Professional Documents
Culture Documents
Feig 2020
Uploaded by
Mazen BarhoushCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Feig 2020
Uploaded by
Mazen BarhoushCopyright:
Available Formats
Articles
Metformin in women with type 2 diabetes in pregnancy
(MiTy): a multicentre, international, randomised, placebo-
controlled trial
Denice S Feig, Lois E Donovan, Bernard Zinman, J Johanna Sanchez, Elizabeth Asztalos, Edmond A Ryan, I George Fantus, Eileen Hutton,
Anthony B Armson, Lorraine L Lipscombe, David Simmons, Jon F R Barrett, Paul J Karanicolas, Siobhan Tobin, H David McIntyre, Simon Yu Tian,
George Tomlinson, Kellie E Murphy, on behalf of the MiTy Collaborative Group*
Summary
Lancet Diabetes Endocrinol Background Although metformin is increasingly being used in women with type 2 diabetes during pregnancy, little
2020; 8: 834–44 data exist on the benefits and harms of metformin use on pregnancy outcomes in these women. We aimed to
This online publication has investigate the effects of the addition of metformin to a standard regimen of insulin on neonatal morbidity and
been corrected. The corrected
mortality in pregnant women with type 2 diabetes.
version first appeared at
thelancet.com/diabetes-
endocrinology on Methods In this prospective, multicentre, international, randomised, parallel, double-masked, placebo-controlled trial,
October 13, 2020 women with type 2 diabetes during pregnancy were randomly assigned from 25 centres in Canada and four in Australia
See Comment page 802 to receive either metformin 1000 mg twice daily or placebo, added to insulin. Randomisation was done via a web-based
*A list of collaborators in the computerised randomisation service and stratified by centre and pre-pregnancy BMI (<30 kg/m² or ≥30 kg/m²) in a
MiTy trial is provided in the ratio of 1:1 using random block sizes of 4 and 6. Women were eligible if they had type 2 diabetes, were on insulin, had
appendix (pp 4–10) a singleton viable pregnancy, and were between 6 and 22 weeks plus 6 days’ gestation. Participants were asked to check
Department of Medicine, their fasting blood glucose level before the first meal of the day, before the last meal of the day, and 2 h after each meal.
University of Toronto, Toronto,
Insulin doses were adjusted aiming for identical glucose targets (fasting glucose <5·3 mmol/L [95 mg/dL], 2-h
ON, Canada (Prof D S Feig MD,
B Zinman MD, postprandial glucose <6·7 mmol/L [120 mg/dL]). Study visits were done monthly and patients were seen every
I George Fantus MD, 1–4 weeks as was needed for standard clinical care. At study visits blood pressure and bodyweight were measured;
L L Lipscombe MD, patients were asked about tolerance to their pills, any hospitalisations, insulin doses, and severe hypoglycaemia events;
G Tomlinson PhD,
K E Murphy MD); Lunenfeld-
and glucometer readings were downloaded to the central coordinating centre. Participants, caregivers, and outcome
Tanenbaum Research Institute, assessors were masked to the intervention. The primary outcome was a composite of fetal and neonatal outcomes, for
Toronto, ON, Canada which we calculated the relative risk and 95% CI between groups, stratifying by site and BMI using a log-binomial
(Prof D S Feig, B Zinman, I George regression model with an intention-to-treat analysis. Secondary outcomes included several relevant maternal and
Fantus, K E Murphy); Sinai Health
System, Mount Sinai Hospital,
neonatal outcomes. The trial was registered with ClinicalTrials.gov, NCT01353391.
Toronto, ON, Canada (Prof D S
Feig, B Zinman, I George Fantus, Findings Between May 25, 2011, and Oct 11, 2018, we randomly assigned 502 women, 253 (50%) to metformin and
K E Murphy); Cumming School 249 (50%) to placebo. Complete data were available for 233 (92%) participants in the metformin group and 240 (96%) in
of Medicine, Department of
Medicine, Department of
the placebo group for the primary outcome. We found no significant difference in the primary composite neonatal
Obstetrics and Gynecology, outcome between the two groups (40% vs 40%; p=0·86; relative risk [RR] 1·02 [0·83 to 1·26]). Compared with women in
University of Calgary, Calgary, the placebo group, metformin-treated women achieved better glycaemic control (HbA1c at 34 weeks’ gestation
AB, Canada (L E Donovan MD); 41·0 mmol/mol [SD 8·5] vs 43·2 mmol/mol [–10]; 5·90% vs 6·10%; p=0·015; mean glucose 6·05 [0·93] mmol/L vs
Alberta Children’s Hospital
Research Institute, Calgary, AB,
6·27 [0·90] mmol/L; difference –0·2 [–0·4 to 0·0]), required less insulin (1·1 units per kg per day vs 1·5 units per kg per
Canada (L E Donovan); day; difference –0·4 [95% CI –0·5 to –0·2]; p<0·0001), gained less weight (7·2 kg vs 9·0 kg; difference –1·8 [–2·7 to –0·9];
Sunnybrook Research Institute, p<0·0001) and had fewer caesarean births (125 [53%] of 234 in the metformin group vs 148 [63%] of 236 in the placebo
Toronto, ON, Canada group; relative risk [RR] 0·85 [95% CI 0·73 to 0·99]; p=0·031). We found no significant difference between the groups in
(J Johanna Sanchez PhD,
J F R Barrett MD,
hypertensive disorders (55 [23%] in the metformin group vs 56 [23%] in the placebo group; p=0·93; RR 0·99 [0·72 to 1·35]).
P J Karanicolas MD, S Tobin HBSc, Compared with those in the placebo group, metformin-exposed infants weighed less (mean birthweight 3156 g [SD 742]
S Y Tian PhD); Sunnybrook vs 3375 g [742]; difference –218 [–353 to –82]; p=0·002), fewer were above the 97th centile for birthweight (20 [9%] in the
Health Sciences Centre,
metformin group vs 34 [15%] in the placebo group; RR 0·58 [0·34 to 0·97]; p=0·041), fewer weighed 4000 g or more at
Toronto, ON, Canada
(E Asztalos MD, J F R Barrett, birth (28 [12%] in the metformin group vs 44 [19%] in the placebo group; RR 0·65 [0·43 to 0·99]; p=0·046), and
P J Karanicolas); University of metformin-exposed infants had reduced adiposity measures (mean sum of skinfolds 16·0 mm [SD 5·0] vs 17·4 [6·2]
Alberta, Edmonton, AB, Canada mm; difference –1·41 [–2·6 to –0·2]; p=0·024; mean neonatal fat mass 13·2 [SD 6·2] vs 14·6 [5·0]; p=0·017). 30 (13%)
(E A Ryan MD); McMaster
infants in the metformin group and 15 (7%) in the placebo group were small for gestational age (RR 1·96 [1·10 to 3·64];
University Hamilton, ON,
Canada (E Hutton PhD); p=0·026). We found no significant difference in the cord c-peptide between groups (673 pmol/L [435] in the metformin
Dalhousie University, Halifax, group vs 758 pmol/L [595] in the placebo group; p=0·10; ratio of means 0·88 [0·72 to 1·02]). The most common adverse
NS, Canada (A B Armson MD); event reported was gastrointestinal (38 [27%] events in the metformin group and 38 [22%] events in the placebo group).
Women’s College Hospital,
Toronto, ON, Canada
(L L Lipscombe); Western Sydney Interpretation We found several maternal glycaemic and neonatal adiposity benefits in the metformin group. Along
University, Sydney, NSW with reduced maternal weight gain, insulin dosage, and rate of caesarean sections, and improved glyacaemic
834 www.thelancet.com/diabetes-endocrinology Vol 8 October 2020
Articles
control, the lower adiposity and infant size measurements resulted in fewer large infants but a higher proportion of Australia (D Simmons MD);
small-for-gestational-age infants. Understanding the implications of these effects on infants will be important to Mater Research, University of
Queensland, South Brisbane,
properly advise patients who are contemplating the use of metformin during pregnancy. QLD, Australia
(H D McIntyre MD); Department
Funding Canadian Institutes of Health Research, Lunenfeld-Tanenbaum Research Institute, University of Toronto. of Medicine, University Health
Network, Toronto, ON, Canada
(G Tomlinson); and Department
Copyright © 2020 Elsevier Ltd. All rights reserved. of Obstetrics and Gynecology,
University of Toronto, Toronto,
Introduction Metformin is a biguanide, which is commonly used as ON, Canada (K E Murphy)
In the past 20 years, the prevalence of type 2 diabetes in first-line therapy in the management of type 2 diabetes, Correspondence to:
pregnancy has more than doubled,1 driven primarily by a but the drug’s role during pregnancy remains Professor Denice S Feig,
Mount Sinai Hospital, Toronto,
younger age of onset2 and by an increasing prevalence of controversial.6 Potential theoretical benefits include ON, M5T 3L9, Canada
maternal obesity.3 Pregnant women with type 2 diabetes reduction in glucose and insulin resistance, lowered d.feig@utoronto.ca
are often from Black, Hispanic, Asian, and Indigenous insulin requirements, and reduced maternal weight gain. See Online for appendix
ethnic groups; typically have overweight or obesity; and Metformin crosses the placenta7 and might also lower
are often economically disadvantaged.4 Pregnant women glucose and insulin resistance in the fetus, leading to
with type 2 diabetes are at high risk for adverse pregnancy reductions in the number of infants who are large for
outcomes including increased rates of pre-eclampsia and gestational age and other fetal morbidities, such as
caesarean section in mothers, and congenital anomalies, neonatal hypoglycaemia8 and respiratory distress
perinatal mortality, preterm birth, being large for syndrome, and pregnancy loss. However, because fetal
gestational age, and neonatal intensive care unit (NICU) metformin concentrations are similar or higher than
admissions in infants,1,4 and achieving optimal glucose those in the mother,7 potential safety concerns exist. Some
control is challenging.4 These women often require high studies of women with gestational diabetes have found
insulin doses,5 which are uncom fortable, costly, and increased overweight or obesity in metformin-exposed
associated with increased gestational weight gain, which children.9 Pregnant women with type 2 diabetes are
might further contribute to large-for-gestational-age increasingly prescribed metformin despite insufficient
infants and increased perinatal morbidity.3 Thus, an knowledge of the drug’s short-term and long-term effects.10
urgent unmet need exists to identify the optimal Five small studies of metformin use in women with
management for this at-risk population. type 2 diabetes in pregnancy have been reported,11–15 with
Research in context
Evidence before this study mortality and serious morbidity. However, compared with those
We searched MEDLINE for articles published before in the placebo group, metformin-treated women and their
March 7, 2020, with no language restrictions. We used the infants had several benefits, including better glycaemic control,
search terms “diabetes mellitus or diabetes” AND, “pregnancy” lower insulin requirements, less gestational weight gain, and
OR “pregnancy in diabetics”, AND “metformin” AND fewer caesarean births. Compared with those in the placebo
“randomized controlled trial”. We identified five small studies, group, infants of mothers taking metformin weighed an average
two of which examined neonatal outcomes. One study showed of 210 g less, were less likely to be extremely large for gestational
reduced maternal hypoglycaemia, neonatal hypoglycaemia, age and to weigh 4000 g or more at birth, and had reduced
and neonatal intensive care unit (NICU) admissions in the adiposity measures. More infants were, however, small for
metformin group, and the other showed reduced pregnancy- gestational age in the metformin group than in the placebo
induced hypertension, gestational weight gain, neonatal group.
