Professional Documents
Culture Documents
Swu Phinma, College of Pharmacy 2020: Wr/Urinalysis - Html#Ixzz6Zxlj RQKH /Product-Manual/3008 - 3B - Urinalysis
Uploaded by
Trex MarciiiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Swu Phinma, College of Pharmacy 2020: Wr/Urinalysis - Html#Ixzz6Zxlj RQKH /Product-Manual/3008 - 3B - Urinalysis
Uploaded by
Trex MarciiiCopyright:
Available Formats
Course Code: BIO 024
LAS # 8
BIOCHEMISTRY LABORATORY
URINALYSIS
Activity Title: URINALYSIS Materials:
Objectives: At the end of this activity, you should be able to: Pen, Notes & LAS ( materials are
reflected in each activity)
1. understand the reasons of urinalysis test
1. Perform a gross physical examination on simulated patient urine References:
samples. https://www.surgeryencyclope
dia.com/St-
2. test for the presence of protein in patient urine samples. Wr/Urinalysis.html#ixzz6ZXlj
3. analyse cases RqKH
https://www.3bscientific.com
1. /product-
manual/3008_3B_Urinalysis
Overview
Urine is a liquid containing many waste products that otherwise might be toxic if they were allowed to remain
in the body. The kidneys, part of the excretory system, filter blood circulating throughout the body and remove
toxins. The toxins are removed and beneficial materials are returned back to the circulatory system. The
kidneys also serve to regulate the amount of substances circulating throughout the body. In other words, a
material may be beneficial to the body but in high enough quantities it is able to do harm. The kidneys filter
this material and allow necessary, beneficial levels of the substance to be reabsorbed while filtering the rest out
with waste.
Urinalysis is the analysis of physical and chemical properties of urine. Urine can be a complex mixture of
many components. There is no “set” formula for the composition of urine. It can vary greatly day-to-day or
hour-to-hour. Urine appearance and composition can be affected by many factors such as diet, level of physical
activity (or inactivity), environmental conditions, or fluid intake. Salts, urea, by-products of metabolism, amino
acids and proteins, enzymes, pigments, carbohydrates, or medications are examples of substances that may
appear in a normal urine sample and again, the amount of these substances may vary based on circumstances.
It is a group of manual and/or automated qualitative and semi-quantitative tests performed on a urine sample.
A routine urinalysis usually includes the following tests: color, transparency, specific gravity, pH, protein,
glucose, ketones, blood, bilirubin, nitrite, urobilinogen, and leukocyte esterase. Some laboratories include a
microscopic examination of urinary sediment with all routine urinalysis tests. If not, it is customary to perform
the microscopic exam, if transparency, glucose, protein, blood, nitrite, or leukocyte esterase is abnormal.
Purpose
Routine urinalyses are performed for several reasons:
general health screening to detect renal and metabolic diseases
diagnosis of diseases or disorders of the kidneys or urinary tract
monitoring of patients with diabetes
SWU PHINMA, College of Pharmacy 2020
Course Code: BIO 024
LAS # 8
BIOCHEMISTRY LABORATORY
URINALYSIS
In addition, quantitative urinalysis tests may be performed to help diagnose many specific disorders, such as
endocrine diseases, bladder cancer, osteoporosis, and porphyrias (a group of disorders caused by chemical
imbalance). Quantitative analysis often requires the use of a timed urine sample. The urinary microalbumin
test measures the rate of albumin excretion in the urine using laboratory tests. This test is used to monitor the
kidney function of persons with diabetes mellitus. In diabetics, the excretion of greater than 200 μg/mL
albumin is predictive of impending kidney disease.
Precautions
Voided specimens
All patients should avoid intense athletic training or heavy physical work before the test, as these activities may
cause small amounts of blood to appear in the urine. Many urinary constituents are labile, and samples should
be tested within one hour of collection or refrigerated. Samples may be stored at 36–46°F (2–8°C) for up to 24
hours for chemical urinalysis tests; however, the microscopic examination should be performed within four
hours of collection, if possible. To minimize sample contamination, women who require a urinalysis during
menstruation should insert a fresh tampon before providing a urine sample.
