Professional Documents
Culture Documents
Fundamentals of Nursing Day 1
Uploaded by
JolensOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fundamentals of Nursing Day 1
Uploaded by
JolensCopyright:
Available Formats
Fundamentals of Nursing (sparks can trigger explosion)
3. Use: Cotton fabric
Date: 08/18 23 (wool and silk trigger static electricity)
Lecturer: Alvin Andrade
C. Colorless & Odorless
NURSING PROCEDURES 1. Prone: LEAKAGE (not visible)
HANDWASHING II. METHODS OF 02 DELIVERY DEVICES
Purpose: TO PREVENT INFECTION & SPREAD OF
DISEASES. 1. Nasal Canula - Nasal prongs
(24-40%)
I. MAJOR COMPONENTS 2. Simple Face mask
1. Running water (40-406)
2. Rubbing-Friction (MOST IMPORTANT COMPONENT) 3. Non-Rebreather - delivers the highest possible O2
3. Antimicrobial solution - Cleansing Agent (95-100%)
4. Venturi mask- delivers the most accurate amount of
II. TYPES O2
(24-40%)
1. Medical Handwashing-ordinary handwashing
PULSE OXIMETER -measures the amount of 02
(CLEAN TECHNIQUE) Pa02 - 80-100 mmHg (N)
after rinsing hands should be held below the O2 Sat - 95%-100% (N)
elbows. Others: (essential for arterial blood gas)
20-30 seconds pH (power of Hydrogen) -7.35-7.45 (N)
2. Surgical Handwashing 7.40 (Neutral point)
(STERILE TECHNIQUE) PCO2-35-45 (N)
after rinsing, hands should bel held above the HCO3-22-26 (N)
elbows.
3-5 minutes NRSING CONSIDERATION WHEN ADMINGSTERING 02:
1 Assess for: HYPOXIA-phases
OXYGEN THERAPY
Early: Late:
Purpose: TO IMPROVE TISSUE OXYGENATION • Pulse
Carbon Dioxide maintains HYPOXIC DRIVE- • Respiration
stimuli for breathing. • BP
• Acidic in nature (CO2) (Compensation) Restlessness Cyanosis
• Alkaline in nature (O2)
2. Verify doctors' order
COPD- (Respiratory Acidosis) • 2-7L/M (independent)
↑ CO2 counter out by: • more than 3L/M (dependent)
O2 (alkaline)-2-3L/M 3. Position
• Fowlers
I. MAJOR CHARACTERISTICS
A. Dry Gas - to prevent dryness of mucus membrane: 4. Regulate 02 flow accurately
1. Humidifier: sterile H20 Excessive of administration may lead to:
2. Perform: Oral care • Decrease O2
3. Lubricant: water-based • Retrolental Fibroplasia- retinal damage
B. Supports Combustion (explodes) (Irreversible)
1. Place: NO SMOKING SIGN
2. Check: electrical devices
TANK COLORS: a) Soak: H202 (1/2 strength) -Container 1
Green-Oxygen b) Clean: PNSSContainer 2
Gray Carbon dioxide
Brown-Helium 6. Remove: Soiled dressing (at the back of the flange)
Yellow - Compressed Air 7. Wear: STERILE GLOVES (changing of gloves)
Black – Nitrogen Note: wear 2 gloves already on #3
Blue-Inhaled anesthesia (DOUBLE GLOVING)
Red-Fire extinguisher 8. Suction: Outer cannula
Check: Expiration date Types:
Nasopharyngeal - secretions in the nasopharynx
TRACHEOSTOMY Oropharyngeal - secretions in the oropharynx
Tracheal- secretions on the outer cannula (not
Surgical opening in the trachea in the trachea)
9.Insert: Inner Cannula
Purpose: ESTABLISH AN AIRWAYProvide a long-term CLOCKWISE
airway support Note:
Removal Counterclockwise
I.BASIC PARTS: Insertion Clockwise
1 Outer Cannula 10. Clean: Flanged the site by the use of
serves as an artificial airway directly inserted to a) Sterile OS (gauze)
the trachea b) PNSS
2. Inner Cannula Note:
inserted inside the outer cannula 11. Apply: Sterile dressing (#6)
3. Obturator a) Size: 4x4
guide wire, used to directly insert both cannula b) Appearance: Y-shaped
in the respiratory tract
must be kept BEDSIDE 12. Change: Ties (before removing the old ties, secure
4. Flange first the new ties)
located at the distal portion of the cannula a) Apply new ties first
Secured by tapes & ties b) Then, remove old ties (square knots)
c) Distance from neck: I finger breadth
II.NURSING CONSIDERATIONS WHEN PERFORMING
TRACHEOTOMY Tracheostomy care must be done EVERY DAY!
