Professional Documents
Culture Documents
Lupus Nephritis and NP SLE
Uploaded by
divisiimunOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lupus Nephritis and NP SLE
Uploaded by
divisiimunCopyright:
Available Formats
ORIGINAL ARTICLE
Clinical features and mortality in Chinese with
lupus nephritis and neuropsychiatric lupus:
A 124-patient study
Min Feng, Jun Lv, Sha Fu, Bo Liu, Ying Tang, Xia Wan, Peifen Liang, Yuchun Zeng, Jingao Li, Yanying Lu,
Xiaomei Li, Anping Xu
Department of Nephrology, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, China
Background: Few investigation has focused on the patients with lupus nephritis (LN) and neuropsychiatric systemic lupus
erythematosus (NPSLE). This study was aimed to investigate the clinical features, mortality, and the predictors for mortality of this
group of patients. Materials and Methods: Medical records were retrospectively reviewed in Sun Yat-sen Memorial Hospital from
1996 to 2012. Data of demographic information, clinical manifestations, laboratory tests, SLE disease activity index 2000 (SLEDAI-
2K) score, diagnosis, complications, treatment, and mortality was collected. Results: A total of 124 patients were included in our
study. Thirty-five (29.1%) patients had glomerular filtration rate <60 ml/min/1.73 m2, while 24 (19.4%) experienced acute kidney
injury (AKI). Thirteen of the 19 American College of Rheumatology defined NPSLE syndromes were identified. The most frequent
manifestation was seizure disorder (56/124, 45.2%), followed by psychosis (37/124, 29.8%) and cerebrovascular disease (35/124,
28.2%). One hundred and five (84.7%) patients had SLEDAI-2K scores ≥15, the mean of which was 21.5 ± 6.2. The mortality during
hospitalization was 12.9% (16/124) with NP involvement itself being the leading cause of death (7/16, 43.8%). Multivariate logistic
regression confirmed that age <14 years at onset of NPSLE (odds ratios [OR]: 9.95, 95% confidence intervals [CI]: 1.43-69.36, P =
0.020), AKI (OR: 10.40, 95% CI: 2.33-46.48, P = 0.002) and pneumonia (OR: 4.52, 95% CI: 1.14-17.96, P = 0.032) were risk factors for
mortality, while cyclophosphamide (CYC) treatment (OR: 0.09, 95% CI: 0.02-0.54, P = 0.008) was a protective factor. Conclusion:
Most of SLE patients with LN and new-onset NPSLE are in an active disease state. NP manifestation itself was the leading cause of
death during hospitalization. Childhood-onset NPSLE, AKI and pneumonia might be predictors of mortality, whereas CYC treatment
might improve the prognosis.
Key words: Lupus nephritis, mortality, multivariate logistic regression, neuropsychiatric systemic lupus erythematosus
How to cite this article: Feng M, Lv J, Fu S, Liu B, Tang Y, Wan X, Liang P, Zeng Y, Li J, Lu Y, Li X, Xu A. Clinical features and mortality in Chinese
with lupus nephritis and neuropsychiatric lupus: A 124-patient study. J Res Med Sci 2014;19:414-9.
INTRODUCTION PATIENTS AND METHODS
Systemic lupus erythematosus (SLE) is a complicated Patients
disease that has different outcomes mainly depends This was a retrospective study. Medical records were
on the manifestations and treatments. The kidney and reviewed of all SLE patients with LN and new-onset
the nervous system are o en involved in SLE, which NP manifestations who were admi ed to Sun Yat-sen
named lupus nephritis (LN) and neuropsychiatric Memorial Hospital of Sun Yat-sen University, Guangzhou,
SLE (NPSLE) respectively. It has been reported that China, from April 1996 to September 2012. Besides the
3.5-27.8% of LN patients accompanied with NP clinical features, we particularly focused on the mortality
manifestations,[1,2] while 40-80% of NPSLE patients during hospitalization and the associated factors.
had nephritis.[3-5] Both of these two complications are
associated with increased morbidity and mortality.[6-8] Systemic lupus erythematosus was defined by 1997 revised
Until date, few investigation has focused on the American College of Rheumatology (ACR) classification
population of patients both having LN and NPSLE. criteria.[9] Disease activity at onset of NPSLE was evaluated
In our study, we retrospectively reviewed the data using the SLE disease activity index 2000 (SLEDAI-2K).[10]
of SLE patients with LN and new-onset NPSLE in The scores were evaluated before treatment.
our center, aiming to investigate the clinical features,
mortality during hospitalization and the predictors Lupus nephritis was defined as persistent proteinuria
for outcome. more than 0.5 g/day or proteinuria more than 3+
Address for correspondence: Prof. Anping Xu, Department of Nephrology, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, 107 West Yanjiang
Road, Guangzhou - 510 120, China. E-mail: anpxu_sys@163.com
Received: 05-02-2014; Revised: 05-03-2014; Accepted: 16-04-2014
| May 2014 | Journal of Research in Medical Sciences 414
Feng, et al.: Clinical features and mortality in Chinese with LN and NPSLE
if quantitation not performed, or cellular casts-might mg plus dexamethasone (DXM) 5 or 10 mg weekly, with or
be red cell, hemoglobin, granular, tubular, or mixed.[9] without repeated injection depending on the severity and
Urine analysis, 24-h proteinuria, serum creatinine, serum the response to this treatment, which could be combined
albumin, glomerular filtration rate (GFR), presence of with other systemic immunosuppressive agents.
hypertension and presence of acute kidney injury (AKI)
were collected to evaluate the degree of renal injury. GFR We analyzed the data of demographic information, clinical
was estimated for the purpose of evaluating the renal manifestations, laboratory tests, SLEDAI-2K scores,
function by the Modification of Diet in Renal Disease diagnosis, complications, treatment, and mortality during
method. [11] Hypertension was defined as values ≥140 hospitalization.
mmHg systolic blood pressure (SBP) and/or ≥90 mmHg
diastolic blood pressure (DBP) in adults[12] and SBP and/or Ethical consideration
DBP persistently 95th percentile or more measured at least This study was approved by the Ethics Commi ee in Sun
three separate occasions with the auscultatory method in Yat-sen Memorial Hospital of Sun Yat-sen University,
children and adolescents.[13] AKI was defined by the Kidney Guangzhou, China.