hypoglycaemia, and NICU admissions. However, these studies
Implications of all the available evidence
were limited by methodological issues, including small sample
Although we found no significant difference in a composite of
sizes, insufficient appropriate allocation assignment, masking,
serious neonatal outcomes in women with type 2 diabetes
and intention-to-treat analysis. Thus, little evidence exists to
treated with metformin or placebo added to insulin, secondary
guide clinicians on the use of metformin as an adjunct to insulin
analysis showed several maternal glycaemic and neonatal
in women with type 2 diabetes in pregnancy.
adiposity benefits in the metformin group. The lower adiposity
Added value of this study and infant size measurements resulted in fewer large infants
To our knowledge, this is the first large, adequately powered, but a higher proportion of small-for-gestational-age infants.
multicentre, international, double-masked, placebo-controlled Understanding the implications of these effects on infants will
trial in women with type 2 diabetes during pregnancy, randomly be important to properly advise women who are
assigned to the addition of metformin or placebo to their contemplating the use of metformin during pregnancy.
standard regimen of insulin. We found no significant difference Longer term surveillance of these infants is essential to
between groups in the primary composite outcome of neonatal investigate the significance of these findings.
www.thelancet.com/diabetes-endocrinology Vol 8 October 2020 835
Articles
two reporting neonatal outcomes.11,12 One study showed ultrasound. Women were initially included from
reduced maternal hypoglycaemia, neonatal hypoglycaemia, 12 weeks’ gestation; however, after the first three recruits
and NICU admissions in the metformin group,11 and the the inclusion criteria were expanded to allow entry from
other showed reduced pregnancy-induced hypertension, 6 weeks because we hypothesised that longer and earlier
gestational weight gain, neonatal hypoglycaemia, and duration of treatment might be beneficial. Women were
NICU admissions.12 These studies were limited by excluded if they had type 1 diabetes, known intolerance
methodological issues, including small sample sizes and or contraindications to metformin, or if they had
insufficient appropriate allocation assignment, masking, previously participated in MiTy (appendix p 11).
and intention-to-treat analysis. Thus, little evidence exists Participants were recruited when visiting their
to guide clinicians on the use of metformin as an adjunct endocrinologist or obstetrician at their hospital clinic.
to insulin in women with type 2 diabetes in pregnancy. In patients taking metformin before entering the study,
The aim of the Metformin in Women with Type 2 the metformin was stopped before randomisation.
Diabetes in Pregnancy (MiTy) trial was to investigate Participants gave written informed consent.
whether the addition of metformin to a standard regimen The protocol has been previously published.17
of insulin, would increase or decrease the risk of neonatal Participating sites and collaborators are provided in the
morbidity and mortality in pregnant women with type 2 appendix (pp 4–10). The protocol, written by the principal
diabetes. investigator (DSF), was approved by the steering
committee, the Mount Sinai Hospital Ethics Review Board
Methods (NSP 104011), and by research ethics boards at each site.
Study design and participants Metformin use in MiTy was approved by Health
The MiTy trial was a multicentre, international, placebo- Canada. The trial was overseen by a steering committee
controlled, double-masked, randomised trial involving and done in accordance with the Declaration of Helsinki.
29 hospital centres, 25 in Canada and four in Australia.
Eligible centres had to be able to provide care to women Randomisation and masking
with type 2 diabetes during pregnancy, offer care to Women were randomly assigned to receive either
infants who required admission to the NICU, and verify metformin or placebo in addition to a standard regimen of
that all components of the trial could be completed. insulin, which usually included short-acting insulin before
Women were eligible if they were aged 18–45 years, meals and long-acting insulin before bed. Participants,
diagnosed with type 2 diabetes before pregnancy or caregivers, and outcome assessors were masked to the
before 20 weeks’ gestation (with at least two of the assignment. Randomisation was done at Sunnybrook
following: fasting glucose ≥7·0 mmol/L [126 mg/dL], Research Institute, Toronto, ON, Canada, via a web-based
≥11·1 mmol/L [≥200 mg/dL] on a 2-h 75 g oral glucose computerised randomisation service and stratified by
tolerance test, or HbA1c ≥48 mmol/mol [≥6·5%]),16 centre and pre-pregnancy body mass index (BMI; <30 or
receiving insulin, and had a live singleton fetus between ≥30 kg/m²). Within strata, allocation was assigned in a
6 and 22 weeks plus 6 days’ gestation confirmed by ratio of 1:1 using random block sizes of 4 and 6.
Procedures
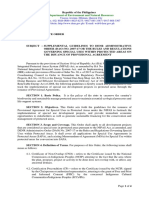
502 women randomly assigned
Both groups were asked to check their fasting blood
glucose level before the first meal of the day, before the
last meal of the day, and 2 h after each meal. Insulin doses
253 allocated to metformin 249 allocated to placebo were adjusted aiming for identical glucose targets (fasting
glucose <5·3 mmol/L [95 mg/dL], 2 h postprandial
glucose <6·7 mmol/L [120 mg/dL]). Study visits were
9 withdrew participation* 5 withdrew participation†
4 lost to follow-up 2 lost to follow-up monthly for the remainder of the pregnancy. Patients
7 missing data 2 missing data were seen every 1–4 weeks as was needed for standard
clinical care. At study visits, blood pressure and bodyweight
233 with complete data for the primary 240 with complete data for the were measured; patients were asked about tolerance to
outcome primary outcome their pills, any hospitalisations, insulin doses, and severe
hypoglycaemia events; and glucometer readings were
253 included in primary analysis using 249 included in primary analysis downloaded to the central coordinating centre. Pill counts
multiple imputation using multiple imputation were done with each change of pill bottle to assess
compliance.
Figure 1: Trial profile To maintain masking and limit the number and
*Reasons included family issues (n=2); patient moved outside of study area (n=1); intervention intolerance or
severity of side-effects, metformin (500 mg) and placebo
gastrointestinal side effects and decided to withdraw (n=1); did not want team to access medical records (n=3); not
interested, bad timing, or overwhelmed (n=1); and discontinued intervention and decided to withdraw (n=1). pills were gradually increased over 2 weeks to a final dose
†Reasons included intervention intolerance or gastrointestinal side effects and decided to withdraw (n=2); not of two pills, twice daily (appendix p 33). The placebo pill
interested, bad timing, overwhelmed (n=2); and discontinued intervention and decided to withdraw (n=1). was identical in appearance, taste, and consistency to
836 www.thelancet.com/diabetes-endocrinology Vol 8 October 2020
Articles
Metformin Placebo Metformin Placebo
(n=253) (n=249) (n=253) (n=249)
Maternal age at randomisation, 34·7 (5·0) 35·0 (4·6) (Continued from previous column)
years
Self-reported ever smoker 29 (12%) 27 (11%)
Age range, years 19·1–44·4 19·4–44·9
Insulin dose at randomisation, 0·64 (0·51); 0·68 (0·51);
Ethnicity kg per day 0·53 (0·24–0·83) 0·57 (0·26–0·90)
European 77 (30%) 75 (30%) Presence of diabetes complications
Non-European 176 (70%) 174 (70%) Retinopathy†† 5 (2·0%) 8 (3·2%)
Aboriginal 18 (7%) 17 (7%) Nephropathy 11 (4·3%) 19 (7·6%)
African or Caribbean origin 40 (16%) 36 (15%) Hypertension‡‡ 45 (17·8%) 48 (19·3%)
East Asian origin 26 (10%) 30 (12%) Chronic hypertension 44 (17·4%) 48 (19·3%)
Hispanic origin 5 (2%) 7 (3%) Blood pressure§§
Middle Eastern origin 14 (6%) 10 (4%) Systolic (mm Hg) 119·2 (13·3) 118·8 (13·5)
Pacific Islands origin 3 (1%) 3 (1%) Diastolic (mm Hg) 72·3 (9·4) 73·0 (9·3)
South Asian 32 (13%) 48 (19%) Metformin used before 170 (67%) 171 (69%)
Multi-ethnic 14 (6%) 10 (4%) pregnancy within past
12 months
Other 18 (7%) 11 (4%)
Metformin used during first 160 (63%) 148 (59%)
Unknown 6 (2%) 2 (<1%)
trimester
Previous pregnancies* 197 (78%) 199 (80%)
Data are mean (SD), n (%), or median (IQR). *In the metformin group 171 (68%)
Gestational age at 16·5 (4·0) 16·4 (3·8)
women had 1–4 previous pregnancies and 26 (10%) women had >4 previous
randomisation, weeks
pregnancies. In the placebo group 168 (68%) women had 1–4 previous
Pre-pregnancy weight, kg† 90·5 (21·3) 90·0 (21·9) pregnancies and 31 (12%) women had >4 previous pregnancies. †One (<1%)
Pre-pregnancy BMI, kg/m² 33·5 (7·1) 33·8 (7·4) participant was missing data in the metformin group and three (1%) were missing
data in the placebo group; pre-pregnancy weight was self-reported. ‡Seven (3%)
Weight at randomisation, kg 94·4 (21·4) 93·5 (21·8)
participants were missing data in the metformin group and six (2%) were missing
BMI at randomisation, kg/m² 35·0 (7·1) 35·2 (7·2) data in the placebo group. §48 (19%) participants were missing data in the
BMI at randomisation 194 (77%) 190 (76%) metformin group and 45 (18%) were missing data in the placebo group.
≥30 kg/m² ¶Met any of the following criteria: immigrated to Canada or Australia within
5 years of study entry, marital status was single, or highest attained education
Diagnosis of type 2 diabetes 209 (83%) 225 (90%)
was secondary school or less. ||Two (<1%) participants were missing data in the
before pregnancy
metformin group. **Comprised smoking during pregnancy, alcohol consumption
Family history of type 2 diabetes 205 (81%) 211 (85%) during pregnancy, or recreational drug use during pregnancy. ††One (<1%)
Polycystic ovary syndrome 43 (17%) 45 (18%) participant in the metformin group listed retinopathy but did not indicate type.
