Professional Documents
Culture Documents
Hyperacute Liver Failure With Multi-Organ Dysfunction Syndrome (MODS) by Leptospirosis: A Case Report
Uploaded by
Minerva Medical Treatment Pvt LtdOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hyperacute Liver Failure With Multi-Organ Dysfunction Syndrome (MODS) by Leptospirosis: A Case Report
Uploaded by
Minerva Medical Treatment Pvt LtdCopyright:
Available Formats
Short Article
Hyperacute Liver Failure with Multi-organ Dysfunction Syndrome
(MODS) by Leptospirosis: A Case Report
Nilay Tripathi1*, Naresh Rajpal1, Gaurav Jain1, Prashant Katiyar2
Department of Internal Medicine, Vivekananda Polyclinic and Institute of Medical Sciences, Ramakrishna Mission Sevashrama, Lucknow, India
1
2
Department of Gastroenterology, Vivekananda Polyclinic and Institute of Medical Sciences, Ramakrishna Mission Sevashrama, Lucknow, India
Abstract
Introduction: Leptospirosis may have multi-organ involvement in its severe form with potentially life-threatening consequences.
However, acute fulminant hepatic failure is very uncommonly reported. A case study is presented here with fulminant hepatic
failure and a diagnostic dilemma for etiology.
Case history: A 40-year-old man with no significant medical history presented with fever, muscle pain, weakness, and pain
in the upper abdomen. On clinical work, he has developed multi-organ hepatic, respiratory, and renal failure. A timely workup
was done, but due to the rapid progression of the disease, the patient succumbed to the disease in the intensive care unit by the
time his report for positive leptospirosis test arrived.
Conclusion: Leptospirosis must be considered as an important differential diagnosis of acute liver failure patients. An early
suspicion for leptospirosis in patients with fulminant hepatic failure and multi-organ failure in India particularly in the rainy
season is warranted owing to its high mortality rate.
Keywords: leptospirosis, Acute fulminant hepatic failure, Multi organ dysfunction syndrome.
I ntroduction MODS in leptospirosis, this study aims to contribute to the
existing body of knowledge, guide clinical decision-making,
Leptospirosis is a priority zoonotic disease under one health
and ultimately improve the prognosis for patients affected
program with worldwide distribution.[1-3] Previously thought
by this critical condition, such diagnosis often gets missed
to be a disease of rural populations and sewage workers,
despite efforts by the one health program for prevention and
it is re-emerging as a potentially life-threatening disease
control of Zoonotic diseases through sentinel surveillance
in urban populations. Although it is endemic in southern
sites for capacity building of epidemiologists, clinicians, and
and western parts of India,[4-6] leptospirosis has also been
microbiological laboratories.
recently reported from eastern and northern India, where
it was earlier thought to be non-existent.[7-14] Despite being Case History
common, its diagnosis is often ignored or delayed because of This is a case history of a 40year old man who was admitted
a low index of suspicion and protean presentation. However, to our hospital with chief complaints of severe pain in the
detailed data on leptospirosis’s frequency, degree, and type of upper abdomen for 4 days, fever with chills for 3 days, severe
hepatic dysfunction are limited. The present study highlights
a patient who presented with clinical problems confusing
in the clinical setting and could be easily managed once Address for correspondence: Nilay Tripathi,
suspected and found positive on an investigation. By shedding Department of Internal Medicine, Vivekananda Polyclinic and Institute of Medical
light on the complexities of hyperacute liver failure with Sciences, Ramakrishna Mission Sevashrama, Lucknow, India
E‑mail: tripathinilay@yahoo.co.in
Access this article online
This is an open access journal, and articles are distributed under the terms of the Creative Commons
Quick Response Code Attribution‑NonCommercial‑ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work
Website: non‑commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
www.iapsmupuk.org
How to cite this article: Tripathi N, Rajpal N, Jain G, Katiyar P.
Hyperacute Liver Failure with Multi-organ Dysfunction Syndrome
DOI: (MODS) by Leptospirosis: A Case Report. Indian J. of Com. Health.
10.47203/IJCH.2023.v35i02.020 2023;35(2):243-245.
