Professional Documents
Culture Documents
AUBF Prelim Topics
Uploaded by
Jean Calubag CatalanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
AUBF Prelim Topics
Uploaded by
Jean Calubag CatalanCopyright:
Available Formats
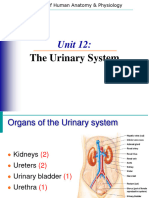
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
Blood enters the capillaries > afferent arteriole> flows through
the glomerulus> efferent arteriole
Nephron - functional units (1 to 1.5 million) Sizes of these arterioles
help to create the hydrostatic pressure differential
2 types of nephrons: important for glomerular filtration
Cortical nephrons maintain consistency of glomerular capillary pressure and
approximately 85% of nephrons renal blood flow within the glomerulus
cortex of the kidney
responsible primarily for removal of waste Smaller size of the efferent arteriole
products increases the glomerular capillary pressure
reabsorption of nutrients
Juxtamedullary nephrons (Before returning to the renal vein)
longer loops of Henle blood from the efferent arteriole enters> peritubular capillaries>
primary function is concentration of the urine vasa recta> cortex and medulla of the kidney close to the tubules
Kidney Peritubular capillaries
clear waste products selectively from the blood surround the proximal and distal convoluted tubules
maintain the body’s essential water and electrolyte reabsorption of essential substances from the fluid
balances (proximal convoluted tubule)
final adjustment of the urinary composition (distal
Renal functions: convoluted tubule)
a. renal blood flow
b. glomerular filtration Vasa recta
c. tubular reabsorption loops of Henle in juxtamedullary nephrons (adjacent to
d. tubular secretion ascending and descending)
Renal Blood Flow Osmotic gradient (salt concentration)
renal artery supplies blood to the kidney major exchanges of water and salts take place between the
human kidneys (approximately 25% of the blood pumped blood and the medullary interstitium
through the heart) necessary for renal concentration
Bsmls- 3c l Catalan, Jean C.
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
Average body size 3 glomerular filtration barrier cellular layers
1.73 m2 of surface a. the capillary wall membrane
b. the basement membrane (basal lamina)
Total renal blood flow c. visceral epithelium of Bowman’s capsule
1200 mL/min
Endothelial cells of the capillary wall
Total renal plasma flow containing pores and are referred to as fenestrated (differs)
600 to 700 mL/min pores increase capillary permeability but do not allow the
passage of large molecules and blood cells
Glomerular filtration rate (GFR)
calculated determine whether the observed measurements Basement membrane
represent normal function restriction of large molecules occurs as the filtrate
Glomerular Filtration Thin membranes
consists of a coil (eight capillary lobes) covering the filtration slits formed by the intertwining foot
processes of the podocytes of the inner layer of Bowman’s
Walls of Glomerular Filtration capsule
glomerular filtration barrier
Structure of the glomerular filtration barrier
located within Bowman’s capsule
contains a shield of negativity that repels molecules with a
serves as a nonselective filter of plasma substances
positive charge
with molecular weights less than 70,000
shield is very important because albumin (the primary
protein associated with renal disease) has a positive charge
Several factors influence the actual filtration process
and would easily pass through the barrier
cellular structure of the capillary walls and Bowman’s
capsule
Glomerular Pressure
hydrostatic pressure and oncotic pressure
renin-angiotensin-aldosterone system (RAAS) Hydrostatic pressure
resulting from the smaller size of the efferent arteriole
Cellular Structure of the Glomerulus glomerular capillaries enhances filtration
Plasma filtrate must pass through; (opposition of pressures from the fluid within Bowman’s capsule
and oncotic pressure of unfiltered plasma proteins in the glomerular
capillaries)
Bsmls- 3c l Catalan, Jean C.
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
Autoregulatory mechanism (juxtaglomerular apparatus) Renin
maintains the glomerular blood pressure at a relatively an enzyme produced by the juxtaglomerular cells
constant rate regardless of fluctuations in systemic blood secreted and reacts with the blood-borne substrate
pressure angiotensinogen to produce the inert hormone
angiotensin I
Dilation of the afferent arterioles and constriction of the angiotensin I (passes through the alveoli of the lungs)> angiotensin-
efferent arterioles when blood pressure drops; converting enzyme ACE (change) > angiotensin II (active form)>
decrease in blood flowing through the kidney corrects renal blood flow in the following ways:
preventing an increase in the blood level of toxic waste
products. a. causing vasodilation of the afferent arterioles and
increase in blood pressure constriction of the efferent arterioles
results in constriction of the afferent arterioles to prevent b. stimulating reabsorption of sodium and water in the
overfiltration or damage to the glomerulus proximal convoluted tubules, and
c. triggering the release of the sodium-retaining hormone
Renin-Angiotensin-Aldosterone System aldosterone by the adrenal cortex
flow of blood to and within the glomerulus d. antidiuretic hormone by the hypothalamus
system responds to changes in blood pressure and plasma
sodium content systemic blood pressure and plasma sodium content
increase, the secretion of renin decreases
Juxtaglomerular apparatus the actions of angiotensin II produce a constant pressure
consists of the juxtaglomerular cells within the nephron.
macula densa
every minute approximately two to three million glomeruli
Low plasma sodium content filter
resulting in a decreased overall blood volume and approximately 120 mL of water-containing low-molecular-
subsequent decrease in blood pressure weight substances
macula densa senses such changes, a cascade of reactions filtration is nonselective
within the RAAS occurs
Bsmls- 3c l Catalan, Jean C.
