Professional Documents
Culture Documents
MED II 1.03 Heart Diseases Series
Uploaded by
CRUZ Jill EraCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
MED II 1.03 Heart Diseases Series
Uploaded by
CRUZ Jill EraCopyright:
Available Formats
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
symptoms first then right sided symptoms to determine
OUTLINE exclusivity of right sided symptoms or the progression of
I. Heart Failure (HF)
left sided symptoms that leads to right sided symptoms)
A. Epidemiology
B. Etiology
C. Global Considerations
D. Prognosis
E. Pathogenesis
F. Symptoms
G. Physical Examination
H. Diagnosis
I. Management
I. Heart Failure (HF)
• Complex clinical syndrome
• Results from structural or functional impairment of
HFrEF HRpEF
Heart Failure with a reduced Hear Failure with a preserved
Ejection Fraction (formerly EF (formerly known as diastolic
known as systolic failure) failure)
Although HF once was thought to arise primarily in the setting of a
depressed left ventricular ejection fraction, studies have shown that
approximately one-half (1/2) of patients who develop HF have a
normal or preserved EF. (*Harrison’s)
ventricular filling or ejection of blood
A. Epidemiology
• 2% overall prevalence of heart failure (HF) affects 6-10% of
people over the age of 65.
• Relative incidence is LOWER in WOMEN
o But women constitute one-half of the cases of
Heart Failure (HF).
B. Etiology
RIGHT SIDED FAILURE LEFT SIDED FAILURE
• Coronary artery disease (CAD) (MOST COMMON) –
Fatigue Paroxysmal nocturnal dyspnea
predominant cause in men and women
Increased Peripheral venous Elevated pulmonary capillary o Responsible for 60-75% of cases of HF.
pressure wedge o Hx – look for history of “angina” specially during
Ascites Cough, Crackles, Wheezing physical exertion and history of heart attack or
Enlarged Liver & Spleen Blood tinged sputum angiogram or diagnosed history of CAD
Distended Jugular Veins Restlessness • Hypertension – contributes to the development of HF in
Anorexia & Complaints of GI Confusion • 75% of patients, including most patients with CAD.
distress o Important history for the development of heart
Swelling in Hands & Fingers Orthopnea failure
Dependent Edema Tachycardia *(Harrison’s) Both CAD and hypertension interact to augment the
Exertional Dyspnea risk for Heart Failure (HF), as does diabetes mellitus.
Cyanosis
• Most common cause of right sided heart failure symptoms
are same with the causes of left sided heart failure as well.
(In history taking, take into consideration left sided
INTERNAL MEDICINE II Milanes, Gwapo Marquez 1 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
(Harrison’s page 1764: Section 4: Disorders of the Heart)
New York Heart Association (NYHA) Classes
NYHA class I NYHA class II NYHA class III NYHA class IV
-No -Slight -Marked -Inability to
limitations on limitation on limitation on carry on any
physical physical physical activity
activities activities activities without
symptoms
-No overt -Comfortable -Comfortable
(Harrison’s page 1763: Section 4: Disorders of the Heart) symptoms at rest, but at rest, but -Presence of
• Depends on 2-D echo to differentiate the 3. ordinary less than symptoms
physical ordinary even at rest
• In high-output state, also check for systemic problems like
activity activity
thyroid problem and arteriovenous fistula which may causes causes
cause signs and symptoms for heart failure. symptoms of symptoms of
heart failure heart failure
C. Global Considerations
• Rheumatic heart disease – most common cause of Heart D. Prognosis
Failure in Africa and Asia. • 30-40% die within a year of Diagnosis
• Chaga’s disease – most common cause of Heart Failure in • 60-70% die within 5 years, mainly from worsening HF or as
South America a sudden event
• (Harrison’s) Hypertension is an important cause of Heart • 30-70% annual mortality rate for NYHA class 4
failure in African and African-American populations. • Thus, assessment of FUNCTIONAL STATUS – is an
• Diabetes Mellitus (DM) accelerates atherosclerosis and IMPORTANT predictor of patient outcome.
often associated with hypertension. (3 P’s of Diabetes: o Patient improvement with medication should be
Polydipsia, Polyphagia, Polyuria) noted.
• (Harrison’s) Anemia – is a frequent concomitant factor in
Heart Failure in many developing Nations E. Pathogenesis
PATHOGENESIS OF HEART FAILURE WITH A DEPRESSED EJECTION
FRACTION
Compensatory Mechanisms:
1. Adrenergic nervous system
2. Renin-Angiotensin-Aldosterone System (RAAS)
3. Cytokine system
INTERNAL MEDICINE II Milanes, Gwapo Marquez 2 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
ACTIVATION OF A FAMILY OF COUNTERVAILING VASODILATORY
MOLECULES
• Atrial and Brain natriuretic peptides (ANP and BNP)
• Prostaglandins (PGE2 and PGI2)
• Nitric oxide (NO)
• Offsets the excessive peripheral vascular vasoconstriction.