Over two dozen drugs are known to interfere with various chemical urinalysis tests. These include:
ascorbic acid
chlorpromazine
L-dopa
nitrofurantoin (Macrodantin, Furadantin)
penicillin
phenazopyridine (Pyridium)
rifampin (Rifadin)
tolbutamide
The preservatives that are used to prevent loss of glucose and cells may affect biochemical test results. The use
of preservatives should be avoided whenever possible in urine tests.
Description
Routine urinalysis consists of three testing groups: physical characteristics, biochemical tests, and microscopic
evaluation.
Physical tests
The physical tests measure the color, transparency (clarity), and specific gravity of a urine sample. In some
cases, the volume (daily output) may be measured. Color and transparency are determined from visual
observation of the sample.
COLOR. Normal urine is straw yellow to amber in color. Abnormal colors include bright yellow,
brown, black (gray), red, and green. These pigments may result from medications, dietary sources, or diseases.
For example, a pale yellow may simply indicate excessive fluid intake but also may be a sign of diabetes
insipidus, a pink to red urine may be caused by blood or hemoglobin, beets, medications, and some porphyrias.
Straw to amber colored urine may be a sign of dehydration resulting from fever or other illness .Black-gray
urine may result from melanin (melanoma) or homogentisic acid (alkaptonuria, a result of a metabolic
disorder). Bright yellow urine may be caused by bilirubin (a bile pigment) or may indicate a high level of
SWU PHINMA, College of Pharmacy 2020
Course Code: BIO 024
LAS # 8
BIOCHEMISTRY LABORATORY
URINALYSIS
vitamins, especially B vitamins. . An olive green to Green urine could be caused by certain bacterial infections
or the presence of bile pigments ( biliverdin) or certain medications. Orange urine may be caused by some
medications or excessive urobilinogen (chemical relatives of urobilinogen). Brown urine may be caused by
excessive amounts of prophobilin or urobilin (a chemical produced in the intestines) or Brown to black tones
may be signs of phenol or heavy metal poisoning.
TRANSPARENCY. Normal urine is transparent. Turbid (cloudy) urine may be caused by either
normal or abnormal processes. Normal conditions giving rise to turbid urine include precipitation of crystals,
mucus, or vaginal discharge. Abnormal causes of turbidity include the presence of blood cells, yeast, and
bacteria.
SPECIFIC GRAVITY. The specific gravity of urine is a measure of the concentration of dissolved
solutes (substances in a solution), and it reflects the ability of the kidneys to concentrate the urine (conserve
water). Specific gravity is usually measured by determining the refractive index of a urine sample
(refractometry) or by chemical analysis. Specific gravity varies with fluid and solute intake. It will be increased
(above 1.035) in persons with diabetes mellitus and persons taking large amounts of medication. It will also be
increased after radiologic studies of the kidney owing to the excretion of x ray contrast dye. Consistently low
specific gravity (1.003 or less) is seen in persons with diabetes insipidus. In renal (kidney) failure, the specific
gravity remains equal to that of blood plasma (1.008–1.010) regardless of changes in the patient's salt and
water intake. Urine volume below 400 mL per day is considered oliguria (low urine production), and may occur
in persons who are dehydrated and those with some kidney diseases. A volume in excess of 2 liters (slightly
more than 2 quarts) per day is considered polyuria (excessive urine production); it is common in persons with
diabetes mellitus and diabetes insipidus.
Biochemical tests
Biochemical testing of urine is performed using dry reagent strips, often called dipsticks. A urine dipstick
consists of a white plastic strip with absorbent microfiber cellulose pads attached to it. Each pad contains the
dried reagents needed for a specific test. The person performing the test dips the strip into the urine, lets it sit
for a specified amount of time, and compares the color change to a standard chart.
