Professional Documents
Culture Documents
Nilai Rujukan Hematologi Anak
Uploaded by
irdinamarchsyaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nilai Rujukan Hematologi Anak
Uploaded by
irdinamarchsyaCopyright:
Available Formats
PAGE 300
2023 July; 29(3): 300 - 305
p-ISSN 0854-4263 e-ISSN 2477-4685
Available at www.indonesianjournalofclinicalpathology.org
Hematology Reference Values in Indonesian Children
Ina S. Timan1,2, Aryati3
1
Department of Clinical Pathology, Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia. E-mail: ina_st_ui@yahoo.com
2
Faculty of Medicine and Health Sciences, Universitas Kristen Krida Wacana, Jakarta, Indonesia
3
Department of Clinical Pathology, Faculty of Medicine, Universitas Airlangga/Dr. Soetomo General Academic Hospital, Surabaya,
Indonesia
ABSTRACT
Every clinical laboratory has to establish its reference ranges for every parameter analyzed. These reference values are
intervals considered normal in a healthy person's physiological condition. It will be used by the clinician or other health
professionals to interpret the laboratory test results of the patient for making diagnostic decisions, monitoring patient
therapy, and predicting the prognosis and it is also used in epidemiology studies. A reference range is defined as an interval
in which 95% of a reference population's values fall. It is very crucial to establish reference intervals for the local population
as it is sometimes affected by ethnicity, nutrition, food habits, and economic and other local conditions. Hematology is the
most common test performed in a clinical laboratory, and the most used parameter by the clinician including pediatricians.
There up to now no well-established reference interval for hematological parameters in pediatrics and children in Indonesia.
The reference interval used for hematology parameters in Indonesia is based on reference intervals from other countries or
the manufacturer of the hematology analyzers used in a particular laboratory. Establishing a population-specific
hematology reference interval is very difficult for pediatrics and children, so it is rarely performed. This study aims to compile
the results of hematology parameters from Indonesian children to establish an Indonesian reference value for hematology.
The method used was compiling data for the hematology parameter intervals based on studies performed in the Indonesian
population and presented as 95% confidence intervals. A pediatric reference range for several hematology parameters has
been established based on 3 groups of age in Indonesian children.
Keyword: Hematology reference interval, Indonesian children
INTRODUCTION An age-related hematology reference value is
needed for the interpretation of the results.
Hematology parameters are the most common Hematology parameters are often used as a
test asked by clinicians, especially pediatricians for screening test and based on the results in
making clinical decisions. Hematology parameters comparison with the reference values, the clinician
are mostly performed using automated blood cell can order other parameters for diagnosing the
counters, in Indonesia the parameters analyzed are condition of the patients.2,3
for hemoglobin, hematocrit, red blood cell count, red Reference ranges can differ based on gender,
blood cell indices, white blood cell count, white age, geographic condition, altitude, ethnic
blood cell differential count, and platelets. These are background, nutrition, and food habit in each
the most basic hematology tests performed in a country. Normal hematology values presented as the
basic small blood cell counter. Many larger reference value is needed for every country for
instruments can perform more than 30 hematology optimal care of the patients. The reference range for
parameters simultaneously using only around pediatric patients are very difficult to obtain, unlike
150-300 mL whole blood. It is a very efficient test, adult reference values, which can be obtained from
using a small amount of blood, and generating many medical check-up patients or blood donors, healthy
useful parameters, especially in babies and small baby or children are rarely asked to be tested. No
children.1,2 current Indonesian-based pediatric hematology
Hematology parameters give information for use reference values are available, hopefully, this
in routine assessment for diagnosis of red blood reference value will be very useful for the care of the
cells, white blood cells, platelet disorders, infectious children in Indonesia.1,4,5 By compiling data from
diseases, immune status, choosing the right several studies in Indonesia, a more specific
management plan for the patients, monitoring the reference range for Indonesian children can be
outcome of therapy, and predicting the prognosis. established.
Hematology Reference Values - Timan, et al.
Indonesian Journal of Clinical Pathology and Medical Laboratory, 2023 July, 29 (3) : 300 - 305 PAGE 301
METHODS values interval in hematology is usually categorized
as newborns, infants, babies, children, and teenagers
By compiling data from reports and publications or young adults.1,5,6 In Table 1 the hematology
on the hematology parameter studies in Indonesia a parameters are grouped into babies (1 year old),
reference range was established. Data were primary school-aged children (between 7 to 12 years
compiled from a study of 1-year-old healthy babies, old), and secondary school-aged teenagers
healthy primary school children in Jakarta, and (between 13 to 15 years old). Results were quoted
secondary school children in West Java. All of these from 3 different studies, all subjects were healthy
studies were performed in Cipto Mangunkusumo children, as evaluated by pediatricians. The studies
Hospital using Sysmex automated blood cell were performed in Jakarta and West Java, Indonesia,
counters. The reference values were categorized into all using Sysmex hematology analyzers.7-9
3 groups; babies, children from 8 to 12 years old, and The results of the hematology parameters in 12
children older than 12 to 15 years old.6-9 months old babies were deducted from studies in
Jakarta, in middle-income families. The reference
Results for reference values of hematology in values in primary school-age children aged 8-12
children years old were taken from studies in Jakarta, also in
The reference range for hematology parameters middle-income families, and the reference values in
in various age groups is different. The reference the older children were from secondary school
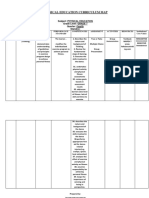
