Professional Documents
Culture Documents
637
Uploaded by
Sharuk AhamedOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
637
Uploaded by
Sharuk AhamedCopyright:
Available Formats
RESEARCH PAPER
Warning Signs on Short Hammersmith Neonatal Neurological
Examination and Correlation With Hammersmith Infant Neurological
Examination Global Score in Preterm Infants: A Prospective Cohort Study
MANISHA BHANDANKAR, DEEPA METGUD
Department of Pediatrics, Jawaharlal Nehru Medical College, Belgaum, Karnataka.
Correspondence to: Dr Manisha Bhandankar, Professor of Pediatrics, Jawaharlal Nehru Medical College, Belgaum, Karnataka.
manisha.bhandankar1970@gmail.com
Received: April 22, 2022; Initial review: June 1, 2022; Accepted: March 3, 2023.
Objective: To describe the findings of short Hammersmith Neona- abnormal signs on short HNNE. 12 (37.5%) AGA infants and 6
tal Neurologic examination (HNNE) in preterm small for gestational (30%) SGA infants had global score <65 at mean corrected age
age (SGA) and appropriate for gestational age (AGA) infants at (SD) of 4.3 (0.7) weeks and 4.5 (0.8) weeks, respectively. Very
term equivalent age (TEA) and to correlate it with the global score of preterm, birth weight <1000 g and SGA was significantly associated
Hammersmith Infant Neurologic Examination (HINE) performed at with global scores <65.
4-6 months of corrected age.
Conclusion: Early identification of warning signs among SGA in-
Methods: This prospective cohort study was conducted at the high fants using Short HNNE screening at TEA can be useful to initiate
risk follow-up clinic of our center. 52 preterm infants born <35 early intervention. There was no statistically significant difference in
weeks gestation were examined using HNNE at TEA and followed- global scores by HINE among AGA and SGA infants in early in-
up till 4-6 months of corrected age to estimate HINE. fancy.
Results: 20 infants (38.5%) had warning signs and 9 (17.3%) had Keywords: Low birth weight, Prognosis, Small for gestational age.
Published online: March 20, 2023; PII: S097475591600513
P
reterm infants are known to be at high risk for within the reference range (90%); the lateral columns include
developmental delays because of their gestatio- all the warning signs and the last line indicates abnormal
nal age, morbidities associated with prematurity, signs. The authors have reported that the short HNNE was
and consequences of interventions in the neonatal able to identify 98.5% preterm infants with an abnormal full
intensive care unit (NICU) [1]. Additionally, adequate neurologic examination (complete HNNE) at term [7,8]. The
intrauterine growth of fetus is essential for normal extra- Hammersmith infant neurological examination (HINE) has
uterine growth and development [2,3]. Early recognition of been proposed as a simple and scorable early neurological
abnormal neurologic signs as predictors of neurodevelop- examination tool for the diagnosis of cerebral palsy for
mental delay in infants at risk due to prematurity and related evaluating infants between 2 months and 24 months of age.
morbidities is essential to introduce early intervention [4-6]. Significant correlation between the HNNE and HINE score
to predict infants at risk of cerebral palsy in early infancy has
Several tools are available to screen infants from
been reported [9]. Similar data regarding short HNNE has
neonatal period to identify those at risk of developmental
not been reported.
delay. Hammersmith neonatal neurological examination
(HNNE), initially developed by Dubowitz in 1981, has 34
Invited Commentary:Page 619
items assessing tone, motor patterns, observation of
spontaneous movements, reflexes, visual and auditory India is a major contributor of preterm and low birth
attention, and behavior. Short Hammersmith neonatal weight infants with intrauterine growth restriction. A quick
neurological examination is a screening tool consisting of 12 and reliable screening tool such as short HNNE can be of
items modified from original complete HNNE. This tool is significant help in identification of infants in the busy follow-
used to assess the posture, tone, movement, reflexes, and up clinics.
