Professional Documents
Culture Documents
Mechanisms of Pain
Uploaded by
Pembaca sejatiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mechanisms of Pain
Uploaded by
Pembaca sejatiCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/11784538
Mechanisms of pain
Article in Proceedings of the National Academy of Sciences · November 2001
DOI: 10.1073/pnas.211373398 · Source: PubMed
CITATIONS READS
115 1,082
3 authors, including:
Cheryl Stucky
Medical College of Wisconsin
182 PUBLICATIONS 10,288 CITATIONS
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
TRPA1 in inflammatory pain View project
Mechanisms of sanshool-induced paresthesia View project
All content following this page was uploaded by Cheryl Stucky on 02 December 2014.
The user has requested enhancement of the downloaded file.
From the Academy
Mechanisms of pain
Cheryl L. Stucky*†, Michael S. Gold‡, and Xu Zhang§
*Department of Cell Biology, Neurobiology, and Anatomy, Medical College of Wisconsin, Milwaukee, WI 53226; ‡Department of Oral and Craniofacial
Biological Sciences, University of Maryland, Baltimore, MD 21201; and §Institute of Neuroscience, Shanghai Institute of Life Sciences,
Chinese Academy of Sciences, Shanghai 200031, China
Persistent or chronic pain is the primary reason people seek medical care, yet current therapies are either inadequate for certain types
of pain or cause intolerable side effects. Recently, pain neurobiologists have identified a number of cellular and molecular processes that
lead to the initiation and maintenance of pain. Understanding these underlying mechanisms has given significant promise for the
development of more effective, more specific pain therapies in the near future.
Persistent Pain Is a Major Public Health Problem Today properties of neurotransmitters, receptors, and ion channels can
ultimately result in increased functional activity of neurons in the
O ver one-third of the world’s population suffers from persistent
or recurrent pain, costing the American public alone approx-
imately $100 billion each year in health care, compensation, and
pain pathway. Conversely, plasticity can decrease the body’s own
pain inhibitory systems, resulting ultimately in increased pain.
litigation (1). Chronic pain is associated with conditions such as Injury, inflammation, and disease can all cause neuronal plasticity
back injury, migraine headaches, arthritis, herpes zoster, diabetic and increased pain by means of increased excitatory or decreased
neuropathy, temporomandibular joint syndrome, and cancer. Many inhibitory mechanisms. Plasticity can result in short-term changes
of the currently available pain therapies are either inadequate or that last minutes to hours, or long-term changes which may be
cause uncomfortable to deleterious side effects. Chronic pain permanent.
results not just from the physical insult but also from a combination Why Focus on the Primary Afferent Neuron?
of physical, emotional, psychological, and social abnormalities.
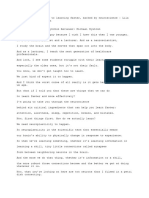
Pain transduction and perception is extensive and complex, involv-
Because many pains persist after an insult is healed, the ongoing
ing fundamental biological events at multiple levels of the nervous
pain rather than the injury underlies the patient’s disability. Un-
system (Fig. 1). Our Frontiers of Science session was not intended
treated pain may become self-perpetuating because pain has im-
to be a comprehensive review of the latest findings at all levels of
munosuppressive effects that leave patients susceptible to subse-
the pain pathway. Instead, we focused on the place where sensation
quent diseases. It is now clear that if we can effectively treat the pain
of pain is initiated, the primary afferent nociceptor. Nociceptors are
despite the underlying cause, it will be possible for patients to regain
a subpopulation of primary sensory neurons that are activated by
normal functioning. The key to more successful pain treatment is
‘‘noxious’’ stimuli, i.e., stimuli that can produce tissue damage.
to understand the mechanisms that generate and maintain chronic
Compelling evidence suggests that plasticity in nociceptors contrib-
pain.
utes substantially to the increased pain one feels in the presence of
FROM THE
ACADEMY
Why Is Pain a New Frontier of Science? injury. Plasticity in nociceptors is critical for both the development
The onset of the 21st century is an incredibly exciting time in pain and maintenance of plasticity in the central nervous system (2).
biology. Information from recent studies in basic pain research is That many receptors and ion channels recently identified are
virtually exploding and has revealed numerous novel targets for the found specifically in nociceptors makes these proteins very good
advent of new pain therapies. Major advances have occurred at targets for eliminating pain without inducing side effects. Finally,
levels spanning from molecular studies that have identified trans- the accessibility of the peripheral nervous system makes noci-
duction proteins in nociceptors to cortical imaging studies which ceptors a logical target for the development of novel therapeutic
reveal how pain is experienced on a cognitive level (2, 3). Two key interventions.
lines of discovery have been (i) molecular兾cellular transduction Do Specific Types of Nociceptors Mediate Different
mechanisms and (ii) neuronal plasticity. Types of Pain?
