Professional Documents
Culture Documents
PR03671
Uploaded by
Dalia ExtrapolisCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PR03671
Uploaded by
Dalia ExtrapolisCopyright:
Available Formats
Update on the Diagnosis and Management of Feline Cholangiohepatitis
Stanley L. Marks, BVSc, PhD, Diplomate ACVIM (Internal Medicine, Oncology), Diplomate ACVN
University of California, Davis, School of Veterinary Medicine
Davis, CA, USA
Two major types of inflammatory liver disease have been described based on histologic features;
cholangiohepatitis (acute and chronic) and lymphocytic portal hepatitis.
Acute Cholangiohepatitis is characterized by infiltration of large numbers of neutrophils into portal areas
of the liver and into bile ducts. Disruption of the periportal limiting plate results in necrosis of hepatocytes
adjacent to portal areas and infiltration of neutrophils into hepatic lobules. Acute cholangiohepatitis may begin as
an ascending bacterial infection within the biliary tract; however, bacteria are only isolated in a few cases.
Organisms include Bacteroides, Actinomyces, E. coli, Clostridia, and alpha hemolytic Streptococcus. Congenital or
acquired abnormalities of the biliary system, including anatomic abnormalities of the gall bladder or common bile
duct and gallstones may predispose to cholangiohepatitis. Inspissation of bile which may cause partial or
complete obstruction of the common bile duct, gall bladder, or intrahepatic bile ducts frequently accompany
cholangiohepatitis and may require treatment before the cholangiohepatitis can be controlled or resolved.
Chronic Cholangiohepatitis is probably a later stage of acute cholangiohepatitis. It is characterized by a
mixed inflammatory infiltrate in portal areas and bile ducts consisting of neutrophils, lymphocytes, and plasma
cells. Unlike acute cholangiohepatitis, bile duct hypertrophy and portal fibrosis are prominent. In terminal stages,
chronic cholangiohepatitis may progress to biliary cirrhosis (also termed sclerosing cholangitis).
Diseases frequently associated with cholangiohepatitis include inflammatory bowel disease and
pancreatitis. Eighty three percent of cats with cholangiohepatitis had concurrent inflammatory infiltrates in the
duodenum and/or jejunum and 50% had pancreatic lesions. This association has lead to the use of the term
“triaditis” to describe affected cats. Inflammatory bowel disease may give rise to retrograde bacterial invasion of
the common bile duct with resultant pancreatitis and cholangiohepatitis. Despite the high incidence of
inflammatory infiltrates in the small intestine, diarrhea is not a frequent finding in cats with cholangiohepatitis.
Lymphocytic Portal Hepatitis appears to be distinct from acute and chronic cholangiohepatitis. It is
characterized by infiltration of lymphocytes and plasma cells, but not neutrophils, into portal areas but not into
bile ducts. Variable degrees of bile duct hypertrophy and fibrosis are present; however, lymphocytic portal
hepatitis does not progress to biliary cirrhosis. Lymphocytic portal hepatitis is a frequent finding in old cats. This
condition is felt to reflect an immune-mediated disease; however, this has not been substantiated to date.
CLINICAL SIGNS
Clinical signs associated with inflammatory liver diseases are variable and nonspecific and are frequently similar
to those associated with hepatic lipidosis. Partial or complete anorexia is the most common, and sometimes the
only, clinical sign. Other less frequently observed clinical signs include weight loss, depression, vomiting,
diarrhea, and fever. Cats with acute cholangiohepatitis tend to be younger (mean age 3.3 years) than cats with
chronic cholangiohepatitis (mean age 9.0 years), lymphocytic portal hepatitis (8.2 years) or hepatic lipidosis
(mean age 6.2 years). Male cats are more frequently affected with acute cholangiohepatitis. Cats with acute
cholangiohepatitis are more acutely and severely ill than cats with most other types of liver disease. Prominent
clinical signs in acute cholangiohepatitis include fever, depression, and dehydration.