motor milestones in the both term and preterm infants at term
equivalent age (TEA). The proforma has a central grey In this study, we intended to examine preterm infants
column that covers the spectrum of neurologic findings (born <35 weeks gestational age) at TEA using short HNNE
INDIAN PEDIATRICS 637 VOLUME 60__AUGUST 15, 2023
30 SHORT HNNE AND HINE IN PRETERMS
and then at four to six months of corrected age using HINE. Kerala. The findings were recorded in the standardized form
The primary objective was to describe the preterm infants and scored as per the protocol.
using short HNNE at TEA and to correlate it with the HINE
Neurosonogram was done as part of routine protocol at
global score performed at four to six months of corrected
TEA. All the infants received early stimulation and inter-
age. The secondary objective was to compare this finding
vention as deemed necessary during follow-up from trained
among small for gestational age (SGA) and adequate for
psychologists and physiotherapists.
gestational age (AGA) infants.
Statistical analysis: Data were analyzed using statistical
METHODS
software R version 4.0.2 and Microsoft Excel. Continuous
This prospective observational study was conducted among variables were represented by mean (SD)/median (range)
a cohort of preterm infants less than 35 weeks who were and categorical variables represented by frequency and
identified to be SGA or AGA at birth and followed-up in the percentage. Chi-square test was used to check the association
high-risk follow-up clinic of a tertiary care hospital in between categorical variables and t test/Mann-Whitney test
Karnataka from October, 2019 to September, 2020. to compare mean/distributions between groups. Monte-
Carlo simulation used in chi-square test was used to assess
Ethical clearance was obtained from the ethics
the primary and secondary objectives of the study.
committee of Jawaharlal Nehru Medical College and a
written informed consent was obtained from the parents. RESULTS
Preterm infants born <35 weeks gestation discharged from
Out of total 99 infants who were examined at 40 weeks of
the NICU and followed-up at the high-risk baby clinic of the
gestation (39+1 to 41+6 weeks), 52 infants were examined
hospital were included. Infants with proven intrauterine
using both short HNNE and HINE during the study period
infection, major congenital malformations requiring surgery,
and were included in the analysis (Fig. 1). Twenty infants
proven inborn errors of metabolism, and proven genetic/
were SGA and 32 infants were in AGA group. Table I gives
syndromic condition known to be associated with
the demographic details of the infants enrolled in the study.
developmental delay before enrolment were excluded. The
infants were categorized based on birthweight into SGA Among 52 infants, 20 (38.4%) had warning signs and 9
(below 10th centile) and AGA (between 10th to 90th centile) (17.3%) had abnormal signs using Short HNNE at TEA.
based on Fenton preterm growth chart [9]. Sixteen (80%) of these infants with warning signs were very
preterm, and rest four were extreme preterm. Fourteen
Based on previous studies of 15% abnormal findings
infants had single warning sign and six infants (11.5%) had
among preterm infants using complete HNNE, the sample
≥2 warning signs. Maximum number of infants had warning
size with percentage of maximum error as 10% at 95%CI
signs in the spontaneous activity and head control. The mean
was calculated as 49 [8,11,12].
(SD) age of assessment for HINE was 4.4 (0.7) months and
Demographic details, antenatal risk factors and anthro- the median (range) HINE Global score was 66 (35-74). Most
pometry were recorded in a structured form at the time of infants scored low on reflexes and reactions component of
follow-up. Both the examinations were done by either of the HINE.