Disease Improving Global Outcomes guideline.[14] Specific
investigations for LN such as renal biopsy were carried Statistical analysis
out in part of the patients. Histopathologic lesions of LN Results with continuous data were presented as mean
were categorized according to the classification revised by ± standard deviation, while the data did not follow a
International Society of Nephrology (ISN) and the Renal symmetric distribution presented with median (range).
Pathology Society (RPS) in 2003.[15] Categorical data were presented as the absolute count
and percentage. Associated factors of mortality during
Neuropsychiatric systemic lupus erythematosus was hospitalization were analyzed by univariate analysis and
defined by the ACR nomenclature and case definitions multivariate logistic regression. Odds ratios (OR) and 95%
published in 1999,[16] excluding the comorbid conditions confidence intervals (CI) were calculated. Statistical analysis
and concomitant factors of offending drugs, central was performed using SPSS 19.0 (IBM® SPSS® Statistics).
nervous system infection, tumor and known metabolic P < 0.05 was considered to be statistically significant.
derangements; e.g., hypoglycemia, ketoacidosis, hypoxemia,
uremia, or electrolyte imbalance. Many of the patients RESULTS
underwent neurological investigations such as magnetic
resonance imaging (MRI) of nervous system, computerized Demographic information
tomographic scanning of the head, electroencephalograms Our study examined the medical records of 124 hospitalized
and cerebrospinal fluid (CSF) examination as part of the SLE patients with both kidney involvement and new-onset
diagnostic evaluation of nervous system involvement. NP manifestations. There were 111 females and 13 males,
Abnormal CSF examinations were defined as described with a ratio 8.5-1. The mean age at onset of NPSLE was 29.2 ±
elsewhere.[17] The identification and classification of NPSLE 13.4 years (range: 10-72 years). 10 (8.1%) were under 14 years
was confirmed by at least two neurologists or psychiatrists old at the onset of NPSLE. The median duration of SLE was
independently. 36 months (range: 0-264 months), while the median duration
of LN was 8 months (range: 0-216 months). Fi y-one patients
All patients received oral corticosteroids, which consisted (41.1%) had nephritic manifestations at the time of initial
of prednisone 1 mg/kg/day or methylprednisolone (MP) diagnosis of SLE, while only 5 (4.0%) had both nephritic and
0.8 mg/kg/day for 8 weeks followed by tapering dose as NP manifestations at the onset of SLE [Table 1].
indicated. Besides, a er the onset of NPSLE, most of them
had received additional one or more immunosuppressive Nephritic characteristics
strategies as follows: (1) Pulse intravenous MP (IVMP) Nephritic characteristics of 124 patients at the onset of NP
therapy consisted of IVMP 0.5~1.0 g/day for 3~5 days manifestations were presented as follows: One hundred and
as a cycle, with or without other cycles 1~4 weeks later fi een patients (92.7%) had proteinuria, of which 45 (36.3%)
depending on the severity of disease and the effect of this had 24-h proteinuria ≥3.5 g. Nearly, half of the patients
treatment; (2) oral or IV cyclophosphamide (CYC) 0.2 (54/124, 43.5%) presented with hypertension. Thirty-five
mg/kg/day, or a single dose of IV CYC 0.5~1.0 g/1.73 m2 (29.1%) patients had impaired renal function with GFR <60
monthly; (3) other systemic immunosuppressive therapy ml/min/1.73 m2, while 24 (19.4%) experienced AKI. Only 22
included oral mycophenolate mofetil (MMF) 0.5~1.5 g/day, (17.7%) patients had performed percutaneous renal biopsy
oral azathioprine (AZA) 2~2.5 mg/kg/day, oral ciclosporin during the onset period of NP manifestation or before, ISN/
(CsA) 3~5 mg/kg/day or oral tacrolimus 0.08~0.1 mg/kg/day; RPS Class II LN was the most frequent pathologic type (9/22,
(4) intrathecal injection (IT) of methotrexate (MTX) 5 or 10 40.9%), followed by Class I (4/22, 18.2%), Class III (3/22,
415 Journal of Research in Medical Sciences | May 2014 |
Feng, et al.: Clinical features and mortality in Chinese with LN and NPSLE
13.6%), Class IV (3/22, 13.6%) and Class V (3/22,13.6%). Only three. Central nervous system involvement accounted for
one patient had totally normal urine and renal function 98.4% (122/165) with only 1.6% (2/165) of peripheral nervous
during the onset of NPSLE, who had been proven ISN/RPS system. The most frequent manifestation was seizure
Class I LN by renal biopsy 5 years before. disorder, followed by psychosis, cerebrovascular disease,
headache and mood disorder [Table 2].
Neuropsychiatric characteristics
Magnetic resonance imaging of the nervous system was the
A total of 165 NP events occurred in 124 patients. Thirteen of
most widely used investigation in NPSLE patients, with
the 19 ACR syndromes were identified in our study [Table 2].
50 out of 72 (69.4%) patients showing abnormal findings.
80 patients (64.5%) presented with one set of NP symptoms, 49 (39.5%) patients had performed lumbar puncture, and
while 44 (35.5%) had more than one with a maximum of increased protein level was the most frequent abnormal
manifestations of CSF [Table 2].
Table 1: Demographic information
Characteristic Patients SLE disease activity and other characteristics
(n = 124) One hundred and five (84.7%) patients had SLEDAI-
Gender (n [%]) 2K scores ≥15, the mean of which was 21.5 ± 6.2, with
Male 13 (10.5)
the highest of 35. One hundred and eighteen patients
Female 111 (89.5)
(95.2%) had positive anti-nuclear antibodies, 111 (89.5%)
Age at onset of NPSLE (years; mean±SD) 29.2±13.4
had elevated anti-dsDNA antibodies, 99 (79.8%) had
Age <14 years at onset of NPSLE (n [%]) 10 (8.1)
Age at initial diagnosis of SLE (years; mean±SD) 25.5±12.3
decreased serum complement C3 level, 72 (58.1%) had
Age <14 years at initial diagnosis of SLE (n [%]) 24 (19.4) decreased serum complement C4 level, 112 (90.3%) had
SLE duration (months; median [range]) 36 (0-264) accelerated erythrocyte sedimentation rate. With regard
LN duration (months; median [range]) 8 (0-216) to the complication, 35 (28.2%) patients were accompanied
Having LN at initial diagnosis of SLE (n [%]) 51 (41.1) by pneumonia.
