Professional Documents
Culture Documents
0068KJR - KJR 10 121
Uploaded by
Astrid GayatriOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
0068KJR - KJR 10 121
Uploaded by
Astrid GayatriCopyright:
Available Formats
Necrotizing Fasciitis versus Pyomyositis:
Discrimination with Using MR Imaging
Jee Hyun Seok, MD1
Objective: We wanted to evaluate the MR findings for differentiating between
Won-Hee Jee, MD1
necrotizing fasciitis (NF) and pyomyositis (PM).
Kyung-Ah Chun, MD1
Ji-Young Kim, MD1 Materials and Methods: The MR images of 19 patients with surgically con-
Chan-Kwon Jung, MD2 firmed NF (n = 11) and pathologically confirmed PM (n = 8) were retrospectively
Yang Ree Kim, MD3 reviewed with regard to the presence or absence of any MRI finding criteria that
could differentiate between them.
Wan-Kyu Eo, MD5
Yang-Soo Kim, MD4 Results: The patients with NF had a significantly greater prevalence of the fol-
Yang Guk Chung, MD4 lowing MR findings (p < 0.05): a peripheral band-like hyperintense signal in mus-
cles on fat-suppressed T2-weighted images (73% of the patients with NF vs. 0%
of the patients with PM), peripheral band-like contrast enhancement (CE) of mus-
cles (82% vs. 0%, respectively) and thin smooth enhancement of the deep fascia
(82% vs. 13%, respectively). The patients with PM had a significantly greater
prevalence of the following MRI findings (p < 0.05): a diffuse hyperintense signal
in muscles on fat-suppressed T2-weighted images (27% of the patients with NF
vs. 100% in the patients with PM), diffuse CE of muscles (18% vs. 100%, respec-
Index terms :
Soft tissue tively), thick irregular enhancement of the deep fascia (0% vs. 75%, respectively)
Infection and intramuscular abscess (0% vs. 88%, respectively). For all patients with NF
Necrotizing fasciitis and PM, the superficial fascia and muscle showed hyperintense signals on T2-
Pyomyositis, MR weighted images and CE was seen on fat-suppressed CE T1-weighted images.
The subcutaneous tissue and deep fascia showed hyperintense signals on T2-
DOI:10.3348/kjr.2009.10.2.121
weighted images and CE was seen in all the patients with NF and in seven
(88%) of the eight patients with PM, respectively.
Korean J Radiol 2009;10:121-128 Conclusion: MR imaging is helpful for differentiating between NF and PM.
Received August 18, 2008; accepted
after revision September 30, 2008.
Departments of 1Radiology, 2Pathology,
N
3
Internal Medicine and 4Orthopedic ecrotizing fasciitis (NF) is a rapidly progressive, life-threatening illness
Surgery, The Catholic University of Korea;
5
Department of Internal Medicine, Kyung that’s characterized by necrosis and suppuration (1-4). It is often difficult
Hee University, Korea to differentiate NF from cellulitis or pyomyositis (PM) according to the
Address reprint requests to:
initial clinical presentation (1, 5). However, prompt and aggressive surgical treatment
Won-Hee Jee, MD, Department of is required to prevent a fatal outcome for patients with NF, whereas other soft tissue
Radiology, Kangnam St. Mary’s Hospital,
The Catholic University of Korea, 505
infections such as PM or cellulitis do not require emergency surgery (2-6). There have
Banpo-dong, Seocho-gu, Seoul 137-701, been some reports (2, 7, 8) that have tried to discriminate NF from cellulitis with using
Korea.
MR imaging. To the best of our knowledge, however, there have been only a few
Tel. (822) 590-2784
Fax. (822) 599-6771 reports (2, 9) regarding the differentiation between NF and PM with using MR
e-mail: whjee@catholic.ac.kr imaging.
The purpose of this study was to evaluate the MR findings for discriminating
between NF and PM.
Korean J Radiol 10(2), April 2009 121
Seok et al.
images (3,000-4,600/63-112 [repetition time msec/echo
time msec]) and the T1-weighted (450-800/10-21) images
MATERIALS AND METHODS
were obtained in the axial plane. The T2 weighted spectral
Patients fat saturation inversion recovery (SPIR) sequence (3,000-
The ethics committees at our institutions did not require 4,600/63-112 [repetition time msec/echo time msec]) was
informed patient consent for this retrospective study. MR obtained by the Philips scanner, and this was equivalent to
imaging was performed for 19 patients with clinically the FS FSE T2-weighted sequence obtained by the GE
suspected NF from July 2003 through June 2007, and the scanner. The FSE T2-weighted images (3,000-4,600/63-
findings were retrospectively reviewed. Eleven surgically 112) were obtained for at least one orthogonal plane. For
proven patients were included in this study. We had 28 18 patients, the axial and longitudinal FS T1-weighted spin
patients with clinically suspected PM, although 20 patients echo images (450-800/10-21) were obtained after
among them were excluded due to the absence of cultured administration of 0.1 mmol per kilogram of body weight of
organisms. The MR images from the 11 patients with gadopentetate dimeglumine (Magnevist; Bayer Schering,
surgically confirmed NF and the eight patients with Berlin, Germany). The matrix size was 192-256 × 256
pathologically confirmed PM from July 2003 through June and the number of averaging was one or two. The section
2007 were included in this study. All the cases were identi- thickness and intersection gap were variable for different
fied by reviewing the pathologic databases and the sites of involvement. The echo train length was 8-16.
operative records. Microorganisms were cultured in seven
patients with NF. There were 14 men and 5 women with Evaluation of the MR Images
an age range of 14 to 87 years (mean age: 49 years). The The MR images were analyzed on the high-resolution
11 patients with NF were eight men and three women with monitors (2,048 × 2,560 matrix, 10-bit viewable gray
an age range from 14 to 73 years (mean age: 43 years). scale) of a picture archiving and communication system.
