Professional Documents
Culture Documents
Глушко Сльоз 2м-18-9 ЕНДОТЕЛІАЛЬНА ДИСФУНКЦІЯ ЯК ФАКТОР РОЗВИТКУ ПОРУШЕННЯ ФУНКЦІЇ НИРОК У ХВОРИХ НА ГІПОТИРЕОЗ
Uploaded by
Глушко Світлана МиколаївнаCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Глушко Сльоз 2м-18-9 ЕНДОТЕЛІАЛЬНА ДИСФУНКЦІЯ ЯК ФАКТОР РОЗВИТКУ ПОРУШЕННЯ ФУНКЦІЇ НИРОК У ХВОРИХ НА ГІПОТИРЕОЗ
Uploaded by
Глушко Світлана МиколаївнаCopyright:
Available Formats
ENDOTHELIAL DYSFUNCTION AS A FACTOR IN THE
DEVELOPMENT OF RENAL DYSFUNCTION IN PATIENTS WITH
HYPOTHYROIDISM
Viun Tetiana
Ph.D., Assistant of General Practice department - Family Medicine
Hlushko Svitlana
Sloz Diana
Students
Kharkiv National Medical University
Kharkiv, Ukraine
viun.tatiana@gmail.com
smhlushko.2m18@knmu.edu.ua
dvsloz.2m18@knmu.edu.ua
Introduction. The endothelium is an organ of internal secretion that
controls the tone of blood vessels, protects them from the negative effects of
circulating cells and substances, regulates the transfer of soluble substances to
the cells of the vessel wall, and also controls immune, inflammatory and
reparative processes, maintains the balance of local hemostasis processes.
Today, the endothelium is considered another target organ. It is known that a
violation of its function, known as endothelial dysfunction (ED), is an important
component of the development of many diseases. Several studies have
confirmed that hypothyroidism can lead to endothelial dysfunction.
The main goal of our work is to analyze the scientific literature with the
aim of summarizing information about the current views of the influence of
endothelial dysfunction on kidney function in patients with primary
hypothyroidism.
Materials and methods. 188 patients with detected hypothyroidism who
are registered with an endocrinologist took part in the study. The average age of
the patients was 56 years, with a medical history of about 8 years. The control
group also included 30 people who did not have any thyroid diseases.
The criteria for inclusion in the study provide for the presence of a
previously confirmed diagnosis of hypothyroidism, provided that the level of
TSH exceeds 4.0 mIU/l. A criterion is also the presence of reduced levels of
free thyroxine (fT4) less than 10.3 pmol/l and free triiodothyronine (fT3) less
than 2.3 pmol/l. In addition, it is important that the patient gives voluntary
consent to participate in the study.
Exclusion criteria from the study are such factors as cerebral circulation
disorders, any form of coronary heart disease, arterial hypertension above the
first degree, chronic diseases of the cardiovascular system in the anamnesis.
Persons with chronic kidney and liver diseases, oncological diseases,
autoimmune diseases, pregnancy, taking hypolipidemic drugs and mental
diseases are also excluded.
A comprehensive laboratory-instrumental study of kidney function and
assessment of endothelial function was performed at baseline, 3 and 6 months
after treatment using a test with reactive hyperemia. The basis for the analysis
was the assessment of endothelium-dependent vasodilatation (EDVD) of the
brachial artery (BA). The reaction of BA to the phase of reactive hyperemia,
which is manifested by dilation by more than 10% of the initial value, is
considered normal. If the LVEF was less than 10% or vasoconstriction was
observed, the patient was considered to have endothelial dysfunction. Similarly
to the sample with reactive hyperemia, the endothelium-independent
vasodilatation index was calculated - the relative change in the internal diameter
of the PA after sublingual administration of nitromint. The level of
vasculoendothelial growth factor (VEGF) in blood plasma was also determined.
All patients underwent a complete general clinical examination, including
measurements of body mass index (BMI), thyroid hormone (TSH) and TSH
levels at the beginning of the study and after 6 months of treatment. The
presence of kidney damage was determined by the presence of violations of the
permeability of the glomerular filter, which was manifested by the presence of
albuminuria and indicators of the glomerular filtration rate (GFR) calculated
according to the CKD-EPI formulas. To assess the impact of the autoimmune
process in the thyroid gland, as well as BMI, patients were divided into four
groups: the first consisted of 45 patients with hypothyroidism on the
background of autoimmune thyroiditis (AIT) without obesity; the second - 46
patients with AIT with hypothyroidism and obesity; the third - 47 patients with
obvious hypothyroidism without obesity; the fourth - 50 patients with obvious
hypothyroidism with obesity. There were no significant differences between
patients in the main and control groups in terms of age, gender, and baseline
therapy.
