Professional Documents
Culture Documents
Bioethics Final
Uploaded by
Keanu Win Catipay0 ratings0% found this document useful (0 votes)
13 views9 pages1. The document discusses various end-of-life medical topics including abortion, surrogacy, euthanasia, life support, and advance directives.
2. It outlines different types of abortion and surrogacy arrangements, as well as considerations around when abortion may be morally acceptable and the potential issues with surrogacy.
3. Key aspects of end-of-life care are explained, including withholding and withdrawing life support, palliative care, and the difference between ordinary and extraordinary care treatments. The document also discusses euthanasia and assisted suicide.
Original Description:
Reviewer
Original Title
Bioethics-Final
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document1. The document discusses various end-of-life medical topics including abortion, surrogacy, euthanasia, life support, and advance directives.
2. It outlines different types of abortion and surrogacy arrangements, as well as considerations around when abortion may be morally acceptable and the potential issues with surrogacy.
3. Key aspects of end-of-life care are explained, including withholding and withdrawing life support, palliative care, and the difference between ordinary and extraordinary care treatments. The document also discusses euthanasia and assisted suicide.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
13 views9 pagesBioethics Final
Uploaded by
Keanu Win Catipay1. The document discusses various end-of-life medical topics including abortion, surrogacy, euthanasia, life support, and advance directives.
2. It outlines different types of abortion and surrogacy arrangements, as well as considerations around when abortion may be morally acceptable and the potential issues with surrogacy.
3. Key aspects of end-of-life care are explained, including withholding and withdrawing life support, palliative care, and the difference between ordinary and extraordinary care treatments. The document also discusses euthanasia and assisted suicide.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 9
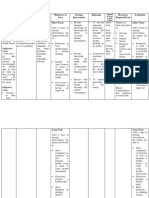
Week 8 - Procreative aspect (people playing
Abortion as God) (iniisip ng tao na kaya
- Premature termination of a nilang bumuhay ng tao)
pregnancy. - Ginagawang business
- Expulsion of non-viable fetus
Types of Abortion Surrogacy
1. Natural/Spontaneous/ Accidental - Carrying pregnancy for intended
Abortion parents
- Removal through accidental Surrogate - substitute or deputy for another
causes. person in specific role
2. Direct/Intentional Abortion
- Planned removal before it Types of Surrogacy
has become viable / survived Gestational Surrogacy
3. Therapeutic Abortion - The child is not biologically
- Removal of fetus in order to related to surrogate mother
save mother from death - Also called host surrogacy
4. Eugenic/ Selective/ Abortion on /full surrogacy
Fetal Indication Pros: - Same sex marriage
- Discovered that the fetus has - Maintain a genetic link to their child
anatomical defects & can’t - Create a meaningful relationship
lived once delivered. with their surrogate
5. Indirect Abortion Cons: - generally a legally complex & costly
- Fetus will be removed as a process
secondary effect of the - Requires intended parents to
procedure done to save the abandon some control as someone
mother's life. else carries the pregnancy
- If the proposed mother is using
When is abortion become morally right? her own eggs in the surrogacy
1. Always MORALLY WRONG - kase process, she will have to undergo
nagteterminate ka ng life fertility treatments and other
medical procedures.
Artificial Insemination by Husband (AIH) 2. Traditional surrogacy - The
- Sa husband mismo galing yung surrogate mother uses her own
sperm egg and is artificially inseminated
Artificial Insemination by donor (AID) using sperm from the intended
- Same as that of AIH except that the father or a donor.
sperm donor is used instead of the - Also known as partial
husband. surrogacy/ genetic surrogacy
What is Morally Wrong in Artificial
Insemination? Pros: - usually less expensive
- it damages the correct term/ - Intended mothers do not need to
prescribe use of marriage undergo medical procedures (eggs
- No unitive aspect of husband & wife will not be harvested).
Cons: - A traditional surrogate has parental
rights and the power to change her ● Cardiopulmonary resuscitation
mind and keep the baby. The (CPR)
