Professional Documents
Culture Documents
Module 2 Urine
Uploaded by
Giulia Nădășan-CozmaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Module 2 Urine
Uploaded by
Giulia Nădășan-CozmaCopyright:
Available Formats
MODULE 2: URINALYSIS
Introduction Urinalysis is a very useful diagnostic tool available to the practitioner and
performed in every veterinary practice. Urinalysis is performed as part of the animal routine
check, to diagnose and/or monitor urinary tract infection/inflammation, renal dysfunction
and to investigate selected metabolic disorders. Routine urinalysis includes macroscopic
examination, specific gravity (USG), dipstick analysis, wet sediment examination/urine
cytology, often culture testing and other specialised tests. In this module, we will focus our
attention on the microscopic examination of urine sediment and on the diagnosis of
inflammatory, infectious and neoplastic processes affecting the uro-genital system.
HOW TO COLLECT AND PREPARE URINE SAMPLES
1. Sample collection and handling
There are three methods of sample collection: free catch, catheterization and bladder
cystocentesis. Each of these techniques has its pros and cons and will be discussed below.
• Free catch sampling: this is the easiest way to collect urine. In dogs, the sample is
generally collected mid-stream, meaning partway through urination. In cats, it is
often collected with the use of a syringe or a pipette from the litter tray with a special
non-absorbent litter. Free catch samples are completely non-invasive and can be
relatively easily collected at home by the owners. The main disadvantage is that they
can get easily contaminated and are therefore not recommended for culture testing.
Moreover, in case inflammatory cells are present, it is not possible to localize where
the inflammatory process origins from, since this can be from any tract of the uro-
genital tract.
• Catheterization: this procedure is rarely indicated and may be used in large breed
dogs where cystocentesis can be technically difficult, when the bladder is nearly
empty or in patients that have been previously catheterized for medical reasons.
Urine samples obtained by catheterization may also be contaminated and may be not
ideal for culture testing. Moreover, the procedure may facilitate the introduction of
infections, therefore care must be taken to perform all steps in a clean environment.
• Cystocentesis: this is a very useful technique to collect urine samples, which are also
suitable for culture testing. The procedure is performed under ultrasound guidance.
Ultrasound gel should be removed at the moment of sample collection as it results in
contamination of the cytology sample. This technique also facilitates the localization
of any inflammatory process as it by-passes the distal part of the uro-genital system.
It may result in microscopic haematuria, which can be difficult to differentiate from
genuine haemorrhage. This does not happen in free catch samples, where the
© Vet CPD Tutored Online CPD Courses
presence of red blood cells indicates haematuria. Contraindication to cystocentesis
include coagulopathies and suspected transitional cell carcinoma, which rarely can be
seeded along the needle tract.
FORUM DISCUSSION What is the collection technique you use more often for
urinalysis? Do you perform urianalysis in-house or do you send it to an external lab?
If you send the sample to an external laboratory, do you always indicate the
collection technique on the submission form?
TIPS Ideal time of collection of urine samples may vary depending on the reason
urinalysis is performed. First morning urine samples are preferred to evaluate real
renal concentration ability, if renal disease is suspected. Randomly timed urine
represent urine that has accumulated within the bladder for minutes to hours and
are ideal to evaluate possible inflammation/infection. Post-prandial urine may be
useful to assess the effects of diet intended to modulate urine pH and to detect post
prandial hyperglycaemia.
Ideally, at least 5 ml of urine should be collected and should be enough for most routine
diagnostic tests, which will be described later into details. Urine samples should be collected
into sterile plain tubes and testing should be carried out as soon as possible, ideally within 30-
60 minutes. Storage for longer time at room temperature may result in a) pH increase b)
degeneration of cells and casts c) dissolution/precipitation of crystals d) decrease of glucose,
ketones, bilirubin e) bacteria proliferation. If analysis is delayed because the sample has to be
sent to an external laboratory, it is recommended to refrigerate (not freeze!) it and protect it
from light. Urine should then be warmed to room temperature and mixed before analysis.
NOTE There is disagreement in the literature regarding the use of borate tubes for culture
testing as a recent study has showed that urine samples collected by cystocentesis and
stored in boric acid were less likely to give a positive culture result compared with those
tested fresh (gold standard) or stored in a plain tube. If boric acid is used, it is important
that the tube is not underfilled as an excess of boric acid may interfere with bacteria.
2. Slide preparation and staining
Wet sediment preparation. A standard amount of well mixed fresh urine (5ml) should be
transferred to a conical-tip tube. The sample should be centrifuged at a slow speed (e.g. 1000-
2000 rpm for 5 minutes) in order not to damage cells and other fragile structures (e.g. casts,
crystals). The supernatant can then be discarded by pipetting or by tipping it out (this
procedure may be riskier especially if no sediment is noted at naked eye). The sediment and
© Vet CPD Tutored Online CPD Courses
the small amounts of fluid left at the bottom of the tube (ideally 0.5ml) should be
resuspended and a drop of it is added to a clean smear and is followed by adding a coverslip
on top. I personally suggest examining unstained urine, however supravital stains (e.g. Sedi-
Stain) are available. These may help in the differentiation of cell types; however, they may be
a font of contamination (e.g. bacteria, stain precipitate) and will cause dilution of the sample
making the estimation of cells number less accurate.
Urine cytology. The sample can be a cytospin preparation if a cytocentrifuge is available.
Alternatively, a small drop of urine sediment can be placed on a plain slide. Slide is then tilted
to ensure that cells spread on a monolayer, air dried (it may take long time!) and then stained.