Changes in clinical signs of hypothyroidism, indicators of endothelial
dysfunction during treatment with levothyroxine, enalapril and atorvastatin
were studied. The method of variational statistical analysis was used for the
analysis.
Research results. Endothelial function was assessed using the
endothelium-dependent vasodilatation (EDVD) index.
The revealed more pronounced ED in patient groups II and IV indicates
the effect of obesity on endothelial dysfunction. In addition, in these groups, the
increase in the diameter of the brachial artery after compression is half as much,
and the EDVD is also smaller than in the control group, by 46.4 and 47.7% (p <
0.05).
According to modern scientific data, VEGF induces the expression of one
of the most powerful factors of ED - endothelin-I.
According to the results of the study, the level of VEGF significantly
increases in the blood plasma of patients with manifest hypothyroidism,
compared to controls. Thus, there was an increase in VEGF in the group with
hypothyroidism on the background of AIT without obesity, 46.5 ± 1.4 pg/ml (p
< 0.05), and in patients with hypothyroidism on the background of AIT and
obesity 48.1 ± 1.8 pg/ml (p < 0.05). In patients with postoperative
hypothyroidism, 43.0 ± 1.5 pg/ml (p < 0.05) — in patients without
hypothyroidism and up to 45.8 ± 2.5 pg/ml (p < 0.05) in patients with
postoperative hypothyroidism. hypothyroidism and obesity.
According to the data of correlation analysis, a direct correlation of
medium strength was found between the level of VEGF and the level of TSH in
the I group of patients, in the II group - a strong direct correlation, in the III
group - a moderate direct correlation, and in the IV group - a significant direct
correlation.
The relationship between the level of VEGF and the level of antibodies to
thyroid peroxidase was found in groups I and II, and in groups III and IV this
relationship is absent.
In addition, there is a direct moderate relationship between the levels of
VEGF and total cholesterol in patients of groups I and III, significant in groups
II and IV.
According to these data, the level of VEGF increases in patients with
hypothyroidism with and without obesity, but the highest indicators are
registered in patients with hypothyroidism on the background of AIT.
For a more detailed description of the results of patient treatment,
depending on the scheme, each group was divided into 2 subgroups. Subgroup
A included basic treatment of LT4, subgroup B - complex treatment - LT4,
atorvastatin 20 mg per day for 6 months and enalapril. Treatment included two
stages. The first stage included dose titration of levothyroxine (LT4) and
enalapril. Enalapril was prescribed to patients, with an initial dose of 2.5
mg/day, and it was increased until the maximum possible dose was reached,
taking into account their hemodynamic parameters. The second stage of
treatment included the addition of atorvastatin at a dose of 20 mg/day to
individually selected doses of LT4 and enalapril.
In the patients of the first and second groups, compensation of
hypothyroidism after 6 months led to a probable increase in EDVD. However,
with complex treatment with atorvastatin and enalapril, the changes in EDVD
were significantly better (p < 0.05) already after 3 and 6 months. In the groups
with postoperative hypothyroidism, the appointment of levothyroxine
contributed to the tendency towards the increase of EDVD, but the changes
were not probable even after 6 months. While in patients who received complex
treatment, EDVD probably increased already after 3 months.
Analyzing the dynamics of the VEGF level in patients with basic and
complex treatment, the following data were obtained: in group I (with AIT
without obesity), in patients who received complex therapy with atorvastatin
and enalapril, the VEGF level decreased from 46.5 ± 1.1 to 39, 9 ± 1.7 pg/ml,
(on average by 14.2%), a slight decrease was found in group IA - from 46.4 ±
2.6 to 44.7 ± 3.8 pg/ml. In group II (with AIT and obesity) against the
background of basic treatment, the content of VEGF decreased improbably, and
in patients with complex treatment from 47.7 ± 1.7 to 37.4 ± 2.2 pg/ml (by
21.7%) . In subgroup IIIA (manifest hypothyroidism without obesity, basic
treatment) - a decrease in VEGF is unlikely, IIIB - an average decrease of
25.3%. In patients with manifest hypothyroidism with obesity who received
basic treatment (subgroup IVA), VEGF decreased from 45.9 ± 1.8 to 39.9 ± 1.5
pg/ml (on average by 13%), in the subgroup with complex treatment (IVB)
from 45.6 ± 4.9 to 33.6 ± 0.98 pg/ml, i.e. by 26.5% on average.