Jaundice and altered liver size are frequently the only findings that direct attention to liver disease. In
severe cases, ecchymotic hemorrhages and/or prolonged bleeding from venipuncture sites may occur. Jaundice is
most easily observed in the sclera but may also be observed in the soft palate or under the tongue. When liver size
Copyright © 2003 All Rights Reserved
Waltham USA, Inc
All rights including that of translation into other languages, reserved. Photomechanical reproduction (photocopy, microcopy) of this
publication or parts thereof without written permission from Waltham USA, Inc. is prohibited. The opinions expressed in these proceedings
are those of the authors and not necessarily those of Waltham.
is evaluated radiographically, hepatomegaly is a frequent finding in feline liver disease but cannot be used to
differentiate amongst the various causes.
LABORATORY EVALUATION
Hematologic and biochemical testing are essential to establish a diagnosis of liver disease. Although there are
trends that differentiate inflammatory liver diseases from hepatic lipidosis and hepatic neoplasia, liver cytology
or histopathology is essential to establish a definitive diagnosis. Fasting bile acids is the test that is most
consistently abnormal in all types of inflammatory liver diseases and hepatic lipidosis. Laboratory changes
typically seen with acute cholangiohepatitis include mild neutrophilia and left shift, normal to slight increase in
serum bilirubin and serum alkaline phosphatase (SAP) and a substantial increase in alanine aminotransferase
(ALT). This profile tends to differentiate acute cholangiohepatitis from chronic cholangiohepatitis, hepatic
lipidosis, and hepatic neoplasia. Laboratory changes typical of chronic cholangiohepatitis include substantial
increases in serum bilirubin, SAP, and ALT. Other associated changes may include mild nonregenerative anemia,
hyperglobulinemia, lymphocytosis, and hyperglycemia. Laboratory alterations associated with lymphocytic
portal hepatitis include normal to variably increased serum bilirubin, ALT, and SAP. When all inflammatory liver
diseases are compared to hepatic lipidosis, hepatic lipidosis cases tend to have higher total bilirubin
concentrations, and higher ALT and SAP. The hallmarks of hepatic lipidosis include jaundice, 10-fold or greater
increases in ALT and SAP, without a corresponding increase in gamma glutamyl transferase (GGT). In other
forms of liver disease in cats, increases in GGT tend to parallel increases in SAP.
When the clinical chemistry profile reveals evidence of liver disease, hyperthyroidism should be ruled out.
Hyperthyroid cats frequently have changes in ALT and SAP that may be indistinguishable from those associated
with inflammatory liver diseases. The increased enzyme concentrations normalize with treatment of
hyperthyroidism. Pathologic changes in liver associated with hyperthyroidism have not been well characterized.
LIVER IMAGING
Abdominal ultrasonography is often helpful in evaluation of extrahepatic disorders associated with
cholangiohepatitis. Most cats with acute or chronic cholangiohepatitis or with lymphocytic portal hepatitis have
variable or no detectable alterations in the echogenicity of the hepatic parenchyma. Conversely, most cats with
hepatic lipidosis have hyperechoic hepatic parenchyma. Bile duct abnormalities may be observed in
cholangiohepatitis. These abnormalities include gall bladder and/or common bile duct distention, cholelithiasis,
cholecystitis, and bile sludging. The normal gall bladder is anechoic and appears round in the transverse scan and
pear-shaped in the longitudinal scan. It is important to remember that gallbladder filling occurs normally with
fasting, therefore, caution must be exercised in interpreting gall bladder enlargement in an anorectic or fasting
cat. The common bile duct can usually be seen as an anechoic, tortuous, tubular structure 2 to 4 mm in diameter
with an echogenic wall. Distention of the gall bladder and common bile duct (i.e., greater than 5 mm in diameter)
occurs as a result of cholecystitis, or biliary obstruction. The gall bladder wall may become thickened as a result of
inflammation or edema. The thickened gall bladder wall has a layered or “double-walled” appearance. Bile
sludge within the gall bladder or common bile duct appears echogenic.