Received: 16-04-2023, Accepted: 06-05-2023, Published: 30-06-2023
Nilay Tripathi, et al.: Leptospirosis with multi-organ dysfunction syndrome
weakness for 3 days, and yellowish discoloration of urine for hematological investigations report showed the following
3 days. Apparently, a remarkably short history narrated by results: Table 1. It showed moderate anemia (Hb-8.2gm/dl),
the patient that he was asymptomatic 5 days back when the leucocytosis, prolonged prothrombin time more than twice
patient felt sudden onset sharp upper abdominal pain which of control, mild jaundice with significantly high SGOT (3290
was acute in onset, gradually progressive, dull aching, non- U/l), and SGPT (3450 U/l) levels suggesting acute hepatic
radiating with no aggravating factors but was relieved only failure. The patient had acute renal failure too with raised
on IV tramadol injection. He was admitted to a local hospital serum creatinine 4.19 mg/dl). Arterial blood gas analysis
as a case of acute abdomen. Urgent ultrasound was done, showed severe metabolic acidosis pH-7.01, PaCO2-30 mmHg,
which showed altered echotexture of bilateral kidneys with PaO2-156 at FiO2-0.4, and HCO3—18.6.
normal size suggesting medical renal disease and also showed We also found that the patient reported negative results for
heterogenous hepatic echotexture but the pancreas appeared malaria antigen, typhoid DOT, dengue, hepatitis B antigen,
to be normal. The patient was referred to us as he might need
HCV, and HIV antibody tests. Hepatitis A viral screening also
admission to the intensive care unit.
yielded negative results. We also sent a test for leptospirosis
The following day, the patient developed a high-grade
Ig M with Elisa, which was positive but sadly, the report was
fever that was acute in onset and was followed by yellowish
received post-death of the patient. His presumptive diagnosis
discoloration of urine and altered sensorium during the
is based on Faine’s criteria (Part A and B score- 28) (table
hospital stay. His Glasgow Coma Scale (GCS) rapidly
2). The diagnosis was further confirmed as leptospirosis by
deteriorated to 5. The patient developed respiratory failure
positive Elisa IgM by the next day.
with tachypnoea (respiratory rate 28 bpm and arterial blood
On the second day of the ICU stay, urine output started
saturation 80%. He was immediately intubated and put on
deteriorating and the nephrologist advised dialysis. Still, it
mechanical ventilation; subsequently, his biochemical and
could not be started as the patient developed hypotension and
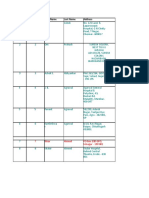
Table 1: Showing first-day blood reports with very high leucocyte gastric bleeding with petechial hemorrhagic spots all over the
count, creatinine and liver enzymes body. The patient’s condition deteriorated rapidly and they
Name of test Report Normal reference went into cardiac arrest probably because of severe metabolic
Haemoglobin 8.2 gm/dl 11-15 gm/dl acidosis. He was revived by cardiopulmonary resuscitation
Total Leucocyte count 13800 5000-10000 but with a second arrest on the subsequent day the patient
could not be revived again and died after 3 days of admission.
Platelet count 1.2 lac/ml 1.5-4.5 lac/ml
Prothrombin time ratio (INR) 4.6 0.8-1.1 D iscussion
S creatinine 4.19 mg/dl 0.6-1.2 mg/dl The present report describes a case of hyperacute liver
S Bilirubin 2.6 mg/dl 0.2-1.2 mg/dl failure due to leptospirosis infection, the less common cause
SGOT 3290 U/l 5-40 U/l of liver failure. The confirmative diagnosis of leptospirosis
SGPT 3450 U/l 7-56 U/l was made based on the criteria according to modified Faine’s
S Amylase 48 U/l 23-85 U.l criteria score of more than 26 from Part A, and Part C.