The eight patients with PM were six men and two women The MR images were retrospectively reviewed by the
with an age range from 26 to 87 years (mean age: 58 consensus of two reviewers who were blinded to the
years). clinical data. Involvement of the superficial and deep
We also reviewed the clinical manifestations of NF and fasciae, muscles and subcutaneous tissue, the pattern of
PM. Nine patients (82%) with NF and five patients (63%) muscle involvement and the presence of intramuscular
with PM had the following underlying conditions: diabetes abscess was assessed, as well as the CE pattern of the fascia
mellitus, systemic lupus erythematosus, a history of and muscle.
malignancy or a renal transplantation state. Two patients The pattern of an abnormal signal or the CE of muscle
(18%) with NF were over 60 years old, whereas five was classified as peripheral band-like or diffuse. An
patients (63%) with PM were over 60 years old. A history abnormal muscle signal or CE was classified as peripheral
of local trauma was present for three patients (27%) with band-like if it was particularly prominent along the fascia,
NF and there was no history of local trauma for the despite being accompanied with some diffuse abnormal
patients with PM. signal within the muscle. We classified an abnormal signal
or the CE of muscle as diffuse if it was diffusely observed
MR Imaging within the muscle without a prominent abnormal signal
The MR examinations were performed within 1 to 10 along the fascia. On the FS CE T1-weighted images, the CE
days (median: 5 days, mean: 5.8 days) for the cases of NF, pattern of fascia was assessed as follows: thin smooth or
and within 6 to 90 days (median: 14 days, mean: 32.2 thick irregular. Muscle involvement was assessed in terms
days) for the cases of PM after the onset of symptoms, of the anatomical compartments. If an abnormal muscle
respectively. MR imaging was performed with one of the signal was observed in three or more anatomical compart-
two 1.5-T MR units (Achieva, Philips Medical Systems, ments on the axial FS T2-weighted images and the FS CE
Best, The Netherlands; Twin Speed, GE Medical Systems, T1-weighted images, then it was regarded as multicompart-
Milwaukee, WI). The best fitting coil (body array coil or a ment involvement.
shoulder coil) was used for the suspected area of involve-
ment. The variations in the field of view for different sites Statistical Analysis
of involvement ranged from 15 cm to 40 cm for the axial Statistical analysis was performed using Fisher’s exact
plane, and from 20 cm to 35 cm for the sagittal or coronal test. For all the statistical comparisons, significance was
plane. defined as p values < 0.05.
The fat-suppressed (FS) fast spin-echo (FSE) T2-weighted
122 Korean J Radiol 10(2), April 2009
MRI Discrimination between Necrotizing Fasciitis and Pyomyositis
mental involvement. Unilateral involvement was observed
in all the patients with either NF or PM.
RESULTS
The causative organisms in the patients with NF were as
Clinical Data follows: streptococcus pyogenes (n = 2), polymicrobial
The patients with either NF or PM complained of non- organisms (n = 2), staphylococcus aureus (n = 1), strepto-
specific symptoms that included painful swelling, tender- coccus group F (n = 1), mycobacterium species (n = 1) or
ness or a local heat sensation. Three patients (27%) with no growth (n = 2). On the other hand, staphylococcus
NF presented with bullae formation on their skin. NF and aureus (n = 6) was the most common causative organism in
PM both affected the lower extremities more frequently the eight patients with PM (Table 1).
than upper extremities: lower leg (n = 5), buttocks through
thigh (n = 3), arm (n = 2) and thigh (n = 1) for the NF MR Imaging
patients; buttocks (n = 2), buttocks through thigh (n = 2), Patients with NF had a significantly greater prevalence of
lower leg (n = 2), thigh (n = 1) and upper arm (n = 1) for the following MR findings (p < 0.05): peripheral band-like
the PM patients. Ten patients (91%) with NF showed hyperintense signals in muscles on the FS T2-weighted
multi-compartmental involvement except for one patient images (73% for the NF patients vs. 0% for the PM
with single-compartmental involvement. Five patients patients), peripheral band-like CE of muscles (82% vs. 0%,
(63%) with PM showed single-compartmental involve- respectively), thin smooth enhancement of deep fascia
ment, and three other PM patients showed multi-compart- (82% vs. 13%, respectively) and multicompartment
A B
Fig. 1. 51-year-old man with surgically confirmed necrotizing
fasciitis.
A. Axial fat-suppressed T2-weighted image (TR/TE, 4,000/87)
shows peripheral band-like high signal intensity (arrows) in
involved muscles of anterior, lateral and posterior compartments of
left lower leg. Hyperintense signal is seen along deep fascia
(arrowheads) as well as along superficial fascia.