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
Difference between the compositions of the filtrate and the Electrochemical energy
plasma this interaction transfers the substance across the cell
membranes and back into the bloodstream
absence of plasma protein, any protein-bound substances,
and cells Passive transport
differences in their concentration or electrical potential on
Analysis of the fluid
opposite sides of the membrane.
shows the filtrate to have a specific gravity of 1.010 These physical differences are called gradients
chemically an ultrafiltrate of plasma
Passive reabsorption of water
all parts of the nephron except the ascending loop of Henle
Tubular Reabsorption the walls of which are impermeable to water.
the body cannot lose 120 mL of water-containing essential Urea
substances every minute passively reabsorbed in the proximal convoluted tubule and
plasma ultrafiltrate enters the proximal convoluted tubule the ascending loop of Henle, and
through cellular transport mechanisms (begin reabsorbing
these essential substances and water) Passive reabsorption of sodium
accompanies the active transport of chloride in the
Reabsorption Mechanisms ascending loop
The cellular mechanisms are termed; plasma concentration
active transport a substance that is normally completely reabsorbed reaches
passive transport an abnormally high level
the filtrate concentration exceeds the maximal
Active transport reabsorptive capacity (Tm)
the substance to be reabsorbed must combine with a carrier the substance begins appearing in the urine.
protein
responsible for the reabsorption of glucose, amino acids plasma concentration
and salts in the proximal convoluted tubule, chloride in the active transport stops is termed the renal threshold
ascending loop of Henle, and sodium in the distal
convoluted tubule
Bsmls- 3c l Catalan, Jean C.
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
For glucose, the plasma renal threshold is 160 to 180 mg/dL, The sodium and chloride leaving the filtrate in the ascending loop
and glucose appears in the urine when the plasma prevent dilution of the medullary interstitium by the water
concentration reaches this level. reabsorbed
from the descending loop.
Renal threshold and the plasma concentration Maintenance of this osmotic gradient is essential for the
can be used to distinguish between excess solute filtration final concentration of the filtrate when it reaches the
and renal tubular damage collecting duct
Active transport of more than two-thirds of the filtered sodium out Concentration of the filtrate leaving the ascending loop is
of the proximal convoluted tubule quite low owing to the reabsorption of salt and not water in
accompanied by the passive reabsorption of an equal that part of the tubule
amount of water Reabsorption of sodium continues in the distal convoluted
the fluid leaving the proximal convoluted tubule still tubule, but it is now under the control of the hormone
maintains the same concentration as the ultrafiltrate aldosterone, which regulates reabsorption in response to
the body’s need for sodium
Tubular Concentration
Collecting Duct Concentration
Renal concentration
begins in the descending and ascending loops of Henle, The final concentration of the filtrate through the reabsorption
where of water begins in the late distal convoluted tubule and continues in
the filtrate is exposed to the high osmotic gradient of the the collecting duct
renal medulla
Reabsorption depends on the osmotic gradient in the
Water (removed by osmosis in the descending loop of Henle)> medulla and the hormone vasopressin (antidiuretic
sodium and chloride (reabsorbed in the ascending loop)> Excessive hormone [ADH])
reabsorption of water ( filtrate passes through the highly the dilute filtrate in the collecting duct comes in contact
concentrated medulla is prevented by the water-impermeable walls with the higher osmotic concentration of the medullary
of the ascending loop) interstitium, passive reabsorption of water would occurthe
process is controlled by the presence or absence of ADH
selective reabsorption process A high level of ADH increases permeability, resulting in
called the countercurrent mechanism increased reabsorption of water, and a low-volume
serves to maintain the osmotic gradient of the medulla concentrated urine
Bsmls- 3c l Catalan, Jean C.
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
absence of ADH renders the walls impermeable to water, dissociate from their carrier proteins, which results in their
resulting in a large volume of dilute urine transport into the filtrate by the tubular cells
The major site for removal of these nonfiltered substances
production of aldosterone is controlled by the body’s is the proximal convoluted tubule
sodium concentration
production of ADH is determined by the state of body Acid–Base Balance
hydration blood pH of 7.4,the blood must buffer and eliminate the
the chemical balance in the body is actually the final excess acid formed by dietary intake and body metabolism
determinant of urine volume and concentration (maintain n.ph)
The concept of ADH control can be summarized in the following buffering capacity of the blood
manner: depends on bicarbonate (HCO3 –) readily filtered by the
↑Body Hydration = ↓ADH = ↑Urine Volume glomerulus returned to the blood to maintain the proper pH
↓Body Hydration = ↑ADH = ↓Urine Volume
secretion of hydrogen ions (H+)
Tubular Secretion prevents the filtered bicarbonate from being excreted in the
involves the passage of substances from the blood in the urine
peritubular capillaries to the tubular filtrate causes the return of a bicarbonate ion to the plasma
provides for almost 100% reabsorption of filtered
2 major functions: bicarbonate and occurs primarily in the proximal convoluted
eliminating waste products not filtered by the glomerulus tubule
regulating the acid–base balance in the body through the As a result of their small molecular size, hydrogen ions are
secretion of hydrogen ions. readily filtered and reabsorbed. the actual excretion of
excess hydrogen ions also depends on tubular secretion.
Foreign substances (medications)
cannot be filtered by the glomerulus because they are ammonia reacts with the H+
bound to plasma proteins to form the ammonium ion (NH4 +)
The resulting ammonium ion is excreted in the urine
When these protein-bound substances enter the peritubular A disruption in these secretory functions can result in
capillaries metabolic acidosis or renal tubular acidosis, the inability to
develop a stronger affinity for the tubular cells produce an acid urine
Bsmls- 3c l Catalan, Jean C.