Table 1. The reference value of hematology parameters in babies, children and teenagers7-9
Parameter Unit Mean SD Range
Baby 12 months (N=100)
Hemoglobin g/dL 11.5 0.99 9.5-13.5
Hematocrit % 34.8 2.56 30-40
6
Red Blood Cell (RBC) 10 /mL 4.69 0.32 4.05–5.33
Mean Cell Volume (MCV) fL 74.4 4.81 65-84
Mean Cell Hemoglobin (MCH)* pg 24.9 20-28
Mean Cell Hemoglobin Concentration (MCHC) g/dL 33.1 1.26 31-36
3
White Blood Cell (WBC)* 10 /mL 12.6 7.4–17.5
3
Platelet * 10 /mL 267 155.09 106–523
Red Cell Distribution Width (RDW-SD) fL 40.9 3.31 34.5-47.1
Children 8-12 years (N=120)
Hemoglobin (Hgb) g/dL 12.8 0.86 11.1–14.5
Hematocrit (Hct) % 36.3 2.11 32.1–40.5
6
Red Blood Cell (RBC) 10 /mL 4.55 0.29 3.97–5.13
Mean Cell Volume (MCV) fL 80 3.37 73–87
Mean Cell Hemoglobin (MCH)* pg 28.1 26-30
Mean Cell Hemoglobin Concentration (MCHC) g/dL 35.2 0.91 33-37
3
White Blood Cell (WBC)* 10 /mL 8.2 1.97 4.3–12.1
3
Platelet (PLT)* 10 /mL 369 204-534
Children-Teenagers 12-15 years (N= 60)
Hemoglobin (Hgb)* g/dL 13.3 11.2-15.2
Hematocrit (Hct)* % 39.4 34–43.3
6
Red Blood Cell (RBC) 10 /mL 4.77 0.47 3.83–5.71
Mean Cell Volume (MCV)* fL 83.4 61.4-89.6
Mean Cell Hemoglobin (MCH)* pg 28.3 19.3–30.4
Mean Cell Hemoglobin Concentration g/dL 33.9 32-35
(MCHC)*
3
White Blood Cell (WBC) 10 /mL 7.5 1.64 4.2–10.8
3
Platelet (PLT) 10 /mL 311 69.08 173-449
Red Cell Distribution Width (RDW-CV)* fL 13.1 11.8–16.6
Results were calculated as mean ±2SD except those marked with * were calculated as 5th to 95th percentile
Hematology Reference Values - Timan, et al.
Indonesian Journal of Clinical Pathology and Medical Laboratory, 2023 July, 29 (3) : 300 - 305 PAGE 302
children in West Java, also in middle-income anemia as normocytic, microcytic, and macrocytic.
families.7-9 MCH is the average amount of hemoglobin in RBC,
its value lowers in iron deficiency and other
The use of reference values hypochromic anemia. MCHC is the average
Reference interval values should be provided for concentration in a certain volume of RBC, the ratio of
each laboratory result produced by the laboratory. It hemoglobin to hematocrit. The MCH and MCHC are
is used as a decision-making tool to differentiate used to measure the hemoglobin concentration in
between the healthy and diseased populations, for the RBC, classifying it as hypochromic,
physicians to determine the management of the normochromic, or hyperchromic. The RDW can give
patients. Reference values are usually derived from information on normal or increased variation in the
normal healthy subjects. Determination of reference size of RBC, known as the degree of anisocytosis.
range values is very difficult in pediatric subjects; it MCHC can be used together with MCV and RDW for
changes with age due to physiological determining the possible cause of anemia. Normal
developments from birth to adolescence and the MCHC values can be observed in kidney disease,
rare opportunity to get blood from healthy pediatric bone marrow failure, and hemolytic anemia. Low
subjects. Normal subjects can also give different MCHC can be found in iron deficiency, thalassemia,
results based on the nutrient variation, socio- sideroblastic anemia, and anemia of chronic disease.
economic condition, and different altitudes in each An increase in MCHC can occur in hereditary
area of Indonesia.10,11 spherocytosis and liver disease.14
Hematology parameters basically consisted of An increase in RDW even within normal limits of
the parameters for RBC, WBC, and platelets. Each normal CBC results, should be confirmed by blood
group consisted of several parameters. Modern smear and further investigated. RDW changes can be
blood cell counters can give more extended results observed in impending anemia, iron deficiency,
based on calculation and conventional impedance hemoglobinopathies, and kidney disease. The
method, they can also use flow cytometry and combination of the anemia type and RDW will be
cytochemistry for detection and calculations.1 more useful. Normal RDW with microcytic MCV can
It is sometimes difficult to collect venous blood be found in thalassemia, normal RDW with
from babies and very small children. A study to normocytic MCV can be observed in anemia of
evaluate the measurement of CBC by venous and chronic disease and hereditary spherocytosis, an RBC
capillary blood in children below age 5-9 years with with macrocytic MCV can be found in liver disease or
acute gastroenteritis showed that it has still good preleukemic condition. High RDW in microcytic MCV
reliability with sensitivity and specificity of 86-98% can be observed in iron deficiency anemia, and high
and accuracy of 95%. Comparison of matched pairs RDW with normocytic RBC can be found in combined
showed some slightly higher red blood cell counts, anemia, sickle cell disease, and sideroblastic anemia.
hemoglobin, and platelets.12 High RDW with macrocytic red blood cells can be
found in B12 and folate deficiency.14,15
Detection of anemia and polycythemia Results of red cell abnormalities can be used as a
Containing oxygen-carrying capacity, causing base to do more specific tests to know the cause of
insufficiency to meet the body' Hematology the abnormalities. Pediatric anemia can be caused by
parameters are very useful for clinicians. It gives acute, chronic, or iatrogenic blood loss; decreased
information on the condition and changes in RBC, erythrocyte production; increased destruction of
WBC, platelets, and their cross interactions. The RBC erythrocytes, as with hemolysis; or shortened
parameters can give information on the hemoglobin, erythrocyte survival. Polycythemia is most
hematocrit, RBC count, RBC indices, and red cell commonly defined as a venous hematocrit greater
distribution width. Based on the results clinicians can than 65%.1,4,13
interpret whether the subject is normal, have anemia Reference values and cut-off points from
or hemoconcentration, or polycythemia. Anemia is publications can identify populations with a higher
defined as a deficiency in the concentration of RBC risk of anemia and facilitate its management and
and the hemoglobin s physiological needs. It can monitoring, also assessing prevention methods.5 The
also give information on the type of anemia, World Health Organization (WHO) has
suspected nutrient deficiency, hemoglobinopathies, recommended the classification of anemia based on
and other red cells abnormalities.1,4,13 hemoglobin levels (Table 2).4,15
The red cell indices, such as MCV are used for The WHO cut-off points for determining anemia
quantifying the size of the RBC and classifying in babies and children differed. The lower
Hematology Reference Values - Timan, et al.