This procedure is required when neoplasia is suspected and there is an increased number of
epithelial cells with abnormal morphology on the wet preparation but also when there is
equivocal evidence of bacteria on sediment examination. The only downside of this procedure
is that it is not possible to quantify the number of cells and structures per high power field, as
the reference values present in the literature are referred to wet sediment examination only.
URINALYSIS
The laboratory assessment of urine samples includes the following steps. Everything that is
not microscopy related will be discussed briefly as the module/course is focused on the
cytology of fluids. For more information regarding these topics, I recommend reading
dedicated urinalysis textbooks, in particular the Atlas of Canine and Feline Urinalysis by
Theresa E. Rizzi published in 2017 by Wiley/Blackwell.
a) Macroscopic examination: normal canine/feline urine should be pale to deep yellow
(depending on the concentration) and clear or only mildly turbid. Abnormal urine
colour should be documented and is referred as pigmenturia. As an example, the
presence of red urine may reflect the presence of haematuria, haemoglobinuria
and/or myoglobinuria. The presence of deeply yellow to orange or green urine may
indicate the presence of bilirubinuria. Increased cells or other non-cellular elements
generally result in urine being turbid.
b) Specific gravity: this is an indicator of urine weight compared with an equal volume of
distilled water. This should always be performed with a refractometer as the urine
dipstick is not accurate for this. Healthy dogs have USG ranging between 1.015 and
1.045, whereas cats have values in the range of 1.035-1.060. These values may vary
during the day and pre-prandial morning samples are preferred to estimate the real
urine concentration ability. Certain substances if present in large amounts (e.g.
glucose, protein) may have an impact on USG results. Therefore, USG values should
TIPS If the urine is very turbid, this can be centrifuged, and USG tested on the
supernatant. Very turbid or pigmented urine may also interfere with the reading
of the urine dipsticks.
© Vet CPD Tutored Online CPD Courses
be interpreted together with the clinical context (PU/PD, dehydration) and other
biochemistry data (e.g. urea, creatinine, SDMA). Other conditions affecting renal
concentration ability should also be recorded (e.g. diabetes insipidus, pyometra,
hypercalcaemia). For example, isosthenuric urine (1.008-1.012) together with
azotaemia and no other underlying conditions, are supportive of renal dysfunction
and indicate kidneys are unable to concentrate urine.
c) Chemical analysis: this is commonly performed with reagent strips (dipsticks) which
measure the following parameters: pH, glucose, ketones, bilirubin, blood, myoglobin,
leukocytes and protein. The principle behind these tests is a colorimetric reaction
(concentration dependent) that is then read either by naked eye or by using an
automated spectrophotometer. Results are provided in a semiquantitative fashion.
Since dipsticks are manufactured for humans, not all the available tests are
appropriate for use in veterinary species (in particular leukocytes). pH measurement
is reliable only if performed on a fresh sample. Glucosuria should be interpreted in
conjunction with the serum glucose levels and may be due to stress, diabetes mellitus
or tubular dysfunction. Glucosuria may also predispose to urinary tract infections,
therefore culture testing is always advised in these cases. Protein dipstick results
should always be interpreted in the context of urine concentration and sediment
results. For example, a urine sample with SG of 1.010 and urine protein 2+ on dipstick,
contains twice as much protein as urine with a USG of 1.020 and the same dipstick
protein result. In the presence of inflammation or infection, the elevation in protein
will likely be due to this and not to a genuine renal pathology. Since, false positive and
false negative protein results may occur (especially in cats), urine protein creatinine
ratio (UPCR) may be a preferred way to quantify proteinuria. However, this will be still
be influenced by the presence of any inflammation / haemorrhage. Positive blood
dipstick results should be interpreted together with the urine sediment results in
order to differentiate haematuria (positive dipstick for blood, red blood cells on the
sediment) from haemoglobinuria (positive dipstick for blood, no red blood cells on the
sediment). Bilirubin may be present in concentrated urine from healthy dogs, but it
should not be identified in cats, unless there is haemolytic anaemia or some degree of
cholestasis.
d) Wet sediment examination: this will be discussed into details in the following section
and is a key point of urinalysis. It is the only test that can confirm (or rule out) the
presence of an inflammatory process affecting the uro-genital tract.
e) Urine cytology: this refers to a urine sample stained with regular Romanowsky-type
stain and is indicated when neoplasia is suspected and there is an increased number
of epithelial cells with abnormal morphology on the wet preparation but also when
© Vet CPD Tutored Online CPD Courses
there is equivocal evidence of bacteria on sediment examination. This will be
discussed into details later in the module.
f) Urine culture: these results should always be interpreted in the context of the clinical
signs, sampling method and wet sediment findings, in order to establish its clinical
significance. As general rule, bacterial growth is more likely to be significant if it is pure
(instead of mixed), it comes from a cystocentesis sample and there is concurrent
inflammation visible on microscopic examination of the sediment. The ideal sample
for culture testing is fresh urine; as discussed earlier, it is still controversial, the benefit
of collecting the urine in boric acid tubes. Positive culture results in the absence of
cytological evidence of bacteria is not uncommon, as microbiology testing is more
sensitive than cytology for the identification of bacteria. Negative culture results in
the presence of bacteria on cytology may occasionally occur. Possible explanations for
this include: 1) bacteria non-viable for culture testing (e.g. effect of antibiotics,
exposure of sample to high temperature, excessive boric acid added) 2) bacteria viable
but not successfully cultured 3) bacteria requiring longer incubation (>24h) 4) the
“bacteria” seen were actually particulate debris in the urine.
