Professional Documents
Culture Documents
Class 2
Uploaded by
hari dharshan0 ratings0% found this document useful (0 votes)
2 views65 pagesCopyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
2 views65 pagesClass 2
Uploaded by
hari dharshanCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 65
CELL INJURY
• ETIOLOGY OF CELL INJURY
• The causes of cell injury, reversible or irreversible, may be broadly classified into two large groups:
• A. Genetic causes
• B. Acquired causes
• Based on underlying agent, the acquired causes of cell injury can be further categorised as under:
• 1. HYPOXIA AND ISCHAEMIA. Hypoxia is the most common cause of cell injury.
• The most common mechanism of hypoxic cell injury is by reduced supply of blood to cells i.e. ischaemia.
• However, oxygen deprivation of tissues may result from other causes as well e.g. in anaemia, carbon
monoxide poisoning, cardiorespiratory insufficiency, and increased demand of tissues.
• 2. PHYSICAL AGENTS. Physical agents in causation of disease are: mechanical trauma (e.g. road
accidents); thermal trauma (e.g. by heat and cold); electricity; radiation (e.g. ultraviolet and ionising); and
rapid changes in atmospheric pressure.
• 3. CHEMICALS AND DRUGS. An ever increasing list of chemical agents and drugs may cause cell injury.
Important examples include: chemical poisons such as cyanide, arsenic, mercury; strong acids and alkalis;
environmental pollutants; insecticides and pesticides; oxygen at high concentrations; hypertonic glucose and
salt; social agents such as alcohol and narcotic drugs; and therapeutic administration of drugs.
• 4. MICROBIAL AGENTS. Injuries by microbes include infections caused by bacteria, rickettsiae, viruses,
fungi, protozoa, metazoa, and other parasites.
• 5. IMMUNOLOGIC AGENTS. Immunity is a 'double-edged sword'- protects the host against various injurious
agents but it may also turn lethal and cause cell injury e.g. hypersensitivity reactions; anaphylactic reactions;
and autoimmune diseases.
• 6. NUTRITIONAL DERANGEMENTS. A deficiency or an excess of nutrients may result in nutritional
imbalances.
• 7. PSYCHOLOGIC FACTORS. There are no specific biochemical or morphologic changes in common
acquired mental diseases due to mental stress, strain, anxiety, overwork and frustration e.g. depression,
schizophrenia. However, problems of drug addiction, alcoholism, and smoking result in various organic
diseases such as liver damage, chronic bronchitis, lung cancer, peptic ulcer, hypertension, ischaemic heart
disease etc.
MORPHOLOGY OF CELL INJURY
• Depending upon the severity of cell injury,
degree of damage and residual effects on
cells and tissue are variable. According to
premises, the cell injury includes following
pathological processes:
• i) dystrophies
• ii) necrosis
• iii) cellular adaptation.
• Dystrophy - a complex pathological
process based on abnormality at pathway
of a histic (cellular) metabolism and
described by quantitative and qualitative
disturubances of cell or tissue structure,
that leads to structural changes and loss
of their functions.
Morphogenetic mechanisms
• 1. Infiltration- it is penetration of substances into cells or
tissues from the outside where there are lot of them,
most frequently form in the epithelium of renal tubule
when protein, glucose and so on are exude with urine.
(diabetes mellitus, glomerulonephritis)
• 2. Transformation it is transition of one substance into
others, for example in the superfluous use of
carbohydrates and proteins they turn into fats and
adiposity appears. (fat dystrophy of the liver, obesity)
• 3. Decomposition is a disintegration of complex
substances, for example lipoprotein membranes in a
cell, in which arise fatty and proteinous dystrophies. (fat
dystrophy of the heart due to destructions of
mitochondrial membrane in myocardial ischemia)
• 4. Perverted (unnatural) synthesis is formation of
substances which in norm are not being found (for
example an amyloid, Melory bodies in alcoholic
hepatitis, multiple [plasma cell] myeloma).
Classification of dystrophies:
• A. According to primary localization of changes:
1. Parenchymatous (endocellular), 2. Stomal-
vascular (mesenchymal, extracellular), 3. Mixed.
• B. According to mainly broken metabolism: 1.
Proteinous (dysproteinoses), 2. Fatty (lipidoses),
3. Carbohydrate, 4. Mineral
• C. According to development: 1. Acquired, 2.
Congenital
• D. According to prevalence: 1. Local,
• 2. Systemic.