Indonesian Journal of Clinical Pathology and Medical Laboratory, 2023 July, 29 (3) : 300 - 305 PAGE 303
Table 2. Anemia classification by WHO4
Hemoglobin (g/dL)
Age Population
Non-Anemia Mild Anemia Moderate Anemia Severe Anemia
6-50 months > 11.0 10-10.9 7- 9.9 < 7.0
5-11 years > 11.5 11-11.4 8-10.9 < 8.0
12-14 years > 12.0 11-11.9 8-10.9 < 8.0
hemoglobin reference values for babies, children, and decreased in females after puberty. There were
and teenagers in Indonesia were slightly lower from no differences according to gender in children
13.6%, 3.5%, and 6.7%, respectively in each age before puberty.19
group. This should be considered when hemoglobin
levels are used for determining anemia in White blood cells and platelet abnormalities
epidemiological studies or in clinical practice. The Using the reference value for WBC or leukocytes,
reference values for hemoglobin, hematocrit, and clinicians can suspect or confirm the presence of
RBC indices (MCV and MCH) showed a slight infection, inflammation, or other conditions. White
increase by age group.7-9 blood cells are the main body defense against invading
The value of RDW can also be applied for microorganisms. The WBC is usually differentiated
screening iron deficiency anemia and differentiating into granulocytes and non-granulocytes. More
it from thalassemia.16 Red cell distribution width can sophisticated hematology analyzers can perform a 5 or
be expressed as RDW-SD or RDW-CV, with the 7 differential count in WBC count using flow
normal reference of 42.5±3.5 fL and 12.8±1.2%, cytometry-based tests.1 Increased WBC or leukocytosis
respectively. These values are almost reported the can be found in most bacterial infections, but some
same in children and adults. The values of RDW infections can cause leucopenia. A very high count of
reported in the Indonesian children study is almost WBC can also be found in leukemoid reactions or
the same (Table 1).1,7-9 leukemia, which should be confirmed by morphology
Nutritional-related anemia is still one of the major studies or other tests. Low WBC count can be found in
burdens in the health care system in the world viral infection, sepsis, or other abnormalities in the
including Indonesia, most subjects are treated as marrow. As observed in Table 1, the WBC slightly
iron deficient anemia. Through several studies, decreased in older children groups. White blood cell
parameters used to detect the anemia were the count can be used for monitoring after treatment of
measurement of hemoglobin and hematocrit, some inflammation, infection and certain malignancy. White
also included the reticulocyte hemoglobin blood cell count can differ up to 14% when taken in the
measurement as a monitoring test. In a study based morning in resting subjects, compared to other times
on Riskesdas 2018, it was reported that 40.4% of of the day, although the diurnal variation is not clear.
children under 5 years old in Indonesia had anemia The WBC count in the babies and children age group is
with 11.2% moderate and severe anemia. Anemia within the same range reported, babies 11±5 103/mL,
was diagnosed if the hemoglobin levels were below children 9±4 103/mL after 12 years old 4-10 103/mL.1,20
11 g/dL. Most anemia was reported only based on The total WBC count and monocyte count were
hemoglobin levels, and erythrocyte indices, which highest at birth then rapidly decreased in the first 6
could predict the cause of anemia were not usually months of life, then showed a slight reduction until 2
analyzed. It can be observed many presumed healthy years of age. Lymphocyte counts were low during
babies have hemoglobin levels under 11 g/dL. infancy and increased to their highest level at 6
Although to diagnose iron deficiency other tests months of age, decreasing moderately again until 9
should be done, such as serum iron, total iron years of age. The pattern of neutrophil count
binding capacity, and ferritin measurement, most changed in the opposite of the lymphocyte. There
anemia in Indonesia were presumed as iron were no patterns of eosinophil and basophil that
deficiency. Iron supplements are rarely given to were related to changes in age. Gender differences
children below 12 years old. Other nutritional anemia were only observed after puberty. Physiological
was very rarely reported although intervention given development had some effect on the changes in the
usually included folic acid and other vitamins.17,18 hematology parameters during infancy to puberty.21
Reference values for hematology are a Changes in the platelet count can be identified as
progressive condition based on age. In a study in thrombocytosis (increase in platelet count) or
Korea in 66.611 children aged 3-17 years old it was thrombocytopenia (decrease in platelet count).
found that RBC increased with age until adulthood, Changes in platelets can be caused by a decrease in
Hematology Reference Values - Timan, et al.