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
Bsmls- 3c l Catalan, Jean C.
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
cleared of a substance per minute.
Standard test measuring:
Glomerular Filtration Tests a. Filtering capacity of the glomeruli
used to measure the filtering capacity of the glomeruli termed b. Measures rate at which kidneys are able to remove
as clearance tests filterable substances from the blood
About 1200 mL of blood (650 mL plasma) passes through the
kidneys, every minute
About 120-125 mL is filtered per minute by the kidneys & this
is referred to as glomerular filtration rate (GFR) RENAL FUNCTION TESTS
With a normal GFR (120-125 mL/min), the glomerular filtrate • U = Concentration of the substance in urine.
formed in an adult is about 175-180 litres/day, out of • V = Volume of urine in ml excreted per minute.
which only 1.5 litres is excreted as urine. • P = Concentration of the substance in plasma.
Clearance test Primary substances used in clearance tests
measures the rate at which the kidneys are able to remove (to 1. Creatinine
clear) a filterable substance from the blood 2. beta2-microglobulin
3. cystatin C
To test accuracy of the substance being measured: 4. radioisotopes
1) Substance analyzed must be neither
reabsorbed nor secreted by the tubules Exogenous procedure
2) Stable in a 24-hour collected urine A test that requires an infused substance
3) Consistent in the plasma level
4) Availability of the substance in the body Endogenous procedure
5) availability of the tests for chemical analysis seldom the method of choice if a suitable test substance is already
of the substance present in the body
Clearance Tests Creatinine Clearance
A variety of substances have been used to measure the GFR a waste product of muscle metabolism that is produced
measures the rate at which the kidneys are able to remove (to enzymatically by creatine phosphokinase from creatine, which
clear) a filterable substance from the blood links with ATP to produce ADP and energy
defined as the volume of plasma that would be completely
Bsmls- 3c l Catalan, Jean C.
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
Newer methods that do not require the collection of timed (24-
hour) urine specimens have been developed using just the serum 6. Cystatin C
creatinine, cystatin C, or beta2-microglobulin values. The results of Low molecular weight
these tests are reported as estimated glomerular filtration rate (eGFR) Potential marker for long-term monitoring of renal function
Constant in serum levels
Clearance Test Substance Independent of age, gender, and muscle mass
Higher analysis cost
1. Urea
Present in all urine specimen but replaced by other
substances Calculations (Creatinine Clearance)
2. Inulin 1. Greatest source of error: improper timed specimen
Polymer of fructose 2. GFR reported in mL/min.
Extremely stable substance not reabsorbed nor secreted by the 3.
tubules
U = urine creatinine in mg/dL
Not a normal body constituent and infused at a constant rate
throughout the testing period V = urine volume in mL/min.
Seldom choice if suitable substance is already present in the body P = plasma creatinine in mg/dL
3. Radionucleotides Ex #1. Calculate the urine volume for a 4-hour specimen measuring
Measures plasma disappearance of infused substances thus 1L:
eliminating need for urine collection 4 hours X 60 minutes = 240 minutes
Injection of radionucleotides to:
1000mL
visualize plasma disappearance of radioactive material
enable visualization of the filtration of one or both kidneys 240 minutes
= 4.17 mL/min (volume)
4. β2microglobulin
Dissociates from human leukocyte antigen and removed from the Standard Formula to calculate millilitres of plasma cleared
plasma by glomerular filtration per minute (C) is:
Increased in patients with inflammatory conditions, autoimmune
disorders, viral infections, multiple myeloma
Beta2-microglobulin (molecular weight 11,800)
Ex #2. Using urine creatinine of 400 mg/dL (U), plasma creatinine
5. Creatinine of 5.0 mg/dL (P), and urine volume of 2500 mL obtained from a
Waste product of muscle metabolism and found at a constant 24-hour specimen (V), calculate the glomerular filtration rate.
rate in the blood
V = 2500 mL = 1.74 mL/min.
Bsmls- 3c l Catalan, Jean C.
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
60 minutes X 24 hours = 1440 minutes Renal Threshold Of A Substance
C = 400 mg/dL (U) X 1.74 mL/min. (V) = 139.2 mL/min. is defined as its concentration in blood (or plasma) beyond
5.0 mg/dL (P) which it is excreted into urine.
Reference values: a. Glucose is 180 mg/dL
• The normal range of creatinine clearance is around 120-145 b. Ketone bodies 3 mg/dL
mL/min. c. Calcium 10 mg/dL
• These values are slightly lower in women. d. Bicarbonate 30 mEq/L
Men (107 to 139 mL/min.)
Women (87 to 107 mL/min.) Tubular maximum (Tm):
The maximum capacity of the kidneys to absorb a particular
Serum creatinine normal range: substance.
Adult male: 0.7-1.4 mg/dl a. Glucose: 350 mg/min
Adult female: 0.6-1.3 mg/dl
Children: 0.5-1.2 mg/dl 2. Tubular Reabsorption Test
Also known as Concentration tests
Clinical Significance in the interpretation of results for
Creatinine Clearance: Water Deprivation Tests
1. Determines the number of functioning nephrons 1. Fishberg Test - patients deprived of fluid for
2. Functional capacity of the nephrons 24 hours prior to measuring the specific
gravity
Results may be used to: 2. Mosenthal Test – compared the volume of
Measure extent of nephron damage day and night urine samples to evaluate
Monitor effectiveness of treatment in the prevention of further concentrating ability
nephron damage
Determine feasibility of administering medications Free Water Clearance
a. How much water must be cleared each minute to produce a urine
Renal Threshold Substances with the same osmolarity as with the plasma
• certain substances in the blood have excretion rate in urine b. Determines the ability of the kidney to respond to the state of
dependent on their concentration. body hydration
• At a normal concentration in the blood, they are completely
reabsorbed by the kidneys.