S Lipase 69 U/l 0-160 U/l
Unfortunately, the patient could not be saved due to rapidly
deteriorating condition of acute exacerbation of acute renal
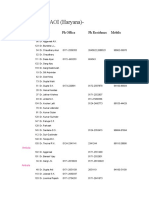
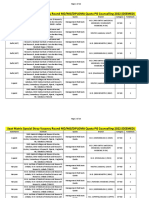
Table 2: Showing diagnostic criteria for leptospirosis. Presumptive diagnosis of leptospirosis is made if: Part A or Part A and Part B score: 26 or
more; Parts A, B, C (Total): 25 or more. A score between 20 and 25 suggests leptospirosis as a possible diagnosis
Clinical Data (Part A) Epidemiological factors (Part B) Bacteriological & Laboratory Findings (Part C)
Headache 2 Rainfall 5 Isolation of Leptospira in culture-Diagnosis Certain
PCR 25
Fever 2 Contract with contaminated 4 Positive Serology
environment
Conjunctival Suffusion 4 Animal Contact 1 Elisa IgM positive 15
Meningism 4 SAT Positive 15
Conjunctival Suffusion 10 Other Rapid Test 15
+Meningism
+Myalgia
Jaundice 1 MAT Single Positive High Titer 25
Albuminuria/Nitrogen 2 MAT-Rising Titer/Seroconversion (Paired sera) 25
retention
Hemoptysis/Dyspnea 2 Any one of test only should be scored latex agglutination test/
Lepto Dipstick/ Lepto Tek Lateral flow/Lepto Tek DriDot test
© 2023 Indian Journal of Community Health 244
Nilay Tripathi, et al.: Leptospirosis with multi-organ dysfunction syndrome
failure with respiratory failure but amply emphasized to 3. Sambasiva RR, Naveen G, P B, Agarwal SK. Leptospirosis
consider leptospirosis too. in India and the rest of the world. Braz J Infect Dis. 2003
According to the above-mentioned criteria, the total score Jun;7(3):178-93. doi: 10.1590/s1413-86702003000300003.
of our patient according to Part A and Part B was 28 which PMID: 14499041.
means the presumptive diagnosis was made. The patient was 4. Izurieta R, Galwankar S, Clem A. Leptospirosis: The
“mysterious” mimic. J Emerg Trauma Shock. 2008 Jan;1(1):21-
having jaundice along with frank liver failure and showed
33. doi: 10.4103/0974-2700.40573. PMID: 19561939; PMCID:
typical renal involvement, headache, and myalgia.
PMC2700559.
The patient coagulopathy was taken care of but the course 5. Vijayachari P, Sugunan AP, Shriram AN. Leptospirosis:
of the disease was so fulminant that even prompt treatment an emerging global public health problem. J Biosci. 2008
and intravenous doxycycline could not save the patient. As Nov;33(4):557-69. doi: 10.1007/s12038-008-0074-z. PMID:
the center was not having any liver transplantation facilities 19208981.
and the aggressive nature of the disease patient could not 6. Sehgal SC. Leptospirosis on the horizon. Natl Med J India. 2000
be shifted to the higher center and ultimately succumbed to Sep-Oct;13(5):228-30. PMID: 11190049.
severe metabolic acidosis and renal failure. 7. Sethi S, Sharma N, Kakkar N, Taneja J, Chatterjee SS, Banga
We required a liver biopsy for the definitive diagnosis, SS, Sharma M. Increasing trends of leptospirosis in northern
but it could not be performed because of severe derangement India: a clinico-epidemiological study. PLoS Negl Trop Dis.
2010 Jan 12;4(1):e579. doi: 10.1371/journal.pntd.0000579.
of the coagulation profile. He developed disseminated
PMID: 20084097; PMCID: PMC2797087.
intravascular coagulopathy too.
8. Manocha H, Ghoshal U, Singh SK, Kishore J, Ayyagari A.
Leptospira infection often has minimal clinical Frequency of leptospirosis in patients of acute febrile illness
manifestations, with about 40% of the infected patients in Uttar Pradesh. J Assoc Physicians India. 2004 Aug;52:623-
seroconverting asymptomatically. Of the remaining 60%, 5. PMID: 15847355.
approximately 90% suffer the milder anicteric form and 10% 9. Gupta N, Rao RS, Bhalla P, Agarwal SK. Seroprevalence of
the more severe icteric form.[2-4] The severe form is associated leptospirosis in Delhi using indirect haemagglutination assay.
with multi-organ involvement, especially hepato-renal, Indian J Med Microbiol. 2004 Apr-Jun;22(2):134-5. PMID:
and a fatality rate of up to 40%.[5] Hepatic involvement in 17642716.
Leptospira infection is not uncommon and can vary from an 10. Sethi S, Sood A, Pooja, Sharma S, Sengupta C, Sharma M.
asymptomatic rise in transaminases to severe icteric hepatitis. Leptospirosis in northern India: a clinical and serological
study. Southeast Asian J Trop Med Public Health. 2003
C onclusion Dec;34(4):822-5. PMID: 15115094.