intended parents would then need - Used to reverse clinical sign
to go to court to gain custody of of death
the child. - Revive
- Loss of cardiac function
2 types of surrogacy arrangements - Some pt don’t want to
1. Altruistic Surrogacy resuscitate
2. Commercial Surrogacy When to stop CPR?
- Futile/ Hopeless
Ethical Issues - More than 30 mins (adult) 15 mins
● Ginawang negosyo (pataasan ng (newborn)
binding) - Advance directives/ Living will
● Male can distribute as many, hindi Life support - our body is a complex
mo alam yung magiging partner mo, machine
kapatid mo pala (incestous) - Lungs
- Heart
To minimize this issue, we need to - Brain
considered our ethical principle Withholding Life support
- Refers to never initiating treatment
Week 9 - Advance directives/ living will
Withhold and Withdraw Life Support - Decision of relatives
- Is withholding life support is
Withholding - hawak mo lang, hindi mo euthanasia? (case to case basis)
ibibigay
- Not to give it at nall Palliative Care - given in geriatric home
Withdrawing - Stop what is already given ● Counseling - providing emotional
support (need ng kausap)
Life Sustaining treatment ● Education - to understand the
● Ordinary Care - Basic Treatment course of disease
- help to prolong the pt life ● Assure pt of safety management
- Must be provided as much as ● Mental diversion, music/ play
possible therapy
Example: IVF, NGT feeding, oxygen, ● Manage expected/ common
quality of daily living complications
● Physical exercise & proper physical
● Extraordinary Care - Invasive movements (walking)
Treatment ● Pharmacologic management
- Present gadgets/ medicines -Multimodal analgesia
are no longer for further use -Relieve pain w/ opioids
due to futility.
Example : Craniotomy , CPR, Experimental
Treatment, Ventilator, dialysis
Euthanasia - “eu” means good, well, nice &
merciful (mercy killing but it’s not mercy, Advance Directives -
killing lang) Advance - Before a thing happens
- “Thanatos” ,=means death/ killing Directives - steps that are to be taken
- Act or practice of ending a life - Legal document in which a person
- Morally wrong bc it damages the specifies what actions should be
sacredness/ sanctity of life (immoral) taken for their health if they are no
(nawawala yung natural end) longer able to make decisions for
themselves
Types of Euthanasia - Written legally recognized
1. Active Euthanasia (Commission) documents that state your choices
- Death is brought by an act about health care treatment
- Example : taking a high dose Purpose:
of drugs, lethal injection. - Appointment of health care proxy
- (Suicide) (Kung sino ang mananagot sa
- Pt can be conscious/ pasyente)
unconscious
2. Passive Euthanasia (Omission) Types of Advance Directive
- Death brought by omission 1. Living will (Health care
- Example: when someone lets directives)
the person die 2. Restricted Directive (in health
- Can be done by withdrawing/ aspect) (estate is not
withholding treatment included) (walang gagalaw
(decided by ethical nyan)
committee) 3. Decision abt life sustaining
procedure in the event the pt
Assisted Suicide is in impending doom (yung
- Physician assisted suicide hindi na kaya mag decide for
- Doctor knowingly helps someone himself)
end their life
- Person likely experiencing Week 10 & 11
persistent/ unending suffering. Moral Responsibility of Nurse
Euthanasia to advance
Issue of Euthanasia directive (Same sa ppt)
● Religious Beliefs & morality
ETHICAL DECISION MAKING PROCESS
● Christianity
● Islam - In ethical decision, we always
● Shinto choose what is right and what is
● judaism good but if dalawa yung good, dun
● Not legal in PH papasok yung ethical decision
● Nurse is obligated to assist in making
passive euthanasia
Problem Analysis
Problem - is a discrepancy between
situation & desired state
Moral uncertainty - when we sense that may gentleness & accuracy)
there is moral problem but we are unsure of 34. Empowerment - you give power to the
the morally correct action (the one that person to decide ( ang magdedecide lagi ay
moves toward what is right & good)