Having both LN and NPSLE at initial diagnosis of SLE (n [%]) 5 (4.0)
NPSLE = Neuropsychiatric systemic lupus erythematosus; SLE = Systemic lupus Treatment
erythematosus; LN = Lupus nephritis; SD = Standard deviation
Pulse IVMP was the most frequent used therapeutic method
(62/124, 50.0%) followed by oral or IV CYC (61/124, 49.2%).
Table 2: NP characteristics 34 (27.4%) patients had received combined treatment of
NP characteristics Number of patients (%) pulse IVMP plus oral or IV CYC. Other immunosuppressive
(n = 124)
drugs such as MMF, AZA, CsA and tacrolimus were
Manifestationsa
administered in 13.7% (17/124), 9.7% (12/124), 5.6% (7/124)
Central nervous system
Seizure disorder 56 (45.2)
and 4.0% (5/124) of patients respectively. At least one IT
Psychosis 37 (29.8) injection with MTX plus CYC was administered to 25
Cerebrovascular disease 35 (28.2) (20.2%) patients.
Headache 14 (11.3)
Mood disorder 10 (8.1) Mortality during hospitalization
Acute confusional state 3 (2.4) The mortality during hospitalization was 12.9% (16/124)
Cognitive dysfunction 3 (2.4) in this group of patients. NP involvement itself being the
Anxiety disorder 2 (1.6) leading cause of death, other causes of death included heart
Myelopathy 2 (1.6) failure, infection, AKI and hemorrhage [Table 3]. One patient
Demyelinating syndrome 1 (0.8)
died of cerebrovascular hemorrhage due to bone marrow
Peripheral nervous system
suppression induced by IT injection of MTX at the 2nd time.
Myasthenia gravis 1 (0.8)
Autonomic disorder 1 (0.8)
Abnormal neuroimaging studies
Correlative factors of mortality during hospitalization
MRI 50/72 (69.4) Univariate analysis showed that age <14 years at onset of
CT scan 14/28 (50.0) NPSLE (P = 0.002), hypertension (P = 0.036), AKI (P < 0.001),
EEG 18/28 (64.3) epilepsy (P = 0.050), pneumonia (P = 0.001), CYC treatment
Abnormal CSF findings (P = 0.006) were the correlative factors of mortality during
Elevated pressure 19/49 (38.8) hospitalization. Multivariate logistic regression further
Increased WBC count 4/49 (8.2) confirmed that age <14 years at onset of NPSLE (OR: 9.95,
Increased protein level 25/49 (51.0) 95% CI: 1.43-69.36, P = 0.020), AKI (OR: 10.40, 95% CI:
a
One patient might have more than one manifestation; NP = Neuropsychiatric;
LN = Lupus nephritis; MRI = Magnetic resonance imaging; CT = Computerized tomographic;
2.33-46.48, P = 0.002) and pneumonia (OR: 4.52, 95% CI:
EEG = Electroencephalogram; CSF = Cerebrospinal fluid; WBC = White blood cell 1.14-17.96, P = 0.032) were risk factors for mortality during
| May 2014 | Journal of Research in Medical Sciences 416
Feng, et al.: Clinical features and mortality in Chinese with LN and NPSLE
hospitalization, while CYC treatment (OR: 0.09, 95% CI: 0.02- the mean SLEDAI-2K score was 21.5 ± 6.2 and 84.7% patients
0.54, P = 0.008) was a protective factor for survival [Table 4]. had SLEDAI-2K scores ≥15, indicating that the disease might
be more severe and more active in our patients. In our
DISCUSSION study, ISN/APS Class II LN (40.9%) was the predominant
pathologic type, whereas Class IV only accounted for 13.6%,
In our study, we investigated the main clinical features of which is different from current LN studies that Class IV
SLE patients with LN and new-onset NPSLE, estimated represents the most common pathologic type no ma er in
the mortality during hospitalization and analyzed the western or Asian countries.[19-22] It may be explained that
correlative factors for mortality. renal biopsy had been performed on only 17.7% of our
patients with NPSLE, who might be in a less severe disease
Clinical features of LN at the onset of NPSLE were state so that could endure the performance of renal biopsy.
investigated in our study. We found that proteinuria (92.7%) And the selecting bias of the patients to perform renal biopsy
presented as the most common manifestation, which is leads to the less severity in renal pathological results.
consistent with that of general LN patients as previously
reported in western countries.[18] The frequency of nephrotic With regard to the NP features, 13 of 19 ACR defined NP
syndrome is 36.3% in our patients with the similarity manifestations occurred in our study. The most frequent NP
of 35-65% reported in western and Asian LN patients manifestation of LN patients was seizure disorder (45.2%),
before.[1,18,19] And what’s more, the frequency of hypertension followed by psychosis (29.8%) and cerebrovascular disease
(43.5%) is similar to previous studies, which reported that (28.2%). The distribution of NP manifestations is different
hypertension appeared in around 15-50% LN patients.[18] in different SLE studies.[5,23-25] It was found that seizure
A previous study showed that AKI occurred in 20.5% LN occurred related to nephritis and cumulative organ damage
patients,[20] which is consistent with the result of 19.4% in our in SLE,[26,27] which might contribute to the high prevalence
investigation. The incidence of impaired renal function with of seizure in our study. Among the examinations for the
a GFR <60 ml/min/1.73 m2 was 29.1% in our study, which diagnosis of NPSLE, MRI of the nervous system was the
is higher than 10-20% of other studies in LN patients.[1,21,22] most widely used neuroimaging technique with a positive
The reason might be that the population in our study was rate of 69.4% in our study, being consistent with 60-78%
the LN patients with new-onset NP manifestations, of which of previous studies on Chinese or other ethnic NPSLE
patients.[23,25,28] CSF analysis found that increased protein
Table 3: Main causes of death during hospitalization
level in 51.0% of patients was the most frequent abnormal
Main causes of death Number of findings, which is similar to 53% of Yu’s study.[5]
patients died (%)
NP involvement 7 (43.8) The mortality during hospitalization of LN patients with
Seizure 5 (31.2) NP manifestation was 12.9%, which is similar to 10.8%
Cerebrovascular hemorrhage 2 (12.5) reported in NPSLE patients.[23] The main reason for death
Heart failure 4 (25.0) was NP involvement itself which is consistent with other
Infection 2 (12.5) NPSLE studies.[23,29] Taking the factors including age at
AKI 1 (6.3)
onset of NPSLE, hypertension, AKI, NP manifestations,
Pulmonary hemorrhage 1 (6.3)
pneumonia and treatments into account, multivariate
Cerebrovascular hemorrhage due to side 1 (6.3)
effect of drug logistic regression found that age <14 years at onset of
Total 16 NPSLE, AKI and pneumonia were associated with death,
NP = Neuropsychiatric; AKI = Acute kidney injury while CYC treatment contributed to survival.
