Professional Documents
Culture Documents
Analgesic, Sedatives, and Hypnotics: Opioid Analgesics
Uploaded by
qgkfjfn6frOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Analgesic, Sedatives, and Hypnotics: Opioid Analgesics
Uploaded by
qgkfjfn6frCopyright:
Available Formats
Analgesic, Sedatives, and OPIOID ANALGESICS
Based on the specific receptors they bind
Hypnotics
to avoid their activity at the receptor, opioid
are classed as full or pure agonist, partial
•Analgesics - Are pain relievers for a
agonist, or mixed agonist-antagonists.
variety of conditions, including headaches,
analgesics diminish inflammation while
• Full agonist are the most commonly used
opioid analgesics alter pain perception in
because they can alter the perception of
the brain.
pain and they don't have ceiling to their
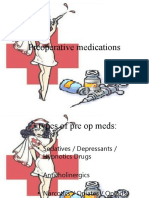
•Sedatives - are a sort of prescription drug
analgesic effects. Pure agonist opioids
that reduces the activity of your brain.
cannot reverse analgesia like the other
They're commonly employed to make you
classes because of the potential abuse of
feel more at ease. They also employ them
it. (Controlled substances)
as anesthetics in general. Sedatives are
• Opioids tend to cause tolerance and
restricted drugs.
physiological dependence with chronic use.
•Hypnotics - are commonly like sedatives;
• This type of analgesics should be
but they are mostly like used to treat lack of
prescribed to terminally ill patients with
sleep. These, too, are restricted drugs.
constant around the clock pain, with
additional "as needed" doses for
PAIN IN SUBJECTIVE
breakthrough pain, and dosages adjusted
- Most of the time, patients seek medical
to achieve pain relief with an acceptable
care because they can feel pain. Pain is
level of side effects.
subjective, it can be experienced only by
the individual person.
SIDE EFFECTS OF OPIOIDS
- The National Health Statistics have
•Sedation
reported that the four most commonly
•Confusion
known pain is in the lower back, neck, and
•Headache and dizziness
facial or jaw pain.
•Hypotension and Bradycardia Urinary
- Analgesics are the prescribed type of
retention
medicine, contraring types of pain.
•Sexual Dysfunction
•Nausea and vomiting
PAIN HAS BOTH PSYCHOLOGICAL AND
•Respiratory and/or emotional dependence;
PHYSIOLOGICAL COMPONENTS
tolerance
•Blurred vision
- Some people have higher pain tolerance
•Seizures with large doses
than others because of conditioning, ethnic
•Rash and pruritus
background, sensitivity and/or physiological
factors. (Depending on the amount of
Precautions with opioids apply to:
endorphins released, and releasing
endorphins may cause placebo effect.)
•Head injury
•Cardiac Disease
Endorphins are endogenous analgesics
•CNS Depression (central nervous system
that the body produces in response to
depression)
extreme pain or excessive exercise.
•GI, hepatic, renal, and thyroid diseases
•Chronic obstructive pulmonary disease Nonopioid Analgesic
•Asthma •Nonopioid are given for the purposes of
relieving mild to moderate pain, fever, and
Interactions include potentiation of the anti- inflammatory conditions, for example
effects of opioids with CNS arthritis. This group of analgesics is also
depressants, including: used as coanalgesic in severe acute or
chronic pain requiring opioids.
•Psychotropics
•Alcohol
•Sedatives and hypnotics
•Muscle relaxants
•Antihistamines
•Antiemetic
•Antihypertensives
TRAMADOL
• Tramadol (Ultram) - is a centrally acting
synthetic analog of codeine with a dual
mechanism action. It produces analgesia
by weak inhibition of norepinephrine and
serotonin reuptake and is an opioid SALICYLATES AND OTHER NSAIDs
receptor agonist.
Salicylates analgesic and anti-
inflammatory actions are associated
primarily with preventing the formation of
prostaglandins and the subsequent
inflammatory response prostaglandins
help to induce.
