Professional Documents
Culture Documents
Jugao, Teresita
Uploaded by
mobai.li.yuCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jugao, Teresita
Uploaded by
mobai.li.yuCopyright:
Available Formats
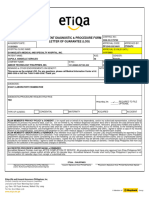
MEDICAL INFORMATION CENTER (MIC)
LETTER OF GUARANTEE (LOG) Number: 02-8895-3308
PLDT Toll Free: 1-800-10-895-3308
IN-PATIENT Email: mic@etiqa.com.ph
TO: Hospital Name CHINESE GENERAL HOSPITAL AND MEDICAL CENTER LOG NO. IP-2542-32904181
UNIT / DEPARTMENT: DATE: 10/03/2023
TEL. / FAX / EMAIL: 028-7114141 TIME: 02:00 PM
This is to certify that, as of this date, below-mentioned patient is a bonafide member of Etiqa Philippines occupying Room No. at PhP 3,800.00/day/category
REGULAR PRIVATE. He / She is entitled to the limits below under his / her plan and all necessary diagnostic and treatment services subject to the conditions /
limitations specified in the policy.
REMARKS:
PLEASE SEND SUMMARY AND ITEMIZED
SOA PRIOR TO DISCHARGE @ LO@etiqa.com.ph
INITIAL COVERAGE IS UP TO 100K
FOR ANY CONCERN PLEASE CONTACT
LO PAUL ANTHONY PEREZ
Paul.Perez@etiqa.com.ph
COMPANY NAME: MANILA ELECTRIC COMPANY (MERALCO) PRODUCT: MedProtect ___ / MedProtect+ ___ CLASS: 3
PATIENT NAME: JUGAO, TERESITA DATE OF BIRTH: 12/11/1957 AGE: 65
ID CARD NO.: 101-02518-263613-302 EFFECTIVE DATE: 01/01/2023 EXPIRY DATE: 12/31/2023
PRINCIPAL NAME: JUGAO, JASON DATE OF BIRTH: 06/02/1980 AGE: 43
RELATIONSHIP: PARENT ROOM & BOARD ALLOWED (AMOUNT/CATEGORY):
LARGE PRIVATE Max of PHP 2200
ADMISSION DATE & TIME: 10/03/2023 DISCHARGE DATE & TIME: 10/03/2023
INITIAL DIAGNOSIS: FINAL DIAGNOSIS:
(C649) MALIGNANT NEOPLASM OF KIDNEY, EXCEPT RENAL PELVIS, (C649) MALIGNANT NEOPLASM OF KIDNEY, EXCEPT RENAL PELVIS,
UNSPECIFIED SIDE UNSPECIFIED SIDE
PROCEDURE/S DONE/RUV/RVS: MAXIMUM BENEFIT LIMIT:
100,000.00
Accordingly, Etiqa Philippines agrees to pay all expenses incurred during his / her confinement based on our agreement, except the following (MARKED):
Difference in Room & Board PHILHEALTH: REQUIRED
All Incremental Charges of 20% for Hospital OPTIONAL
Excess in Professional Fees / PF of Non-Accredited
Ineligible Miscellaneous / Personal Charges Co-insurance / Co-Pay
Take Home Medicines Corridor Deductible
Professional Fees covered under Etiqa Philippines accredited rate:
Doctor's Name Specialty No. of Visit Amount Total
PLAN MEMBER'S PRIVACY POLICY & CONSENT: I, for myself and on behalf of my dependents, and/or my authorized representative, authorize Etiqa Philippines to process my
personal data, such as, but not limited to, my medical diagnosis/utilization data and to disclose the said personal data to necessary third parties such as, but not limited to, my
employer, accredited network providers, headquarter, reinsurers, group policy holders and auditors. I understand that the processing of my personal data shall be used in servicing my
account which includes, but is not limited, to the following benefits administration, medical treatment, and management of the plan. I agree to receive marketing updates and offers. I
agree to obtain a copy of my records relative to my hospitalization, consultation and treatment or any other medical advice in connection with the benefit/claim availed.