‡‡One (<1%) participant in the metformin group developed gestational
First HbA1C during this 55 (17) 56 (20)
hypertension before randomisation.§§12 (5%) participants were missing data in
pregnancy, mmol/mol‡
the metformin group and ten (4%) were missing data in the placebo group.
First HbA1C during this 7·1 (1·6) 7·3 (1·8)
pregnancy, % Table 1: Baseline characteristics
HbA1C concentration at 47 (13) 47 (13)
randomisation, mmol/mol§
HbA1C concentration at 6·42 (1·23) 6·41 (1·16)
components of the primary composite outcome were
randomisation, %
centrally adjudicated except for preterm birth, which was
Low socioeconomic status 109 (43%) 108 (43%)
composite¶ calculated from the estimated due date.
Immigrated to current country|| 115/251 (46%) 117 (47%) Secondary maternal outcomes included glycaemic
Immigrated within past 5 years 33/251 (13%) 31 (12%) control, hypertensive disorders, caesarean section,
Self-reported risky behaviours** 45 (18%) 38 (15%) gestational weight gain, and insulin dose. Glycaemic
(Table 1 continues in next column)
control was assessed by HbA1c and capillary glucose
measures (appendix p 20).
Key secondary neonatal outcomes included individual
metformin. Women were asked to take the pills for the outcomes in the composite, birthweight measures
duration of the pregnancy. (large for gestational age [birthweight >90th percentile],
extreme large for gestational age (birthweight
Outcomes >97th percentile), small for gestational age [birthweight
The primary outcome was a composite of fetal and <10th percentile]) using Canadian national growth
neonatal outcomes including one or more of the curves adjusted for sex and gestational age,18 birthweight
following: pregnancy loss (miscarriage, termination, (≥4000 g), cord blood C-peptide, neonatal adiposity
stillbirth, or neonatal death up to 28 days), preterm birth outcomes (fat mass, calculated using the mathematical
(<37 weeks’ gestation), birth injury, moderate or severe model proposed by Catalano and colleagues,19 which
respiratory distress syndrome, neonatal hypoglycaemia, includes birthweight, length, and flank skin fold; and
and NICU admission lasting >24 h; appendix p 34). All skinfold thicknesses), gestational age at birth, and
www.thelancet.com/diabetes-endocrinology Vol 8 October 2020 837
Articles
length of infant hospital stay (appendix p 35). As part of dispersion) were generated within treatment group. For
a sensitivity analysis we calculated customised birth the primary composite neonatal outcome, we calculated
weight centiles using Gestational Related Optimal the relative risk and 95% CI between groups, stratifying by
Weight (appendix p 29).20 site and BMI using a log-binomial regression model. Any
variables with potential imbalances between groups were
Statistical analysis added in a sensitivity analysis; this criterion led to one
Using a population-based Canadian perinatal database,21 such analysis on the timing of the diabetes diagnosis. We
we calculated that we could expect participants to have an also included an additional analysis assessing the variation
absolute risk of 50% for the primary composite outcome. in the treatment effect with gestational age at first
To have 80% power to detect a 25% relative risk (RR) exposure to drug. An intention-to-treat analysis was used,
reduction (12·5% absolute reduction), at a two-sided with a plan to use logistic regression in a multiple
significance level of 5%, we calculated that we would imputation procedure for the primary outcome if the
need 492 participants, and accounting for loss to follow- outcome was missing in more than 5% of infants, which
up we aimed for 500 participants. could happen if a woman withdrew or was lost to follow-
For baseline covariates, appropriate summary statistics up or if components of the composite outcome were
(means, medians, percentages, and measures of missing for an infant whose observed components did not
satisfy the composite outcome criteria. In this case we also
Metformin Placebo p value Effect size (95% CI) planned to do a complete case analysis in which the data
(n=240) (n=242) that were available would be used for analysis of the
Composite primary outcome* 94/233 (40%) 95/240 (40%) 0·86 RR 1·02 (0·83 to 1·26) composite outcome without imputation. We also planned
Pregnancy loss† 13/227 (6%) 14/236 (6%) 0·81 RR 0·96 (0·46 to 2·01) that in the best-case scenario all missing values would be
Spontaneous abortion or 4 (2%) 4 (2%) 0·97 RR 0·98 (0·25 to 3·79) replaced with negative results for the composite outcome
miscarriage and in the worst-case scenario all missing values would be
Stillbirth (≥20 weeks 2 (<1%) 7 (3%) 0·11 RR 0·28 (0·06 to 1·32) replaced with a positive result for the composite outcome.
gestation)‡ Continuous secondary outcomes were compared using
Termination 2 (<1%) 2 (<1%) 0·84 RR 0·82 (0·12 to 5·5) ANOVA with treatment group and baseline BMI group as
Neonatal death <28 days§ 5/227 (2%) 1/236 (<1%) 0·14 RR 4·96 categorical variables. For binary outcomes, analyses of the
(0·61 to 40·63) secondary outcomes were also adjusted for BMI group
Livebirths 232 229 ·· ·· and site if the number of events was greater than 50. For
Preterm birth <37 weeks 60 (26%) 47 (21%) 0·16 RR 1·27 (0·91 to 1·77) 20–50 events, only BMI group was included and for fewer
Birth injury¶ 1/231 (<1%) 3/228 (1%) 0·37 RR 0·36 (0·04 to 3·36) than 20 events, simple two-group comparisons were
Respiratory distress 11/231 (5%) 8/228 (4%) 0·49 RR 1·36 (0·56 to 3·29) used. For secondary binary events a log-binomial
syndrome¶
regression was used unless outcomes were rare outcomes,
Neonatal hypoglycaemia¶ 27/231 (12%) 34/228 (15%) 0·41 RR 0·82 (0·52 to 1·30)
in which case we used Fisher’s exact test. When possible,
NICU admission >24 h¶ 51/231 (22%) 46/228 (20%) 0·56 RR 1·10 (0·79 to 1·53)
a baseline value for the follow-up variable (eg, HbA1c) was
Gestational age at birth, weeks 37·5 (2·2) 37·6 (2·0) 0·33 Difference –0·2
(–0·6 to 0·2)
added to the model. Two pre-specified subgroup analyses
assessed a differential response to treatment according to
Birthweight, g 3156 (742) 3375 (742) 0·0016 Difference –0·44
(–0·70 to –0·18) whether (1) BMI at randomisation was lower than 30 kg/m²
Birthweight Z score –0·01 (1·47) 0·45 (1·40) 0·0009 Difference –0·28 or 30 kg/m² or more, and (2) start of treatment was at less
(–0·45 to –0·10) than 16 or 16 weeks’ or more gestation. A pre-specified
Large for gestational age, 50 (22%) 66 (29%) 0·067 RR 0·74 (0·54 to 1·02) per-protocol analysis was done excluding women who
>90th centile (adjudicated discontinued medication, withdrew, or had no medication
using Kramer23)
information. We used R (version 3.6.3) for the analysis. A
Extreme large for gestational 20 (9%) 34 (15%) 0·041 RR 0·58 (0·34 to 0·97)
age, >97th centile (using
data safety monitoring board oversaw the trial.
Kramer23) The trial was registered with ClinicalTrials.gov,
Birthweight ≥4000 g 28 (12%) 44 (19%) 0·046 RR 0·65 (0·43 to 0·99) NCT01353391.
Small for gestational age, 30 (13%) 15/228 (7%) 0·026 RR 1·96 (1·10 to 3·64)
<10th centile (using Role of the funding source
Kramer23)|| The funders of the study had no role in study design, data
Sum of skinfolds, mm** 16·0 (5·0) 17·4 (6·2) 0·024 Difference –1·4 collection, data analysis, data interpretation, or writing of
(–2·6 to –0·2)
the manuscript. The corresponding author had full access
Neonatal body fat mass††24 13·2 (6·2) 14·6 (5·0) 0·017 Difference –1·5
(–2·7 to –0·3)
to all the data in the study and had final responsibility for
Cord blood C-peptide 673 (435); 758 (595); 0·10 Ratio of means 0·88
the decision to submit for publication.
(pmol/L)‡‡ 569 (360–901) 626 (433–878) (0·72 to 1·02)
Shoulder dystocia 4 (2%) 4 (2%) 1·0 RR 0·96 (0·25 to 3·69) Results
(Table 2 continues on next page) Between May 25, 2011, and Oct 11, 2018, we randomly
assigned 502 women to either metformin (n=253 [50%])
838 www.thelancet.com/diabetes-endocrinology Vol 8 October 2020
Articles
or placebo (n=249 [50%]). 233 (92%) women in the
Metformin Placebo p value Effect size (95% CI)
metformin group and 240 (96%) women in the placebo (n=240) (n=242)
group were available for the primary outcome (figure 1).
(Continued from previous page)
The last woman gave birth on April 24, 2019, and outcome
Hyperbilirubinaemia§§ 51/227 (23%) 37/227 (16%) 0·06 RR 1·43 (0·99 to 2·07)
collection was completed on June 5, 2019.