• Parenchymatous dystrophies are
dystrophies in which pathological changes
are localized inside the cells of organs
parenchyma in high- specialized cells,
such as myocardiocytes, hepatocyte,
epithelium of renal tubule .
• Proteinous parenchymatous dystrophies
include:
• 1. hyaline-droplet,
• 2. hydropic,
• 3. keratinization dystrophy and
• 4. congenital form of proteinous
parenchymatous dystrophies.
Hyaline-droplet dystrophy.
• Hyaline is a descriptive histologic term for
glassy, homogeneous, eosinophilic
appearance of material in haematoxylin
and eosin-stained sections and does not
refer to any specific substance. Hyaline
change is associated with heterogeneous
pathologic conditions and may be
intracellular or extracellular.
INTRACELLULAR HYALINE.
• 1. Hyaline droplets in the proximal tubular epithelial cells
in cases of excessive reabsorption of plasma proteins
(glomerulonephritis, nephrotic syndrome).
• 2. Hyaline degeneration of voluntary muscle, also called
Zenker's degeneration, occurs in rectus abdominalis
muscle in typhoid fever. The muscle loses its fibrillar
staining and becomes glassy and hyaline.
• 3. Mallory's hyaline represents aggregates of
intermediate filaments in the hepatocytes in alcoholic
liver cell injury.
• 4. Nuclear or cytoplasmic hyaline inclusions seen in
some viral infections.
• 5. Russell's bodies representing excessive
immunoglobulins in the rough endoplasmic reticulum of
the plasma cells (myelomatosis (plasmocytoma, Kahler's
disease)).
• The hyaline-dropical dystrophy is a
severe irreversible kind of dystrophy, it
always ends by coagulation necrosis of
cells and decrease or the loss of the organ
function.
• In the kidney it manifests it self as
proteinuria , cylinderuria, in the blood
arises hypoproteinemia.
Hydropic [vacuolar] dystrophy.
• This is the commonest and earliest form of
cell injury from almost all causes.
• The common causes of cellular swelling
include: bacterial toxins, chemicals,
poisons, burns, high fever, intravenous
administration of hypertonic glucose or
saline etc.
Pathogenesis
• Abnormalities of protein-hydro electrolytic
balance, especially for sodium.
• Membranes damage and activation of
lysosomal hydrolyses
• Macroscopically view of organs and
tissue variates little. The affected organ
such as kidney, liver or heart muscle is
enlarged due to swelling. The cut surface
bulges outwards and is slightly opaque.
Microscopically
• 1. The cells are swollen and the microvasculature
compressed.
• 2. Small clear vacuoles are seen in the cells and
hence the term vacuolar degeneration. These
vacuoles represent distended cisternae of the
endoplasmic reticulum. If there is a lot of liquid and it
fills in the whole cell superseding a nucleus into
periphery, such kind of hydropic [vacuolar] dystrophy
is called ballooning degeneration - especially it is
characteristic of hepatocytes in a viral hepatites.
• Hydropic [vacuolar] dystrophy is severe irreversible
kind of a dystrophy and it always ends in coagulation
necrosis of cells. Except for the liver it happens more
often in a ganglionic cells, adrenal glands,
myocardium .
Keratinization dystrophy
• It is accumulation of keratin substance where in norm it
is not present, or excessive accumulation of keratin
substance where it’s can be in norm (skin). The causes
are: i) avitaminosises, ii) developmental anomalies of a
skin, iii) viral infection, iv) chronic inflammation. The
types of a keratinization dystrophy are:
• 1. hyperkeratosis- it superfluous keratinization on a skin,
sometimes it is present as a “skin horn”
• 2. Ichthyosis- is a congenital hyperkeratosis of skin (the
child born with a thick skin similar to the fish scales,
usually he dies at once)
• 3. Leukoplakia is keratinization of mucous membranes
covered with squamous cell non-keratinizing epithelium .
More often it can be in cervix of the uterus, there can
also be in the oesophagus , oral cavity, etc. Leukoplakia
is dangerous as it lead to squamous cell carcinoma .
Severe plantar hyperkeratosis
Congenital form of proteinous
parenchymatous dystrophies.
• Inheritable parenchymatous proteinous
dystrophias are caused by abnormality of
amino acid metabolism, for example:
• cystianosis,
• tyrosinosis,
• phenyl-pyruvic oligophrenia
(phenylketonuria)
Parenchymatous fatty
dystrophies.