two examiners, who were not blinded to the records. The
examiners learnt the examination from the educational Table I Demographic Details of the Enrolled Infants
videos available at the Hammersmith neurological exami-
AGA (n=32) SGA (n=20)
nation website, and received additional training at CDC,
Female 12 (37.5) 11 (55)
Gestational age (wk)a 31.56 (2.26) 32.11 (2.26)
99 neonates examined at term equivalent age using HNNE Weight at birth (g)a,b 1562.16 1169.75
(492.4) (333.3)
→ 20 infants not brought for follow-up FC at birth (cm) a 29.97 (1.99) 28.73 (2.01)
Length at birth (cm) a 41.65 (3.78) 40.79 (4.01)
→ 17 infants followed-up till 3 mo corrected age
Ventilated 4 (12.5) 5 (25)
→ 10 infants followed-up at 6 mo corrected age Culture proven sepsis 4 (12.5) 5 (25)
Maternal chorioamnionitis 1 (3.12) 1 (5)
52 infants examined at 4-6 mo corrected
→ age using HINE
Two doses of antenatal steroid 10 (31.2) 14 (70)
IVH (Grade I-II) 2 (6.25) 2 (10)
Fig. 1 Flow chart of participants. Values in no. (%) or amean (SD). All P >0.05 except bP <0.001.
INDIAN PEDIATRICS 638 VOLUME 60__AUGUST 15, 2023
BHANDANKAR AND METGUD 31
HINE global score at 4-6 months, it helped us in early
identification of infants with warning signs. Literature review
gives HINE global score cutoff levels in the range of 57 to
66; separately for preterm and term infants from 3 to 12
months of age to predict cerebral palsy [9,14,15]. To explore
the correlation of warning signs with low HINE global
scores, we analyzed the short HNNE data in infants with
HINE global score of ≤65 and noted a trend towards lower
HINE global score (≤65) among SGA infants who had
warning signs on short HNNE. Follow-up data of these
infants to know how many continue to have lower global
scores by the end of two years is pivotal for this study.
The ‘visual orientation’ assessment from HNNE form
SGA: small for gestational age, AGA:appropriate for gestational age. was affected by the iatrogenic pupillary dilatation of the
infants done for ROP examination prior to the neurologic
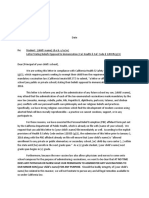
Fig. 2 Box and whisker plot of distribution of median global score examination in the high risk follow-up clinic in ten infants;
in both SGA and AGA group.
hence, we did not analyze this warning sign. This
compromised our understanding of development of infant’s
In subset analysis, warning signs were present among 11 visual function and the final analysis of number of warning
(34.4%) and nine infants (45%) from AGA group and SGA signs in all infants, which is a major limitation of the study.
group, respectively but there was no significant difference
between the two groups in median (IQR) HINE global score The hyperechogenicities reported in neurosonogram in
[66 (35,74) vs 67.5 (38,72); P=0.43]. our study could be evolving periventricular leukomalacia
(Grade 1), which were detected in three infants, of whom two
Eighteen infants had global score ≤65 of whom 12 were infants had >2 warning signs [15]. This is not significant with
AGA and six were SGA infants. Seven infants out of 18 had respect to neurodevelopmental outcome as studies have
single warning sign and three had ≥2 signs on short HNNE reported absence of obvious abnormal findings in neuro-
(all SGA). Presence of even single warning sign on short sonogram, even in presence of cellular insult [17,18].
HNNE examination in SGA group was significantly
associated with global score of ≤65 (P=0.004). The major limitation of this study is loss of data due to
difficulties in follow-up of infants within the study period
On neurosonogram, resolving germinal matrix bleed secondary to the restrictions of the COVID-19 pandemic,
was reported among three infants but none of the infants and iatrogenic pupillary dilatation affecting the assessment
had ventriculomegaly. Periventricular hyperechogeni- of visual orientation during HNNE.
cities were reported in three infants during the follow-up.