Overall, baseline characteristics were well balanced
Congenital anomaly§§ 7/227 (3%) 13/227 (6%) 0·16 RR 0·52 (0·22 to 1·28)
(table 1; appendix pp 13, 14). The mean age of
Length of hospital stay until 5·6 (7·4) 5·5 (8·1) 0·51 Difference –0·3
participants was 35 years, and 194 (77%) women in the first discharge home, days¶¶ (–1·4 to 0·7)
metformin group and 190 (76%) in the placebo group
Data are n (%), mean (SD), or median (IQR), unless otherwise indicated. All analyses were intention to treat. Analysis of
had obesity, and 176 (70%) in the metformin group and the primary composite outcome was adjusted for BMI group assessed at time of randomisation and site. Analyses of the
174 (70%) in the placebo group identified as non- secondary outcomes were also adjusted for BMI group and site if outcomes were continuous, or, for binary outcomes, if
European (table 1). 109 (43%) in the metformin group the number of events was greater than 50. For 20–50 events, only BMI group was included and for <20 events, simple
two-group comparisons were used. RR=risk ratio. NICU=neonatal intensive care unit. BMI=body mass index.
and 108 (43%) in the placebo group were considered *Composite primary outcome: pregnancy loss (miscarriage, termination, stillbirth, or neonatal death), preterm birth,
socioeconomically disadvantaged, defined as having birth injury, respiratory distress, neonatal hypoglycaemia, or NICU lasting >24 h. Seven (3%) participants in the
either immigrated within 5 years of study entry, being metformin group and two (<1%) in the placebo group were missing data. †Early and late pregnancy loss and neonatal
death (spontaneous abortion or miscarriage, termination, stillbirth, or neonatal death). The 28-day neonatal death
single, or having a highest educational attainment of
form was missing for 13 (5%) participants in the metformin group and six (3%) in the placebo group. ‡Reasons for
secondary school or less. Although these criteria are not stillbirths were two unknown in the metformin group; and one intrauterine fetal death, one ketoacidosis in mother, one
validated measures of socioeconomic disadvantage, twisted umbilical cord, one preterm premature rupture of membranes, one spontaneous rupture of membranes, one
each measure by itself has been associated with low severe oligohydramnios, and one cervical insufficiency in the placebo group. §Causes of death were four complications
of preterm birth and one severe intrauterine growth restriction + cardiac abnormalities in the metformin group;
socioeconomic status.22 64 (13%) of 500 women were one complications of preterm birth in the placebo group. ¶One (<1%) missing in the metformin group and
immigrants, with 33 (13%) of 251 in the metformin one (<1%) missing in the placebo group. ||One (<1%) gestational age at birth in the placebo group was 21 weeks and
group and 31 (12%) of 249 in the placebo group having 3 days, so Kramer could not be used to calculate small for gestational age, but based on weight, the baby was not large
for gestational age. **Triceps, subscapular, and supra-iliac skinfolds (n=156 infants in the metformin group and n=179
immigrated within the past 5 years. 160 (63%) in the placebo group). ††Included 155 infants in the metformin group and 180 infants in the placebo group. ‡‡143 cord
participants in the metformin group and 148 (59%) in blood serum samples in the metformin group and 142 cord blood serum samples in the placebo group were included in
the placebo group reported metformin use during the the analysis; estimated effect sizes and p values were calculated in the model using log-values then transformed
back to give ratio of means. §§Five (4%) participants in the metformin group and two (1%) in the placebo group were
first trimester (table 1).
missing data. ¶¶Nine (4%) participants in the metformin group and two (<1%) in the placebo group were missing data.
The median follow-up across livebirths and stillbirths
was 20·9 weeks (IQR 17·6–24·1). We found no difference Table 2: Neonatal outcomes
between the intervention groups in the proportion of
completed visits (appendix p 15); however, more women
in the metformin group than in the placebo group 41·0 mmol/mol [SD 8·5] vs 43·2 mmol/mol [SD –10];
reported that gastrointestinal intolerance was the cause 5·90% [SD 0·78] vs 6·10% [0·94]; p=0·015; table 3) and
of reducing the pill intake below four pills per day lower mean glucose (6·05 mmol/L [0·93] vs 6·27 mmol/L
(appendix p 17). Overall pill compliance (defined as total [0·90]; appendix p 20). We found more episodes per week
pills taken divided by the total that should have been of mild hypoglycaemia in the metformin group than in
taken, stopping at delivery or time of withdrawal and the placebo group. However, the number of women with
excluding patients who had no bottles returned) was mild hypoglycaemic episodes was similar between the
77% in both groups, with approximately 75% of women groups (appendix p 23). We found no difference in the
taking 70% or more of the study pills (appendix p 16). At number of severe hypoglycaemic episodes (appendix p 23).
6 weeks post partum, 127 (60%) women in the metformin Metformin-treated women required less insulin (total
group thought they had been on metformin in the trial, daily insulin dose by 34 weeks’ gestation), and total
and 77 (35%) in the placebo group thought they were on insulin dose as measured by units per kg per day was
metformin (appendix p 18). lower in the metformin group (table 3) than in the
Because 29 (6%) women were missing primary placebo group, as was the percentage of women taking
outcome data, the RR and risk difference of the primary 2 units per kg per day or more (appendix p 24).
outcome were estimated through multiple imputation Women in the metformin group gained less overall
(appendix p 12). We found no significant difference in weight and less weight per week than did women in the
the primary composite outcome between the metformin placebo group (table 3). Fewer women in the metformin
and placebo groups (table 2). In a sensitivity analysis, we group than in the placebo group had excessive
found no significant difference in the primary composite gestational weight gain according to the Institute of
outcome after adjustment for the timing of the diabetes Medicine (IOM) guidelines (appendix p 25).25 More
diagnosis (RR 0·98 [95% CI 0·79–1·21). Complete case women in the metformin group than in the placebo
data, and best-case or worst-case scenarios showed group gained weight below the IOM recommendations
similar results (appendix p 19). (appendix p 25).
By the end of pregnancy, women in the metformin Fewer women in the metformin group had caesarean
group achieved better glycaemic control than did those in sections than did those in the placebo group. We found
the placebo group (mean HbA1c at 34 weeks’ gestation no significant difference in hypertensive disorders
www.thelancet.com/diabetes-endocrinology Vol 8 October 2020 839
Articles
or hyperbilirubinaemia (table 2). Neonatal length of
Metformin Placebo p value Effect size (95% CI)
(n=240) (n=242) hospital stay was similar between the groups (table 2).
The distribution of birthweights was shifted downwards
Maternal weight gain, kg*
across the entire birthweight spectrum in those on
Overall weight gain 7·2 (5·3) 9·0 (4·7) <0·0001 Difference –1·8 metformin (figure 2). More infants in the metformin
(–2·7 to –0·9)
group were small for gestational age (13% vs 7%; RR 1·96
Weekly weight gain 0·4 (0·3) 0·5 (0·3) <0·0001 Difference –0·10
(–0·15 to –0·05) [95% CI 1·10–3·64]; p=0·03) using Canadian population
Last HbA1c concentration in 41·0 (8·5) 43·2 (–10) 0·015 Difference –0·18 charts18 (table 2) and customised centiles (appendix p 29).20
pregnancy, mmol/mol†‡ (–0·33 to –0·03); Intolerance to the study drug was not different between
difference –2·0 the groups when reporting adverse events (table 4).
(–3·6 to –0·3)
Fewer women reported serious adverse events in the
Last HbA1c concentration in 5·90% (0·78) 6·10% (0·94) 0·015 Difference –0·18 (–0·33
metformin group than in the placebo group, but the total
pregnancy, % to –0·03); difference
–2·0 (–3·6 to –0·3) number of serious maternal adverse events was not
Total insulin dose at 34 or 1·1 (1·0) 1·5 (1·1) <0·0001 Difference –0·4 significantly different between the groups (table 4).
36 weeks, units per kg per (–0·5 to –0·2) When examining total maternal adverse events, we
day§ found a similar number of events and a similar number
Total insulin dose at 34 or 109·8 (105·1) 155·3 (134·0) <0·0001 Difference –43·9 of women reporting events in both groups (table 4). We
36 weeks, units per day¶ (–61·5 to –26·2)
found a similar number of infant adverse and serious
Long-acting insulin at 42·8 (46·0) 55·7 (47·6) 0·004 Difference –12·7
34 or 36 weeks, units per (–21·4 to –4·0)
adverse events reported in both groups (table 4).
day|| In a pre-specified subgroup analysis of the primary
Short-acting insulin at 34 66·9 (75·1) 99·1 (108·8) <0·0001 Difference –32·0 outcome stratified by maternal BMI, we found no
or 36 weeks, units per (–49·7 to –14·4) significant variation in the treatment effect between
day** groups (ratio of RRs 1·0, 0·58–1·72; appendix p 32). In the
Caesarean section†† 125/234 (53%) 148/236 (63%) 0·031 RR 0·85 (0·73 to 0·99) subgroup analysis stratified by earlier (<16 weeks) and later
Primary caesarean section 65/125 (52%) 68/148 (46%) 0·32 RR 1·13 (0·89 to 1·44) randomisation, we found no between-group difference
Any hypertensive 55 (23%) 56 (23%) 0·93 RR 0·99 (0·72 to 1·35) (appendix p 32). The effect of metformin did not appear to
disorder‡‡
differ according to the gestational age at which a woman
Gestational hypertension 13 (5%) 15 (6%) 0·82 RR 0·92 (0·46 to 1·85)
entered the study (appendix p 36).
Worsening chronic 20/237 (8%) 22 (9%) 0·68 RR 0·89 (0·51 to 1·56)
hypertension during
The per-protocol analysis results were concordant
pregnancy§§ with the primary analysis for the primary outcome
Pre-eclampsia 37 (15%) 30 (12%) 0·29 RR 1·27 (0·82 to 1·97) (appendix p 30).
Data are mean (SD), n/N (%), or n (%), unless otherwise specified. All analyses were intention to treat. Analyses of the
secondary outcomes were adjusted for BMI group assessed at time of randomisation and site if outcomes were Discussion
continuous, or, for binary outcomes, if the number of events was greater than 50. For 20–50 events, only BMI group was We found no difference between women who received
included and for fewer than 20 events, simple two-group comparisons were used. BMI=body mass index. RR=risk ratio. metformin and those receiving placebo in a composite of
*Nine (4%) participants in the metformin group and four (2%) in the placebo group were missing data. Overall and
weekly weight gain was calculated from measured weight at randomisation. †227 (95%) of 240 participants in the neonatal morbidity and mortality. However, metformin-
metformin group and 235 (97%) of 242 in the placebo group. ‡After adjusting for baseline HbA1c at randomisation. treated women had better glycaemic control, lower
§208 (98%) of 212 participants in the metformin group and 211 (99%) of 213 in the placebo group. ¶211 (99%) of insulin requirements, less gestational weight gain, and
212 participants in the metformin group and 211 (99%) of 213 in the placebo group. ||212 (100%) of 212 participants in
the metformin group and 213 (100%) of 213 in the placebo group. **211 (99%) of 212 participants in the metformin
fewer caesarean births than women in the placebo group
group and 211 (99%) of 213 in the placebo group. ††234 (99%) of 236 participants based on available method of birth did. Infants of mothers taking metformin weighed less,
data. ‡‡Gestational hypertension, worsening chronic hypertension, or pre-eclampsia. §§Three (1%) participants were were less likely to be extremely large for gestational age,
missing data in the metformin group.
and less likely to weigh 4000 g or more at birth compared
Table 3: Maternal outcomes with infants born to mothers taking placebo. Additionally,
metformin-exposed infants displayed reduced adiposity
with reduced skinfold thicknesses, abdominal circum
(table 3), diabetes complications (appendix p 26), or ference, and fat mass. In keeping with lower adiposity
maternal length of hospital stay (appendix p 27). and infant size, we observed a higher proportion of
Birthweight was lower in the metformin group than babies who were small for gestational age in the
in the placebo group, with reduced extreme large for metformin group than in the placebo group.
gestational age and birthweight 4000 g or more (table 2). Notably, by contrast with some previous studies,11,12 we
We also found reductions in neonatal adiposity did not find a difference in serious neonatal outcomes
measures in the metformin group (skinfold thicknesses, when metformin was added to insulin. Given the far
abdominal circumference, and neonatal fat mass; greater statistical power and rigour of the MiTy trial
table 2; appendix p 28). compared with previous trials, this discrepancy is most
We found no difference in the components of the likely explained by previous studies having small sample
composite outcome between groups. We found no sizes, no masking, and excluding women already on
difference in gestational age at birth, shoulder dystocia, insulin.12 The many benefits observed in the metformin
840 www.thelancet.com/diabetes-endocrinology Vol 8 October 2020
Articles
group in our study, including improved glycaemic
Placebo
control and lower rates of very large infants, did not
translate into improvements in the composite outcome. 60
In a previously published randomised trial of women
with type 1 diabetes,26 we observed that improved
Number of infants
40
glycaemic control that was achieved through continuous
glucose monitoring led to a significant reduction in
large-for-gestational-age infants and serious neonatal 20
outcomes such as neonatal hypoglycaemia and NICU
admissions.26 The absence of similar congruence
between indices of infant size and serious neonatal 0
adverse outcomes in the MiTy trial might relate to the
Metformin
lower overall rate of large-for-gestational-age infants and
hyperglycaemia in women with type 2 diabetes. We did 60
not find a difference in stillbirth and perinatal mortality,
but the study did not have power to detect differences in
Number of infants
these rare outcomes, so conclusions should thus be 40
drawn with caution.