Indonesian Journal of Clinical Pathology and Medical Laboratory, 2023 July, 29 (3) : 300 - 305 PAGE 304
production, sequestration, trapped in the spleen, or count below 4000/uL. In COVID-19 infection 83.2%
due to small platelet clumps. These conditions can be of patients also had distinct lymphopenia less than
observed in bacterial or viral infection, sepsis, 1.500/uL and because of the other infection, the
disseminated intravascular coagulation, autoimmune neutrophils increased, which cause the NLR increase
diseases, congenital anomaly syndromes, bleeding, in patients with positive PCR for COVID-19. The NLR
and other conditions. Thrombocytosis can also be became the screening instrument for suspicion of
observed as a physiological reaction in many COVID-19. In smaller children, the decrease of WBC
conditions, or due to contamination of small RBC. and lymphocytes were not so low compared to older
Thrombocytosis can be related to a reactive children or adults. It was related to higher natural
condition such as chronic infection and killer cells in children compared to adults. The
inflammation, malignancy, post-splenectomy, increase of neutrophils correlated with the severity of
acute blood loss, and iron deficiency. It can the disease.22,23
also be related to myeloproliferative neoplasm Platelet counts in children with COVID-19
(essential thrombocytosis, polycythemia vera) or as a infection were reduced more compared to adults. In
part of a congenital disorder.14 severe COVID-19 infections, the platelet counts were
Thrombocytopenia can also be found due to less than 150x103/mL. Platelet to Lymphocyte Ratio
small platelet aggregations in autoimmune (PLR) marker can also be used to evaluate the degree
conditions or in reactive platelets. of infection and is related to cytokine storm in
Thrombocytopenia is often observed in viral COVID-19 infection, just like NLR. This PLR is rarely
infections such as dengue hemorrhagic syndrome, mentioned in children, but PLR greater than 126.7 is a
COVID-19, post-chemotherapy, congenital predictor of the worsening condition of the patient.
disorders (Gaucher disease, neonatal autoimmune The average hemoglobin in children with
thrombocytopenia), splenomegaly or after COVID-19 was significantly reduced, and those with
transfusion, Disseminated Intravascular Coagulation severe conditions also had lower hemoglobin levels.
(DIC).14 Low platelet count should be confirmed to It was proposed that the cause of lower hemoglobin
ensure that it was not caused by a technical error, was related to the increase of ferritin and less iron
check the integrity of the sample, check for the that can be used by the RBC to produce hemoglobin.
presence of microclots, and check in the blood smear It was also reported that this infection also destroys
for platelet satellitism and clumping. Platelets kidney tissues rich in ACE2 receptors, which will
showed a slight diurnal variation of up to 5%, eventually reduce RBC production.22
megakaryocyte platelet release mostly happens late
at night and early morning. The platelets showed a CONCLUSION
slight decrease in the increasing age groups. Platelet
count reported in the Indonesian children is within Hematology is the most common test performed
the same range, babies 200-550 103/mL, children in a clinical laboratory and is also the most used
170-450 103/mL after 12 years old 280±180 103/mL.1 parameter by clinicians, especially pediatricians. An
established reference interval for hematological
Hematology parameters in COVID-19 infection parameters in babies and children in Indonesia
CBC is the most frequent test used in clinical would be very useful in the epidemiological or
practice, the use is more prominent in the COVID-19 clinical setting. The hematology reference ranges
era, especially in the differential count used to were categorized as babies, children aged 8 to 12,
evaluate its role in immunity. In the daily practice and more than 12 to 15 years old. Some of the
with automated blood cell counter, although many pediatric hematology reference values reported
useful parameters can be analyzed using a single slightly differed compared to those used by WHO or
sample of blood not every clinician makes use of its reported in other countries, a specific age and ethnic
interpretation for patient care. Each parameter or reference value will be beneficial in managing
combine parameters can give hints about the pediatric patients.
patient's condition. Lymphocyte and necrophile
counts were used as a factor in distinguishing the REFERENCES
COVID-19 infection from other viral and bacterial
infection.22 1. Bates I. Reference ranges and normal values. In Bain
During the COVID-19 pandemic, WBC counts BJ, Bates I, Laffan MA, Lewis SM(Eds). Dacie and Lewis
plays an important role, especially in lymphocytes Practical hematology. 12th Ed., International China
and neutrophils. It was observed that 25-33.7% of Elsevier, 2107; 8-17.
the patients suffered from leukopenia with a WBC 2. Khusun H, Yip R, Schultink W, Dillon HS. World Health
Hematology Reference Values - Timan, et al.
Indonesian Journal of Clinical Pathology and Medical Laboratory, 2023 July, 29 (3) : 300 - 305 PAGE 305
Organization hemoglobin cut-off points for the Prihatni D. Concordance test of various erythrocyte
detection of anemia are valid for an Indonesian indices for screening of beta thalassemia carrier.
population. J Nutrition, 1999; 129: 1669–74. Indones J Clinical Pathol Med Laboratory, 2022; 28(2):
3. Yalew A, Terefe B, Alem B, Enawgaw B. Hematological 137-42.
reference intervals determination in adults at Gondar 14. Erhabor O, Muhammad HA, Onwuchekwa C, Egenti
University Hospital, Northwest Ethiopia. BMC Res NB. Interpretation of full blood count parameters in
Notes, 2016; 9: 483. health and disease. Haematol Int J, 2021; 5(1): 10080.
4. World Health Organization. Haemoglobin 15. Del Cacho BR, del Castilo YM. Anemia classification
concentrations for the diagnosis of anaemia and and diagnosis. Pediatr Integral, 2021; XXV(5): 214-21.
assessment of severity. VMNIS WHO/NMH/ 16. Mataos JF, Borges KBG, Fernandes APS, Faria JR,
NHD/MNM/11.1. Available from https://apps.who.int Carvalho MG. RDW as a differential parameter
/iris/bitstream/handle/10665/85839/WHO_NMH_NH between microcytic anemias in pure and concomitant
D_MNM_11.1_eng.pdf (accessed Sept 5, 2022). forms. J Bras Patol Med Lab, 2015; 51: 22-7.