Tracheostomy cutt - separates pre URT & LRT
1. Provide: PRIVACY (Avoid embarrassment) mechanical Ventilator - emergency equipment.
2. Position: SEMI FOWLER'S (best) Accidental removal- straighten the neck.
3. Wear: STERILE GLOVES (Sterile Procedure)
4. Open: Sterile Kit (must be available already at the
bedside) Wear: STERILE gines tracheal-secretions on the outer
a) Container 1: H2O2 (1/2 strength)-Hydrogen Cannula (not in the tracked)
peroxide.
b) Container 2: PNSS SUCTIONING
5.Cleaning:
Remove only Inner cannula Purpose: To maintain airway patency.
* outer cannula is my removed by the doctor INDEPENDENT NEG ITV.
In removing inner cannula by the use of
obturator
Direction COUNTER CLOCKWISE
I. NURSING CONSIDERATIONS: Abnormal Lung Sounds
1. Auscultate: Breath sounds ✓Crackles a) Crackles
2. Position: b) Wheezing
unconscious – SIDELYING c) Stridor
Conscious- SEMI FOWLERS d) Rhonchi
SUCTION CATHETER: e) Friction Rus- (Epiglottitis)
3. Size: French (catheter) the bigger the size" the
bigger the catheter CHEST PHYSIOTHERAPY
a) Adult -12-18
b) Child-8-10 AKA: BRONCHOPULMONARY HYGIENE
c) Intart-5-8 Purpose: To REMOVE 2 LOOSEN EXCESSIVE BRONCHIAL
4. Pressure: mmHg "The younger, The weaker SECRETIONS
pressure” DEPENDENT NEG. INTI.
Wall Portable
Adult 100-120 10-15 I.SEVERAL METHODS
Child 98-110 5-10 1. PERCUSSION:
Infant 50-95 2-5 cupped hands
striking
5. Hyper oxygenate: 100% 02 both hands done alternately
6. Wear: Sterile gloves Other terms:
• Suctioning Sterile Procedure a) CHEST/BACK TAPPING
7. Lubricant: b) CLAPPING
a) Nasopharyngeal- water based 2. VIBRATION:
b) Oropharyngeal- PNSS/0.9% NaCl Flat hands
Shaking
8. Length of Insertion: NOSE EAR LOBE Both hands done at the same time
(Approx 5 inches) 3. POSTURAL DRAINAGE:
Note: 1inch= 2.5cm Principle of gravity
9. Introduce suction catheter: WITHOUT SUCTION First and last method to be done
suction while withdrawal
10. Normal time of suctioning: II. NURSING CONSIDERATIONS:
a) 5-10 secs. (best) - to minimize O2 suction a) Check Doctor's order
b) 10-15 secs. b) Auscultate for breath sound
c) Interval: 20-30 seconds c) Best time for Postural Drainage:
d) Maximum time: 3-5 mins to prevent hypoxia • Before meals - to prevent aspiration
11. Withdraw Suction Catheter: Rotating/Circular • If after meals: 2-3 hrs.
motion • Bed time / Early morning.
To prevent mucus membrane damage d) Before performing Postural Drainage:
12. Perform: Oral Care Administer:
13. Hyper oxygenate: 100% Bronchodilators-widen resp tract
14. Auscultate: Breadth sounds Nebulization Therapy / Steam
Determine effectiveness of suctioning Inhalationto liquify mucus
- Crackles= X e) Perform Postural Drainage:
- Normal: BRONCHO VESICULAR Each position: 10-15 mins to prevent
Notes: exhaustion
Normal Lung Sounds Maximum: 30 MIN all throughout The
a) Bronchial procedure
b) Vesicular f) Perform: Percussion & Vibration alternately
c) Broncho vesicular each method: 1-2 Mis
Maximum: 30 MIN entire procedure use of blue paper:
g) After the procedure: Perform oral care blue= Blue-Alkaline (lungs)
h) Auscultate: Breath sounds blue=Red-Acid (stomach)
b) Auscultate- Use of Stethoscope
Whooshing, bubbling, gurgling sounds=
Note: CPT is best done to condition of Cystic Fibrosis stomach
(CPT-applied for problems in secretion) c) X-ray- confirmatory
-COPD is not applicable (obstruction) 10. Secure: Tape in the bridge of the nose
Complication of CPT – HYPOXIA
Feeding: NORMAL - P.O II. FEEDING
1. Position: SEMI FOWLER'S
NUTRITION 2. Check for patches
How to promote appetite? 3. Aspirate for: Residual content
LET THE PATIENT EAT HIS/HER OWN FOOD 1/2 of the amount of previous feeding
(regardless of nutritional benefit) a) if more than the amount of feeding- withhold
b) if less than the amount of feeding.