• Causes of parenchymatous fatty
dystrophies are:
• 1. The hypoxia is the common cause,
especially in such diseases as а) anemias,
b) diseases of the heart, c) lung diseases
• 2. Infections and intoxications, especially
alcohol intoxication
• 3. Ireegular diet and avitaminoses.
Mechanism
• Destruction of endoceilular organels
membranes by increased transport of
triglycerides or fatty acids to affected cells,
decreased mobilization of fat, decreased
use of fat, overproduction of fat in cells
occurs in chronic hypoxic states.
• This mechanism was named
decomposition (phanerosis).
Fatty dystrophia of the liver
• ETIOLOGY. The common causes of fatty liver
include the following: i) Excess alcohol
consumption (most common); ii) starvation; iii)
malnutrition; iv) obesity; v) diabetes mellitus; vi)
chronic illnesses (e.g. tuberculosis); vii) late
pregnancy; viii) hypoxia (e.g. anaemia, cardiac
failure); ix) hepatotoxins (e.g. carbon
tetrachloride, chloroform, ether, aflatoxins and
other poisons); x) certain drugs (e.g.
administration of oestrogen, steroids,
tetracycline etc);
Macroscopically
• The fatty liver is enlarged with a tense,
glistening capsule and rounded margins.
The cut surface bulges slightly and is pale-
yellow to yellow and is greasy to touch, so-
called "goose" liver.
Microscopically
• There are numerous lipid vacuoles in the cytoplasm of
hepatocytes.
• i) The vacuoles are initially small and are present around
the nucleus (microvesicular).
• ii) But with progression of the process, the vacuoles
become larger pushing the nucleus to the periphery of
the cells (macrovesicular).
• iii) At times, the hepatocytes laden with large lipid
vacuoles may rupture and lipid vacuoles coalesce to
form fatty cysts.
• iv) Infrequently, lipogranulomas may appear consisting
of collections of lymphocytes, macrophages, and some
multinucleated giant cells.
• v) Fat in the tissue can be demonstrated by frozen
section followed by fat stains such as Sudan dyes
(Sudan III, IV, Sudan black), oil red and osmic acid.
Fatty dystrophies of the heart.
• Most common cause is chronic hypoxia
(ischemic heart diseases, lung diseases,
anemias). Morphogenic mechanisms are
decomposition and infiltration.
• Macroscopically:The size of heart enlarged, its
cavity dilated, myocardium is flabby, yellow
coloured. Ochroleucous striation is visible under
the endocardium of ventricles, especial in range
of trabeculas and papillary muscles. It may be
compared with tiger skin (tiger heart). This
striation based on local fatty change of
cardiomyocytes.
Microscopically
• Small fatty drops, stained by a liposoluble
- Sudan-III, in yellow-orange colour is
observed in cytoplasm of cardiomyocytes,
localized around venuls and veins. Others,
neighbour cardiomyocytes, don't contain
fatty incorporations. Transversal striation
in cytoplasm of cardiomyocytes is absent,
nucleus are corrugated, intensively
painted by hematoxylin, or are turgent and
weakly painted (karyolyzis).
Congenital (systemic) lipidoses
• lipidoses arise owing to inheritable
deficiency of enzymes metabolizing some
kinds of lipids. In dependence on a kind of
lipoids collecting in cells distinguish:
• cerebrosides (Gaucher's disease),
• sphingomyelinoses (Niemann-Pick
disease),
• gangliosides (Tay-Sachs disease or an
amaurotic idiocy)
Parenchymatous carbohydrate
dystrophies.
• The inheritable carbohydrate dystrophy «glycogenoses»
is caused by absence or failure of the enzyme,
participating in scission of a deposited glycogen. These
are so-called inheritable enzymepaties or storage
diseases. 6 types of glycogenoses are well known:
• Gierke's disease,
• Pompe's disease,
• Mc. Ardle's disease,
• Hers' disease,
• Cori’s disease and
• Andersen disease.
• Morphological diagnostics of a glycogenosis is possible
by biopsy with the help of histocnzymochcmichal
methods
Cytoplasmic organelle damage leads to a variety of injury patterns, most of
which are best seen by electron microscopy. Acute injuries tend to damage an
entire cell, so specific organelle damage is beside the point. However, in some
cases the damage can be cumulative over many years. Here are Mallory bodies
(the red globular material) composed of cytoskeletal filaments in liver cells
chronically damaged from alcoholism. These are a type of "intermediate"
filament between the size of actin (thin) and myosin (thick).