SIDE EFFECT OF SALICYLATES AND
OTHER NSAIDs ESPECIALLY WITH
PROLONGED USE AND/OR HIGH DOSAGE
•prolonged bleeding time
•Bleeding and frequent bruising
•Gastric distress, ulceration, and bleeding
(which may be silent)
•Tinnitus (Ringing or roaring in the ears)
and hearing loss with overdose hepatic
dysfunction renal insufficiency, decrease
urine output with sodium and water
retention and renal failure
•Coma, respiratory failure especially for
children.
•Gastrointestinal (G) symptoms, which can
be minimized by administration with food
or milk or by using an aspirin buffered with • Anti-infective resistance is caused
antacids. by many factors. Therefore, the
strategies needed to combat the
ACETAMINOPHEN problem are also complex.
Acetaminophen (Tylenol) – is used RESISTANCE (Organisms)
extensively in the treatment of mild to
moderate pain and fever. It has very little • Staphylococcus aureus (MRSA)
effect on inflammation, however, • Strains of Enterococci
acetaminophen has fever adverse side • Strains of type A influenza
effects than salicylates. • Mycobacterium tuberculosis
SIDE EFFECTS OF ACETAMINOPHEN SELECTION OF ANTI-INFECTIVE
DRUGS
• Severe liver toxicity
• Renal insufficiency (decrease urine • Site of infection
output) • Status of hepatic and/or renal
• Rash or urticaria function
• Blood dyscaria • Age
• Pregnancy or lactation
• Likelihood of organisms
ANTI-INFECTIVE DRUGS development resistance
• Known allergy to the anti-infective
Are medicines that work to prevent or treat
drug
infections.
ADVERSE REACTIONS
SUBCLASSIFICATIONS
1. ALLERGIC HYPERSENSITIVITY
Antibiotics Antifungal
Aminoglycosides Antituberculosis • Rash, urticaria, mild fever
agents anaphylaxis, dyspnea, chest
Cephalosporins Miscellaneous anti- contractions, shock, collapse.
infections 2. DIRECT TOXICITY
Macrolides Agents for VRE • Ototoxicity, nephrotoxicity,
Penicilins Sulfonamides hepatoxicity, bloods dyscrasias,
Carbapenems Urinary anti- phlebitis, phototoxicity.
infectives 3. INDIRECT TOXICITY, OR
Quinolones Antivirals SUPERINFECTIONS
Tetracyclines Treatment for HIV- • New infection
AIDS infection • Diarrhea, vaginitis, glossitis
VACCINES (or Immunizations)
RESISTANCE
• Vaccines mimic the virus or bacteria
More than 70% that cause HAIs are that cause disease and trigger the
resistant to at least one drug. body’s creation of antibodies.
• Organism build up resistance to drug • These antibodies will provide
that have been used to frequently or protection once a person is infected
improperly, and then the drugs are with the actual disease-causing virus
no longer effective. or bacteria.
ANTIBIOTICS Contraindications
(Penicilins Macrolides, etc.) • Tinnitus, vertigo, and high-frequency
hearing loss
• Refers to large spectrum of
• Reduced renal functions
medicines that are useful for treating
• Dehydration
and preventing infections caused by
• Pregnant and nursing women
bacteria.