NASOGASTRIC TUBE ASSESS: PROPER DIGESTION
Purpose: 4. Flush: 30-60ml of water
1. GAVAGE 5. Height: 12 inches (Normal)
2. LAVAGE Virtue of gravity alters the speed of
3. TO ADMINSTER MEDICATIONS administration.
(X Enteric-Coated) -drug that has specialized coating Too rapid administration will pre dispose to
which is designed to be dissolve in a highly acidic DUMPING SYNDROME- rapid empting
environment (stomach) • less than 12 inches - TOD SLOW
Note: Stomach (parietal cells) produces 2 substances • more than 12 inches - TWO FAST
necessary for digestion: 6. Flush: 30-60 ml of water
• HCL (digests all types of food) 7. Before clamping: Retain some water in the
• Intrinsic factor (digest Vitamin B12) tubeTo prevent introduction of AIR
8. Position After feeding:
I. INSERTION SEMIFOWLERS'S (30 mins)
1. Position: HGH FOWLERS TO PREVENT ASPIRATION
2. Wear: CLEAN/ sterile gloves 9. Change tubings: 3-5 days
3. Lubricant: Water-based
4. Length of Insertion: NOSE-EARS-XYPHOID PARENTERAL NUTRITION
(Approx. 13-18 inches)
Purpose: To promote nourishment intravenously
5. Upon Insertion: HYPER EXTEND the NECK of Note: Enteral Feeding - food directly to the stomach
the patient Ex. NGT, PEG
6. Upon reaching the oropharynx: Parenteral Feeding directly to the blood
o The patients head forward to ensure it
reaches the stomach, not in the lungs. I. STATUS
7. Promote swallowing: SIP OF WATER Partial -no problems in the intestines, only
8. Allow: DEEP BREATHING EXERCISES nutritional deficiency suck as Protein (kwashiorkor) &
9. Check for patency: Methods in checking next fat/carbohydrate (Marasmus)
for – Total- for GI disorders such as intestinal
a) Aspiration-Assess for PH disorders, ulcerative colitis or regional enteritis
Lithmus gaper test
NURSING CONSIDERATIONS:
1. Route: Intravenous
2. Site: SUBCLAVIAN & JUGULAR VEIN (requires large
vein)
3. Contents:
Amino acids
Vitamins
Minerals
Glucose
4. STORAGE: a
a) Refrigerator (before) -body of ref.
b) Room temperature (prior to administration)
ROOMTEMP for 30 mins.
c) DISCARD -(after)/ damage
5. Complications:
a) Glucose imbalances
too fast - HYPER GLYCEMIA
too slow HYPOGLYCEMIA
b) Systemic infection – SEPSIS
glucose attracts bacteria in the insertion
site
6. Monitor:
a) Blood glucose - Glucometer
Normal:80-120 mg/dl
Check: CBG/HGT
Taken: Before breakfast (early morning)
b) Vital signs
Body Temperature (signs of infection)
c) Intake & out put
d) Weight
same:
Patient
Time
Clothes
weighing scale
You might also like
- ANESTHESIA - NOTES-2020 BY Dr. Ajay YadavDocument62 pagesANESTHESIA - NOTES-2020 BY Dr. Ajay YadavAnangsha Datta92% (13)
- Collection of MUET Speaking Topics 2020-2023Document89 pagesCollection of MUET Speaking Topics 2020-2023Cikgu Jessie U. Uchat100% (9)
- Rescue Practices NotesDocument38 pagesRescue Practices NotesNick Honcho CheathamNo ratings yet
- Pearls of Glaucoma ManagementDocument576 pagesPearls of Glaucoma Managementrobeye100% (1)
- Volume 1 Focus PDFDocument47 pagesVolume 1 Focus PDFAjay Kumar GuptaNo ratings yet
- Running Head: MIAH ZAVARRO V3 Miah Zavarro V3 Name Course Institution DateDocument4 pagesRunning Head: MIAH ZAVARRO V3 Miah Zavarro V3 Name Course Institution DateSammy Chege100% (1)
- General Practitioner - Endocrinology MCQsDocument17 pagesGeneral Practitioner - Endocrinology MCQsAsif Newaz100% (3)