Additional tests are available for measuring the levels of bilirubin, protein, glucose, ketones, and urobilinogen
in urine. In general, these individual tests provide greater sensitivity; they therefore permit detection of a lower
concentration of the respective substance. A brief description of the most commonly used dry reagent strip
tests follows.
pH: A combination of pH indicators (methyl red and bromthymol blue) react with hydrogen ions (H + ) to
produce a color change over a pH range of 5.0 to 8.5. pH measurements are useful in determining metabolic or
respiratory disturbances in acid-base balance. For example, kidney disease often results in retention of
H + (reduced acid excretion). pH varies with a person's diet, tending to be acidic in people who eat meat but
more alkaline in vegetarians. pH testing is also useful for the classification of urine crystals.
Protein: Based upon a phenomenon called the "protein error of indicators," this test uses a pH indicator, such
as tetrabromphenol blue, that changes color (at constant pH) when albumin is present in the urine. Albumin is
important in determining the presence of glomerular damage. The glomerulus is the network of capillaries in
the kidneys that filters low molecular weight solutes such as urea, glucose, and salts, but normally prevents
passage of protein or cells from blood into filtrate. Albuminuria occurs when the glomerular membrane is
damaged, a condition called glomerulonephritis.
Glucose (sugar): The glucose test is used to monitor persons with diabetes. When blood glucose levels rise
above 160 mg/dL, the glucose will be detected in urine. Consequently, glycosuria (glucose in the urine) may be
SWU PHINMA, College of Pharmacy 2020
Course Code: BIO 024
LAS # 8
BIOCHEMISTRY LABORATORY
URINALYSIS
the first indicator that diabetes or another hyperglycemic condition is present. The glucose test may be used to
screen newborns for galactosuria and other disorders of carbohydrate metabolism that cause urinary excretion
of a sugar other than glucose.
Ketones: Ketones are compounds resulting from the breakdown of fatty acids in the body. These ketones are
produced in excess in disorders of carbohydrate metabolism, especially Type 1 diabetes mellitus. In diabetes,
excess ketoacids in the blood may cause life-threatening acidosis and coma. These ketoacids and their salts spill
into the urine, causing ketonuria. Ketones are also found in the urine in several other conditions, including
fever; pregnancy; glycogen storage diseases; and weight loss produced by a carbohydrate-restricted diet.
Blood: Red cells and hemoglobin may enter the urine from the kidney or lower urinary tract. Testing for blood
in the urine detects abnormal levels of either red cells or hemoglobin, which may be caused by excessive red
cell destruction, glomerular disease, kidney or urinary tract infection, malignancy, or urinary tract injury.
Bilirubin: Bilirubin is a breakdown product of hemoglobin. Most of the bilirubin produced in humans is
conjugated by the liver and excreted into the bile, but a very small amount of conjugated bilirubin is reabsorbed
and reaches the general circulation to be excreted in the urine. The normal level of urinary bilirubin is below
the detection limit of the test. Bilirubin in the urine is derived from the liver, and a positive test indicates
hepatic disease or hepatobiliary obstruction.
Specific gravity: Specific gravity is a measure of the ability of the kidneys to concentrate urine by conserving
water.
Nitrite: Some disease bacteria, including the lactose-positive Enterobactericeae, Staphylococcus, Proteus,
Salmonella, and Pseudomonas are able to reduce nitrate in urine to nitrite. A positive test for nitrite indicates
bacteruria, or the presence of bacteria in the urine.
Urobilinogen: Urobilinogen is a substance formed in the gastrointestinal tract by the bacterial reduction of
conjugated bilirubin. Increased urinary urobilinogen occurs in prehepatic jaundice (hemolytic anemia),
hepatitis, and other forms of hepatic necrosis that impair the circulation of blood in the liver and surrounding
organs. The urobilinogen test is helpful in differentiating these conditions from obstructive jaundice, which
results in decreased production of urobilinogen.