• Infants or older adults
• These types of medications have no
effect on viral, fungal or other types Drugs interactions
of infections. Use without proper
indication can lead to resistance. • Other ototoxic drugs
That is why antibiotics should not be • General anesthetics or
used for treatment of the common neuromuscular blocking agents
cold, because it is a viral infection. • Antiemetics
Aminoglycosides Cephalosporins (related to penicilins)
Mechanism of action Mechanism of action
• Inhibits protein synthesis in the cell • Semisynthetic beta-lactam
wall, which results in bacterial death. antibiotics produced from certain
species of a fungus
Indications
Indications
To treat:
To treat different infections of:
• Infective endocarditis
• Sepsis • Respiratory tract
• Complicated intraabdominal • Skin
infections • Urinary tract
• Complicates genitourinary infections • Bones and joints
• Some STIs
Representative drugs
• Endocarditis
• Gentamicin Representative drugs
• Amikacin
• Tobramycin • 1st gen: cephalexin, cefazolin
• Neomycin • 2nd gen: cefaclor, cefuroxime
• Streptomycin • 3rd gen: ceftriaxone, ceftazidime,
cefdinir
Adverse effects • 4th gen: cefepime
• Nephrotoxicity • 5th gen: ceftaroline
• Ototoxicity Adverse effects
• Neuromuscular blockade
• CNS symptoms (headache, tremor, • Hypersensitivity
lethargy, numbers, seizures) • Blood dyscrasias
• Blurred vision, rash, or urticaria • Nausea, vomiting, and diarrhea
• Phlebitis with IV administration and
pain at the site of IM injection
• Respiratory distress • Benzodiazepines
• Seizures • Warfarin
• Digoxin
Drug interactions
• Statins
• Increased effectiveness with • Calcium channel blockers
probenecid • Antiarrhythmic agents
• Disulfiram-like reaction (flushing, • Azole antifungals
tachycardia, shock) with alcohol • Quinolones
ingestion and cefotetan
Penicilins
Macrolides
Mechanism of action
Mechanism of action
• Beta-lactam antibiotics produced
• Inhibit RNA protein synthesis and from certain species of a fungus. It is
suppress reproduction of the used in many streptococcal and
bacteria some staphylococcal and
meningococcal infection
Indications
Indications
Treatment of:
Treatment of
• Respiratory tract infections
• Skin conditions (acne) • Syphilis
• STI (if allergic to penicillin) • Used prophylactically to prevent
recurrences of rheumatic fever
Representative drugs
Representative drugs
• Erythromycin
• Roxithromycin • Amoxicillin
• Azithromycin • Ampicillin
• Clarithromycin • Penicillin VK
• Penicillin G
Adverse effect
Adverse effect
• Anorexia, nausea, vomiting,
diarrhea, cramps • Hypersensitivity
• Urticaria • Super infections (especially with oral
• Superinfections ampicillin) and pseudomembranous
colitis
Contraindications
• Nausea, vomiting, and diarrhea
• Liver dysfunction and GI disease • Blood dyscrasias
• Electrocyte • Renal and hepatic disorder (rare)
• Certain cardiovascular disease • CNS effect, example confusion,
anxiety, and seizures.
Drug interactions
Contraindications
• Carbamazepine
• Cyclosporine • History of serious allergy to
• Theophylline penicillins or other beta-lactams
Drug interactions Quinolones
• Potentiation of penicillin with Mechanism of actions
probenecid
• Helps treating many different
• Antagonistic effect (delayed
infections.
absorption) of oral penicillin when
• Should be reserved for infections
given antacids or with food
that require therapy with
• Antagonistic effect of some other
fluoroquinolones such as
anti-infectives on penicillin.
Pseudomonas infection or when a
Carbapenems patient is allergic to other antibiotics
Mechanism of action Indications
• Inhibit bacterial cell growth that • Urinary test
eventually kills the bacteria. • Sinuses
• Lower respiratory tract
Indications
• GI tract
Treatment of: • Skin
• Bones, and joints
• Pneumonia
• Gonorrhea
• Febrile neutropenia
• Intra-abdominal infections Representative drugs
• Diabetic foot infections
• Ciprofloxacin
• Significant polymicrobial infections
• Levofloxacin
Representative drugs • Moxifloxacin
• Meropenem Adverse effects
• Doripenem
• Nausea, vomiting, diarrhea,
• Ertapenem
abdominal pain, and colitis
Adverse effect (especially older adult px.)
• CNS effect – headache, dizziness,
• Injection site reactions confusion, irritability, seizures, and
• Diarrhea anxiety.
• Nausea • Superinfection hypersensitivity
• Vomiting reaction (rare)
• Skin rash • Phototoxicity
• Pruritus
Contraindications
Contraindications
• Older adults, especially with GI
• Colitis disease or arteriosclerosis
• Renal dysfunction • Children or adolescents
• CNS disorders • Doing strenuous exercise
• Hemodialysis • Pregnancy or lactation
Drugs interactions • Seizures disorders
• Cardiac disease
• Valproic acid
Drug interactions • Allergic hyposensitivity (rare)
• Theophylline (ciprofloxacin) Contraindications
• Warfarin
• Pregnancy and lactation
• Antacids and other preparations
• Children under age 8 years
containing Fe, Mg, Zn, Ca.
