Professional Documents
Culture Documents
Laan 2020
Uploaded by
clauxavOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Laan 2020
Uploaded by
clauxavCopyright:
Available Formats
News and Opinions
“No-ICU-Unless” Policy for Tumor Craniotomy
Mark ter Laan and Ronald HMA Bartels
During postoperative outpatient visits of oncology patients, we need for standard ICU admission after tumor craniotomy. We
often ask how they have experienced the perioperative period. have introduced a “no-ICU-unless” policy and compared length
Most are surprised by the fact that everything went so well and that of stay, costs, patient satisfaction, and complications with 1 year
they could leave the hospital a couple of days after surgery. The before introduction. We have shown that patients were satisfied
only thing that had bothered them was the stay in the intensive with this changed postoperative regimen. Furthermore,
care unit (ICU). They experienced a noisy, busy, and stressful complications were not increased and costs were reduced.
environment that contributed to disturbed sleep. These patient One could question which criteria should be used to select
testimonials have generated 2 important questions: 1) Why are we patients who should and who should not have intensive moni-
still surprised that patients are dismissed after a tumor craniotomy toring postoperatively. Possibly randomized trials, prospective
within 2 or 3 days and 2) if the ICU stay is so stressful, do we still registries, or other studies could help identify these criteria more
need this? specifically. On the basis of our findings, it is unlikely that others
Brain surgery used to be extremely risky with high morbidity will show that standard postoperative ICU admittance for all tu-
and mortality. This has improved since the introduction of peri- mor craniotomy cases will be either significantly safer or more
operative corticosteroid use and further with advancements made cost-effective. Therefore we propose not to wait for further studies
in anesthesiologic and surgical techniques. Nevertheless, we seem on this matter but rather to adopt the pragmatic approach of our
to uphold the idea of a “risky business.” Maybe the devastating “no-ICU-unless” policy. In short, this means that patients with a
effects of eventual complications overshadow the enormous supratentorial craniotomy do not need ICU admission unless high
decrease in complication rates. The psychologic impact of this blood loss or long (>6 hours) surgery is anticipated by the surgeon
kind of surgery certainly affects doctors and, especially, patients or unless anesthesiologists find the need for extra monitoring
and their relatives’ expectations regarding risks. The psychologic based on American Society of Anesthesiologists score or
burden will not be decreased by a standard admission to the ICU functional status. We do recommend involving nursing staff in
but should be managed by listening to the fears and worries of our changing perioperative regimen and increasing check-ups and
patients. Empathetic doctors and nurses can manage expectations monitoring possibilities in the ward for the first 6 hours. We
and are of utmost importance to decrease the psychologic impact hypothesize that such a policy would suit other patients
associated with any kind of brain surgery. (infratentorial lesions) as well.
Therefore we asked ourselves: Do we need intensive post- We live in a time where we need to be more and more conscious
operative care after tumor craniotomy as a default for all patients? about the costs of health care. The concept of “just to be on the
As described in our recent publication,1 we set out to check some safe side” does not seem to suit this era. As we have shown,
600 recent tumor cases for serious complications and hardly found patient satisfaction can be improved and costs can be reduced
any. In 1 of the complicated cases, postoperative hematoma did not without increasing complication rates. To recognize these kinds of
occur until day 2, when the patient was already readmitted to the opportunities, we should reconsider habits based on concepts that
normal neurosurgical ward. The low incidence of serious are no longer valid. A skeptical and open-minded attitude toward
complications in combination with the realization that they occur everything we have become used to do is paramount in order to be
after postoperative day 1 as well reinforced our doubt for the able to recognize and change these habits.
craniotomy: complications, length of stay, and Department of Neurosurgery, Radboud University Medical
REFERENCE costs. Neurosurgery. 2020;86:E54-E59. Center, Nijmegen, The Netherlands
1. Ter Laan M, Roelofs S, Van Huet I, Adang EMM, 1878-8750/$ - see front matter ª 2020 Elsevier Inc. All
Bartels RHMA. Selective intensive care unit rights reserved.