5. Mansyur M, Khoe LC, Karman MM, Ilyas M. Improving 17. Juffrie M, Helmyati S, Hakimi M. Nutritional anemia in
workplace-based intervention in Indonesia to prevent Indonesia children and adolescents: diagnostic
and control anemia. J Prim Care Community Health, reliability for appropriate management. Asia Pac J Clin
2019; 10: 1-7. Nutr, 2020; 29(Suppl 1): S18-31.
6. Timan IS, Aulia D, Atmakusuma D, Sudoyo A, 18. Djaiman SPH, Nurhidayati N, Kristanto AY.
Windiastuti E, Kosasih A. Some hematological Determinants of anemia in children under five years in
problems in Indonesia. Int J Hematol, 2002; 76 (1): Indonesia. 2022. Available from: https://ejournal2
286–290. litbang.kemkes.go.id/index.php/mpk/article.
7. Funahara Y. Reports field evaluation for anemia https://doi.org/10.22435/mpk.v32i 1.5360 (accessed
Indonesia. Japan Society for the Promotion of Science. Feb 1, 2023).
Kobe, 2000; 19. Nah EH, Kim S, Cho S, Cho HI. Complete blood count
8. Firmansyah A. Reports field survey for children in reference intervals and patterns changesbacros
South Jakarta. Faculty of Medicine University of pediatric, adult and geriatric ages in Korea. Ann Lab
Indonesia, Jakarta, 2007; Med, 2018; 38: 503-11.
9. Timan IS, Tatsumi N, Funahara Y, Aulia D, Margono S, 20. Benson VS, Hartl S, Barnes N, Galwey N, Dyke MKV,
Sayogo S, et al. Anemia in Indonesian school children. et al. Blood eosinophil counts in the general
ICMR Annals, 2000; 20: 223–230. population and airways disease: A comprehensive
10. El Nageh MM, Heuck CC, Appel W, Vandepitte J, review and meta-analysis. Eur Respir J, 2022; 59:
Engbaek K, Gibbs WN. Pre-analytical control. In basic 2004590.
of quality assurance for intermediate and peripheral 21. Li K, Peng YG, Yan RH, Song WQ, Peng XX, Ni X. Age
laboratory. WHO Publication, 1992; 1-7. dependent changes in total and differential white
11. Cho SM, Lee SG, Kim HS, Kim JH. Establishing pediatric blood cell count in children. Chinese Med J, 2020;
reference intervals for 13 biochemical analytes 133(16): 1900-6.
derived from normal subjects in a pediatric 22. Liu L, She J, Bai Y, Liu W. SARS-CoV-2 infection:
endocrinology clinic in Korea. Clinical Biochemistry, Differences in hematological parameters between
2014; 47: 268–71. adults and children. Int J Gen Med, 2021; 14: 3035-47.
12. Wiesniewska HW, Nowak JK, Dabrowski M, 23. Kosmeri C,Koumpis E, Tsabouri S, Siomou E, Makis A.
Szydlowska P, Szczepanik M, et al. Reliability of Hematological manifestations of SARS-CoV-2 in
complete blood count in children with acute children. Pediatr Blood Cancer, 2020; 67e: 1-9.
gastroenteritis. Frontiers in Paed, 2021; 9: 1-6.
13. Nurazizah R, Handika RS, Sahiratmadja E, Ismiarto YD,
Hematology Reference Values - Timan, et al.
You might also like
- Financial Planning GodrejDocument199 pagesFinancial Planning GodrejriteshnaikNo ratings yet
- Padeye Deign.Document14 pagesPadeye Deign.Bolarinwa100% (3)
- 1888 For Almost DUMMIES - Robert J WielandDocument126 pages1888 For Almost DUMMIES - Robert J Wielandpropovednik100% (1)
- Hematology Reference Values in Indonesian ChildrenDocument16 pagesHematology Reference Values in Indonesian ChildrenRini WidyantariNo ratings yet
- Blues A La Machito - CongasDocument2 pagesBlues A La Machito - CongasDavid ScaliseNo ratings yet
- Ethics and Social ResponsibilityDocument16 pagesEthics and Social Responsibilitypallavi50% (2)
- TAT For Issuing Blood Products in EmergencyDocument4 pagesTAT For Issuing Blood Products in Emergencyirdinamarchsya100% (1)
- Case Study Walking The WalkDocument3 pagesCase Study Walking The Walk9899 Mariam Akter Marketing100% (1)
- Primer On Probation Parole and Exec Clemency ApprovedDocument2 pagesPrimer On Probation Parole and Exec Clemency ApprovedMinerva LopezNo ratings yet
- BS EN ISO 14253 12017 (The British Standards Institution) (Z-Library) PDFDocument32 pagesBS EN ISO 14253 12017 (The British Standards Institution) (Z-Library) PDFMohammed SirelkhatimNo ratings yet
- Haematologist-Reviewed Peripheral Blood Smear in PDocument6 pagesHaematologist-Reviewed Peripheral Blood Smear in PElba AlvarezNo ratings yet
- Prinsip Kerja MGITDocument6 pagesPrinsip Kerja MGITirdinamarchsyaNo ratings yet
- 382-Article Text-1808-1-10-20210816Document8 pages382-Article Text-1808-1-10-20210816Dr. Asaad Mohammed Ahmed BabkerNo ratings yet
- Salinan 58088-ID-nilai-rujukan-hematologi-orang-dewasa-noDocument9 pagesSalinan 58088-ID-nilai-rujukan-hematologi-orang-dewasa-nodian artasariNo ratings yet
- RI, Hema&immnoDocument9 pagesRI, Hema&immnoHabtamu WondifrawNo ratings yet
- Anemia in Pre-School Children-Does Time Change Anything?Document5 pagesAnemia in Pre-School Children-Does Time Change Anything?NZ FreelancersNo ratings yet
