Professional Documents
Culture Documents
SF 3 Dehydration Decalcification
Uploaded by
FRANCIS ANDREI H. MIRAOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
SF 3 Dehydration Decalcification
Uploaded by
FRANCIS ANDREI H. MIRACopyright:
Available Formats
Histotechnology– LECTURE (1st SEMESTER)
Instructor: Sir CHARLES ANDRE VLILACERAN <3
Transcribed by: FRANCIS ANDREI H. MIRA
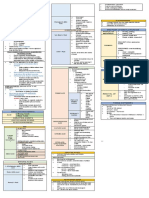
LECTURE 3: DECALCIFICATION, DEHYDRATION, AND CLEARING
FACTORS INFLUENCING THE RATE OF
DECALCIFICATION
1. CONCENTRATION
o The concentration of active agent will affect the rate at
which calcium is removed.
▪ Higher Concentration = faster removal of Calcium
▪ Greater Concentration = prone to shrinkage or
morphologic reactions to tissues (ie. Cell
damage).
o Published formulations for decalcifying solutions strike
a balance between speed and degree of tissue
damage.
o It must be remembered that the concentration of active
agent will be depleted as it (miscible) combines with
calcium and so it is wise to use a large volume of
NOTE: Histopathological Image of a bone trabeculae. It is not decalcifier and renew it several times during the
readily identifiable due to precipitates and artifacts. This is due decalcification process.
to incomplete decalcification (DC). Strongly strained with
Hematoxylin, and any calcium substances present in the tissue 2. TEMPERATURE
are hardly stained. If there is incomplete decalcification, there is o Increased temperature will speed up the decalcification
the over-decalcification (ODC). Difficulty in tissue cutting is rate but will also increase the rate of tissue damage so
also probably in incomplete DC. ODC reacts with stains during must be employed with great care.
the staining process. Tissues that are subject to ODC are hardly o Increase in Temp = Increased Risk for Tissue Damage
stained with Eosin, hindering examination of basophilic
structures in tissues. 3. AGITATION
o Gentle agitation may increase the rate slightly.
DECALCIFICATION o Impractical if done manually.
• Technique for removing minerals from bone or other
calcified tissue so that good-quality paraffin sections can be 4. FLUID ACCESS
prepared that will preserve the essential microscopic o As with fixation, fresh decalcifier should have ready
elements. access to all surfaces of the specimen. This will
• Carried out after the specimen has been thoroughly fixed enhance diffusion and penetration into the specimen
and prior to routine processing to paraffin. and facilitate solution, ionization, and removal of
calcium.
• If the calcified areas in tissue specimens are substantial, it
o It should penetrate the tissue as much as possible.
may be impossible to obtain decent sections without first
Obtain these tissues with proper gross examination
decalcifying the specimen.
and proper fixation.
• A GOOD DECALCIFYING AGENT MUST BE:
o CAPABLE OF REMOVING CALCIUM SALTS FROM
TISSUES COMPLETELY WITHOUT PRODUCING I. ACID DECALCIFYING AGENTS
CONSIDERABLE DESTRUCTION OF CELLS AND • Most widely used agents for decalcification of large
TISSUE COMPONENTS. amounts of bony tissues.
o WILL NOT AFFECT THE STAINING CAPACITY OF • Stable, easily available, relatively inexpensive
THE CELL (Specifically the nucleus) A. NITRIC ACID
• Calcium may be removed by one of the following agents: B. HYDROCHLORIC ACID
o 1. Acids C. FORMIC ACID
o 2. Chelating Agents D. TRICHLOROACETIC ACID
o 3. Ion Exchange Resins E. SULFUROUS ACID
o 4. Electrical Ionization (Electrophoresis) F. CHROMIC ACID
G. CITRIC ACID
NOTE: Decalcification sections are used for the NOTE: Acid Decalcifying Agents in higher concentrations induce
examination of bone (iliac crest, femoral head, tissue shrinkage or dysmorphic tissue processing results.
