Vulnerability of The Urban EnvironmentDocument11 pagesVulnerability of The Urban EnvironmentKin LeeNo ratings yet
- Upper Gi f1 Survival GuideDocument1 pageUpper Gi f1 Survival GuideNathan Hovis JeffreysNo ratings yet
- Aphids and Ants, Mutualistic Species, Share A Mariner Element With An Unusual Location On Aphid Chromosomes - PMCDocument2 pagesAphids and Ants, Mutualistic Species, Share A Mariner Element With An Unusual Location On Aphid Chromosomes - PMC2aliciast7No ratings yet
- .. - Bcsbi - .Document2 pages.. - Bcsbi - .Varun GopalNo ratings yet
- Timberwolf TW 230DHB Wood Chipper Instruction ManualDocument59 pagesTimberwolf TW 230DHB Wood Chipper Instruction Manualthuan100% (1)
- CA500Document3 pagesCA500Muhammad HussainNo ratings yet
- Campus DrinkingDocument2 pagesCampus DrinkingLiHertzi DesignNo ratings yet
- Materials Management in Hospital Industry Nandi ProjectDocument27 pagesMaterials Management in Hospital Industry Nandi Projectkumaraswamy226No ratings yet
- Articulo de Las 3 Tesis Por BrowDocument30 pagesArticulo de Las 3 Tesis Por BrowJHIMI DEIVIS QUISPE ROQUENo ratings yet
- Gulayan Sa Barangay OrdinanceDocument2 pagesGulayan Sa Barangay OrdinancekonsinoyeNo ratings yet
- RA 9344 (Juvenile Justice and Welfare Act)Document10 pagesRA 9344 (Juvenile Justice and Welfare Act)Dan RamosNo ratings yet
- Sheehan SyndromeDocument6 pagesSheehan SyndromeArvie TagnongNo ratings yet
- A Guide To LU3 PDFDocument54 pagesA Guide To LU3 PDFMigs MedinaNo ratings yet
- Variant Perception - Recessions and ShocksDocument15 pagesVariant Perception - Recessions and ShocksVariant Perception Research80% (5)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (29)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- Troubled: A Memoir of Foster Care, Family, and Social ClassFrom EverandTroubled: A Memoir of Foster Care, Family, and Social ClassRating: 4.5 out of 5 stars4.5/5 (27)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (59)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (45)