NOTE Dogs with hyperadrenocorticism and diabetes mellitus may have positive
urine culture results, despite the absence of clinical signs of UTI and sometimes
even absence of bacteriuria or pyuria on sediment examination. This condition is
referred as silent UTI. In patients with hyperadrenocorticism, this due to the
immunosuppressive state induced by endogenous steroids. Therefore, culture
testing is always recommended in these patients.
g) Other tests that may be needed include urine protein creatinine ratio (UPCR),
microalbuminuria and urine protein electrophoresis for the quantification and
characterisation of proteinuria. It is also possible to perform urine cortisol: creatinine
ratio (UCCR), mainly to rule out canine hyperadrenocorticism, PCR testing for selected
infectious agents e.g. Leptospira, Distemper virus urinary catecholamines and
metadrenalines for the diagnosis of pheochromocytoma, detection of toxic
substances (e.g. ethylene glycol, lead, illicit drugs), and detection of selected amino
acids.
CYTOLOGICAL EXAMINATION OF URINE SEDIMENT
When approaching the examination of unstained urine sediment, it is important to remember
a few crucial steps. These include:
a) Ensure the microscope condenser is lowered. This will increase the contrast and will
make easier identification and recognition of cellular and non-cellular structures.
© Vet CPD Tutored Online CPD Courses
b) Scan the whole area at 10x to identify cellular areas, crystals and casts. Move then at
higher magnification (40x) to identify cell types and possible infectious agents. In
selected cases, it may be needed to go at 100x.
c) When examining the wet sediment, it is a good practice to count the number of each
cells and structures in 10 fields and take the average (cells/structures per high power
field).
d) For evaluation of possibly inflammatory/infectious conditions, crystalluria, cast
formation, examination of wet sediment is sufficient in most cases. When neoplasia is
suspected and evaluation of the epithelial cell component is required, the urine
sample has to be regularly stained.
• “Normal” cytology findings Normal urine is acellular or contains rare epithelial cells
from different tracts of the urinary system (transitional cells/squamous cells). These
may be more numerous in samples collected by catheterism as it is a more traumatic
collection technique. Few red blood cells are often seen in samples obtained from
catheterism or cystocentesis as result of iatrogenic blood contamination. Very rare
leukocytes and crystals may also be noted.
•
• Haematuria vs blood contamination The presence of red blood cells is considered
significant when there are >5 rbcs in 5 hpf 40x. It may be iatrogenic and therefore
related to blood contamination during catheterism or cystocentesis. Iatrogenic
haemorrhage should not be a differential for free catch samples, however, in female
entire dogs, red blood cells found in urine may also origin from the genital tract. The
presence of red blood cells in urine may also indicate genuine haemorrhage and is
often associated to some degree of anaemia and/or thrombocytopenia. In unstained
wet preparations, red blood cells appear as clear round disks, smaller than WBCs and
often crenated. When stained, they maintain the typical round shape and are more
reddish in colour.
NOTE As described earlier, presence/absence of red blood cells on urine sediment
helps in the interpretation of positive blood dipstick results and allows
differentiation between haemoglobinuria and haematuria. However, in the
presence of low USG, red blood cells lysis may occur making more complicated the
differentiation between these two conditions. This concept does not apply to urine
samples that are immediately analysed after collection.
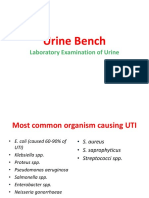
• Inflammation/infection this is a common finding and is usually accompanied by an
increased number of neutrophils (>5 WBC per hpf 40x – wet sediment), which may or
may not be associated with bacteria (rods and/or cocci). When there is evidence that
bacteria are involved in the inflammatory process, the term urinary tract infection
(UTI) is used. This can be the primary cause for the clinical signs observed or it may be
© Vet CPD Tutored Online CPD Courses
secondary to underlying conditions (e.g. urolithiasis, neoplasms). Infection is
confirmed when bacteria are observed within the cytoplasm of neutrophils (if the
urine sample is very fresh). When bacteria are free in the background, they may reflect
contamination or infection. Contamination is more likely if the bacteria population is
mixed and is the sample has been obtained by free catch or catheterism. Infection is
more likely if the sample has been obtained by cystocentesis and one type only of
bacteria is observed.
NOTE The absence of bacteria on cytology does not rule out infection, as
sensitivity of cytology for the detection of bacteria is significantly lower than
culture testing. This can increase if urine cytology is performed together with wet
sediment examination. At least 10000 bacilli/mL or 100000 cocci/mL are required
for detection on light microscopy.
Other infectious agents that can be rarely seen include fungal hyphae/yeasts (e.g.
Candida, Aspergillus) or parasites (e.g. Pearsonema/Capillaria). Other inflammatory
cell types, in particular macrophages, may sometimes be noted. Neutrophils and
macrophages are relatively easy to be recognised on stained urine samples because
of their typical morphology (U-shaped nuclei in neutrophils). Unfortunately, this
cannot be appreciated in unstained urine and their identification relies on size (slightly
larger than red blood cells) and appearance (granular texture).
Knowing the sample collection type may also help to localise the inflammation. If a
cystocentesis sample shows inflammation, this must be located somewhere between
the kidneys and the bladder.
Epithelial cells (transitional and/or squamous) are often present and may show some
degree of atypia, which can make difficult, often impossible, differentiating dysplasia
from neoplasia. Definitive diagnosis may rely on repeating sample analysis when
inflammation has solved or by performing further tests (e.g. histopathology, BRAF
mutation test). The clinical picture is also critical in the diagnostic process (any distinct
bladder mass, in particular at the level of the trigone?). More details about epithelial
cell types and diagnostic dilemmas when both epithelial and inflammatory cells are
present, are discussed later in the module.
© Vet CPD Tutored Online CPD Courses
Fig.1 Urinary tract infection in a dog. Urine sediment stained (A) and unstained (B).
Note the increased number of inflammatory cells, mostly neutrophils, few epithelial
cells, red blood cells and bacteria.