dissected/amputated specimens), bone marrow and for
the diagnosis of tumors, infections, and for other
purposes. Apart from pone, other samples receivable that
A. NITRIC ACID
can be submit to decalcification are: (1) tissues undergoing • Most common and fasted decalcifying agent.
degenerative processes (necrosis, dystrophic calcification), • Can be a simple decalcifying agent or combined with other
(2) Walls of blood vessels, lung, kidney, or somewhere else reagents.
where metastatic calcification occurs. POORLY FIXED • Recommended at 5-10%
SPECIMENS, become macerated (softened) during DC • MAIN DISADVANTAGE:
and will stain poorly afterwards. o Inhibits nuclear stains and destroys tissues especially
in concentrated solutions.
THE HOMIES <3 | MLS-2E 1
CLINICAL CHEMISTRY – LECTURE
A.1 AQUEOUS NITRIC ADDITIVE SOLUTION 10% B. HYDROCHLORIC ACID
• COMPONENT • Inferior to nitric acid because of its lower action and greater
o Concentrated Nitric Acid distortion.
o Distilled Water • May produce good nuclear staining when used in 1%
• DECALCIFICATION TIME (DCT): solution with 70% Alcohol.
o 12-24 HOURS
• Recommended for urgent biopsies, needle and small B.1 VON EBNER’S FLUID
biopsies to permit rapid diagnosis within 24 hours or less. • COMPONENT
o Saturated aqueous solution of NaCl 36%
A.2 FORMOL NITRIC ACID (10%) o Concentrated HCl
• COMPONENT o Distilled Water
o Concentrated Nitric Acid • Recommended for teeth and small pieces of bone
o Strong Formaldehyde (40%)
o Distilled Water C. FORMIC ACID
• DECALCIFICATION TIME (DCT): • Moderate acting decalcifying agent with better nuclear
o 1-3 Days staining and less tissue distortion
• PROS • Safer to handle than Nitric or HCl
o Rapid-acting for urgent biopsies • For decalcification of post-mortem tissue but not for
o Nuclear Staining is relatively good urgent examinations
• CONS • THE ONLY WEAK ACID USED EXTENSIVELY AS A
o Nitrous acid formation (yellow color) will impair staining PRIMARY DECALCIFYING AGENT.
reaction of the cell. • COMPONENT:
▪ Prevented by neutralizing the tissue with o Formic Acid
5% Sodium Sulfate and washing it with running o Formal Saline 10%
tap water for at least 12 hours; or • DECALCIFICATION TIME:
▪ Addition with 0.1% Urea to Pure Concentrated o 2-7 days
Nitric Acid to make discoloration disappear • Suitable for most routine surgical specimens when
without considerably affecting the efficiency of the immunohistochemical staining is needed.
decalcifying solution. • Relatively slow, not suitable for urgent specimens.
o You can hasten decalcification by increasing the
A.3 PERENYI’S FLUID proportion of formic acid to 25mL but such
• COMPONENT concentration may interfere with staining results.
o Nitric Acid 10% o Higher concentrations tend to disrupt tissue samples.
o Chromic Acid 0.5% • Requires neutralization with 5% sodium sulfate.
o Absolute Ethyl Alcohol
• DECALCIFICATION TIME (DCT): D. FORMIC ACID – SODIUM CITRATE SOLUTION
o 2-7 Days • COMPONENT:
• PROS o Aqueous sodium citrate 20%
o Decalcifies and softens at the same time. o Formic acid 45%
o Good nuclear and cytoplasmic staining. • DECALCIFICATION TIME:
o Maceration is avoided due to the presence of o 3-14 Days
chromic acid and alcohol. • Better nuclear staining than nitric acid method.
• CONS • Recommended for autopsy materials, bone marrow,
o Slow decalcifying agent for dense bones, not cartilage and tissues studied for research purposes.
recommended for urgent works. • Relatively slow, not recommended for urgent specimens.
• Requires neutralization with 5% sodium sulfate.
