Professional Documents
Culture Documents
Do Varus or Valgus Outliers Have Higher Forces in The Medial or Lateral Compartments Than Those Which Are In-Range After A Kinematically Aligned Total Knee Arthroplasty
Uploaded by
Asmed El SalugOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Do Varus or Valgus Outliers Have Higher Forces in The Medial or Lateral Compartments Than Those Which Are In-Range After A Kinematically Aligned Total Knee Arthroplasty
Uploaded by
Asmed El SalugCopyright:
Available Formats
KNEE
Do varus or valgus outliers have higher forces
in the medial or lateral compartments than
those which are in-range after a kinematically
aligned total knee arthroplasty?
LIMB AND JOINT LINE ALIGNMENT AFTER KINEMATICALLY
ALIGNED TOTAL KNEE ARTHROPLASTY
T. J. Shelton, Aims
A. J. Nedopil, The aims of this study were to determine the proportion of patients with outlier varus or
S. M. Howell, valgus alignment in kinematically aligned total knee arthroplasty (TKA), whether those with
M. L. Hull outlier varus or valgus alignment have higher forces in the medial or lateral compartments
of the knee than those with in-range alignment and whether measurements of the
From Department of alignment of the limb, knee and components predict compartment forces.
Orthopaedic Surgery,
Patients and Methods
University of The intra-operative forces in the medial and lateral compartments were measured with an
California, Davis, instrumented tibial insert in 67 patients who underwent a kinematically aligned TKA during
Sacramento, United passive movement. The mean of the forces at full extension, 45° and 90° of flexion
States determined the force in the medial and lateral compartments. Measurements of the
alignment of the limb and the components included the hip-knee-ankle (HKA) angle,
proximal medial tibial angle (PMTA), and distal lateral femoral angle (DLFA). Measurements
of the alignment of the knee and the components included the tibiofemoral angle (TFA),
T. J. Shelton, MD, MS,
Orthopaedic Surgeon,
tibial component angle (TCA) and femoral component angle (FCA). Alignment was
Department of Orthopaedic measured on post-operative, non-weight-bearing anteroposterior (AP) scanograms and
Surgery
A. J. Nedopil, MD,
categorised as varus or valgus outlier or in-range in relation to mechanically aligned criteria.
Orthopaedic Surgeon,
Department of Orthopaedic Results
Surgery The proportion of patients with outlier varus or valgus alignment was 16%/24% for the HKA
University of California, Davis,
4860 Y Street, Suite 3800, angle, 55%/0% for the PMTA, 0%/57% for the DLFA, 25%/12% for the TFA, 100%/0% for the
Sacramento, California 95817, TCA, and 0%/64% for the FCA. In general, the forces in the medial and lateral compartments
USA.
of those with outlier alignment were not different from those with in-range alignment
S. M. Howell, MD,
except for the TFA, in which patients with outlier varus alignment had a mean paradoxical
Orthopaedic Surgeon,
Department of Biomedical force which was 6 lb higher in the lateral compartment than those with in-range alignment.
Engineering
None of the measurements of alignment of the limb, knee and components predicted the
University of California, Davis,
Davis, California 95616, USA. force in the medial or lateral compartment.
M. L. Hull, PhD, Professor of Conclusion
Engineering, Department of
Mechanical Engineering, Although kinematically aligned TKA has a high proportion of varus or valgus outliers using
Department of Biomedical mechanically aligned criteria, the intra-operative forces in the medial and lateral
Engineering, Department of
Orthopaedic Surgery compartments of patients with outlier alignment were comparable with those with in-range
University of California, Davis, alignment, with no evidence of overload of the medial or lateral compartment of the knee.
USA, Davis, California 95616
Correspondence should be sent Cite this article: Bone Joint J 2017;99-B:1319–28.
to T. J. Shelton; email:
trevorjshelton@gmail.com The principle of mechanically-aligned total mechanically aligned criteria (Table I). The
knee arthroplasty (TKA) is that durability of alignment of the components and the limb may
©2017 The British Editorial
Society of Bone & Joint the components is achieved by referencing be related using the hip-knee-ankle (HKA)
Surgery them at the time of implantation to the angle, the proximal medial tibial angle
doi:10.1302/0301-620X.99B10.
BJJ-2017-0066.R1 $2.00 mechanical axis of the femur and tibia in the (PMTA) and distal lateral femoral angle
coronal plane.1-6 Target ranges for varus and (DLFA) (Fig. 1). The alignment of the compo-
Bone Joint J
2017;99-B:1319–28. valgus have been described by Parratte et al6 nents and the knee may be measured using the
Received 16 January 2017; for the limb and components, and by Ritter et al5 tibiofemoral angle (TFA), tibial component angle
Accepted after revision 23 June
2017 for the knee and components, based on (TCA) and femoral component angle (FCA).
VOL. 99-B, No. 10, OCTOBER 2017 1319
1320 T. J. SHELTON, A. J. NEDOPIL, S. M. HOWELL, M. L. HULL
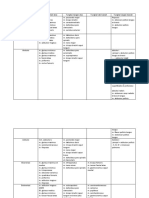
Table I. Range of measurements that categorise the alignment of the limb, knee and components as in-range, varus
outlier and valgus outlier according to mechanical alignment criteria
In-range category Varus outlier category Valgus outlier category
Measurements of limb and component
alignment1
Hip-knee-ankle angle 0° (SD, 3o) < -3o > 3o
Proximal medial tibial angle 87o to 93o < 87o > 93o
Distal lateral femoral angle 87o to 93o > 93o < 87o
Measurements of knee and component
alignment2
Tibiofemoral angle 2.5o to 7.4o < 2.5o > 7.4o
Tibial component angle > 0o < 0o
Femoral component angle 1.9o to 8o < 1.9o > 8o
Parratte et al provided in-range and outlier measures for limb and component alignment. Ritter et al5 provided in-range
6
and outlier measures for knee and component alignment
Hip knee ankle angle Proximal medial tibia angle Distal lateral femoral angle
Fig. 1a
Tibiofemoral angle Tibial component angle Femoral component angle
Fig. 1b
Composite images showing measurements of: a) alignment of the limb and components and; b) alignment of the
knee and components. The hip-knee-ankle angle is the angle between a line connecting the mechanical axes (MA) of
the femur and tibia. The proximal medial tibial angle is that between the tibial joint line and the MA of the tibia. The
distal lateral femoral angle is that between the femoral joint line and the MA of the femur. The tibiofemoral angle is
that between the anatomical axes (AA) of the femur and tibia. The tibial component angle is that between a line per-
pendicular to the proximal tibial joint line and the AA of the tibia. The femoral component angle is that between a line
perpendicular to the distal femoral joint line and the AA of the femur.