11. Chaudhry R, Premlatha MM, Mohanty S, Dhawan B, Singh KK,
Leptospirosis must be considered an important differential
Dey AB. Emerging leptospirosis, North India. Emerg Infect
diagnosis of acute liver failure patients owing to its Dis. 2002 Dec;8(12):1526-7. doi: 10.3201/eid0812.020052.
high mortality rate and growing incidence in India, PMID: 12498680; PMCID: PMC2738520.
particularly in rainy seasons and when the risk factors are 12. Kaur IR, Sachdeva R, Arora V, Talwar V. Preliminary survey
present. Sensitization of epidemiologists, clinicians, and of leptospirosis amongst febrile patients from urban slums of
microbiological laboratories is required for the identification East Delhi. J Assoc Physicians India. 2003 Mar;51:249-51.
of such cases under one health program for the prevention PMID: 12839344.
and control of Zoonotic diseases through the strengthening 13. Chauhan V, Mahesh DM, Panda P, Mokta J, Thakur S. Profile
of sentinel surveillance sites. of patients of leptospirosis in sub-Himalayan region of North
India. J Assoc Physicians India. 2010 Jun;58:354-6. PMID:
R eferences 21125775.
1. Levet t PN. Leptospirosis. Clin Microbiol Rev. 2001 14. Goswami RP, Goswami RP, Basu A, Tripathi SK, Chakrabarti
Apr;14(2):296-326. doi: 10.1128/CMR.14.2.296-326.2001. S, Chattopadhyay I. Predictors of mortality in leptospirosis:
PMID: 11292640; PMCID: PMC88975. an observational study from two hospitals in Kolkata, eastern
2. Dutta TK, Christopher M. Leptospirosis--an overview. J Assoc India. Trans R Soc Trop Med Hyg. 2014 Dec;108(12):791-6.
Physicians India. 2005 Jun;53:545-51. PMID: 16121811. doi: 10.1093/trstmh/tru144. Epub 2014 Oct 30. PMID: 25359
245 Indian Journal of Community Health ¦ Volume 35 ¦ Issue 2 ¦ April - June 2023
You might also like
- JCIMCR v3 1706Document2 pagesJCIMCR v3 1706Mohan ChikkalaNo ratings yet
- Acute Fulminent Leptospirosis With Multi-Organ Failure: Weil's DiseaseDocument4 pagesAcute Fulminent Leptospirosis With Multi-Organ Failure: Weil's DiseaseMuhFarizaAudiNo ratings yet
- It Is Time To Review Concepts On Renal Involvement in Leprosy Pre and Post Treatment Evaluation of 189 PatientsDocument5 pagesIt Is Time To Review Concepts On Renal Involvement in Leprosy Pre and Post Treatment Evaluation of 189 PatientsAdhyt PratamaNo ratings yet
- 2 +Severe+LeptospirosisDocument6 pages2 +Severe+LeptospirosisYhuzz Toma5No ratings yet
- 51 Sumantro EtalDocument3 pages51 Sumantro EtaleditorijmrhsNo ratings yet
- BJSTR MS Id 001072Document4 pagesBJSTR MS Id 001072Jatin SinghNo ratings yet
- Medicine: Systemic Lupus Erythematosus With Guillian - Barre SyndromeDocument5 pagesMedicine: Systemic Lupus Erythematosus With Guillian - Barre SyndromeShri RamNo ratings yet
- 2018 JSM Volume15 Supplement 3 JulyDocument2 pages2018 JSM Volume15 Supplement 3 JulyAmr Amin RagabNo ratings yet
- Salmonella Hepatitis: An Uncommon Complication of A Common DiseaseDocument3 pagesSalmonella Hepatitis: An Uncommon Complication of A Common DiseaseMudassar SattarNo ratings yet
- Article Koskina ArchDocument8 pagesArticle Koskina ArchElli SymeonidouNo ratings yet
- Case ReflectionDocument7 pagesCase ReflectionAmanat KangNo ratings yet
- Pediatric Systemic Lupus Erythematosus Associated With AutoimmuneDocument9 pagesPediatric Systemic Lupus Erythematosus Associated With AutoimmunegistaluvikaNo ratings yet
- MedicineDocument5 pagesMedicineRoyd Jesse Kwibisa JrNo ratings yet