• Patients exposed to direct sunlight
• Sucralfate (Carafate)
• Liver or GI disease
Tetracyclines • Renal disease (doxycycline
preferred)
Mechanism of actions
Drug interactions
• Interferes with the ability of the
bacteria to produce certain vital • Antacids, calcium supplements, or
proteins for bacterial growth. magnesium laxatives
• Iron preparations and zinc
Indications
• Antidiarrheal agents containing
Treatment of some infection disease kaolin, pectin, bismuth
caused by: • Dairy products
• Oral contraceptives
• Rickettsia
• Chlamydia
• Some uncommon bacteria
Antifungals (Fluconazole, Micafungin,
• Rocky mountain spotted fever
etc.)
• Atypical pneumonia
• Some STIs • Used to treat specific susceptible
• Severe inflammatory acne fungal disease
Representative drugs Amphotericin B
• Doxycycline Mechanism of Action
• Tigecycline
• Administered IV for the treatment of
• Minocycline
severe systematic, potentially fatal
Adverse effects infections caused by susceptible
fungi including candida.
• Nausea, vomiting, and diarrhea
• Superinfections (vaginitis and Indications
stomatitis) Treatment severe fungal infections
• Photosensitivity, with exaggerated resulting from:
sunburn
• Discolored teeth (fetus and young • Immunosuppressive therapy
children) • Patients with AIDS
• Retarded bone growth (fetus and • Severe illness
young children)
Adverse effects
• Hepatic or renal toxicity
• CNS symptoms: vertigo and cerebral • Headache
edema • Chills
• Thrombophlebitis • Fever
• Hypotension • Dizziness
• Tachypnea • Headache
• Malaise
Drug interactions
• Muscle and joint pain, and weakness
• Anorexia • Warfarin (Increased prothrombin
• Nausea time could cause hemorrhage)
• Vomiting • Oral antidiabetic agents
• Cramps (hypoglycemia can result)
• Nephrotoxicity • Rifampin (can lead to clinical failure
• Hypokalemia and hypomagnesemia of fluconazole)
• Statins (increased risk of myopathy;
Drug interactions except pravastatin)
• Lipid-based product (abelcet) • Benzodiazepines (increased CNS
increases the tolerability of the drug effect)
without compromising its antifungal Micafungin (mycamine)
effect.
• Belongs to one of the newer classes
Fluconazole
of antifungals.
• One of the most widely prescribe Mechanism of action
antifungal agents
• Given IV that provide new treatment
Mechanism of actions
options against candida and
• Acts against many fungal pathogens aspergillus
including candida without serious Indications
toxicity of amphotericin B
Treatment of:
Indications
• Esophageal candidiasis
Treatment of:
• Candidemia
• Oropharyngeal and esophageal • For stem cell transplantation
candidiasis prophylaxis
• Serious systemic candida infections
Adverse effects
(e.g., urinary tract and blood stream
infections) • Headaches and fever
• Nausea, vomiting and diarrhea
Contraindications
• Infusion reaction
• Pregnant or nursing women • Neutropenia
• Hepatic or renal disease • Hypokalemia and hypomagnesemia
Adverse effects Contraindications
• Moderate nausea • Patients under 18 years old
• Vomiting • Pregnancy and breast-feeding
• Abdominal pain • Liver dysfunction
• Diarrhea • Renal disease
• Hepatic abnormalities
Drug interactions Isoniazid (H or INH)
• There are no major drug interactions Mechanism of action
Nystatin • Inhibits the synthesis of mycolic
acids, an essential component of the
Mechanism of action
bacterial cell wall.
• Structurally related to amphotericin Adverse effects
B
• Nausea, vomiting, diarrhea
Indications
• Dizziness, blurred vision, headache,
Treatment: and fatigue
• Numbness and weakness of
• oral cavity candidiasis extremities
used as: • Hepatic toxicity
• fungicide in the topical treatment of Contraindications
skin and mucous membrane (mouth, • Chronic liver disease or alcoholics
or vagina)
• Impaired renal functions
Adverse effects • Hepatic toxicity (children’s dosage
should be limited to 10-15 mg/kg,
• Side effects are rare but may respectively)
occasionally include nausea,
vomiting, and diarrhea with high oral Indications
done.