Moral/ ethical dilemma - requires a choice Principles of Ethics and Research
between two option that are equally
unfavorable & mutually exclusive ● Nuremberg code of 1947
- formulated 50 years ago, in august 1947 in
Pattern of decision making Numberg Germany by American judges
sitting in judgement of Nazi doctors accused
1. Recognizing a problem of conducting murderous and torturous
2. Gathering data human experiments in the concentration
3. Comparing options/action implies camps (the so -called Doctors Trial).
uncertainty – list of options (kinukuha mga prisoners for trials at bawal
4. Making a choice/implemented decision silang
tumanggi)
Nursing Process and Ethical Decision • Ethics principles for human
Making experimentation resulting
from Nazi
1. Ethical decision-making models are • Focus on human rights and welfare
related to nursing care in
the ethical realm in the same way that the 10 Elements of The Numberg Code
nursing process is
related to nursing care in the physical realm. 1. Voluntary informed consent (top priority)
(based o autonomy)
2. As nurses we commonly use the nursing 2. Fruitful result for the good of the society
process model for (based on theoretical theorist)
decision making. 3. Prior on animals & prior knowledge the
problems
3. Utilizing logical thinking and intuitive 4.Avoidance of unnecessary physical/
knowing, the nursing mental injury (go back to ethical principle
process is a deliberate activity that provides nonmaleficence)
a systematic 5. Banning of known lethal/ disable
method for nursing practice procedures
6. Degree of risk should not exceed limit
Attributes of an Effective Ethical (benefit is the top priority)
Decision Maker 7. Proper preparation & proper facilities to
prevent injury or death (nonmaleficence)
1. Moral integrity – binds all of a person’s 8. Performance of experiments only by
moral virtues into a coherent package it scientifically qualified persons. (perform a
creates a wholeness and stability of task w/ minimal risk)
character that leads to trustworthiness. 9. Participants may freely end the
- rightness of an act experimentation (based on autonomy)
(kabuuan ng buong 10. The experiment must stop if it proves
opag katao mo at walang pwedeng too dangerous (nonmaleficence)
makasira nito dahil nabuo
na ‘to simula nung pag ka bata mo) Declaration of Helsinki (pertains to the
2. Compassion- delivered in a degree that person who will conduct research )
it will not be abused (kapag naabuse, it’s - Statement of ethical principles for medical
not compassion) research involving human participants,
3. Caring - Related to compassion (dapat including identifiable human material and
data; doctors doing medical research on Research Ethics Committees
patients (basis for • Transparent, independent, and qualified
good clinical practice) • Follow norms
• For all involved in medical research • Approve protocol
• Basis for Good Clinical Practice (GCP) • Monitor study, approve amendments, and
General Principles receive final report
• Purpose: understand disease, improve Privacy And Confidentiality – protect the
interventions (like covid vaccines) privacy of research
• Human participants necessary subjects (hindi identified ung taong
• Primacy of patient’s best interest: health, kukuhanin mo)
well-being, rights
• Duty and responsibility of researcher even Informed Consent – for capable: voluntary,
if with consent of participants (treat subject informed. For not
properly) capable: legally authorized representative;
• Subject to ethical standards: International
and national guidelines cannot reduce Belmont Report 1976 (all about the use
Helsinki of human subjects)
• Respect and protect participants 1. Respect for person: protecting the
• Minimize harm to environment autonomy of all people & treating
• Qualified researcher them w/ courtesy & respect &
• Fair access to research allowing for informed consent
2. Beneficence: the philosophy of “do
Risks, Burdens, and Benefits no harm”, while maximizing the
benefits for the research project
• Pre-assess then monitor (based on nonmaleficence)
• Importance of objectives outweigh R/B for 3. Justice: ensuring reasonable,
participants.Benefits outweigh risks for non-exploitative, & well- considered
participants and groups affected and procedures (administered fairly)
managed
• Measures to minimize implemented Ethical Issues Related to Evidenced
• Once risks outweigh the benefits or if there Based Practice
is already a clear outcome: assess if - Evidence-based practice is a systematic
research should be continued interconnecting scientifically generated
evidence with the tacit knowledge of the
Vulnerable Groups and Individuals expert practitioner
• Increased likelihood of wrong and harm – Ethical issues involved in EBP
Special protection (underaged, preg, elders, 1. Status of evidence
poor) 2. Client Autonomy
• Responsive to their health needs 3. Conflict of interest
• Cannot be done on non-vulnerable
• Stand to benefit from result Ethico-Moral Obligations of The Nurse In
Evidence-Based Practices
Scientific Requirements and Research
Protocols 1. Golden Rule
• Conform to accepted scientific principles 2. The principle of Totality – The whole is
• Respect animals greater than its parts
• Complete protocol including addressed 3. Epikia – There is always an exemption to
ethical considerations the rule
• Post-trial provisions indicated 4. One who acts through as agent is herself
responsible – instrument to the crime, 2. Timeliness Refers to completion of health