Computer-assisted navigation, robotics and patient specific the knee between those whose mechanical alignment is
instrumentation have been developed in order to achieve within the range or is an outlier.2,6,8
mechanical alignment within these ranges in order to Kinematic alignment is a surgical technique that closely
improve the durability and function of the components.7 restores the native alignment of the limb and distal femoral
However, long-term follow-up studies have not shown any and proximal tibial joint lines.9-14 There have been three
differences in the survival of the components or function of meta-analyses, three randomised trials and a national
THE BONE & JOINT JOURNAL
DO VARUS OR VALGUS OUTLIERS HAVE HIGHER FORCES IN THE MEDIAL OR LATERAL COMPARTMENTS 1321
Table II. Comparisons of clinical characteristics, pre-operative conditions, function for patients in the present study and two studies
of kinematically aligned total knee arthroplasty with three- and six-year follow-up.11,12
Parameters Present study (n = 67) Three-year study (n = 215) Six-year study (n = 219) p-value
Clinical characteristics
Age (yrs) 69 (SD 7 A) 69 (SD 10 A) 74 (SD 10 B) < 0.0001
Gender (male) (%) 33 (49) 87 (41) 82 (39) NS (0.2817)
Body mass index (kg/m2) 29 (SD 5 A) 30 (SD 5 A,B) 31 (SD 6 B) 0.0643
Pre-operative knee conditions
Knee extension (°) 11 (SD 7 A) 8 (SD 8 B) 10 (SD 8 A) 0.0031
Knee flexion (°) 111 (SD 11) 114 (SD 13) 113 (SD 13) NS (0.2232)
Valgus (-)/Varus (+) Deformity (°) 1 (SD 13 A) -2 (SD 8 B) -1 (SD 6 A, B) 0.0061
Pre-operative function
Oxford knee score 23 (SD 8 A) 20 (SD 8 B) 18 (SD 8 B) 0.0002
For each parameter means annotated with a different letter ( ) are significantly different from p < 0.05; like letters (either A-A or A-AB)
A, B
indicate no difference between columns whereas different letters (A-B) indicate significant differences
SD, standard deviation; NS, non-significant
multicentre study which have shown that patients whose II). A post hoc analysis had compared patients in the pre-
components are introduced with kinematic alignment have sent study with those in two representative studies11,12 of
significantly better relief of pain, function, range of flexion kinematically aligned TKAs and showed no clinically sig-
and have a more normal feeling knee joint when compared nificant differences in age, proportion of women, body
with those whose components are introduced with mechan- mass index, pre-operative extension, flexion, varus or val-
ical alignment.9,10,15-21 Two randomised trials have shown gus deformities and the Oxford Knee Score. The indications
similar clinical outcomes between the two forms of align- for TKA included disabling symptoms from the knee which
ment.22,23 had not resolved following conservative treatment, radio-
Soft-tissue imbalance accounts for 35% of early revision graphic evidence of Kellgren-Lawrence Grade II to IV
TKAs in the United States and may present as instability or arthritic changes or osteonecrosis, any severity of varus or
stiffness as well as high compressive forces in the tibial valgus deformity as measured when non-weight-bearing
compartments, leading to local overload, loosening and with a goniometer and any severity of flexion contracture.
wear of the insert.24-26 Recently, it has become possible to Exclusion criteria included those undergoing a revision
assess the effect of the bone cuts on ligament balance intra- TKA and those with an inflammatory arthropathy.
operatively during passive flexion-extension movement of All patients were treated with a posterior cruciate liga-
the components and by measuring the compression force in ment (PCL) retaining (CR) primary TKA by a single sur-
the medial and lateral compartments with an instrumented geon (SMH) using a midvastus approach (Vanguard CR;
tibial insert.27 Kinematic alignment can allow outlier varus Zimmer Biomet, Warsaw, Indiana). Kinematic alignment
and valgus mechanical alignment (Table I).10,11,28,29 It is not was performed using a calipered technique with manual
known, however, whether patients with outlier varus or instruments without a soft-tissue release.10,12 Five intra-
valgus kinematic alignment have higher compartment operative quality assurance checks aligned the components
forces than those with in-range alignment. to the restored joint line of the knee. The first minimised
We conducted a retrospective review of patients treated flexion of the femoral component by positioning the start-
with a kinematically aligned TKA asking: (1) what propor- ing hole for the intramedullary positioning rod midway
tion of patients have outlier varus or valgus alignment of between the top of the intercondylar notch and aligning it
the limb, knee and components, based on mechanical crite- parallel to the anterior femoral cortex.30 The second set the
ria?; (2) do patients with outlier varus or valgus alignment femoral component relative to the native tibiofemoral artic-
have higher forces in the medial or lateral compartments ular surface using a caliper and adjusting the thickness of
than those with in-range alignment? and; (3) do measure- the distal and posterior femoral resections to within stand-
ments of alignment of the limb, knee and component pre- ard deviation (SD) 0.5 mm of the thickness of the condyles
dict the forces in the medial and lateral compartments? of the femoral component after compensating for cartilage
wear and the bone cut.28 The third set the rotation of the
Patient and Methods tibial component parallel to the flexion-extension plane of
This study is a retrospective review of patients who under- the knee by aligning the anteroposterior axis of the tibial
went primary kinematically aligned TKA with intra- component parallel to the flexion-extension plane of the
operative measurements of the forces in the medial and lat- knee by rotating the component parallel to a line drawn
eral compartments. A total of 67 patients were identified overlying the axis of the elliptical shape of the lateral tibial
from 148 consecutive primary kinematically aligned TKAs condyle.31 The fourth set the tibial component relative to
performed between July 2016 and November 2016 (Table the varus-valgus angle of the native tibial joint line using a
VOL. 99-B, No. 10, OCTOBER 2017
1322 T. J. SHELTON, A. J. NEDOPIL, S. M. HOWELL, M. L. HULL
caliper to measure the thickness of the medial and lateral cycle with three levels (cycle one, two, three). The ICCs for
tibial condyles at the base of the tibial spines and adjusting the force in the medial compartment were 0.95 at full
the tibial resection until the varus-valgus laxity with trial extension, 0.96 at 45° and 0.97 at 90° of flexion, and the
components was negligible in full extension, which repli- force in the lateral compartment was 0.89 at full extension,
cates the laxity of the native knee in full extension.32 0.82 at 45° and 0.96 at 90° of flexion. Of the six analyses,
Removal of posterior osteophytes without release of the intra-observer repeatability was excellent in four and good
posterior cruciate ligament allowed correction of a flexion in two.
contracture to full extension. Contractures of > 30° occa- Continuous variables were reported as mean with SD and
sionally required release of the posterior capsule from the range. Discrete variables were reported as numbers and
femur but did not require additional resection of distal fem- proportions (percentage). The force in each compartment
oral bone. The final quality assurance check set the tibial was recorded as the mean of the forces at full extension, 45°
component relative to the slope of the native tibial joint line and 90° of flexion.38 For each measurement of alignment, a
by adjusting the flexion-extension of the tibial resection single factor ANOVA determined whether the forces in the
until measurement of the offset of the anterior tibia from medial and lateral compartments were different between
the distal medial femoral condyle with trial components patients with outlier varus, outlier valgus and in-range
matched that of the knee at the time of exposure and the alignment. When there was a significant difference, a post
passive rotation of the tibia on the femur had a mean of hoc Tukey’s test was used to determine which categories of
14°, which replicates the mean laxity of the native knee in alignment were different. A linear regression analysis was
90° of flexion.12,32,33 Indicators of alignment such as the used to compute the coefficient of determination (r2) to
femoral and tibial mechanical axes, the transepicondylar determine whether the measurements of the HKA angle,
axis and the border of the tibial tubercle are not used when PMTA, DLFA, TFA, TCA and FCA predicted the force in
performing kinematic alignment.34 All components were the medial and lateral compartments. Computations were
cemented. The thickness of the tibial insert was selected and performed with software (JMP, Cary, North Carolina).
opened but not implanted at this stage. Statistical significance was set at p < 0.05.