• Potentiation by phenytoin
Drug interactions • Increase risk of hepatotoxicity w/
rifampin.
• No significant drug interactions • Alcohol
because of its lack of absorption • Antacids
from the gut.
Rifampin
Antituberculosis (ethambutol,
isoniazid, etc.) Mechanism of action
• Tuberculosis (tb) is caused by a • Inhibits bacterial RNA polymerase,
bacterium called Myobacterium the enzyme responsible for DNA
tuberculosis, which primarily attacks transcription.
the lungs.
Adverse effects
These drugs are administered to:
• Nausea, vomiting, diarrhea
1. Treat latent or asymptomatic • Dizziness, blurred vision, headache,
infection and fatigue
2. Treat active clinical tuberculosis and • Numbness and weakness of
prevent relapse extremities
• Hepatic toxicity
• Body fluids colored red-orange
• Hypersensitivity reaction, with flu-like Pyrazinamide (Z or PZA)
symptoms
Mechanism of actions
Contraindications
• Converts a special enzyme to an
• Chronic liver disease or alcoholics active form which inhibits the
• Impaired renal functions synthesis of fatty acids
• Hepatic toxicity (children’s dosage
Adverse effects
should be limited to 10-15 mg/kg,
respectively) • Hepatic toxicity
• Gout
Ethambutol (E or EMB)
• Hypersensitivity
Mechanism of action • GI disturbance
• Inhibits the arabinosyltransferases, Contraindications
preventing formation of the cell wall
components arabinogalactan and • Patient with history of gout
lipoarabinomannan, and preventing • Dizziness
cell division. • Severe hepatic disease or
alcoholism
Adverse effect • Children (potential toxicity)
• Optic neuritis • Pregnant or nursing women
• Dermatitis Streptomycin
• Pruritus
• Headache Mechanism of action
• Malaise • Inhibits protein synthesis and causes
• Ever the death of microbial cells
• Confusion
• Joint pain Adverse effects
• GI symptoms • Ototoxicity
• Occasional peripheral neuritis • nephrotoxicity
Contraindications
• Visual testing before and during
therapy
• Impaired renal function
• Diabetes
• Ocular defects
• Children under 1-3
• Pregnancy (caution)
• Patients with gout
You might also like
- Depression & Anxiety: What You Need To Know About Treatment with Medications, Herbs & SupplementsFrom EverandDepression & Anxiety: What You Need To Know About Treatment with Medications, Herbs & SupplementsNo ratings yet
- Therapeutics in Endo-2Document67 pagesTherapeutics in Endo-2mahmoudNo ratings yet
- Fibromyalgia : The Complete Guide to Healing Fibromyalgia NaturallyFrom EverandFibromyalgia : The Complete Guide to Healing Fibromyalgia NaturallyNo ratings yet
- PAiN SYnDrOmEs (Reviewer)Document19 pagesPAiN SYnDrOmEs (Reviewer)Agum, Philip James P.No ratings yet
- AntianxietyDocument8 pagesAntianxiety39 Nayan BhagatNo ratings yet
- Psychotherapeutic Drug 2Document7 pagesPsychotherapeutic Drug 2Michaela BernadasNo ratings yet
- Neurosis: - An Accumulation of Anxiety and Tension Which Leads To Emotional Changes and Abnormal BehaviorDocument18 pagesNeurosis: - An Accumulation of Anxiety and Tension Which Leads To Emotional Changes and Abnormal BehaviorNESLEI ANN LIBUNAONo ratings yet
- Anne Goza BSN-2B: Spinal CordDocument11 pagesAnne Goza BSN-2B: Spinal CordSiseneg Soled SotnasNo ratings yet
- Analgesic & Anesthetic: Dr. Yunita Sari Pane, MsiDocument92 pagesAnalgesic & Anesthetic: Dr. Yunita Sari Pane, Msiqori fadillahNo ratings yet