We assessed the utility of short HNNE in recording
DISCUSSION warning signs among preterm infants. This may be useful in a
Short HNNE is a screening tool which takes few minutes to busy resource-limited setting to identify infants (SGA in
perform if the infant is alert and active (Brazelton stage 4-5) particular) who require regular follow-up and may thus be
compared to that of complete HNNE, which requires 10-15 benefited from timely early intervention [6,15]. Further
minutes [13]. In our study, six infants (11.5%) had ≥2 research through large studies, and long-term follow-up till
warning signs with no significant correlation between minimal two years corrected age is necessary to understand
warning signs, abnormal signs on short HNNE and HINE which warning and/or abnormal signs on short HNNE during
global score. Romeo, et al. [7] reported that in the 380 very infancy have correlation with low global scores by two years
pre-term infants, 5% had two and 1% had >2 warning signs of age.
with good correlation to lower optimality score on complete Ethics clearance: EIC, Jawaharlal Nehru Medical College
HNNE. Among the infants with warning signs three each Institutional Ethics Committee on Human subjects’ research; No.
were very preterm and extreme preterm infants. Spittle, et al. MDC/DOME/226 dated Dec 28, 2019.
[14] have reported that 25% of infants who were born Contributors: MB: designed and conducted the study, analyzed
moderately or late preterm scored suboptimal on complete and interpreted the data, drafted the manuscript. DM: substantial
HNNE score. contributions to the conception or design of the work, inter-
pretation of data for the work and revising the manuscript critically.
Though, we found a non-significant association between Both authors approved the version to be published and agree to be
the findings of short HNNE among preterm infants and the accountable for all aspects of the work in ensuring that questions
INDIAN PEDIATRICS 639 VOLUME 60__AUGUST 15, 2023
32 SHORT HNNE AND HINE IN PRETERMS
WHAT THIS STUDY ADDS?
• Preterm infants with one or more warning signs on short Hammersmith Neonatal Neurological Examination may
have lower global score by Hammersmith Infant Neurological Examination during early infancy.
related to the accuracy or integrity of any part of the work are 2021;63:939-46.
appropriately investigated and resolved. 9. Connors R, Sackett V, Machipisa C, et al. Assessing the utility
Funding: None; Competing interests: None stated. of neonatal screening assessments in early diagnosis of
cerebral palsy in preterm infants. Brain Sci. 2022;12:847.
REFERENCES
10. Fenton TR, Kim JH. A systematic review and metaanalysis to
1. Gladstone M, Oliver C, Van den Broek N. Survival, morbid- revise the Fenton growth chart for preterm infants. BMC
ity, growth and developmental delay for babies born preterm Pediatr. 2013;13:1-13.
in low and middle income countries–a systematic review of 11. Drillien CM. Abnormal neurologic signs in the first year of life
outcomes measured. PLoS One. 2015;10: e0120566. in low birthweight infants: possible prognostic significance.
2. Nosarti C, Murray RM, Hack M, editors. Neurodevelopmen- Dev Med Child Neurol. 1972;14:575-84..
tal outcomes of preterm birth: from childhood to adult life. 12. Romeo DM, Cioni M, Palermo F, et al. Neurological
Cambridge University Press; 2010;2010:1-277. assessment in infants discharged from a neonatal intensive
3. Romeo DM, Brogna C, Sini F, et al. Early psychomotor care unit. Eur J Paediatr Neurol. 2013;17:192-8.
development of low-risk preterm infants: Influence of 13. Brazelton TB, Nugent JK. Neonatal behavioral assessment
gestational age and gender. Eur J Paediatr Neurol. 2016;20: scale. Cambridge University Press; 1995.
518-23. 14. Spittle AJ, Walsh JM, Potter C, et al. Neurobehaviour at term-
4. Levine TA, Grunau RE, McAuliffe FM, et al. Early childhood equivalent age and neurodevelopmental outcomes at 2 years in
neurodevelopment after intrauterine growth restriction: A infants born moderate-to-late preterm. Dev Med Child Neurol.
systematic review. Pediatrics. 2015;135:126-41. 2017;59:207-15.