accessory or accomplice care notes immediately within time specific
5. No one is obliged to betray herself – You care
cannot betray yourself 3. Use of Space Empty lines or spaces are
6. The end doesn't justify the means avoided to prevent late-entry of data.
7. Defects of nature may be corrected (hindi 4. Use of Abbreviations Abbreviations or
lahat papalitan mo) acronyms that are
8. If one is willing to cooperate in the act, no internationally/institutionally accepted
justice is done to him. 5. Follow-up All follow-up activities related
9. A little more or a little less does not to client care
change the substance of an act. 6. Correcting Errors In isolated cases when
10. No one is held to impossible () errors in documentation are committed it is
advised that the SLIDE rule (Baker, 2000)
Guidelines and Protocol in be utilized
Documentation and Health Care Records 7. Recording Medication Administration
Administration of medications are
The NCCS Documentation Standard immediately documented after
- Documents are permanent legal records administration
that provide a comprehensive sequential 8. Recording Assistance with Care There
description of relevant facts, data, and are numerous circumstances that one nurse
information about the patient’s health status. is assisted by another nurse in performing a
- Documentation of nursing actions done to specific nursing intervention
a patient is critical to determine if the 9. Designated Recorder in Emergency
expected standard of care was rendered to Situations During emergency situations
a particular patient. there must be a designated recorder
10. Clarification of Orders Medical orders
Importance of documentation that are poorly written require nurses to call
1. Facilitates interdisciplinary the writer for clarification.
communication 11. Recording a Telephone Conversation
2. Coordinates care with a Client Telephone conversation with a
3. Provides information client does not give the nurse the benefit
4. Serves as bases for reimbursement of verifying objective findings
5. Reflects quality and timeliness of nursing 12. Interactions with other Health-care
care Professionals It is the responsibility of the
6. Is utilized as legal document during nurse when formulating nursing care
permissible courtroom plans to include outcomes
13. Client Education Educational
Characteristics Of Good Documentation interventions and related health
1. Factual teachings that provide comprehensive
2. Complete information to clients must be documented
3. Current (Timely) 14. Documenting an Incident in the
4. Organized Health-care Record It is
5. Compliant with standards imperative that all incidents that occured
6. Accurate with its corresponding pertinent data are
documented in the client’s health record.
Guidelines In Documentation
ETHICAL CONSIDERATION IN
1. Objective/Factual Documentation Direct LEADERSHIP MANAGEMENT
observations and objective descriptions of - Accdg to Birkholz, Moral Decision
interventions rendered to clients are making is imperative to arrive at an
recorded. ethical action/ intervention.
Moral Decision – Making 5. Principle of Well-formed
Conscience
• Right -To attain true goals of human life by
• Wring responsible actions, in every free decisions
• Forbidden involving an ethical question, people are
• Duty morally obliged to do the following:
• Good - the act by which we apply to our own
• Corrupt - be aware of facts & ethical norms
- refers to the ability to discern what is -Having a morally certain judgement of
morally right from conscience
morally wrong that requires moral -Act accordingly to this well formed
reflectiveness on the meaning of good and conscience
bad, Olson (2002) -Accept responsibility for our actions
- It refers to the ability to draw conclusions -Informed consent to medical treatment
from the discernment to develop -Patients have the right to receive
convictions. information and ask questions about
- discernment – wisdom, clarification, study recommended treatments so that they can
the facts. make well-considered decisions about care.
- Moral – is a discernment wherein
deliberating the issue existing hindi ka lang Ethical Dilemma
basta basta umoo or nag a-agree pero - is a problem in the decision-making
kinikilatis mo sya process between two possible options,
neither of which is absolutely acceptable
Four Principles of Moral from an ethical perspective;
Discernment/Judgment - Ex. thief. Bakit ang mga magnanakaw
hindi nahuhuli? Edi yung dilemma mo
1. Principle of Formal Cooperation naman is “ay ok lang naman pala mag
- it occurs when someone intentionally helps nakaw eh kase sila hindi nga nahuhuli, edi
another person carry out a sinful act. (sino ako din magnanakaw nalang” (mga teh wag
yung nag isip na gumawa ng mali) nyo gagawin yun ah?
2. Principle of Material Cooperation kahit kapit na tayo sa patalim
- when a person's actions unintentionally HAHAHAHAHA)
help another person do something wrong.