- Nsaid'S and Opioid AnalgesicsDocument18 pagesNsaid'S and Opioid AnalgesicsruchikaNo ratings yet
- Sedative HypnoticsDocument32 pagesSedative HypnoticsgehaNo ratings yet
- Anxiolytics: DR Neelam Joshi Department of PsychiatryDocument16 pagesAnxiolytics: DR Neelam Joshi Department of Psychiatryविजय मैनालीNo ratings yet
- Null 5Document3 pagesNull 5مجهول المجهولNo ratings yet
- Pain ManagementDocument68 pagesPain Managementapi-734449276No ratings yet
- Cmpi MidtermDocument185 pagesCmpi MidtermAubrey MadelaineNo ratings yet
- Drug Study of FluoxetineDocument2 pagesDrug Study of FluoxetineLance De GuzmanNo ratings yet
- Analgesics Agents ZJDocument37 pagesAnalgesics Agents ZJDanial HassanNo ratings yet
- WEEK 6 7-CNS Medications StudentDocument83 pagesWEEK 6 7-CNS Medications Studentx8jdbj5gphNo ratings yet
- Sedation, Analgesia & Patient Controlled Analgesia 2Document28 pagesSedation, Analgesia & Patient Controlled Analgesia 2Arshad SyahaliNo ratings yet
- Gerontology Lec 7 (Pain)Document2 pagesGerontology Lec 7 (Pain)Aleczis Dela CruzNo ratings yet
- Pharmacology - Central Nervous SystemDocument10 pagesPharmacology - Central Nervous System22bgu0805msNo ratings yet
- Central Nervous System 1 2 DEFINTIONS OF TERMSDocument3 pagesCentral Nervous System 1 2 DEFINTIONS OF TERMSKristina Mae BayanoNo ratings yet
- Perioperative Pain ManagementDocument6 pagesPerioperative Pain ManagementAya RandallNo ratings yet
- Anestesia Umum: Dr. Ganda P. Sibabiat., Span., KicDocument14 pagesAnestesia Umum: Dr. Ganda P. Sibabiat., Span., KicPin Han NaNo ratings yet
- Anestesia Umum: Dr. Ganda P. Sibabiat., Span., KicDocument14 pagesAnestesia Umum: Dr. Ganda P. Sibabiat., Span., KicMichael TambunanNo ratings yet
- Analgesic Drugs: Dr. Jim AmisiDocument65 pagesAnalgesic Drugs: Dr. Jim AmisiMike AnnisNo ratings yet
- Central Nervous System AgentsDocument20 pagesCentral Nervous System AgentsshannenNo ratings yet
- Pain Classification and Cancer Pain ManagementDocument50 pagesPain Classification and Cancer Pain ManagementAli Aftab100% (1)
- Nm-Lec15 - (Anxiolytics, Sedatives & Hypnotics)Document39 pagesNm-Lec15 - (Anxiolytics, Sedatives & Hypnotics)geng gengNo ratings yet
- 1 Semester: Anti-Migraine Agents Are Used To Treat Migraine HeadachesDocument26 pages1 Semester: Anti-Migraine Agents Are Used To Treat Migraine HeadachesMARY BERNADETTE EGANANo ratings yet
- Conscious Sedation: Hayel Gharaibeh, MD. Anesthesia ConsultantDocument84 pagesConscious Sedation: Hayel Gharaibeh, MD. Anesthesia ConsultantKhaled GharaibehNo ratings yet
- Basics of Opioid Prescribing - Part II: Pain Management and OpioidsDocument8 pagesBasics of Opioid Prescribing - Part II: Pain Management and Opioidsga_boxNo ratings yet
- Year 8 Science C7Document94 pagesYear 8 Science C7Ventus TanNo ratings yet
- Anxiolytic and Hypnotic DrugsDocument3 pagesAnxiolytic and Hypnotic Drugsskoee dbswjNo ratings yet
- Analgesia 2Document3 pagesAnalgesia 2DanielleNo ratings yet
- Pain Relief: Bagian Anestesiologi RSUD Ulin - FK UNLAM BanjarmasinDocument51 pagesPain Relief: Bagian Anestesiologi RSUD Ulin - FK UNLAM BanjarmasinIntan Alwaystry TobehappyNo ratings yet
- Temazepam (Restoril)Document1 pageTemazepam (Restoril)E100% (2)
- Commonly Used Medication For Older AdultsDocument3 pagesCommonly Used Medication For Older AdultsRaze AlemaniaNo ratings yet
- Psychopharmacology Article StyleDocument9 pagesPsychopharmacology Article StyleLizethNo ratings yet