5. Chaudhari S, Kulkarni S, Pandit A, et al. Neurological 15. Romeo DM, Ricci D, Brogna C, et al. Use of the hammer-
assessment at three months as a predictor for developmental smith infant neurological examination in infants with cerebral
outcome in high risk infants. Indian Pediatr. 1993;30:528-31. palsy: A critical review of the literature. Dev Med Child Neu-
6. Novak I, Morgan C, Adde L, et al. Early, accurate diagnosis rol. 2016;58:240-5.
and early intervention in cerebral palsy: Advances in diagnosis 16. Ahya KP, Suryawanshi P. Neonatal periventricular leukoma-
and treatment. JAMA Pediatr. 2017;171:897-907. lacia: Current perspectives. Res Rep Neonatol. 2018;8:1-8.
7. Romeo DM, Ricci D, van Haastert IC, et al. Neurologic 17. Limperopoulos C, Bassan H, Gauvreau K, et al. Does
assessment tool for screening preterm infants at term age. J cerebellar injury in premature infants contribute to the high
Pediatr. 2012;161:1166-8. prevalence of longterm cognitive, learning, and behavioral
8. Romeo DM, Cowan FM, Haataja L, et al. Hammersmith infant disability in survivors? Pediatrics. 2007;120:584-93.
neurological examination for infants born preterm: Predicting 18. Hagberg H, Mallard C, Jacobsson B. Role of cytokines in pre-
outcomes other than cerebral palsy. Dev Med Child Neurol. term labour and brain injury. BJOG. 2005;112:16-8.
INDIAN PEDIATRICS 640 VOLUME 60__AUGUST 15, 2023
You might also like
- NUR 151 P1 EXAM REVIEWDocument13 pagesNUR 151 P1 EXAM REVIEWJilkiah Mae Alfoja Campomanes100% (2)
- Principal Letter Opposed ImmunizationDocument2 pagesPrincipal Letter Opposed Immunizationmpnaidu13111998100% (1)
- Maxillectomy A ReviewDocument17 pagesMaxillectomy A ReviewDr. T. Balasubramanian100% (3)
- Hammersmith in GhanaDocument10 pagesHammersmith in GhanaAndrea PederziniNo ratings yet
- The Problems of Moderate Preterm Infants: Seminars in PerinatologyDocument4 pagesThe Problems of Moderate Preterm Infants: Seminars in Perinatologysam crushNo ratings yet
- Psychomotor Development and Minor Anomalies in Children Exposed To Antiepileptic Drugs in Utero: A Prospective Population-Based StudyDocument6 pagesPsychomotor Development and Minor Anomalies in Children Exposed To Antiepileptic Drugs in Utero: A Prospective Population-Based StudyAhmed AllamNo ratings yet
- Use of The Hammersmith Infant Neurological Examination in Infants With Cerebral Palsy: A Critical Review of The LiteratureDocument6 pagesUse of The Hammersmith Infant Neurological Examination in Infants With Cerebral Palsy: A Critical Review of The LiteratureshodhgangaNo ratings yet
- Hammersmith High Risk ProgramDocument8 pagesHammersmith High Risk ProgramAndrea PederziniNo ratings yet
- Neurodevelopmental Outcomes of Infants with Meconium Aspiration SyndromeDocument9 pagesNeurodevelopmental Outcomes of Infants with Meconium Aspiration SyndromeVictor CuevaNo ratings yet
- Early Neurologic Assessment in Preterm-Infants: Integration of Traditional Neurologic Examination and Observation of General MovementsDocument7 pagesEarly Neurologic Assessment in Preterm-Infants: Integration of Traditional Neurologic Examination and Observation of General MovementsAnonymous QOCn5dNo ratings yet