Leukocytes: The presence of white blood cells in the urine usually signifies a urinary tract infection, such as
cystitis, or renal disease, such as pyelonephritis or glomerulonephritis.
Microscopic examination
A urine sample may contain cells that originated in the blood, the kidney, or the lower urinary tract.
Microscopic examination of urinary sediment can provide valuable clues regarding many diseases and
disorders involving these systems.
The presence of bacteria or yeast and white blood cells helps to distinguish between a urinary tract infection
and a contaminated urine sample. White blood cells are not seen if the sample has been contaminated. The
presence of cellular casts (casts containing RBCs, WBCs, or epithelial cells) identifies the kidneys, rather than
the lower urinary tract, as the source of such cells. Cellular casts and renal epithelial (kidney lining) cells are
signs of kidney disease.
The microscopic examination also identifies both normal and abnormal crystals in the sediment. Abnormal
crystals are those formed as a result of an abnormal metabolic process and are always clinically significant.
Normal crystals are formed from normal metabolic processes; however, they may lead to the formation of renal
calculi, or kidney stones.
SWU PHINMA, College of Pharmacy 2020
Course Code: BIO 024
LAS # 8
BIOCHEMISTRY LABORATORY
URINALYSIS
Preparation
A urine sample is collected in an unused disposable plastic cup with a tight-fitting lid. A randomly voided
sample is suitable for routine urinalysis, although the urine that is first voided in the morning is preferable
because it is the most concentrated. The best sample for analysis is collected in a sterile container after the
external genitalia have been cleansed using the midstream void (clean-catch) method. This sample may be
cultured if the laboratory findings indicate bacteruria.
To collect a sample using the clean-catch method:
Females should use a clean cotton ball moistened with lukewarm water (or antiseptic wipes provided
with collection kits) to cleanse the external genital area before collecting a urine sample. To prevent
contamination with menstrual blood, vaginal discharge, or germs from the external genitalia, they
should release some urine before beginning to collect the sample.
Males should use a piece of clean cotton moistened with lukewarm water or antiseptic wipes to cleanse
the head of the penis and the urethral meatus (opening). Uncircumcised males should draw back the
foreskin. After the area has been thoroughly cleansed, they should use the midstream void method to
collect the sample.
For infants, a parent or health care worker should cleanse the baby's outer genitalia and surrounding
skin. A sterile collection bag should be attached to the child's genital area and left in place until he or
she has urinated. It is important to not touch the inside of the bag, and to remove it as soon as a
specimen has been obtained.
Urine samples can also be obtained via bladder catheterization, a procedure used to collect uncontaminated
urine when the patient cannot void. A catheter is a thin flexible tube that a health care professional inserts
through the urethra into the bladder to allow urine to flow out. To minimize the risk of infecting the patient's
bladder with bacteria, many clinicians use a Robinson catheter, which is a plain rubber or latex tube that is
removed as soon as the specimen is collected. If urine for culture is to be collected from an indwelling catheter,
it should be aspirated (removed by suction) from the line using a syringe and not removed from the bag in
order to avoid contamination.
Suprapubic bladder aspiration is a collection technique sometimes used to obtain urine from infants younger
than six months or urine directly from the bladder for culture. The doctor withdraws urine from the bladder
into a syringe through a needle inserted through the skin.
Note: Due to unavailability of chemicals at home, at this time you will just perform what can be done at your
home.
Activity # 1 Determination of the Presence of Protein in the Urine
Objectives:
1. Perform a gross physical examination on simulated patient urine samples.
2. Test for the presence of protein in patient urine samples.
SWU PHINMA, College of Pharmacy 2020
Course Code: BIO 024
LAS # 8
BIOCHEMISTRY LABORATORY
URINALYSIS
Materials:
Urine samples ( from 3 different patients or individuals)
Hot Water
Jar with cover
Plastic cups or plastic glass
Marking pens
Part 1: Physical Observation
1. Using a marking pen, label each of your four plastic cups as follows: “A,” “B,” “C,”
2. Using the marking on the cups, fill each cup to approx. 15ml mark with the appropriate urine sample.
Be sure to add the correct sample to each labelled cup.