LIVER CYTOLOGY/HISTOPATHOLOGY
Liver cytology or tissue biopsy is essential in differentiating inflammatory liver diseases from hepatic lipidosis
and neoplasia. The use of fine needle aspirates eliminates the need for anesthesia and markedly reduces the
chance of hemorrhage. The diagnostic utility of liver cytology is controversial. Several reports indicate that
cytologic evaluation is highly efficient in identifying hepatic lipidosis and hepatic lymphoma; however,
inflammatory liver diseases are more difficult to identify cytologically. Results of another retrospective study,
Copyright © 2003 All Rights Reserved
Waltham USA, Inc
All rights including that of translation into other languages, reserved. Photomechanical reproduction (photocopy, microcopy) of this
publication or parts thereof without written permission from Waltham USA, Inc. is prohibited. The opinions expressed in these proceedings
are those of the authors and not necessarily those of Waltham.
however, indicate poor correlation between liver cytology and histopathology. Cytologically, hepatic lipidosis is
characterized by clusters of hepatocytes in which the cytoplasm is distended with lipid-filled droplets. Malignant
lymphoma cells readily exfoliate and can be diagnosed by cytologic evaluation. Cytologic diagnosis of
inflammatory liver diseases is hampered by blood contamination, which introduces variable numbers of blood
leukocytes into the samples. Therefore, the cytologist is left to determine whether leukocytes are of blood origin
or represent inflammatory lesions within the liver.
Ultrasound-guided aspiration and biopsy techniques more consistently produce diagnostic specimens than
do blind techniques. Ultrasound-guided fine needle aspiration can be used to sample bile as well as hepatic
parenchyma. Such samples can be examined cytologically to look for inflammatory cells and bacteria and can be
cultured to confirm bacterial infections. Optimal evaluation, in a relatively stable patient, would consist of 2 or 3
ultrasound-guided liver biopsies and collection of a bile sample under ultrasound guidance. Touch impressions
of the liver biopsy specimen may be done to produce good quality slides for cytologic evaluation. In a clinically
unstable patient, ultrasound-guided fine needle aspiration is recommended. Sonography can be used to monitor
for excessive hemorrhage 5 to 10 minutes after aspiration or biopsy.
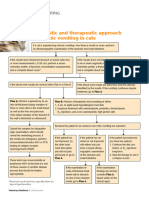
TREATMENT
The major specific therapy for acute and chronic cholangiohepatitis is antibiotics. Surgical intervention has been
recommended if discrete choleliths or complete biliary obstruction is identified. When complete extrahepatic bile
duct obstruction is identified, surgical decompression and biliary-to-intestinal diversion (i.e.,
cholecystoduodenostomy or cholecystojejunostomy) is recommended. Bacterial culture and sensitivity testing of
bile, liver aspirate or biopsy specimens, choleliths, or gall bladder specimens, should be used to select appropriate
antimicrobial agents whenever possible. Antibiotics chosen for treatment of cholangiohepatitis should be excreted
in the bile in active form, and should be active against aerobic and anaerobic intestinal coliforms. Tetracycline,
ampicillin, amoxicillin, erythromycin, chloramphenicol, and metronidazole are excreted in the bile in active form;
however, several of these have significant adverse side effects. Erythromycin is not effective against gram-
negative bacteria, tetracycline is hepatotoxic, and chloramphenicol may cause anorexia. As a result, ampicillin or
amoxicillin combined with clavulanic acid is frequently used. All are broad-spectrum antibiotics, effective against
both gram-negative and gram-positive organisms, and are well tolerated by cats. These drugs may be combined
with metronidazole to extend the spectrum to anaerobes and more coliforms. Treatment with antibiotics for 2
months or longer is recommended.
When cats with chronic cholangiohepatitis fail to respond to antibiotic therapy alone within 2 to 3 weeks,
prednisolone is usually added as an empirical treatment. The anti-inflammatory and immunosuppressive
properties of prednisolone may be beneficial in limiting hepatocellular injury. Additionally, prednisolone may
enhance appetite. An immunosuppressive dose of prednisolone (2.2–4 mg/kg q24h) should be used initially. The
dosage is slowly tapered to an alternate day dose (1–2 mg/kg q48h) for long-term maintenance. Biochemical
values should be monitored prior to each reduction in dosage. If the clinical and biochemical response is
satisfactory, doses as low as 0.5 mg/kg q 48 hours may be sufficient for long-term maintenance. Long-term
corticosteroid treatment is well tolerated by most cats and side effects are usually minimal.
Ursodeoxycholic acid (Actigall) is recommended for cats with all types of inflammatory liver disease. It has
anti-inflammatory, immunomodulatory, and antifibrotic properties as well as increasing fluidity of biliary
secretions. Ursodeoxycholic acid has safely been administered to cats at a dose of 10 to 15 mg/kg q24h PO.