B, C. Axial T1-weighted image (TR/TE, 450/12) (B) and fat-
suppressed contrast-enhanced T1-weighted image (550/12) (C)
show peripheral band-like enhancement (arrows) of involved
muscles. Thin smooth enhancement is seen along deep fascia
(arrowheads) as well as along superficial fascia. Patient underwent
emergency fasciectomy. Streptococcus pyogenes was cultured.
Korean J Radiol 10(2), April 2009 123
Seok et al.
Table 1. Summary of Treatment, Outcome and Prognosis for 19 Patients with Necrotizing Fasciitis and Pyomyositis
Patient No./Age(y)/Gender Treatment Organism Cultured Outcome
1/73/M Debridement Streptococcus group F Cure
2/51/M Fasciotomy No growth Cure
3/39/M Fasciotomy Streptococcus pyogenes Cure
4/37/M Debridement No growth Cure
5/66/F Debridement Streptococcus pyogenes Cure
6/33/M Debridement N/A Cure
7/40/F Fasciotomy N/A Cure
8/26/F Fasciotomy Mycobacterium species Death
9/46/M Amputation Streptococcus group D, enterobacter, Amputation
pseudomonas aureginosa, enterococcus
10/48/M ID, debridement Streptococcus group F, coagulase negative staphylococcus Cure
11/14/M Fasciectomy, ID Staphylococcus aureus Cure
12/63/M ID Staphylococcus aureus Cure
13/26/M Antibiotics Staphylococcus aureus Cure
14/73/F Antibiotics Streptococcus pyogenes Cure
15/63/M Antibiotics Staphylococcus aureus Cure
16/87/M ID Staphylococcus aureus Cure
17/29/F Antibiotics Staphylococcus aureus Cure
18/41/M ID Staphylococcus aureus Cure
19/79/M Antibiotics Hemophilus influenzae Cure
Note.─ No. 1-11 are patients with necrotizing fasciitis and No. 12-19 are patients with pyomyositis.
ID = incision and drainage, N/A = not available
Table 2. MR Findings of Necrotizing Fasciitis and Pyomyositis
MR Findings Necrotizing Fasciitis Pyomyositis P
Deep fascia
Hyperintense signal on T2WI 100 (11/11) 088 (7/8) 0.228 a
Presence of contrast enhancement 082 (9/11) 088 (7/8) 0.737 a
Thin smooth enhancement 082 (9/11) 013 (1/8) 0.002 a
Thick irregular enhancement 000 (0/11) 075 (6/8) 0.002 a
Superficial fascia
Hyperintense signal on T2WI 100 (11/11) 100 (8/8) -
Presence of contrast enhancement 100 (11/11) 100 (8/8) -
Thin smooth enhancement 091 (10/11) 050 (4/8) 0.046 a
Thick irregular enhancement 009 (1/11) 050 (4/8) 0.046 a
Muscle
Presence of muscle involvement 100 (11/11) 100 (8/8) -
Peripheral band-like involvement on FS T2WI 073 (8/11) 000 (0/8) 0.002 a
Diffuse involvement on FS T2WI 027 (3/11) 100 (8/8) 0.002 a
Presence of contrast enhancement 100 (11/11) 100 (8/8) -
Peripheral band-like enhancement 082 (9/11) 000 (0/8) 0.000 a
Diffuse enhancement 018 (2/11) 100 (8/8) 0.000 a
Presence of intramuscular abscess 000 (0/11) 088 (7/8) 0.000 a
Thick irregular wall of abscess - 100 (7/7) -
Subcutaneous involvement 100 (11/11) 088 (7/8) 0.228 a
Multicompartmental involvement 091 (10/11) 038 (3/8) 0.013 a
Note.─ Numbers indicate percent followed by fraction in parentheses.
a = Significance for Fisher’s exact test, FS T2WI = fat-suppressed T2-weighted images
124 Korean J Radiol 10(2), April 2009
MRI Discrimination between Necrotizing Fasciitis and Pyomyositis
A B
C D
Fig. 2. 37-year-old man with surgically confirmed necrotizing
fasciitis.
A. Axial fat-suppressed T2-weighted image (TR/TE, 4,400/81)
shows peripheral band-like high signal intensity (arrows) in
involved muscles of anterior, medial and posterior compartments of
left thigh. Hyperintense signal is seen along deep fascia
(arrowheads) as well as along superficial fascia.
B, C. Axial T1-weighted image (TR/TE, 450/15) (B) and fat-
suppressed contrast-enhanced T1-weighted image (600/15) (C)
show peripheral band-like enhancement (arrows) of involved
muscle and thin smooth enhancement of deep fascia
(arrowheads). Patient underwent emergency fasciectomy.
Streptococcus pyogenes was cultured.
D. Histopathologic specimen reveals marked neutrophilic and
histiocytic infiltrates and necrosis of fascia (Hematoxylin & Eosin
staining; original magnification, ×200).
E. Photomicrograph of histologic specimen shows severe inflam-
matory changes and necrosis in muscle (Hematoxylin & Eosin
staining; original magnification, ×100). Patient underwent
emergency fasciectomy. Streptococcus pyogenes was cultured.