It can be concluded that the use of complex therapy with the addition of
enalapril and atorvastatin reduces the formation of VEGF.
Conclusion. The obtained results indicate that people with
uncompensated hypothyroidism have a violation of endothelium-dependent
vasodilatation (ESVD). However, no violations in the mechanisms of
endothelium-independent vasodilatation were detected.
The obtained correlations show the mutual influence of thyroid
hypofunction, obesity and hypercholesterolemia on the development of
endothelial dysfunction in people with primary hypothyroidism.
Endothelial dysfunction (ED) is an important factor in the development of
atherosclerosis, complications associated with atherothrombosis, heart failure,
as well as in the formation of clinical manifestations of some cardiovascular
diseases. To study the effect of ED on kidney function, an analysis was
conducted comparing one of the indicators of endothelial dysfunction - GFR
and GFR. It was found that there is a reversible relationship between them,
which was moderately expressed in groups I and II, and weak, but positive in
groups III and IV. Therefore, it can be argued that ED has a negative effect on
kidney function in patients with hypothyroidism.
The obtained results of treatment with the use of levothyroxine, enalapril
(ACE inhibitor) and atorvastatin confirm the probable improvement of the
endothelium in patients with hypothyroidism regardless of its origin and the
presence of obesity. Thus, the combined use of levothyroxine, enalapril (an
ACE inhibitor) and atorvastatin significantly inhibits the formation of VEGF
and improves endothelial function.
You might also like
- Complementary and Alternative Medical Lab Testing Part 8: UrologyFrom EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyRating: 3 out of 5 stars3/5 (1)
- Prevalence of Dyslipidemia, Vitamin B12 Deficiency and Depression in Patients With Subclinical, Newly Diagnosed and Established HypothyroidismDocument9 pagesPrevalence of Dyslipidemia, Vitamin B12 Deficiency and Depression in Patients With Subclinical, Newly Diagnosed and Established HypothyroidismIJAR JOURNALNo ratings yet
- Management of Occult GI Bleeding: A Clinical GuideFrom EverandManagement of Occult GI Bleeding: A Clinical GuideMicheal TadrosNo ratings yet
- A Study of Electrocardiographic Changes in Thyroid DisordersDocument5 pagesA Study of Electrocardiographic Changes in Thyroid Disordersnurharyanti darmaningtyasNo ratings yet
- Medi 94 E1123Document7 pagesMedi 94 E1123ardytawaradaniNo ratings yet
- Turkish Journal Subclinical HypothyroidismDocument5 pagesTurkish Journal Subclinical HypothyroidismAminaNo ratings yet
- New England Journal Medicine: The ofDocument13 pagesNew England Journal Medicine: The ofFirdausul Ma'rifahNo ratings yet
- Nejmoa1603825 PDFDocument11 pagesNejmoa1603825 PDFPsikiatri KlenderNo ratings yet
- Adverse Effects of Hemodialysis On Kidney PatientsDocument30 pagesAdverse Effects of Hemodialysis On Kidney PatientsTania Alsyabilla aaNo ratings yet
- Hypertension Control in African-American Patients With Chronic Kidney DiseaseDocument3 pagesHypertension Control in African-American Patients With Chronic Kidney Diseaseandikaagus13No ratings yet
- ManuscriptDocument17 pagesManuscriptAnonymous y6NmP9NHkYNo ratings yet
- ConclusionDocument2 pagesConclusionanzarNo ratings yet
- 13 Vol. 7 Issue 10 October 2016 IJPSR RA 66001 PDFDocument8 pages13 Vol. 7 Issue 10 October 2016 IJPSR RA 66001 PDFSami SamiNo ratings yet
- Individual and Family Experience in Maintain Client HypertensionDocument6 pagesIndividual and Family Experience in Maintain Client HypertensionAlif TriyuningsiNo ratings yet