An instrumented tibial insert that matched the thickness
of the selected insert was placed in the tibial baseplate Results
(Verasense, Orthosensor Inc., Dania Beach, Florida). The Many patients treated with a kinematically aligned TKA
tablet screen that displayed the forces in the medial and lat- had outlier varus or valgus mechanical alignment (Figs 2 to
eral compartments in pounds was rotated away from the 5); the proportion was 16% and 24% for the HKA angle,
view of the surgeon. Towel clips were applied proximal and 55% and 0% for the PMTA, 0% and 57% for the DLFA,
distal to the patella to close the extensor mechanism provi- 25% and 12% for the TFA, 100% and 0% for the TCA and
sionally. One hand of the surgeon lifted the posterior thigh 0% and 64% for the FCA.
to flex the knee while the dorsum of the other hand sup- In general, patients with outlier varus or valgus align-
ported the heel so as not to compress or rotate the limb. The ment did not have higher forces in the medial or lateral
knee was passively cycled from full extension to full flexion compartments than those aligned in-range (Table III).
three times to precondition the knee. A video camera on a Those with outlier varus and valgus alignment of the HKA
smartphone simultaneously recorded the forces on the tab- angle, PMTA, and DLFA did not have different mean forces
let screen and the flexion of the knee during three cycles of in the medial and lateral compartments from those aligned
passive movement. in-range (p = 0.2642 to 0.9512) (Figs 2 and 3). Patients
On the day of discharge, each patient had an anteropos- with outlier varus and valgus alignment of the TFA and
terior rotationally controlled CT scanogram of the limb, FCA did not have different mean forces in the medial
with the patient supine and non-weight-bearing to mimic compartment from those aligned in-range (p = 0.4596 to
the intra-operative alignment.11,12 The HKA angle, PMTA, 0.8191) (Fig. 4). Those with outlier varus alignment of the
DLFA, TFA, TCA, and FCA had previously been validated TFA had a mean paradoxical force of 11 lbs (SD 11) in the
using an open source medical image viewer (Horos; Horos lateral compartment that was 6 lbs greater than the mean of
Project) (Fig. 1).1,5,6,35-37 those aligned in-range 5 lbs (SD 5) (p = 0.0314) and not
The study had institutional ethical approval (993987-1). significantly different from the mean of those with outlier
Statistical analysis. In order to quantify intra-observer valgus alignment 7 lbs (SD 9). (Fig. 5). Patients with outlier
repeatability of the measurements of the forces in the varus and valgus alignment of the FCA did not have
medial and lateral compartments, one surgeon (SMH) pas- significantly different mean forces in the lateral compart-
sively flexed and extended the knee three times on 15 ran- ment from those aligned in-range (p = 0.5225). All patients
domly selected patients. A single factor analysis of variance had outlier varus alignment of the TCA. However, the
(ANOVA) with repeated measures computed the intraclass mean forces in the medial and lateral compartments in
correlation coefficient (ICC) for the force in the medial and these patients were not significantly different from those
lateral compartments at full extension, 45° and 90° of flex- patients with in-range alignment of the HKA angle, PMTA,
ion. The factor was the cycle of passive flexion-extension DLFA, and FCA (p = 0.4596 to 0.8191).
THE BONE & JOINT JOURNAL
DO VARUS OR VALGUS OUTLIERS HAVE HIGHER FORCES IN THE MEDIAL OR LATERAL COMPARTMENTS 1323
Table III. Lists of the forces in the medial and lateral compartments for the measurements of alignment of the limb, knee and components for patients
categorised as in-range, varus outlier, or valgus outlier according to mechanical alignment criteria
Medial compartment force (lbs) Lateral compartment force (lbs)
In-range Varus outlier Valgus outlier In-range Varus outlier Valgus outlier
Measurements of limb and
component alignment
Hip-knee-ankle angle 21 (SD 18; 0 to 68) 19 (SD 18; 0 to 58) 21 (SD 18; 0 to 62) 7 (SD 9; 0 to 36) 5 (SD 5;0 to 12) 10 (SD 6;2 to 21)
Proximal medial tibial angle 21 (SD 17; 0 to 59) 21 (SD 19; 0 to 68) - 8 (SD 8; 0 to 28) 6 (SD 7;0 to 36) -
Distal lateral femoral angle 21 (SD 17; 0 to 59) - 20 (SD 18; 0 to 68) 7 (SD 8; 0 to 36) - 8 (SD 7; 0 to 28)
Measurements of knee and
component alignment
Tibiofemoral angle 21 (SD 19; 0 to 68) 19 (SD 14; 0 to 48) 23 (SD 15; 1 to 46) 5 (SD 5A; 0 to 18) 11 (SD 11B; 0 to 36) 9 (SD 7 A,B; 0 to 21)
Tibial component angle - 21 (SD 18; 0 to 68) - - 7 (SD 8;0 to 36) -
Femoral component angle 19 (SD 17; 0 to 59) - 22 (SD 18; 0 to 68) 6 (SD 7; 0 to 28) - 8 (SD 8; 0 to 36)
For each parameter means annotated with a different letter (A, B) are significantly different from p < 0.05; like letters (either A-A or A-AB) indicate no
difference between columns whereas different letters (A-B) indicate significant differences
SD, standard deviation
80 Medial tibial compartment forces (lbs) 80 80
Medial tibial compartment forces (lbs)
Medial tibial compartment forces (lbs)
70 70 70
60 60 60
50 50 50
40 40 40
30 30 30
20 20 20
10 10 10
0 0 0
n = 40 n = 11 n = 16 n = 30 n = 37 n = 29 n = 38
-10 -10 -10
In range Varus outlier Valgus outlier In range Varus outlier In range Valgus outlier
(-3° to 3°) (< 3°) (> 3°) (87° to 93°) (< 87°) (87° to 93°) (< 87°)
Fig. 2a Fig. 2b Fig. 2c
Quantile box-plots and scanograms showing the force in the medial compartment and the number (n) of patients with in-range and varus and valgus
outlier alignment of the hip-knee-ankle angle (a), proximal medial tibial angle (b) and distal lateral femoral angle (c) after kinematically aligned total
knee arthroplasty. For each mechanical alignment, the force in the medial compartment was not significantly different between patients grouped
according to outlier and in-range categories.
Measurements of the HKA angle, PMTA, DLFA, TFA, sibility that it might have more patients with outlier varus
TCA, and FCA did not predict the force in the medial or the and valgus alignment and be associated with high intra-
lateral compartment (r2 ranged from 0.0017 to 0.0581). operative forces in the medial and lateral compartments of
the knee, suggesting malalignment.
Discussion The main findings of our study were that patients treated
Kinematically aligned TKA restores the native alignment of with kinematically aligned TKA had a high proportion of
the limb rather than a neutral mechanical axis4,10,11,28,29,39 outlier varus and valgus alignment of the limb, knee, and
and because this alignment uses a different target and dif- components according to mechanically aligned criteria.