- COVID-19 Related Acute Necrotizing Encephalopathy Presenting in The Early Postoperative PeriodDocument8 pagesCOVID-19 Related Acute Necrotizing Encephalopathy Presenting in The Early Postoperative PeriodElli SymeonidouNo ratings yet
- Endo 2012Document7 pagesEndo 2012Muhammad Anshory AkNo ratings yet
- Kasus 2Document3 pagesKasus 2AndiandiNo ratings yet
- 12b Clinical Update Example 2018Document9 pages12b Clinical Update Example 2018Ana BienneNo ratings yet
- Case Report: Severe Hyperbilirubinemia: A Rare Complication of Lyme DiseaseDocument4 pagesCase Report: Severe Hyperbilirubinemia: A Rare Complication of Lyme DiseaseDhruva PatelNo ratings yet
- Sas S9Document9 pagesSas S9Ralph Louie ManagoNo ratings yet
- Medical Mycology Case ReportsDocument3 pagesMedical Mycology Case ReportsReza FaisalNo ratings yet
- COVID19 Carvalho Et Al AJG PreproofDocument10 pagesCOVID19 Carvalho Et Al AJG PreproofRhara MillatinaNo ratings yet
- Ebsco ContentServerDocument7 pagesEbsco ContentServerHailey LapineNo ratings yet
- HES 032 Case Analysis Week 3Document4 pagesHES 032 Case Analysis Week 3Arsie CalvoNo ratings yet
- Kawasaki DiseaseDocument22 pagesKawasaki DiseaseMax LocoNo ratings yet
- A Case of Typhoid Fever Presenting With Multiple ComplicationsDocument4 pagesA Case of Typhoid Fever Presenting With Multiple ComplicationsCleo CaminadeNo ratings yet
- 68 JMSCRDocument3 pages68 JMSCRVani Junior LoverzNo ratings yet
- Banerji Chron HepatitisDocument4 pagesBanerji Chron HepatitisdaspranabNo ratings yet
- Revision de LesDocument12 pagesRevision de Lesroberto mendezNo ratings yet
- Title Retrospective Review of Typhoid and Paratyphoid Fever in A Regional HospitalDocument32 pagesTitle Retrospective Review of Typhoid and Paratyphoid Fever in A Regional HospitalHam FGNo ratings yet
- An Open-Label Pilot Study of Adrenocorticotrophic Hormone in The Treatment of IgA Nephropathy at High Risk of Progression Zand2019Document8 pagesAn Open-Label Pilot Study of Adrenocorticotrophic Hormone in The Treatment of IgA Nephropathy at High Risk of Progression Zand2019Calvin Tanuwijaya Stick BolaNo ratings yet
- LepsDocument4 pagesLepslynharee100% (1)
- Mesenteric Adenitis As A Differential Appendicitis PDFDocument5 pagesMesenteric Adenitis As A Differential Appendicitis PDFJasmine EffendiNo ratings yet
- Mesenteric Adenitis As A Differential Appendicitis PDFDocument5 pagesMesenteric Adenitis As A Differential Appendicitis PDFJasmine EffendiNo ratings yet
- 1476 1645 Article p479Document6 pages1476 1645 Article p479Yuyun RasulongNo ratings yet
- Research Article: Neutropenic Sepsis in The ICU: Outcome Predictors in A Two-Phase Model and Microbiology FindingsDocument9 pagesResearch Article: Neutropenic Sepsis in The ICU: Outcome Predictors in A Two-Phase Model and Microbiology Findings28121998No ratings yet
- Case 37-2020: A 35-Year-Old Man With Lymphadenopathy and PetechiaeDocument11 pagesCase 37-2020: A 35-Year-Old Man With Lymphadenopathy and PetechiaePatriciaNo ratings yet
- Top Trials in Gastroenterology & HepatologyFrom EverandTop Trials in Gastroenterology & HepatologyRating: 4.5 out of 5 stars4.5/5 (7)
- A Pregnant Woman With Gross Hematuria and Acute Kidney InjuryDocument2 pagesA Pregnant Woman With Gross Hematuria and Acute Kidney InjuryChe GuevaraNo ratings yet
- Dengue Haemorragik Fever Di Ruang Icu Rssi BanjarmasinDocument18 pagesDengue Haemorragik Fever Di Ruang Icu Rssi BanjarmasinAhmad Syamsul ThelionAremaNo ratings yet