• Crystals. Many of these (e.g. struvite) are incidentally found in urine from healthy
animals and not necessarily result in the formation of macroscopic uroliths/stones.
Therefore, the clinical significance of their presence has to be interpreted in the
context of the full clinical picture. Crystal evaluation should be performed on fresh
urine because crystals can form and/or dissolve on sample storage and with
temperature change. Their evaluation is usually semiquantitative (few, moderate
numbers, high numbers) and is generally performed at low power (4x, 10x). The most
common forms of crystals are discussed below.
o Struvite: these are also known as magnesium ammonium phosphate crystals
and have a typical coffin-shaped appearance. They are common in both dogs
and cats and may be an incidental finding. They are more commonly seen in
© Vet CPD Tutored Online CPD Courses
concentrated and alkaline urine as these factors encourage their precipitation.
In dogs, they are often associated with UTI as urease-producing bacteria (e.g.
Staphylococcus, Proteus) leads to increase pH and encourage their formation.
In cats, they are usually found in sterile samples.
o Calcium oxalate dihydrate: these are also common in both dogs and cats and
can be an incidental finding. They are variably sized square crystals with a
classic Maltese cross formation in the middle. They are generally associated
with acidic urine. Their presence may also be associated with hypercalcaemia.
A variant (monohydrate) characterised by an oblong shape can be seen in
patients with ethylene glycol toxicity or hypercalcaemia.
o Ammonium biurates: these crystals, when present, have always a clinical
significance. They are darkish brown/yellow spherical structures often with
typical pointed protuberances. They can be seen in Dalmatians and Bulldogs,
which have an inborn defect of purine metabolism, leading to excretion of
insoluble uric acid. In other breeds, they usually reflect porto-systemic shunt
(PSS) or hepatic dysfunction. Therefore, if found, bile acid stimulation test and
imaging studies should be considered.
o Bilirubin: these can be seen in very low numbers in concentrated urine samples
from healthy dogs but not in cats. In high numbers, they are associated with
hepatobiliary diseases and/or intravascular haemolysis.
o Others: other crystals less commonly seen in dogs and cats include cystine,
tyrosine, cholesterol, calcium phosphate, uric acid, amorphous crystals and
drug crystals (sulphonamides crystals, xanthine crystals).
Fig.2 Struvite crystals (left) and calcium oxalate dihydrate crystals (right) from
unstained canine urine sediment samples.
© Vet CPD Tutored Online CPD Courses
Fig.3 Ammonium biurates crystals (left) and bilirubin crystals (right) from unstained
canine urine sediment samples.
Fig.4 Sulpha crystals – drug related (left) and cystine crystals (right) from canine urine
sediment samples
• Casts are usually indicative of renal tubular pathology and are the result of the
combination between Tamm-Horsfall mucoprotein secreted by renal tubular cells
incorporated with cell debris, plasma proteins, lipid, etc. They present as large
cylindrical bodies with blunt, tapered or irregular ends but parallel sides. They are very
fragile especially in alkaline urines; therefore, they are easier to appreciate in fresh
samples. Their numbers do not correlate with the severity of the disease or if this is
reversible/irreversible. Casts are classified into hyaline casts, granular casts, cellular
casts, fatty casts and waxy casts, depending on the area of the tubule they formed,
how long they have been in the tubule for, and which cells/structures they contain.
Their microscopic appearance varies a little bit; however, they may look very similar.
• Hyaline casts: smooth, transparent bodies, with no central structures. Rare hyaline
casts in concentrated urine from healthy dogs and cats can be a normal finding.
Increased numbers are seen with glomerular proteinuria or after strenuous exercise.
• Granular casts: these may contain fine or coarse granular and may derived also from
degeneration of cellular casts. Increased numbers indicate tubular cell degeneration,
© Vet CPD Tutored Online CPD Courses
necrosis or inflammation but very rare granular casts may be seen in urines of healthy
animals.
• Cellular casts: these forms when rbcs, wbc or epithelial cells are incorporated in the
Tamm-Horsfall. They are always pathological and indicate tubular damage. Rbcs casts
may suggest glomerular or tubular haemorrhage. Wbcs casts indicate renal tubule
inflammation. Epithelial casts occur when there is active tubular degeneration or
necrosis.
• Fatty casts: these are the results of incorporation of lipid material and are due to
similar causes.
• Waxy casts: they are the result of deterioration of granular or epithelial cell casts. They
are often seen in chronic renal disease.
Fig.4 Casts formation within renal tubule (left) and types of casts (right). From
https://eclinpath.com/
Fig.5 Large numbers of granular casts in the urine sediment of a cat with acute kidney
disease caused by lily toxicosis.
• Other elements these may include exogenous material (contaminant), particularly
common in free catch samples, sperm, vegetable material, lipid droplets (frequent in
v and lubricants, the latter appearing as amorphous deeply pink/eosinophilic material.
© Vet CPD Tutored Online CPD Courses
Fig.6 Frequent sperm in an unstained urine sample from a male dog
• Epithelial cells Before discussing the topic neoplasia, it is important to understand
which cell types, different from leukocytes, can be find in urine samples, how to
recognise them and how to differentiate them from their neoplastic counterpart.
There are three main types of epithelial cells than can be seen in urine samples. Their
evaluation is easier in stained urine samples. These include:
a) Squamous epithelial cells: these cells often origin from the distal tract of the
urinary tract (or from the surrounding skin) and are not clinically significant.
They are characterised by having abundant cytoplasm with angular borders.