- Unit 2-CNS and ANS (Part 3) Modified 2021Document30 pagesUnit 2-CNS and ANS (Part 3) Modified 2021Donia ShormanNo ratings yet
- AnalgesicDocument62 pagesAnalgesicAnjum IslamNo ratings yet
- Drugs Used in The Treatment of Pain and Affecting The Musculoskeletal SystemDocument34 pagesDrugs Used in The Treatment of Pain and Affecting The Musculoskeletal SystemAnna Lin YeeNo ratings yet
- Opioid Analgesics & AntagonistsDocument13 pagesOpioid Analgesics & AntagonistsVidi IndrawanNo ratings yet
- Anesthetic DrugsDocument7 pagesAnesthetic DrugsSpahneNo ratings yet
- PainDocument22 pagesPainMary PeterNo ratings yet
- Ilovepdf Merged-4Document208 pagesIlovepdf Merged-4Claudia Vargas AndinoNo ratings yet
- InsomniaDocument32 pagesInsomniaemanmohamed3444No ratings yet
- Psychiatric Mental State: Unrelated To Sexual Stimulation or DesireDocument9 pagesPsychiatric Mental State: Unrelated To Sexual Stimulation or DesirePricel Quinones FrutoNo ratings yet
- Archivetempfinal RevisionDocument140 pagesArchivetempfinal RevisionSheza FarooqNo ratings yet
- Conscious Sedation: Prof - Med. Nabil H. Mohyeddin Intensive Care &anesthesiologyDocument84 pagesConscious Sedation: Prof - Med. Nabil H. Mohyeddin Intensive Care &anesthesiologyKhaled GharaibehNo ratings yet
- AnalgesicDocument56 pagesAnalgesicMuhammad hilmiNo ratings yet
- The Nervous System: Blood Brain BarrierDocument17 pagesThe Nervous System: Blood Brain BarrierSuleiman AbdallahNo ratings yet
- Fo Analgetik Opioid - Blok6Document65 pagesFo Analgetik Opioid - Blok6Rhena Fitria KhairunnisaNo ratings yet
- 6comfort and Pain ManagementDocument63 pages6comfort and Pain ManagementRomalyn AcquidanNo ratings yet
- Referat CA Cervik BLM Donehttps://imgv2-2-F.scribdassets - Com/img/document/357536777/325x421/51b6aa5708/1554126020?v 1Document25 pagesReferat CA Cervik BLM Donehttps://imgv2-2-F.scribdassets - Com/img/document/357536777/325x421/51b6aa5708/1554126020?v 1desmawitaNo ratings yet
- DruggggggDocument43 pagesDruggggggmonesabiancaNo ratings yet
- ReviewerDocument64 pagesReviewerDanica FrancoNo ratings yet
- Pain and Palliative - Topic DiscussionDocument7 pagesPain and Palliative - Topic Discussionapi-535001113No ratings yet
- Current Treatment Options in The Management of Severe Pain: William Campbell MD, PHD, Frca, Ffarcsi, FfpmrcaDocument10 pagesCurrent Treatment Options in The Management of Severe Pain: William Campbell MD, PHD, Frca, Ffarcsi, FfpmrcaJonathan TulipNo ratings yet
- Problem Solving in General Practice: Part ThreeDocument2 pagesProblem Solving in General Practice: Part ThreeAs Minhas OrigensNo ratings yet
- Yashaswini Pader - Resume - Abroad AssistDocument3 pagesYashaswini Pader - Resume - Abroad AssistMuneer Basha SkNo ratings yet
- Social and Political Issues Debate TopicsDocument6 pagesSocial and Political Issues Debate TopicsbjdevhervehroheghghbhbhotbhhortbhNo ratings yet
- Nursing Research Position StatementDocument3 pagesNursing Research Position StatementFranck Duprey MvogoNo ratings yet
- Applying To The AmcDocument72 pagesApplying To The AmcgracieMD100% (1)
- Roe TemplateDocument31 pagesRoe TemplateLoredana Radu100% (7)
- BenlystaDocument21 pagesBenlystaChrisNo ratings yet
- Sleep Bruxism: Therapeutic Possibilities Based in EvidencesDocument8 pagesSleep Bruxism: Therapeutic Possibilities Based in EvidencesmutiaNo ratings yet