Efficacy has not been established for any type of feline liver disease, but clinical trials in human patients with
hepatitis support improved quality of life. Adverse effects in cats are uncommon and usually limited to mild
diarrhea.
Copyright © 2003 All Rights Reserved
Waltham USA, Inc
All rights including that of translation into other languages, reserved. Photomechanical reproduction (photocopy, microcopy) of this
publication or parts thereof without written permission from Waltham USA, Inc. is prohibited. The opinions expressed in these proceedings
are those of the authors and not necessarily those of Waltham.
Cats with acute cholangiohepatitis require aggressive supportive care. These cats are frequently acutely ill
and have fluid and electrolyte derangements, which should be corrected. Treatment with injectable vitamin K1 (5
mg/cat q 1–2 days IM) can be given if bleeding diatheses develop. Hepatic encephalopathy appears to be
relatively uncommon in cats with acquired liver diseases and is manifest most frequently by excessive salivation.
Hepatic encephalopathy can be managed by giving lactulose orally (0.5–1.0 ml/kg q8h PO) with or without
addition of enteric antibiotics (neomycin 20 mg/kg q8–12h PO).
Response of cholangiohepatitis cats to therapy should be monitored through use of serial complete blood
counts and chemistry profiles. Persistent increases in ALT activity and serum total bilirubin concentration and/or
increasing SAP activity suggest that treatment has been inadequate. The approach to treatment of lymphocytic
portal hepatitis is based on the hypothesis that the liver injury is immune-mediated. Immunosuppressive doses of
corticosteroids are used as described above for chronic cholangiohepatitis. Anecdotal reports indicate prolonged
improvement in clinical signs with prednisolone treatment. Others, however, report poor control of disease
progression with corticosteroid treatment. Azathioprine (0.3 mg/kg PO q48–72 h) has been tried but side effects,
including inappetence and leukopenia, limit its use. Low dose weekly methotrexate therapy has been used in a
few affected cats.
Response to treatment for lymphocytic portal hepatitis is difficult to assess because the disease is very
slowly progressive. A persistent increase in ALT and/or increasing total serum bilirubin concentration during
corticosteroid treatment indicate that the disease is inadequately controlled.
PROGNOSIS
Limited studies of the response of cholangiohepatitis cases to antibiotic treatment suggest that survival of cats
with acute and chronic cholangiohepatitis is similar. Approximately half of the cats’ die or are euthanized within
1 year after diagnosis, 40% survive between 1 and 5 years, and the rest can be expected to have prolonged
survivals beyond 5 years Hopefully, initiation of standard treatment protocols combined, when needed, with
surgical correction of bile duct obstruction will increase the number of cats with long-term survival. Cats with
lymphocytic portal hepatitis appear to have a better prognosis compared to cholangiohepatitis. Of 23 cats that
were available for follow-up, 30% survived less than 1 year, 44% survived between 1 and 5 years, and 26%
survived longer than 5 years. Mean survival time for cats surviving longer than 1 year was 51.8 months, with 22%
of cats still alive at the time of follow-up.
REFERENCES
1. Gagne J, Weiss DJ, Armstrong PJ: Histopathologic evaluation of feline inflammatory liver disease. Vet Pathol 33:521,
1996.
2. Cole TL, Center SA, Flood SN, et al. Diagnostic comparison of needle and wedge biopsy specimens of the liver in dogs
and cats. J Am Vet Med Assoc. 15;220(10):1483-90, 2002.
3. Willard MD, Weeks BR, Johnson M. Fine-needle aspirate cytology suggesting hepatic lipidosis in four cats with
infiltrative hepatic disease. J Feline Med Surg. 1(4):215-20, 1999.
4. Weiss DJ, Armstrong PJ, and Gagne JM. Feline Cholangiohepatitis. In: Kirk’s Current Veterinary Therapy XIII (ed,
Bonagura JD). W.B Saunders Company, Philadelphia. 672-674, 2000.
5. Center SA. Diseases of the gallbladder and biliary tree. In: Strombeck’s Small Animal Gastroenterology, 3rd edition. (eds,
Guilford WG, Center SA, Strombeck DR, Williams DA, and Meyer DJ). W.B. Saunders Company, Philadelphia. 860-888,
1996.