№ 19 HYDROPIC DYSTROPHY OF HEPATOCYTES
Staining: hematoxylin- eosin
Designations:
1- Hydropic (vacuolar) dystrophia of hepatocytes
You might also like
- Usmle Step 2 CK Recalls 2021 3jz DR NotesDocument22 pagesUsmle Step 2 CK Recalls 2021 3jz DR Notesmed student100% (2)
- Cellular Injury and AdaptationsDocument145 pagesCellular Injury and AdaptationsAjmal RockzzNo ratings yet
- Heavy Metals and Their AntagonistsDocument42 pagesHeavy Metals and Their AntagonistsMohammad AzharuddinNo ratings yet
- Addenbrooke Cognitive ExaminationDocument11 pagesAddenbrooke Cognitive ExaminationAshlin BaijuNo ratings yet
- Mechanisms of Cell InjuryDocument21 pagesMechanisms of Cell Injuryبراءة أحمد السلاماتNo ratings yet
- H&PEDocument2 pagesH&PEDanielleNo ratings yet
- Leukocytosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandLeukocytosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Anatomy & Degenerations of Peripheral RetinaDocument29 pagesAnatomy & Degenerations of Peripheral RetinaNeelam Khatwani100% (1)
- Cellinjury 151004125508 Lva1 App6892Document147 pagesCellinjury 151004125508 Lva1 App6892Ajmal RockzzNo ratings yet
- Pathology Lecture SeriesDocument168 pagesPathology Lecture SeriesButch DumdumNo ratings yet
- Lecture 1 Cell Injury Adpation and DeathDocument39 pagesLecture 1 Cell Injury Adpation and Deathyat yat szeNo ratings yet
- L2 Physiology EOY MCQs AnsweredDocument366 pagesL2 Physiology EOY MCQs Answeredcarolinegatwiri08No ratings yet
- 2004 FRACP Written Examination Paediatrics & ChildDocument32 pages2004 FRACP Written Examination Paediatrics & ChildMedicEd100% (1)
- Evaluating Exam Review and Guide 2018 PDFDocument762 pagesEvaluating Exam Review and Guide 2018 PDFAthullia George83% (24)
- Must To Know HemaDocument44 pagesMust To Know HemaKaycee Gretz LorescaNo ratings yet
- Oral Diagnosis Tests GuideDocument128 pagesOral Diagnosis Tests GuideAya Abdelhakim 2216No ratings yet
- Cellular Injury and NecrosisDocument68 pagesCellular Injury and NecrosisAl-Rejab JabdhirahNo ratings yet
- SchistosomaDocument5 pagesSchistosomasarguss14100% (1)
- Cell InjuryDocument118 pagesCell InjuryShanzayNo ratings yet
- 2024 MYMAXICARE BROCHURE RatesDocument17 pages2024 MYMAXICARE BROCHURE RatesJuliet CoNo ratings yet
- Cell Injury, Death, and Adaptation: DefinitonsDocument37 pagesCell Injury, Death, and Adaptation: Definitonsyasobaby100% (1)
- CELL INJURY, DEATH, AND ADAPTATION: CAUSES AND MECHANISMSDocument46 pagesCELL INJURY, DEATH, AND ADAPTATION: CAUSES AND MECHANISMSeri_tariganNo ratings yet
- Cell Injury Notes-1Document63 pagesCell Injury Notes-1Stefanie VirniaNo ratings yet
- NewGeneral Pathology2Document305 pagesNewGeneral Pathology2Tahir AzizNo ratings yet
- General Pathology: Cell Injury, Adaptation and NecrosisDocument305 pagesGeneral Pathology: Cell Injury, Adaptation and NecrosisTahir AzizNo ratings yet
- Cell Injury and AdaptationDocument18 pagesCell Injury and AdaptationNazneen ShawarNo ratings yet
- 1 Cell InjuryDocument69 pages1 Cell InjuryOsama OsamaNo ratings yet
- Path Anat Part 1Document184 pagesPath Anat Part 1Javier Saad100% (1)
- 4 I Morpho - Reversible Cell InjuryDocument21 pages4 I Morpho - Reversible Cell InjuryKartikey MishraNo ratings yet
- Introduction to Pathological Anatomy Lecture 1Document18 pagesIntroduction to Pathological Anatomy Lecture 1Praveen NayakNo ratings yet
- Cell and Tissue InjuryDocument60 pagesCell and Tissue InjurydesiNo ratings yet