- Research Article: Acupuncture For Functional Dyspepsia: A Single Blinded, Randomized, Controlled TrialDocument10 pagesResearch Article: Acupuncture For Functional Dyspepsia: A Single Blinded, Randomized, Controlled TrialairinNo ratings yet
- Apem 2018 23 1 38Document5 pagesApem 2018 23 1 38Dewi PrasetiaNo ratings yet
- Researcharticle Open Access: Mahdieh Abbasalizad Farhangi, Parvin Dehghan, Siroos Tajmiri and Mehran Mesgari AbbasiDocument9 pagesResearcharticle Open Access: Mahdieh Abbasalizad Farhangi, Parvin Dehghan, Siroos Tajmiri and Mehran Mesgari AbbasilolaNo ratings yet
- Clinical Study: Thyroid Dysfunction and Autoantibodies Association With Hypertensive Disorders During PregnancyDocument6 pagesClinical Study: Thyroid Dysfunction and Autoantibodies Association With Hypertensive Disorders During PregnancyihdinzNo ratings yet
- Iaim 2017 0407 06Document6 pagesIaim 2017 0407 06Nur WahyuniNo ratings yet
- Research Study JournalDocument27 pagesResearch Study JournalHyacinth A RotaNo ratings yet
- B-Cell Function and Thyroid Dysfunction: A Cross-Sectional StudyDocument8 pagesB-Cell Function and Thyroid Dysfunction: A Cross-Sectional StudyAbdi KebedeNo ratings yet
- The Prevalence, Risk Factors and Clinical Correlates of Obesity in Chinese Patients WithDocument20 pagesThe Prevalence, Risk Factors and Clinical Correlates of Obesity in Chinese Patients WithjhuNo ratings yet
- Dialyzer Membrane Permeability and Survi PDFDocument7 pagesDialyzer Membrane Permeability and Survi PDFNurul SaufikaNo ratings yet
- E2 Journal of Hypertension Vol 35, E-Supplement 3, November 2017Document1 pageE2 Journal of Hypertension Vol 35, E-Supplement 3, November 2017Sadam_fasterNo ratings yet
- Long-term follow-up of Japanese type 2 diabetes patients in lifestyle intervention studyDocument9 pagesLong-term follow-up of Japanese type 2 diabetes patients in lifestyle intervention studyPutri HakimNo ratings yet
- Levothyroxine Treatment Improves fT4 Levels in Subclinical Hypothyroid PatientsDocument10 pagesLevothyroxine Treatment Improves fT4 Levels in Subclinical Hypothyroid PatientsmutimutimutiNo ratings yet
- Clinical Study Results in Paediatric PatientsDocument9 pagesClinical Study Results in Paediatric PatientsM J garments TprNo ratings yet
- DNB Vol25 No2 142Document7 pagesDNB Vol25 No2 142Apsopela SandiveraNo ratings yet
- Versus: Pentoxifylline Prednisolone For Severe Alcoholic Hepatitis: A Randomized Controlled TrialDocument7 pagesVersus: Pentoxifylline Prednisolone For Severe Alcoholic Hepatitis: A Randomized Controlled TrialAhmad Faisal MaulanaNo ratings yet
- Acupuncture For Constipation in Patients With Stroke: Protocol of A Systematic Review and Meta-AnalysisDocument10 pagesAcupuncture For Constipation in Patients With Stroke: Protocol of A Systematic Review and Meta-AnalysisYUTRILIANo ratings yet
- Research Article: Acupuncture For Functional Dyspepsia: A Single Blinded, Randomized, Controlled TrialDocument9 pagesResearch Article: Acupuncture For Functional Dyspepsia: A Single Blinded, Randomized, Controlled Trialmazh21No ratings yet
- The Impact of Socioeconomic Status and Nutritional Biochemical Markers On Quality of Life of Chronic Dialysis Patients?Document7 pagesThe Impact of Socioeconomic Status and Nutritional Biochemical Markers On Quality of Life of Chronic Dialysis Patients?Pablo AlvarezNo ratings yet
- Family Member-Based Supervision of Patients With Hypertension: A Cluster Randomized Trial in Rural ChinaDocument8 pagesFamily Member-Based Supervision of Patients With Hypertension: A Cluster Randomized Trial in Rural ChinaAchmad YasinNo ratings yet
- Articulo Cientfico InglesDocument10 pagesArticulo Cientfico InglesGloria MariaNo ratings yet
- Study of Thyroid Profile in Geriatric and Non Geriartic Diabetes MellitusDocument8 pagesStudy of Thyroid Profile in Geriatric and Non Geriartic Diabetes MellitusIJAR JOURNALNo ratings yet