A.4 PHLOROGLUCIN NITRIC ACID
• COMPONENT E. TRICHLOROACETIC ACID
o Concentrated Nitric Acid • COMPONENT:
o Phloroglucin o TCA
o Nitric Acid (10%) o Formol Saline 10%
• DECALCIFICATION TIME (DCT): • DECALCIFICATION TIME:
o 12-24 hours o 4-8 DAYS
• SPECIFICALLY, THE MOST RAPID DECALCIFYING • PROS
AGENT, recommended for urgent works. o Does not require washing out, may be removed by
• CONS several changes of 90% Alcohol, improving tissue
o Poor nuclear staining dehydration.
o Prolonged decalcification produces extreme tissue • CONS
distortion. o Weak decalcifying agent, not used for dense tissues
(Poor penetrating action).
o Suitable only for small spicules of bone
o Very slow acting
THE HOMIES <3 | MLS-2E 2
CLINICAL CHEMISTRY – LECTURE
F. SULFUROUS ACID 3 WAYS TO MEASURE THE EXTENT OF
• Weak decalcifying solution suitable only for minute pieces DECALCIFICATION
of bone 1. Physical or • By touching or bending the tissue with
Mechanical Method the fingers to determine the
G. CHROMIC ACID (FLEMMING'S FLUID) consistency of tissues.
• COMPONENT • By pricking the tissue with a fine
o Chromic Acid needle/probe.
o Osmium Tetroxide 2. X-ray Radiological • Very expensive, although it is the most
o Glacial Acetic Acid method ideal, most sensitive and most
• PROS reliable method.
o May be used as fixative and decalcifying agent • Good but not always convenient.
• CONS • Not recommended for mercuric
o Inhibition of nuclear staining with hematoxylin chloride-fixed tissues (radio-opacity
o Forms precipitates requiring frequent changes of will interfere with the plate
solution interpretation).
3. Chemical method/ • Simple, reliable and convenient
H. CITRIC ACID - CITRATE BUFFER SOLUTION Calcium Oxalate test method recommended for routine
(PH 4.5) purposes (still favoured).
• COMPONENTS: • Decalcifying fluid is changed every 24-
o Citric acid (monohydrate) aqueous solution 7% 48 hrs Solutions used:
o 1. Concentrated Ammonium
o Ammonium citrate (anhydrous) aqueous solution 7.4%
Hydroxide
o Zinc sulfate aqueous solution 1% o 2 Saturated Aqueous
o Few drops of Chloroform Ammonium Oxalate
• DECALCIFICATION TIME: • Detection of calcium in acid solutions
o 6 DAYS by precipitation of insoluble calcium
• PROS hydroxide or calcium oxalate
o Permits excellent nuclear and cytoplasmic staining • Presence of cloudiness indicates the
without cell or tissue distortion. presence of Ca (incomplete
• CONS decalcification)
o Action is too slow for routine purposes.
DEHYDRATION AND CLEARING
CHELATING AGENTS
• Substances which combine with calcium ions and other NOTE: Remember that when talking about this, dehydration is
salts (iron and magnesium) to form weakly dissociated done for the paraffin-embedding phase as paraffin is not
complexes and facilitate removal of calcium salt. miscible (cannot combine) with water. The process
• Most common chelating agent: EDTA removes the fixative and the water from the tissues and
o Used as an anticoagulant and water softener replacing it with a dehydrating fluid. The presence of water
o Commercial name: in the tissues will cause the tissue components to
▪ Versene, Sequestrene disintegrate as no wax (i.e. paraffin) will hold them together.
Clearing is done to replace the dehydrating fluid (i.e.
alcohol) with a fluid that is totally miscible with the
NOTE: Very much advisable since it isn’t harmful and doesn’t
dehydrating fluid and the embedding medium.
cause disruption to tissue samples and but its cons is it has slow
Decalcification can be skipped if examination revealed no
penetration (slow-acting) on tissues and requires a large
calcium salts or deposits to be removed.
volume, and is very expensive.
DEHYDRATION
ION-EXCHANGE RESIN • The process of removing intracellular and extracellular
• lon exchange resin (ammonium form of polystyrene resin) water from the tissue following fixation (if decalcification is
hastens decalcification. not require) and prior to wax impregnation (clearing).