- Hiding in The Water: Clinical Problem-SolvingDocument6 pagesHiding in The Water: Clinical Problem-SolvingtabareeNo ratings yet
- Urinary Tract InfectionDocument10 pagesUrinary Tract InfectionEbtehal AbedNo ratings yet
- Erosive GastritisDocument20 pagesErosive GastritisAlliah CasingNo ratings yet
- Management of HemophagocyticDocument10 pagesManagement of HemophagocyticAlexander CanoNo ratings yet
- Leptospirosis CasosDocument2 pagesLeptospirosis CasosfelipeNo ratings yet
- Gastroenterología y Hepatología: Scientific LettersDocument2 pagesGastroenterología y Hepatología: Scientific LettersAswin ArinataNo ratings yet
- Respiratory Tract Infection and Diarrhea As Risk Factors For Relapsing Nephrotic SyndromeDocument3 pagesRespiratory Tract Infection and Diarrhea As Risk Factors For Relapsing Nephrotic SyndromeRudi Saputra BskNo ratings yet
- Ceftriaxone Compared With Sodium Penicillin G For Treatment of Severe LeptospirosisDocument9 pagesCeftriaxone Compared With Sodium Penicillin G For Treatment of Severe LeptospirosisFifi SumarwatiNo ratings yet
- Multidrug-Resistant Tuberculosis and Culture Conversion With BedaquilineDocument10 pagesMultidrug-Resistant Tuberculosis and Culture Conversion With BedaquilineSteven RichardNo ratings yet
- MainDocument3 pagesMainMila KarmilaNo ratings yet
- Pi Is 0016508519325685Document14 pagesPi Is 0016508519325685Sefrilia Miftahul JannahNo ratings yet
- Case Report - TOCILIZUMAB IN CKDDocument5 pagesCase Report - TOCILIZUMAB IN CKDDenisa Carmen ColiofNo ratings yet
- Case Study Direct Observed Therapy (Dot) : College of NursingDocument3 pagesCase Study Direct Observed Therapy (Dot) : College of NursingMM ViedorNo ratings yet
- ITU Comparacion 7 - 14 Dias de TtoDocument9 pagesITU Comparacion 7 - 14 Dias de TtoJohana Zamudio RojasNo ratings yet
- KhifzhonCOVID 19CaseReportActaMedicaIndonesianaDocument6 pagesKhifzhonCOVID 19CaseReportActaMedicaIndonesianaMeike ElvanaNo ratings yet
- Disseminated Tuberculosis Presenting As An Acute AbdomenDocument6 pagesDisseminated Tuberculosis Presenting As An Acute AbdomenIJAR JOURNALNo ratings yet
- Effect of Prednisolone During Defervescence in Dengue Haemorrhagic Fever: An Open Label Controlled StudyDocument4 pagesEffect of Prednisolone During Defervescence in Dengue Haemorrhagic Fever: An Open Label Controlled StudyFabiola StellaNo ratings yet
- Delay in Diagnosis of Extra-Pulmonary Tuberculosis by Its Rare Manifestations: A Case ReportDocument5 pagesDelay in Diagnosis of Extra-Pulmonary Tuberculosis by Its Rare Manifestations: A Case ReportSneeze LouderNo ratings yet
- Acute Liver Failure in Dengue Shock SyndromeDocument3 pagesAcute Liver Failure in Dengue Shock SyndromeInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- PARADocument31 pagesPARAMinerva Medical Treatment Pvt LtdNo ratings yet
- 3.6.4 Event ReportDocument288 pages3.6.4 Event ReportMinerva Medical Treatment Pvt LtdNo ratings yet
- Delhi School Teachers Forum WWW - Dstf.InDocument3 pagesDelhi School Teachers Forum WWW - Dstf.InMinerva Medical Treatment Pvt LtdNo ratings yet
- 1669976294-Wboa Elections 2022-23 Voter ListDocument21 pages1669976294-Wboa Elections 2022-23 Voter ListMinerva Medical Treatment Pvt Ltd100% (1)
- 11-Article Text-35-1-10-20180206Document13 pages11-Article Text-35-1-10-20180206Minerva Medical Treatment Pvt LtdNo ratings yet
- BDS Examiners Panel List 2013Document352 pagesBDS Examiners Panel List 2013Minerva Medical Treatment Pvt LtdNo ratings yet
- Acrsi Directory 1Document344 pagesAcrsi Directory 1Minerva Medical Treatment Pvt LtdNo ratings yet