3. Observe each of the samples for color and clarity. Record the color and clarity of each sample.
Part 2: Test for the Presence of Protein
4. Divide each sample into 2 and label A1 & A2, B1&B2 and C1 &C2 .
5. Put all the samples labelled as #1 in the hot water placed inside a bowl and leave all samples labelled as
# 2 at room temperature.
6. After 5-minutes, remove the jars out of the hot water, and compare the heated and unheated urine. If
the heated sample is cloudy, it contains protein. Protein is normally not found in urine and may be a
sign of high blood pressure, diabetes, or kidney disease. Record your results.
7. Take pictures with your results and post it in our designated platform.
Results
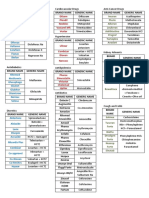
Normal A1 A2 B1 B2 C1 C2
Color
Transparency/Clarity
Protein
Enumerate & Discuss:
1. Enumerate the abnormal colors and possible cause of the color change of the urine.
2. Discuss, why the color of the turns cloudy after heating if there is a presence of protein?
SWU PHINMA, College of Pharmacy 2020
Course Code: BIO 024
LAS # 8
BIOCHEMISTRY LABORATORY
URINALYSIS
Activity # 2 Case Analysis
DATA
Control Px X Px Y Px Z
Color yellow yellow Dark straw, amber yellow
Clarity clear clear clear clear
pH 6.7 6.7 8.9 6.7
Glucose (+/-) (-) (+) (-) (-)
Protein (+/-) (-) (-) (+) (-)
Calcium (+/-) (-) (-) (-) (+)
Questions:
1. Patient X is an overweight 36 year old male. He has recently lost a significant amount of weight though he is
constantly hungry and thirsty. The patient also complained of feeling tired and run down frequently. Based on
the symptoms described and the result of the patient’s urine tests, what do you believe is the most probable
diagnosis?
2. Patient Y is a 21 year old female that has been experiencing a fever and nausea. She is a vegetarian but while
sick has had trouble keeping both food and liquids down. Her doctor suspects it is a bacterial infection. Are
there any symptoms in her urine test results to support this?
3. Patient Z is 65 year old female in for a routine checkup. She is not complaining of any symptoms and
generally feels fine. Is there anything in the results of her urine test that a doctor may want to investigate
further?
4. What was the purpose of the control urine sample in this investigation?
5. Does urinalysis prove the presence of disorder or disease? Explain.
6. If a patient will take an Ascorbic Acid prior to Urinalysis, what is the possible effect on the results? Explain.
7. How medications like antibiotics such as aminoglycosides, cephalosporins and penicillin’s affect the
urinalysis?