(nag contribute/ nadamay) Process of Ethical Decision Making
3. Principle of Lesser Evil 1) Gather data and identify conflicting moral
- The principle that when faced with claims (Cerebral Activity)
selecting from two immoral options, the one 2) Identify key participants ( wag isali ang
which is least immoral should be chosen. mga dapat hindi na kasali. Focus on who
(The gravity, the impact. Kahit maliit na will receive the big impact)
aksyon even less or great evil kapag nag 3) Determine moral perspective and phase
participate ka evil pa din) of moral development
4. Principle of Double Effect of key participants – (who is really involved)
- This principle aims to provide specific 4) Determine desired outcomes
guidelines for determining when it is morally (something right & good for pt)
permissible to perform an action in pursuit 5) Identify options (alternatives)
of a good end in full knowledge that the 6) Act on the choice
action will also bring about bad results. (in 7) Evaluate outcomes of actions
doing something good, the bad is
spontaneously occurs)
MEANING AND SERVICE VALUE OF
MEDICAL CARE ETHICAL ISSUES RELATED TO
• Cost-effective TECHNOLOGY IN THE DELIVERY OF
1. Allocation of Health Resources HEALTHCARE
- limited resources for health should
be allocated to maximize the health Benefits & Challenges of Technology
benefits for the population served 1. Reducing Healthcare Costs
- Quantitative ka pero quality ang nakuha 2. Predicting Epidemics
mo 3. Improving quality of life/quality care
- Sa konting gastos makakuha ka ng 4. Reducing Healthcare Waste
benefits 5. Improving Mobility/Access
- Equity means giving more to the person 6. Developing New Drugs and
who needed the most. Treatments (vaccine)
- Costs are measured in monetary terms; 7. Security E.G. Data Hacking/Phishing
benefits are measured 8. Volume of Data In Icloud
in health improvements.- Cost-effectiveness 9. Dangers with AI central data point
is not merely an economic concern, 10. Impersonal patient-healthcare
because improving people's health and provider relationship (nawawala
well-being is a moral concern, and an yung tender loving care)
allocation of resources that is not cost- 11. Connectivity & Cost
effective produces fewer benefits than 12. Fast & numerous changes
would have been possible with a different
allocation Current Technology: Issues & Dilemma
- Security
2. Equity (Give to the one who needs it - Portability
the most ) - Cost
- is concerned with the distribution of - Real-time events (can it really br
benefits and costs to distinct individuals or done)
groups. - Equity (provided for those pt who
- Equity in health care distribution is need the most)
complex and embodies several distinct - Justice
moral concerns or issues that this chapter
delineates (Brock 2003a) CONTINUING EDUCATION PROGRAM ON
ETHICO- MORAL PRACTICE IN NURSING
Issues involving access to care
Lobbying- The act or process influencing
1) Access to Quality Care ( Patients want to public officials to promote something /
be able to access their healthcare when secure the passage of legislation
they want and need it)
2) Geographic and Manpower Shortage Advocacy - the act or process of promoting
3) Limited education a cause or proposal
4) Poor infrastructures
5) Cost (kahit walang babayaran sa hospital Code of Ethics for nurses
pero yung mga cost sa byahe, pagkain
ganun) 1. Article 2 - Registered Nurse &
6) Scientific evidence vs Cultural Practice People
Ethical Principle
a. Values, customs, & spiritual beliefs
held by individuals shall be
respected
b. Individual freedom to make rational
& unconstrained decisions shall be international efforts to meet
respected (Principle of Autonomy) health and social needs of the people as a
c. Personal information acquired in the contributing member of society is a noble
process of giving nursing care shall concern of a Registered Nurse.
be held in strict confidence.
(Principle of Confidentiality) Article VI. Registered Nurses and the
Profession
Article II. Registered Nurses and People 1. Maintenance of loyalty to the nursing
1. Values, customs, and spiritual beliefs profession and preservation of its integrity
held by individuals shall be respected. are ideal.
2. Individual freedom to make rational and 2. Compliance with the by-laws of the
unconstrained decisions shall be respected. accredited professional organization
3. Personal information acquired in the (PNA),and other professional
process of giving nursing care shall be held organizations of which the Registered Nurse
in strict confidence. is a member, is a lofty duty.
3. Commitment to continual learning and
Article III. Registered Nurses and active participation
Practice in the development and growth of the
1. Human life is inviolable. profession are commendable obligations.
2. Quality and excellence in the care of the 4. Contribution to the improvement of the
patients are the goals of nursing practice. socio-economic conditions and general
3. Accurate documentation of actions and welfare of nurses through
outcomes of delivered care is the hallmark appropriate legislation is a practice and a
of nursing accountability. visionary mission.
4. Registered Nurses are the advocates of
the patients: they shall take appropriate Article VII. Administrative Penalties,
steps to safeguard their rights and Repealing Clause and Effectivity
privileges. 1. The Certification and Registration of the
5. Registered Nurses are aware that their Registered Nurse shall either be revoked or
actions have professional, ethical, moral, suspended for violation of any provisions of
and legal dimensions. They strive to this Code.
perform their work in the best interest of all
concerned.
Article IV. Registered Nurses and
Co-workers
1. The Registered Nurse is in solidarity with
other members of the healthcare team in
working for the patient’s best interest.
2. The Registered Nurse maintains collegial
and collaborative working relationship with
colleagues and other health care providers
Article V. Registered Nurses, Society,
and Environment
1. The preservation of life, respect for
human rights, and promotion of healthy
environment shall be a commitment
of a Registered Nurse.