- Dystrophy Apoptosis NecrosisDocument41 pagesDystrophy Apoptosis NecrosisAbuFreihNo ratings yet
- PRIMARY BASE MEDICINE PATHOLOGYDocument49 pagesPRIMARY BASE MEDICINE PATHOLOGYMuhammad Ivan Adhar 19000105No ratings yet
- Morpho - Pathology Final Summary: Chapter 1: Cellular Reactions To AggressionDocument21 pagesMorpho - Pathology Final Summary: Chapter 1: Cellular Reactions To Aggressiondjxela89No ratings yet
- Cell Injury Pathology Types Causes MechanismsDocument17 pagesCell Injury Pathology Types Causes MechanismsAli AzizNo ratings yet
- Pathomorphology Final ExamDocument262 pagesPathomorphology Final ExamMann SarwanNo ratings yet
- Renal and Urinary System PathologyDocument70 pagesRenal and Urinary System PathologykiflomNo ratings yet
- Pathophysiology Chapter Summary: Cellular Changes and Disease ProcessesDocument8 pagesPathophysiology Chapter Summary: Cellular Changes and Disease ProcessesMozaLootahNo ratings yet
- Introduction To Pathology: Cell InjuryDocument5 pagesIntroduction To Pathology: Cell InjuryMara ZnagoveanuNo ratings yet
- III. Irreversible Cell Injury (Cell Death)Document42 pagesIII. Irreversible Cell Injury (Cell Death)Manal ElnemrNo ratings yet
- Cellular Responses To Stress and Toxic Insults: Adaptation, Injury, and DeathDocument26 pagesCellular Responses To Stress and Toxic Insults: Adaptation, Injury, and DeathHusam ShawaqfehNo ratings yet
- Renal and Urinary System Pathology: by Dr. Kiflom H. Sep, 2021 GCDocument258 pagesRenal and Urinary System Pathology: by Dr. Kiflom H. Sep, 2021 GCkiflomNo ratings yet
- Pengantar Patologi AnatomiDocument47 pagesPengantar Patologi AnatomiChristian V. H. TambaNo ratings yet
- Control of Cell Injury Homeostasis via FeedbackDocument30 pagesControl of Cell Injury Homeostasis via FeedbackAhmad KhoiruddinNo ratings yet
- Cell injuryDocument29 pagesCell injuryDrVnita VaishyaNo ratings yet
- Introducrion To PathologyDocument39 pagesIntroducrion To PathologyAyman ElsirNo ratings yet
- Circulating KineticsDocument82 pagesCirculating KineticsJilycamae COSMODNo ratings yet
- Cellular Injury and Death MechanismsDocument5 pagesCellular Injury and Death MechanismsAFSAL appuNo ratings yet
- Cell Injury MechanismsDocument87 pagesCell Injury MechanismsYashaswi SharmaNo ratings yet
- Cell Injury - 09.08.2023.ppt-1Document38 pagesCell Injury - 09.08.2023.ppt-1Abdur RaquibNo ratings yet
- Lecture 3 - The Cell and Reaction To Injury - 2 Sep 2006Document19 pagesLecture 3 - The Cell and Reaction To Injury - 2 Sep 2006api-3703352No ratings yet
- Cellular Injury, Adaptation and Cell DeathDocument14 pagesCellular Injury, Adaptation and Cell DeathGilo IlaganNo ratings yet
- Cell InjuryDocument77 pagesCell InjuryDEVASTATOR XNo ratings yet
- Cell Injury, Cell Death, and Adaptations: Dr. I Made Naris Pujawan, M.Biomed, SP - PADocument27 pagesCell Injury, Cell Death, and Adaptations: Dr. I Made Naris Pujawan, M.Biomed, SP - PAlindaNo ratings yet
- 2 Metabolic DisordersDocument72 pages2 Metabolic DisordersDonia HnainiaNo ratings yet
- Cell Injury: Yodit Getahun, MDDocument26 pagesCell Injury: Yodit Getahun, MDWolderufaelNo ratings yet
- Cell InjuryDocument19 pagesCell InjuryْNo ratings yet
- Dystrophy 1Document15 pagesDystrophy 1Ammar NasirNo ratings yet
- Cell Injury 2018Document56 pagesCell Injury 2018Mihaela IurescuNo ratings yet
- Cell Injury: Ii PharmdDocument51 pagesCell Injury: Ii PharmdBharath GowdaNo ratings yet