Copyright © 2003 All Rights Reserved
Waltham USA, Inc
All rights including that of translation into other languages, reserved. Photomechanical reproduction (photocopy, microcopy) of this
publication or parts thereof without written permission from Waltham USA, Inc. is prohibited. The opinions expressed in these proceedings
are those of the authors and not necessarily those of Waltham.
You might also like
- Portal Vein Thrombosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandPortal Vein Thrombosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Feline Cholangiohepatitis: AbstractDocument7 pagesFeline Cholangiohepatitis: AbstractibnuzikrillahNo ratings yet
- Liver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesFrom EverandLiver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesNo ratings yet
- Clinical Chemistry LiverDocument6 pagesClinical Chemistry LiverMustafa Salah MahdiNo ratings yet
- Uworld GI NotesDocument17 pagesUworld GI NotesAyodeji SotimehinNo ratings yet
- Approach To The Jaundiced Cat - WSAVA 2015 Congress - VINDocument6 pagesApproach To The Jaundiced Cat - WSAVA 2015 Congress - VINdmantsioNo ratings yet
- Chronic Liver FailureDocument4 pagesChronic Liver FailureJasmine Faith SilvaNo ratings yet
- Cirrhosis of LiverDocument6 pagesCirrhosis of LiverpakdejackNo ratings yet
- VIN Hepatobiliary Disease in CatsDocument11 pagesVIN Hepatobiliary Disease in Catsmmatthew74No ratings yet
- Chronic Liver Disease and CirrhosisDocument5 pagesChronic Liver Disease and Cirrhosisaqil ithninNo ratings yet
- Colangitis FelinaDocument22 pagesColangitis FelinaJuan K SeguraNo ratings yet
- Ontent Reviewers: Contributors:: Rishi Desai, MD, MPH Kaia Chessen Tanner Marshall, MS Will Wei Anca-Elena StefanDocument13 pagesOntent Reviewers: Contributors:: Rishi Desai, MD, MPH Kaia Chessen Tanner Marshall, MS Will Wei Anca-Elena StefanAgnes TanicNo ratings yet
- Liver CirrhosisDocument8 pagesLiver CirrhosisDiana DeciuNo ratings yet
- Etiology, Pathophysiology, and Clinical Manifestations of CholecystitisDocument3 pagesEtiology, Pathophysiology, and Clinical Manifestations of CholecystitisGerriNo ratings yet
- HcirhosisDocument11 pagesHcirhosisChetendra IndoliaNo ratings yet
- Sirrhosis HatiDocument6 pagesSirrhosis HatikimokberusungNo ratings yet
- hpb0011 0194Document9 pageshpb0011 0194ocramusNo ratings yet
- Hepatobiliary Tract and Pancreatic Pathology Assignment - PAYSONDocument22 pagesHepatobiliary Tract and Pancreatic Pathology Assignment - PAYSONRodrigo Joseph PaysonNo ratings yet
- Atlas of Liver Pathology - Chapter 8 Biliary Tree DiseaseDocument45 pagesAtlas of Liver Pathology - Chapter 8 Biliary Tree DiseaseShabir HussainNo ratings yet
- HepaticDocument5 pagesHepaticCosmin StoicaNo ratings yet
- Gallbladder DiseaseDocument67 pagesGallbladder DiseaseKhadira MohammedNo ratings yet
- Jaundice: Presented by Dr. Pollock Prepared by Christopher Edwards Tintanalli Chapter 84, Pgs. 560-561 October 2005Document46 pagesJaundice: Presented by Dr. Pollock Prepared by Christopher Edwards Tintanalli Chapter 84, Pgs. 560-561 October 2005Nurlaila ElaNo ratings yet
- PancreatitisDocument6 pagesPancreatitisreerwrr qeqweNo ratings yet
- Liver Focus 20Document7 pagesLiver Focus 20Sanja CirkovicNo ratings yet
- Assessment of Jaundice in The Hospitalized Patient PDFDocument16 pagesAssessment of Jaundice in The Hospitalized Patient PDFlaura canoNo ratings yet