Molecular兾Cellular Mechanisms Nociceptors are extremely heterogeneous, differing in the neuro-
Elegant molecular genetic studies conducted in the past few years transmitters they contain, the receptors and ion channels they
have now enabled us to identify specific molecules that are involved express, their speed of conduction, their response properties to
in the processes of pain transduction. A giant step forward came noxious stimuli, and their capacity to be sensitized during inflam-
with the identification of proteins called vanilloid receptors, which mation, injury, and disease. Significant progress toward alleviating
allow us to detect noxious heat (4, 5). The VR1 protein is a heat pain will occur if we are able to achieve the following goals: (i)
transducer because it converts thermal energy into an electrical determine the function of these different subpopulations of noci-
signal (action potentials) that is sent to the central nervous system, ceptors, (ii) determine whether specific subpopulations mediate
enabling us to detect a stimulus as painfully hot. Without the VR1 distinct types of pain, and (iii) identify what cellular and molecular
receptor, one does not effectively detect noxious heat, particularly targets are altered on specific populations of nociceptors during
in the setting of inflammation (6, 18). Recently, basic pain research- different types of pain. Ultimately, these aims will allow the
ers have identified a number of transduction molecules that will
clearly be key targets in developing pioneering pain therapies (7).
This paper is a summary of a session presented at the third annual Chinese–American
Neuronal Plasticity Frontiers of Science symposium, held October 20 –22, 2000, at the Arnold and Mabel
Plasticity is a term used to refer to changes that occur in the Beckman Center of the National Academies of Science and Engineering in Irvine, CA.
established nervous system. Changes in neuronal structure; con- Abbreviations: IB4, isolectin B4; CCK, cholecystokinin.
nections between neurons; and alterations in the quantity and †To whom reprint requests should be addressed. E-mail: cstucky@mcw.edu.
www.pnas.org兾cgi兾doi兾10.1073兾pnas.211373398 PNAS 兩 October 9, 2001 兩 vol. 98 兩 no. 21 兩 11845–11846
neuropeptides but expresses a surface carbohydrate group that
selectively binds to a plant lectin called isolectin B4 (IB4). This
subpopulation of neurons is supported by glial-derived neurotro-
phic factor during early postnatal development (9, 10). The IB4-
binding neurons project to a different region of the spinal dorsal
horn (inner lamina II) that contains primarily local spinal inter-
neurons. Important questions are whether these two types of
nociceptors have different functional responses to painful stimuli
and whether they have distinct roles in specific types of pain.
We use isolated sensory neurons to examine the response
properties of nociceptors to painful stimuli. By using patch-clamp-
recording techniques, we found that IB4-positive nociceptors have
larger magnitude voltage-gated sodium currents. In contrast, IB4-
negative nociceptors had larger noxious heat-induced ion currents,
suggesting that IB4-negative nociceptors are the nociceptors that
respond intensely to noxious heat (11). In addition, IB4-negative
nociceptors are much more responsive to noxious chemicals that
Fig. 1. Painful stimuli such are elevated during inflammation, including low pH and serotonin
as intense heat activate the (C.L.S., unpublished data). One hypothesis, which remains to be
peripheral terminals of noci-
tested, is that IB4-positive nociceptors mediate neuropathic pain,
ceptors. Action potentials are
transmitted along the affer-
whereas IB4-negative nociceptors mediate inflammatory pain (12).
ent axons to the spinal cord. Why Is Morphine Ineffective in Treating Nerve Injury Pain?