• Removes calcium ions from formic acid, thereby • Naturally carried out using some reagents (dehydrating
increasing solubility from the tissue. agents/dehydrants) that mixes with and has a certain
• Not recommended for fluids containing mineral acids such affinity for water so that it may penetrate easily between the
as Nitric Acid or HCl. tissue cells.
• Ideal Volume:
ELECTRICAL IONIZATION (ELECTROPHORESIS) o Not less than 10x the volume of tissue to be dehydrated
• Process whereby positively charged calcium ions are
attracted to a negative electrode (cathode) and COMMONLY USED DEHYDRATING AGENTS
subsequently removed from the decalcifying solution.
• Time required for decalcification is thereby shortened due A. ALCOHOL REAGENTS
to the heat and electrolytic reaction produced in this • Dehydration is best accomplished by the use of increasing
process. grades of alcohols, beginning with 70% (70>95>100)
• Principle applied is similar to that of chelating agents; with • Transfer of tissue directly from formalin to higher grades of
the main difference that this process utilize electricity and alcohol (85%-95%) is risky since it could lead to distortion
is dependent upon a supply of direct current to remove of tissues (shrinkage and hardening of tissues).
calcium deposits. • Concentrated solutions (above 80%) makes tissue hard,
• SOLUTION USED: brittle and difficult to cut.
o 88% Formic acid • Prolonged storage in lower concentrations (below 70%)
o Concentrated HCl tend to macerate the tissue.
o Distilled water
THE HOMIES <3 | MLS-2E 3
CLINICAL CHEMISTRY – LECTURE
• Tissue stored in 70%-80% may interfere with the staining • Clearing agent must be miscible with the dehydrating agent,
properties of the specimen. paraffin wax, and mounting medium.
• The word clearing is used because, in addition to removing
A.1 ETHANOL/ETHYL ALCOHOL alcohol, many of these substances have the property of
• Undoubtedly the best dehydrating agent (fast acting, mixes making tissues transparent/translucent.
with water and organic solvents and penetrates tissues • Ideal amount:
easily). o Not less than 10x the volume of the tissue.
• Has the advantage of not being poisonous and not very
expensive. COMMONLY USED CLEARING AGENTS
• Should be at least 99.7% pure. A. XYLENE
• Excellent and true clearing agent.
A.2 ISOPROPANOL/ISOPROPYL ALCOHOL • CLEARING TIME:
o 30 mins to 2 hours (usual)
• Should be used if good grade absolute ethyl alcohol is not
o 15 – 30 mins (urgent biopsies)
easily available.
• PROS
• A substitute to good-grade absolute ethyl alcohol
o Most rapid clearing agent
o Cheap and does not extract out aniline dyes
A.3 METHANOL/METHYL ALCOHOL o It is miscible with absolute alcohol and paraffin
• Toxic dehydrating agent o Can be used with celloidin sections
• For blood and tissue films and for smear preparations • CONS
o It is highly flammable.
A.4. BUTANOL/BUTYL ALCOHOL o When dehydration is not complete, the xylene
• Utilized for plant and animal micro-techniques becomes milky when the tissue or section is added.
B. ACETONE (CH3COCH3) B. TOLUENE
• Substitute to xylene or benzene.
• Cheap, rapid dehydrating agent utilized for most urgent
• Miscible with alcohol and paraffin.
biopsies (30 minutes – 2 hours).
• It is not carcinogenic but highly concentrated. Emits fumes
• Its use is limited to small pieces of tissues due to its extreme
that are highly toxic upon prolonged exposure.
volatility and flammability.
• It acts slower than benzene and is expensive.
• CLEARING TIME:
C. DIOXANE/DIETHYLENE DIOXIDE
o 1-2 hours
• Excellent dehydrating agent and clearing agent
• Miscible to water, melted paraffin, alcohol and xylol/xylene C. BENZENE
• Expensive and toxic, extremely dangerous (main • Rapid acting, recommended for urgent biopsies and routine
disadvantage). purposes.