Bsmls- 3c l Catalan, Jean C.
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
b. turbidity
3. Tubular Secretion and Renal Blood Flow Tests c. Odor
Test to measure tubular secretion of nonfiltered substances d. Volume
and renal blood flow e. Viscosity
1. ρ-amino hippuric acid test (PAH) using the dye f. Sweetness
phenolsulfonphthalein
a. test substance easily removed from the blood each time it Modern urinalysis basic observation
comes in contact with a functional renal Tissue a. physical examination of urine
b. does not combine with plasma proteins b. chemical analysis
c. removed completely from the blood c. microscopic examination of urinary sediment
d. not anymore performed especially using the dye PSP because
of concern over interference of medications and elevated History of medicine (well-known names)
waste products in patient’s serum Hippocrates
e. possible anaphylactic shock Who wrote a book on “uroscopy” 5th century BCE
Frederik Dekkers’
2. Titratable Acidity & Urinary Ammonia Discovery in 1694 of albuminuria by boiling urine (Chemical testing
a. Ability of kidney to produce acid urine depends on tubular progressed from “ant testing” and “taste testing” for glucose)
excretion of ammonia by the cells of the DCT Thomas Bryant
b. Inability to produce acid urine: Renal Tubular Acidosis The Charlatans called “pisse prophets,” became the subject of a
c. Measurement of total hydrogen ion excretion in urine book published in 1627
Thomas Addis
Quantitating the microscopic sediment
Richard Bright
Introduced the concept of urinalysis as part of a doctor’s routine
patient examination in 1827
History and Importance
Two unique characteristics of a urine specimen account
References study of urine
for this continued popularity:
found in drawings of cavemen and in Egyptian hieroglyphics
1. Urine is a readily available and easily collected
(Edwin Smith Surgical Papyrus)
specimen
bladder-shaped flask of urine
2. Urine contains information, which can be obtained by
inexpensive laboratory tests, about many of the body’s
Basic observations
major metabolic functions.
a. color
Bsmls- 3c l Catalan, Jean C.
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
Clinical and Laboratory Standards Institute (CLSI) Major inorganic substances solid dissolved in urine
Defines urinalysis as “the testing of urine with procedures a. Chloride
commonly performed in an expeditious, reliable, accurate, safe, b. Sodium
c. Potassium
and cost-effective manner”
Dietary intake
Urine Formation influences the concentrations of these inorganic
Kidneys continuously form urine as an ultrafiltrate of Plasma compounds, making it difficult to establish normal levels
Re-absorption of water and filtered substances essential
to body function converts approximately 170,000 mL of Other substances found in urine include:
a. Hormones
filtered plasma to the average daily urine output of 1200 mL.
b. Vitamins
c. medications
Urine Composition
Urine Urine Volume
consists of urea and other organic and inorganic chemicals Water
dissolved in water A major body constituent
It may contain formed elements, such as cells, casts, crystals, It determined by the body’s state of hydration.
mucus, and bacteria (↑ indicative of disease)
95% water Factors that influence urine volume
5% solutes a. fluid intake
Influence factors of solute b. fluid loss from non renal sources
a. dietary intake c. variations in the secretion of antidiuretic hormone
b. physical activity d. to excrete increased amounts of dissolved solids glucose or
c. body metabolism salts
d. endocrine functions
The normal daily urine
Urea 1200 to 1500 mL
a metabolic waste product produced in the liver from
the breakdown of protein and amino acids
It range of
600 to 2000 mL considered normal
Other organic substances
a. Creatinine Oliguria
b. Uric acid a decrease in urine output
less than 1 mL/kg/hr in infants
Bsmls- 3c l Catalan, Jean C.
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
less than 0.5 mL/kg/hr in children Although appearing to be dilute, a urine specimen from a
less than 400 mL/day in adults patient with diabetes mellitus has a high specific gravity because
of the in creased glucose content
- commonly seen when the body enters a state of dehydration as a
result of excessive water loss from vomiting, diarrhea, perspiration, Diabetes insipidus
results from a decrease in the production or function of
or severe burns
antidiuretic hormone (ADH)
Anuria the water necessary for adequate body hydration is not
reabsorbed from the plasma filtrate
Day time
the urine is truly dilute and has a low specific gravity. Fluid loss in
cessation of urine flow both diseases is compensated by increased ingestion of water
may result from any serious damage to the kidneys or (polydipsia), producing an even greater urine volume. Polyuria
decrease in the flow of blood to the kidneys accompanied by increased fluid intake is often the first symptom
of either disease
Nocturia
An increase in the nocturnal excretion of urine
Polyuria
an increase in daily urine volume
2.5 L/day in adults (greater than normal value)
2.5 to 3 mL/kg/day in children
- is often associated with diabetes mellitus and diabetes insipidus
however, it may be artificially induced by diuretics, caffeine, or
alcohol, all of which suppress the secretion of antidiuretic hormone.
Diabetes mellitus
caused by a defect either in the pancreatic production of insulin
or in the function of insulin (↑ results of body glucose
concentration)
The kidneys do not reabsorb excess glucose, necessitating
excretion of increased amounts of water to remove the
dissolved glucose from the body
Bsmls- 3c l Catalan, Jean C.