The central terminals of IB4-
Opioid analgesics such as morphine are universally regarded as the
negative unmyelinated noci-
ceptors synapse in lamina I
most powerful pain-relieving drugs. Morphine acts through the
and outer lamina II, whereas -opioid receptor to inhibit signals that transmit pain (13). Pain that
IB4-positive unmyelinated no- follows direct injury to a peripheral nerve is called neuropathic pain.
ciceptors terminate in inner Unfortunately, it is still not known what mechanisms underlie this
lamina II. By means of chemi- prevalent pain syndrome. Neuropathic pain is an anomaly because
cal transmission, nociceptors it is insensitive to morphine as well as other opioid drugs and is
activate spinal neurons that currently best managed with antidepressants and antiepileptics (14).
send axons across the spinal Neuropathic pain may be insensitive to morphine because damage
cord and up fiber tracts and
of primary afferent nerves results in decreased expression of
terminate in the medulla,
midbrain, and thalamus. Tha-
-opioid receptors on nociceptors and spinal neurons in the pain
lamic neurons project to re- pathway, thus reducing the efficacy of morphine (15). In addition,
gions of the cortex including other substances may modulate the efficacy of morphine. For
the somatosensory cortex. example, when the neuropeptide cholecystokinin (CCK) is applied
to the spinal cord, it reduces the inhibitory effects of morphine (16).
At the cellular level, -receptors and CCK receptors are expressed
in the same spinal neurons, suggesting that CCK may directly inhibit
development of novel pain therapies that target specific mecha-
actions of morphine by means of signaling mechanisms within a
nisms on identified populations of nociceptors. given neuron (17). Furthermore, activation of -receptors increases
Nociceptors can be divided into two general types. A-fiber release of CCK neuropeptide, which then reduces the effectiveness
nociceptors have lightly myelinated axons, conduct action potentials of morphine in a feedback manner (17). Thus, multiple mecha-
rapidly, and have medium- to large-diameter cell bodies. A-fibers nisms, including decreased -receptors and increased CCK-
mediate the fast, pricking quality of pain. C-fibers have unmyeli- induced inhibition of morphine, make opioids ineffective in treating
nated axons, conduct action potentials slowly, and have small- neuropathic pain.
diameter cell bodies. C-fibers mediate the slower, burning quality Understanding the molecular and cellular mechanisms that
of pain. C-fibers comprise around 70% of all nociceptors. Two underlie the initiation of pain and the development and main-
classes of C-fibers have been identified. One class contains a variety tenance of plasticity in primary afferent and spinal neurons will
of neuropeptides, including substance P and calcitonin gene-related undoubtedly reveal novel targets for the discovery of more
peptide, and expresses trkA receptors, the high-affinity receptor for effective, more specific pain therapies.
nerve growth factor (8). These neurons project to the outermost
region of the spinal dorsal horn (lamina I and outer lamina II) and This work was supported by National Institutes of Health Grants
terminate largely on spinal neurons that project to higher-order NS40538-01 (to C.L.S.) and NS36929 (to M.S.G.), and by Nature Science
pain centers in the brain (Fig. 1). The other class contains few Foundation of China Grant 39840160 (to X.Z.).
1. Loeser, J. D., Butler, S. H., Chapman, C. R. & Turk, K. C., eds. (2001) Bonica’s Management 10. Bennett, D. L., Michael, G. J., Ramachandran, N., Munson, J. B., Averill, S., Yan, Q.,
of Pain (Lippincott, Philadelphia). McMahon, S. B. & Priestley, J. V. (1998) J. Neurosci. 18, 3059–3072.
2. Woolf, C. J. & Salter, M. W. (2000) Science 288, 1765–1768. 11. Stucky, C. L. & Lewin, G. R. (1999) J. Neurosci. 19, 6497–6505.
3. Hunt, S. P. & Mantyh, P. W. (2001) Nat. Rev. Neurosci. 2, 83–91. 12. Snider, W. D. & McMahon, S. B. (1998) Neuron 20, 629–632.
4. Caterina, M. J., Schumacher, M. A., Tominaga, M., Rosen, T. A., Levine, J. D. & Julius, D. 13. Matthes, H. W., Maldonado, R., Simonin, F., Valverde, O., Slowe, S., Kitchen, I., Befort, K., Dierich,
(1997) Nature (London) 389, 816–824. A., Le Meur, M., Dolle, P., et al. (1996) Nature (London) 383, 819–823.
5. Caterina, M. J., Rosen, T. A., Tominaga, M., Brake, A. J. & Julius, D. (1999) Nature
14. Watson, C. P. (2000) Clin. J. Pain 16, Suppl., S49–S55.
(London) 398, 441–446.