• It is miscible with absolute alcohol and paraffin.
D. CELLOSOLVE/ETHYLENE GLYCOL MONOETHYL • Highly flammable
ETHER • Carcinogenic or may damage bone marrow.
• Dehydrates rapidly and not harmful to tissues • CLEARING TIME:
• Toxic by inhalation, skin contact, and ingestion (use o 15-60 minutes
propylene-based glycol esters).
D. CHLOROFORM
E. TRIETHYL PHOSPHATE • Best traditional clearing agents for routine use
• Gives the widest latitude
• Tissues can be transferred directly after fixation and
washing. • Recommended for tough (skin, fibroid, and decalcified
tissues) and large tissue specimens.
• Used to dehydrate sections and smears following certain
stains. • Also best for nervous tissue, lymph nodes, granulation
tissue, fetal and other delicate, highly cellular specimens.
• Does not make tissues transparent and it is toxic to the liver
F. TETRAHYDROFURAN (hepatoxic) after prolonged inhalation.
• Dehydrates and clears tissues since it is miscible to water • CLEARING TIME:
and paraffin. o 6-24 hours.
• IT is toxic if ingested or inhaled. Vapors cause nausea,
dizziness, and headache. E. CEDARWOOD OIL
• It is an eye and skin irritant and prolonged exposure (up to • Clears both paraffin and celloidin sections
6 months) may cause conjunctival irritation. • Recommended for CNS tissues and cytological studies
(esp. smooth muscles and skin)
CLEARING • Very expensive and it requires 2 changes in clearing
• OTHER TERM: DEALCOHOLIZATION solution
o We replace the dehydrating fluid with a fluid that is • Quality is not always uniform and good
miscible with the dehydrating fluid and embedding • Action is extremely slow
media. • Becomes milky on prolonged storage.
• The process whereby alcohol or a dehydrating agent is • CLEARING TIME:
removed from the tissue and replaced by a fluid (clearing o 2-3 days
agent) that will dissolve the wax with which the tissue must
be impregnated.
THE HOMIES <3 | MLS-2E 4
CLINICAL CHEMISTRY – LECTURE
F. ANILINE OIL
• Recommended for clearing embryos and very delicate
specimens since it clears 70% alcohol without excessive
tissue shrinkage and hardening.
G. CLOVE OIL
• Removes aniline dyes and dissolves celloidin, tissues
become brittle.
• Its quality is not guaranteed due to its tendency to be
adulterated.
• Not suitable for routine purposes because it is expensive.
H. CARBON TETRACHLORIDE (CCL4)
• Properties are very similar to chloroform but it is cheaper
• Toxic on prolonged exposure
I. TETRAHYDROFURAN
• Dehydrates and clears at the same time since it is miscible
in both water and paraffin.
J. METHYL BENZOATE/METHYL SALICYLATE
• Slow-acting clearing agents that can be used when double
embedding techniques are required.