- Cholestasis Definisi: Penghentian Atau Supresi Aliran Empedu, Dengan Penyebab Intrahepatik Atau Ekstrahepatik EtiologiDocument18 pagesCholestasis Definisi: Penghentian Atau Supresi Aliran Empedu, Dengan Penyebab Intrahepatik Atau Ekstrahepatik EtiologiElsya ParamitasariNo ratings yet
- Gallbladder IIDocument22 pagesGallbladder IIAli SafaaNo ratings yet
- Cholestatic DiseasesDocument12 pagesCholestatic DiseasesJohNo ratings yet
- College of Medicine: Thi Qar UniversityDocument30 pagesCollege of Medicine: Thi Qar Universityhussain AltaherNo ratings yet
- Hepatic Cirrhosis and Hepatitis: Dr. Lubna DwerijDocument69 pagesHepatic Cirrhosis and Hepatitis: Dr. Lubna DwerijNoor MajaliNo ratings yet
- Progesterone Has Been Shown To Decrease Gall-Bladder Motility, WhichDocument9 pagesProgesterone Has Been Shown To Decrease Gall-Bladder Motility, WhichFerreze AnnNo ratings yet
- Progesterone Has Been Shown To Decrease Gall-Bladder Motility, WhichDocument9 pagesProgesterone Has Been Shown To Decrease Gall-Bladder Motility, WhichFerreze AnnNo ratings yet
- Alcoholic Liver Disease: Last Updated: January 19, 2024Document16 pagesAlcoholic Liver Disease: Last Updated: January 19, 2024Tselmeg TselmegNo ratings yet
- Case Study On Alcoholic Liver DiseaseDocument20 pagesCase Study On Alcoholic Liver DiseaseHomework PingNo ratings yet
- B9781416049197X50014 B978141604919750178X MainDocument4 pagesB9781416049197X50014 B978141604919750178X MainMANGNo ratings yet
- Cirrosis Adnd Its ComplicationDocument50 pagesCirrosis Adnd Its Complicationnathan asfahaNo ratings yet
- 2017 UpToDateDocument13 pages2017 UpToDateThiago HübnerNo ratings yet
- Cirrhosis of LiverDocument22 pagesCirrhosis of LiverKrini Tandel50% (2)
- Liver Diseases: Lecture On Pathological Anatomy For The 3-rd Year StudentsDocument27 pagesLiver Diseases: Lecture On Pathological Anatomy For The 3-rd Year StudentsRodriguez Vivanco Kevin DanielNo ratings yet
- Chapter 8Document89 pagesChapter 8Harith AtrisNo ratings yet
- Fulminant Hepatic FailureDocument10 pagesFulminant Hepatic FailureAira Anne Tonee VillaminNo ratings yet
- The Most Common Presenting Symptoms in CD Are Fatigue and Abdominal Pain While in UC Bloody BM and Diarrhea Are Most CommonDocument3 pagesThe Most Common Presenting Symptoms in CD Are Fatigue and Abdominal Pain While in UC Bloody BM and Diarrhea Are Most CommonElle ReyesNo ratings yet
- Surgery Osce PrepDocument94 pagesSurgery Osce PrepSamara AliNo ratings yet
- Department of Faculty SurgeryDocument40 pagesDepartment of Faculty SurgeryMandar GokhaleNo ratings yet
- Cirrhosis of The Liver: GlossaryDocument21 pagesCirrhosis of The Liver: GlossaryNophNo ratings yet
- Examen IM-gastroenterologieDocument15 pagesExamen IM-gastroenterologieNicola BereholschiNo ratings yet
- HepatitisDocument4 pagesHepatitisAlambusha ShuklaNo ratings yet
- CirrosisDocument44 pagesCirrosisflorilett marian cifuentesNo ratings yet
- Feline Hepatic Disease: Dennis Zawie, D.V.M., and Michaels. GarveyDocument30 pagesFeline Hepatic Disease: Dennis Zawie, D.V.M., and Michaels. GarveyValentinaJiménezNo ratings yet
- Pancreatitis: Pancreatitis Is Inflammation of The Pancreas. It Occurs When Pancreatic Enzymes (Especially Trypsin)Document6 pagesPancreatitis: Pancreatitis Is Inflammation of The Pancreas. It Occurs When Pancreatic Enzymes (Especially Trypsin)tianallyNo ratings yet
- Hepatobiliary CasesDocument55 pagesHepatobiliary CasesMeghana MaddaliNo ratings yet
- CholecystitisDocument12 pagesCholecystitisMariela HuertaNo ratings yet
- Liver Function TestsDocument14 pagesLiver Function Testsshihochan100% (2)