ferent bone cuts than mechanical alignment, there is a pos- Secondly, those with outlier varus or valgus alignment
VOL. 99-B, No. 10, OCTOBER 2017
1324 T. J. SHELTON, A. J. NEDOPIL, S. M. HOWELL, M. L. HULL
80 80 80
Lateral tibial compartment forces (lbs)
Lateral tibial compartment forces (lbs)
Lateral tibial compartment forces (lbs)
70 70 70
60 60 60
50 50 50
40 40 40
30 30 30
20 20 20
10 10 10
0 0 0
n = 40 n = 11 n = 16 n = 30 n = 37 n = 29 n = 38
-10 -10 -10
In range Varus outlier Valgus outlier In range Varus outlier In range Valgus outlier
(-3° to 3°) (< 3°) (> 3°) (87° to 93°) (< 87°) (87° to 93°) (< 87°)
Fig. 3a Fig. 3b Fig. 3c
Quantile box-plots and scanograms showing the force in the lateral compartment and the number (n) of patients with in-range and varus and valgus
outlier alignment of the hip-knee-ankle angle (a), proximal medial tibial angle (b), and distal lateral femoral angle (c) after kinematically aligned total
knee arthroplasty. For each mechanical alignment, the force in the lateral compartment was not significantly different between patients grouped
according to outlier and in-range categories
generally did not have higher forces in the medial and lat- The proportion of patients treated with a kinematically
eral compartments than those with in-range alignment. aligned TKA with outlier varus and valgus alignment of the
Thirdly, measurements of alignment of the limb, knee and limb, knee and components as determined by mechanically
components did not predict the forces in the medial or lat- aligned criteria was generally higher than in those treated
eral compartments. with a mechanically aligned TKA (Table IV).5,6,37,42 For the
The study has limitations. First, our results represent the HKA angle, the proportion of patients with a kinematically
use of one design of PCL retaining (CR) TKA and may not aligned TKA who have outlier valgus alignment was three
be applicable to other designs such as PCL substituting times higher than with a mechanically aligned TKA. The
(posterior stabilised) TKAs, which have higher forces in the proportion of patients with a kinematically aligned TKA
lateral compartment.38 Secondly, the measurements of non- who have outlier varus alignment of the PMTA of 55% and
weight-bearing intra-operative forces in the medial and lat- outlier valgus alignment of the DLFA of 57% were both
eral compartments and post-operative alignment might dif- higher than those for a mechanically aligned TKA of 6%
fer from weight-bearing measurements post-operatively. and 3% respectively. For the TCA, the proportion of kine-
The weight-bearing status should be consistent when matically aligned patients with outlier varus alignment of
making measurements of the forces intra-operatively and 100% was higher than in those with a mechanically aligned
the alignment post-operatively. We measured the intra- TKA of 18%. For the FCA, the proportion of patients with
operative compartment forces during passive movement a kinematically aligned TKA with outlier valgus alignment
of the knee and the post-operative alignment on non- of 64% was higher than in those with a mechanically
weight-bearing CT scanograms with care so as not to aligned TKA of 8%. As kinematic alignment has a high
apply manual compression across the knee. Even though proportion of outlier varus and valgus alignment and
intra-operative and weight-bearing post-operative forces because the patients with outlier alignment had the same
in the compartments might differ, there is value in meas- low forces in the medial and lateral compartments as those
uring these forces intra-operatively as they predict post- with in-range alignment, the criteria for mechanical align-
operative function.38,40,41 ment of categorising the alignment of the limb, knee and
THE BONE & JOINT JOURNAL
DO VARUS OR VALGUS OUTLIERS HAVE HIGHER FORCES IN THE MEDIAL OR LATERAL COMPARTMENTS 1325
80 80 80
Medial tibial compartment forces (lbs)
Medial tibial compartment forces (lbs)
Medial tibial compartment forces (lbs)
70 70 70
60 60 60
50 50 50
40 40 40
30 30 30
20 20 20
10 10 10
0 0 0
n = 42 n = 17 n=8 n = 67 n = 24 n = 43
-10 -10 -10
In range Varus outlier Valgus outlier Varus outlier In range Valgus outlier
(2.5° to 7.4°) (< 2.5°) (> 7.4°) (< 0°) (1.9° to 8°) (8° or >)
Fig. 4a Fig. 4b Fig. 4c
Quantile box-plots and scanograms showing the force in the medial compartment and the number (n) of patients with in-range and varus and valgus
outlier alignment of the tibiofemoral angle (TFA), tibial component angle (TCA) and femoral component angle (FCA) after a kinematically aligned
total knee arthroplasty. For the TFA and FCA, the mean force in the compartment was not significantly different between patients grouped according
to outlier and in-range categories. A statistical analysis could not be performed for the TCA as all patients had varus outlier alignment.
components as a varus and valgus outlier should not be of varus loosening of 0% and of posterior subsidence or
applied to kinematic alignment. wear of the tibial component of 0.2% at two- to nine-year
One clinical benefit of a kinematically ligned TKA is that follow-up, and an incidence of catastrophic failure of 0% at
low forces in the medial and lateral compartments were three years and 2.5% at six years post-operatively.11,12,44
achieved without soft-tissue release, by restoring the native Finally, the mean intra-operative compartment forces in the
alignment of the limb, knee and joint lines. The forces in the present study were lower than the mean in vitro forces
medial and lateral compartments of a kinematically aligned predicted by a computer simulation of a kinematically
TKA were generally lower than those in a mechanically aligned TKA.16,45
aligned TKA in whom soft-tissue releases were Positioning components to restore the native alignment
performed.27,38,41,43 In our study, the mean force in the of the limb, knee and joint lines, which is the target of kin-
medial and lateral compartments of 17 lbs (SD 21) and 8 lbs ematic alignment, might explain the poor prediction of the
(SD 7) respectively, of a kinematically aligned TKA, were forces in the medial and the lateral compartments by meas-
three to six times lower than those of 50 lbs (SD 71) and urements of the post-operative HKA angle, PMTA, DLFA,
31 lbs (SD 44), respectively, reported for a mechanically TFA, TCA, and FCA. An in vitro study showed that the
aligned TKA when these forces were in full extension, 45° magnitude and the range of the sum of the forces in the
and 90° of flexion.38 medial and lateral compartments were small and narrow,
A second benefit is that low intra-operative between 1 lb and 26 lbs in extension after kinematically
compartment forces are associated with a low risk of aligned femoral and tibial components were introduced in
overload, wear of the insert and tibial loosening24,26 and 13 normal cadaveric knees.Low compartment forces in full
with better outcomes and function, than high intra-opera- extension are notable because full extension is the position
tive compartment forces.27,38,41,43 A third benefit is that with the least laxity and consequently the highest compart-
low compartment forces explain the high rate of implant ment forces.32,46 Forces in the compartments that are small
survival for kinematically aligned TKAs with an incidence and vary little between patients might not be sensitive
VOL. 99-B, No. 10, OCTOBER 2017
1326 T. J. SHELTON, A. J. NEDOPIL, S. M. HOWELL, M. L. HULL
80 80 80
Lateral tibial compartment forces (lbs)
Lateral tibial compartment forces (lbs)
Lateral tibial compartment forces (lbs)
70 70 70
A A
60 B B 60 60
50 50 50
40 40 40
30 30 30
20 20 20
10 10 10
0 0 0
n = 42 n = 17 n=8 n = 67 n = 24 n = 43
-10 -10 -10
In-range Varus outlier Valgus outlier Varus outlier In range Valgus outlier
(2.5° to 7.4°) (< 2.5°) (> 7.4°) (< 0°) (1.9° to 8°) (8° or >)
Fig. 5a Fig. 5b Fig. 5c
Quantile box-plots and scanograms showing the force in the lateral compartment and the number (n) of patients with in-range and varus and valgus
outlier alignment of the tibiofemoral angle (TFA) (a), tibial component angle (TCA) (b) and femoral component angle (FCA) (c) after a kinematically
aligned TKA. For the TFA, the mean force in the lateral compartment was 11 lbs (standard deviation (SD) 11), in those with varus outlier alignment
(A) it was 5lbs (SD 5) greater than those aligned in-range (B) (p < 0.0314) and was not different from the 7lbs (SD 9) of force in those with valgus
outlier alignment (A, B). A statistical analysis could not be performed for the TCA as all the patients had a varus outlier alignment. For the FCA, the
mean force in the lateral compartment was not significantly different between patients grouped according to outlier and in-range categories.