15. Zhang, X., Bao, L., Shi, T. J., Ju, G., Elde, R. & Hokfelt, T. (1998) Neuroscience 82, 223–240.
6. Caterina, M. J., Leffler, A., Malmberg, A. B., Martin, W. J., Trafton, J., Petersen-Zeitz,
K. R., Koltzenburg, M., Basbaum, A. I. & Julius, D. (2000) Science 288, 306–313. 16. Kellstein, D. E., Price, D. D. & Mayer, D. J. (1991) Brain Res. 540, 302–306.
7. McCleskey, E. W. & Gold, M. S. (1999) Annu. Rev. Physiol. 61, 835–856. 17. Zhang, X., de Araujo, Lucas, G., Elde, R., Wiesenfeld-Hallin, Z. & Hokfelt, T. (2000)
8. Averill, S., McMahon, S. B., Clary, D. O., Reichardt, L. F. & Priestley, J. V. (1995) Eur. Neuroscience 95, 197–207.
J. Neurosci. 7, 1484–1494. 18. Davis, J. B., Gray, J., Gunthorpe, M. J., Hatcher, J. P., Davey, P. T., Overend, P.,
9. Molliver, D. C., Wright, D. E., Leitner, M. L., Parsadanian, A. S., Doster, K., Wen, D., Yan, Harries, M. H., Latcham, J., Clapham, C., Atkinson, K., et al. (2000) Nature (London)405,
Q. & Snider, W. D. (1997) Neuron 19, 849–861. 183–187.
11846 兩 www.pnas.org兾cgi兾doi兾10.1073兾pnas.211373398 Stucky et al.
View publication stats
You might also like
- نسخة Lecture - PAIN Assessment & ManagementDocument52 pagesنسخة Lecture - PAIN Assessment & Managementjsoal100% (1)
- Flow State Brainwave Entrainment GuideDocument36 pagesFlow State Brainwave Entrainment Guidekriskris12345No ratings yet
- Pathophysiology of Pain: A Practical PrimerDocument7 pagesPathophysiology of Pain: A Practical PrimerAngelina FebrianNo ratings yet
- Neuropathic Myofascial PainDocument18 pagesNeuropathic Myofascial PainAngela PagliusoNo ratings yet
- Referred Muscle Pain Basic and Clinical FindingsDocument9 pagesReferred Muscle Pain Basic and Clinical FindingsaavalverdeNo ratings yet
- Sensation and Perception 9th Edition Goldstein Test BankDocument10 pagesSensation and Perception 9th Edition Goldstein Test Bankmelissaperezwzoeaksjgn100% (13)
- For Nasari 2012Document8 pagesFor Nasari 2012basma adianaNo ratings yet
- Future of Pain - MelzacDocument1 pageFuture of Pain - MelzacJonasMarçaloNo ratings yet
- Central Mechanisms of Pathological PainDocument9 pagesCentral Mechanisms of Pathological PainRocio DominguezNo ratings yet
- Central Sensitization Implications For The Diagnosis and Treatment of PainDocument14 pagesCentral Sensitization Implications For The Diagnosis and Treatment of PainrameshkulkarNo ratings yet
- NIH Public Access: Author ManuscriptDocument31 pagesNIH Public Access: Author Manuscriptvicente gaticaNo ratings yet
- Artigos Coderre1997Document65 pagesArtigos Coderre1997JonasMarçaloNo ratings yet
- Original Reports: Characterization of Hyperacute Neuropathic Pain After Spinal Cord Injury: A Prospective StudyDocument9 pagesOriginal Reports: Characterization of Hyperacute Neuropathic Pain After Spinal Cord Injury: A Prospective Studyezequiel zaragoza juarezNo ratings yet
- Pain Conundrums - Which Hypothesis - Central Nervous System Sensitization Versus Peripheral AMM Nov 2 - 0Document3 pagesPain Conundrums - Which Hypothesis - Central Nervous System Sensitization Versus Peripheral AMM Nov 2 - 0mirimatuNo ratings yet
- Vol47 03 ReviewDocument23 pagesVol47 03 ReviewOla AwnyNo ratings yet
- The Neurobiology of Acute PainDocument8 pagesThe Neurobiology of Acute PainEduardoSilveiraNo ratings yet
- Finnerup Et Al 2020 Neuropathic Pain From Mechanisms To TreatmentDocument44 pagesFinnerup Et Al 2020 Neuropathic Pain From Mechanisms To TreatmentintermediosamberesNo ratings yet