E
Korean J Radiol 10(2), April 2009 125
Seok et al.
involvement (91% vs. 38%, respectively) (Table 2) (Figs. showed hyperintense signals on the T2-weighted images,
1, 2). and CE was seen on the FS CE T1-weighted images in all
Patients with PM had a significantly greater prevalence the patients with NF and in seven (88%) of the eight
of the following MR findings (p < 0.05): diffuse hyperin- patients with PM.
tense signals in the involved muscles on the FS T2-
weighted images (27% in the NF patients vs. 100% in the DISCUSSION
PM patients), diffuse CE of the involved muscles (18% vs.
100%, respectively), thick and irregular enhancement of The number of patients with NF has increased during the
deep fascia (0% vs. 75%, respectively) and intramuscular recent decades, and this is possibly due to a recent
abscess formation (0% vs. 88%, respectively) (Table 2) mutation of a subtype of group A beta-hemolytic
(Fig. 3). Streptococci (10, 11). PM is a primary bacterial infection
In all the patients with NF and PM, the superficial fascia involving the skeletal muscles (4, 9, 12). Although NF can
and muscles showed hyperintense signals on the T2- expand rapidly through the facial planes and along the
weighted images and CE was seen on the FS CE T1- underlying muscles, the overlying skin often resembles that
weighted images. The subcutaneous tissue and deep fascia of patients afflicted with cellulitis or PM (2). NF can only
A B
Fig. 3. 29-year-old woman with pathologically confirmed pyomyosi-
tis.
A. Axial fat-suppressed T2-weighted image (TR/TE, 3,200/96)
shows diffuse hyperintense signal (arrows) in soleus and lateral
head of gastrocnemius muscles, and this is confined to posterior
compartment of lower leg. Streaky hyperintense signal is seen in
subcutaneous tissue. Hyperintense signal is seen along deep
fascia (arrowheads) as well as along superficial fascia.
B, C. Axial T1-weighted image (TR/TE, 480/17) (B) and axial fat-
suppressed contrast-enhanced T1-weighted image (784/17) (C)
shows diffuse enhancement (arrows) of involved muscles and
subcutaneous tissue. Thick irregular enhancement is seen along
deep fascia (arrowheads) as well as along superficial fascia.
Staphylococcus aureus was cultured. Patient recovered after
antibiotic therapy.
126 Korean J Radiol 10(2), April 2009
MRI Discrimination between Necrotizing Fasciitis and Pyomyositis
be confirmed during surgery: extensive undermining of the and deep fasciae showed a hyperintense signal on the T2-
surrounding tissue is typically observed and the facial weighted images and CE was seen, like that of a prior
plane lacks resistance to a blunt instrument (7, 13). report (7). However, such an abnormal signal and
Our prevalence (100%) of an abnormal signal in the enhancement of the deep fascia were not unique findings
muscle of NF patients was consistent with the previous for NF, which is consistent with other previous studies (3,
report by Schmid et al. (7) that an intramuscular increased 17). Instead, in this present study, the enhancement
signal was seen in 10 of 11 cases of NF and intramuscular pattern of the deep fascia was significantly different for the
CE was seen in seven of nine cases with NF, respectively. two patient groups. Most patients (82%) with NF showed
However, our prevalence was much higher than the thin smooth CE of the deep fascia, while most patients
prevalence reported in a study by Rahmouni et al. (14) (75%) with PM showed thick irregular enhancement of
that seven (54%) of 13 MR images of the patients with this area.
necrotizing soft-tissue infections showed poorly defined The major limitations of this study include that the MR
areas of hyperintensity within muscles on the T2-weighted reviewers knew that all the patients had confirmed NF or
images. This difference could be related to the fact that we PM. This may have increased the sensitivity of detecting
added the fat-suppression technique to the CE T1- each of the MR findings. Another limitation is the small
weighted imaging as well as to the FSE T2-weighted number of patients, and particularly the number of patients
imaging. On the other hand, our prevalence (100%) of an with PM. This could be related to the fact that only
abnormal signal in muscle in PM patients was consistent pathologically confirmed patients with PM and who had
with the previous report by Gordon et al. (12) that an MR imaging were included in this study, although the
intramuscular increased signal was seen on the T2- prevalence of PM is much higher than the prevalence of
weighted images of all 11 patients with PM. NF. One other limitation of our study was that the study
In particular, we found that patients with NF showed a was confined to infectious conditions such as NF and PM,
peripheral band-like hyperintense signal in muscles on the because we excluded such noninfectious conditions as
FS T2-weighted images and peripheral band-like CE in idiopathic inflammatory myopathy, noninfectious inflam-
muscles on the FS CE T1-weighted images, and this was in matory eosinophilic fasciitis, rheumatic diseases, phlebe-
contrast to the PM patients who had a diffuse hyperintense dema, lymphedema, exertional muscle injury and other
signal on the FS T2-weighted images, and diffuse CE in tumorous conditions such as lymphoma. Thus, other
muscles. The difference between NF and PM may stem conditions except for PM might have MR findings that are
from the fact that the focus of NF disease is fascia, while similar to those of NF.
the focus of PM disease is muscle. NF patients often In conclusion, the muscle involvement pattern on the FS
present with multi-compartmental involvement, while T2-weighted images, as well as the enhancement pattern of
most cases of PM present with single-compartmental muscle and fascia on the FS CE T1-weighted images, can
involvement. help differentiate NF from PM.