Table IV. Comparison of studies of mechanical and kinematic alignment that report the proportion (%) of patients with a varus or
valgus outlier alignment for measurements of the limb, knee and components
Study
Method of HKA angle HKA angle PMTA varus PMTA valgus DLFA varus DLFA valgus
alignment varus outlier valgus outlier outlier outlier outlier outlier
6
Parratte et al Mechanical 10 7
Luyckx et al37 Mechanical 26 8
Magnussen et al42 Mechanical 6 1 4 3
Present Study Kinematic 16 24 55 0 0 57
Method of TFA varus TFA valgus TCA varus TCA valgus FCA varus FCA valgus
alignment outlier outlier outlier outlier outlier outlier
Ritter et al5 Mechanical 17 12 18 0 26 8
Present study Kinematic 25 12 100 0 0 64
HKA, hip-knee-ankle; PMTA, proximal medial tibial angle; DLFA, distal lateral femoral angle; TFA, tibiofemoral angle; TCA, tibial compo-
nent angle; FCA, femoral component angle
enough to predict alignment of the PMTA, DLFA, and ponent set in 3° more valgus from the native tibial joint
HKA angles. Patients with a post-operative PMTA of 0°, 3° line. Placement of the tibial component in 1° and 2° more
and 6° varus after kinematic alignment that matches the valgus than the native tibial joint line increases the force in
native pre-operative PMTA should have small comparable the medial compartment in extension by 18 lbs and 54 lbs
compartment forces that differ within a narrow range. respectively, when soft tissues are left intact.47,48 Hence, the
However, a patient with a decrease in the post-operative poor prediction of forces in the medial and the lateral com-
PMTA of 0° varus after kinematic alignment, from a native partments by the measurements of alignment suggests that
pre-operative PMTA of 3° varus, would have a tibial com- the intra-operative quality assurance checks of adjusting
THE BONE & JOINT JOURNAL
DO VARUS OR VALGUS OUTLIERS HAVE HIGHER FORCES IN THE MEDIAL OR LATERAL COMPARTMENTS 1327
the thicknesses of the distal femoral and proximal tibial 13. Miller EJ, Pagnano MW, Kaufman KR. Tibiofemoral alignment in posterior stabi-
resections set the femoral and tibial components relative to lized total knee arthroplasty: Static alignment does not predict dynamic tibial plateau
loading. J Orthop Res 2014;32:1068–1074.
the native joint lines and restored the native alignment of 14. Ji HM, Han J, Jin DS, Seo H, Won YY. Kinematically aligned TKA can align knee
the limb and knee. joint line to horizontal. Knee Surg Sports Traumatol Arthrosc 2016;24:2436–2441.
In conclusion, categorising the alignment of the limb, knee 15. Niki Y, Sassa T, Nagai K, et al. Mechanically aligned total knee arthroplasty car-
ries a risk of bony gap changes and flexion-extension axis displacement. Knee Surg
and components as varus and valgus outlier or in-range, Sports Traumatol Arthrosc 2017 February 21. (Epub ahead of print).
according to criteria of mechanical alignment, cannot pre- 16. Nakamura S, Tian Y, Tanaka Y. The effects of kinematically aligned total knee
dict the intra-operative forces in the medial and lateral arthroplasty on stress at the medial tibia: A case study for varus knee. Bone Joint Res
2017;6:43–51.
compartments after a kinematically aligned TKA. These
17. Matsumoto T, Takayama K, Ishida K. Radiological and clinical comparison of kin-
findings do not support the concept of categorising alignment ematically versus mechanically aligned total knee arthroplasty. Bone Joint J 2017;99-
as an outlier when performing this procedure.11,12 B:640–646.
18. Li Y, Wang S, Wang Y, Yang M. Does Kinematic Alignment Improve Short-Term
Functional Outcomes after Total Knee Arthroplasty Compared with Mechanical Align-
Take home message: ment? A Systematic Review and Meta-analysis. J Knee Surg 2017 May 01. (Epub
- Kinematic alignment has a high proportion of varus and ahead of print).
valgus outliers according to mechanical alignment criteria 19. Lee YS, Howell SM, Won YY, et al. Kinematic alignment is a possible alternative
to mechanical alignment in total knee arthroplasty. Knee Surg Sports Traumatol
- Medial and lateral tibial compartment forces of subjects with varus or Arthrosc 2017 April 24. (Epub ahead of print)
valgus outlier alignment were comparable with those with in-range 20. Courtney PM, Lee GC. Early Outcomes of Kinematic Alignment in Primary Total
alignment. Knee Arthroplasty: A Meta-Analysis of the Literature. J Arthroplasty 2017;32:2028–
2032.
Author contributions: 21. Nam D, Nunley RM, Barrack RL. Patient dissatisfaction following total knee
T. J. Shelton: Study design, Data collection, Data analysis, Writing the paper. replacement: a growing concern? Bone Joint J 2014;96-B(11 Supple A):96–100.
A. J. Nedopil: Study design, Data collection, Data analysis, Writing the paper.
S. M. Howell: Study design, Data collection, Data analysis, Writing the paper. 22. Waterson HB, Clement ND, Eyres KS, Mandalia VI, Toms AD. The early out-
M. L. Hull: Study design, Data collection, Data analysis, Writing the paper. come of kinematic versus mechanical alignment in total knee arthroplasty: a prospec-
tive randomised control trial. Bone Joint J 2016;98-B:1360–1368.
The study was approved by our ethical committee. 23. Young SW, Walker ML, Bayan A, et al. The Chitranjan S. Ranawat Award: No Dif-
No benefits in any form have been received or will be received from a commer- ference in 2-year Functional Outcomes Using Kinematic versus Mechanical Align-
cial party related directly or indirectly to the subject of this article. ment in TKA: A Randomized Controlled Clinical Trial. Clin Orthop Relat Res
2017;475:9–20.
This article was primary edited by S. P. F. Hughes and first proof edited by J. Scott.
24. Kuster MS, Stachowiak GW. Factors affecting polyethylene wear in total knee
arthroplasty. Orthopedics 2002;25(2 Suppl):235–242.
25. Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award
References paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res
1. Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat 2002;404:7–13.
award: is neutral mechanical alignment normal for all patients? The concept of con- 26. Berend ME, Ritter MA, Meding JB, et al. Tibial component failure mechanisms in
stitutional varus. Clin Orthop Relat Res 2012;470:45–53. total knee arthroplasty. Clin Orthop Relat Res 2004;428:26–34.
2. Bonner TJ, Eardley WG, Patterson P, Gregg PJ. The effect of post-operative 27. Gustke KA, Golladay GJ, Roche MW, Elson LC, Anderson CR. A new method for
mechanical axis alignment on the survival of primary total knee replacements after a defining balance: promising short-term clinical outcomes of sensor-guided TKA. J
follow-up of 15 years. J Bone Joint Surg [Br] 2011;93-B:1217–1222. Arthroplasty 2014;29:955–960.
3. Eckhoff DG, Bach JM, Spitzer VM, et al. Three-dimensional mechanics, kinemat- 28. Howell SM, Papadopoulos S, Kuznik KT, Hull ML. Accurate alignment and high
ics, and morphology of the knee viewed in virtual reality. J Bone Joint Surg [Am] function after kinematically aligned TKA performed with generic instruments. Knee
2005;87-A(Suppl 2):71–80. Surg Sports Traumatol Arthrosc 2013;21:2271–2280.
29. Nunley RM, Ellison BS, Zhu J, et al. Do patient-specific guides improve coronal
4. Gu Y, Howell SM, Hull ML. Simulation of total knee arthroplasty in 5° or 7° valgus:
alignment in total knee arthroplasty? Clin Orthop Relat Res 2012;470:895–902.
A study of gap imbalances and changes in limb and knee alignments from native. J
Orthop Res 2016 November 25. (Epub ahead of print). 30. Ettinger M, Calliess T, Howell SM. Does a positioning rod or a patient-specific
guide result in more natural femoral flexion in the concept of kinematically aligned
5. Ritter MA, Davis KE, Meding JB, et al. The effect of alignment and BMI on failure total knee arthroplasty? Arch Orthop Trauma Surg 2017;137:105–110.
of total knee replacement. J Bone Joint Surg [Am] 2011;93-A:1588–1596.