THE HOMIES <3 | MLS-2E 5
You might also like
- SF-2 - Fixation and FixativesDocument9 pagesSF-2 - Fixation and FixativesFRANCIS ANDREI H. MIRANo ratings yet
- 3 Decalcification and DehydrationDocument5 pages3 Decalcification and DehydrationAngel RamosNo ratings yet
- 1 Decalcification of Calcified TissueDocument2 pages1 Decalcification of Calcified TissueAngel RamosNo ratings yet
- Decal-Clear NotesDocument3 pagesDecal-Clear NotesbarbiegahibNo ratings yet
- Dawson 1926Document2 pagesDawson 1926lauraserranogonzalez517No ratings yet
- Decalcification: By: Riman Mustafa IbrahimDocument21 pagesDecalcification: By: Riman Mustafa IbrahimdaliaNo ratings yet
- Histopath Trans 5 DecalcificationDocument10 pagesHistopath Trans 5 Decalcification3A PEÑA AndreaNo ratings yet
- Decalcification: MR G.P. Tiwari Technologist Tata Memorial HospitalDocument42 pagesDecalcification: MR G.P. Tiwari Technologist Tata Memorial HospitalGulab Chand Tiwari Tiwari100% (5)
- MT112 Histopath Lec DecalcificationDocument5 pagesMT112 Histopath Lec Decalcificationanti romantic txtNo ratings yet
- Decalcificati ON& Dehydration: By: Riman Mustafa IbrahimDocument21 pagesDecalcificati ON& Dehydration: By: Riman Mustafa IbrahimdaliaNo ratings yet
- L13. Tissue ProcessingDocument5 pagesL13. Tissue ProcessingTomNo ratings yet
- ASCP - InternationalDocument8 pagesASCP - InternationalWildercino RANo ratings yet
- Fixation and Processing College of American PathologistsDocument5 pagesFixation and Processing College of American Pathologistslansangan.regine.coeliNo ratings yet
- Histo 1Document3 pagesHisto 1VE NI CENo ratings yet
- Case Report Pulp Calcification: Case Reports With Difficult Endodontic ProblemDocument4 pagesCase Report Pulp Calcification: Case Reports With Difficult Endodontic ProblemHeng SiekhongNo ratings yet
- HP DecalcificationDocument7 pagesHP DecalcificationMalliga SundareshanNo ratings yet
- CalcificationDocument27 pagesCalcificationjsendaoNo ratings yet
- Histopathology Lab Activity 7Document3 pagesHistopathology Lab Activity 7BANGA, MICHAEL LEWIS M.No ratings yet
- HISTO-S01-T01-Histology & Its Methods of StudyDocument5 pagesHISTO-S01-T01-Histology & Its Methods of StudyShelahNo ratings yet
- Fixation & Fixatives: Histology ProcedureDocument14 pagesFixation & Fixatives: Histology ProcedureAsyeon GhaziNo ratings yet
- DECALCIFICATIONDocument4 pagesDECALCIFICATIONNelcy De Los SantosNo ratings yet
- Histopathology MidtermDocument2 pagesHistopathology MidtermAncestral garmentsNo ratings yet
- 7.2 HCT DecalcificationDocument1 page7.2 HCT DecalcificationGwen Kirsten AtayanNo ratings yet
- Factors Influencing DecalcificationDocument2 pagesFactors Influencing DecalcificationPork TapewormNo ratings yet
- Histopath MidtermDocument6 pagesHistopath MidtermAysha AishaNo ratings yet
- 04 HistotechniquesDocument70 pages04 HistotechniquesJulliene Dadole100% (1)
- Crystal GrowingDocument4 pagesCrystal GrowingLuis Petrikowski :3No ratings yet
- Try-In and Cementation of CrownsDocument10 pagesTry-In and Cementation of CrownsJohnny PakNo ratings yet
- Unit 4 and 5 CombinedDocument205 pagesUnit 4 and 5 CombinednagasudhanNo ratings yet
- Histopath Review 2017 (3.0 Hrs Lecture) Notes PDFDocument111 pagesHistopath Review 2017 (3.0 Hrs Lecture) Notes PDFPerlieCaguete100% (1)
- 1 Lab Report Sedimentation' Water Unit Operations Group 3 Bejarano Moreno Laura, Burgos Lopez Laura, Camacho LinaDocument8 pages1 Lab Report Sedimentation' Water Unit Operations Group 3 Bejarano Moreno Laura, Burgos Lopez Laura, Camacho LinaLaura Bejarano MorenoNo ratings yet