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
Specimen Collection straw. The transfer straw has a needle and an evacuated tube
urine is a biohazardous substance that requires the observance holder
of Standard Precautions
Gloves should be worn at all times when in contact with the Labels
specimen Patient’s name
Identification number
Containers Date and time of collection
Specimens must be collected in
a. Clean Additional information
b. dry Patient’s age
c. leak-proof containers Location
d. screw-top lids Healthcare provider’s name
e. wide mouthand flat bottom to facilitate collection (female
patients) - Labels must be attached to the container, not to thelid, and should
f. Disposable containers should be use not become detached if the container is refrigerated or frozen
g. variety of sizes and shapes
h. bags with adhesive for the collection of pediatric specimens Requisitions
i. large containers for 24-hour specimens Requisition form (manual or computerized)
accompany specimens delivered to the laboratory
match the information on the specimen label
Capacity of the container
50 mL
Additional information on the form
allows 12 mL of specimen needed for microscopic analysis
a. method of collection or type of specimen
and repeat analysis
b. possible interfering medications
c. patient’s clinical information
Packaged sterile containers with secure
closures should beused for microbiologic urine studies
- The time the specimen is received in the laboratory should be
recorded on the form
- Sterile containers are also suggested if more than 2 hours elapse
between specimen collection and analysis.
-A designed sterile containers are available that have a lid with a
transfer device that can be assessed with a device called a transfer
Bsmls- 3c l Catalan, Jean C.
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
Specimen Rejection Specimen Preservation
Improperly labeled and collected specimens should be rejected by Most routinely used method of preservation
the laboratory, and appropriate personnel should be notified to refrigeration at 2°C to 8°C (decreases bacterial growth and
collect a new specimen. Unacceptable situations include: metabolism)
1. Specimens in unlabeled containers
2. Nonmatching labels and requisition forms - If the urine is to be cultured, it should be refrigerated
3. Specimens contaminated with feces or toilet paper during transit and kept refrigerated until cultured up to
4. Containers with contaminated exteriors 24 hours
5. Specimens of insufficient quantity
6. Specimens that have been improperly transported Types of Specimens
Laboratories should have a written policy detailing their To obtain a specimen that is representative of a patient’s
conditions for specimen rejection. metabolic state, regulation of certain aspects of specimen
collection is often necessary.
Specimen Handling
a urine specimen is so readily available and easily collected Special conditions may include
often leads to laxity in the treatment of specimen after its time
collection length
Changes in urine composition take place not only in vivo but method of collection
also in vitro, thus requiring correct handling procedures patient’s dietary and medicinal intake
Specimen Integrity Random Specimen
Specimen most commonly received specimen
delivered to the laboratory promptly and tested within 2 hours may be collected at any time but the actual time of voiding
A specimen that cannot be delivered and tested within 2 hours should be recorded on the container
should be refrigerated or have an appropriate chemical useful for routine screening tests to detect obvious
preservative abnormalities
- Most significant changes that may occur in a specimen allowed to - it may also show erroneous results resulting from dietary intake or
unpreserved at room temperature for longer than 2 hours physical activity just before collection.
(presence and growth of bacteria)
First Morning Specimen
ideal screening specimen
Bsmls- 3c l Catalan, Jean C.
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
require the patient to make an additional trip to the laboratory Many solutes exhibit diurnal variations
essential for preventing false-negative pregnancy tests a. catecholamines
and for evaluating orthostatic proteinuria b. 17- hydroxysteroids
first morning specimen is a concentrated specimen c. electrolytes
- The patient should be instructed to collect the specimen - When the concentration of the substance to be measured changes
immediately on arising and to deliver it to the laboratory within 2 with diurnal variations and with daily activities such as exercise,
hours or keep it refrigerated. meals, and body metabolism, 24-hour collection is required If the
concentration of a particular substance remains constant, the
specimen may be collected over a shorter period.
- The concentration of a substance in a particular period must be
calculated from the urine volume produced during that time.
On its arrival in the laboratory, a 24-hour specimen must be
thoroughly mixed and the volume accurately measured and
recorded.
- All specimens should be refrigerated or kept on ice during the
collection period and may also require addition of a chemical
preservative.
Catheterized Specimen
collected under sterile conditions by passing a hollow tube
(catheter) through the urethra into the bladder
24-Hour (or Timed) Specimen
Most commonly requested test in C.S
A carefully timed specimen must be used to produce accurate bacterial culture
quantitative results
The patient must begin and end the collection period with an Midstream Clean-Catch Specimen
empty bladder an alternative to the catheterized specimen
lowest concentration is in the early morning provides a safer, less traumatic method for obtaining urine for
highest concentration occurs in the afternoon bacterial culture and routine urinalysis
It provides a specimen that is less contaminated by epithelial
Bsmls- 3c l Catalan, Jean C.