31. Nedopil AJ, Howell SM, Hull ML. Does Malrotation of the Tibial and Femoral
6. Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative Components Compromise Function in Kinematically Aligned Total Knee Arthroplasty?
mechanical axis alignment on the fifteen-year survival of modern, cemented total Orthop Clin North Am 2016;47:41–50.
knee replacements. J Bone Joint Surg [Am] 2010;92-A:2143–2149. 32. Roth JD, Howell SM, Hull ML. Native Knee Laxities at 0 degrees, 45 degrees, and
7. Allen MM, Pagnano MW. Neutral mechanical alignment: Is it Necessary? Bone 90 degrees of Flexion and Their Relationship to the Goal of the Gap-Balancing Align-
Joint J 2016;98-B(1 Suppl A):81–83. ment Method of Total Knee Arthroplasty. J Bone Joint Surg [Am] 2015;97:1678–1684.
8. Vanlommel L, Vanlommel J, Claes S, Bellemans J. Slight under correction fol- 33. Heesterbeek P, Keijsers N, Jacobs W, Verdonschot N, Wymenga A. Posterior
lowing total knee arthroplasty results in superior clinical outcomes in varus knees. cruciate ligament recruitment affects antero-posterior translation during flexion gap
Knee Surg Sports Traumatol Arthrosc 2013;21:2325–2330. distraction in total knee replacement. An intraoperative study involving 50 patients.
Acta Orthop 2010;81:471–477.
9. Calliess T, Bauer K, Stukenborg-Colsman C, et al. PSI kinematic versus non-PSI
34. Howell SM, Hull ML. Kinematic Alignment in Total Knee Arthroplasty. In: Scott S,
mechanical alignment in total knee arthroplasty: a prospective, randomized study.
ed. Insall and Scott Surgery of the Knee Philadelphia: Elsevier, 2017:1784–1796.
Knee Surg Sports Traumatol Arthrosc 2017;25:1743–1748.
35. Colebatch AN, Hart DJ, Zhai G, et al. Effective measurement of knee alignment
10. Dossett HG, Estrada NA, Swartz GJ, LeFevre GW, Kwasman BG. A randomised using AP knee radiographs. Knee 2009;16:42–45.
controlled trial of kinematically and mechanically aligned total knee replacements:
two-year clinical results. Bone Joint J 2014;96-B:907–913. 36. Sabharwal S, Zhao C, Edgar M. Lower limb alignment in children: reference values
based on a full-length standing radiograph. J Pediatr Orthop 2008;28:740–746.
11. Howell SM, Papadopoulos S, Kuznik K, Ghaly LR, Hull ML. Does varus align- 37. Luyckx T, Vanhoorebeeck F, Bellemans J. Should we aim at under correction
ment adversely affect implant survival and function six years after kinematically when doing a total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc
aligned total knee arthroplasty? Int Orthop 2015;39:2117–2124. 2015;23:1706–1712.
12. Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML. Does a kinematically 38. Meneghini RM, Ziemba-Davis MM, et al. Can Intraoperative Sensors Determine
aligned total knee arthroplasty restore function without failure regardless of align- the “Target” Ligament Balance? Early Outcomes in Total Knee Arthroplasty. J Arthro-
ment category? Clin Orthop Relat Res 2013;471:1000–1007. plasty 2016;31:2181–2187.
VOL. 99-B, No. 10, OCTOBER 2017
1328 T. J. SHELTON, A. J. NEDOPIL, S. M. HOWELL, M. L. HULL
39. Gu Y, Roth JD, Howell SM, Hull ML. How Frequently Do Four Methods for 45. Ishikawa M, Kuriyama S, Ito H, et al. Kinematic alignment produces near-normal
Mechanically Aligning a Total Knee Arthroplasty Cause Collateral Ligament Imbal- knee motion but increases contact stress after total knee arthroplasty: A case study
ance and Change Alignment from Normal in White Patients? J Bone Joint Surg [Am] on a single implant design. Knee 2015;22:206–212.
2014;96:101.
46. Roth JD. How Well Does Kinematically Aligned Total Knee Arthroplasty Prevent Clin-
40. Gustke KA, Golladay GJ, Roche MW, et al. Increased satisfaction after total knee ically Important Changes in Passive Knee Function? An In Vitro Biomechanical Study
replacement using sensor-guided technology. Bone Joint J 2014;96-B:1333–1338. of Tibiofemoral Laxities and Contact. Biomedical Engineering. https://search.pro-
41. Jacobs CA, Christensen CP, Karthikeyan T. Greater Medial Compartment Forces quest.com/openview/aef897d8f2a52b0586ac1b547e2d5c2a/1.pdf?pq-orig-
During Total Knee Arthroplasty Associated With Improved Patient Satisfaction and site=gscholar&cbl=18750&diss=y (date last accessed 23 August 2017).
Ability to Navigate Stairs. J Arthroplasty 2016;31(9 Suppl):87–90. 47. Roth JD, Howell SM, Hull ML. Which Malrotations of the Femoral and Tibial Com-
42. Magnussen RA, Weppe F, Demey G, Servien E, Lustig S. Residual varus align- ponents Cause a Clinically Undesirable Change in the Difference in Contact Force
ment does not compromise results of TKAs in patients with preoperative varus. Clin Between the Medial and Lateral Compartments at 0°, 45°, and 90° of Flexion in Total
Orthop Relat Res 2011;469:3443–3450. Knee Arthroplasty? American Academy of Orthopedic Surgeons 2017. https://
43. Gustke KA, Golladay GJ, Roche MW, Elson LC, Anderson CR. Primary TKA www.aaos.org/ (date last accessed 27 June 2017).
patients with quantifiably balanced soft-tissue achieve significant clinical gains 48. Roth JD, Howell SM, Hull ML. How Sensitive Are the Forces in the Tibial Compart-
sooner than unbalanced patients. Adv Orthop 2014;2014:628695. ments and Varus-Valgus Laxities to Varus-Valgus Adjustments of the Tibial Compo-
44. Nedopil AJ, Howell SM, Hull ML. What mechanisms are associated with tibial nent in Kinematically Aligned Total Knee Arthroplasty? Annual Meeting of Orthopedic
component failure after kinematically-aligned total knee arthroplasty? Int Orthop Research Society. http://www.ors.org/2017annualmeeting/ (date last accessed 27
2017;41:1561–1569. June 2017).