Nuclei are often small, round and centrally located.
b) Prostatic epithelial cells: these cells are mainly observed in prostatic wash
samples. They are small cuboidal cells with strong tendency to form cluster
and often showing a honeycomb arrangement.
c) Transitional epithelial cells: these cells cover most of the urinary tract and
prostate in male dogs. Their morphology is more variable than the other cell
types but is usually characterised by a round appearance, variable size
depending on the site of origin (smaller when from the proximal tract of the
urinary system, larger from the distal parts). Nucleus is round and central. N:C
ratio is higher than in squamous cells.
d) Renal epithelial cells: similar to transitional cells with a more caudate
appearance. They origin from the renal pelvis and are not seen very often.
© Vet CPD Tutored Online CPD Courses
Fig.7 Epithelial cells commonly seen in urine/prostatic wash samples.
Rare epithelial cells may be seen in urine from healthy and numbers/types mainly
depend on the collection technique that has been used. All these cell types may
undergo dysplastic changes, in particular in association with inflammation, urolithiasis
or exposure to toxins, and can mimic neoplasia. These dysplastic changes include
anisocytosis, anisokaryosis, increased nucleus:cytoplasm ratio, coarse granular
chromatin, prominent nucleoli and sometimes also binucleation and presence of
mitotic figures. Squamous metaplasia may also occur, and transitional cells may
appear similar to normal squamous cells. Because of this, care must be taken before
diagnosing neoplasia in the presence of inflammation, in particular when the clinical
picture is not supportive of it. Further investigations are always warranted in these
cases.
The most common neoplasm affecting the urinary tract in both dogs and cats is
transitional cell carcinoma. Other neoplasms include papilloma, prostatic carcinoma,
squamous cell carcinomas, renal/bladder lymphoma, primary renal carcinoma and
rarely also sarcomas.
Transitional cell carcinoma (TCC) also referred to as urothelial carcinoma (UC), is the
most common form of malignant neoplasm of the urinary tract in dogs, accounting for
50% to 75% of reported cases of canine urinary bladder cancer. The aetiology is not
completely understood but is likely to be multifactorial and prevalence appears to be
higher in certain breeds, in particular Scottish Terrier dogs, which have a 21-fold
increased risk. Dogs usually present with lower urinary tract signs (e.g. haematuria,
stranguria, pollakiuria, dysuria), and many have concurrent urinary tract infections
(UTIs) that may initially delay the diagnosis. Resolving the infection may temporarily
alleviate the clinical signs, and patients often present with a several-month history of
lower urinary tract signs. Grossly, TCC usually presents as a solitary papillary,
polypoid, or sessile mass. The most common location in dogs is the trigone of the
urinary bladder, but this neoplasm can also arise from the renal pelvis, ureters,
urethra, or prostate. In a necropsy study of 137 dogs with TCC, nodal and distant
© Vet CPD Tutored Online CPD Courses
metastases were found in 42% and 58% of dogs, respectively. The lung was the most
common site of distant metastases, followed by other abdominal organs, bones (e.g.
lumbar spine) and skin. In cats, it is less common, and it may arise in different tract of
the bladder and urinary tract.
From a diagnostic point of view, urine sediment examination reveals neoplastic cells
in a limited percentage of cases and is unlikely to provide a definitive diagnosis. Direct
fine-needle aspiration of the mass is the technique providing the highest cellular
samples for analysis, although the potential for seeding neoplastic cells is a
consideration. Therefore, traumatic catheterization (also called suction biopsy) is
often preferred. Cytologically, TCC are characterised by clusters of cuboidal to
polygonal epithelial cells of transitional origin as described above. Features of atypia
vary but may be marked. Interestingly, it is quite common to observed characteristic
intracytoplasmic pinkish round structures refereed as Melamed Wolinska bodies,
which can sometimes displace the nucleus to the periphery of the cell.
© Vet CPD Tutored Online CPD Courses
Fig.8 (A+B) Aspirate from transitional cell carcinoma in a dog. Note the presence of a
main population of transitional epithelial cells with variable degree of atypia, including
anisokaryosis (black arrow). Note also the Melamed Wolinska bodies (red arrow) and
mitotic figure (green arrow).
When cells have a typical transitional morphology, exhibit marked criteria of
malignancy and there is no evidence of inflammation or infection, a diagnosis of TCC
can be easily achieved by cytology. This may not be possible when neoplastic cells are
well differentiated or in the presence of concurrent inflammation since morphology
of well differentiated neoplastic cells and hyperplastic/dysplastic transitional cells may
overlap. In those cases, further diagnostic investigations should be considered and
may include histopathology and/or BRAF mutation testing.
Conventionally, biopsy and histopathologic evaluation are required to confirm a
diagnosis of canine TCC and are particularly important when a definitive cytological
diagnosis is not possible. More recently, new non-invasive techniques have been
described and have shown very promising results. These include molecular testing for
BRAF mutation, which is a PCR based assay that searches for a single mutation in a
gene called BRAF within transitional epithelial cells. This mutation has been identified
in up to 85% of TCC cases and to date this has never been recorded in urine specimens
neither from healthy dogs nor in patients with inflammatory or dysplastic processes
affecting the genitourinary tract. This means that finding the BRAF mutation is
© Vet CPD Tutored Online CPD Courses
confirmatory for TCC but the lack of it does not entirely rule it out, since false negative
results may occur. One of the main advantages of this test is that it can be performed
on almost any diagnostic sample that contains transitional epithelial cells, including
pre-stained cytology smears with equivocal diagnosis, which means no additional
samples are required. Molecular testing for BRAF mutation may also be considered as
a screening test in free-catch urine samples of healthy dogs with an increased risk of
developing TCC, likely enabling identification of these cases at early and even
preclinical stages of the disease. Once a dog has been diagnosed as positive for BRAF
mutation and shown to have TCC, repeat analysis may also be used over time to
monitor changing levels of the mutational load detected in free-catch urine during
treatment.