- THE Maharashtra Factories Rules, 1963Document19 pagesTHE Maharashtra Factories Rules, 1963arvindtsarkarNo ratings yet
- Fundamentals of Nursing Day 1 & 2Document6 pagesFundamentals of Nursing Day 1 & 2JolensNo ratings yet
- Fundamentals of Nursing CompletedDocument8 pagesFundamentals of Nursing CompletedJolensNo ratings yet
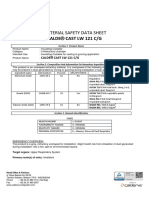
- Safety Data SheetDocument2 pagesSafety Data SheetFuadul lamiNo ratings yet
- Kerr PlatiniteDocument1 pageKerr PlatinitemarosnaxNo ratings yet
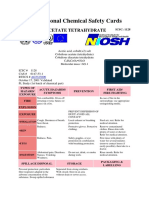
- International Chemical Safety Cards: Cobalt (Ii) Acetate TetrahydrateDocument3 pagesInternational Chemical Safety Cards: Cobalt (Ii) Acetate TetrahydrateAjung SatriadiNo ratings yet
- International Chemical Safety CardsDocument3 pagesInternational Chemical Safety CardsAmatirNo ratings yet
- Oxygen TherapyDocument35 pagesOxygen Therapylala byuNo ratings yet
- International Chemical Safety Cards EthanolDocument2 pagesInternational Chemical Safety Cards EthanolCarlos Gil100% (1)
- 14062b PDFDocument56 pages14062b PDFأحمد العريقيNo ratings yet
- Poster Irrigation System in EndodonticDocument2 pagesPoster Irrigation System in EndodonticMonika LohakpureNo ratings yet
- Hydrocarbon MonitoringDocument40 pagesHydrocarbon MonitoringalexNo ratings yet
- Contact Cleaner 2000Document7 pagesContact Cleaner 2000Ronaldo glenn SinabaribaNo ratings yet
- Surgical Asepsis, AntisepsisDocument3 pagesSurgical Asepsis, AntisepsisLê Xuân SangNo ratings yet
- Presentation On AnnoxiaDocument22 pagesPresentation On AnnoxiaReda El-DahshoryNo ratings yet
- MS LAB Oxygenation Nursing SkillsDocument9 pagesMS LAB Oxygenation Nursing SkillsRouwi DesiatcoNo ratings yet
- Icsc 1451 - Potassium SulfateDocument2 pagesIcsc 1451 - Potassium Sulfatewidyy universeNo ratings yet
- Gastroent 04 E10Document7 pagesGastroent 04 E10PraistonNo ratings yet
- MsdsDocument7 pagesMsdsFebriansyah AnandyaNo ratings yet
- Funda MidtermsDocument13 pagesFunda MidtermsMutya XDNo ratings yet
- Ren Sac405#accurus#810 MSD 20180302 2Document6 pagesRen Sac405#accurus#810 MSD 20180302 2Che Wei LinNo ratings yet
- Cooper Industries - Chico A Sealing CompoundDocument6 pagesCooper Industries - Chico A Sealing Compoundjaredf@jfelectric.com100% (3)
- Material Safety Data Sheet: Makhro 2.4-DbDocument4 pagesMaterial Safety Data Sheet: Makhro 2.4-DbTititoo Acuñaa CRNo ratings yet
- Msds Calde Cast LW 121 CGDocument5 pagesMsds Calde Cast LW 121 CGAfronie Cepoz D'nextNo ratings yet
- MSDS Conqor 303ADocument5 pagesMSDS Conqor 303AJose AlejandroBlancoNo ratings yet
- Chapter 2 - Safety in The Hematology LaboratatoryDocument10 pagesChapter 2 - Safety in The Hematology LaboratatoryMonica DomingoNo ratings yet
- Equipment Demonstration: National Neonatology ForumDocument53 pagesEquipment Demonstration: National Neonatology ForumSatya Prakash TiwariNo ratings yet
- Cedar FiberDocument6 pagesCedar Fibersajad gohariNo ratings yet
- Pac MSDSDocument4 pagesPac MSDSdiNo ratings yet
- Chemical Hazard Bulletin: Ecolab M290Document1 pageChemical Hazard Bulletin: Ecolab M290MARKNo ratings yet
- SOP PEMBERIAN OKSIGENASI - Id.enDocument4 pagesSOP PEMBERIAN OKSIGENASI - Id.enWiradianto PutroNo ratings yet