PLAN MEMBER'S UNDERTAKING & REMINDER: Plan Member must sign AFTER availment. Unused LOG should immediately be reported to Etiqa Philippines' Account
Reconciliation Exit Clearance. Final computation of your coverage will be made once Etiqa Philippines' Medical Claims Payables Department adjudicates your claims considering any
of the following: (a) any call-less availment; (b) reimbursement claims; and (c) unprocessed claims that are yet to be billed by the accredited network providers. I agree that any
availment may be denied under circumstances such as concealment and procedures not related to the illness. I agree to settle for billback any incurred ineligible excess charges on
benefits. I render Etiqa Philippines free from any liability on the collection of the acquired excess charges on benefits.
ACCREDITED PROVIDER'S UNDERTAKING & REMINDER:
Accredited Network Provider must sign AFTER COMPLETION OF SERVICE. All procedures/tests must have prior approval from Etiqa Philippines' MIC. For immediate payment,
please submit all bills within 30 calendar days. Accredited Network Provider shall notify Etiqa Philippines if payment is not received within 30 calendar days from receipt of submitted
bills. Send all billing statements and original supporting documents to Etiqa Philippines' Medical Claims Payables Department together with this LOG.
Date & Time Prepared: Conforme:
Issued by: Checked by: Date & Time Faxed:
PAUL ANTHONY PEREZ PAUL ANTHONY PEREZ Signature Over Printed Name of PlanMember and/or
Faxed by: Authorized Representative
Supervisor /
Liaison / MIC Officer Received by: Date & Time:
Team Leader
Original - Etiqa Philippines MedClaim's copy Blue - Hospital's copy Green - Etiqa Philippines MOD's copy
You might also like
- De Leon, Charmagne BDocument1 pageDe Leon, Charmagne BHasmin CortezNo ratings yet
- Diagnostic 20231124083541Document1 pageDiagnostic 20231124083541Lucia LizardaNo ratings yet
- Outpatient Diagnostic & Procedure Form Letter of Guarantee (Log)Document1 pageOutpatient Diagnostic & Procedure Form Letter of Guarantee (Log)selinaberina18No ratings yet
- Fermin, Ma. Corazon T. (MMC) 2Document1 pageFermin, Ma. Corazon T. (MMC) 2Moggie FerminNo ratings yet
- Arcega Florence Diane R. 3 15 24. RevisedDocument1 pageArcega Florence Diane R. 3 15 24. RevisedMark BaniagaNo ratings yet
- Arcega Arnel S. 3 15 24. RevisedDocument1 pageArcega Arnel S. 3 15 24. RevisedMark BaniagaNo ratings yet
- Arcega Maria Lucia R. 3 15 24 RevisedDocument1 pageArcega Maria Lucia R. 3 15 24 RevisedMark BaniagaNo ratings yet
- Outpatient Consultation Form Letter of Guarantee (Log) : Number: 02-8895-3308 PLDT Toll Free: 1-800-10-895-3308Document1 pageOutpatient Consultation Form Letter of Guarantee (Log) : Number: 02-8895-3308 PLDT Toll Free: 1-800-10-895-3308hsam.arianegracecdenagaNo ratings yet
- APE LOG Miguel de ChavezDocument1 pageAPE LOG Miguel de ChavezNica de ChavezNo ratings yet
- Referral Control Sheet For Out Patient Consultation (RCS 1)Document3 pagesReferral Control Sheet For Out Patient Consultation (RCS 1)larie4mae4montefalcoNo ratings yet