- Cambios Neuroplasticos en El Dolor Musculo Esqueletico Crónico Un Revision 2012Document18 pagesCambios Neuroplasticos en El Dolor Musculo Esqueletico Crónico Un Revision 2012Daniela Leyton PezoaNo ratings yet
- NIH Public Access: Author ManuscriptDocument33 pagesNIH Public Access: Author ManuscriptMarcus Dos SantosNo ratings yet
- 875111Document6 pages875111Sms KhNo ratings yet
- Nihms 396443Document12 pagesNihms 396443kickinghorse892No ratings yet
- Pain ProcessingDocument12 pagesPain ProcessingKunal KatyayanNo ratings yet
- The Physiology of Pain Mechanisms: From The Periphery To The BrainDocument26 pagesThe Physiology of Pain Mechanisms: From The Periphery To The BrainEto ShengeliaNo ratings yet
- 2014 Chronic Pain. The Role of Learning and Brain PlasticityDocument12 pages2014 Chronic Pain. The Role of Learning and Brain PlasticityCristian OyarzoNo ratings yet
- New Concept of Pain and Treatment of Spinal Segmental SensitizationDocument3 pagesNew Concept of Pain and Treatment of Spinal Segmental Sensitizationheaven6938No ratings yet
- Pathological Pain and The Neuroimmune InterfaceDocument36 pagesPathological Pain and The Neuroimmune InterfacecontatofornazaNo ratings yet
- Tracey (2007) - The Cerebral Signature For Pain Perception and Its ModulationDocument15 pagesTracey (2007) - The Cerebral Signature For Pain Perception and Its ModulationLuciana AraújoNo ratings yet
- Pain Classifitation 2 PDFDocument11 pagesPain Classifitation 2 PDFAnnisa BrilianNo ratings yet
- Neuropathic Pain: Redefinition and A Grading System For Clinical and Research Purposes - TreedeDocument8 pagesNeuropathic Pain: Redefinition and A Grading System For Clinical and Research Purposes - TreedeNahu SteinmannNo ratings yet
- Biomedicine & Pharmacotherapy: S. Ronchetti, G. Migliorati, D.V. Del FinoDocument8 pagesBiomedicine & Pharmacotherapy: S. Ronchetti, G. Migliorati, D.V. Del FinoPutri Aswariyah RamliNo ratings yet
- Topical Meds for Neuropathic Orofacial PainDocument13 pagesTopical Meds for Neuropathic Orofacial PainMarco Antonio Morales OsorioNo ratings yet
- Neuropathic Pain A Maladaptive Response of The NerDocument34 pagesNeuropathic Pain A Maladaptive Response of The NerMayNo ratings yet
- PCT 2Document20 pagesPCT 2Wialda Dwi rodyahNo ratings yet
- SC 2015225Document11 pagesSC 2015225elbueno21No ratings yet
- 2010 Acute Pain - MurphyDocument10 pages2010 Acute Pain - MurphypNo ratings yet
- TL 1Document4 pagesTL 1ĐôngNo ratings yet
- Cervero 2000 (Neurobiologia Del Dolor)Document5 pagesCervero 2000 (Neurobiologia Del Dolor)Valery Andrea Sáez VegaNo ratings yet
- UntitledDocument5 pagesUntitledClinton MandelaNo ratings yet
- Ain and Sycho Affective IsordersDocument20 pagesAin and Sycho Affective IsordersmoiNo ratings yet
- Neuropathic Painn PDFDocument20 pagesNeuropathic Painn PDFkaktusNo ratings yet
- Astrocytes in Chronic Pain and ItchDocument19 pagesAstrocytes in Chronic Pain and ItchMerly JHNo ratings yet
- Mechanisms of Acupuncture-Electroacupuncture On Persistent PainDocument38 pagesMechanisms of Acupuncture-Electroacupuncture On Persistent PainPaulo SantosNo ratings yet
- 2017 A Neurobiologist's Attempt To Understand Persistent PainDocument8 pages2017 A Neurobiologist's Attempt To Understand Persistent PainCristian OyarzoNo ratings yet
- Cagnie2013 Physiological Effects of Dry NeedlingDocument8 pagesCagnie2013 Physiological Effects of Dry NeedlingWahyu FathurrachmanNo ratings yet