- د978-1-62808-755-0_eBookDocument9 pagesد978-1-62808-755-0_eBookahmadburhan770No ratings yet
- Retic IronDocument4 pagesRetic IronIndahNo ratings yet
- Relationship Between Hemoglobin and Platelet Count Among MBBS StudentsDocument5 pagesRelationship Between Hemoglobin and Platelet Count Among MBBS StudentsIJAR JOURNALNo ratings yet
- The Cutoff Values of Indirect Indices For Measuring Insulin Resistance For Metabolic Syndrome in Korean Children and AdolescentsDocument6 pagesThe Cutoff Values of Indirect Indices For Measuring Insulin Resistance For Metabolic Syndrome in Korean Children and AdolescentsSathyanarayana SrikantaNo ratings yet
- Hubungan Umur Dan Gender Dan AlbuminDocument6 pagesHubungan Umur Dan Gender Dan Albuminnandy surya kusumaNo ratings yet
- Salinan 58088-ID-nilai-rujukan-hematologi-orang-dewasa-noDocument13 pagesSalinan 58088-ID-nilai-rujukan-hematologi-orang-dewasa-nodian artasariNo ratings yet
- Paediatrica Indonesiana: Original ArticleDocument4 pagesPaediatrica Indonesiana: Original ArticleInge Dackrisna DaudNo ratings yet
- Publication For NeoMass AAAC 2019Document11 pagesPublication For NeoMass AAAC 2019Ranjith EswaranNo ratings yet
- Jalm 0366Document12 pagesJalm 0366Erick MartinezNo ratings yet
- Age-Sex Related in Hematological Values of Sandalwood Pony Horses (Equus Caballus) in East Sumba, NTTDocument7 pagesAge-Sex Related in Hematological Values of Sandalwood Pony Horses (Equus Caballus) in East Sumba, NTTmatius markusNo ratings yet
- Abnormal Laboratory ResultsDocument3 pagesAbnormal Laboratory Resultstotty331117867No ratings yet
- Older Blood RBC StoredDocument14 pagesOlder Blood RBC StoredPRADEEPNo ratings yet
- Interpreting Statistics in Medical Literature: A Vade Mecum For Surgeons1 1no Competing Interests DeclaredDocument19 pagesInterpreting Statistics in Medical Literature: A Vade Mecum For Surgeons1 1no Competing Interests DeclaredvigneshNo ratings yet
- HB SahliDocument10 pagesHB SahliDewi Miranda SaputriNo ratings yet
- MCN 12870Document31 pagesMCN 12870Megan HarperNo ratings yet
- 1833 Manuscript 7430 1 10 20180428Document6 pages1833 Manuscript 7430 1 10 20180428sagarNo ratings yet
- Discriminatory Precision of Neutrophil Gelatinase Associated Lipocalin in Detection of Urinary Tract Infec Tion in Children: A Systematic Review and Meta-AnalysisDocument14 pagesDiscriminatory Precision of Neutrophil Gelatinase Associated Lipocalin in Detection of Urinary Tract Infec Tion in Children: A Systematic Review and Meta-AnalysisFlorencia VazquezNo ratings yet
- Characteristics and Predictive Value of PDFDocument13 pagesCharacteristics and Predictive Value of PDFMedefound IngravityNo ratings yet
- Sample Size Guidelines For LogDocument10 pagesSample Size Guidelines For LogHospital BasisNo ratings yet
- 10 11648 J JFMHC 20180401 11 PDFDocument4 pages10 11648 J JFMHC 20180401 11 PDFFusvita MerdekawatiNo ratings yet
- Adiposity ReboundDocument9 pagesAdiposity ReboundImanuel Far-FarNo ratings yet
- RRHGBX RetrieveDocument14 pagesRRHGBX Retrieve585mh4krp6No ratings yet
- Journal Hemoglobin Profile Thalassemia 4 PDFDocument4 pagesJournal Hemoglobin Profile Thalassemia 4 PDFRake AndaraNo ratings yet
- Role of Hematological Scoring System in Diagnosis of Neonatal SepsisDocument7 pagesRole of Hematological Scoring System in Diagnosis of Neonatal SepsisIJAR JOURNALNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument15 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive Biologybidan22No ratings yet
- Establishing Reference Ranges of Hematological Parameters From Malian Healthy AdultsDocument11 pagesEstablishing Reference Ranges of Hematological Parameters From Malian Healthy AdultsnurulNo ratings yet
- Hematological Profile of Normal Pregnant Women in Lagos, NigeriaDocument6 pagesHematological Profile of Normal Pregnant Women in Lagos, NigeriadinaNo ratings yet
- 1 MultimethodassessmentDocument8 pages1 MultimethodassessmentRoberto Alexis Molina CampuzanoNo ratings yet
- 46-51 WinandaDocument7 pages46-51 WinandaRIMA MELATI ANGGRAENINo ratings yet
- The Association of Blood Pressure and Primary Open-Angle Glaucoma: A Meta-AnalysisDocument23 pagesThe Association of Blood Pressure and Primary Open-Angle Glaucoma: A Meta-AnalysisSarah Martinauli HarahapNo ratings yet
- Jurding AnakDocument12 pagesJurding AnakRuri TatembaNo ratings yet
- Chen 2013Document6 pagesChen 2013malaNo ratings yet
- Haematological Changes in Malaria-Infected Children in North-West NigeriaDocument6 pagesHaematological Changes in Malaria-Infected Children in North-West NigeriamubarakNo ratings yet
- Reference Intervals For Serum Creatinine in Nepal.Document5 pagesReference Intervals For Serum Creatinine in Nepal.editorjmstNo ratings yet