Table 4: Correlative factors of mortality during hospitalization
Factors Dead group Survival group Univariate analysis P Multivariates P
(n = 16) (n [%]) (n = 108) (n [%]) OR (95%CI) analysis OR (95%CI)
Age <14 years at onset of NPSLE 5 (31.3) 5 (4.6) 9.36 (2.34-37.47) 0.002* 9.95 (1.43-69.36) 0.020*
Hypertension 10 (62.5) 44 (40.7) 3.33 (1.08-10.25) 0.036* — 0.132
AKI 8 (50.0) 16 (14.8) 7.97 (2.58-24.63) <0.001* 10.40 (2.33-46.48) 0.002*
Epilepsy 11 (68.8) 45 (41.7) 3.08 (1.00-9.48) 0.050* — 0.657
Pneumonia 11 (68.8) 24 (22.2) 7.65 (2.41-24.27) 0.001* 4.52 (1.14-17.96) 0.032*
CYC 2 (12.5) 59 (54.6) 0.12 (0.03-0.55) 0.006* 0.09 (0.02-0.54) 0.008*
Pulse IVMP + CYC 2 (12.5) 32 (29.6) 0.34 (0.07-1.58) 0.168 — —
IT injection 3 (18.8) 22 (20.4) 0.90 (0.24-3.45) 0.880 — —
*Statistically significant; NPSLE = Neuropsychiatric systemic lupus erythematosus; GFR = Glomerular filtration rate; AKI = Acute kidney injury; CYC =Cyclophosphamide; IVMP =
Intravenous methylprednisolone; IT = Intrathecal; OR = Odds ratio; CI = Confidence interval
417 Journal of Research in Medical Sciences | May 2014 |
Feng, et al.: Clinical features and mortality in Chinese with LN and NPSLE
It has been reported that approximately 15-20% of patients series the number of patients that received this treatment
with SLE are diagnosed during childhood,[30] which is similar was too small to have favorable result. The effects of
to our study with the result of 19.4%. Moreover, we also MMF, AZA, CsA and tacrolimus in NPSLE are uncertain,
found that the proportion of children under 14 years old in which were only reported sporadically.[43-46] In our study,
the deaths was significantly higher than that in the survivals only a li le part of patients had been prescribed these
(31.5% vs. 4.6%). Childhood-onset NPSLE was found to be immunosuppressive drugs.
an independent risk factor for mortality in our investigation,
which might be explained by the previous studies showing In summary, most SLE patients with both LN and new-onset
that childhood-onset SLE has a more aggressive course, NPSLE are in an active disease state. NP manifestation
higher rates of renal and NP involvement and higher itself is the leading cause of death during hospitalization
mortality rate compared with adult-onset SLE.[31,32] in this group of patients. Childhood-onset NPSLE, AKI and
pneumonia might be predictors of mortality, whereas CYC
In SLE, a considerable proportion of patients present with treatment might improve the prognosis. However, this is
AKI as reported by many previous studies. In our study, only a retrospective investigation with some limitations that
AKI appeared in 19.4% of patients, which appeared more may bias the results. A prospective follow-up study with
frequently in the deaths than in the survivals (50.0% vs. a large number of patients needs to be conducted for the
14.8%) as being a predictor of mortality. Looking into a purpose of confirming the results.
previous AKI study, the authors found that SLE patients
with AKI had significantly higher proportions of neurologic ACKNOWLEDGMENTS
disorder and higher SLEDAI-2K scores, what’s more, AKI
was an independent risk factor for renal outcome.[20] SLE We thank Dr. Jing Hou (School of Public Health and Primary Care,
with AKI seems to be more active and more severe, by which The Chinese University of Hong Kong) for her help with statistical
our result might be partially explained. consultation.
Infection is a common complication of corticosteroids and AUTHORS’ CONTRIBUTIONS
other immunosuppressive drugs, which is severe and
not easy to control in some cases. Pneumonia is the most MF carried out the design and coordinated the study,
common type of infection in the SLE patients,[33] and it is participated in most of the experiments and prepared the
associated with death as previous study reported.[34] In our manuscript. JL, SF, BL coordinated and carried out all the
study, we found that the incidence of pneumonia in the experiments. YT, XW, PFL, YCZ, JGL, YYL, XML, and APX
deaths was significantly higher than that in the survivals provided assistance for all experiments. All authors have
(68.8% vs. 22.2%), which was found to be a risk factor for read and approved the content of the manuscript.
mortality. Our result is consistent with the previous result
as mentioned above.[34] REFERENCES
1. Zheng ZH, Zhang LJ, Liu WX, Lei YS, Xing GL, Zhang JJ, et al.
Various studies about treatment of LN have been reported, Predictors of survival in Chinese patients with lupus nephritis.
which have shown the effectiveness of CYC, MMF, CsA, Lupus 2012;21:1049-56.
tacrolimus and AZA on LN.[35-37] But as so far, study about 2. Vyas S, Hidalgo G, Baqi N, Von Gizyki H, Singh A. Outcome in
treatment of NPSLE is not that abundant. The only one African-American children of neuropsychiatric lupus and lupus
nephritis. Pediatr Nephrol 2002;17:45-9.
controlled clinical trial in NPSLE is the study comparing
3. Garin EH, Donnelly WH, Fennell RS 3rd, Richard GA. Nephritis in
the efficacy of IV CYC and IVMP. The result showed that IV systemic lupus erythematosus in children. J Pediatr 1976;89:366-71.