- MSDS NanoIntegris-IsoSolution GHSDocument8 pagesMSDS NanoIntegris-IsoSolution GHSAbdelkrim KhediriNo ratings yet
- Hydrogen Chloride 0163: April 2000Document2 pagesHydrogen Chloride 0163: April 2000vivekpattniNo ratings yet
- Microsoft Word - 520 BLV MsdsDocument1 pageMicrosoft Word - 520 BLV MsdsEdwiin TamayoNo ratings yet
- Cytosine 5 MethyltransferaseDocument3 pagesCytosine 5 MethyltransferaseNabilahNo ratings yet
- 861-868 Series MsdsDocument2 pages861-868 Series MsdsMangesh MohiteNo ratings yet
- Material Safety Data Sheet: Gear Oli SaeDocument1 pageMaterial Safety Data Sheet: Gear Oli Saeslamet4riadiNo ratings yet
- Acetone 0087: April 1994Document2 pagesAcetone 0087: April 1994vivekpattniNo ratings yet
- KGD Pemicu 2 Bagian 2: Mutiara Lirendra 405130147Document25 pagesKGD Pemicu 2 Bagian 2: Mutiara Lirendra 405130147MutiaraNo ratings yet
- Nordbak Wearing Compd MsdsDocument5 pagesNordbak Wearing Compd MsdsAnonymous LeC3YexoBoNo ratings yet
- Lab 2 UltrasonicproximitysensorDocument8 pagesLab 2 UltrasonicproximitysensorSyamim DaudNo ratings yet
- Bacteriologic Specimen Collection V.1Document4 pagesBacteriologic Specimen Collection V.1smclab eqasNo ratings yet
- Material Safety Data Sheet (MSDS) Carbon Monoxide Please Ensure That This MSDS Is Received by An Appropriate Person Date: January 2015 Ref: MS114Document2 pagesMaterial Safety Data Sheet (MSDS) Carbon Monoxide Please Ensure That This MSDS Is Received by An Appropriate Person Date: January 2015 Ref: MS114Savan JaviaNo ratings yet
- Spesifikasi, MEDIPIA Endoscope Washer & Disinfector ENDO CLEAN 2000Document1 pageSpesifikasi, MEDIPIA Endoscope Washer & Disinfector ENDO CLEAN 2000Kasi Pelayanan MedikNo ratings yet
- PSIS - BISCO Silicones HT-1510Document5 pagesPSIS - BISCO Silicones HT-1510mukeshNo ratings yet
- Material Safety Data Sheet X-CIDE 207: 1. Chemical Product and Company IdentificationDocument7 pagesMaterial Safety Data Sheet X-CIDE 207: 1. Chemical Product and Company IdentificationLuis Gomez JimenezNo ratings yet
- Material Data Sheet of TK 711Document4 pagesMaterial Data Sheet of TK 711anon_610231150No ratings yet
- Safe Airway Society Covid 19Document6 pagesSafe Airway Society Covid 19Ghina AlifahNo ratings yet
- Clean R Carb Carburetor CleanerDocument6 pagesClean R Carb Carburetor CleanerNabeel maqsoodNo ratings yet
- Cleaning Chemical Cc1-Tech Specs-Eng-R2-PtDocument4 pagesCleaning Chemical Cc1-Tech Specs-Eng-R2-PtsgpttechNo ratings yet
- Endoscope Reprocessing Risk and Current Risk PracticeDocument65 pagesEndoscope Reprocessing Risk and Current Risk PracticeHosam GomaaNo ratings yet
- 30 Per Cycle (1, 2, 3, 28, 29, 1) 5 Cycle: Other Purpose New Product/new UseDocument1 page30 Per Cycle (1, 2, 3, 28, 29, 1) 5 Cycle: Other Purpose New Product/new UseEushane Chiya M. SyNo ratings yet
- Datasheet Digital Sensor Maintenance PDFDocument8 pagesDatasheet Digital Sensor Maintenance PDFRuben OlivaresNo ratings yet
- Carbon Tetrachloride 0024: April 2000Document2 pagesCarbon Tetrachloride 0024: April 2000vivekpattniNo ratings yet
- DT Template (Edited)Document19 pagesDT Template (Edited)Abhinav JhaNo ratings yet
- Downloads Ir File v1 1831Document1 pageDownloads Ir File v1 1831Vinoth SenthilNo ratings yet