A peripheral band-like abnormal signal in our patients
with NF is in contrast to the previous report (7) that the References
intramuscular signal was diffusely increased on the T2- 1. Wilson B. Necrotizing fasciitis. Am J Surg 1952;18:416-431
2. Brothers TE, Tagge DU, Stutley JE, Conway WF, Del Schutte H
weighted images and it showed diffuse CE. We assume
Jr, Byrne TK. Magnetic resonance imaging differentiates
that this discrepancy is related to the different criteria of between necrotizing and non-necrotizing fasciitis of the lower
analysis. In this present study, an abnormal signal or CE of extremity. J Am Coll Surg 1998;187:416-421
muscle was classified as peripheral band-like instead of 3. Arslan A, Pierre-Jerome C, Borthne A. Necrotizing fasciitis:
diffuse if it was particularly prominent along the fascia, and unreliable MRI findings in the preoperative diagnosis. Eur J
Radiol 2000;36:139-143
this was despite being accompanied by some diffuse
4. McAllister L. Masses that may mimic soft tissue tumors. In:
abnormal signal within the muscle. Intramuscular abscess Kransdorf MJ, Murphey MD, eds. Imaging of soft tissue tumors,
was not observed in our NF patients and this is in sharp 2nd ed. Philadelphia, Lippincott Williams & Wilkins, 2006:511-
contrast to the previous report (7) that abscesses were 572
identified in six among the nine cases of NF. Thus, a 5. Wall DB, de Virgilio C, Black S, Klein SR. Objective criteria
may assist in distinguishing necrotizing fasciitis from nonnecro-
further study with a larger study population may be
tizing soft tissue infection. Am J Surg 2000;179:17-21
needed. 6. Beauchamp NJ Jr, Scott WW Jr, Gottlieb LM, Fishman EK. CT
Liquefaction tissue necrosis and inflammatory edema evaluation of soft tissue and muscle infection and inflammation:
both contribute to the accumulation of fluid in the fascia a systematic compartmental approach. Skeletal Radiol
(15, 16). Indeed, in each of our NF subjects, the superficial 1995;24:317-324
Korean J Radiol 10(2), April 2009 127
Seok et al.
7. Schmid MR, Kossmann T, Duewell S. Differentiation of 12. Gordon BA, Martinez S, Collins AJ. Pyomyositis: characteristics
necrotizing fasciitis and cellulitis using MR imaging. AJR Am J at CT and MR imaging. Radiology 1995;197:279-286
Roentgenol 1998;170:615-620 13. Stamenkovic I, Lew PD. Early recognition of potentially fatal
8. Duewell S, Hagspiel KD, Zuber J, von Schulthess GK, Bollinger necrotizing fasciitis. The use of frozen-section biopsy. N Engl J
A, Fuchs WA. Swollen lower extremity: role of MR imaging. Med 1984;310:1689-1693
Radiology 1992;184:227-231 14. Rahmouni A, Chosidow O, Marthieu D, Gueorguieva E, Jazaerli
9. Revelon G, Rahmouni A, Jazaerli N, Godeau B, Chosidow O, N, Radier C, et al. MR imaging in acute infectious cellulitis.
Authier J, et al. Acute swelling of the limbs: magnetic resonance Radiology 1994;192:493-496
pictorial review of fascial and muscle signal changes. Eur J 15. Struk DW, Munk PL, Lee MJ, Ho SG, Worsley DF. Imaging of
Radiol 1999;30:11-21 soft tissue infections. Radiol Clin North Am 2001;39:277-303
10. Martin DR, Single LA. Molecular epidemiology of group A 16. Fugitt JB, Puckett ML, Quigley MM, Kerr SM. Necrotizing
streptococcus M type 1 infections. J Infect Dis 1993;167:1112- fasciitis. Radiographics 2004;24:1472-1476
1117 17. Loh NN, Ch’en IY, Cheung LP, Li KC. Deep fascial hyperinten-
11. Bisno AL, Stevens DL. Streptococcal infections of skin and soft sity in soft-tissue abnormalities as revealed by T2-weighted MR
tissues. N Engl J Med 1996;334:240-245 imaging. AJR Am J Roentgenol 1997;168:1301-1304
128 Korean J Radiol 10(2), April 2009
You might also like
- Physicians 10-2023Document27 pagesPhysicians 10-2023PRC Baguio100% (1)
- Cranial Nerves AssessmentDocument3 pagesCranial Nerves AssessmentNursesLabs.comNo ratings yet
- List of Nursing OrganizationsDocument3 pagesList of Nursing OrganizationsShehada Marcos BondadNo ratings yet
- Sasaran & Program Kerja K3L 2018 PT. HOCO (Rev.1)Document1 pageSasaran & Program Kerja K3L 2018 PT. HOCO (Rev.1)dennisjuntakNo ratings yet
- Sleep Deprivation and School QuestionnaireDocument2 pagesSleep Deprivation and School Questionnairethe-big-g92% (25)