- Early feeding problems predict outcomes in cerebral palsyDocument4 pagesEarly feeding problems predict outcomes in cerebral palsyMuhammad Yusril JalilNo ratings yet
- 2017-Journal of Paediatrics and Child HealthDocument1 page2017-Journal of Paediatrics and Child HealthAna SopaNo ratings yet
- 2016 InfanibDocument5 pages2016 InfanibMelina Defita SariNo ratings yet
- NIH Public Access: Author ManuscriptDocument21 pagesNIH Public Access: Author ManuscriptanyNo ratings yet
- Article NeonatesDocument7 pagesArticle NeonatesFaisal YousafNo ratings yet
- Sharma2011 Article GrowthAndNeurosensoryOutcomesODocument6 pagesSharma2011 Article GrowthAndNeurosensoryOutcomesOSayak ChowdhuryNo ratings yet
- Dubowitz Infants Born To Subtance UseDocument6 pagesDubowitz Infants Born To Subtance UseAndrea PederziniNo ratings yet
- Hiv 2023Document10 pagesHiv 2023Neonatología HGO4No ratings yet
- HIPOACUSIA12Document5 pagesHIPOACUSIA12cristianNo ratings yet
- Risk Factors for Failed Neonatal Hearing Screening and Their Relationship to Screening OutcomesDocument6 pagesRisk Factors for Failed Neonatal Hearing Screening and Their Relationship to Screening OutcomesRendra SyaniNo ratings yet
- Asphyxia's Effect on Head Circumference in Children Aged 6-24 MonthsDocument9 pagesAsphyxia's Effect on Head Circumference in Children Aged 6-24 Monthsmail junkNo ratings yet
- Rossi 2019Document8 pagesRossi 2019Ivana ThiodoraNo ratings yet
- Diagnostic ACCURACYDocument26 pagesDiagnostic ACCURACYRirin FebriantiNo ratings yet
- 33873-Article Text-121761-1-10-20170831Document6 pages33873-Article Text-121761-1-10-20170831AnggaNo ratings yet
- Abnormal placentation ultrasound and histology correlationsDocument314 pagesAbnormal placentation ultrasound and histology correlationsDiana-Elena ComandasuNo ratings yet
- Precht L 1997Document3 pagesPrecht L 1997Javiera Rodriguez QuezadaNo ratings yet
- Developmental Interventions in the NICU May Boost Cognitive DevelopmentDocument8 pagesDevelopmental Interventions in the NICU May Boost Cognitive DevelopmentMirza RisqaNo ratings yet
- A Behavioral Method For Efficient Screening of Visual Acuity in Young InfantsDocument9 pagesA Behavioral Method For Efficient Screening of Visual Acuity in Young InfantsWistya Eka mahadewiNo ratings yet
- Gestational AgeDocument7 pagesGestational AgeLilisNo ratings yet
- Influencing Factors of The Neurodevelopment of High-Risk InfantsDocument6 pagesInfluencing Factors of The Neurodevelopment of High-Risk InfantsDewi NurNo ratings yet
- 2174 8646 1 PBDocument5 pages2174 8646 1 PBKiran PantheeNo ratings yet
- Abstract Booklet 2010Document50 pagesAbstract Booklet 2010Danijela VukicevicNo ratings yet
- 1377 FullDocument23 pages1377 FullPutri Wahyuni AllfazmyNo ratings yet
- Prenatal 3Document6 pagesPrenatal 3nur fadhilahNo ratings yet
- Developmental Outcomes of OKDocument12 pagesDevelopmental Outcomes of OKIkaDian PuspitanzaNo ratings yet
- Universal Newborn Hearing Screening 2001Document11 pagesUniversal Newborn Hearing Screening 2001Alexander AdrielNo ratings yet
- life-14-00480Document13 pageslife-14-00480Shahmeer HassanNo ratings yet
- Dhawan 2016Document6 pagesDhawan 2016lilisNo ratings yet