- Sensitivity and specificity of procalcitonin in diagnosing neonatal sepsisDocument5 pagesSensitivity and specificity of procalcitonin in diagnosing neonatal sepsishardianNo ratings yet
- Differences Between Human Plasma and Serum Metabolite ProfilesDocument6 pagesDifferences Between Human Plasma and Serum Metabolite ProfilesjoaquimmendesNo ratings yet
- Wellcomeopenres 3 16570Document17 pagesWellcomeopenres 3 16570Naila MudzalifahNo ratings yet
- IntJMedPublicHealth 2015 5 4 322 165963Document6 pagesIntJMedPublicHealth 2015 5 4 322 165963dudidumNo ratings yet
- Platelet width as clue to diabetes complicationsDocument3 pagesPlatelet width as clue to diabetes complicationsDr. Asaad Mohammed Ahmed BabkerNo ratings yet
- Statistics Biology Experiments Medicine Pharmacy Agriculture FisheryDocument15 pagesStatistics Biology Experiments Medicine Pharmacy Agriculture Fisherykavya nainitaNo ratings yet
- A Study On Growth Profiles in Children With Thalassemia Major Between 2-10 Years of Age On Regular Transfusions and Oral Chelation TherapyDocument9 pagesA Study On Growth Profiles in Children With Thalassemia Major Between 2-10 Years of Age On Regular Transfusions and Oral Chelation TherapysagarNo ratings yet
- Sampling Methods ExplainedDocument12 pagesSampling Methods ExplainedPUBG HackerNo ratings yet
- Analysis of Aso Titres Among Paediatric Age Group Patientsattending A Tertiary Care Hospital Secunderabad Telangana PDFDocument5 pagesAnalysis of Aso Titres Among Paediatric Age Group Patientsattending A Tertiary Care Hospital Secunderabad Telangana PDFWeal AlhaidaryNo ratings yet
- Soluble Endothelial Protein C Receptor Levels in Egypt - 2018 - Pediatric HematoDocument4 pagesSoluble Endothelial Protein C Receptor Levels in Egypt - 2018 - Pediatric HematoMichael John AguilarNo ratings yet
- Current Databases On Biological Variation: Pros, Cons and ProgressDocument10 pagesCurrent Databases On Biological Variation: Pros, Cons and ProgressCarlos PardoNo ratings yet
- 1382-Article Text-5022-1-10-20180430 PDFDocument4 pages1382-Article Text-5022-1-10-20180430 PDFFadillNo ratings yet
- Anemia in Pregnancy in Malaysia: A Cross-Sectional Survey: Original ArticleDocument10 pagesAnemia in Pregnancy in Malaysia: A Cross-Sectional Survey: Original ArticleThomson AffendyNo ratings yet
- Hematologic Dysfunction Criteria in Critically Ill ChildrenDocument5 pagesHematologic Dysfunction Criteria in Critically Ill ChildrenHardian RakhmawardanaNo ratings yet
- Regression Models For Twin StudiesDocument11 pagesRegression Models For Twin StudiesMemoyErandiNo ratings yet
- Iron Def IJPDocument5 pagesIron Def IJPPrahbhjot MalhiNo ratings yet
- 79 - 6 - 506.pdf Filename UTF-8''79 (6) 506 PDFDocument6 pages79 - 6 - 506.pdf Filename UTF-8''79 (6) 506 PDFvindra30No ratings yet
- Prevalence and Risk Factors of Anemia in Under Five-Year-Old Children in Children's HospitalDocument4 pagesPrevalence and Risk Factors of Anemia in Under Five-Year-Old Children in Children's Hospitalindahsarizahab 28No ratings yet
- Long-Term Neurobehavioral and Quality of Life Outcomes of Critically Ill Children After Glycemic ControlDocument12 pagesLong-Term Neurobehavioral and Quality of Life Outcomes of Critically Ill Children After Glycemic ControlRayhand MubarakhNo ratings yet
- Winter School Immuno Flyer 2020Document2 pagesWinter School Immuno Flyer 2020irdinamarchsyaNo ratings yet
- Permintaan Lab Disertai Ket KlinisDocument1 pagePermintaan Lab Disertai Ket KlinisirdinamarchsyaNo ratings yet
- Lab Result in EnglishDocument3 pagesLab Result in EnglishirdinamarchsyaNo ratings yet
- Pre Training Discussion - BD FACSLyricDocument48 pagesPre Training Discussion - BD FACSLyricirdinamarchsyaNo ratings yet
- 2021 Course Outline Operations Management Tutorial MTM C10Document5 pages2021 Course Outline Operations Management Tutorial MTM C10irdinamarchsyaNo ratings yet
- Competency Are Your Staff Adequately TrainedDocument36 pagesCompetency Are Your Staff Adequately TrainedirdinamarchsyaNo ratings yet
- Academic Program 2020Document2 pagesAcademic Program 2020irdinamarchsyaNo ratings yet
- Audit ToolDocument1 pageAudit ToolirdinamarchsyaNo ratings yet
- AACB Jill Tate ScholarshipDocument3 pagesAACB Jill Tate ScholarshipirdinamarchsyaNo ratings yet
- Thesis Complete Uganda PDFDocument143 pagesThesis Complete Uganda PDFirdinamarchsyaNo ratings yet
- Competency Are Your Staff Adequately TrainedDocument22 pagesCompetency Are Your Staff Adequately TrainedirdinamarchsyaNo ratings yet
- Strengthening Regional Viral Hepatitis Laboratory CapacityDocument23 pagesStrengthening Regional Viral Hepatitis Laboratory CapacityirdinamarchsyaNo ratings yet
- Competency Are Your Staff Adequately TrainedDocument22 pagesCompetency Are Your Staff Adequately TrainedirdinamarchsyaNo ratings yet