We found improved glycaemic control and lower insulin
20
requirements in the metformin group, with fewer women
requiring higher insulin doses than in the placebo group.
This finding is in agreement with a study23 of 390 patients 0
with insulin-treated type 2 diabetes outside of pregnancy, −4·0 −3·5 −3·0 −2·5 −2·0 −1·5 −1·0 −0·5 0·0 0·5 1·0 1·5 2·0 2·5 3·0 3·5 4·0
in which metformin use was associated with improved Birthweight Z score
glycaemic control and a reduced insulin dose of 7·5 units
Figure 2: Birthweight distributions in infants of women in the metformin and placebo groups
per day. In MiTy, women on metformin had a substantially
greater reduction of 45 units fewer insulin per day. Given
that almost half of participants were considered to have which can influence maternal weight gain and thus infant
low socioeconomic status, such a reduction in insulin size.3 Another possible mechanism might be a direct effect
dose could result in substantial cost savings improving of metformin on fetal growth.6 Metformin activates AMP
affordability for lower-income women with type 2 diabetes. kinase and leads to the inhibition of the mechanistic target
Women on metformin also gained less weight during of the rapamycin (mTOR) pathways, which are regulators
pregnancy than did those who received placebo, of placental amino acid transport.6 The inhibition of these
consistent with findings in previous trials in women and other growth differentiation pathways could contribute
with gestational diabetes.8 This finding might be due to to the attenuated fetal growth observed.
the reduced insulin requirements, or to direct effects of In addition to fewer large infants, we found more
metformin, which can cause anorexia and weight infants who were small for gestational age in the
reduction via increases in growth differentiation factor metformin group than in the placebo group. This finding
15 concentrations.24 Excess gestational weight gain is was reported in one previous study of women with type 2
associated with an increase in the risk of pre-eclampsia, diabetes12 and is important because infants who are small
large-for-gestational-age infants, and preterm birth, for gestational age might have an increased risk of
especially in women with obesity,3 and increases the risk perinatal complications27 and potential long-term con
of postpartum weight retention. In our study, in which sequences such as neurodevelopmental delay affecting
76% of women had obesity before pregnancy, this school performance,28 obesity, hypertension, diabetes,
finding represents an additional accrual of adipose and cardiovascular disease, similar to infants of mothers
tissue, further increasing the risk of long-term obesity. with under-nutrition.29 The distribution of birthweight
We found that infants of women in the metformin group was shifted downwards across the entire population of
had a lower birthweight, were less likely to be extremely metformin-exposed infants relative to the placebo group.
large, and had reduced adiposity compared with those Whether this increase in the number of small infants
born in the placebo group, which is consistent with represents smaller but healthy infants or pathologically
findings of previous studies in women with gestational growth-restricted infants is unclear. The underlying
diabetes.9 Several mechanisms might explain these cause of being born small for gestational age in the
findings. In our study, women who received metformin metformin-exposed infants is unknown. The increased
had better glycaemic control and less excess maternal number of small infants could be related to effects of
weight gain, both of which can lower the risk of being born metformin on mothers leading to reduced food intake.30
large for gestational age. Also, women on metformin This change could affect weight gain, glycaemic control,
required less insulin than did those in the placebo group, and nutrient supply. Inhibition of mTOR might
www.thelancet.com/diabetes-endocrinology Vol 8 October 2020 841
Articles
Metformin Placebo Effect size Metformin Placebo Effect size
(n=253) (n=249) (95% CI) (n=253) (n=249) (95% CI)
Women reporting 76 (30%) 87 (35%) Rate ratio (Continued from previous column)
adverse events 0·86 (0·67–1·11)
Total maternal serious 6 16 Rate ratio
Total maternal adverse 139 170 Rate ratio adverse events 0·41 (0·16–1·09)
events 0·83 (0·62–1·11)
Respiratory 0 1 (6%) ··
Gastrointestinal 38 (27%) 38 (22%) ··
Diabetic ketoacidosis 0 1 (6%) ··
Nausea or vomiting 15 (11%) 19 (11%) ··
Other 1 (17%) 0 ··
Allergies 2 (1%) 1 (<1%) ··
Obstetric 1 (17%) 3 (19%) ··
Cardiac 3 (2%) 5 (3%) ··
Hyperglycaemia 1 (17%) 2 (13%) ··
Dermatological 2 (1%) 4 (2%) ··
Gastrointestinal 0 1 (6%) ··
Gynaecological 1 (<1%) 2 (1%) ··
Cardiac 1 (17%) 3 (19%) ··
Haematological 3 (2%) 5 (3%) ··
Infections 0 1 (6%) ··
Headaches 6 (4%) 11 (7%) ··
Musculoskeletal 0 1 (6%) ··
Hyperglycaemia 0 2 (1%) ··
Renal 1 (17%) 1 (6%) ··
Infections 6 (4%) 7 (4%) ··
Nausea or vomiting 0 1 (6%) ··
Musculoskeletal 7 (5%) 9 (5%) ··
Vascular 1 (17%) 0 ··
Neurological 2 (1%) 4 (2%) ··
Psychological 0 1 (6%) ··
Obstetric 10 (7%) 6 (4%) ··
Infants with adverse 1 (<1%) 1 (<1%) ··
Other 0 2 (1%) ·· events
Otolaryngological 3 (2%) 3 (2%) ·· Total infant adverse 1 1 ··
Ophthalmological 1 (<1%) 0 ·· events
Pneumonia or lower 2 (1%) 1 (<1%) ·· Infants with serious 2 (<1%) 1 (<1%) ··
respiratory infection adverse events
Psychological 3 (2%) 0 ·· Total infant serious 2 1 ··
Renal 0 1 (<1%) ·· adverse events
Respiratory 28 (20%) 42 ·· Respiratory 1 (50%) 1 (100%) ··
Thyroid cancer 1 (<1%) 0 ·· Weight loss 1 (50%) 0 ··
Urinary tract infection 6 (4%) 8 (5%) ·· Data are n or n (%), unless otherwise indicated. RR=risk ratio.
Women reporting 5 (2%) 15 (6%) RR 0·33
Table 4: Adverse events
serious adverse events (0·11–0·83)
(Table 4 continues in next column)
understanding the relative implications of these findings
downregulate pathways involved with protein synthesis, is important to properly advise patients who are
cell growth, and proliferation.6 Metformin inhibits contemplating the use of metformin during pregnancy.
folate-related pathways, which could result in reduced Such effects on growth might have long-term conseq
cell growth and nutrient restriction.6 Metformin might uences. In a systematic review and meta-analysis of
also directly affect placental function and nutrient neonatal, infant, and childhood growth following
transfer and might have direct fetal effects affecting the metformin exposure, results showed that, when
fetal metabolic milieu, cell metabolism, and insulin compared with infants born to women using insulin
secretion.6 In our study, more women in the metformin with gestational diabetes, neonates born to mothers
group gained weight under that of the recommended using metformin exhibited lower birthweights, had a
guidelines, which might have played a role in the lower ponderal index, and were less likely to be large for
increased rate of infants who were small for gestational gestational age at birth.9,34 In infancy, the metformin-
age. As well, very tight glycaemic control (ie, lower mean exposed children were heavier, and by age 5–9 years
glucose of 4·8 mmol/L [86 mg/dL]) has resulted in small- they had an increased BMI compared with infants
for-gestational-age infants in some studies.31 However, in whose mothers were given insulin.9 This finding,
our study, glycaemic control in the metformin group was however, is based on a paucity of data and divergent
not exceptionally tight (mean glucose 6·1 mmol/L findings exist. For example, in one study the authors
[109 mg/dL]). In studies of non-diabetic women with suggested that the glycaemic milieu during pregnancy
obesity32 and women with polycystic ovary syndrome33 is crucial, with protective effects of metformin in infants
using metformin during pregnancy, no effect on exposed to poorer glycaemic control but deleterious
birthweight and no increase in the number of infants effects in infants whose mothers had tight glycaemic
born small for gestational age was found, suggesting a control during pregnancy.34 Further research is needed
direct effect of metformin on growth might be less likely to understand the long-term effects of metformin on
than an indirect effect. Regardless of the cause, children.
842 www.thelancet.com/diabetes-endocrinology Vol 8 October 2020
Articles
In addition to the randomised, double-masked, trial oversight. GT and SYT did the statistical analyses. All authors
placebo-controlled design, and low attrition, this trial had contributed to interpretation of the data. DSF wrote the first draft.