Prostate: this is another organ part of the uro-genital system that may undergo
pathological changes including inflammation (e.g. prostatitis, prostatic abscesses),
hyperplastic processes (benign prostatic hyperplasia - BPH), squamous metaplasia,
prostatic/para-prostatic cysts ad neoplasia, the latter including transitional cell
carcinoma but also prostatic adenocarcinoma. Prostatic samples may be obtained
directly through the urethra (prostatic massage or lavage), ejaculation, or ultrasound
guided direct FNA of the gland. Of all the conditions previously listed, it may be worth
to spend a few words on benign prostatic hyperplasia (BPH). This is the most common
prostatic disorder in adult entire male dog (very rare in cats) as it is testosterone
dependent. It usually causes a symmetrical enlargement of the prostate which is often
associated with clinical signs and sometimes also concurrent prostatitis. Presumptive
diagnosis can be achieved by combining signalment, clinical picture and cytological
findings. These are characterised by the presence of large clusters of mature prostatic
epithelial cells with a typical honeycomb appearance. Well differentiated prostatic
epithelial neoplasms may appear similar and definitive diagnosis relies on
histopathology. The most effective treatment for this condition is castration.
© Vet CPD Tutored Online CPD Courses
Fig.9 Ultrasound guided fine needle aspirate from an enlarged prostate of a dog with
benign prostatic hyperplasia (BPH). Note the well differentiated prostatic epithelial
cells with a typical honeycomb appearance.
KEY CONCEPTS
• Knowing the collection technique of urine samples is crucial for a correct
interpretation of urinalysis findings.
• If possible, evaluation of fresh urine is preferred, especially for the
evaluation of certain parameters (e.g. pH) and structures (crystals, casts,
cells).
• Wet sediment analysis is indicated for evaluation of suspect inflammation,
infection, crystalluria and casts.
• When there is suspicion for neoplasia, wet sediment analysis should be
accompanied by regular urine cytology (stained sample).
• Transitional cell carcinoma (TCC) is the most common neoplasia of the
urinary tract affecting both canine and feline species and has characteristic
cytological features.
• When a definitive cytological diagnosis of TCC is not possible, further
diagnostic investigations should be considered. These include
histopathology and evaluation of BRAF mutation.
© Vet CPD Tutored Online CPD Courses
You might also like
- A Simple Guide to Blood in Stools, Related Diseases and Use in Disease DiagnosisFrom EverandA Simple Guide to Blood in Stools, Related Diseases and Use in Disease DiagnosisRating: 3 out of 5 stars3/5 (1)
- Abusive RelationshipsDocument10 pagesAbusive RelationshipsGiulia Nădășan-CozmaNo ratings yet
- Urine Cytology: Christine BadilloDocument21 pagesUrine Cytology: Christine BadilloChristine BadilloNo ratings yet
- Urinalysis and Body Fluid CollectionsDocument48 pagesUrinalysis and Body Fluid CollectionsladydianamacNo ratings yet
- Complete Urinalysis: A. Physical Characteristics of UrineDocument8 pagesComplete Urinalysis: A. Physical Characteristics of UrineKryza Dale Bunado BaticanNo ratings yet
- MICROSCOPIC URINE ANALYSISDocument89 pagesMICROSCOPIC URINE ANALYSISLucia SurduNo ratings yet
- English 3-Q4-L7 ModuleDocument19 pagesEnglish 3-Q4-L7 ModuleZosima Abalos100% (1)
- Urine Collection in CytologyDocument12 pagesUrine Collection in CytologyjunaidiabdhalimNo ratings yet
- Urine Analysis ExplainedDocument22 pagesUrine Analysis Explainedsvrlax60% (5)
- Cytopreparatory Technique: Ama AfrahDocument49 pagesCytopreparatory Technique: Ama Afrahreuben kwotaNo ratings yet
- Lesson 10Document66 pagesLesson 10Angel joyce ValenciaNo ratings yet
- Urinary Tract InfectionsDocument44 pagesUrinary Tract Infectionstummalapalli venkateswara rao100% (2)
- Lab Exercise 11 Urine Specimen CollectionDocument7 pagesLab Exercise 11 Urine Specimen CollectionArianne Jans MunarNo ratings yet
- Stool Exam Methods - Detect Parasites with AccuracyTITLE Diagnosing Parasites in Stool - Laboratory Techniques Explained TITLE Parasite Detection in Stool - Proper Collection and Examination MethodsDocument27 pagesStool Exam Methods - Detect Parasites with AccuracyTITLE Diagnosing Parasites in Stool - Laboratory Techniques Explained TITLE Parasite Detection in Stool - Proper Collection and Examination MethodsAnastasiaNo ratings yet
- Self-Assessment Color Review Moriello's Small Animal Dermatology Fundamental Cases and Concepts 2nd Edition PDFDocument307 pagesSelf-Assessment Color Review Moriello's Small Animal Dermatology Fundamental Cases and Concepts 2nd Edition PDFGiulia Nădășan-CozmaNo ratings yet