- Screenshot 2022-11-17 at 1.03.38 PMDocument1 pageScreenshot 2022-11-17 at 1.03.38 PMMaritess Ogalesco0% (1)
- Generate LOADocument1 pageGenerate LOAangel.domingo0309No ratings yet
- Authorization LetterDocument7 pagesAuthorization Letterkanduri.ajaykanthreddyNo ratings yet
- Referral Control Sheet For Out Patient Consultation (RCS 1)Document3 pagesReferral Control Sheet For Out Patient Consultation (RCS 1)larie4mae4montefalcoNo ratings yet
- Paramount Health Services & Insurance Tpa Private Limited: Deficiency Letter Without PrejudiceDocument2 pagesParamount Health Services & Insurance Tpa Private Limited: Deficiency Letter Without PrejudiceHemantNo ratings yet
- MD Imran Final ApprovalDocument3 pagesMD Imran Final ApprovalASHISH BANSALNo ratings yet
- Pasco, Roxanne Gean P - 6Document2 pagesPasco, Roxanne Gean P - 6Rens KSNo ratings yet
- Op - Zapanta, Annabelle PDFDocument2 pagesOp - Zapanta, Annabelle PDFWendylNo ratings yet
- Intellicare Reimbursement Form UPDATEDDocument2 pagesIntellicare Reimbursement Form UPDATEDPhilip Sardan100% (1)
- Reimbursement Form - GamayonDocument2 pagesReimbursement Form - Gamayonreese93No ratings yet
- 2024-2025 Hmo Advisory & EnrollmentDocument14 pages2024-2025 Hmo Advisory & EnrollmentJona ReyesNo ratings yet
- Claim Form GeneralDocument1 pageClaim Form GeneralTanya Rose-AppleNo ratings yet
- DolatreDocument1 pageDolatrejohnlester delacruzNo ratings yet
- Mace Consult Form Maceii2113030Document1 pageMace Consult Form Maceii2113030Angel CapinpinNo ratings yet
- Ihp FHP PF - 2023Document8 pagesIhp FHP PF - 2023Mantra ServicesNo ratings yet
- Mace Consult Form Maceii3078507Document1 pageMace Consult Form Maceii3078507johnlester delacruzNo ratings yet
- Authorization LetterDocument7 pagesAuthorization LetterRishi UpadhyayNo ratings yet
- LOA Diagnostic WorkupDocument1 pageLOA Diagnostic WorkupVincent VillaruzNo ratings yet
- Referral Letter: Employees State Insurance CorporationDocument1 pageReferral Letter: Employees State Insurance CorporationafakraipurNo ratings yet
- Claim FormDocument1 pageClaim FormJoshua DraculanNo ratings yet
- Refferalform1Document1 pageRefferalform1ikshikachristian2000No ratings yet
- Change Request Form: This Is A Watermark For Trial Version, Register To Get Full One!Document1 pageChange Request Form: This Is A Watermark For Trial Version, Register To Get Full One!Kumari MadhumitaNo ratings yet
- Claim FormDocument1 pageClaim FormSupriya KandukuriNo ratings yet
- Approval 1681777245981Document1 pageApproval 1681777245981Yasushiko KobayashiNo ratings yet
- Generate LOADocument1 pageGenerate LOAdead9122No ratings yet
- 192.168.1.206 Eclaims Cashless Viewletter - Aspx intPreIDDocument2 pages192.168.1.206 Eclaims Cashless Viewletter - Aspx intPreIDshivamNo ratings yet
- Rev 3 RAWAT JALAN INDIVIDUAL InggrisDocument2 pagesRev 3 RAWAT JALAN INDIVIDUAL InggrisمولديياNo ratings yet
- NOW HEALTH Claim - Form - Uae - RsaDocument2 pagesNOW HEALTH Claim - Form - Uae - RsaWilliam IsaacNo ratings yet
- AckoPolicy PHQWRBKzxvw6TQrqrRPzzgDocument4 pagesAckoPolicy PHQWRBKzxvw6TQrqrRPzzgajptl92No ratings yet