- Burning Mouth Syndrome and Treatment With ParoxetinDocument2 pagesBurning Mouth Syndrome and Treatment With ParoxetinFitri AngginiNo ratings yet
- Peds ?Document51 pagesPeds ?gissy0522No ratings yet
- Publikasi Dayen 20720014 Stikes Guna Bangsa YogyakartaDocument12 pagesPublikasi Dayen 20720014 Stikes Guna Bangsa YogyakartadayenNo ratings yet
- Advanced Post Graduate Diploma in Clinical Research & PharmacovigilanceDocument2 pagesAdvanced Post Graduate Diploma in Clinical Research & PharmacovigilanceAbin ChandrakumarNo ratings yet
- Barriers To Effective Nursing LeadershipDocument14 pagesBarriers To Effective Nursing LeadershipTristan CunananNo ratings yet
- Community Health and Development - CMC Vellore PDFDocument24 pagesCommunity Health and Development - CMC Vellore PDFKrishnaveni MurugeshNo ratings yet
- Curriculum: Minimal Access UrologyDocument14 pagesCurriculum: Minimal Access UrologyANOOP HANDANo ratings yet
- Designed by Sitra Hassen: Dilla University Department of ArchitectureDocument7 pagesDesigned by Sitra Hassen: Dilla University Department of ArchitectureSitra HassenNo ratings yet
- Medical MalpracticeDocument10 pagesMedical MalpracticeSakshi Suri100% (2)
- Chapter 3: Legal Aspects of NursingDocument6 pagesChapter 3: Legal Aspects of NursingKaren Joyce Costales MagtanongNo ratings yet
- Case Reviews in Ophthalmology Expert Consult - OnlDocument2 pagesCase Reviews in Ophthalmology Expert Consult - Onldr. mostakNo ratings yet
- Psychia Ncp-MetchelDocument9 pagesPsychia Ncp-MetchelCarmelita SaltNo ratings yet
- Physician's Examination FormDocument1 pagePhysician's Examination FormMason FrasherNo ratings yet
- Mazhaume Eugan CVDocument5 pagesMazhaume Eugan CVMaxwell MandikumbaNo ratings yet
- TOP Dialysis Centres in MumbaiDocument2 pagesTOP Dialysis Centres in MumbaiTerminal VelocityNo ratings yet
- Management of Healthcare Workers (HCW) Exposed To Confirmed Covid-19 Case in Hospital Shah AlamDocument1 pageManagement of Healthcare Workers (HCW) Exposed To Confirmed Covid-19 Case in Hospital Shah AlamNurhafizah IbrahimNo ratings yet
- Patton FullerDocument5 pagesPatton FullerJacques OwokelNo ratings yet
- Adj 12563Document5 pagesAdj 12563anushiNo ratings yet
- Nephrology Certification Examination Blueprint - American Board of Internal MedicineDocument4 pagesNephrology Certification Examination Blueprint - American Board of Internal MedicineabimorgNo ratings yet
- Peter Dickinson: Return To The CaseDocument5 pagesPeter Dickinson: Return To The Casebella swanNo ratings yet
- ScriptDocument27 pagesScriptIqrarNo ratings yet
- Group 11-Project ProposalDocument1 pageGroup 11-Project ProposalRichaNo ratings yet
- Plastic Surgery Logbook Batch A - EditedDocument11 pagesPlastic Surgery Logbook Batch A - EditedRidham RanaNo ratings yet
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (23)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosFrom Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosRating: 4.5 out of 5 stars4.5/5 (207)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Algorithms to Live By: The Computer Science of Human DecisionsFrom EverandAlgorithms to Live By: The Computer Science of Human DecisionsRating: 4.5 out of 5 stars4.5/5 (722)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- An Autobiography of Trauma: A Healing JourneyFrom EverandAn Autobiography of Trauma: A Healing JourneyRating: 5 out of 5 stars5/5 (2)