- Introduction: Recommendations For The Diagnosis, Assessment, and Treatment of Neuropathic PainDocument2 pagesIntroduction: Recommendations For The Diagnosis, Assessment, and Treatment of Neuropathic PainFran WermannNo ratings yet
- Exercise and Neuropathic Pain: A General Overview of Preclinical and Clinical ResearchDocument16 pagesExercise and Neuropathic Pain: A General Overview of Preclinical and Clinical ResearchderisonmarsinovabakaraNo ratings yet
- Greene, S. A. Chronic Pain Pathophysiology and Treatment Implications. Topics in Companion Animal Medicine, v.25, n.1, p.5-9. 2010 PDFDocument5 pagesGreene, S. A. Chronic Pain Pathophysiology and Treatment Implications. Topics in Companion Animal Medicine, v.25, n.1, p.5-9. 2010 PDFFran WermannNo ratings yet
- Neuropathic Pain: Definition, Assessment and Epidemiology: SciencedirectDocument10 pagesNeuropathic Pain: Definition, Assessment and Epidemiology: SciencedirectLidwina ApyakaNo ratings yet
- Neuroscience and Biobehavioral Reviews: Xiao Xiao, Yu-Qiu ZhangDocument12 pagesNeuroscience and Biobehavioral Reviews: Xiao Xiao, Yu-Qiu ZhangYoga MatNo ratings yet
- Pain Theories PDFDocument7 pagesPain Theories PDFAndreea-Alexandra LupuNo ratings yet
- Euroscience: Molecular, Cellular and Circuit Basis of Cholinergic Modulation of PainDocument14 pagesEuroscience: Molecular, Cellular and Circuit Basis of Cholinergic Modulation of PainPriyabrata HalderNo ratings yet
- FSP DolorDocument15 pagesFSP DoloranyNo ratings yet
- Fneur 14 1104817Document6 pagesFneur 14 1104817geowalker7092No ratings yet
- Peripheral and Central Hyperexcitability: Differential Signs and Symptoms in Persistent PainDocument16 pagesPeripheral and Central Hyperexcitability: Differential Signs and Symptoms in Persistent PainJonasMarçaloNo ratings yet
- Barriers To Reconceptulization of Chronic Pain Moseley PDFDocument6 pagesBarriers To Reconceptulization of Chronic Pain Moseley PDFpfi_jenNo ratings yet
- Trigger Point PhenomenaDocument8 pagesTrigger Point PhenomenaMario Tapia LeitonNo ratings yet
- TL 4Document4 pagesTL 4ĐôngNo ratings yet
- Neuronal CC Chemokines: The Distinct Roles of CCL21 and CCL2 in Neuropathic PainDocument10 pagesNeuronal CC Chemokines: The Distinct Roles of CCL21 and CCL2 in Neuropathic Painrocambolescas perthNo ratings yet
- AliliDocument3 pagesAliliSaf Tanggo DiampuanNo ratings yet
- Mechanisms and Manifestations in Musculoskeletal.4 PDFDocument17 pagesMechanisms and Manifestations in Musculoskeletal.4 PDFRodrigo Yarzábal RodríguezNo ratings yet
- Fdocuments - in - The Puzzle of Pain Loss of Mobility Evasive Movements The Puzzle of PainDocument21 pagesFdocuments - in - The Puzzle of Pain Loss of Mobility Evasive Movements The Puzzle of PainMARIA TERAPEUTANo ratings yet
- Chronic Myeloid Leukemia: 2020 Update On Diagnosis, Therapy and MonitoringDocument19 pagesChronic Myeloid Leukemia: 2020 Update On Diagnosis, Therapy and MonitoringPembaca sejatiNo ratings yet
- USG Doppler Principles and ApplicationsDocument4 pagesUSG Doppler Principles and ApplicationsPembaca sejatiNo ratings yet
- AddictionscienceDocument75 pagesAddictionsciencePembaca sejatiNo ratings yet
- List Obat Baksos NasionalDocument2 pagesList Obat Baksos NasionalPembaca sejatiNo ratings yet
- Sleep An Elixir For LifeDocument3 pagesSleep An Elixir For LifederrickNo ratings yet
- Script 2Document6 pagesScript 2pjoyie0708No ratings yet