All authors reviewed and provided critical revisions to the manuscript.
several strengths. To our knowledge, this is the first large,
appropriately powered, and methodologically sound Declaration of interests
DSF reports grants from the Canadian Institutes of Health Research,
randomised trial of metformin versus placebo added to Lunenfeld-Tanenbaum Research Institute, and the University of Toronto
insulin in women with type 2 diabetes in pregnancy. The Department of Medicine; non-financial support from Apotex, Bayer
trial had adequate statistical power to detect important (Asencia), and Roche Diabetes Care; and personal fees from Medtronic
effects on the primary outcome and provided a precise and Novo Nordisk. IGF reports grants from the Canadian Institutes of
Health Research. PJK reports grants from the Canadian Institutes of
estimate of the treatment effect. The participants were Health Research. JJS reports grants from the Canadian Institutes of Health
from diverse ethnic and socioeconomic backgrounds, Research. ST reports grants from the Canadian Institutes of Health
making the results generalisable to pregnant women Research. All other authors declare no competing interests.
with type 2 diabetes. Pill compliance was good and data Data sharing
collection was almost complete, with almost all randomly The data are available from the corresponding author, upon providing a
assigned women and their neonates included in the detailed protocol for the proposed study, information about the funding
and resources you have to carry out the study, and approval by the MiTy
primary outcome analysis. The protocol had been Steering Committee.
previously published and statistical analyses pre-
Acknowledgments
specified. However, some limitations existed. The trial was funded by the Canadian Institutes of Health Research,
The trial took 9 years to complete and care practices the Lunenfeld-Tanenbaum Research Institute, Toronto, ON, Canada,
could have changed over the years. Given that this placebo- and the Department of Medicine, University of Toronto, Toronto, ON,
Canada. The study drugs, metformin and placebo, were provided by
controlled, randomised trial was randomly blocked,
Apotex, Toronto, ON, Canada, and Bayer (Asencia) and Roche Diabetes
changes in care are unlikely to have affected the outcome Care provided the glucometers and strips. We thank all the women with
of the trial. The results might not apply to women on type 2 diabetes who participated in the trial. We also acknowledge the
metformin alone. However, a trial by Ainuddin and invaluable support from the 29 diabetes research and clinical care teams
and the Clinical Trials Services research team at Sunnybrook Research
colleagues12 showed that most women with type 2 diabetes
Institute, Toronto, ON, Canada. We thank the data safety monitoring
needed insulin in addition to metformin, with only 15% on board for overseeing the trial: Kevin Thorpe, Lelia Duley, and
metformin alone. Although the results do not directly Michael Bracken. We would also like to acknowledge our steering
apply to women with gestational diabetes, those with committee member Arne Ohlsson for his very wise counsel and
dedication to the trial. Arne Ohlsson unfortunately passed away before the
gestational diabetes and marked hyperglycaemia who are
writing of this manuscript. We are indebted to him for his important
diagnosed early in pregnancy might more closely resemble contributions and support for this trial.
our study population, and thus be affected by these References
findings. Finally, clearance of metformin is increased in 1 Feig DS, Hwee J, Shah BR, Booth GL, Bierman AS, Lipscombe LL.
pregnancy and a more marked effect on outcomes might Trends in incidence of diabetes in pregnancy and serious perinatal
outcomes: a large, population-based study in Ontario, Canada,
have been seen with a higher dose of metformin. 1996–2010. Diabetes Care 2014; 37: 1590–96.
In summary, although we found no significant difference 2 Lascar N, Brown J, Pattison H, Barnett AH, Bailey CJ, Bellary S.
in the primary composite outcome of serious neonatal Type 2 diabetes in adolescents and young adults.
Lancet Diabetes Endocrinol 2018; 6: 69–80.
outcomes in women with type 2 diabetes treated with
3 Santos S, Voerman E, Amiano P, et al. Impact of maternal body
metformin or placebo, added to insulin, we found several mass index and gestational weight gain on pregnancy complications:
(secondary, pre-specified) maternal glycaemic and neonatal an individual participant data meta-analysis of European, North
American and Australian cohorts. BJOG 2019; 126: 984–95.
adiposity benefits in the metformin group, including
4 Murphy HR, Bell R, Cartwright C, et al. Improved pregnancy
improved glycaemic control, lower insulin requirements, outcomes in women with type 1 and type 2 diabetes but substantial
less weight gain, fewer caesarean births, lower birthweight clinic-to-clinic variations: a prospective nationwide study.
and adiposity measures, and fewer extreme large-for- Diabetologia 2017; 60: 1668–77.
5 Langer O, Anyaegbunam A, Brustman L, Guidetti D, Levy J,
gestational-age, but more small-for-gestational-age infants. Mazze R. Pregestational diabetes: insulin requirements throughout
Understanding the implications of these effects on infants pregnancy. Am J Obstet Gynecol 1988; 159: 616–21.
will be important to properly advise patients who are 6 Nguyen L, Chan SY, Teo AKK. Metformin from mother to unborn
child—are there unwarranted effects? EBioMedicine 2018;
contemplating the use of metformin during pregnancy. 35: 394–404.
Follow-up of metformin-exposed infants into childhood, 7 Vanky E, Zahlsen K, Spigset O, Carlsen SM. Placental passage of
adolescence, and adulthood will be crucial to gain a broader metformin in women with polycystic ovary syndrome. Fertil Steril
2005; 83: 1575–78.
understanding of the effect of metformin on the future
8 Butalia S, Gutierrez L, Lodha A, Aitken E, Zakariasen A,
health of exposed infants. Donovan L. Short- and long-term outcomes of metformin compared
Contributors with insulin alone in pregnancy: a systematic review and meta-
DSF, BZ, JJS, EA, EAR, GF, ABA, JFRB, GT, and KEM designed the analysis. Diabet Med 2017; 34: 27–36.
study. DSF, LED, BZ, JJS, EA, EAR, IGF, EH, ABA, LLL, DS, JFRB, PJK, 9 Tarry-Adkins JL, Aiken CE, Ozanne SE. Neonatal, infant, and
childhood growth following metformin versus insulin treatment for
SYT, GT, and KEM designed the statistical analysis plan. EA, JFRB, PK,
gestational diabetes: a systematic review and meta-analysis.
JJS, and ST supervised the trial operations, data collections, data quality
PLoS Med 2019; 16: e1002848.
control, and programming for the statistical analyses. DSF, LED, EAR,
10 Cesta CE, Cohen JM, Pazzagli L, et al. Antidiabetic medication use
ABA, DS, HDM, JJS, and ST contributed to the data collection. DSF, BZ,
during pregnancy: an international utilization study.
EA, EAR, GF, ABA, LLL, DS, JFRB, PJK, GT, and KEM provided overall BMJ Open Diabetes Res Care 2019; 7: e000759.
www.thelancet.com/diabetes-endocrinology Vol 8 October 2020 843
Articles
11 Ibrahim MI, Hamdy A, Shafik A, Taha S, Anwar M, Faris M. 24 Coll AP, Chen M, Taskar P, et al. GDF15 mediates the effects of
The role of adding metformin in insulin-resistant diabetic pregnant metformin on body weight and energy balance. Nature 2020;
women: a randomized controlled trial. Arch Gynecol Obstet 2014; 578: 444–48.
289: 959–65. 25 Rasmussen KM, Yaktine AL, US Institute of Medicine. Committee
12 Ainuddin JA, Karim N, Zaheer S, Ali SS, Hasan AA. Metformin to reexamine IOM pregnancy weight guidelines. Weight gain
treatment in type 2 diabetes in pregnancy: an active controlled, during pregnancy: reexamining the guidelines. Washington DC,
parallel-group, randomized, open label study in patients with USA: National Academies Press, 2009.
type 2 diabetes in pregnancy. J Diabetes Res 2015; 2015: 325851. 26 Feig DS, Donovan LE, Corcoy R, et al. Continuous glucose
13 Beyuo T, Obed SA, Adjepong-Yamoah KK, Bugyei KA, Oppong SA, monitoring in pregnant women with type 1 diabetes (CONCEPTT):
Marfoh K. Metformin versus insulin in the management of a multicentre international randomised controlled trial. Lancet 2017;
pre-gestational diabetes mellitus in pregnancy and gestational 390: 2347–59.
diabetes mellitus at the Korle Bu Teaching Hospital: a randomized 27 Mendez-Figueroa H, Truong VT, Pedroza C, Chauhan SP. Morbidity
clinical trial. PLoS One 2015; 10: e0125712. and mortality in small-for-gestational-age infants: a secondary
14 Hickman MA, McBride R, Boggess KA, Strauss R. Metformin analysis of nine MFMU network studies. Am J Perinatol 2017;
compared with insulin in the treatment of pregnant women with 34: 323–32.
overt diabetes: a randomized controlled trial. Am J Perinatol 2013; 28 Savchev S, Sanz-Cortes M, Cruz-Martinez R, et al.
30: 483–90. Neurodevelopmental outcome of full-term small-for-gestational-age
15 Waheed S, Malik FP, Mazhar SB. Efficacy of metformin versus infants with normal placental function. Ultrasound Obstet Gynecol
insulin in the management of pregnancy with diabetes. 2013; 42: 201–06.
J Coll Physicians Surg Pak 2013; 23: 866–69. 29 Barker DJ, Hales CN, Fall CH, Osmond C, Phipps K, Clark PM.
16 Feig DS, Berger H, Donovan L, et al. Diabetes and pregnancy. Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and
Can J Diabetes 2018; 42 (suppl 1): S255–82. hyperlipidaemia (syndrome X): relation to reduced fetal growth.
17 Feig DS, Murphy K, Asztalos E, et al. Metformin in women with Diabetologia 1993; 36: 62–67.
type 2 diabetes in pregnancy (MiTy): a multi-center randomized 30 Coll AP, Chen M, Taskar P, et al. GDF15 mediates the effects of
controlled trial. BMC Pregnancy Childbirth 2016; 16: 173. metformin on body weight and energy balance. Nature 2020;
18 Kramer MS, Platt RW, Wen SW, et al. A new and improved 578: 444–48.
population-based Canadian reference for birth weight for 31 Langer O, Levy J, Brustman L, Anyaegbunam A, Merkatz R,
gestational age. Pediatrics 2001; 108: E35. Divon M. Glycemic control in gestational diabetes mellitus—how
19 Catalano PM, Thomas AJ, Avallone DA, Amini SB. Anthropometric tight is tight enough: small for gestational age versus large for
estimation of neonatal body composition. Am J Obstet Gynecol 1995; gestational age? Am J Obstet Gynecol 1989; 161: 646–53.
173: 1176–81. 32 Chiswick C, Reynolds RM, Denison F, et al. Effect of metformin on
20 Gardosi J, Francis A, Turner S, Williams M. Customized growth maternal and fetal outcomes in obese pregnant women
charts: rationale, validation and clinical benefits. (EMPOWaR): a randomised, double-blind, placebo-controlled trial.
Am J Obstet Gynecol 2018; 218 (2S): S609–18. Lancet Diabetes Endocrinol 2015; 3: 778–86.
21 Joseph KS, Fahey J, Canadian Perinatal Surveillance System. 33 Vanky E, Stridsklev S, Heimstad R, et al. Metformin versus placebo
Validation of perinatal data in the Discharge Abstract Database of from first trimester to delivery in polycystic ovary syndrome:
the Canadian Institute for Health Information. Chronic Dis Can a randomized, controlled multicenter study. J Clin Endocrinol Metab
2009; 29: 96–100. 2010; 95: e448–55.