2. The establishment of linkages with the
public in promoting local, national, and
You might also like
- Geron 3FDocument5 pagesGeron 3FJeann sumbillaNo ratings yet
- BIOETHICSDocument4 pagesBIOETHICSMutya XDNo ratings yet
- Resource Unit SampleDocument16 pagesResource Unit SampleShania CabucosNo ratings yet
- Bioethics FinalsDocument5 pagesBioethics FinalsRenalyn Dela cruzNo ratings yet
- Bioethics NOTES 108 - Week 2Document6 pagesBioethics NOTES 108 - Week 2ArmySapphireNo ratings yet
- Ncmhce108 Endterm NotesDocument3 pagesNcmhce108 Endterm NotesNicole GutierrezNo ratings yet
- I BelieveDocument4 pagesI Believeapi-306698224No ratings yet
- MarriageDocument2 pagesMarriageAnntel RoseNo ratings yet
- Psych - ArcDocument4 pagesPsych - ArcMae PenaredondoNo ratings yet
- Medical Law WordDocument6 pagesMedical Law Wordarezoo bahramiNo ratings yet
- Nursing Assessment IIDocument5 pagesNursing Assessment IImyer pasandalanNo ratings yet
- Ncma218: BSN 2Nd Year Summer Midterm 2022: Bachelor of Science in Nursing 2YCDocument16 pagesNcma218: BSN 2Nd Year Summer Midterm 2022: Bachelor of Science in Nursing 2YCChesca DomingoNo ratings yet
- Midterm QuizDocument2 pagesMidterm QuizChariza MayNo ratings yet
- Moral Issues of Birth DeformitiesDocument3 pagesMoral Issues of Birth DeformitiesPham PhamIoNo ratings yet
- Mapeh Reviewer Q1Document2 pagesMapeh Reviewer Q1spawnn NVX7No ratings yet
- MMM Exam 3 Extended PacketDocument7 pagesMMM Exam 3 Extended PacketMakenzie LyonNo ratings yet
- Dignity in Death and Dying 2nd Topic Bio FinalsDocument53 pagesDignity in Death and Dying 2nd Topic Bio Finalsjanmishelle208No ratings yet
- BioethicsDocument2 pagesBioethicsRitik DhageNo ratings yet
- Biomedical EthicsDocument16 pagesBiomedical Ethicssarah.sardonNo ratings yet
- Ethical PrincipleDocument8 pagesEthical PrinciplepetalcorinaltheaNo ratings yet
- Issues in ContraceptionDocument48 pagesIssues in ContraceptionAnne Mel BariquitNo ratings yet
- Longevity with Healthy, Vibrant Energy for Life!: Syncing Heart Intelligence, Brain Willpower, and Divine SelfFrom EverandLongevity with Healthy, Vibrant Energy for Life!: Syncing Heart Intelligence, Brain Willpower, and Divine SelfNo ratings yet
- Psychology: General Psychology Instructor: Mrs. Mary Ann B. BautistaDocument3 pagesPsychology: General Psychology Instructor: Mrs. Mary Ann B. BautistaSherly Mae Delarosa DionelaNo ratings yet
- Medical Ethics: Principle of ConfidentialityDocument3 pagesMedical Ethics: Principle of ConfidentialityyayayanizaNo ratings yet
- ethics 2 - نسخةDocument4 pagesethics 2 - نسخةYousef KhalifaNo ratings yet
- Euthanasia & Function of CCH FMT Date-1st April 2022Document5 pagesEuthanasia & Function of CCH FMT Date-1st April 2022C2c C2cNo ratings yet
- Simply Told - Kenneth S. Jaffrey REVISED by Jonas SunshineDocument34 pagesSimply Told - Kenneth S. Jaffrey REVISED by Jonas SunshineJonas Sunshine CallewaertNo ratings yet
- IsyuDocument30 pagesIsyuChristy JopiaNo ratings yet
- PrinciplesDocument2 pagesPrinciplesShehada Marcos BondadNo ratings yet
- Fetal Medicine 1. 2. Set Agenda / Purpose of Consultation 3. History (Relevant) - Check GestationDocument12 pagesFetal Medicine 1. 2. Set Agenda / Purpose of Consultation 3. History (Relevant) - Check GestationfouziatariqNo ratings yet
- Healing Through Awareness and RecallDocument91 pagesHealing Through Awareness and RecallHeka Astro Tarot100% (1)
- 10 Harmful Myths That Prevent Us From Being Healthy & Fully Alive!From Everand10 Harmful Myths That Prevent Us From Being Healthy & Fully Alive!No ratings yet