- Diagnostic Accuracy of Zero-Echo Time MRI For The Evaluation of Cervical Neural Foraminal StenosisDocument20 pagesDiagnostic Accuracy of Zero-Echo Time MRI For The Evaluation of Cervical Neural Foraminal StenosisThiago Astil RizzettoNo ratings yet
- CT MRI TBsadadDocument5 pagesCT MRI TBsadadArief RachmanNo ratings yet
- Angioleiomyoma in Soft Tissue of Extremities: MRI FindingsDocument4 pagesAngioleiomyoma in Soft Tissue of Extremities: MRI FindingsLuis Javier del PozoNo ratings yet
- 1369 Full PDFDocument9 pages1369 Full PDFIqbal AbdillahNo ratings yet
- Spec MRI Distinguish Acue TM of NMOSD N Infarction. Kister Et Al 2015Document21 pagesSpec MRI Distinguish Acue TM of NMOSD N Infarction. Kister Et Al 2015Ido BramantyaNo ratings yet
- Displasia Cortical de TaylorDocument11 pagesDisplasia Cortical de TaylorOscar F. Ochoa RuizNo ratings yet
- Incidental Findings of The Lumbar Spine at MRI During Herniated Intervertebral Disk Disease EvaluationDocument5 pagesIncidental Findings of The Lumbar Spine at MRI During Herniated Intervertebral Disk Disease EvaluationDyah Gaby KesumaNo ratings yet
- Seguridad Social en AlemaniaDocument8 pagesSeguridad Social en AlemaniaMichael RojasNo ratings yet
- Jms 21041483Document28 pagesJms 21041483Afra Eslis NoatoNo ratings yet
- Magnetic Resonance Imaging For The Detection of Nasopharyngeal CarcinomaDocument4 pagesMagnetic Resonance Imaging For The Detection of Nasopharyngeal CarcinomaFebri W FinisiaNo ratings yet
- Tumores en CuelloDocument6 pagesTumores en CuellokalixinNo ratings yet
- Primitive Neuroectodermal Tumors: A Clinical and Radiological Analysis of Six CasesDocument8 pagesPrimitive Neuroectodermal Tumors: A Clinical and Radiological Analysis of Six CasestaufikolingNo ratings yet
- Fibrosing Inflammatory Pseudotumors Involving The Skull Base: MR and CT Manifestations With Histopathologic ComparisonDocument7 pagesFibrosing Inflammatory Pseudotumors Involving The Skull Base: MR and CT Manifestations With Histopathologic ComparisonNicolas SaputraNo ratings yet
- CT and MR Imaging Features of Primary Central Nervous System Lymphoma in Norway, 1989-2003Document8 pagesCT and MR Imaging Features of Primary Central Nervous System Lymphoma in Norway, 1989-2003Alfina RahmiNo ratings yet
- Neurol J Southeast Asia 1999 4: 83 - 88: LCS Tan, YY Sitoh, HTL TjiaDocument6 pagesNeurol J Southeast Asia 1999 4: 83 - 88: LCS Tan, YY Sitoh, HTL Tjiarani suwadjiNo ratings yet
- Bone Marrow Edema Syndrome 1Document8 pagesBone Marrow Edema Syndrome 1drbane123No ratings yet
- Diagnosis and Classification in MRI of Brucellar SpondylitisDocument6 pagesDiagnosis and Classification in MRI of Brucellar SpondylitisMANGNo ratings yet
- Distinguishing Benign Notochordal Cell Tumors From Vertebral ChordomaDocument9 pagesDistinguishing Benign Notochordal Cell Tumors From Vertebral ChordomaOM JHANo ratings yet
- MR IntracranIal menIngIomas!!! Vazno!!!Document5 pagesMR IntracranIal menIngIomas!!! Vazno!!!StefanNo ratings yet
- Imaging of The Scrotum: Beyond SonographyDocument12 pagesImaging of The Scrotum: Beyond Sonographyasriani DewiNo ratings yet
- Primary Extraskeletal Ewing Sarcoma of The Sinonasal Tract - A Rare Case Report and Review of The LiteratureDocument7 pagesPrimary Extraskeletal Ewing Sarcoma of The Sinonasal Tract - A Rare Case Report and Review of The LiteraturemohammadsayfooNo ratings yet
- Pulsed Electromagnetic Field in Patients With Shoulder Impingement SyndromeDocument6 pagesPulsed Electromagnetic Field in Patients With Shoulder Impingement SyndromeHanna RikaswaniNo ratings yet
- The Diagnostic Relationship With Clinical and Neuroimaging Studies of Patients With Back PainDocument5 pagesThe Diagnostic Relationship With Clinical and Neuroimaging Studies of Patients With Back PainCentral Asian StudiesNo ratings yet
- Imaging in RadiculopathyDocument17 pagesImaging in RadiculopathyFerdy DamaraNo ratings yet
- Bone MarrowDocument5 pagesBone MarrowDanaAmaranducaiNo ratings yet
- Sipola. Detection and Quantification of Rotator Cuff Tears With Ultrasonography and Magnetic Resonance Imaging - A ProsDocument9 pagesSipola. Detection and Quantification of Rotator Cuff Tears With Ultrasonography and Magnetic Resonance Imaging - A Prossteven saputraNo ratings yet