- 1437 Eng PDFDocument1 page1437 Eng PDFHaleem Ur Rashid BangashNo ratings yet
- Physicochemical and Sensory Evaluation of Mixed Juices From Banana, Pineapple and Passion Fruits During StorageDocument12 pagesPhysicochemical and Sensory Evaluation of Mixed Juices From Banana, Pineapple and Passion Fruits During StorageRichionNo ratings yet
- Sabarimala: Virtual-Q Booking CouponDocument2 pagesSabarimala: Virtual-Q Booking CouponST COMMNICATIONNo ratings yet
- Walkthrough21 PDFDocument51 pagesWalkthrough21 PDFAnas SantyNo ratings yet
- ArticleDocument10 pagesArticleperley.matiasNo ratings yet
- Text of The Timothy J. Barber ActDocument2 pagesText of The Timothy J. Barber ActThe Livingston County NewsNo ratings yet
- Finnish Dental Health GlossaryDocument5 pagesFinnish Dental Health GlossaryVeronicaGelfgrenNo ratings yet
- JUSHI Safety Data SheetDocument11 pagesJUSHI Safety Data SheetSofya AndarinaNo ratings yet
- D2 0905 Paediatric Reference Intervals - An Update - Tina YenDocument25 pagesD2 0905 Paediatric Reference Intervals - An Update - Tina YenkamalNo ratings yet
- Fact Sheet 3 - Food Safety Laws, Regulations and Standards AssessorDocument8 pagesFact Sheet 3 - Food Safety Laws, Regulations and Standards Assessorshanmugam thevapriyanNo ratings yet
- Product CatalogueDocument22 pagesProduct CatalogueSHRUTEE SINGHNo ratings yet
- Ovarian Stimulation Strategies: Maximizing Efficiency in ARTDocument21 pagesOvarian Stimulation Strategies: Maximizing Efficiency in ARTImelda HutagaolNo ratings yet
- Clinical Image - Max 1st MolarDocument2 pagesClinical Image - Max 1st MolarShriya SingiNo ratings yet
- COVID-19 and A-Dec Dental Equipment Infection Control: Dear Valued CustomerDocument4 pagesCOVID-19 and A-Dec Dental Equipment Infection Control: Dear Valued CustomerAlleirbag KajnitisNo ratings yet
- Spiritual CareDocument7 pagesSpiritual CareSyarief NurseNo ratings yet
- Lab Design Guide ChecklistDocument9 pagesLab Design Guide ChecklistTanveer AzizNo ratings yet
- EAPPQ4W4CADocument9 pagesEAPPQ4W4CAPhebi ReyNo ratings yet
- Multi-Mechanism Skin Brightening Sabi WhiteDocument6 pagesMulti-Mechanism Skin Brightening Sabi WhiteMuhammad Akhyar RosyidiNo ratings yet
- Operating RoomDocument13 pagesOperating RoomrichardNo ratings yet
- Theoretical Foundations in Nursing - 1ST YearDocument12 pagesTheoretical Foundations in Nursing - 1ST YearcelinnechelsybenitezNo ratings yet
- New Grad Banner Cover Letter RevisedDocument1 pageNew Grad Banner Cover Letter Revisedapi-621660715No ratings yet
- JCO On CD-ROM (Copyright © 1998 JCO, Inc.), Volume 1984 Jan (35 - 37) - A Therapeutic Method For Selected TMJ PatientsDocument6 pagesJCO On CD-ROM (Copyright © 1998 JCO, Inc.), Volume 1984 Jan (35 - 37) - A Therapeutic Method For Selected TMJ PatientssaberNo ratings yet
- 33 Exp Jan 20Document35 pages33 Exp Jan 20Muhammad YousufNo ratings yet
- Amandeep Kaur Nursing Demonstrator Ionurc, Goindwal Sahib, PunjabDocument20 pagesAmandeep Kaur Nursing Demonstrator Ionurc, Goindwal Sahib, PunjabSanjay Kumar SanjuNo ratings yet
- Technical Document - AquaSnap Microbial DetectionDocument1 pageTechnical Document - AquaSnap Microbial DetectionanjukkuttiNo ratings yet
- Notice of Post DisqualificationDocument3 pagesNotice of Post DisqualificationMelody Frac ZapateroNo ratings yet