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
cells and bacteria Second specimen
representative of the actual urine than the routinely voided used as a control for bladder and kidney infection If it is
specimen positive, the results from the third specimen are invalid
because infected urine has contaminated the specimen
Suprapubic Aspiration
collected by external introduction of a needle through the Pre- and Post-Massage Test
abdomen into the bladder a clean-catch mid stream urine specimen is collected
provides a sample for bacterial culture that is completely a second urine sample is collected after the prostate is
free of extraneous contamination massaged
The specimen can also be used for cytologic examination a positive result is significant bacteriuria in the post-massage
specimen of greater than 10 times the premassage count
Prostatitis Specimen Pediatric Specimens
Several methods are available to detect the presence of Soft, clear plastic bags with hypoallergenic skin adhesive to
prostatitis attach to the genital area of both boys and girls
Three-Glass Collection Sterile specimens may be obtained by catheterization or by
Male mid stream clean-catch procedure suprapubic aspiration
1. the first urine passed, it is collected in a sterile container
2. the midstream portion is collected in another sterile container Routine specimen analysis
3. the prostate is then massaged so that prostate fluid will be 1. ensure the area is free of contamination
passed with the remaining urine into a third sterile container 2. Attach the bag firmly over the genital area avoiding the anus
3. When enough specimen has been collected, remove the bag
Quantitative cultures and label it or pour the specimen into container and label the
performed on all specimens container following institutional policy
First and third specimens Microbiology specimens
examined microscopically 1. clean the area with soap and water and sterilely dry the area,
In prostatic infection removing any residual soap residue
Third specimen 2. Firmly apply a sterile bag
will have a white blood cell/ high-power field count and a 3. Sterilely transfer collected specimen into a sterile container
bacterial count 10 times that of the first specimen and label the container
macrophages containing lipids may also be present.
Drug Specimen Collection
Urine specimen collection is the most vulnerable part of
a drug-testing program.
Bsmls- 3c l Catalan, Jean C.
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
The chain of custody (COC) is the process that provides this
documentation of proper sample identification from the time
of collection to the receipt of laboratory results
For urine specimens to withstand legal scrutiny, it is necessary
to prove that no tampering of the specimen occurred, such as
substitution, adulteration, or dilution.
Proper identification of the individual whose information is
indicated on the label is required. Either photo identification or
positive identification by an employer representative with
photo ID is acceptable
Urine specimen collections may be “witnessed” or “un
witnessed.”
The urine temperature must be taken within 4 minutes
from the time of collection
The temperature should read within the range of 32.5°C to
37.7°C. The urine color is also inspected to identify any signs of
contaminants
Bsmls- 3c l Catalan, Jean C.
TAGUM DOCTORS COLLEGE INC.
PRE-LIM
Urinalysis and Body Fluids Romans 8:28
Bsmls- 3c l Catalan, Jean C.
You might also like
- Urine ProductionDocument17 pagesUrine ProductionLeonardo Balondo DulaNo ratings yet
- Renal Anatomy & Physiology OverviewDocument5 pagesRenal Anatomy & Physiology OverviewChristopher BucuNo ratings yet
- Renal Function SummaryDocument5 pagesRenal Function SummaryBanana QNo ratings yet
- Anatomy Excretory System NotesDocument5 pagesAnatomy Excretory System NotesrincyNo ratings yet
- ANATOMI FISIOLOGI - PakaiDocument54 pagesANATOMI FISIOLOGI - PakaihairunnisaaaNo ratings yet
- Phys 7Document77 pagesPhys 7sakwork30No ratings yet
- Urinary System and Nephron AnatomyDocument59 pagesUrinary System and Nephron AnatomyLove Jovellanos ÜNo ratings yet
- Urinary System: G R O U P 4 - B S N 1 - 5Document59 pagesUrinary System: G R O U P 4 - B S N 1 - 5Love Jovellanos ÜNo ratings yet
- Renal Physio 1-3 (2018)Document15 pagesRenal Physio 1-3 (2018)Janica Marie RagsacNo ratings yet
- Analysis of Urine and Body Fluids FunctionsDocument5 pagesAnalysis of Urine and Body Fluids FunctionsBEVERLY JANE LLUVERASNo ratings yet
- Glomerular Filtration: An Overview: Mary Jo HolechekDocument8 pagesGlomerular Filtration: An Overview: Mary Jo HolechekagaasfaNo ratings yet
- Filtrasi GlomerulusDocument41 pagesFiltrasi GlomerulusFaishalNo ratings yet