ACTIVATION OF NEUROHORMONAL SYSTEMS IN HEART FAILURE
• Decreased CO (Cardiac Output) in HF
o *Continued increase in heart beat → the faster
the progression of HF
• “unloading” of high-pressure baroreceptors (reason why
we also give RAAS inhibitors)
• Loss of inhibitory parasympathetic tone
• Generalized increase in efferent sympathetic tone (reason
why we give Beta-blockers)
• Non-osmotic release of AVP (Arginine-Vasopressin) from
the pituitary
• AVP or ADH (powerful vasoconstrictor) ↑permeability of
the renal collecting ducts → reabsorption of free water.
o *That is why we see patients with bipedal
edema, sometime ascites, that is why we give
diuretics.
• Sympathetic stimulation of the kidney
o → activation of the RAAS
o → promotes salt & water retention
o → vasoconstriction of the peripheral
vasculature, myocyte hypertrophy, myocyte cell
death, and myocardial fibrosis (once fibrosis has
settled, medicines may not have any effect
anymore, cardiac transplantation might be the
course)
* Harrison’s, page 1765, Figure 252-2.
*Review: Most potent Vasoconstrictor = Angiotensin II
INTERNAL MEDICINE II Milanes, Gwapo Marquez 3 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
F. Symptoms
VENTRICULAR REMODELLING
• Changes in LV mass, volume, and shape and the • Cardinal sign of HF – Fatigue and shortness of breath
composition of the heart. • Dyspnea in HF
• Occur after cardiac muscle injury and/or abnormal o MOST IMPORTANT mechanism is PULMONARY
hemodynamic loading conditions CONGESTION with accumulation of interstitial or
• May contribute independently to the progression of HF.
• (leftmost) note the part of the acute infraction → Infract
zone thinning & elongation (fibrous scars) → Spherical
Ventricular Dilatation (there is an increased Interstitial
Collagen and Myocyte Hypertrophy)
• Reason why some MI patients are given anti-
platelet/fibrinolysin/angioplasty.
intra-alveolar fluid.
• Exercise: if the left ventricle is dilated what valve is
*First thing you could find in an X-ray of HF is Cardiomegaly and
affected? Answer: Mitral Valve (reason in anatomy, the
signs of pulmonary congestion/edema.
chordae tendinea is attached to the papillary muscle of the
left ventricle → in turn pulling it and cannot close → leads
• Orthopnea
to mitral regurgitation (incompetence))
o Dyspnea occurring in the recumbent position
o Redistribution of fluid from the splanchnic
circulation and lower extremities into the central
circulation during recumbency.
o Resultant increase in pulmonary capillary
pressure.
INTERNAL MEDICINE II Milanes, Gwapo Marquez 4 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
• Paroxysmal Nocturnal Dyspnea (PND)
o Acute episodes of severe shortness of breath
and coughing that occur at night and awaken the
patient from sleep.
o Usually, 1-3 hours after the patient retires
o Due to increased pressure in the bronchial
arteries leading to airway compression
• Cheyne-Stokes Respiration
o Periodic respiration or cyclic respiration
o Present in 40% of patients with advanced HF and
usually associated with low cardiac output.
o Caused by an increased sensitivity of the
respiratory center to atrial PCO2.
o There is an apneic phase, during which arterial
PO2 falls and arterial PCO2 rises, which lead to
o Hyperventilation and hypocapnia, followed by
recurrence of apnea.
• Gastrointestinal symptoms • Cardiac examination
o Anorexia, nausea, and early satiety associated o Frequently does not provide useful information
with abdominal pain and fullness about the severity of HF
o Related to edema of the bowel and/or a o PMI (Point of Maximal Impulse) usually is
congested liver. (RUQ pain = distended Glisson’s displaced below the fifth intercostal space
Capsule) and/or lateral to the midclavicular line.
• Cerebral symptoms o In some patients, a third heart sound (S3) is
o Confusion, disorientation, and sleep and mood audible and palpable at the apex.