CYC was more effective than IVMP in the treatment of acute, 4. Cameron JS. Lupus nephritis in childhood and adolescence. Pediatr
severe NPSLE.[38] Except for that, several retrospective studies Nephrol 1994;8:230-49.
have also shown the effectiveness of CYC in NPSLE,[39,40] 5. Yu HH, Lee JH, Wang LC, Yang YH, Chiang BL. Neuropsychiatric
which is consistent with our result that CYC treatment was manifestations in pediatric systemic lupus erythematosus: A
20-year study. Lupus 2006;15:651-7.
a protective factor for survival. Meanwhile, a small trial has
6. Ward MM, Pyun E, Studenski S. Mortality risks associated with
found that IVMP plus IV CYC made favorable outcome in specific clinical manifestations of systemic lupus erythematosus.
severe NLSLE children.[41] In our study, although it seemed Arch Intern Med 1996;156:1337-44.
that pulse IVMP plus CYC treatment was prescribed more 7. Rubin LA, Urowitz MB, Gladman DD. Mortality in systemic lupus
frequently in the survivals than in the deaths (29.6% vs. erythematosus: The bimodal pa ern revisited. Q J Med 1985;55:87-98.
8. Gibson T, Myers AR. Nervous system involvement in systemic
12.5%), but the difference was not significant (P = 0.168),
lupus erythematosus. Ann Rheum Dis 1975;35:398-406.
which might be due to only a small number of patients had 9. Hochberg MC. Updating the American College of Rheumatology
received this combined treatment. IT injection of MTX plus revised criteria for the classification of systemic lupus
DXM was reported to be effective in NPSLE,[42] but in our erythematosus. Arthritis Rheum 1997;40:1725.
| May 2014 | Journal of Research in Medical Sciences 418
Feng, et al.: Clinical features and mortality in Chinese with LN and NPSLE
10. Gladman DD, Ibañez D, Urowitz MB. Systemic lupus erythematosus 29. Zirkzee EJ, Huizinga TW, Bollen EL, van Buchem MA,
disease activity index 2000. J Rheumatol 2002;29:288-91. Middelkoop HA, van der Wee NJ, et al. Mortality in neuropsychiatric
11. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more systemic lupus erythematosus (NPSLE). Lupus 2014;23:31-8.
accurate method to estimate glomerular filtration rate from serum 30. Cassidy JT, Pe y RE. Textbook of Pediatric Rheumatology. 5th ed.
creatinine: A new prediction equation. Modification of Diet in Philadelphia: Elsevier Saunders; 2005.
Renal Disease Study Group. Ann Intern Med 1999;130:461-70. 31. Tucker LB, Uribe AG, Fernández M, Vilá LM, McGwin G, Apte M,
12. ESH/ESC Task Force for the Management of Arterial et al. Adolescent onset of lupus results in more aggressive disease
Hypertension. 2013 Practice guidelines for the management of and worse outcomes: Results of a nested matched case-control
arterial hypertension of the European Society of Hypertension study within LUMINA, a multiethnic US cohort (LUMINA LVII).
(ESH) and the European Society of Cardiology (ESC): ESH/ Lupus 2008;17:314-22.
ESC Task Force for the Management of Arterial Hypertension. J 32. Brunner HI, Gladman DD, Ibañez D, Urowitz MD, Silverman ED.
Hypertens 2013;31:1925-38. Difference in disease features between childhood-onset and
13. Lurbe E, Cifkova R, Cruickshank JK, Dillon MJ, Ferreira I, adult-onset systemic lupus erythematosus. Arthritis Rheum
Invi i C, et al. Management of high blood pressure in children 2008;58:556-62.
and adolescents: Recommendations of the European Society of 33. Goldblatt F, Chambers S, Rahman A, Isenberg DA. Serious
Hypertension. J Hypertens 2009;27:1719-42. infections in British patients with systemic lupus erythematosus:
14. Kellum JA, Lameire N, Aspelin P. KDIGO clinical practice guideline Hospitalisations and mortality. Lupus 2009;18:682-9.
for acute kidney injury. Kidney Int Suppl 2012;2:1-138. 34. Souza DC, Santo AH, Sato EI. Mortality profile related to systemic
15. Weening JJ, D’Agati VD, Schwartz MM, Seshan SV, Alpers CE, lupus erythematosus: A multiple cause-of-death analysis. J
Appel GB, et al. The classification of glomerulonephritis in Rheumatol 2012;39:496-503.
systemic lupus erythematosus revisited. Kidney Int 2004;65: 35. Lightstone L. Lupus nephritis: Where are we now? Curr Opin
521-30. Rheumatol 2010;22:252-6.
16. The American College of Rheumatology nomenclature and case 36. Bomback AS, Appel GB. Updates on the treatment of lupus
definitions for neuropsychiatric lupus syndromes. Arthritis Rheum nephritis. J Am Soc Nephrol 2010;21:2028-35.
1999;42:599-608. 37. Tesar V, Hruskova Z. Treatment of proliferative lupus nephritis:
17. William WC. Dejong’s the Neurologic Examination. 7th ed. China: A slowly changing landscape. Nat Rev Nephrol 2011;7:96-109.
Lippinco Williams and Wilkins; 2013. p. 737-44. 38. Barile-Fabris L, Ariza-Andraca R, Olguín-Ortega L, Jara LJ, Fraga-
18. Cameron JS. Lupus nephritis. J Am Soc Nephrol 1999;10:413-24. Mouret A, Miranda-Limón JM, et al. Controlled clinical trial of
19. Yokoyama H, Okuyama H, Yamaya H. Clinicopathological insights IV cyclophosphamide versus IV methylprednisolone in severe
into lupus glomerulonephritis in Japanese and Asians. Clin Exp neurological manifestations in systemic lupus erythematosus.
Nephrol 2011;15:321-30. Ann Rheum Dis 2005;64:620-5.
20. Zhu D, Qu Z, Tan Y, Yu F, Zhao MH. Acute kidney injury in Chinese 39. Neuwelt CM, Lacks S, Kaye BR, Ellman JB, Borenstein DG. Role
patients with lupus nephritis: A large cohort study from a single of intravenous cyclophosphamide in the treatment of severe
center. Lupus 2011;20:1557-65. neuropsychiatric systemic lupus erythematosus. Am J Med
21. Martins L, Rocha G, Rodrigues A, Santos J, Vasconcelos C, 1995;98:32-41.
Correia J, et al. Lupus nephritis: A retrospective review of 78 cases 40. Sanna G, Bertolaccini ML, Mathieu A. Central nervous system
from a single center. Clin Nephrol 2002;57:114-9. lupus: A clinical approach to therapy. Lupus 2003;12:935-42.