SWU PHINMA, College of Pharmacy 2020
You might also like
- Bacte TestDocument10 pagesBacte TestRiondalionNo ratings yet
- Echocardiographic Anatomy in The FetusDocument14 pagesEchocardiographic Anatomy in The FetusAnonymous hOHi6TZTnNo ratings yet
- COMPLETE BLOOD COUNT Lecture GuideDocument9 pagesCOMPLETE BLOOD COUNT Lecture GuideKaycee Gretz LorescaNo ratings yet
- Fundamentals of NursingDocument16 pagesFundamentals of Nursingsorilla_franceschelNo ratings yet
- Culture MediaDocument6 pagesCulture MediaMeiYeng,rmtNo ratings yet
- Saudi Council ExamDocument23 pagesSaudi Council ExamFarooq MohammadNo ratings yet
- OUR LADY OF FATIMA UNIVERSITY MEDICAL LABORATORY SCIENCE BATCH 2024 ANALYSIS OF URINEDocument18 pagesOUR LADY OF FATIMA UNIVERSITY MEDICAL LABORATORY SCIENCE BATCH 2024 ANALYSIS OF URINESarah EugenioNo ratings yet
- DNA Mutations: Types, Causes and EffectsDocument28 pagesDNA Mutations: Types, Causes and EffectsCaroline Nguyen100% (1)
- 13 Biochemical Tests For Gram Negative Bacilli PDFDocument51 pages13 Biochemical Tests For Gram Negative Bacilli PDFSHUPATUSSAINo ratings yet
- Therapeutic Drug MonitoringDocument8 pagesTherapeutic Drug MonitoringLourdette TorrefielNo ratings yet
- Pharmacy Guidelines and Instructions For DAIDS Clinical Trials Networks March 2016Document41 pagesPharmacy Guidelines and Instructions For DAIDS Clinical Trials Networks March 2016GerifalteNo ratings yet
- Principles of Clinical Chemistry AutomationDocument25 pagesPrinciples of Clinical Chemistry AutomationChristine Rodriguez-Guerrero50% (2)
- ConnectivetissuepptDocument20 pagesConnectivetissuepptChicco De AngelisNo ratings yet
- Medical Laws and Regulations SummaryDocument16 pagesMedical Laws and Regulations SummaryNeririNo ratings yet
- Body Fluids Analysis LectureDocument17 pagesBody Fluids Analysis LectureAsd Asd100% (1)
- Tietz's Applied Laboratory MedicineFrom EverandTietz's Applied Laboratory MedicineMitchell G. ScottRating: 3 out of 5 stars3/5 (1)
- Construction Manpower SafetyDocument25 pagesConstruction Manpower SafetyFritz BalasabasNo ratings yet
- Analysis of Urine Reveals E. coli InfectionDocument5 pagesAnalysis of Urine Reveals E. coli InfectionHaridha ChandranNo ratings yet
- Microscopic Examination of UrineDocument4 pagesMicroscopic Examination of UrineGlaiza Erika Baes GudaNo ratings yet
- Agglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4From EverandAgglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4No ratings yet
- Key Acupoints PDFDocument6 pagesKey Acupoints PDFthouartu50% (2)
- Capillaria PhilippinenensisDocument4 pagesCapillaria PhilippinenensisnadalabelNo ratings yet
- Stage A Chemical Pathology OSPE Sample QuestionsDocument10 pagesStage A Chemical Pathology OSPE Sample QuestionsHabib UllahNo ratings yet
- Basic Clinical Chemistry TestsDocument49 pagesBasic Clinical Chemistry TestsMegbaru100% (1)
- Specimen Considerations (Part 2)Document8 pagesSpecimen Considerations (Part 2)Race MendezNo ratings yet
- A. B. C. A. B. C. D.: Clinical Chemistry II - Prelims (Bandala)Document19 pagesA. B. C. A. B. C. D.: Clinical Chemistry II - Prelims (Bandala)IceNo ratings yet
- BSC Licensure Sample QuestionsDocument144 pagesBSC Licensure Sample QuestionsSAMMY0% (1)
- Aubf Lab Types of Urine SpecimenDocument18 pagesAubf Lab Types of Urine SpecimenNerizaNo ratings yet