admission after adult supratentorial tumor https://doi.org/10.1016/j.wneu.2020.01.099
406 www.SCIENCEDIRECT.com WORLD NEUROSURGERY, https://doi.org/10.1016/j.wneu.2020.01.099
You might also like
- Case Studies of Postoperative Complications after Digestive SurgeryFrom EverandCase Studies of Postoperative Complications after Digestive SurgeryNo ratings yet
- Asa 2013Document1,076 pagesAsa 2013Marwa Mahrous100% (4)
- Technical Aspects of Focal Therapy in Localized Prostate CancerFrom EverandTechnical Aspects of Focal Therapy in Localized Prostate CancerEric BarretNo ratings yet
- Guidance For Return To Practice For Otolaryngology-Head and Neck SurgeryDocument10 pagesGuidance For Return To Practice For Otolaryngology-Head and Neck SurgeryLeslie Lindsay AlvarezNo ratings yet
- Perioperative Medicine: The Pathway To Better Surgical CareDocument28 pagesPerioperative Medicine: The Pathway To Better Surgical CareLee SungjongNo ratings yet
- Textbook of Urgent Care Management: Chapter 39, Ensuring Patient SafetyFrom EverandTextbook of Urgent Care Management: Chapter 39, Ensuring Patient SafetyNo ratings yet
- Postoperative Care: Who Should Look After Patients Following Surgery?Document5 pagesPostoperative Care: Who Should Look After Patients Following Surgery?kishanm77No ratings yet
- RO-ILS Case StudyDocument4 pagesRO-ILS Case Studyapi-458422967No ratings yet
- Tutorials in Surgery For 4th Medical StudentsDocument180 pagesTutorials in Surgery For 4th Medical StudentsAnonymous jSTkQVC27bNo ratings yet
- 1.7 Right Person, Right Place, Right Time PDFDocument3 pages1.7 Right Person, Right Place, Right Time PDFKaren Osorio GilardiNo ratings yet
- Romanian Journal Analyzes Ethics of Hospital Stays After Tonsil SurgeryDocument4 pagesRomanian Journal Analyzes Ethics of Hospital Stays After Tonsil SurgeryMeva'a RogerNo ratings yet
- Module 1 Case StudyDocument7 pagesModule 1 Case StudyDivine ParagasNo ratings yet
- CX Preprotesica OOODocument4 pagesCX Preprotesica OOOMich ReynosoNo ratings yet
- Thesis On Incisional HerniaDocument4 pagesThesis On Incisional Herniapsmxiiikd100% (1)
- Surgical Preoperative Assessment - What To Do and Why? Student BMJDocument3 pagesSurgical Preoperative Assessment - What To Do and Why? Student BMJEd FitzgeraldNo ratings yet
- Radiation Safety-Nicolette SawickiDocument4 pagesRadiation Safety-Nicolette Sawickiapi-484758207No ratings yet
- Peninsula Cornwall - Pressure DamageDocument33 pagesPeninsula Cornwall - Pressure DamageDeepa JeyaseelanNo ratings yet
- Kakulamarri Pranav Ra2 10-13-17Document3 pagesKakulamarri Pranav Ra2 10-13-17api-373095622No ratings yet
- Incisional Hernia ThesisDocument5 pagesIncisional Hernia Thesisgbwy79ja100% (1)
- Cts ArticlesDocument4 pagesCts ArticlesdrarunraoNo ratings yet
- Thesis Topics in Interventional RadiologyDocument7 pagesThesis Topics in Interventional Radiologygjfcp5jb100% (2)
- Response ToDocument7 pagesResponse ToReza AbdarNo ratings yet
- Misconceptions and Safety in Radiation OncologyDocument5 pagesMisconceptions and Safety in Radiation Oncologyapi-692385376No ratings yet
- My Own Opinion TextDocument3 pagesMy Own Opinion TextM. Ricko NugrohoNo ratings yet
- Radiation Safety Paper 1Document3 pagesRadiation Safety Paper 1api-633087057No ratings yet
- Management of Pertrochanteric Fractures inDocument8 pagesManagement of Pertrochanteric Fractures inantonio dengNo ratings yet
- Ro-Ils PaperDocument4 pagesRo-Ils Paperapi-502011468No ratings yet
- Safety EssayDocument5 pagesSafety Essayapi-350437453No ratings yet