THE BONE & JOINT JOURNAL
You might also like
- Orthodontically Driven Corticotomy: Tissue Engineering to Enhance Orthodontic and Multidisciplinary TreatmentFrom EverandOrthodontically Driven Corticotomy: Tissue Engineering to Enhance Orthodontic and Multidisciplinary TreatmentFederico BrugnamiNo ratings yet
- Ahn 2015Document9 pagesAhn 2015osmann52No ratings yet
- The Journal of ArthroplastyDocument5 pagesThe Journal of Arthroplastyosman gorkemNo ratings yet
- Bue Cking 2015Document5 pagesBue Cking 2015Ashish UpadhyayNo ratings yet
- Stiehl 2001Document9 pagesStiehl 2001GERARDO TORRES RUIZNo ratings yet
- Radiographic Evaluation in Hip and Knee Replacement - HNRDocument29 pagesRadiographic Evaluation in Hip and Knee Replacement - HNRSri MahadhanaNo ratings yet
- Kim 2007Document6 pagesKim 2007GERARDO TORRES RUIZNo ratings yet
- Total Knee Replacement Wear DuringDocument8 pagesTotal Knee Replacement Wear DuringRob GNNo ratings yet
- PathomechanicsDocument8 pagesPathomechanicsMike B AndersonNo ratings yet
- 14 - Factors Affectiong Rom ..... 3-10Document6 pages14 - Factors Affectiong Rom ..... 3-10dfrasNo ratings yet
- First Metatarsal Frontal RotationDocument6 pagesFirst Metatarsal Frontal RotationBrianNo ratings yet
- Does Use of A Variable Distal Femur Resection Angle Improve Radiographic Alignment in Primary Total Knee ArthroplastyDocument6 pagesDoes Use of A Variable Distal Femur Resection Angle Improve Radiographic Alignment in Primary Total Knee ArthroplastyAsmed El SalugNo ratings yet
- In Vivo Knee Moments and Shear After Total Knee ArthroplastyDocument7 pagesIn Vivo Knee Moments and Shear After Total Knee ArthroplastyJobin VargheseNo ratings yet
- Yamazaki 2021Document6 pagesYamazaki 2021Nelson Guerra ZabaletaNo ratings yet
- Intramedullary Control of Distal Femoral Resection Results in Precise Coronal Alignment in TKADocument7 pagesIntramedullary Control of Distal Femoral Resection Results in Precise Coronal Alignment in TKAAsmed El SalugNo ratings yet
- Jurnal 5Document7 pagesJurnal 5JAQUELINENo ratings yet
- Hospital, UK: B-16 Analysis of Knee Kinematics With Computer NavigationDocument1 pageHospital, UK: B-16 Analysis of Knee Kinematics With Computer NavigationMaria BrehaNo ratings yet
- A Computer-Assisted Navigation Technique For Complex Primary Knee Arthroplasty With Intra-Articular Bone Defect and Instability: A Case Report and Literature ReviewDocument7 pagesA Computer-Assisted Navigation Technique For Complex Primary Knee Arthroplasty With Intra-Articular Bone Defect and Instability: A Case Report and Literature ReviewNorawee WainipitapongNo ratings yet
- A Simple Method For Accurate Rotational Positioning of The Femoral Component in Total Knee ArthroplastDocument8 pagesA Simple Method For Accurate Rotational Positioning of The Femoral Component in Total Knee ArthroplastShivamNo ratings yet
- Learning From The Learning Curve in Tota PDFDocument7 pagesLearning From The Learning Curve in Tota PDFcarl marxNo ratings yet
- 1 s2.0 S2211568418302286 MainDocument9 pages1 s2.0 S2211568418302286 Mainketrin marokoNo ratings yet
- The Advantages of Circular External FixaDocument6 pagesThe Advantages of Circular External FixaPriscilla PriscillaNo ratings yet
- Laprade 2012Document11 pagesLaprade 2012Aaron BNo ratings yet
- Review-THE ROLE OF KNEE BRACES AFTER ACL LESIONDocument10 pagesReview-THE ROLE OF KNEE BRACES AFTER ACL LESIONAndreea TudoseNo ratings yet
- Limited Rotation of The 3-44Document6 pagesLimited Rotation of The 3-44HAKAN PARNo ratings yet
- Anatomy and Bio Mechanics of The KneeDocument15 pagesAnatomy and Bio Mechanics of The KneeaimanshalpyNo ratings yet
- Liu 2019Document7 pagesLiu 2019Aulia Siti NuraininNo ratings yet
- coronal alignment -historical review, future directionDocument6 pagescoronal alignment -historical review, future directionMohan DesaiNo ratings yet
- FUNCTIONAL AND RADIOGRAPHIC SHORT-TERM OUTCOME EVALUATION OF THE TOTAL KNEE ARTHROPLASTY IN PANTI RAPIH HOSPITAL YOGYAKARTA - AZETA ARIF - Final Fellow IHKSDocument39 pagesFUNCTIONAL AND RADIOGRAPHIC SHORT-TERM OUTCOME EVALUATION OF THE TOTAL KNEE ARTHROPLASTY IN PANTI RAPIH HOSPITAL YOGYAKARTA - AZETA ARIF - Final Fellow IHKSazeta_arif5466No ratings yet
- 3 0576.1 GLBL en The Shape Matters Story FINALDocument12 pages3 0576.1 GLBL en The Shape Matters Story FINALAnil Chowadary Anil ChowadaryNo ratings yet
- 10 1016@j Joca 2006 02 024Document7 pages10 1016@j Joca 2006 02 024Roman PopescuNo ratings yet
- Aots 1 PDFDocument5 pagesAots 1 PDFmohan hanumanNo ratings yet
- Significance of Dynamic Mobility in Restoring Vertebral Body Height in VertebroplastyDocument4 pagesSignificance of Dynamic Mobility in Restoring Vertebral Body Height in VertebroplastyRamy ElmasryNo ratings yet
- At 0624Document6 pagesAt 0624DanDezideriuIacobNo ratings yet
- CB Britton03Document10 pagesCB Britton03steigmannNo ratings yet
- Robotic Arm-Assisted Versus Manual Total Hip Arthroplasty A Propensity Score Matched Cohort StudyDocument9 pagesRobotic Arm-Assisted Versus Manual Total Hip Arthroplasty A Propensity Score Matched Cohort StudyShiv KolheNo ratings yet
- Alterations of 3D Acetabular and Lower Limb Parameters in Adolescent Idiopathic ScoliosisDocument8 pagesAlterations of 3D Acetabular and Lower Limb Parameters in Adolescent Idiopathic ScoliosisAren BizdikianNo ratings yet
- Online First: Lower Extremity Muscle Strength After Anterior Cruciate Ligament Injury and ReconstructionDocument11 pagesOnline First: Lower Extremity Muscle Strength After Anterior Cruciate Ligament Injury and ReconstructionDevi MigiekaNo ratings yet
- Journal of Biomechanics: Clare K. Fitzpatrick, Paul J. RullkoetterDocument9 pagesJournal of Biomechanics: Clare K. Fitzpatrick, Paul J. RullkoettermoonNo ratings yet
- The Accuracy of Positioning of A Custom-Made Implant Within A Large Acetabular Defect at Revision Arthroplasty of The HipDocument6 pagesThe Accuracy of Positioning of A Custom-Made Implant Within A Large Acetabular Defect at Revision Arthroplasty of The HipIrina DesyatykhNo ratings yet
- Outcome Assesment of Proximal Fibular Osteotomy in Medial Compartment Knee OsteoarthritisDocument3 pagesOutcome Assesment of Proximal Fibular Osteotomy in Medial Compartment Knee OsteoarthritisPrashant GuptaNo ratings yet
- Slight Femoral Under-Correction Versus Neutral Alignment in Total Knee Arthroplasty With Preoperative Varus Knees: A Comparative StudyDocument8 pagesSlight Femoral Under-Correction Versus Neutral Alignment in Total Knee Arthroplasty With Preoperative Varus Knees: A Comparative Studyfebyan yohanesNo ratings yet
- In Vivo Knee Moments and Shear After TotDocument7 pagesIn Vivo Knee Moments and Shear After TotGERARDO TORRES RUIZNo ratings yet
- It's "ALL" in The Knees: A Review of The Anterolateral LigamentDocument16 pagesIt's "ALL" in The Knees: A Review of The Anterolateral LigamentAlMarcheseNo ratings yet