- Urinalysis Conclusion: Observing Urine Color, Amount, Clarity & pHDocument2 pagesUrinalysis Conclusion: Observing Urine Color, Amount, Clarity & pHOMMONANo ratings yet
- Why morning urine best for urinalysis detectionDocument5 pagesWhy morning urine best for urinalysis detectionabigail lausNo ratings yet
- Aub F Urine Screening For Metabolic DisordersDocument4 pagesAub F Urine Screening For Metabolic DisordersRomie SolacitoNo ratings yet
- Common Plating Media For Clinical Bacteriology (From Bailey & Scott's Diagnostic Microbiology, 12th Ed)Document2 pagesCommon Plating Media For Clinical Bacteriology (From Bailey & Scott's Diagnostic Microbiology, 12th Ed)Elizabeth Enjambre HernaniNo ratings yet
- RCS PreparationDocument3 pagesRCS PreparationMaria Charlene OrpillaNo ratings yet
- 6 - HemoglobinopathiesDocument55 pages6 - HemoglobinopathiesSara BakerNo ratings yet
- EXPT3-IMSELAB-Screening Test For Phagocytic EngulfmentDocument21 pagesEXPT3-IMSELAB-Screening Test For Phagocytic EngulfmentJulie Ann GarceraNo ratings yet
- Lab Clin Test BankDocument87 pagesLab Clin Test Bankemms meNo ratings yet
- Bacteseminar DSSMDocument4 pagesBacteseminar DSSMPrincess AguirreNo ratings yet
- الملزمة الحديثة بعد التعديلclsDocument118 pagesالملزمة الحديثة بعد التعديلclsraghdah alhogail100% (1)
- Clinical Microscopy ReviewerDocument7 pagesClinical Microscopy ReviewerDayledaniel SorvetoNo ratings yet
- Reviewbasic 130709233435 Phpapp02Document130 pagesReviewbasic 130709233435 Phpapp02Andi Namirah100% (1)
- M6 Histopath ImpregantionAndEmbeddingDocument4 pagesM6 Histopath ImpregantionAndEmbeddingninaNo ratings yet
- Urine Specific Gravity MeasurementsDocument1 pageUrine Specific Gravity MeasurementsDennis ValdezNo ratings yet
- Plasma ProteinsDocument8 pagesPlasma ProteinsAaryan50% (2)
- Special TopicsDocument8 pagesSpecial Topicskatherine ruizNo ratings yet
- Clinical Chemistry Assignment 1Document3 pagesClinical Chemistry Assignment 1Lana ZyoudNo ratings yet
- CC Bishop QuestionsDocument3 pagesCC Bishop QuestionsJohanna Kate DiestroNo ratings yet
- Urine Preservatives - SLUDocument2 pagesUrine Preservatives - SLUShana Flame Haze0% (1)
- MedtechDocument7 pagesMedtechLyudmyla GillegoNo ratings yet
- Yeast Invasion of Male's Central Nervous SystemDocument9 pagesYeast Invasion of Male's Central Nervous SystemRomie SolacitoNo ratings yet
- Chem Tech Manual ProcedureDocument4 pagesChem Tech Manual ProcedureChristine Rodriguez-GuerreroNo ratings yet
- CC Partii&III NotesDocument30 pagesCC Partii&III NotesAnielle Mongaya100% (1)
- 1 - MCQs Classified اسئله د محمد امامDocument68 pages1 - MCQs Classified اسئله د محمد امامAhmed GaberNo ratings yet
- Hemoglo-: (Cyanmethemoglobin Method)Document2 pagesHemoglo-: (Cyanmethemoglobin Method)sharik masoodNo ratings yet
- 4 - HemoglobinopathiesDocument19 pages4 - HemoglobinopathiesHamzehNo ratings yet
- Biochemical MethodsDocument119 pagesBiochemical MethodsElias Libay100% (1)
- Estimation of Blood Glucose by Glucometer andDocument15 pagesEstimation of Blood Glucose by Glucometer andmaya hawani100% (1)
- Automated Clinical Chemistry Analyzer-2-2565Document48 pagesAutomated Clinical Chemistry Analyzer-2-2565อัมพกา ทองแท้No ratings yet
- CASE STUDY URINALYSIS DIAGNOSISDocument5 pagesCASE STUDY URINALYSIS DIAGNOSISEdita DevanaNo ratings yet