- Lecture 19 Urinary Sys BIOL3571 F2023Document55 pagesLecture 19 Urinary Sys BIOL3571 F2023thesoccerprince.10No ratings yet
- Renal Physiology PDFDocument12 pagesRenal Physiology PDFLolitaNo ratings yet
- Renal Function AubfDocument11 pagesRenal Function AubfHANNA CASANDRA GARCIANo ratings yet
- Urine FormationDocument49 pagesUrine FormationCor GuerreroNo ratings yet
- Chronic Kidney Disease in Children New Trends in ManagementDocument103 pagesChronic Kidney Disease in Children New Trends in Managementfranklin ifioraNo ratings yet
- Strasinger AUBFDocument44 pagesStrasinger AUBFangela tanteoNo ratings yet
- Renal Physiology and Fluid BalanceDocument71 pagesRenal Physiology and Fluid BalanceparthNo ratings yet
- Fundamental of Urinary System (2020)Document55 pagesFundamental of Urinary System (2020)Nadya PutriNo ratings yet
- The Kidneys: DevelopingDocument18 pagesThe Kidneys: Developingmaria sanchezNo ratings yet
- Renal Lecture 1 PDFDocument29 pagesRenal Lecture 1 PDFSirajum MuneeraNo ratings yet
- The Normal Kidney: Pediatrics 2 The Urinary System and Urinary Tract InfectionsDocument4 pagesThe Normal Kidney: Pediatrics 2 The Urinary System and Urinary Tract Infectionssarguss14No ratings yet
- UrinaryDocument68 pagesUrinaryPharmswipe KenyaNo ratings yet
- Function: FiltrationDocument2 pagesFunction: FiltrationSaad KhanNo ratings yet
- Urinary System TransesDocument5 pagesUrinary System Transesadrielvamos28No ratings yet
- Basic Dialysis Theory SweenyDocument28 pagesBasic Dialysis Theory SweenyAmmar YasserNo ratings yet
- Kidney Functions and AnatomyDocument17 pagesKidney Functions and AnatomyAmy Lalringhluani100% (1)
- Chapter 26: Introduction To The Urinary SystemDocument37 pagesChapter 26: Introduction To The Urinary Systemmaatela7sasNo ratings yet
- Renal Physiology and FunctionDocument4 pagesRenal Physiology and FunctionDayledaniel Sorveto100% (1)
- D - Renal PhysiologyDocument26 pagesD - Renal PhysiologyMohamad Zekry ZuhairyNo ratings yet
- Renal PhysiologyDocument129 pagesRenal PhysiologyPhysiology by Dr Raghuveer100% (3)
- Urinalysis Anatomy and PhysiologyDocument3 pagesUrinalysis Anatomy and PhysiologyMonica DomingoNo ratings yet
- K10 Kuliah NefrourologiDocument170 pagesK10 Kuliah NefrourologimarinanananaNo ratings yet
- VSP-UG-7 (Kidney - Excretory System)Document50 pagesVSP-UG-7 (Kidney - Excretory System)6qhx62pr42No ratings yet
- Pathophysiology of KidneysDocument35 pagesPathophysiology of KidneysAli Aborges Jr.No ratings yet
- RFT FinalDocument90 pagesRFT Finaldr JoeNo ratings yet
- ANPH111 REVIEWER [URINARY & ENDOCRINE]Document7 pagesANPH111 REVIEWER [URINARY & ENDOCRINE]Maria Clarisse ReyesNo ratings yet
- CH ExcretionDocument9 pagesCH ExcretionlatasabarikNo ratings yet
- Renal Physiology: Xiaohong XiaDocument128 pagesRenal Physiology: Xiaohong XiashaheenNo ratings yet
- Chapter 20 HomeostasisDocument8 pagesChapter 20 HomeostasisLisa AllisyaNo ratings yet
- Chapter 33 - Organization of The Urinary SystemDocument4 pagesChapter 33 - Organization of The Urinary SystemErik CollaoNo ratings yet
- 10th Grade Chapter 12 Part 2 (the Human Excretory System)Document16 pages10th Grade Chapter 12 Part 2 (the Human Excretory System)baselfawadlehNo ratings yet
- LESSON 3 Renal Function and TestsDocument63 pagesLESSON 3 Renal Function and TestsFaith TambongNo ratings yet
- Renal Physiology: Done byDocument28 pagesRenal Physiology: Done byJanine Marie Kathleen Uy-CuanangNo ratings yet
- Kidney Physiology (Q & A)Document28 pagesKidney Physiology (Q & A)ramadan100% (1)
- K10 (Histopatologi Kelainan Ginjal)Document181 pagesK10 (Histopatologi Kelainan Ginjal)Nyimas Yuli YantiNo ratings yet
- Physiology, Lecture 6, Urinary SystemDocument74 pagesPhysiology, Lecture 6, Urinary SystemAli Al-QudsiNo ratings yet
- MBBS renal physiology lecture notesDocument129 pagesMBBS renal physiology lecture notesNayyer Khan83% (6)
- Renal PhysiologyDocument8 pagesRenal PhysiologyAlejandra Bautista OsorioNo ratings yet
- MC I Modular Reviewer Urinary SystemDocument12 pagesMC I Modular Reviewer Urinary SystemSteiner LimNo ratings yet
- Urinary System: Quick Review Review of Urinary Anatomy & Physiology Ureters, Bladder, UrethraDocument6 pagesUrinary System: Quick Review Review of Urinary Anatomy & Physiology Ureters, Bladder, UrethraLongyapon Sheena StephanieNo ratings yet
- Urinary SystemDocument9 pagesUrinary SystemPrincess OrsinoNo ratings yet
- Regulating Renal Blood Flow and Glomerular FiltrationDocument41 pagesRegulating Renal Blood Flow and Glomerular FiltrationAfk SystemNo ratings yet
- 3.4 Homeostasis in Humans (Volume 2) : Prepared By: PN Nadhirah Binti Abdul Haziz Biology Teacher SMK Puteri WilayahDocument15 pages3.4 Homeostasis in Humans (Volume 2) : Prepared By: PN Nadhirah Binti Abdul Haziz Biology Teacher SMK Puteri WilayahPutri MalayaNo ratings yet