- Clinical Microscopy Technical ManualDocument10 pagesClinical Microscopy Technical ManualSharon ChuaNo ratings yet
- Hematuria, (Blood in Urine) A Simple Guide to The Condition, Related Diseases And Use in Diagnosis of DiseasesFrom EverandHematuria, (Blood in Urine) A Simple Guide to The Condition, Related Diseases And Use in Diagnosis of DiseasesRating: 5 out of 5 stars5/5 (2)
- Small Animal DermatologyDocument1,527 pagesSmall Animal DermatologyGiulia Nădășan-Cozma100% (2)
- Urine ExaminationDocument36 pagesUrine ExaminationPrahlad singh100% (3)
- 01 - 2007Document92 pages01 - 2007Edgar A BernalNo ratings yet
- Clinical Nephrology Dialysis and TransplantationDocument1,539 pagesClinical Nephrology Dialysis and Transplantationalrafeek1050100% (1)
- Urine Analysis-Lab Report Biochem 3Document8 pagesUrine Analysis-Lab Report Biochem 3Syazmin Khairuddin83% (12)
- Physiology Lab Report 10 - UrinalysisDocument19 pagesPhysiology Lab Report 10 - Urinalysisbenamos100% (10)
- Hair Loss in CatsDocument6 pagesHair Loss in CatsGiulia Nădășan-CozmaNo ratings yet
- Fire Protection Focus for TunnelsDocument12 pagesFire Protection Focus for Tunnelsfrank100% (1)
- 1856-Cian - The Role of Cytology in Urinalysis of Dogs and CaDocument4 pages1856-Cian - The Role of Cytology in Urinalysis of Dogs and CaYaiza Garcia CasadoNo ratings yet
- Urine CytologyDocument15 pagesUrine CytologyNaruto ShikamaruNo ratings yet
- Urinalysis Dipstick InterpretationDocument14 pagesUrinalysis Dipstick InterpretationGamaliel VentoNo ratings yet
- Answers: Wide Mouthed ContainerDocument4 pagesAnswers: Wide Mouthed ContainerShafici CqadirNo ratings yet
- Macroscopic Urinalysis, Performed Manually Using Bayer MultistixDocument12 pagesMacroscopic Urinalysis, Performed Manually Using Bayer MultistixKevin TranNo ratings yet
- UrianalisisDocument17 pagesUrianalisisPAOLA ANDREA TAPIAS PUINNo ratings yet
- Examination of The Urine Sediment: Specimen CollectionDocument1 pageExamination of The Urine Sediment: Specimen CollectionSufariu MirelaNo ratings yet
- Complete Urinalysis and Urine Test-2Document34 pagesComplete Urinalysis and Urine Test-2azuraNo ratings yet
- Lab Diagnosis of UTIsDocument27 pagesLab Diagnosis of UTIsasalizwa ludlalaNo ratings yet
- UrinalysisDocument15 pagesUrinalysisarchivos primeroNo ratings yet
- Urinalysis - Chemical, Physical and Microscopic Examination of UrineDocument6 pagesUrinalysis - Chemical, Physical and Microscopic Examination of UrineGaurav KatariaNo ratings yet
- 4 - Urine BenchDocument37 pages4 - Urine BenchChiizu iraNo ratings yet
- Fecal, Blood and Urine ExaminationDocument6 pagesFecal, Blood and Urine ExaminationSyed ArslanNo ratings yet
- Stool ExaminationDocument108 pagesStool ExaminationBig ZeroNo ratings yet
- 38 - Semen - Analysis TerjemahanDocument27 pages38 - Semen - Analysis TerjemahanShofia CahyaNo ratings yet
- Routine UrinalysisDocument4 pagesRoutine UrinalysisEricka Zai FLORESNo ratings yet
- Manual urinalysis guideDocument37 pagesManual urinalysis guideAdhya TiaraNo ratings yet
- Gribblesch21 UrinalysisDocument4 pagesGribblesch21 UrinalysisShuhada HamidNo ratings yet
- Urinalysis Is A Diagnostic Physical, Chemical, and Microscopic Examination ofDocument4 pagesUrinalysis Is A Diagnostic Physical, Chemical, and Microscopic Examination ofjadeyjadeNo ratings yet
- Urine Specimen Types and CollectionDocument7 pagesUrine Specimen Types and CollectionRyan KadavilNo ratings yet
- UrinalysisDocument5 pagesUrinalysisKreshnik HAJDARINo ratings yet
- URINALYSIS TESTING GUIDEDocument6 pagesURINALYSIS TESTING GUIDEThanz Pamela Gargueña Guisihan100% (1)
- Pur UrinalDocument76 pagesPur UrinalDarío AsteteNo ratings yet
- Investigations of The Urinary System: Group 4Document53 pagesInvestigations of The Urinary System: Group 4YvonneNo ratings yet
- Introduction To UrinalysisDocument12 pagesIntroduction To UrinalysisfaysalhusseinfaysalhusseinNo ratings yet
- Lesson 21 PDFDocument4 pagesLesson 21 PDFShirmayne TangNo ratings yet
- Detecting Occult Blood and Parasites in StoolDocument2 pagesDetecting Occult Blood and Parasites in StoolKagami TaigaNo ratings yet
- Lr12 - UrinalysisDocument2 pagesLr12 - UrinalysisJhobhel Christopher GalivoNo ratings yet
- PMLS 2 Chapter Summary - YraudaDocument5 pagesPMLS 2 Chapter Summary - YraudaKeizzy YraudaNo ratings yet
- Clinicalpathologyppt 220319134410Document27 pagesClinicalpathologyppt 220319134410PrakashNo ratings yet
- Fecal Analysis (Stool Analysis) Nursing ResponsibilitiesDocument4 pagesFecal Analysis (Stool Analysis) Nursing ResponsibilitiesDonna IlarNo ratings yet
- Blocked CatDocument9 pagesBlocked CatBê LagoNo ratings yet