- Histopathology DECALCIFICATIONDocument2 pagesHistopathology DECALCIFICATIONJan Melli BalatbatNo ratings yet
- Histopath Trans 4 FixationDocument25 pagesHistopath Trans 4 Fixation3A PEÑA AndreaNo ratings yet
- Pulp Capping MaterialDocument21 pagesPulp Capping MaterialMohammad Abdul adheem100% (1)
- Fractures Avulsion EtcDocument5 pagesFractures Avulsion EtcAmanda HuggetNo ratings yet
- Histology Its Methods of StudyDocument6 pagesHistology Its Methods of StudyA18- Jessa Mae DayagNo ratings yet
- Histology - Lesson 1 - IntroDocument5 pagesHistology - Lesson 1 - IntroAngelina AquinoNo ratings yet
- Crystallization (Final)Document23 pagesCrystallization (Final)ANH Nguyễn Hoàng VânNo ratings yet
- Colloidal DispersionDocument27 pagesColloidal DispersionVISHNU RAJ VNo ratings yet
- Fresh Tissue ExaminationDocument6 pagesFresh Tissue ExaminationChiizu iraNo ratings yet
- Gravity Separation Lecture 5Document16 pagesGravity Separation Lecture 5Syazwan ShafriNo ratings yet
- Lecture 2 Dna Ectraction Non Organic MethodDocument21 pagesLecture 2 Dna Ectraction Non Organic MethodRahat WazireNo ratings yet
- DECALCIFICATIONDocument10 pagesDECALCIFICATIONPriyanshiNo ratings yet
- Pulpcappingagents 160810093642Document67 pagesPulpcappingagents 160810093642Justforkiddslaserdental ChNo ratings yet
- Bone Decalcification 1Document22 pagesBone Decalcification 1lalemchanie16No ratings yet
- COARSE DISPERSIONS ReviewedDocument80 pagesCOARSE DISPERSIONS ReviewedThando ComeNo ratings yet
- LAB Histopathologic-Technique EmbeddingInfiltration Finals 002Document3 pagesLAB Histopathologic-Technique EmbeddingInfiltration Finals 002Jashmine May TadinaNo ratings yet
- PHCM223 - Lecture 11 - SS16 - 516Document31 pagesPHCM223 - Lecture 11 - SS16 - 516erorcrept100% (1)
- HPCT Lec Week 3 - Fresh Tissue Examination, Special Tissue Processing, Fixation.Document3 pagesHPCT Lec Week 3 - Fresh Tissue Examination, Special Tissue Processing, Fixation.Marc Jeff GabasaNo ratings yet
- 04a Decalcification Activity PDFDocument3 pages04a Decalcification Activity PDFSang SungNo ratings yet
- Gravimetric Analysis MidtermDocument3 pagesGravimetric Analysis MidtermMerylle Erika Sta. MariaNo ratings yet
- Histopathologic Technique: Two KeyplayersDocument19 pagesHistopathologic Technique: Two KeyplayersHadjar MitmugNo ratings yet
- Ch4 3 Watertreatment CoagDocument56 pagesCh4 3 Watertreatment CoagSUBHAM KumarNo ratings yet
- Caderno UC1 HistologyDocument15 pagesCaderno UC1 HistologyantonietohNo ratings yet
- GB Clin ManDocument20 pagesGB Clin ManȘenchea Crina ElenaNo ratings yet
- Colloids DR - RanaDocument87 pagesColloids DR - RanaAhmad Nouri100% (1)
- Operative Dentistry, QuintessenceDocument5 pagesOperative Dentistry, QuintessenceОлександр Байдо100% (1)
- Introduction To HistologyDocument32 pagesIntroduction To Histologyzainab100% (1)
- Long-Term Sealing Ability of A Calcium Hydroxide SealerDocument3 pagesLong-Term Sealing Ability of A Calcium Hydroxide SealerAmelia RahmayantiNo ratings yet
- Reverse Osmosis Treatment of Drinking WaterFrom EverandReverse Osmosis Treatment of Drinking WaterRating: 3.5 out of 5 stars3.5/5 (4)
- Chapter 10 Tute Solutions PDFDocument7 pagesChapter 10 Tute Solutions PDFAi Tien TranNo ratings yet