22. Uthman IW, Muffarij AA, Mudawar WA, Nasr FW, Masri AF. 41. Baca V, Lavalle C, García R, Catalán T, Sauceda JM, Sánchez G,
Lupus nephritis in Lebanon. Lupus 2001;10:378-81. et al. Favorable response to intravenous methylprednisolone and
23. Zhou HQ, Zhang FC, Tian XP, Leng XM, Lu JJ, Zhao Y, et al. Clinical cyclophosphamide in children with severe neuropsychiatric lupus.
features and outcome of neuropsychiatric lupus in Chinese: J Rheumatol 1999;26:432-9.
Analysis of 240 hospitalized patients. Lupus 2008;17:93-9. 42. Xuan Z, Yi D, Fu-Lin T, Fen-Chun Z. Central nervous system
24. Hanly JG. Diagnosis and management of neuropsychiatric involvement in systemic lupus erythematosus in a hospital-based
SLE. Nat Rev Rheumatol 2014;10:338-47. Feb 11. doi:10.1038/ study of 171 cases: The possible therapeutic role of intrathecal
nrrheum.2014.15 therapy. J Clin Rheumatol 1999;5:314-9.
25. Abdul-Sattar AB, Goda T, Negm MG. Neuropsychiatric 43. Benseler SM, Silverman ED. Neuropsychiatric involvement in
manifestations in a consecutive cohort of systemic lupus pediatric systemic lupus erythematosus. Lupus 2007;16:564-71.
erythematosus; a single center study. Int J Rheum Dis 2013;16: 44. Popescu A, Kao AH. Neuropsychiatric systemic lupus
715-23. erythematosus. Curr Neuropharmacol 2011;9:449-57.
26. Appenzeller S, Cendes F, Costallat LT. Epileptic seizures in 45. Mok CC. Mycophenolate mofetil for non-renal manifestations
of systemic lupus erythematosus: A systematic review. Scand J
systemic lupus erythematosus. Neurology 2004;63:1808-12.
Rheumatol 2007;36:329-37.
27. Hanly JG, Urowitz MB, Su L, Gordon C, Bae SC, Sanchez-
46. Kizu H, Dobashi H, Kameda T, Susaki K, Kawanishi M, Ishida T.
Guerrero J, et al. Seizure disorders in systemic lupus erythematosus
Improvement of irregularity of brain vessel walls in systemic lupus
results from an international, prospective, inception cohort study.
erythematosus by tacrolimus. Clin Rheumatol 2011;30:715-8.
Ann Rheum Dis 2012;71:1502-9.
28. Steup-Beekman GM, Zirkzee EJ, Cohen D, Gahrmann BM,
Emmer BJ, Steens SC, et al. Neuropsychiatric manifestations in Source of Support: This work was supported by grant from Guangdong
patients with systemic lupus erythematosus: Epidemiology and Natural Science Foundation (S2012010009667) and Guangdong Science
radiology pointing to an immune-mediated cause. Ann Rheum and Technology Planning Project (2011B031800122), Conflict of Interest:
None declared.
Dis 2013;72 Suppl 2:ii76-9.
419 Journal of Research in Medical Sciences | May 2014 |
You might also like
- Clinical Neuroimmunology: Multiple Sclerosis and Related DisordersFrom EverandClinical Neuroimmunology: Multiple Sclerosis and Related DisordersNo ratings yet
- 1536 FullDocument7 pages1536 FullJosue LayedraNo ratings yet
- ArchRheumatol 32 21Document5 pagesArchRheumatol 32 21indriNo ratings yet
- Goh 2013Document11 pagesGoh 2013Mauliddyah AyuNo ratings yet
- Clinical Presentation of Neuropsychiatric Systemic Lupus Erythematosus and Demographic and Radiological Characteristics of PatientsDocument7 pagesClinical Presentation of Neuropsychiatric Systemic Lupus Erythematosus and Demographic and Radiological Characteristics of Patientsijmp7No ratings yet
- Paediatrica Indonesiana: Lukman Oktadianto, Risky Vitria Prasetyo, Ninik Asmaningsih Soemyarso, Mohammad Sjaifullah NoerDocument6 pagesPaediatrica Indonesiana: Lukman Oktadianto, Risky Vitria Prasetyo, Ninik Asmaningsih Soemyarso, Mohammad Sjaifullah Noerazwin lubisNo ratings yet
- Artigo Base SimoneDocument5 pagesArtigo Base SimoneWolfgang ThyerreNo ratings yet
- Cancer - 2000 - LossosDocument7 pagesCancer - 2000 - LossoslathifatulNo ratings yet
- Contentserver 3Document11 pagesContentserver 3api-278377715No ratings yet
- Neurology2018881847 PDFDocument9 pagesNeurology2018881847 PDFFelipe MNo ratings yet
- Juvenile Lupus Erythematosus: Fourteen Years of Experience: Juvenil Lupus Eritematozus: On Dört Yıllık DeneyimDocument8 pagesJuvenile Lupus Erythematosus: Fourteen Years of Experience: Juvenil Lupus Eritematozus: On Dört Yıllık DeneyimRahman SetiawanNo ratings yet
- Yu 2006Document8 pagesYu 2006Josue LayedraNo ratings yet
- 10 1016@j Semarthrit 2020 12 004Document78 pages10 1016@j Semarthrit 2020 12 004karol castellonNo ratings yet
- 7 Management of Neuropsychiatric Lupus: John G. HanlyDocument23 pages7 Management of Neuropsychiatric Lupus: John G. HanlyNungki TriandariNo ratings yet
- Clinical Predictors and Differential Diagnosis of Posterior Reversible Encephalopathy SyndromeDocument7 pagesClinical Predictors and Differential Diagnosis of Posterior Reversible Encephalopathy SyndromekidNo ratings yet
- P300 in Patients With Epilepsy - The DifDocument241 pagesP300 in Patients With Epilepsy - The DifasasakopNo ratings yet
- A Case of Male Sle: An Unusual PresentationDocument4 pagesA Case of Male Sle: An Unusual PresentationIJAR JOURNALNo ratings yet