- Post Hospitalizion Clain FormDocument3 pagesPost Hospitalizion Clain FormPadmini SubramaniamNo ratings yet
- Apollo Change Request Form PDFDocument1 pageApollo Change Request Form PDFJituNo ratings yet
- Reimbursement Request FormDocument1 pageReimbursement Request FormAlvin Lorenz CaprichoNo ratings yet
- Axa IDocument2 pagesAxa IalredhamuhamadNo ratings yet
- Approval 1679880369230Document1 pageApproval 1679880369230Joel BugtongNo ratings yet
- Aon - Aia Ghs Claim Form - Oct 2014Document3 pagesAon - Aia Ghs Claim Form - Oct 2014John SmithNo ratings yet
- Aon Care GHS Claim FormDocument5 pagesAon Care GHS Claim FormGelson Herrera0% (5)
- Backupnew PreAuthLetters ALIssuance 2022 SBIGI APR 28-04-2022-16-59-01 5456830Document2 pagesBackupnew PreAuthLetters ALIssuance 2022 SBIGI APR 28-04-2022-16-59-01 5456830MahanNo ratings yet
- Reimbursement Request Form PDFDocument2 pagesReimbursement Request Form PDFLarrae LucilaNo ratings yet
- NEW Takaful Hospital and Surgical Claim Form - Sun Life Malaysia Takaful PDFDocument4 pagesNEW Takaful Hospital and Surgical Claim Form - Sun Life Malaysia Takaful PDFamadkacakNo ratings yet
- Log FormsDocument2 pagesLog FormsHihiNo ratings yet
- Change Request Form PDFDocument1 pageChange Request Form PDFdarshankumar999No ratings yet
- Claim Form NewDocument4 pagesClaim Form Newparvazahmed03191No ratings yet
- PhilGASEA Medicard 20161012Document19 pagesPhilGASEA Medicard 20161012Anileto Boleche100% (3)
- CAPREALTD01 - Pre-authorisationReplyLetterA - ASHAHI1 - P 20140613 03-33-20Document3 pagesCAPREALTD01 - Pre-authorisationReplyLetterA - ASHAHI1 - P 20140613 03-33-20RohitNo ratings yet
- Reimbursement Request FormDocument1 pageReimbursement Request FormRodvin BuadaNo ratings yet
- Reimbursement Request Form: Jayson Delos Reyes 43-00-00134-00865-0 1 White and CaseDocument2 pagesReimbursement Request Form: Jayson Delos Reyes 43-00-00134-00865-0 1 White and CaseJayson Delos ReyesNo ratings yet
- Referral Control Sheet For Out-Patient Consultation (RCS 1) : Valid UntilDocument2 pagesReferral Control Sheet For Out-Patient Consultation (RCS 1) : Valid UntilClaire Melody CalumpangNo ratings yet
- Authorization Letter RaviDocument1 pageAuthorization Letter RaviTanmoy Pal ChowdhuryNo ratings yet
- A Guide for Medical Case Managers: Stop Loss Insurance for Medical ProfessionalsFrom EverandA Guide for Medical Case Managers: Stop Loss Insurance for Medical ProfessionalsNo ratings yet
- NFDN 1002 - PCDocument3 pagesNFDN 1002 - PCapi-276773856No ratings yet
- Cot Lesson PlanDocument5 pagesCot Lesson PlanDada Dela VegaNo ratings yet
- Screw Retained Vs Cement Retained Implant-Supported Fixed Dental ProsthesisDocument11 pagesScrew Retained Vs Cement Retained Implant-Supported Fixed Dental ProsthesisMario Troncoso AndersennNo ratings yet
- Rishum 1 262421216 2Document1 pageRishum 1 262421216 2HellcroZNo ratings yet
- BSRTDocument1 pageBSRTPaul John HipolitoNo ratings yet
- Outpatient Clinic (Hospital Department) - WikipediaDocument6 pagesOutpatient Clinic (Hospital Department) - WikipediaG MNo ratings yet
- 2021 Dignity Health AZ Preferred MPD - FINAL v1Document94 pages2021 Dignity Health AZ Preferred MPD - FINAL v1Juan Gutierrez AZ-GilbertNo ratings yet