- 4 What Is Nature CureDocument35 pages4 What Is Nature CureAnonymous fO8xe7rMyANo ratings yet
- NSTP Reviewer 1Document8 pagesNSTP Reviewer 1Andrea MaderaNo ratings yet
- JSJ Self Help Guide PDFDocument27 pagesJSJ Self Help Guide PDFhernan letelier marinNo ratings yet
- Assessment (Subjective / Objective Data) Nursing Diagnosis Planning Interventions RationaleDocument2 pagesAssessment (Subjective / Objective Data) Nursing Diagnosis Planning Interventions RationaleMaria Lourdes CruzNo ratings yet
- Ethics (Online Activity) : MACAHILOS, Patricia MaeDocument3 pagesEthics (Online Activity) : MACAHILOS, Patricia MaePatricia Mae MacahilosNo ratings yet
- ATI END COMP ReviewDocument19 pagesATI END COMP ReviewTori Roland100% (1)
- ATI 4th Quarter Review - Judith Miller VideosDocument19 pagesATI 4th Quarter Review - Judith Miller VideosTori RolandNo ratings yet
- Untreated Trauma: The Signs, Sources and Science: Video 2 WorksheetDocument6 pagesUntreated Trauma: The Signs, Sources and Science: Video 2 Worksheetemdiesus100% (1)
- Renaud Acim Dallas 2014Document91 pagesRenaud Acim Dallas 2014Meral Şevik Çağlayan100% (6)
- Unit 1 NOTESDocument11 pagesUnit 1 NOTESgrad_nurse_2015No ratings yet
- American Site Draft in Large FontDocument37 pagesAmerican Site Draft in Large Fontmusa1976No ratings yet
- By: Christine G. Dela CruzDocument34 pagesBy: Christine G. Dela CruzMuhammad AbeeshNo ratings yet
- NAME: Cañete, Princess Laira V. BSN 3-YB-18Document1 pageNAME: Cañete, Princess Laira V. BSN 3-YB-18Laira CañeteNo ratings yet
- Semifinal Ethics Real 14Document136 pagesSemifinal Ethics Real 14musa.juhanyNo ratings yet
- EuthanesiaDocument58 pagesEuthanesiatarshaNo ratings yet
- 5 Tell Me SimplyDocument30 pages5 Tell Me SimplyAnonymous fO8xe7rMyANo ratings yet
- Pe ReviewerDocument3 pagesPe ReviewerjenideealinsunurinNo ratings yet
- Religion ReviewDocument5 pagesReligion ReviewWilliam BorgesonNo ratings yet
- Magna YeDocument3 pagesMagna YeDiane Ronalene Cullado MagnayeNo ratings yet
- AbortionDocument2 pagesAbortiond8xz5c8tftNo ratings yet
- TFN ReviewDocument7 pagesTFN ReviewJezzabel Kyra BadayosNo ratings yet
- Community Health NursingDocument4 pagesCommunity Health NursingAbmil Ching TinggalongNo ratings yet
- Summary Guide: Dr. Gundry's Diet Evolution: Turn Off the Genes That Are Killing You and Your Waistline by Dr. Steven Gundry | The Mindset Warrior Summary Guide: (Weight Loss, Anti-Aging & Longevity, Anti-Inflammatory Diet)From EverandSummary Guide: Dr. Gundry's Diet Evolution: Turn Off the Genes That Are Killing You and Your Waistline by Dr. Steven Gundry | The Mindset Warrior Summary Guide: (Weight Loss, Anti-Aging & Longevity, Anti-Inflammatory Diet)No ratings yet
- Roper Logan TierneyDocument26 pagesRoper Logan TierneyBerylle TibunsayNo ratings yet
- Febrile Seizures Epilepsy OSCE Counselling PaediatricsDocument6 pagesFebrile Seizures Epilepsy OSCE Counselling PaediatricsJJ Lim100% (1)
- PERITONEALDocument4 pagesPERITONEALKeanu Win CatipayNo ratings yet
- Course Task 2 Application of Bioethical Principles 1Document3 pagesCourse Task 2 Application of Bioethical Principles 1Keanu Win CatipayNo ratings yet
- Cu 10Document1 pageCu 10Keanu Win CatipayNo ratings yet
- FNCP Alcohol DrinkingDocument2 pagesFNCP Alcohol DrinkingKeanu Win CatipayNo ratings yet
- NCMB 210 - Course Task 1.0Document3 pagesNCMB 210 - Course Task 1.0Keanu Win CatipayNo ratings yet
- NCMB 210 - Course Task 1.0Document2 pagesNCMB 210 - Course Task 1.0Keanu Win CatipayNo ratings yet
- D2 FC Mnchan 1Document24 pagesD2 FC Mnchan 1Keanu Win CatipayNo ratings yet