- Renal Reflections: Exploring the Marvels of Nephrology: The Intricate Ballet of Kidney Functions UnveiledFrom EverandRenal Reflections: Exploring the Marvels of Nephrology: The Intricate Ballet of Kidney Functions UnveiledNo ratings yet
- Reverse Osmosis Treatment of Drinking WaterFrom EverandReverse Osmosis Treatment of Drinking WaterRating: 3.5 out of 5 stars3.5/5 (4)
- Specimen Transport and Storage Group 2Document19 pagesSpecimen Transport and Storage Group 2Jean Calubag CatalanNo ratings yet
- Hematology Lec PrelimDocument3 pagesHematology Lec PrelimJean Calubag CatalanNo ratings yet
- Pre Final ActivitiesDocument2 pagesPre Final ActivitiesJean Calubag CatalanNo ratings yet
- TrendssDocument1 pageTrendssJean Calubag CatalanNo ratings yet
- Rubella VirusDocument14 pagesRubella VirusJean Calubag CatalanNo ratings yet
- Elaizah PeDocument20 pagesElaizah PeJean Calubag CatalanNo ratings yet
- Pre Final ActivitiesDocument2 pagesPre Final ActivitiesJean Calubag CatalanNo ratings yet
- Rubella VirusDocument14 pagesRubella VirusJean Calubag CatalanNo ratings yet
- Hematology Lec PrelimDocument3 pagesHematology Lec PrelimJean Calubag CatalanNo ratings yet
- Histopathology - Lec Prelim 1Document43 pagesHistopathology - Lec Prelim 1Jean Calubag CatalanNo ratings yet
- Defense BacteriologyDocument2 pagesDefense BacteriologyJean Calubag CatalanNo ratings yet
- ENTEROBACTERIACEADocument12 pagesENTEROBACTERIACEAJean Calubag CatalanNo ratings yet
- Body Fluid 1Document55 pagesBody Fluid 1Anonymous z3afjyy1aNo ratings yet
- AUBF Notes 1Document11 pagesAUBF Notes 1Ice100% (4)
- Nephrotic and Nephritic - SyndromeDocument35 pagesNephrotic and Nephritic - SyndromeadinayNo ratings yet
- Class Activity Urine FormationDocument2 pagesClass Activity Urine FormationMaryam SheiduNo ratings yet
- 1987 NBDE 1 ASDA (Biochemistry & Physiology)Document63 pages1987 NBDE 1 ASDA (Biochemistry & Physiology)Karol BryantNo ratings yet
- AUBF Group 1 Chapter 8Document12 pagesAUBF Group 1 Chapter 8Gerald John PazNo ratings yet
- Dr.P.Sankaranarayanan MD: Emeritus Professor of Medicine Acs Medical College & HospitalDocument81 pagesDr.P.Sankaranarayanan MD: Emeritus Professor of Medicine Acs Medical College & HospitalvaishnaviNo ratings yet
- Fluids and Electrolytes NCM 101Document142 pagesFluids and Electrolytes NCM 101France John Evangelista Torres100% (2)
- BDS 2nd Year DM NotesDocument34 pagesBDS 2nd Year DM NotesPUBG VS FREE FIRENo ratings yet
- نماذج اسئلة الهيئة السعودية للتخصصات الصحية للاخصائيين والاطباء بالمختبراتDocument68 pagesنماذج اسئلة الهيئة السعودية للتخصصات الصحية للاخصائيين والاطباء بالمختبراتAhmed GaberNo ratings yet
- OU SumberDocument5 pagesOU SumberAnggaNo ratings yet
- Endocrine and Urinary SystemDocument5 pagesEndocrine and Urinary SystemShereen ManabilangNo ratings yet
- Reviews: Pathophysiology and Management of Hypokalemia: A Clinical PerspectiveDocument10 pagesReviews: Pathophysiology and Management of Hypokalemia: A Clinical PerspectiveWenny OktavianiNo ratings yet
- UrinaryDocument68 pagesUrinaryPharmswipe KenyaNo ratings yet
- MCQDocument14 pagesMCQalphonsajohnNo ratings yet
- ChoiDocument19 pagesChoiLuciana RafaelNo ratings yet
- UntitledDocument9 pagesUntitled박준수No ratings yet
- Internal Medicine - CardiologyDocument122 pagesInternal Medicine - CardiologySoleil Daddou100% (2)
- NBTS 03 RM SolDocument21 pagesNBTS 03 RM Solavik2001sharmaNo ratings yet
- PCO Answer Key-RED PACOPDocument40 pagesPCO Answer Key-RED PACOPViviengail GalosNo ratings yet
- PathoPhysiology of Renal Failure (Overview)Document7 pagesPathoPhysiology of Renal Failure (Overview)Tiger Knee100% (3)
- Biology Notes - CH - 5 Life Processes2Document5 pagesBiology Notes - CH - 5 Life Processes2AISHA AMAL ANDIKATTILASSLAM ANDIKATTILNo ratings yet
- MUST KNOW CLINICAL MICROSCOPY URINALYSISDocument43 pagesMUST KNOW CLINICAL MICROSCOPY URINALYSISMerhella Amor Suerte MendozaNo ratings yet
- IB BIO Midterm PrepDocument92 pagesIB BIO Midterm Prepptzpwpjk7gNo ratings yet
- Urinary SystemDocument34 pagesUrinary SystemJULIANNE ANACTANo ratings yet
- 4 - Kunci Jawaban Ipa Ucun 2 Smp-Mts - 2014-2015Document26 pages4 - Kunci Jawaban Ipa Ucun 2 Smp-Mts - 2014-2015shafa narariyaNo ratings yet
- Biology ProjectDocument24 pagesBiology ProjectMujib Ur RahmanNo ratings yet
- Misbah 2016-Tip AnswersDocument269 pagesMisbah 2016-Tip AnswersMahsa PourghasemNo ratings yet
- Urinary SystemDocument20 pagesUrinary SystemKelvin Mallari100% (1)
- Pharmacotherapeutics, Pharmacokinetics, and PharmacodynamicsDocument40 pagesPharmacotherapeutics, Pharmacokinetics, and PharmacodynamicsPerry BearNo ratings yet





































![ANPH111 REVIEWER [URINARY & ENDOCRINE]](https://imgv2-2-f.scribdassets.com/img/document/719863043/149x198/56e32fc029/1712198043?v=1)