- Ati - RN Comprehensive Predictor 2023 RemediationDocument21 pagesAti - RN Comprehensive Predictor 2023 Remediationseansdrew2No ratings yet
- Generic The Unbranding of Modern Medicine (Jeremy A. Greene) (Z-Library) PDFDocument391 pagesGeneric The Unbranding of Modern Medicine (Jeremy A. Greene) (Z-Library) PDFdebraNo ratings yet
- ResearchDocument47 pagesResearchgkzunigaNo ratings yet
- Drug MenaceDocument12 pagesDrug MenaceMyles Ninon LazoNo ratings yet
- Family Life Cycle Stage Major Task 2 Order Changes in Family Status Required To Proceed DevelopmentallyDocument6 pagesFamily Life Cycle Stage Major Task 2 Order Changes in Family Status Required To Proceed DevelopmentallyAris Jasper NacionNo ratings yet
- Usaid Jobs South SudanDocument20 pagesUsaid Jobs South SudanRobert AzihembaNo ratings yet
- Master of Hospital AdministrationDocument3 pagesMaster of Hospital AdministrationDEEPESH RAINo ratings yet
- Melanoma Pathology Reporting and StagingDocument10 pagesMelanoma Pathology Reporting and StagingLizbeth QuinteroNo ratings yet
- AnnexA KonsultaProvidersMinimumRequirementsDocument3 pagesAnnexA KonsultaProvidersMinimumRequirementsAlayzah Guiamalon Masukat0% (1)
- NCMB317 Act1 MidtermDocument2 pagesNCMB317 Act1 MidtermMAUREIN ANNE TEPACENo ratings yet
- Essay Health CareDocument7 pagesEssay Health Careimmkhuwhd100% (2)
- 1 +Bharath+Biotech+PPTDocument20 pages1 +Bharath+Biotech+PPTTapan SharmaNo ratings yet
- Case Presentation Format 3Document1 pageCase Presentation Format 3Priya Sharma Sabarad100% (3)
- Telenursing PDFDocument10 pagesTelenursing PDFSujatha J JayabalNo ratings yet
- Assessment Nursing Diagnosis Outcome Identification Planning Intervention Rationale Evaluation Subjective Data: Short Term: IndependentDocument2 pagesAssessment Nursing Diagnosis Outcome Identification Planning Intervention Rationale Evaluation Subjective Data: Short Term: IndependentDimple Castañeto Callo100% (1)
- Document 12Document1 pageDocument 12selbal0% (1)
- History of Clinical PsychologyDocument3 pagesHistory of Clinical PsychologyaeetjcduvNo ratings yet
- The Impact of The COVID 19 Pandemic On Low Income Households in The Philippines Impending Human Capital CrisisDocument20 pagesThe Impact of The COVID 19 Pandemic On Low Income Households in The Philippines Impending Human Capital CrisisKim DumaganNo ratings yet
- Self Assesment Alat KesehetanDocument20 pagesSelf Assesment Alat KesehetanHariyadiAlldhiAchildNo ratings yet
- Guidebook For Preacc Entrylevelstandards SHCO PDFDocument162 pagesGuidebook For Preacc Entrylevelstandards SHCO PDFArun Kumar100% (3)
- Academic Record Cgfns PDFDocument2 pagesAcademic Record Cgfns PDFSdgfh Wanda100% (1)
- SBS Academic ProceduresDocument91 pagesSBS Academic ProceduresManuel Guilherme VooghtNo ratings yet
- A Comprehensive Strategic Analysis of The Environmental Scanning of Iranian Public Hospitals: A Prospective ApproachDocument16 pagesA Comprehensive Strategic Analysis of The Environmental Scanning of Iranian Public Hospitals: A Prospective ApproachWafa QenoNo ratings yet