- № 15. PM with hepatolienal syndrome, portal hypertension, jaund - Яссін КумаілDocument8 pages№ 15. PM with hepatolienal syndrome, portal hypertension, jaund - Яссін Кумаілabo salehNo ratings yet
- Hepatobiliaryneoplasia: Laura E. SelmicDocument11 pagesHepatobiliaryneoplasia: Laura E. SelmicJuan DuasoNo ratings yet
- Primary Biliary Cirrhosis and Other Ductopenic Diseases: Alastair D. Burt, BSC, MD CHB, Frcpath, FibiolDocument18 pagesPrimary Biliary Cirrhosis and Other Ductopenic Diseases: Alastair D. Burt, BSC, MD CHB, Frcpath, Fibiollourdes marquezNo ratings yet
- AscitesDocument71 pagesAscitessohilaw210No ratings yet
- Diagnosis and Treatment of Liver DiseaseDocument5 pagesDiagnosis and Treatment of Liver DiseaseHéctor MaldonadoNo ratings yet
- Alcoholic Liver Disease - StatPearls - NCBI BookshelfDocument10 pagesAlcoholic Liver Disease - StatPearls - NCBI Bookshelfd99452727No ratings yet
- Approach To Jaundice (1) .PPT ALAWAJIDocument28 pagesApproach To Jaundice (1) .PPT ALAWAJIayuNo ratings yet
- ACVIM Consensus Statement On Pancreatitis in CatsDocument21 pagesACVIM Consensus Statement On Pancreatitis in CatswilverNo ratings yet
- Chronic Vomiting in CatsDocument1 pageChronic Vomiting in CatsDalia ExtrapolisNo ratings yet
- Ultrasonographic Differences Between Dogs and Cats - Today's Veterinary PracticeDocument19 pagesUltrasonographic Differences Between Dogs and Cats - Today's Veterinary PracticeDalia ExtrapolisNo ratings yet
- Griffin2018 Feline Abdominal Ultrasonography Whats Normal What's Abnormal PancreasDocument19 pagesGriffin2018 Feline Abdominal Ultrasonography Whats Normal What's Abnormal PancreasCassiaNo ratings yet
- Spec FPL Treatment For Feline PancreatitisDocument3 pagesSpec FPL Treatment For Feline PancreatitisDalia ExtrapolisNo ratings yet
- Feline PancreatitisDocument13 pagesFeline PancreatitisKary Isabel Fuenzalida MaripanguiNo ratings yet
- American Society For Laser Medicine and Surgery Abstracts 47Document12 pagesAmerican Society For Laser Medicine and Surgery Abstracts 47Dalia ExtrapolisNo ratings yet
- Mansfield 2001Document8 pagesMansfield 2001Constanza GaticaNo ratings yet
- Tissue Welding: American Society For Laser Medicine and Surgery Abstracts 55Document19 pagesTissue Welding: American Society For Laser Medicine and Surgery Abstracts 55Dalia ExtrapolisNo ratings yet
- Toward A Contingent Resource-Based Theory: The Impact of Information Asymmetry On The Value of Capabilities in Veterinary MedicineDocument28 pagesToward A Contingent Resource-Based Theory: The Impact of Information Asymmetry On The Value of Capabilities in Veterinary MedicineDalia ExtrapolisNo ratings yet
- Bayesian Accelerated Failure Time Analysis With Application To Veterinary EpidemiologyDocument17 pagesBayesian Accelerated Failure Time Analysis With Application To Veterinary EpidemiologyDalia ExtrapolisNo ratings yet
- Crate Conditioning of Bongo (Tragelaphus Eurycerus) For Veterinary and Husbandry Procedures at The Denver Zoological GardensDocument8 pagesCrate Conditioning of Bongo (Tragelaphus Eurycerus) For Veterinary and Husbandry Procedures at The Denver Zoological GardensDalia ExtrapolisNo ratings yet
- Raymond Lo - The Feng Shui of Swine FluDocument1 pageRaymond Lo - The Feng Shui of Swine Fluay2004jan100% (1)
- Web Aggregator SyllabusDocument5 pagesWeb Aggregator Syllabussam franklinNo ratings yet
- Standard Into-Plane Fueling Service Levels and SafetyDocument8 pagesStandard Into-Plane Fueling Service Levels and SafetyPrekelNo ratings yet