- Basic pathology concepts for cellular adaptations and accumulationsDocument54 pagesBasic pathology concepts for cellular adaptations and accumulationsaimi BatrisyiaNo ratings yet
- Intracellular Accumulations: Lipids, Proteins, PigmentsDocument8 pagesIntracellular Accumulations: Lipids, Proteins, PigmentsRohit NaiduNo ratings yet
- Cell Injury & Cellular Adaptations: Dr. Vigneshwara N Junior Resident, ImchDocument113 pagesCell Injury & Cellular Adaptations: Dr. Vigneshwara N Junior Resident, ImchAjmal RockzzNo ratings yet
- Degenerative ChangesDocument45 pagesDegenerative ChangesAbhishek JhaNo ratings yet
- Cell Injury and AdaptationDocument96 pagesCell Injury and AdaptationNayela AkramNo ratings yet
- PDF DocumentDocument47 pagesPDF DocumentkiarashNo ratings yet
- Understanding Cell Growth, Injury, Adaptation and DeathDocument76 pagesUnderstanding Cell Growth, Injury, Adaptation and Deathkasper mkNo ratings yet
- Early Cell Injury and Homeostasis Leading To Point of No Return Causes of Cellular InjuryDocument17 pagesEarly Cell Injury and Homeostasis Leading To Point of No Return Causes of Cellular InjurysridharNo ratings yet
- م 4Document10 pagesم 4Najwa AbdualgaderNo ratings yet
- Necrosis and Cellualr AdaptationDocument56 pagesNecrosis and Cellualr AdaptationEs SarveshNo ratings yet
- 2.cell Injury& Cell DeathDocument53 pages2.cell Injury& Cell Deathyaqeenallawi23No ratings yet
- Dermatology MiniOSCE 2Document352 pagesDermatology MiniOSCE 2Gmail JONo ratings yet
- DiphenhydrAMINE Monograph For ProfessionalsDocument12 pagesDiphenhydrAMINE Monograph For Professionalsioana teodorescuNo ratings yet
- Handbook of Ocular Disease ManagementDocument63 pagesHandbook of Ocular Disease ManagementSmaraNo ratings yet
- Wegeners GranulomatosisDocument65 pagesWegeners GranulomatosisLily HaslinaNo ratings yet
- Mental Status: Ateneo de Zamboanga UniversityDocument10 pagesMental Status: Ateneo de Zamboanga UniversitySheryhan Tahir BayleNo ratings yet
- Curs VII - Terapii SistemiceDocument229 pagesCurs VII - Terapii SistemiceHucay EduardNo ratings yet
- Gotu Kola Herbal Medicine Guide to Healing PropertiesDocument23 pagesGotu Kola Herbal Medicine Guide to Healing Propertiesglenn johnstonNo ratings yet
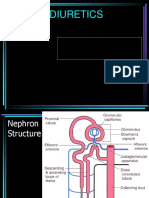
- DIURETICSDocument39 pagesDIURETICSFrancisNo ratings yet
- Emergency Red Flags: DR - Magdy Khames AlyDocument58 pagesEmergency Red Flags: DR - Magdy Khames AlyJerry AbleNo ratings yet
- Gingival Enlargement - DelDocument64 pagesGingival Enlargement - DeldelsaNo ratings yet
- Task 1. Active Learning Template: Assessment Teamwork and CollaborationDocument2 pagesTask 1. Active Learning Template: Assessment Teamwork and CollaborationAce FabrigasNo ratings yet
- T3 - Pack Code DetailsDocument302 pagesT3 - Pack Code DetailskiranNo ratings yet
- 0-0013 PDFDocument24 pages0-0013 PDFisabellaprie3No ratings yet
- Serum Ferritin - Past, Present and FutureDocument21 pagesSerum Ferritin - Past, Present and FutureAleksandar KitanovskiNo ratings yet
- Secondary Bsi 508Document77 pagesSecondary Bsi 508hansenNo ratings yet
- Health Psychology Canadian 4th Edition Taylor Solutions ManualDocument32 pagesHealth Psychology Canadian 4th Edition Taylor Solutions ManualJosephWilliamsinaom100% (13)
- Nursing Care Plan For Peritonitis NCPDocument2 pagesNursing Care Plan For Peritonitis NCPyamie sulongNo ratings yet
- (Physio A) ECG (Javier)Document4 pages(Physio A) ECG (Javier)AliNo ratings yet