- PG GQ Stray List-1-2Document136 pagesPG GQ Stray List-1-2Minerva Medical Treatment Pvt Ltd100% (1)
- MDMS 2022 Stray Round Notice 30-11-22Document50 pagesMDMS 2022 Stray Round Notice 30-11-22Minerva Medical Treatment Pvt LtdNo ratings yet
- 5f5f5581c90carajsthan SampleDocument8 pages5f5f5581c90carajsthan SampleMinerva Medical Treatment Pvt LtdNo ratings yet
- CheckDocument208 pagesCheckMinerva Medical Treatment Pvt LtdNo ratings yet
- Acute Kidney Injury in Crush Syndrome and Renal Disaster-Experience in Bangladesh After Garment Factory CollapseDocument6 pagesAcute Kidney Injury in Crush Syndrome and Renal Disaster-Experience in Bangladesh After Garment Factory CollapseMinerva Medical Treatment Pvt LtdNo ratings yet
- Day 2Document1 pageDay 2Minerva Medical Treatment Pvt LtdNo ratings yet
- 19-Article Text-62-1-10-20180126Document2 pages19-Article Text-62-1-10-20180126Minerva Medical Treatment Pvt LtdNo ratings yet
- 2709468899InstituteList Patientsfilled June3Document4 pages2709468899InstituteList Patientsfilled June3Minerva Medical Treatment Pvt LtdNo ratings yet
- 3188-Article Text-4910-1-10-20211113Document3 pages3188-Article Text-4910-1-10-20211113Minerva Medical Treatment Pvt LtdNo ratings yet
- Details of Students Admitted Through NEET PG 2020 21-1-700Document700 pagesDetails of Students Admitted Through NEET PG 2020 21-1-700Minerva Medical Treatment Pvt LtdNo ratings yet
- Book 1Document174 pagesBook 1Minerva Medical Treatment Pvt LtdNo ratings yet
- Management of Donor Kidneys With Double Renal.9Document5 pagesManagement of Donor Kidneys With Double Renal.9Minerva Medical Treatment Pvt LtdNo ratings yet
- Gastrointestinal 132Document8 pagesGastrointestinal 132Minerva Medical Treatment Pvt LtdNo ratings yet
- Eng - OUT SOURCE & Recognised PVT Hosp - To EDPDocument8 pagesEng - OUT SOURCE & Recognised PVT Hosp - To EDPMinerva Medical Treatment Pvt LtdNo ratings yet
- Book 1 CDocument61 pagesBook 1 CMinerva Medical Treatment Pvt LtdNo ratings yet
- National Institute of Mental Health and Neuro Sciences Institute of National Importance BengaluruDocument13 pagesNational Institute of Mental Health and Neuro Sciences Institute of National Importance BengaluruMinerva Medical Treatment Pvt LtdNo ratings yet
- GraduateDocument2,232 pagesGraduateMinerva Medical Treatment Pvt LtdNo ratings yet
- Members City PhoneDocument6 pagesMembers City PhoneMinerva Medical Treatment Pvt LtdNo ratings yet
- Notice 4 PGA Schedule RevisedDocument2 pagesNotice 4 PGA Schedule RevisedMinerva Medical Treatment Pvt LtdNo ratings yet
- Final Result of SS 2022 Round 1Document208 pagesFinal Result of SS 2022 Round 1Minerva Medical Treatment Pvt LtdNo ratings yet
- List of Permitted ASUH Colleges For The Session 2020 21 09.03.2021 - 0Document35 pagesList of Permitted ASUH Colleges For The Session 2020 21 09.03.2021 - 0Minerva Medical Treatment Pvt LtdNo ratings yet
- CV 2020 1Document5 pagesCV 2020 1Minerva Medical Treatment Pvt LtdNo ratings yet
- (DEEMED) Seat Matrix Stray Vacancy Round MD MS DIPDocument26 pages(DEEMED) Seat Matrix Stray Vacancy Round MD MS DIPMinerva Medical Treatment Pvt LtdNo ratings yet
- 3 Neurodevelopmental DisorderDocument11 pages3 Neurodevelopmental DisorderLorie Jane De GuzmanNo ratings yet
- Drtbalu'S Otolaryngology Online: Acute LaryngitisDocument3 pagesDrtbalu'S Otolaryngology Online: Acute LaryngitisAnish RajNo ratings yet