- Consensus Paper of The WFSBP Task Force On Biological Markers of Dementia The Role of CSF and Blood Analysis in The Early and Differential DiagnosisDocument17 pagesConsensus Paper of The WFSBP Task Force On Biological Markers of Dementia The Role of CSF and Blood Analysis in The Early and Differential DiagnosisDeepthi Chandra Shekar SuraNo ratings yet
- Short-Term Outcome of Proliferative Lupus Nephritis A Single Center StudyDocument12 pagesShort-Term Outcome of Proliferative Lupus Nephritis A Single Center StudyTJPRC PublicationsNo ratings yet
- 2022 Clinical Features and Risk Factors of Mortality in Patients With Posterior Reversible Encephalopathy SyndromeDocument7 pages2022 Clinical Features and Risk Factors of Mortality in Patients With Posterior Reversible Encephalopathy SyndromeSafitri MuhlisaNo ratings yet
- Encephalitis and Aseptic Meningitis: Short-Term and Long-Term Outcome, Quality of Life and Neuropsychological FunctioningDocument9 pagesEncephalitis and Aseptic Meningitis: Short-Term and Long-Term Outcome, Quality of Life and Neuropsychological FunctioningRoberto SoehartonoNo ratings yet
- Mayoclinproc 85-5-004Document6 pagesMayoclinproc 85-5-004Alain SánchezNo ratings yet
- Correlation of Neutrophil-Lymphocyte Ratio (NLR) With Sofa Score As A Parameter of Organic Dysfunction of Sepsis Patients in ICU Haji Adam Malik (HAM) General Hospital MedanDocument5 pagesCorrelation of Neutrophil-Lymphocyte Ratio (NLR) With Sofa Score As A Parameter of Organic Dysfunction of Sepsis Patients in ICU Haji Adam Malik (HAM) General Hospital MedanInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- FocusDocument9 pagesFocusAdéline NolinNo ratings yet
- Central Pontine and Extrapontine Myelinolysis. A Systematic ReviewDocument8 pagesCentral Pontine and Extrapontine Myelinolysis. A Systematic ReviewFernando Vazquez SSNo ratings yet
- Seizure in SLE PatientDocument7 pagesSeizure in SLE PatientdivisiimunNo ratings yet
- Clinical Predictors of Active LN Development in Children - Evidence From The UK JSLE Cohort StudyDocument9 pagesClinical Predictors of Active LN Development in Children - Evidence From The UK JSLE Cohort StudyDavidAkbarNo ratings yet
- MRI and 2D-CSI MR Spectroscopy of The BrainDocument10 pagesMRI and 2D-CSI MR Spectroscopy of The BrainСергей ЛесорубNo ratings yet
- Status Epilepticus in Adults: A Study From Nigeria: SciencedirectDocument6 pagesStatus Epilepticus in Adults: A Study From Nigeria: SciencedirectLuther ThengNo ratings yet
- Acute Renal Failure in Critically Ill Surgical Patients PDFDocument7 pagesAcute Renal Failure in Critically Ill Surgical Patients PDFRomán Jiménez LópezNo ratings yet
- Rodelo Et Al 2023 Predicting Kidney Outcomes Among Latin American Patients With Lupus Nephritis The Prognostic Value ofDocument13 pagesRodelo Et Al 2023 Predicting Kidney Outcomes Among Latin American Patients With Lupus Nephritis The Prognostic Value ofjose pablo quero reyesNo ratings yet
- No Diabetic Lumbosacral RadiculopathyDocument11 pagesNo Diabetic Lumbosacral RadiculopathyHamza JubranNo ratings yet
- 0004 282X Anp 74 09 0718 PDFDocument5 pages0004 282X Anp 74 09 0718 PDFUtari UbNo ratings yet
- AjjababananaDocument7 pagesAjjababananaNaeny BlegurNo ratings yet
- Hant PDFDocument6 pagesHant PDFRodrigo AriasNo ratings yet
- The Clinical Characteristics of Leukopenia in PatiDocument12 pagesThe Clinical Characteristics of Leukopenia in PatipcovarrubiasNo ratings yet
- The NORSE (New-Onset Refractory Status Epileptic Us) SyndromeDocument4 pagesThe NORSE (New-Onset Refractory Status Epileptic Us) Syndromebenghooi75No ratings yet
- Kocyigit 2012Document8 pagesKocyigit 2012Rengganis PutriNo ratings yet
- Case Series: Neuropsychiatric Symptoms With Pediatric Systemic Lupus ErythematosusDocument4 pagesCase Series: Neuropsychiatric Symptoms With Pediatric Systemic Lupus ErythematosusJosue LayedraNo ratings yet
- Accepted Manuscript: Cellular ImmunologyDocument17 pagesAccepted Manuscript: Cellular ImmunologyGracia Yodianvi Pratiwi2No ratings yet
- 1 s2.0 S1658361211701731 Main PDFDocument11 pages1 s2.0 S1658361211701731 Main PDFMakmur SejatiNo ratings yet
- NIH Public Access: Author ManuscriptDocument13 pagesNIH Public Access: Author ManuscriptSyaiful ArifinNo ratings yet
- Chen 2018Document10 pagesChen 2018Maximiliano MahardhikaNo ratings yet
- Part 2diagnostic of NPH PDFDocument13 pagesPart 2diagnostic of NPH PDFrys239No ratings yet
- Kim 2016Document6 pagesKim 2016Phúc Thịnh TrầnNo ratings yet
- Optimized Combination of Circulating Biomarkers AsDocument8 pagesOptimized Combination of Circulating Biomarkers AsAndreea MoalesNo ratings yet
- Research ArticleDocument9 pagesResearch ArticlemahadianismailnstNo ratings yet
- Correlation Between Cell Free DNA Levels and Medical Evaluation of Disease Progression in Systemic Lupus Erythematosus PatientsDocument8 pagesCorrelation Between Cell Free DNA Levels and Medical Evaluation of Disease Progression in Systemic Lupus Erythematosus PatientsSilvia PeresNo ratings yet
- RJR - 2019 - 3 - Art-02 - CRISTINA GOFITA - CRPS DIAGNOSISDocument8 pagesRJR - 2019 - 3 - Art-02 - CRISTINA GOFITA - CRPS DIAGNOSISmihail.boldeanuNo ratings yet