22 Shavers VL. Measurement of socioeconomic status in health 34 Rowan JA, Rush EC, Plank LD, et al. Metformin in gestational
disparities research. J Natl Med Assoc 2007; 99: 1013–23. diabetes: the offspring follow-up (MiG TOFU): body composition
23 Wulffele MG, Kooy A, Lehert P, et al. Combination of insulin and and metabolic outcomes at 7–9 years of age.
metformin in the treatment of type 2 diabetes. Diabetes Care 2002; BMJ Open Diabetes Res Care 2018; 6: e000456.
25: 2133–40.
844 www.thelancet.com/diabetes-endocrinology Vol 8 October 2020
You might also like
- Complementary and Alternative Medical Lab Testing Part 10: ObstetricsFrom EverandComplementary and Alternative Medical Lab Testing Part 10: ObstetricsNo ratings yet
- Nej Mo A 1509819Document10 pagesNej Mo A 1509819Fhirastika AnnishaNo ratings yet
- Contraception for the Medically Challenging PatientFrom EverandContraception for the Medically Challenging PatientRebecca H. AllenNo ratings yet
- Metformin Vs Insulin GDMDocument20 pagesMetformin Vs Insulin GDMBrenda ValdespinoNo ratings yet
- Mity Kids 3Document3 pagesMity Kids 3api-660408385No ratings yet
- Pediatrics 2012 Aja NieDocument7 pagesPediatrics 2012 Aja NiePutu BudiastawaNo ratings yet
- A Randomized, Controlled Trial of Liraglutide For Adolescents With ObesityDocument12 pagesA Randomized, Controlled Trial of Liraglutide For Adolescents With ObesityJosé Luis ChavesNo ratings yet
- Pediatric Diabetes - 2018 - Candler - Treatment Adherence and BMI Reduction Are Key Predictors of HbA1c 1 Year AfterDocument7 pagesPediatric Diabetes - 2018 - Candler - Treatment Adherence and BMI Reduction Are Key Predictors of HbA1c 1 Year AfterPraska BalabanovaNo ratings yet
- A Randomized, Controlled Trial of Liraglutide For Adolescents With ObesityDocument12 pagesA Randomized, Controlled Trial of Liraglutide For Adolescents With ObesityWarun KumarNo ratings yet
- Feig 2017Document13 pagesFeig 2017Lembaga Pendidikan dan PelayananNo ratings yet
- Embarazo DiabetesDocument10 pagesEmbarazo DiabetesMaria Gabriela AguilarNo ratings yet
- Quality of Life of Children With Type 1 Diabetes: A Systematic ReviewDocument12 pagesQuality of Life of Children With Type 1 Diabetes: A Systematic ReviewNila Sari ChandraNo ratings yet
- Adolescent Dairy Product Consumption and Risk of Type 2 Diabetes in Middle-Aged WomenDocument8 pagesAdolescent Dairy Product Consumption and Risk of Type 2 Diabetes in Middle-Aged WomenWoodyNo ratings yet
- Nejmoa 2206038Document12 pagesNejmoa 2206038Juan David Arboleda LopezNo ratings yet
- Tirzepatide Once Weekly For The Treatment of Obesity Nejmoa2206038Document12 pagesTirzepatide Once Weekly For The Treatment of Obesity Nejmoa2206038Salah ArafehNo ratings yet
- Evaluation of A Smartphone Nutrition and Physical Activity Application To Provide Lifestyle Advice To Pregnant Women: The SNAPP Randomised TrialDocument11 pagesEvaluation of A Smartphone Nutrition and Physical Activity Application To Provide Lifestyle Advice To Pregnant Women: The SNAPP Randomised TrialTaís CidrãoNo ratings yet
- A Case Presentation of An Adult With Gestational Diabetes Mellitus FinalDocument59 pagesA Case Presentation of An Adult With Gestational Diabetes Mellitus FinalJM PunzalanNo ratings yet
- Mediterranean-Style Diet in Pregnant Women With Metabolic Risk Factors (ESTEEM) : A Pragmatic Multicentre Randomised TrialDocument20 pagesMediterranean-Style Diet in Pregnant Women With Metabolic Risk Factors (ESTEEM) : A Pragmatic Multicentre Randomised Trialconstantius augustoNo ratings yet
- Eficácia de Um Programa Intensivo de Visitação Domiiliar Liderado Por Enfermeiras para Mães Adolescentes de Primeira ViagemDocument10 pagesEficácia de Um Programa Intensivo de Visitação Domiiliar Liderado Por Enfermeiras para Mães Adolescentes de Primeira ViagemMarcia RodriguesNo ratings yet
- Gestational Diabetes Research PaperDocument16 pagesGestational Diabetes Research Paperapi-251486092No ratings yet
- Instrumento 1 UsaDocument39 pagesInstrumento 1 Usajorgin chavezNo ratings yet
- Clinical StudyDocument8 pagesClinical StudyanitaNo ratings yet
- Evaluating The Effects of Insulin, Metformin and Glibenclamide On The Pups' Prefrontal Cortex and Oxidative Stress Markers of Streptozotocin-Induced Diabetic Pregnant RatsDocument10 pagesEvaluating The Effects of Insulin, Metformin and Glibenclamide On The Pups' Prefrontal Cortex and Oxidative Stress Markers of Streptozotocin-Induced Diabetic Pregnant RatsMediterr J Pharm Pharm SciNo ratings yet
- Risks Associated With Obesity in Pregnancy (Final Accepted Version)Document47 pagesRisks Associated With Obesity in Pregnancy (Final Accepted Version)SamarNo ratings yet
- Optimal Diets SLDocument69 pagesOptimal Diets SLAliza Dewi FortuaNo ratings yet
- Metformin For GDMDocument7 pagesMetformin For GDMRoro WidyastutiNo ratings yet
- Disease Specific Knowledge and Lifestyle Behavior in Patients With Diabetes Mellitus 2016 Obesity MedicineDocument4 pagesDisease Specific Knowledge and Lifestyle Behavior in Patients With Diabetes Mellitus 2016 Obesity MedicineLiaAriestaNo ratings yet
- The Safety of Proton Pump Inhibitors (Ppis) in Pregnancy: A Meta-AnalysisDocument5 pagesThe Safety of Proton Pump Inhibitors (Ppis) in Pregnancy: A Meta-AnalysisSilvia AryaniNo ratings yet
- Esteves 2012Document15 pagesEsteves 2012Nawaf RuwailiNo ratings yet
- Physical Activity Intensity and Type 2 Diabetes Risk in Overweight Youth A Randomized TriaDocument27 pagesPhysical Activity Intensity and Type 2 Diabetes Risk in Overweight Youth A Randomized TriaMilenckaVidalConsiglieriNo ratings yet
- Holl 2003Document8 pagesHoll 2003Bogdan NeamtuNo ratings yet
- Espghan 2015 - Abstracts JPGN FinalDocument963 pagesEspghan 2015 - Abstracts JPGN FinalAdriana RockerNo ratings yet
- Insulin and MMDocument9 pagesInsulin and MMAkreditasi InternaNo ratings yet
- Lockman 2021Document17 pagesLockman 2021wahyuni yuniNo ratings yet
- Articles: BackgroundDocument14 pagesArticles: BackgroundhudaNo ratings yet
- A Randomised Clinical Trial Comparing Myoinositol and Metformin in PCOSDocument7 pagesA Randomised Clinical Trial Comparing Myoinositol and Metformin in PCOSAtika NajlaNo ratings yet
- OGTT and Adverse Outcome 2020Document10 pagesOGTT and Adverse Outcome 2020Nuraida baharuddinNo ratings yet
- Ten-Year Single-Center Experience of The Ketogenic Diet: Factors in Uencing Efficacy, Tolerability, and ComplianceDocument8 pagesTen-Year Single-Center Experience of The Ketogenic Diet: Factors in Uencing Efficacy, Tolerability, and ComplianceMarcin CiekalskiNo ratings yet
- Perubahan Status Gizi Pada Anak Dengan Leukemia Limfoblastik Akut Selama TerapiDocument6 pagesPerubahan Status Gizi Pada Anak Dengan Leukemia Limfoblastik Akut Selama TerapiRisty Fatmawati LNo ratings yet
- Outi Pellonper A, Kati Mokkala, Noora Houttu, Tero Vahlberg, Ella Koivuniemi, Kristiina Tertti, Tapani R Onnemaa, and Kirsi LaitinenDocument9 pagesOuti Pellonper A, Kati Mokkala, Noora Houttu, Tero Vahlberg, Ella Koivuniemi, Kristiina Tertti, Tapani R Onnemaa, and Kirsi LaitinenLisa Citrawildani07No ratings yet
- Maternal and Perinatal Maternal and Perinatal Outcome of Maternal Obesity Outcome of Maternal Obesity at RSCM in 2014-2019 at RSCM in 2014-2019Document1 pageMaternal and Perinatal Maternal and Perinatal Outcome of Maternal Obesity Outcome of Maternal Obesity at RSCM in 2014-2019 at RSCM in 2014-2019heidi leeNo ratings yet
- New-Guthrie2015Document10 pagesNew-Guthrie2015Ser Eldrin GarciaNo ratings yet
- 265 Full PDFDocument8 pages265 Full PDFNurul Rezki Fitriani AzisNo ratings yet
- Diabetes GAM 2015Document7 pagesDiabetes GAM 2015Anonymous qsegfnnOdNo ratings yet
- Fast FoodDocument8 pagesFast Foodkangna_sharma20No ratings yet
- Ournal of Linical Ncology: OriginalDocument12 pagesOurnal of Linical Ncology: OriginalHadeer EhabNo ratings yet
- Accepted Manuscript: 10.1016/j.nut.2018.05.021Document28 pagesAccepted Manuscript: 10.1016/j.nut.2018.05.021sergedemirdjian1990No ratings yet
- Pilot Project For Education of Gestational Diabetes Mellitus (GDM) Patients - Can It Be Beneficial?Document5 pagesPilot Project For Education of Gestational Diabetes Mellitus (GDM) Patients - Can It Be Beneficial?Moh Halim MukhlasinNo ratings yet
- I J R P S: Metformin Compared To Insulin For The Management of Gestational DiabeticDocument5 pagesI J R P S: Metformin Compared To Insulin For The Management of Gestational DiabeticAbed AlhaleemNo ratings yet
- Maternal and Fetal Outcomes of Obese Pregnant Women: A Prospective Cohort StudyDocument5 pagesMaternal and Fetal Outcomes of Obese Pregnant Women: A Prospective Cohort StudyCostin VrabieNo ratings yet
- Type 1 Diabetes Impairs Female Fertility Even Before It Is DiagnosedDocument8 pagesType 1 Diabetes Impairs Female Fertility Even Before It Is DiagnosedAuliana FENo ratings yet
- Intl J Gynecology Obste - 2023 - Kouiti - Replacement of Watching Television With Physical Activity and The Change inDocument8 pagesIntl J Gynecology Obste - 2023 - Kouiti - Replacement of Watching Television With Physical Activity and The Change inlucynag1997No ratings yet
- New England Journal Medicine: The ofDocument12 pagesNew England Journal Medicine: The ofJesusNo ratings yet