- Colon, Rectum and Anus: Anatomic, Physiologic and Diagnostic Bases For Disease ManagementDocument368 pagesColon, Rectum and Anus: Anatomic, Physiologic and Diagnostic Bases For Disease ManagementBogdan TrandafirNo ratings yet
- The Cost of Vaccine Injuries Vs Treatment For Measles: Forbes Article Vaers SiteDocument1 pageThe Cost of Vaccine Injuries Vs Treatment For Measles: Forbes Article Vaers Siteapi-282292331No ratings yet
- Oral Mucositis in Head and Neck CancerDocument21 pagesOral Mucositis in Head and Neck Canceras1073545No ratings yet
- Algae, Protozoa and FungiDocument46 pagesAlgae, Protozoa and FungiGlenn M. ApuhinNo ratings yet
- 5.05 Don't Hold Your BreathDocument5 pages5.05 Don't Hold Your BreathSummer BNo ratings yet
- The Effect of Icariin On Bone Metabolism and Its Potential Clinical ApplicationDocument12 pagesThe Effect of Icariin On Bone Metabolism and Its Potential Clinical ApplicationBrenda MartinsNo ratings yet
- Intregrated Management of Neonatal Illness (0-2 MonthsDocument30 pagesIntregrated Management of Neonatal Illness (0-2 MonthsMeena Koushal100% (1)
- Hip Joint Restoration: EditorsDocument958 pagesHip Joint Restoration: EditorsOrhan Ramazan100% (1)
- Dermatitis: DefinitionDocument5 pagesDermatitis: DefinitionSuhas IngaleNo ratings yet
- Case PresentationDocument22 pagesCase PresentationManjunath ArunachalamNo ratings yet
- Educational Year Guvendere Secondary School 2Nd Term 5Th Grades 1St English Written ExamDocument3 pagesEducational Year Guvendere Secondary School 2Nd Term 5Th Grades 1St English Written ExamEce Vural ErçinNo ratings yet
- The Homeopathic Choice For ChildrenDocument6 pagesThe Homeopathic Choice For ChildrenLaura GambaNo ratings yet
- Oral Health Guidelines in Comprehensive Cleft CareDocument79 pagesOral Health Guidelines in Comprehensive Cleft CareKassim OboghenaNo ratings yet
- Embryogenesis and Development of TMJDocument40 pagesEmbryogenesis and Development of TMJDr. Fatema HajiNo ratings yet
- PainDocument14 pagesPainAmer Abdulla SachitNo ratings yet
- Chandanpreet KaurDocument54 pagesChandanpreet KaurHarpreet ThindNo ratings yet
- Participate in OHS ProcessDocument40 pagesParticipate in OHS Processmelkamu endaleNo ratings yet
- Hair Loss (About, Types and Treatment) WhatsMedi ResearchDocument5 pagesHair Loss (About, Types and Treatment) WhatsMedi ResearchSiddharth Choudhery100% (1)
- 3 BakteriDocument30 pages3 BakteriBagoes KurniadiNo ratings yet
- Global Business Network: Part IIDocument34 pagesGlobal Business Network: Part IITruthSeeker21No ratings yet
- Trio Remedies - Compiled by DR - KhanDocument7 pagesTrio Remedies - Compiled by DR - KhanGold Sunrise100% (1)
- TUBERCULOSISDocument18 pagesTUBERCULOSISPabloNo ratings yet
- Dietary Advice With or Without Oral Nutritional Supplements For Disease-Related Malnutrition in Adults. Cochrane Database of Systematic Reviews.Document141 pagesDietary Advice With or Without Oral Nutritional Supplements For Disease-Related Malnutrition in Adults. Cochrane Database of Systematic Reviews.Đỗ Trần Giang SơnNo ratings yet
- Penetrating Abdominal Trauma ManagementDocument27 pagesPenetrating Abdominal Trauma ManagementhoangducnamNo ratings yet
- EntrectinibDocument12 pagesEntrectinibMaria Cristina Alarcon NietoNo ratings yet
- ABG AnalysisDocument9 pagesABG AnalysisHoney PrasadNo ratings yet
- 7) Adherent LeucomaDocument6 pages7) Adherent LeucomaDasNo ratings yet
- Gum Disease Natural Remedy p01Document14 pagesGum Disease Natural Remedy p01silvof100% (2)