- Improving Adherence and Biomedical Markers in Hemodialysis Patients: The Effects of Relaxation TherapyDocument9 pagesImproving Adherence and Biomedical Markers in Hemodialysis Patients: The Effects of Relaxation TherapyheriNo ratings yet
- Involuntary Weight Loss. Does A Negative Baseline Evaluation Provide Adequate Reassurance?Document5 pagesInvoluntary Weight Loss. Does A Negative Baseline Evaluation Provide Adequate Reassurance?nacxit6No ratings yet
- Jurnal Tatalaksana 2Document7 pagesJurnal Tatalaksana 2winny kartikaNo ratings yet
- 1161-Article Text-4602-1-10-20211228Document6 pages1161-Article Text-4602-1-10-20211228amar prasadNo ratings yet
- Hypertension Among Older Adults in Low-And Middle-Income Countries: Prevalence, Awareness and ControlDocument13 pagesHypertension Among Older Adults in Low-And Middle-Income Countries: Prevalence, Awareness and ControlErniRukmanaNo ratings yet
- Wang 2012Document7 pagesWang 2012pelinNo ratings yet
- 1161 Jphi QCRDDocument6 pages1161 Jphi QCRDamar prasadNo ratings yet
- Hypertension Research PaperDocument73 pagesHypertension Research PaperLadylace AmandyNo ratings yet
- Hypertension ThesisDocument31 pagesHypertension ThesisNavin AdhikariNo ratings yet
- Quality of life in patients with adenomyosis and endometrial processesDocument6 pagesQuality of life in patients with adenomyosis and endometrial processesDeni Prasetyo UtomoNo ratings yet
- Journal Pre-Proof: Clinical NutritionDocument19 pagesJournal Pre-Proof: Clinical NutritionThay SousaNo ratings yet
- Effect of Patient Education Intervention On Medication AdherenceDocument17 pagesEffect of Patient Education Intervention On Medication AdherenceDavid LomentigarNo ratings yet
- Tight GlycemicDocument10 pagesTight GlycemicIsmail Mohammed AbdelgawadNo ratings yet
- Ircmj 17 06 20705 PDFDocument7 pagesIrcmj 17 06 20705 PDFUchi SuhermanNo ratings yet
- Impact of A Nurse Short Message Service Intervention For Patients With DiabetesDocument6 pagesImpact of A Nurse Short Message Service Intervention For Patients With DiabetesFatima Akbar.No ratings yet
- 3E - Agustin, Anne Julia - Group 1 - Case 7,8Document5 pages3E - Agustin, Anne Julia - Group 1 - Case 7,8Anne Julia AgustinNo ratings yet
- Emerging Therapeutic Options For Non-Alcoholic Fatty Liver DiseaseDocument13 pagesEmerging Therapeutic Options For Non-Alcoholic Fatty Liver Diseasew57t4yrkt6No ratings yet
- Thyroid Dysfunction and Anaemia in A Large Population-Based StudyDocument5 pagesThyroid Dysfunction and Anaemia in A Large Population-Based StudyRaissa Metasari TantoNo ratings yet
- National Nutrition and Health Sur Vey (Nnhes) : Atherosclerosis - Related Diseases and Risk FactorsDocument11 pagesNational Nutrition and Health Sur Vey (Nnhes) : Atherosclerosis - Related Diseases and Risk FactorsGene Alfonso BanawaNo ratings yet
- Tulburari MetaboliceDocument8 pagesTulburari MetaboliceAlexandra AlexandraNo ratings yet
- Da QingDocument18 pagesDa QingAlina PopaNo ratings yet
- Effects of Electroacupuncture and Chinese Kidney-Nourishing Medi-Cine On Polycystic Ovary Syndrome in Obese PatientsDocument7 pagesEffects of Electroacupuncture and Chinese Kidney-Nourishing Medi-Cine On Polycystic Ovary Syndrome in Obese PatientsKe XuNo ratings yet
- 28-1552560065Document5 pages28-1552560065180045No ratings yet
- Ebsco ContentServerDocument7 pagesEbsco ContentServerHailey LapineNo ratings yet
- The Efficacy of A Health Program and A Food Diary in Blood Sugar Control of Patients With Type 2 DiabetesDocument7 pagesThe Efficacy of A Health Program and A Food Diary in Blood Sugar Control of Patients With Type 2 DiabetesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Stanford MSE FlowchartDocument1 pageStanford MSE FlowchartJoseyNo ratings yet