- Spinal Tuberculosis: Imaging Features On MRIDocument6 pagesSpinal Tuberculosis: Imaging Features On MRIEster JuanitaNo ratings yet
- Scientific Abstracts Friday, 14 June 2019 1015Document1 pageScientific Abstracts Friday, 14 June 2019 1015حسام الدين إسماعيلNo ratings yet
- Proton Magnetic Resonance Spectroscopy MRS of Metastatic Brain TumorsDocument10 pagesProton Magnetic Resonance Spectroscopy MRS of Metastatic Brain TumorsolgaNo ratings yet
- Kiuru 2002Document6 pagesKiuru 2002Laraib KanwalNo ratings yet
- Space Occupying Lesions of Central Nervous System: A Radiological and Histopathological CorrelationDocument6 pagesSpace Occupying Lesions of Central Nervous System: A Radiological and Histopathological CorrelationRaja WartegNo ratings yet
- Payer 2015Document10 pagesPayer 2015esinsubozatliNo ratings yet
- Vertebral Endplate Change As A Feature of Intervertebral Disc Degeneration: A Heritability StudyDocument7 pagesVertebral Endplate Change As A Feature of Intervertebral Disc Degeneration: A Heritability StudySitti Hajar ArdasNo ratings yet
- SAVULESCU Et Al 2021 Rpms of Lumbar Area Effective On Radiculopathy PainDocument5 pagesSAVULESCU Et Al 2021 Rpms of Lumbar Area Effective On Radiculopathy PainperruchoudNo ratings yet
- Osteoradionecrosis of The Subaxial Cervical Spine Following Treatment For Head and Neck CarcinomasDocument8 pagesOsteoradionecrosis of The Subaxial Cervical Spine Following Treatment For Head and Neck CarcinomasakreditasiNo ratings yet
- Keller Et Al 2011 EpilepsiaDocument10 pagesKeller Et Al 2011 EpilepsiaLaura Gonzalez TamayoNo ratings yet
- Ewing'S Sarcoma: Imaging FeaturesDocument9 pagesEwing'S Sarcoma: Imaging FeaturesRachelMayaMalauNo ratings yet
- Intracranial Yolk Sac Tumor in An Adult Patient: MRI, Diffusion-Weighted Imaging and H MR Spectroscopy FeaturesDocument4 pagesIntracranial Yolk Sac Tumor in An Adult Patient: MRI, Diffusion-Weighted Imaging and H MR Spectroscopy FeaturestiaraNo ratings yet
- 2018 Ultrasonido Terapéutico Con Medición en Pacientes Con RadiculopatíaDocument8 pages2018 Ultrasonido Terapéutico Con Medición en Pacientes Con RadiculopatíaCarlos JaimeNo ratings yet
- Two Decades of Advances in Muscle Imaging in Children From P - 2021 - NeuromuscDocument13 pagesTwo Decades of Advances in Muscle Imaging in Children From P - 2021 - NeuromuscSuzie Simone Mardones SilvaNo ratings yet
- Primary Leiomyosarcoma of The Spine: An Analysis of Imaging Manifestations and Clinicopathological FindingsDocument9 pagesPrimary Leiomyosarcoma of The Spine: An Analysis of Imaging Manifestations and Clinicopathological Findingst7xs5mchfzNo ratings yet
- MRI Findings of 26 Patients With Parsonage-Turner SyndromeDocument6 pagesMRI Findings of 26 Patients With Parsonage-Turner SyndromeTopciu Mihaela FeliciaNo ratings yet
- MRI SeizuresDocument7 pagesMRI SeizuresMarco MalagaNo ratings yet
- Diagnosis of Carpal Tunnel SyndromeDocument11 pagesDiagnosis of Carpal Tunnel SyndromeMrAppleNo ratings yet
- Diagnostic Utility of Ultrasonography Versus Nerve Conduction Studies in Mild Carpal Tunnel SyndromeDocument10 pagesDiagnostic Utility of Ultrasonography Versus Nerve Conduction Studies in Mild Carpal Tunnel SyndromeJP ChenNo ratings yet
- Z Score SISCOMDocument9 pagesZ Score SISCOMAiswarya HariNo ratings yet
- Reliability of Diagnosis of Soft Cervical Disc Prolapse Using Spurling's TestDocument5 pagesReliability of Diagnosis of Soft Cervical Disc Prolapse Using Spurling's Testapi-479716004No ratings yet
- JournalDocument6 pagesJournalmandipNo ratings yet
- Kerasnoudis 2014Document10 pagesKerasnoudis 2014Laura A M MNo ratings yet
- 0040JKSMRM JKSMRM 17 8Document11 pages0040JKSMRM JKSMRM 17 8M P ChakravortyNo ratings yet
- Clavicle Fracture Following Neck Dissection: Imaging Features and Natural CourseDocument6 pagesClavicle Fracture Following Neck Dissection: Imaging Features and Natural CourseAngel IschiaNo ratings yet
- RNM Dinamica 2Document6 pagesRNM Dinamica 2Alfredo GuiroyNo ratings yet
- Radiol 2332031111Document8 pagesRadiol 2332031111nimaelhajjiNo ratings yet