- Nonblood Body Fluid TestsDocument13 pagesNonblood Body Fluid TestsAnne Gabrielle EspadaNo ratings yet
- The Test Urine CultureDocument13 pagesThe Test Urine CultureAnonymous 5aoV2RWWAwNo ratings yet
- TeachingDocument18 pagesTeachingDeep PatelNo ratings yet
- Competency Appraisal - Diagnostic TestsDocument7 pagesCompetency Appraisal - Diagnostic TestsMj BrionesNo ratings yet
- Exp 10 (MW 130-430)Document10 pagesExp 10 (MW 130-430)Jane RayeNo ratings yet
- Exercise 14: Macroscopic and Chemical Examination of UrineDocument11 pagesExercise 14: Macroscopic and Chemical Examination of UrineAfif PusamaniaNo ratings yet
- URINARY TRACT INFECTION GUIDEDocument43 pagesURINARY TRACT INFECTION GUIDEhendraNo ratings yet
- Swu Phinma, College of Pharmacy 2020: Wr/Urinalysis - Html#Ixzz6Zxlj RQKH /Product-Manual/3008 - 3B - UrinalysisDocument7 pagesSwu Phinma, College of Pharmacy 2020: Wr/Urinalysis - Html#Ixzz6Zxlj RQKH /Product-Manual/3008 - 3B - UrinalysisTrex MarciiiNo ratings yet
- What Is Bacteriuria? When Is It Significant?Document6 pagesWhat Is Bacteriuria? When Is It Significant?SAMMYNo ratings yet
- Uroanalisis AnormalDocument13 pagesUroanalisis AnormalMyke EstradaNo ratings yet
- Are Essential Fatty Acids EffectiveDocument16 pagesAre Essential Fatty Acids EffectiveGiulia Nădășan-CozmaNo ratings yet
- Alternative Forages For GoatsDocument27 pagesAlternative Forages For GoatsGiulia Nădășan-CozmaNo ratings yet
- Demand for E-ZPass and Gas GuzzlersDocument11 pagesDemand for E-ZPass and Gas GuzzlersYonn Me Me KyawNo ratings yet
- Eco 2203-1 (Notes To Date)Document102 pagesEco 2203-1 (Notes To Date)Joseph KhaembaNo ratings yet
- Math 7 - Week 2 SummativeDocument1 pageMath 7 - Week 2 SummativeBrian Mary0% (1)
- Gujarat Technological University Subject: VLSI Technology & Design Code:2161101 Topic - 3 - MOS TransistorDocument122 pagesGujarat Technological University Subject: VLSI Technology & Design Code:2161101 Topic - 3 - MOS Transistorbakoliy218No ratings yet
- Readme P006Document7 pagesReadme P006paras99No ratings yet
- Advanced Image Stylization With Extended Difference-of-GaussiansDocument10 pagesAdvanced Image Stylization With Extended Difference-of-Gaussianse_gorodinskyNo ratings yet
- The Madhya Pradesh Public Trusts Act 1951Document13 pagesThe Madhya Pradesh Public Trusts Act 1951Zenith ChhablaniNo ratings yet
- American Folk Song Lesson PlanDocument1 pageAmerican Folk Song Lesson Planapi-2844060150% (1)
- Jurnal Saraf PDFDocument11 pagesJurnal Saraf PDFkade silabanNo ratings yet
- 01 Lezione 1 Working LifeDocument18 pages01 Lezione 1 Working LifeVincenzo Di PintoNo ratings yet
- Slingfox RC NotesDocument2 pagesSlingfox RC NotesgauravwordsNo ratings yet
- AtropineDocument6 pagesAtropineNiluh Komang Putri PurnamantiNo ratings yet
- Botanical Survey of IndiaDocument7 pagesBotanical Survey of IndiaParamjit Singh100% (2)
- English Language Communication Skills Lab Manual: Name Roll No. Branch SectionDocument39 pagesEnglish Language Communication Skills Lab Manual: Name Roll No. Branch SectionSurendrakumar ThotaNo ratings yet
- SAT Writing Notes CollegeboardDocument43 pagesSAT Writing Notes CollegeboardEric JoNo ratings yet
- Ulep vs. Legal Clinic, Inc., 223 SCRA 378, Bar Matter No. 553 June 17, 1993Document19 pagesUlep vs. Legal Clinic, Inc., 223 SCRA 378, Bar Matter No. 553 June 17, 1993CherNo ratings yet
- Acc702 - Cost and Management Accounting 1. Assignment 1 - QuestionairesDocument4 pagesAcc702 - Cost and Management Accounting 1. Assignment 1 - QuestionairesLyle BulletzNo ratings yet
- Biochemistry of InflamationDocument45 pagesBiochemistry of Inflamationmichot feleguNo ratings yet
- ForeverDocument2 pagesForeverLymberth BenallaNo ratings yet
- Skema Pppa Kimia k2 2014 (Set 1)Document10 pagesSkema Pppa Kimia k2 2014 (Set 1)Siva Guru0% (1)
- The Impact of Cultural Intelligence On Global BusinessDocument5 pagesThe Impact of Cultural Intelligence On Global BusinessAna Mihaela IstrateNo ratings yet
- Sr. Business Analyst RoleDocument6 pagesSr. Business Analyst RoleDrafting YTNo ratings yet
- Introduction To Constitution of IndiaDocument13 pagesIntroduction To Constitution of IndiaCHRISTINA GAYEN MONDAL100% (1)
- UNITED STATES, Appellee, v. Joseph AITORO, Defendant, AppellantDocument14 pagesUNITED STATES, Appellee, v. Joseph AITORO, Defendant, AppellantScribd Government DocsNo ratings yet
- Thesis Jur ErbrinkDocument245 pagesThesis Jur Erbrinkgmb09140No ratings yet
- Literary Terms: Literatura/litteratura (Derived Itself From Littera: Letter or Handwriting)Document2 pagesLiterary Terms: Literatura/litteratura (Derived Itself From Littera: Letter or Handwriting)Berr WalidNo ratings yet
- InequalitiesDocument6 pagesInequalitiesapi-235135985No ratings yet