- Cord Serum Albumin Predicts Risk of Neonatal JaundiceDocument3 pagesCord Serum Albumin Predicts Risk of Neonatal JaundiceSuman MondalNo ratings yet
- JCP 10 3 85983Document6 pagesJCP 10 3 85983Davit SoesantoNo ratings yet
- Bosanquet Etal DMCN 2013Document9 pagesBosanquet Etal DMCN 2013ramopavelNo ratings yet
- Risk Factors For Hypoxic Ischemic Encephalopathy in ChildrenDocument5 pagesRisk Factors For Hypoxic Ischemic Encephalopathy in ChildrenSaqib AtherNo ratings yet
- Meta AnalysisDocument16 pagesMeta AnalysisSabu Joseph100% (1)
- Icbt07i4p369 PDFDocument6 pagesIcbt07i4p369 PDFretNo ratings yet
- DMCN 14205Document8 pagesDMCN 14205rgo17No ratings yet
- JurdingDocument6 pagesJurdingsiti hazard aldinaNo ratings yet
- HineDocument7 pagesHineAkhila Chowdary100% (1)
- Neonatal MRI To Predict Neurodevelopmental Outcomes in Preterm InfantsDocument10 pagesNeonatal MRI To Predict Neurodevelopmental Outcomes in Preterm InfantsJuan Camilo LandazuriNo ratings yet
- Khan 2014Document11 pagesKhan 2014RelviGuzmanApazaNo ratings yet
- Neuroimagenes en Preterminos y Rendimiento EscolarDocument15 pagesNeuroimagenes en Preterminos y Rendimiento EscolarAlejandroVeraVargasNo ratings yet
- Grzeskowiak Et al-2016-BJOG: An International Journal of Obstetrics & GynaecologyDocument10 pagesGrzeskowiak Et al-2016-BJOG: An International Journal of Obstetrics & GynaecologyPrima Hari PratamaNo ratings yet
- The Newborn Early Warning (NEW) System: Development of An At-Risk Infant Intervention SystemDocument5 pagesThe Newborn Early Warning (NEW) System: Development of An At-Risk Infant Intervention Systemeneng latipa dewi100% (1)
- Valcamonico 2007Document7 pagesValcamonico 2007Lissaberti AmaliahNo ratings yet
- Evidencias VojtaDocument9 pagesEvidencias VojtaRommel AndresNo ratings yet
- INFANIBDocument8 pagesINFANIBandrea sierraNo ratings yet
- Estudio Del Desarrollo Psicomotor en Pacientes Prematuros Durante El Primer Año de VidaDocument4 pagesEstudio Del Desarrollo Psicomotor en Pacientes Prematuros Durante El Primer Año de VidaKrla OrellNo ratings yet
- Articol 1Document7 pagesArticol 1nistor97No ratings yet
- Prematurity Effects on Auditory Brainstem ResponseDocument8 pagesPrematurity Effects on Auditory Brainstem ResponseHanum AmeliaNo ratings yet
- pr201825 PDFDocument6 pagespr201825 PDFlama mansourNo ratings yet
- Retrospective Analysis of Risk Factors For Low 1-Minute Apgar Scores in Term NeonatesDocument10 pagesRetrospective Analysis of Risk Factors For Low 1-Minute Apgar Scores in Term Neonatesputri vinia /ilove cuteNo ratings yet
- Risk Factors For Neonatal Asphyxia Occurrence at General Hospital Dr. M. Soewandhie, SurabayaDocument6 pagesRisk Factors For Neonatal Asphyxia Occurrence at General Hospital Dr. M. Soewandhie, SurabayaFatimah FadilahNo ratings yet
- Hammersmith NeonatalDocument3 pagesHammersmith Neonataljulianamd87No ratings yet
- Pregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsFrom EverandPregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsNo ratings yet
- Mongolian SpotsDocument9 pagesMongolian SpotsiekafzNo ratings yet
- Monitoring Vital Signs Detects COVID-19 Using WearablesDocument7 pagesMonitoring Vital Signs Detects COVID-19 Using WearablesMaxandrea Beatrice ArmillaNo ratings yet