- Evaluation of Clinical Outcomes With Metformin Therapy in South Indian Pcos WomenDocument5 pagesEvaluation of Clinical Outcomes With Metformin Therapy in South Indian Pcos WomenRAPPORTS DE PHARMACIENo ratings yet
- Jur DingDocument8 pagesJur DingDeyaSeisoraNo ratings yet
- RRL3 RLRLDocument18 pagesRRL3 RLRLRowena BayalanNo ratings yet
- Jurnal AncDocument8 pagesJurnal AncNidia FantikasariNo ratings yet
- Effect of Inositol Sterioisomers at Different Dosages in Gestational DiabetesDocument8 pagesEffect of Inositol Sterioisomers at Different Dosages in Gestational DiabetesMohsin HassamNo ratings yet
- Comparison of Serum Levels of Vitamin D and Inflammatory Markers Between Women With Gestational Diabetes Mellitus and Healthy Pregnant ControlDocument8 pagesComparison of Serum Levels of Vitamin D and Inflammatory Markers Between Women With Gestational Diabetes Mellitus and Healthy Pregnant ControlTaufik RizalNo ratings yet
- Medi 102 E33898Document7 pagesMedi 102 E33898ade lydia br.siregarNo ratings yet
- Derichebourg - Universal Registration Document 2020-2021Document256 pagesDerichebourg - Universal Registration Document 2020-2021Abhijeet ShindeNo ratings yet
- Lozada Vs MendozaDocument4 pagesLozada Vs MendozaHarold EstacioNo ratings yet
- Khenpo Tsultrim Gyamtso Rinpoche - Meditation On EmptinessDocument206 pagesKhenpo Tsultrim Gyamtso Rinpoche - Meditation On Emptinessdorje@blueyonder.co.uk100% (1)
- Tropical Design Reviewer (With Answers)Document2 pagesTropical Design Reviewer (With Answers)Sheena Lou Sangalang100% (4)
- Fire Safety Management - Traditional Building Part#2Document194 pagesFire Safety Management - Traditional Building Part#2Yoyon Haryono100% (1)
- Draft DAO SAPA Provisional AgreementDocument6 pagesDraft DAO SAPA Provisional AgreementStaff of Gov Victor J YuNo ratings yet
- The Gift of ADHDDocument233 pagesThe Gift of ADHDGerman Rosales Vargas100% (3)
- Introduction To Communication Systems: James Flynn Sharlene KatzDocument15 pagesIntroduction To Communication Systems: James Flynn Sharlene KatzAnisari MeiNo ratings yet
- Degree Program Cheongju UniversityDocument10 pagesDegree Program Cheongju University심AvanNo ratings yet
- Pentagram Business PlanDocument13 pagesPentagram Business PlantroubledsoulNo ratings yet
- Planning and Design of A Cricket StadiumDocument14 pagesPlanning and Design of A Cricket StadiumTenu Sara Thomas50% (6)
- Children's LiteratureDocument13 pagesChildren's Literaturerexson de villaNo ratings yet
- Albert Einstein's Riddle - With Solution Explained: October 19, 2009 - AuthorDocument6 pagesAlbert Einstein's Riddle - With Solution Explained: October 19, 2009 - Authorgt295038No ratings yet
- Periodic Table & PeriodicityDocument22 pagesPeriodic Table & PeriodicityMike hunkNo ratings yet
- Text Mohamed AliDocument2 pagesText Mohamed AliARYAJAI SINGHNo ratings yet
- 1219201571137027Document5 pages1219201571137027Nishant SinghNo ratings yet
- 2beloved Lizzo PDFDocument1 page2beloved Lizzo PDFAntwerpQueerChoir AQCNo ratings yet
- Life Without A Centre by Jeff FosterDocument160 pagesLife Without A Centre by Jeff Fosterdwhiteutopia100% (5)
- Franieboy Ponce, BSIT-1, - DAY 2 ACTIVITYDocument2 pagesFranieboy Ponce, BSIT-1, - DAY 2 ACTIVITYFrancisco PonceNo ratings yet
- Research Methods in Accounting & Finance Chapter 5Document27 pagesResearch Methods in Accounting & Finance Chapter 5bikilahussenNo ratings yet
- WWW - Nswkendo IaidoDocument1 pageWWW - Nswkendo IaidoAshley AndersonNo ratings yet
- How A Type 4 Multiverse WorksDocument4 pagesHow A Type 4 Multiverse WorksIdkNo ratings yet
- UNIT VI. Gunpowder and ExplosivesDocument6 pagesUNIT VI. Gunpowder and ExplosivesMariz Althea Jem BrionesNo ratings yet
- ISO 9001 QuizDocument4 pagesISO 9001 QuizGVS Rao0% (1)
- Right To Freedom From Torture in NepalDocument323 pagesRight To Freedom From Torture in NepalAnanta ChaliseNo ratings yet
- Principles of Marketing: Quarter 1 - Module 6: Marketing ResearchDocument17 pagesPrinciples of Marketing: Quarter 1 - Module 6: Marketing ResearchAmber Dela Cruz100% (1)
- Strength Exp 2 Brinell Hardness TestDocument13 pagesStrength Exp 2 Brinell Hardness Testhayder alaliNo ratings yet
- Block-1 Communication IGNOUDocument81 pagesBlock-1 Communication IGNOUr kumarNo ratings yet
- 215 Final Exam Formula SheetDocument2 pages215 Final Exam Formula SheetH.C. Z.No ratings yet
- Hotel BookingDocument1 pageHotel BookingJagjeet SinghNo ratings yet
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)
- Rewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryFrom EverandRewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryRating: 4.5 out of 5 stars4.5/5 (157)
- An Autobiography of Trauma: A Healing JourneyFrom EverandAn Autobiography of Trauma: A Healing JourneyRating: 5 out of 5 stars5/5 (2)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsFrom EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsRating: 4.5 out of 5 stars4.5/5 (38)
- My Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesFrom EverandMy Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesRating: 5 out of 5 stars5/5 (70)
- Somatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionFrom EverandSomatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionNo ratings yet
- The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeFrom EverandThe Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeRating: 4.5 out of 5 stars4.5/5 (140)
- Summary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDFrom EverandSummary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDRating: 4.5 out of 5 stars4.5/5 (167)
- The Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeFrom EverandThe Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeRating: 4.5 out of 5 stars4.5/5 (49)
- Rapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreFrom EverandRapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreRating: 5 out of 5 stars5/5 (17)
- Triggers: How We Can Stop Reacting and Start HealingFrom EverandTriggers: How We Can Stop Reacting and Start HealingRating: 5 out of 5 stars5/5 (58)
- Summary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisFrom EverandSummary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (5)
- Embrace Your Weird: Face Your Fears and Unleash CreativityFrom EverandEmbrace Your Weird: Face Your Fears and Unleash CreativityRating: 4.5 out of 5 stars4.5/5 (124)
- Heal the Body, Heal the Mind: A Somatic Approach to Moving Beyond TraumaFrom EverandHeal the Body, Heal the Mind: A Somatic Approach to Moving Beyond TraumaRating: 4.5 out of 5 stars4.5/5 (56)
- Brain Inflamed: Uncovering the Hidden Causes of Anxiety, Depression, and Other Mood Disorders in Adolescents and TeensFrom EverandBrain Inflamed: Uncovering the Hidden Causes of Anxiety, Depression, and Other Mood Disorders in Adolescents and TeensRating: 5 out of 5 stars5/5 (2)
- Don't Panic: Taking Control of Anxiety AttacksFrom EverandDon't Panic: Taking Control of Anxiety AttacksRating: 4 out of 5 stars4/5 (12)
- Winning the War in Your Mind: Change Your Thinking, Change Your LifeFrom EverandWinning the War in Your Mind: Change Your Thinking, Change Your LifeRating: 5 out of 5 stars5/5 (558)
- Overcoming Unwanted Intrusive Thoughts: A CBT-Based Guide to Getting Over Frightening, Obsessive, or Disturbing ThoughtsFrom EverandOvercoming Unwanted Intrusive Thoughts: A CBT-Based Guide to Getting Over Frightening, Obsessive, or Disturbing ThoughtsRating: 4.5 out of 5 stars4.5/5 (48)
- BORDERLINE PERSONALITY DISORDER: Help Yourself and Help Others. Articulate Guide to BPD. Tools and Techniques to Control Emotions, Anger, and Mood Swings. Save All Your Relationships and Yourself. NEW VERSIONFrom EverandBORDERLINE PERSONALITY DISORDER: Help Yourself and Help Others. Articulate Guide to BPD. Tools and Techniques to Control Emotions, Anger, and Mood Swings. Save All Your Relationships and Yourself. NEW VERSIONRating: 4.5 out of 5 stars4.5/5 (24)
- Feel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveFrom EverandFeel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveRating: 4 out of 5 stars4/5 (250)
- I Don't Want to Talk About It: Overcoming the Secret Legacy of Male DepressionFrom EverandI Don't Want to Talk About It: Overcoming the Secret Legacy of Male DepressionRating: 4 out of 5 stars4/5 (74)
- Vagus Nerve: A Complete Self Help Guide to Stimulate and Activate Vagal Tone — A Self Healing Exercises to Reduce Chronic Illness, PTSD, Anxiety, Inflammation, Depression, Trauma, and AngerFrom EverandVagus Nerve: A Complete Self Help Guide to Stimulate and Activate Vagal Tone — A Self Healing Exercises to Reduce Chronic Illness, PTSD, Anxiety, Inflammation, Depression, Trauma, and AngerRating: 4.5 out of 5 stars4.5/5 (16)
- When Religion Hurts You: Healing from Religious Trauma and the Impact of High-Control ReligionFrom EverandWhen Religion Hurts You: Healing from Religious Trauma and the Impact of High-Control ReligionRating: 4 out of 5 stars4/5 (11)
- Anxious for Nothing: Finding Calm in a Chaotic WorldFrom EverandAnxious for Nothing: Finding Calm in a Chaotic WorldRating: 4.5 out of 5 stars4.5/5 (1244)