- AIHA ArticleDocument7 pagesAIHA ArticlegffghNo ratings yet
- 8931 26614 2 PB PDFDocument7 pages8931 26614 2 PB PDFMaferNo ratings yet
- Cei 13095Document6 pagesCei 13095karen rinconNo ratings yet
- NLR Bells PalsyDocument4 pagesNLR Bells PalsyIskandar HasanNo ratings yet
- Vol 54 No 2 Patel Selby YekkiralaDocument5 pagesVol 54 No 2 Patel Selby YekkiralaDrashua AshuaNo ratings yet
- Endothelial Dysfunction and Cardiovascular Risk in Lupus Nephritis New Roles For Old PlayersDocument30 pagesEndothelial Dysfunction and Cardiovascular Risk in Lupus Nephritis New Roles For Old PlayersSilvia PeresNo ratings yet
- Sleep Disturbances and Prevalence of Depression in Systemic Lupus Erythematosus Patients Receiving Intravenous CyclophosphamideDocument5 pagesSleep Disturbances and Prevalence of Depression in Systemic Lupus Erythematosus Patients Receiving Intravenous CyclophosphamidevhiiehoNo ratings yet
- 55421-Gagal JantungDocument21 pages55421-Gagal JantungAngie CouthalooNo ratings yet
- Print 2 PDFDocument6 pagesPrint 2 PDFfk unswagatiNo ratings yet
- Lupus PMCDocument8 pagesLupus PMCTuRatna Say ANo ratings yet
- Neutrophil To Lymphocyte and Platelet To LymphocytDocument7 pagesNeutrophil To Lymphocyte and Platelet To LymphocytpriyaNo ratings yet
- Tingkat Kepatuhan Antihipertensi Dan Pengontrolan Tekanan Darah Pasien Rawat Jalan Rs Pku Muhammadiyah BantulDocument6 pagesTingkat Kepatuhan Antihipertensi Dan Pengontrolan Tekanan Darah Pasien Rawat Jalan Rs Pku Muhammadiyah BantulRusnaneeNo ratings yet
- Hepatitis ADocument11 pagesHepatitis AIGA ABRAHAMNo ratings yet
- Respiratory Best RDocument5 pagesRespiratory Best RfrabziNo ratings yet
- FCP (023) Accessing Evidence That MattersDocument20 pagesFCP (023) Accessing Evidence That MattersKerolusMouradNo ratings yet
- Microbial Mechanisms of Pathogenicity - An OverviewDocument23 pagesMicrobial Mechanisms of Pathogenicity - An OverviewVDP GamezNo ratings yet
- SteatorrheaDocument43 pagesSteatorrheaJohnRobynDiezNo ratings yet
- REVISI (Adelita Setiawan 2)Document7 pagesREVISI (Adelita Setiawan 2)Adelita SetiawanNo ratings yet
- Gerson - The Little Enema BookDocument36 pagesGerson - The Little Enema BookBruno GonçalvesNo ratings yet
- Slle Examination Content Guideline - March 05 PDFDocument16 pagesSlle Examination Content Guideline - March 05 PDFYahya Alkamali100% (1)
- Inside The Human BodyDocument1 pageInside The Human BodyKaravanNo ratings yet
- Daftar Sampel ReadyDocument6 pagesDaftar Sampel ReadydindaNo ratings yet
- The Biotherapics Influenzinum and Oscilococcinum in The Treatment of Influenza Virus FluDocument1 pageThe Biotherapics Influenzinum and Oscilococcinum in The Treatment of Influenza Virus Fluweb3351No ratings yet
- Tips For Staying Hydrated During SummerDocument3 pagesTips For Staying Hydrated During SummervasuNo ratings yet
- Assessment Tool For Level 1 Hospital Annex K1 PDFDocument47 pagesAssessment Tool For Level 1 Hospital Annex K1 PDFMadelyn LamanilaoNo ratings yet
- Asge Primer 2017 Pgs117 125 Single PageDocument9 pagesAsge Primer 2017 Pgs117 125 Single PageMani KandanNo ratings yet
- Satuan Kegiatan Prestasi Mahasiswa (SKPM) Fakultas Ilmu Kesehatan Universitas NasionalDocument1 pageSatuan Kegiatan Prestasi Mahasiswa (SKPM) Fakultas Ilmu Kesehatan Universitas NasionalAnonymous DErS9RMmrENo ratings yet
- Do Not Resuscitate: Words Used in The EMS DNR Order Act and FormDocument2 pagesDo Not Resuscitate: Words Used in The EMS DNR Order Act and FormSteven EtheredgeNo ratings yet
- PRELIMINARY ACTIVITY of Module 1Document3 pagesPRELIMINARY ACTIVITY of Module 1Casio, Anthony MaryNo ratings yet
- Vitamin B6 Deficiency As A Cause of Polyneuropathy in POEMS Syndrome Rapid Recovery With Supplementation in Two CasesDocument7 pagesVitamin B6 Deficiency As A Cause of Polyneuropathy in POEMS Syndrome Rapid Recovery With Supplementation in Two CasesYaseen MohamnadNo ratings yet
- Glaukoma - PPTX KoassDocument38 pagesGlaukoma - PPTX Koassdhita01No ratings yet
- KDIGO 2023 Lupus Nephritis Guideline - Public Review - 9 Mar 2023 PDFDocument102 pagesKDIGO 2023 Lupus Nephritis Guideline - Public Review - 9 Mar 2023 PDFlucasnatalia21bNo ratings yet
- PPR - LISTS - Registered Medicine Price List - 20211230Document333 pagesPPR - LISTS - Registered Medicine Price List - 20211230Abdulla KamalNo ratings yet
- Kim Resume PDFDocument1 pageKim Resume PDFapi-548816548No ratings yet
- pedCAT BrochureDocument12 pagespedCAT BrochureVinti Singh100% (1)
- Mispa Count Plus 1Document2 pagesMispa Count Plus 1Tony DanartoNo ratings yet
- Glossary and Acronyms of FreedivingDocument2 pagesGlossary and Acronyms of FreedivingIvo XNo ratings yet
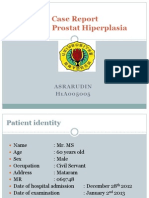
- Lapsus - Asrarudin - BPHDocument18 pagesLapsus - Asrarudin - BPHAsrarudin HamidNo ratings yet
- NCP CalculiDocument8 pagesNCP CalculihailleyannNo ratings yet
- Morning Report Obs FebrisDocument10 pagesMorning Report Obs FebrisJessicaNo ratings yet
- Case Study 2Document37 pagesCase Study 2api-391842100No ratings yet