- Asian Knees - The Size of Tibial Footprint of Anterior Cruciate Ligament and Association With Physical Characteristics in Asian FemalesDocument8 pagesAsian Knees - The Size of Tibial Footprint of Anterior Cruciate Ligament and Association With Physical Characteristics in Asian FemalesfpNo ratings yet
- High Tibial Osteotomy For Osteoarthritis of The KneeDocument6 pagesHigh Tibial Osteotomy For Osteoarthritis of The Kneealyek92No ratings yet
- Surgical Technique For Combined D Wyer Calcaneal Osteotomy and PeronealDocument6 pagesSurgical Technique For Combined D Wyer Calcaneal Osteotomy and PeronealleahbayNo ratings yet
- Effect of Meniscal Loss On Knee Stability After Single-Bundle Anterior Cruciate Ligament ReconstructionDocument9 pagesEffect of Meniscal Loss On Knee Stability After Single-Bundle Anterior Cruciate Ligament Reconstructioni_anitaNo ratings yet
- Scapular Contribution For The End-Range of Shoulder Axial Rotation in Overhead AthletesDocument6 pagesScapular Contribution For The End-Range of Shoulder Axial Rotation in Overhead AthletesJuanma GonzalezNo ratings yet
- Mariconda 2014Document8 pagesMariconda 2014DANILO CARVALHO X-TRAINERNo ratings yet
- The Anatomy of The ACL and Its Importance in ACL ReconstructionDocument6 pagesThe Anatomy of The ACL and Its Importance in ACL Reconstructionlexie beatsNo ratings yet
- Fluoroscopic Analysis of The Kinematics of Deep Exion in Total Knee ArthroplastyDocument4 pagesFluoroscopic Analysis of The Kinematics of Deep Exion in Total Knee Arthroplastyjmhinos4833No ratings yet
- Effect of Foot Rotation On Knee Kinetics and Hamstring Activation in Older Adults With and Without Signs of Knee OsteoarthritisDocument8 pagesEffect of Foot Rotation On Knee Kinetics and Hamstring Activation in Older Adults With and Without Signs of Knee OsteoarthritisDaniel FreireNo ratings yet
- Comparison of The Modified Transtibial Technique, Anteromedial Portal Technique and Outside-In Technique in ACL ReconstructionDocument8 pagesComparison of The Modified Transtibial Technique, Anteromedial Portal Technique and Outside-In Technique in ACL ReconstructionJahid HasanNo ratings yet
- Evaluation of Anterior Oblique Ligament Tension at The Elbow Joint Angleda Cadaver StudyDocument6 pagesEvaluation of Anterior Oblique Ligament Tension at The Elbow Joint Angleda Cadaver StudyDr LAUMONERIENo ratings yet
- Journal of Biomechanics: Josh R. Baxter, Todd J. Hullfish, Wen ChaoDocument5 pagesJournal of Biomechanics: Josh R. Baxter, Todd J. Hullfish, Wen ChaoEma.diazNo ratings yet
- Art 2Document8 pagesArt 2ALEJANDRA GARZÓN CUELLAR.No ratings yet
- The Knee: Parm Johal, Mohammed A. Hassaballa, Jonathan D. Eldridge, Andrew J. PorteousDocument3 pagesThe Knee: Parm Johal, Mohammed A. Hassaballa, Jonathan D. Eldridge, Andrew J. Porteousosman gorkemNo ratings yet
- Jurnal Meniskus Medial Dan Laterall FisioterapiDocument6 pagesJurnal Meniskus Medial Dan Laterall FisioterapiAstrid Nasna LarasatiNo ratings yet
- Ch. 6 Muscular System 2019-Part 2Document95 pagesCh. 6 Muscular System 2019-Part 2icdjpNo ratings yet
- Referat Carpal Tunnel SyndromeDocument25 pagesReferat Carpal Tunnel Syndromegede andreasNo ratings yet
- !emergeortho ProceduresDocument172 pages!emergeortho ProceduresGeorgios Mandelas100% (10)
- Elbow Anatomy: DR Paul Bundi Karau (BSC, MBCHB) Lecturer, Human AnatomyDocument30 pagesElbow Anatomy: DR Paul Bundi Karau (BSC, MBCHB) Lecturer, Human AnatomyGish KioiNo ratings yet
- Effectiveness of Spencer Muscle Energy Technique On Periarthritis ShoulderDocument5 pagesEffectiveness of Spencer Muscle Energy Technique On Periarthritis Shoulderplaboni banerjeeNo ratings yet
- Meniscus TearsDocument29 pagesMeniscus Tearsmaulana ilhamNo ratings yet
- Arthritis: by DR Samra Tahseen Registrar, Radiology LNHDocument86 pagesArthritis: by DR Samra Tahseen Registrar, Radiology LNHAngelic khanNo ratings yet
- Orthopedic DHA MCQDocument18 pagesOrthopedic DHA MCQAsif Newaz91% (11)
- The Shoulder GirdleDocument6 pagesThe Shoulder GirdlekanevwNo ratings yet
- Squat BiomechanicsDocument11 pagesSquat BiomechanicsMarcelopablo7No ratings yet
- Effectiveness of Maitland vs. Mulligan Mobilization Techniques in (Ingles)Document4 pagesEffectiveness of Maitland vs. Mulligan Mobilization Techniques in (Ingles)mauricio castroNo ratings yet
- BioRCI - Electronic Technique GuideDocument16 pagesBioRCI - Electronic Technique GuidematlostNo ratings yet
- Imaging of Sports Injuries in The Foot: James M. LinklaterDocument9 pagesImaging of Sports Injuries in The Foot: James M. Linklaterpjanu86No ratings yet
- Tabel KinesiologiDocument4 pagesTabel KinesiologiMohammad Jofa Rachman PNo ratings yet
- 2019 Lateral Extra-Articular Tenodesis With ACL Reconstruction Demonstrates Better Patient-Reported Outcomes Compared To ACL Reconstruction Alone at 2 Years Minimum Follow-UpDocument9 pages2019 Lateral Extra-Articular Tenodesis With ACL Reconstruction Demonstrates Better Patient-Reported Outcomes Compared To ACL Reconstruction Alone at 2 Years Minimum Follow-Upsumon.huqNo ratings yet
- WhitfieldR PS2016 PostSymposium HandoutsDocument18 pagesWhitfieldR PS2016 PostSymposium Handoutsdeemoney3No ratings yet
- Knee Joint Anatomy & Injuries GuideDocument35 pagesKnee Joint Anatomy & Injuries Guidecode212No ratings yet
- Anatomy, Pathophysiology, Andbiomechanics of Shoulder InstabilityDocument9 pagesAnatomy, Pathophysiology, Andbiomechanics of Shoulder InstabilityDelaram IravaniNo ratings yet
- BRS Gross Anatomy 7th 2012Document506 pagesBRS Gross Anatomy 7th 20126003101008ชวิศ อาภรณ์วิรัตน์No ratings yet
- ACL Rehabilitation ProgressionDocument8 pagesACL Rehabilitation ProgressionTomaž Radko Erjavec ŠnebergerNo ratings yet
- Meniscus Repair Scientific UpdateDocument4 pagesMeniscus Repair Scientific UpdateLarissa GolucciNo ratings yet
- Big Book of Stretch RoutinesDocument21 pagesBig Book of Stretch RoutinesJack0% (1)
- 3.bones of UpperlimbDocument120 pages3.bones of UpperlimbBlessed LoveNo ratings yet
- Penatalaksanaan Fisioterapi Pada Kasus Post Fraktur Clavicula 1/3 Medial Sinistra Di RST Dr. Soedjono MagelangDocument15 pagesPenatalaksanaan Fisioterapi Pada Kasus Post Fraktur Clavicula 1/3 Medial Sinistra Di RST Dr. Soedjono Magelangaraaela 25No ratings yet
- Terrible Triad Injury of The ElbowDocument15 pagesTerrible Triad Injury of The ElbowkenthepaNo ratings yet
- LGS UPPER Extremity FixDocument18 pagesLGS UPPER Extremity FixvirginiaNo ratings yet
- E3 - Tennis Elbow OPDocument3 pagesE3 - Tennis Elbow OPAnonymous qX3Ktq6No ratings yet
- Ankle&fEET Written Procedure-MagsombolDocument2 pagesAnkle&fEET Written Procedure-Magsombolhazell_aseronNo ratings yet
- 7 Minute Rotator Cuff SolutionDocument113 pages7 Minute Rotator Cuff Solutioninstanoodles100% (6)
- Bnorton Soap NotesDocument2 pagesBnorton Soap Notesapi-285530156No ratings yet