- Clinical Neurophysiology: Yukiko Tsuji, Yu-Ichi Noto, Takamasa Kitaoji, Yuta Kojima, Toshiki MizunoDocument5 pagesClinical Neurophysiology: Yukiko Tsuji, Yu-Ichi Noto, Takamasa Kitaoji, Yuta Kojima, Toshiki MizunoSerque777No ratings yet
- Clinical Neurophysiology: Yukiko Tsuji, Yu-Ichi Noto, Takamasa Kitaoji, Yuta Kojima, Toshiki MizunoDocument5 pagesClinical Neurophysiology: Yukiko Tsuji, Yu-Ichi Noto, Takamasa Kitaoji, Yuta Kojima, Toshiki MizunoSerque777No ratings yet
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 2000)Document9 pagesP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 2000)zano_adamNo ratings yet
- SDRCIDocument7 pagesSDRCIRensoBerlangaNo ratings yet
- Abnormal Cerebral Structure in Juvenile Myoclonic Epilepsy Demonstrated With Voxel-Based Analysis of MRIDocument7 pagesAbnormal Cerebral Structure in Juvenile Myoclonic Epilepsy Demonstrated With Voxel-Based Analysis of MRIVj McNo ratings yet
- 2016 5 Focus16163 PDFDocument10 pages2016 5 Focus16163 PDFLuwiNo ratings yet
- JBH5 HiccupsDocument5 pagesJBH5 HiccupsAstrid GayatriNo ratings yet
- Berlin QuestionnaireDocument1 pageBerlin QuestionnaireAstrid GayatriNo ratings yet
- Vitamin D and Living in Northern Latitudes An Endemic Risk Area For Vitamin D DeficiencyDocument16 pagesVitamin D and Living in Northern Latitudes An Endemic Risk Area For Vitamin D DeficiencyJu RiNo ratings yet
- 10 1111-cpr 12915figure129150001Document1 page10 1111-cpr 12915figure129150001Astrid GayatriNo ratings yet
- Contoh Pico Terbaru-Blok EndokrinDocument3 pagesContoh Pico Terbaru-Blok EndokrinIndra ArdiansyahNo ratings yet
- Learning Guide 03Document28 pagesLearning Guide 03Mulugeta GirmaNo ratings yet
- Daftar Obat IntersipDocument15 pagesDaftar Obat Intersipleno voNo ratings yet
- Clinic ListDocument34 pagesClinic Listrayd667No ratings yet
- Rekapan Diah Ayu-UHAMKA-DM Tipe 2Document185 pagesRekapan Diah Ayu-UHAMKA-DM Tipe 2DevinaNo ratings yet
- Dt. 02.04.2023 YMA TlangauDocument4 pagesDt. 02.04.2023 YMA TlangaupatsyNo ratings yet
- Npi-Family Case StudyDocument12 pagesNpi-Family Case StudyGayLah MomblancoNo ratings yet
- Daily Undulating Periodisation Plan TemplateDocument6 pagesDaily Undulating Periodisation Plan TemplateJaron KungNo ratings yet
- University of Makati: J.P. Rizal West Rembo Makati CityDocument3 pagesUniversity of Makati: J.P. Rizal West Rembo Makati Citywheng0814No ratings yet
- Peritonitis Et Causa Demam Typhoid: Kelompok D6Document21 pagesPeritonitis Et Causa Demam Typhoid: Kelompok D6Anjas PrabowoNo ratings yet
- TOPIC 10 - 1019031146 UbaidillahDocument8 pagesTOPIC 10 - 1019031146 UbaidillahUbay SegaNo ratings yet
- Assessment Sheet: Critical Care Patient (Icu / Ccu)Document5 pagesAssessment Sheet: Critical Care Patient (Icu / Ccu)Barrak AldosaryNo ratings yet
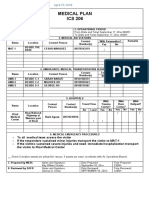
- Ics 206Document1 pageIcs 206Ldrrmo RamonNo ratings yet
- Nonextraction Treatment With Begg TechniqueDocument14 pagesNonextraction Treatment With Begg TechniqueSyed Mohammad Osama AhsanNo ratings yet
- PGM CET 2015 First Round Selection List Dated 30.03.2015Document34 pagesPGM CET 2015 First Round Selection List Dated 30.03.2015Shruthi ShenoyNo ratings yet
- Bowel Prep PresentationDocument14 pagesBowel Prep PresentationnadiarosmanNo ratings yet
- Billing Template and Opd Health PackageDocument8 pagesBilling Template and Opd Health Packagepranit.gumgaonkarNo ratings yet
- Quality Health Services: A Planning GuideDocument64 pagesQuality Health Services: A Planning GuideEdwar RusdiantoNo ratings yet
- Nausea and VomitingDocument3 pagesNausea and VomitingAlthea AlbaniaNo ratings yet
- Presentation IresDocument30 pagesPresentation IresPriyanka Sharma100% (1)
- Sistema ABO, Parte 2Document25 pagesSistema ABO, Parte 2juan pablo padgetNo ratings yet
- Merancang Klinik Kedokteran KeluargaDocument29 pagesMerancang Klinik Kedokteran KeluargaLuthfiyah SalsabillaNo ratings yet
- Annexure Panchkarma - 1st EditionDocument228 pagesAnnexure Panchkarma - 1st EditionSmita SaxenaNo ratings yet
- Dade InnovinDocument7 pagesDade InnovinchaiNo ratings yet
- Rubrics For Triangular Bandaging TechniqueDocument1 pageRubrics For Triangular Bandaging TechniqueBulan A'tin0% (2)