- Ethics Anda LawDocument12 pagesEthics Anda LawSiti Fatimahtusz07No ratings yet
- Day CaseDocument43 pagesDay CaseKamel HadyNo ratings yet
- Research Paper On Nurse AnesthetistDocument6 pagesResearch Paper On Nurse Anesthetistgw1gnz6b100% (1)
- Short and Long-Term Outcomes After Surgical Procedures Lasting For More Than Six HoursDocument8 pagesShort and Long-Term Outcomes After Surgical Procedures Lasting For More Than Six HoursDickyNo ratings yet
- Radiation Safety PaperDocument4 pagesRadiation Safety Paperapi-632529930No ratings yet
- Paediatric Ambulatory Surgery - Perioperative Concerns: Dr. Pramila Chari Dr. Indu SenDocument7 pagesPaediatric Ambulatory Surgery - Perioperative Concerns: Dr. Pramila Chari Dr. Indu SenT RonaskyNo ratings yet
- Anesthesia Management of Ophthalmic Surgery in Geriatric Patients PDFDocument11 pagesAnesthesia Management of Ophthalmic Surgery in Geriatric Patients PDFtiaraleshaNo ratings yet
- Cirugia AmbulatoriaDocument17 pagesCirugia AmbulatoriaCarlos Guillermo Chillihuani CanoNo ratings yet
- Thyroid Surgery DissertationDocument5 pagesThyroid Surgery DissertationDoMyPaperCanada100% (1)
- Dissertation Topics For MD AnaesthesiaDocument4 pagesDissertation Topics For MD AnaesthesiaWhitePaperWritingServicesCanada100% (1)
- Care Elderly 01Document16 pagesCare Elderly 01Emyx MaNo ratings yet
- Pre Hospital PDFDocument4 pagesPre Hospital PDFAndi Tri SutrisnoNo ratings yet
- Paediatric Radiography DissertationDocument4 pagesPaediatric Radiography DissertationGhostWriterCollegePapersHartford100% (1)
- 13 Anaesthesia Outside The OR AC 2016Document18 pages13 Anaesthesia Outside The OR AC 2016Anastesiologi CNo ratings yet
- Uhns Guidelines 2010Document187 pagesUhns Guidelines 2010varrakesh100% (1)
- 37 157 1 PB PDFDocument4 pages37 157 1 PB PDFDhea Amalia WibowoNo ratings yet
- Anesthesia Cosmetic SurgeryDocument7 pagesAnesthesia Cosmetic SurgerySergio ArbelaezNo ratings yet
- Radiation Safety PaperDocument4 pagesRadiation Safety Paperapi-525837437No ratings yet
- Basic Patient NeedsDocument15 pagesBasic Patient NeedsMarggie SalaoNo ratings yet
- Thesis On Episiotomy Wound HealingDocument5 pagesThesis On Episiotomy Wound HealingCollegePapersForSaleCanada100% (2)
- Preoperative, Anesthetic, and Postoperative Care For Rhinoplasty PatientsDocument7 pagesPreoperative, Anesthetic, and Postoperative Care For Rhinoplasty PatientsTarek abo kammerNo ratings yet
- Radiation Safety Essay Ryan MonagoDocument5 pagesRadiation Safety Essay Ryan Monagoapi-632682404No ratings yet
- InterviewDocument3 pagesInterviewapi-486625755No ratings yet
- Assessment and Management of Preoperative AnxietyDocument6 pagesAssessment and Management of Preoperative AnxietyFiorel Loves EveryoneNo ratings yet
- Non-Operatingroom Anesthesia: The Principles of Patient Assessment and PreparationDocument18 pagesNon-Operatingroom Anesthesia: The Principles of Patient Assessment and PreparationEolia EffendiNo ratings yet
- Groot Koerkamp, BasDocument231 pagesGroot Koerkamp, BasHelmy BahdalaNo ratings yet
- 10 1005 - Continuous Patient MonitoringDocument3 pages10 1005 - Continuous Patient MonitoringChristian KleinNo ratings yet
- CDVC and Integrated Practice Unit for Cancer CareDocument6 pagesCDVC and Integrated Practice Unit for Cancer CareAbdullah Alhurani100% (1)
- An Research Surrpunding The Profession, SurgeonDocument6 pagesAn Research Surrpunding The Profession, SurgeonKaizen257No ratings yet
- Roils 1Document4 pagesRoils 1api-574059920No ratings yet