- CRISIL Mutual Fund Ranking: For The Quarter Ended September 30, 2020Document48 pagesCRISIL Mutual Fund Ranking: For The Quarter Ended September 30, 2020MohitNo ratings yet
- Calamity and Disaster Preparedness Chapter IXDocument34 pagesCalamity and Disaster Preparedness Chapter IXANGEL ALBERTNo ratings yet
- AIR Modeller 78 2018Document68 pagesAIR Modeller 78 2018StefanoNo ratings yet
- Battle Healing PrayerDocument9 pagesBattle Healing PrayerSolavei LoanerNo ratings yet
- Chapter 2Document5 pagesChapter 2ERICKA MAE NATONo ratings yet
- Clay Analysis - 1Document55 pagesClay Analysis - 1JCSNo ratings yet
- EDU403 Assignment 1Document6 pagesEDU403 Assignment 1NadiaJawadHussainNo ratings yet
- Karan Chawla and Joshua Lee November 21, 2016 MEDS 3020 - Fall 2016 Dr. Rosevear, Dr. Cartwright, Dr. LiebermanDocument2 pagesKaran Chawla and Joshua Lee November 21, 2016 MEDS 3020 - Fall 2016 Dr. Rosevear, Dr. Cartwright, Dr. LiebermanJeremy DelaneyNo ratings yet
- Eprubete. Culori. UtilizareDocument3 pagesEprubete. Culori. UtilizareCuCUNo ratings yet
- Absenteeism in Public Sector: Presented byDocument25 pagesAbsenteeism in Public Sector: Presented byPravin Rathod50% (2)
- Bad Effects of Festivals On The EnvironmentDocument10 pagesBad Effects of Festivals On The EnvironmentSahil Bohra85% (52)
- Extubation After Difficult IntubationDocument3 pagesExtubation After Difficult Intubationramanrajesh83No ratings yet
- Affidavit: IN WITNESS WHEREOF, I Have Hereunto Affixed MyDocument2 pagesAffidavit: IN WITNESS WHEREOF, I Have Hereunto Affixed Myceleste LorenzanaNo ratings yet
- Components of A Rainwater Harvesting SystemDocument38 pagesComponents of A Rainwater Harvesting SystembudiperNo ratings yet
- Hazard Risk Assessment of Roof of The Mazanine Floor..Document15 pagesHazard Risk Assessment of Roof of The Mazanine Floor..Akhtar BahramNo ratings yet
- Reclaimer Inspection ReportDocument51 pagesReclaimer Inspection ReportThiru Malpathi100% (1)
- ChartDocument27 pagesChartFlorijan ŠafarNo ratings yet
- 2.2 WaterDocument32 pages2.2 WaterHelena GlanvilleNo ratings yet
- Park Ch. 1 - A1000 - Spring13Document21 pagesPark Ch. 1 - A1000 - Spring13lingyeeNo ratings yet
- Future Proofing Cities Toolkit by Craig Applegath 2012-03-01sm PDFDocument20 pagesFuture Proofing Cities Toolkit by Craig Applegath 2012-03-01sm PDFJorge Fernández BaluarteNo ratings yet
- SubstationsDocument39 pagesSubstationspNo ratings yet
- Yume Beauty Price ListDocument1 pageYume Beauty Price ListjessicaelaNo ratings yet
- Types of Shops Shopping: 1. Chemist's 2. Grocer's 3. Butcher's 4. Baker'sDocument1 pageTypes of Shops Shopping: 1. Chemist's 2. Grocer's 3. Butcher's 4. Baker'sMonik IonelaNo ratings yet
- Seed PrimingDocument4 pagesSeed PrimingbigbangNo ratings yet
- The Modern Fire Attack - Phil Jose and Dennis LegearDocument7 pagesThe Modern Fire Attack - Phil Jose and Dennis LegearTomNo ratings yet
- Monopoly Tycoon TipsDocument8 pagesMonopoly Tycoon TipsVictoria SmithNo ratings yet
- Nursing Care of A Family With An InfantDocument26 pagesNursing Care of A Family With An InfantJc GarciaNo ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (24)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- Self-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!From EverandSelf-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!Rating: 5 out of 5 stars5/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)From EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Rating: 4 out of 5 stars4/5 (378)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (58)