- Jurnal AnestesiDocument5 pagesJurnal AnestesiridwanNo ratings yet
- 1 SMDocument7 pages1 SMPiaggio PIAGGIONo ratings yet
- Mumps StudyDocument10 pagesMumps StudyNational Content DeskNo ratings yet
- Open - Oregonstate.education-Foundations of EpidemiologyDocument11 pagesOpen - Oregonstate.education-Foundations of EpidemiologyAMANE COTTAGE HOSPITALNo ratings yet
- Hydrocephalus 9Document9 pagesHydrocephalus 9Shesly PhilominaNo ratings yet
- Meeting The Evolving Demands of Neurointervention: Implementation and Utilization of Nurse PractitionersDocument5 pagesMeeting The Evolving Demands of Neurointervention: Implementation and Utilization of Nurse PractitionersAANPNo ratings yet
- Diabetes HandbookDocument198 pagesDiabetes HandbookKeerthana SivarasaNo ratings yet
- Pulmonary Hypertension: Annals of Internal MedicinetDocument16 pagesPulmonary Hypertension: Annals of Internal MedicinetAlicia TGNo ratings yet
- ASSESSMENT SummerDocument1 pageASSESSMENT SummerThoyotsukha Faeldan123No ratings yet
- Opportunistic Mycoses: Portal of Entry: Respiratory, Mucocutaneous Infectious Particles: Conidia, MyceliaDocument4 pagesOpportunistic Mycoses: Portal of Entry: Respiratory, Mucocutaneous Infectious Particles: Conidia, MyceliaPinay YaunNo ratings yet
- 4 Curs Osteomielita Engl BunDocument41 pages4 Curs Osteomielita Engl BunCatalin PaulNo ratings yet
- Maxillary Immediate Denture: A Case Report: International Journal of Medical and Health ResearchDocument3 pagesMaxillary Immediate Denture: A Case Report: International Journal of Medical and Health Researchnur aslindahNo ratings yet
- Lock, 2010. Treatment Review Adolescent EDDocument13 pagesLock, 2010. Treatment Review Adolescent EDCarolina GarayNo ratings yet
- Pressuring of Acupoints As A Complement To The - 2019 - Journal of AcupunctureDocument9 pagesPressuring of Acupoints As A Complement To The - 2019 - Journal of AcupunctureMatias DamiánNo ratings yet
- Journal Reading (LRDR)Document2 pagesJournal Reading (LRDR)Andrea Albester GarinoNo ratings yet
- Glossary of Patient SafetyDocument352 pagesGlossary of Patient SafetyEman ShalabyNo ratings yet
- Cholecystitis - Complications of Cholecystitis A Comprehensive Contemporary Imaging ReviewDocument17 pagesCholecystitis - Complications of Cholecystitis A Comprehensive Contemporary Imaging ReviewSamuel WidjajaNo ratings yet
- Comprehensive Edited)Document82 pagesComprehensive Edited)mikrobyo_ng_wmsuNo ratings yet
- DulcolaxDocument1 pageDulcolaxKatie McPeekNo ratings yet
- NCLEX Review Question 101-200Document14 pagesNCLEX Review Question 101-200Felimon BugtongNo ratings yet
- Improvement of Pregnant Women Visit in Puskesmas As An Effect of Using Ultrasound in Pregnancy ExaminationDocument12 pagesImprovement of Pregnant Women Visit in Puskesmas As An Effect of Using Ultrasound in Pregnancy ExaminationKharinaNo ratings yet
- MERGEFDocument383 pagesMERGEFmadison DeliNo ratings yet
- Corona Virus: Project COVID-19Document5 pagesCorona Virus: Project COVID-19SiaNo ratings yet
- Open LetterDocument3 pagesOpen Letterapi-652435946No ratings yet
- IM ITE D: Reading Sub-TestDocument20 pagesIM ITE D: Reading Sub-TestAlwin BrightNo ratings yet