- April2019JuniorCriticalCareFellowJDDocument6 pagesApril2019JuniorCriticalCareFellowJDM LubisNo ratings yet
- Internship ReportDocument15 pagesInternship Reportpreethi balakrishnanNo ratings yet
- Professional AdvancementDocument51 pagesProfessional AdvancementReshma AnilkumarNo ratings yet
- Population Trends in INDIADocument8 pagesPopulation Trends in INDIAcheedikrishnaNo ratings yet
- Breech BirthDocument10 pagesBreech Birthcirlce:twoworldsconnectedNo ratings yet
- Implementasi SPM Kesehatan Bayi Baru Lahir di Puskesmas DukuhsetiDocument10 pagesImplementasi SPM Kesehatan Bayi Baru Lahir di Puskesmas DukuhsetiFidia sariNo ratings yet
- No Article Title Time of Publication Authors Journal Name Received Date Revised Date Accepted DateDocument4 pagesNo Article Title Time of Publication Authors Journal Name Received Date Revised Date Accepted DateAnin Kalma MartadinataNo ratings yet
- Tobacco Free Generation Next - M. Amebari NongsiejDocument2 pagesTobacco Free Generation Next - M. Amebari NongsiejM. Amebari NongsiejNo ratings yet
- Continuous Insulin InfusionDocument6 pagesContinuous Insulin Infusionbobobo22No ratings yet
- Nurse Midwife PractionersDocument8 pagesNurse Midwife PractionersVineeta JoseNo ratings yet
- Small Spaces Need Smart Solutions - Kristoffer ThøgersenDocument12 pagesSmall Spaces Need Smart Solutions - Kristoffer ThøgersenTuan Huy Le100% (1)
- Mayasthenia Gravis NclexDocument47 pagesMayasthenia Gravis NclexKrishna SapkotaNo ratings yet
- Theodore Millon On Rosenhan PaperDocument6 pagesTheodore Millon On Rosenhan PaperJuliette WarnesNo ratings yet
- Nestle PolicyDocument29 pagesNestle PolicyMuhammad HarlandNo ratings yet
- Parasitology SummaryDocument7 pagesParasitology Summaryshiner99100% (1)
- Career Day Brochure FinalDocument2 pagesCareer Day Brochure Finalapi-375229945No ratings yet
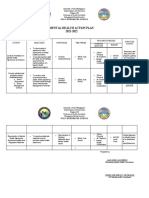
- Mental Health Action PlanDocument2 pagesMental Health Action PlanKenny Ann Grace Batiancila100% (9)
- Alt - Cancer (1) BookDocument419 pagesAlt - Cancer (1) Bookniceia matos100% (3)
- Dragon BoatDocument7 pagesDragon BoatandrewadrianNo ratings yet
- Psychosocial interventions ease suffering in complex palliative care patientsDocument7 pagesPsychosocial interventions ease suffering in complex palliative care patientsSiti Malkah KamilahNo ratings yet
- Mental Health EssayDocument2 pagesMental Health EssayROHITNo ratings yet
- SKF MSDS LGHP 2 PDFDocument5 pagesSKF MSDS LGHP 2 PDFMunkhnasan MonaNo ratings yet
- NYCOSH Letter To DOB Re: OSHA Card Arrests 10262015Document2 pagesNYCOSH Letter To DOB Re: OSHA Card Arrests 10262015Monica NovoaNo ratings yet
- MukokelDocument3 pagesMukokeljulietNo ratings yet
- The Future of Positive Psychology: A Declaration of IndependenceDocument17 pagesThe Future of Positive Psychology: A Declaration of IndependenceEbonnie DiazNo ratings yet
- Patient Information Guide: AH-QF-FO-07Document35 pagesPatient Information Guide: AH-QF-FO-07jose rajanNo ratings yet
- Teks Percakapan Bahasa InggrisDocument2 pagesTeks Percakapan Bahasa Inggrisnaufal456No ratings yet
- Research Proposal On Fast FoodDocument8 pagesResearch Proposal On Fast FoodManish Ravat100% (5)
- Fitness Testing Guide PDFDocument10 pagesFitness Testing Guide PDFdodovadaNo ratings yet
- Understanding Neurology - A Problem-Orientated Approach PDFDocument241 pagesUnderstanding Neurology - A Problem-Orientated Approach PDFAshabul AnharNo ratings yet
- Evidence Based Chinese Medicine HypertensionDocument13 pagesEvidence Based Chinese Medicine Hypertensionpranaji100% (2)