- Hockney-Falco Thesis: 1 Setup of The 2001 PublicationDocument6 pagesHockney-Falco Thesis: 1 Setup of The 2001 PublicationKurayami ReijiNo ratings yet
- Acting White 2011 SohnDocument18 pagesActing White 2011 SohnrceglieNo ratings yet
- Johnson & Johnson Equity Research ReportDocument13 pagesJohnson & Johnson Equity Research ReportPraveen R V100% (3)
- Vitamins - CyanocobalaminDocument12 pagesVitamins - CyanocobalaminK PrashasthaNo ratings yet
- Words of Radiance: Book Two of The Stormlight Archive - Brandon SandersonDocument6 pagesWords of Radiance: Book Two of The Stormlight Archive - Brandon Sandersonxyrytepa0% (3)
- Img 20150510 0001Document2 pagesImg 20150510 0001api-284663984No ratings yet
- Grade 3 - Unit 1 Increase and Decrease PatternDocument7 pagesGrade 3 - Unit 1 Increase and Decrease PatternKyo ToeyNo ratings yet
- DJ Crypto ResumeDocument1 pageDJ Crypto ResumeNitin MahawarNo ratings yet
- 0012 Mergers and Acquisitions Current Scenario andDocument20 pages0012 Mergers and Acquisitions Current Scenario andJuke LastNo ratings yet
- Practice - Test 2Document5 pagesPractice - Test 2Nguyễn QanhNo ratings yet
- Genuine Fakes: How Phony Things Teach Us About Real StuffDocument2 pagesGenuine Fakes: How Phony Things Teach Us About Real StuffGail LeondarWrightNo ratings yet
- The Scope and Method of Economics: © 2007 Prentice Hall Business Publishing Principles of Economics 8e by Case and FairDocument36 pagesThe Scope and Method of Economics: © 2007 Prentice Hall Business Publishing Principles of Economics 8e by Case and FairLangson phiriNo ratings yet
- NAV SOLVING PROBLEM 3 (1-20) .PpsDocument37 pagesNAV SOLVING PROBLEM 3 (1-20) .Ppsmsk5in100% (1)
- Derma Notes 22pages. DR - Vishwa Medical CoachingDocument23 pagesDerma Notes 22pages. DR - Vishwa Medical CoachingΝίκος ΣυρίγοςNo ratings yet
- Chapter 5 Constructing An Agile Implementation PlanDocument4 pagesChapter 5 Constructing An Agile Implementation PlanAHMADNo ratings yet
- Traditional Perceptions and Treatment of Mental Illness in EthiopiaDocument7 pagesTraditional Perceptions and Treatment of Mental Illness in EthiopiaifriqiyahNo ratings yet
- Loctite 586 PDFDocument9 pagesLoctite 586 PDForihimieNo ratings yet
- 2nd Term Project 4º Eso Beauty Canons 2015-16 DefinitivoDocument2 pages2nd Term Project 4º Eso Beauty Canons 2015-16 DefinitivopasferacosNo ratings yet
- Hare and Hyena: Mutugi KamundiDocument18 pagesHare and Hyena: Mutugi KamundiAndresileNo ratings yet
- A Content Analysis of SeabankDocument13 pagesA Content Analysis of SeabankMarielet Dela PazNo ratings yet
- Plastic Properties HandbookDocument15 pagesPlastic Properties HandbookguilloteARGNo ratings yet
- 4th Sept - Marathon Series Lecture 8 - General AwarenessDocument208 pages4th Sept - Marathon Series Lecture 8 - General AwarenessManbir ArinNo ratings yet
- Manuel SYL233 700 EDocument2 pagesManuel SYL233 700 ESiddiqui SarfarazNo ratings yet
- G10 Lesson2 DLPDocument13 pagesG10 Lesson2 DLPAngeles, Mark Allen CNo ratings yet
- Literature Review Template DownloadDocument4 pagesLiterature Review Template Downloadaflsigfek100% (1)
- Boundary Value Analysis 2Document13 pagesBoundary Value Analysis 2Raheela NasimNo ratings yet
- Alfa Week 1Document13 pagesAlfa Week 1Cikgu kannaNo ratings yet
- Existentialism in CinemaDocument25 pagesExistentialism in CinemanormatthewNo ratings yet
- Module 6 Metal Properties and Destructive TestingDocument46 pagesModule 6 Metal Properties and Destructive TestingMiki Jaksic100% (6)