- Manufacture of QCDocument19 pagesManufacture of QCirdinamarchsyaNo ratings yet
- Physician health statement for employmentDocument1 pagePhysician health statement for employmentirdinamarchsyaNo ratings yet
- The Challenges and Benefit of Internal Auditing PDFDocument27 pagesThe Challenges and Benefit of Internal Auditing PDFirdinamarchsyaNo ratings yet
- BJSTR - Challenges in Early Infant Diagnosis of Beta ThalassemiaDocument4 pagesBJSTR - Challenges in Early Infant Diagnosis of Beta ThalassemiairdinamarchsyaNo ratings yet
- Use of Genexpert For Clinically Suspected MDR TBDocument6 pagesUse of Genexpert For Clinically Suspected MDR TBirdinamarchsyaNo ratings yet
- Antibiotik Yg Ada D RSKDDocument1 pageAntibiotik Yg Ada D RSKDirdinamarchsyaNo ratings yet
- 01 - Current Draft WHO-CDC Biosafety RecommendationsDocument32 pages01 - Current Draft WHO-CDC Biosafety RecommendationsitsruriNo ratings yet
- Blood Request FlowchartDocument1 pageBlood Request FlowchartirdinamarchsyaNo ratings yet
- Antibiotik Yg Ada D RSKD PDFDocument1 pageAntibiotik Yg Ada D RSKD PDFirdinamarchsyaNo ratings yet
- Blood Transfusion: Teoman SOYSAL Prof. MDDocument38 pagesBlood Transfusion: Teoman SOYSAL Prof. MDirdinamarchsyaNo ratings yet
- Uji Validasi Metode Tes Alat Hematologi Sysmex Xnl350Document1 pageUji Validasi Metode Tes Alat Hematologi Sysmex Xnl350irdinamarchsyaNo ratings yet
- Bland and Altman Plots in ExcelDocument7 pagesBland and Altman Plots in ExcelirdinamarchsyaNo ratings yet
- Malignant or Benign Leukocytosis: Tracy I. GeorgeDocument10 pagesMalignant or Benign Leukocytosis: Tracy I. GeorgeirdinamarchsyaNo ratings yet
- Hem Lect 12 ThalassemiaDocument48 pagesHem Lect 12 ThalassemiaKholisah MardiyahNo ratings yet
- Establishment of Reference Ranges For SPE in The Pediatric Population - A. FogliDocument1 pageEstablishment of Reference Ranges For SPE in The Pediatric Population - A. FogliirdinamarchsyaNo ratings yet
- BSBPMG522 assessment tasksDocument30 pagesBSBPMG522 assessment tasksPokemon Legend0% (1)
- Kumpulan Soal SynonymDocument10 pagesKumpulan Soal SynonymMuhammad Abi PrasetyoNo ratings yet
- A Enm 201401692Document6 pagesA Enm 201401692Bhabani Sankar SwainNo ratings yet
- Borang Pemarkahan RIMUP (Dazanak Tavantang)Document11 pagesBorang Pemarkahan RIMUP (Dazanak Tavantang)ELLYE ORNELLA SULIMAN MoeNo ratings yet
- Rufino Luna, Et - Al V CA, Et - Al (G.R. No. 100374-75)Document3 pagesRufino Luna, Et - Al V CA, Et - Al (G.R. No. 100374-75)Alainah ChuaNo ratings yet
- Tactical Baptism: Q. Is Major Benson Pain Correct and Justified To Use Waterboarding Against AbuDocument4 pagesTactical Baptism: Q. Is Major Benson Pain Correct and Justified To Use Waterboarding Against AbuLAW10101100% (2)
- Milk Borne Disease 2 (Eng) - 2012Document46 pagesMilk Borne Disease 2 (Eng) - 2012seviandha100% (1)
- Born 1925 EngDocument30 pagesBorn 1925 EngFranz SchindlerNo ratings yet
- Candombe para JoseDocument1 pageCandombe para JosestatuhominisNo ratings yet
- Purposive Communication - WK 3Document7 pagesPurposive Communication - WK 3Alexandre QuintoNo ratings yet
- Directions To Candidates Paper 1 - MedicalDocument29 pagesDirections To Candidates Paper 1 - MedicalMedicEdNo ratings yet
- What Is Dissociative Identity DisorderDocument3 pagesWhat Is Dissociative Identity DisorderShifaDhinaNo ratings yet
- Physical Education Curriculum MapDocument20 pagesPhysical Education Curriculum MapdyonaraNo ratings yet
- (GUIDE) MLBB Dictionary - General Discussion - Mobile Legends - Bang Bang - Mobile - Powered by Discuz!Document7 pages(GUIDE) MLBB Dictionary - General Discussion - Mobile Legends - Bang Bang - Mobile - Powered by Discuz!Jenny Lyn MahinayNo ratings yet
- Adjectives Interconversion of The Degrees of Comparison (Worksheet 3-) Rewrite Each Sentence Using The Other Two Degrees of ComparisonDocument2 pagesAdjectives Interconversion of The Degrees of Comparison (Worksheet 3-) Rewrite Each Sentence Using The Other Two Degrees of ComparisonJeanNo ratings yet
- Sarah Lowthian.: Hello My Name IsDocument3 pagesSarah Lowthian.: Hello My Name Isapi-225679366No ratings yet
- Annotated BibliographyDocument6 pagesAnnotated BibliographyAnonymous 9VRu3ImiEQNo ratings yet
- Review On Internal Combustion Engine Vibrations and MountingsDocument12 pagesReview On Internal Combustion Engine Vibrations and MountingsSanthosh KumarNo ratings yet
- Scada/Ems/Dms: Electric Utilities Networks & MarketsDocument12 pagesScada/Ems/Dms: Electric Utilities Networks & MarketsdoquocdangNo ratings yet
- ENGLSIH LISTENING SKILLS (Question Paper) PDFDocument2 pagesENGLSIH LISTENING SKILLS (Question Paper) PDFGagan H RNo ratings yet
- MATHS Revision DPP No 1Document8 pagesMATHS Revision DPP No 1ashutoshNo ratings yet