- Uss Port Royal (CG 73)Document9 pagesUss Port Royal (CG 73)samlagroneNo ratings yet
- Slip-System Cal PDFDocument13 pagesSlip-System Cal PDFVanaja JadapalliNo ratings yet
- CPG Prevention, Diagnosis & Management of IE PDFDocument182 pagesCPG Prevention, Diagnosis & Management of IE PDFsigitNo ratings yet
- CS/CS/SB 1550: Prescription DrugsDocument49 pagesCS/CS/SB 1550: Prescription DrugsBrandon HoganNo ratings yet
- Purposive Communication: Republic of The Philippines Province of Ilocos Sur Ilocos Sur Community College Vigan CityDocument7 pagesPurposive Communication: Republic of The Philippines Province of Ilocos Sur Ilocos Sur Community College Vigan CityLes GasparNo ratings yet
- 2021062476 (1)Document8 pages2021062476 (1)Naidu SairajNo ratings yet
- How To Make Nano Silica From Extracted Silica Rice Husk (Discussion)Document1 pageHow To Make Nano Silica From Extracted Silica Rice Husk (Discussion)MohdhafizFaiz MdAliNo ratings yet
- Product Brand Management 427 v1Document484 pagesProduct Brand Management 427 v1Adii AdityaNo ratings yet
- Advanced Features and Troubleshooting ManualDocument138 pagesAdvanced Features and Troubleshooting ManualHugo Manuel Sánchez MartínezNo ratings yet
- Karl-Fischer TitrationDocument19 pagesKarl-Fischer TitrationSomnath BanerjeeNo ratings yet
- Bringing Class to Mass: L'Oreal's Plénitude Line Struggles in the USDocument36 pagesBringing Class to Mass: L'Oreal's Plénitude Line Struggles in the USLeejat Kumar PradhanNo ratings yet
- Final MTech ProjectDocument30 pagesFinal MTech ProjectArunSharmaNo ratings yet
- Glover U Business Plan 2022 DigitalDocument25 pagesGlover U Business Plan 2022 DigitalJustin CarruthNo ratings yet
- CH - 3 Class XII Physics (E-Notes)Document9 pagesCH - 3 Class XII Physics (E-Notes)tejasNo ratings yet
- Internal and external factors affecting pricing decisionsDocument6 pagesInternal and external factors affecting pricing decisionsNguyễn YếnNo ratings yet
- Unit 1 Lesson 2 PDFDocument20 pagesUnit 1 Lesson 2 PDFKristyll ArguellesNo ratings yet
- Macroeconomics: University of Economics Ho Chi Minh CityDocument193 pagesMacroeconomics: University of Economics Ho Chi Minh CityNguyễn Văn GiápNo ratings yet
- Rexsteel English72Document10 pagesRexsteel English72Bogie Prastowo MahardhikaNo ratings yet
- Cot 1 Detailed Lesson Plan in Science 10Document3 pagesCot 1 Detailed Lesson Plan in Science 10Arlen FuentebellaNo ratings yet
- Miscellanea: Arab-Sasanian Copper P Esents Varie Ypo OgyDocument24 pagesMiscellanea: Arab-Sasanian Copper P Esents Varie Ypo Ogy12chainsNo ratings yet
- The Law of DemandDocument13 pagesThe Law of DemandAngelique MancillaNo ratings yet
- VRF, MPLS and MP-BGP FundamentalsDocument55 pagesVRF, MPLS and MP-BGP FundamentalsIVAN TANEV100% (2)
- Simple BoxDocument104 pagesSimple BoxTÙNGNo ratings yet
- Yu Gi Oh Card DetailDocument112 pagesYu Gi Oh Card DetailLandel SmithNo ratings yet
- Buwis ButilDocument2 pagesBuwis ButilHelbert Agluba PaatNo ratings yet
- A Closer Look at The Cosmetics Industry and The Role of Marketing TranslationDocument5 pagesA Closer Look at The Cosmetics Industry and The Role of Marketing Translationagnes meilhacNo ratings yet
- International Journal of Infectious DiseasesDocument3 pagesInternational Journal of Infectious DiseasesDetti FahmiasyariNo ratings yet
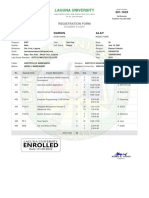
- Darius Registration Form 201 1623 2nd Semester A.Y. 2021 2022Document1 pageDarius Registration Form 201 1623 2nd Semester A.Y. 2021 2022Kristilla Anonuevo CardonaNo ratings yet
- Prueba Final Inglres Robert PalaciosDocument2 pagesPrueba Final Inglres Robert PalaciosCarlos GuerreroNo ratings yet