- Clearance and GFR: Major DR Arabinda Mohan Bhattarai Lecturer (Biochemistry), NAIHSDocument25 pagesClearance and GFR: Major DR Arabinda Mohan Bhattarai Lecturer (Biochemistry), NAIHSChandan SahNo ratings yet
- MCQs in Histochemistry of Biogenic AminesDocument4 pagesMCQs in Histochemistry of Biogenic Aminesashour_abdelsalam6326No ratings yet
- CC Lab 6 TransesDocument6 pagesCC Lab 6 TransesCiara PamonagNo ratings yet
- Lesson 5: Nature of The Clinical LaboratoryDocument8 pagesLesson 5: Nature of The Clinical LaboratoryJohn Daniel AriasNo ratings yet
- 3 Concentration Techniques SedimentationDocument18 pages3 Concentration Techniques SedimentationFatihah JahsmiNo ratings yet
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- Raneem AlbazazDocument33 pagesRaneem AlbazazGordana PuzovicNo ratings yet
- Nursing Care Plan - Docx For CVD (Midterm Case Study)Document8 pagesNursing Care Plan - Docx For CVD (Midterm Case Study)Charisma NecesarioNo ratings yet
- Ophtha Quiz - PACGDocument3 pagesOphtha Quiz - PACGAsif MohammedNo ratings yet
- Texas Complaint - Second Amended Complaint (00135131)Document59 pagesTexas Complaint - Second Amended Complaint (00135131)DoyleRaiznerNo ratings yet
- Granuloma TuberculosisDocument9 pagesGranuloma TuberculosisÁlvaro Alexandro Morales JiménezNo ratings yet
- AdhdDocument7 pagesAdhdAnca CzifraNo ratings yet
- FNCPDocument8 pagesFNCPALESSANDRA SOFIA AMISTOSONo ratings yet
- Xi Cleft (Accumulation Point) : DiagnosisDocument4 pagesXi Cleft (Accumulation Point) : DiagnosisZareen FNo ratings yet
- 0610 w04 QP 1Document16 pages0610 w04 QP 1Vipin DasNo ratings yet
- Nursing Sympathomimetics and SympatholyticsDocument87 pagesNursing Sympathomimetics and SympatholyticsFrancis PeterosNo ratings yet
- Dispensing DrugsDocument1 pageDispensing DrugsIan CalalangNo ratings yet
- Problems faced by construction workers in Tamil NaduDocument3 pagesProblems faced by construction workers in Tamil NaduYamini HarshaNo ratings yet
- Low Vision IntroductionDocument14 pagesLow Vision IntroductionSutrishna PramanikNo ratings yet
- Correlation Between Systemic Risk Factors and Diabetic Macular Edema in Diabetes Mellitus - Dian Paramitasari 1Document8 pagesCorrelation Between Systemic Risk Factors and Diabetic Macular Edema in Diabetes Mellitus - Dian Paramitasari 1Hutami Sri UmmiyatiNo ratings yet
- Pulpectomy PedoDocument30 pagesPulpectomy PedoDr.Harsh100% (1)
- Leishman-Stain Technicaldetails 72320230328.101614Document2 pagesLeishman-Stain Technicaldetails 72320230328.101614RahulNo ratings yet
- Scoliosis Clinical & ExerciseDocument14 pagesScoliosis Clinical & ExercisePurohit_RNo ratings yet
- Single-Cell Map of Diverse Immune Phenotypes in The Breast Tumor MicroenvironmentDocument53 pagesSingle-Cell Map of Diverse Immune Phenotypes in The Breast Tumor MicroenvironmentRoger FigueiredoNo ratings yet
- NCM 109 (ECG and Cardiac Monitoring)Document7 pagesNCM 109 (ECG and Cardiac Monitoring)Kyla BungayNo ratings yet
- Microbiology Flowchart Dr. NikitaDocument2 pagesMicrobiology Flowchart Dr. NikitaKshitij Singh RajputNo ratings yet
- Psychological Trauma: Theory, Research, Practice, and PolicyDocument4 pagesPsychological Trauma: Theory, Research, Practice, and PolicyPerla MontellanoNo ratings yet
- WHO - Adherence ReportDocument211 pagesWHO - Adherence Reportscratch9100% (1)
- Cambridge International AS & A Level: BIOLOGY 9700/21Document20 pagesCambridge International AS & A Level: BIOLOGY 9700/21jamalNo ratings yet