- Newborn Screening StudentDocument39 pagesNewborn Screening StudentKeanu Win CatipayNo ratings yet
- Date Sunday, April 14, 2019 Date: Sha'ban 9, 1440Document7 pagesDate Sunday, April 14, 2019 Date: Sha'ban 9, 1440Ahmad SaadNo ratings yet
- CIOB Membership RegulationsDocument9 pagesCIOB Membership RegulationskasunNo ratings yet
- Untitled 1.odtDocument8 pagesUntitled 1.odtPradyuman SiyalNo ratings yet
- Business LetterDocument4 pagesBusiness LetterEli Abram Dini-ay CabilinNo ratings yet
- Test For Nutrients in FoodsDocument2 pagesTest For Nutrients in FoodsAdrian Alvinson NazarenoNo ratings yet
- Book Review Assignment Book: The Da Vinci Code Group Members: Sadia Jabeen World LiteratureDocument5 pagesBook Review Assignment Book: The Da Vinci Code Group Members: Sadia Jabeen World LiteratureZone MusicNo ratings yet
- Davao Sawmill v. CastilloDocument1 pageDavao Sawmill v. CastilloJulie AnnNo ratings yet
- Why Parents Should Avoid Telling Their Children Fairy Tales SlidesDocument21 pagesWhy Parents Should Avoid Telling Their Children Fairy Tales SlidesGebriellaNo ratings yet
- Research Across FieldsDocument2 pagesResearch Across FieldsBea Dacillo BautistaNo ratings yet
- Sree Padmanabha Swamy Temple Judgment July 13, 2020Document218 pagesSree Padmanabha Swamy Temple Judgment July 13, 2020PGurusNo ratings yet
- 2023 35777 001Document53 pages2023 35777 001Paula Manalo-SuliguinNo ratings yet
- Distance Learning BrochureDocument8 pagesDistance Learning BrochurecaphilNo ratings yet
- The OS/2 Debugging Handbook - Volume I Basic Skills and Diagnostic TechniquesDocument388 pagesThe OS/2 Debugging Handbook - Volume I Basic Skills and Diagnostic TechniquesMichael GreeneNo ratings yet
- Kit InsertDocument8 pagesKit InsertMuhammad HamzarNo ratings yet
- Material For BTS3900&BTS5900 Node Performance Counter Changes (V100R015C10SPC080 Vs V100R015C10)Document14 pagesMaterial For BTS3900&BTS5900 Node Performance Counter Changes (V100R015C10SPC080 Vs V100R015C10)klajdiNo ratings yet
- 5 Bivariate Statistics - P1 - QPDocument7 pages5 Bivariate Statistics - P1 - QPSarah HilyNo ratings yet
- Hanoi Open University PDFDocument18 pagesHanoi Open University PDFLinh ChuNo ratings yet
- S 3300.4 Introduction To Hispanic Literature and Literary AnalysisDocument17 pagesS 3300.4 Introduction To Hispanic Literature and Literary AnalysisElizabeth SoteloNo ratings yet
- Sem Osteoporosis (Edit)Document31 pagesSem Osteoporosis (Edit)Rhomizal MazaliNo ratings yet
- Parable of The SowerDocument1 pageParable of The SowerWrechellejoyNo ratings yet
- Semana2Document66 pagesSemana2Edward A TuerosNo ratings yet
- MedievalPeriod PowerPointDocument25 pagesMedievalPeriod PowerPointmarina guevaraNo ratings yet
- Mobile Computing and Commerce and Pervasive ComputingDocument13 pagesMobile Computing and Commerce and Pervasive Computingasma246No ratings yet
- Palo Alto Sample WorkbookDocument12 pagesPalo Alto Sample WorkbookRavi ChaurasiaNo ratings yet
- Personal Pov On StudentsDocument2 pagesPersonal Pov On Students7xnc4st2g8No ratings yet
- Biomechanics Chapter1Document11 pagesBiomechanics Chapter1mutansNo ratings yet
- Biography of 16th Karmapa and 3d Jamgon KongtrulDocument16 pagesBiography of 16th Karmapa and 3d Jamgon KongtrulSergey SergeyNo ratings yet
- Focusing Experiential ScaleDocument46 pagesFocusing Experiential Scaleagnes windram100% (1)
- Kuhn's Algorithm For Finding The Greatest Matching in A Bipartite GraphDocument6 pagesKuhn's Algorithm For Finding The Greatest Matching in A Bipartite GraphRavi GohelNo ratings yet
- Zimbra OS Admin GuideDocument188 pagesZimbra OS Admin GuideCarlitos CustodioNo ratings yet