- PM3102 Q1Document4 pagesPM3102 Q1rexlloydNo ratings yet
- Final Report BioDocument27 pagesFinal Report BioR FaNo ratings yet
- My Psychology 1st Edition Pomerantz Test BankDocument70 pagesMy Psychology 1st Edition Pomerantz Test Banklinda100% (22)
- Levin - Godukhin - 2017 - Modulating Effect of Cytokines On Mechanisms of Synaptic Plasticity in The BrainDocument11 pagesLevin - Godukhin - 2017 - Modulating Effect of Cytokines On Mechanisms of Synaptic Plasticity in The Brainkeon.arbabi.altNo ratings yet
- Daytime ParahypnagogiaDocument4 pagesDaytime ParahypnagogiaInnerslightNo ratings yet
- Anatomy Physiology and Disease Foundations For The Health Professions 1st Edition Roiger Solutions Manual Full Chapter PDFDocument58 pagesAnatomy Physiology and Disease Foundations For The Health Professions 1st Edition Roiger Solutions Manual Full Chapter PDFrelatermotifef4oq100% (10)
- Nervous System ReviewerDocument26 pagesNervous System ReviewerAllea Marie SabacNo ratings yet
- Module 19Document135 pagesModule 19leomillmendiolaNo ratings yet
- The Physical Self: Brain and The Nervous SystemDocument4 pagesThe Physical Self: Brain and The Nervous System2022105340No ratings yet
- Fluent Speech Neural Basis of Sensorimotor Plasticity in Developmental StutteringDocument32 pagesFluent Speech Neural Basis of Sensorimotor Plasticity in Developmental StutteringLidaConstanzaMendezNo ratings yet
- The Utility of Non-Invasive Brain Stimulation in RDocument10 pagesThe Utility of Non-Invasive Brain Stimulation in RsanagaumiNo ratings yet
- Specialized Astrocytes Mediate Glutamatergic Gliotransmission in The CNSDocument47 pagesSpecialized Astrocytes Mediate Glutamatergic Gliotransmission in The CNSCARDIO 2019No ratings yet
- Introduction To Biopsychology Global 9th Edition Pinel Solutions ManualDocument38 pagesIntroduction To Biopsychology Global 9th Edition Pinel Solutions Manualhudsoncolepiu100% (9)
- Tercer Informe de FisiologiaDocument6 pagesTercer Informe de FisiologiaYanet Onofre PilcoNo ratings yet
- BrainDocument11 pagesBrainAICHANo ratings yet
- Ch03 Questions Answer KeyDocument18 pagesCh03 Questions Answer KeyMichaelNo ratings yet
- Brain Bee R1 P2Document9 pagesBrain Bee R1 P2sarahsyedazakiNo ratings yet
- Sherman Et Al 2023 Multiple Memory Subsystems Reconsidering Memory in The Mind and BrainDocument23 pagesSherman Et Al 2023 Multiple Memory Subsystems Reconsidering Memory in The Mind and BrainChris InNottsNo ratings yet
- Week 11 Content List AND ActivityDocument3 pagesWeek 11 Content List AND ActivityKaitlyn RobisonNo ratings yet
- Biological Basis of Learning and MemoryDocument30 pagesBiological Basis of Learning and MemoryParamesh WaranNo ratings yet
- Cerebral CortexDocument15 pagesCerebral Cortexasa24693No ratings yet
- CNS NeurotransmitterDocument67 pagesCNS NeurotransmitterGreenNo ratings yet
- Mapping Bellvitge 2023Document8 pagesMapping Bellvitge 2023Lluís Cavallé MorenoNo ratings yet
- Learning Objectives Task 1 Attention Perception and Mtor DevelopmentDocument4 pagesLearning Objectives Task 1 Attention Perception and Mtor DevelopmentCarmi ScholtzNo ratings yet
- Molecular Mechanisms Memory FormationDocument6 pagesMolecular Mechanisms Memory FormationdevyaalogeshNo ratings yet
- Nervous System Reflexes and Senses: Physiology Lab-4 October, 2018Document21 pagesNervous System Reflexes and Senses: Physiology Lab-4 October, 2018Madhu LodhiNo ratings yet