disturbances may be observed in patients with
severe HF. (Because of reduced blood flow to the
brain) (particularly seen in HF of elderly patients
w/cerebral atherosclerosis and reduced cerebral
perfusion)
G. Physical Examination
• GENERAL APPEARANCE: In mild or moderate sever HF, Px
appears with no distress at rest, except of feeling
uncomfortable when lying flat for more than a few
minutes. In severe HF (labored breathing, cannot finish
sentence due to shortness of breath, Systolic pressure may
be normal or high, pulse pressure may be diminished,
Sinus tachycardia, Peripheral vasoconstriction → cool • Abdominal examination
extremities and cyanosis of lips and nail beds) o Ascites, a late sign, occurs as a consequence of
• Jugular Veins
increased pressure in the hepatic veins and the
o Provides an estimation of right atrial pressure veins draining the peritoneum
• Pulmonary Examination
o Pulmonary crackles (rales and crepitations)
result from the transudation of fluid from the
intravascular space into the alveoli
▪ Crackles on the later part of inspiration
(Px may sometimes present with
Ronchi or Wheezes)
▪ In asthmatic Px usually presents early,
if asthma seems to develop (i.e 50-60
y/o), look for risk factors of HF because
of what we call Cardiac Wheeze
/(expiratory wheezing or Cardiac
asthma), secondary to HF. • Extremities
o Peripheral edema is a cardinal manifestation of
HF, but it is non-specific
o Symmetric and dependent in HF
o Occurs predominantly in the ankles and the
periorbital region in ambulatory patients
INTERNAL MEDICINE II Milanes, Gwapo Marquez 5 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
o In the sacral area (presacral edema) and the
scrotum in bedridden patients.
• Cardiac Cachexia
o In severe chronic HF, there may be marked
weight loss and cachexia
o Cause maybe multifactorial
o When present, cachexia augurs a poor overall
prognosis. o Cardiac MRI
35:20 ▪ Provides a comprehensive analysis of
cardiac anatomy and function and is
H. Diagnosis now the gold standard for assessing
LV mass and volumes.
• Key to making the diagnosis is to have a high index of
suspicion, particularly for high-risk patients.
• Routine Laboratory Testing:
o CBC (complete Blood Count)
o Electrolytes
o BUN (Blood Urea Nitrogen)
o Serum Creatinine
o Hepatic Enzymes
o Urinalysis
• ECG
o To assess cardiac rhythm and determine the
presence of LV hypertrophy or a prior MI
(presence or absence of Q-waves) as well as to
determine QRS width to ascertain whether the
patient may benefit from resynchronization • EF: most useful index of LV function
therapy. • Stroke volume ÷ EDV
• Normal EF (≥ 50%)- systolic function is
usually adequate
• Significantly depressed EF (<40%) –
contractility is usually depressed
• Biomarkers
o BNP and NT-proBNP
▪ Released from the failing heart
▪ Relatively sensitive markers for the
• Chest X-ray
o Provides useful information about cardiac size
and shape, as well as the state of the pulmonary
vasculature, and may identify non-cardiac causes
of the patient’s symptoms.
• Non-invasive cardiac imaging presence of HF with depressed EF
o Essential for the diagnosis, evaluation,
and management of HF • Treadmill or bicycle exercise testing
o 2D echo o Not routinely advocated
▪ Provide a semi-quantitative o Useful for assessing the need for cardiac
assessment of LV size and transplantation in patients with advanced HF
function as well as the presence o Peak oxygen uptake (VO2) <14mL/Kg per min. →
or absence of valvular and/or relatively poor prognosis
regional wall motion o Better survival when transplanted than when
abnormalities treated medically.
INTERNAL MEDICINE II Milanes, Gwapo Marquez 6 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
• IV Diuretic Agents
o Rapidly and effectively relieves symptoms of
congestion
o Essential when oral drug absorption is impaired
o Continuous infusion may be needed to reduce
toxicity and maintain stable serum drug levels.
• Cardiorenal Syndrome
o Being recognized increasingly as a complication
of ADHF
o Reflects the interplay between abnormalities of
the heart and kidney function, with deteriorating
function of one organ while therapy is
administered to preserve the other.
I. Management • Ultrafiltration
Heart Failure with preserved ejection fraction o An invasive fluid removal technique that may
• Therapeutic targets supplement the need for diuretic therapy
o Control of congestion o Controlled rates of fluid removal, neutral effects
o Stabilization of heart rate and blood pressure on serum electrolytes, and decreased
o Improve exercise tolerance neurohormonal activity
• Clinical Pearls: o Referred to as aquapheresis in recognition of its
o Even as efforts to control hypertension in HFpEF electrolyte depletion-sparing effects.
are critical • Vascular therapy
o Evaluation for and correction of underlying o Vasodilators including intravenous nitrates,
ischemia may be beneficial. nitroprusside, and neseritide (a brain type
o Appropriate identification and treatment of natriuretic peptide) have been advocated for
sleep disordered breathing should be strongly upstream therapy in an effort to stabilize ADHF.
considered. • Inotropic Therapy
o Excessive decrease in preload with vasodilators o Impairment of myocardial contractility often
may lead to underfilling the ventricle and accompanies ADHF.
subsequent hypotension and syncope. o Pharmacologic agents that increase intracellular
concentrations of CAMP via direct or indirect
Acute Decompensated Heart Failure pathways
• General Principle o Sympathomimetic amines (dobutamine) and
o A heterogenous clinical syndrome most often phosphodiesterase-3 inhibitors (milrinone)
resulting in need for hospitalization due to
confluence of interrelated abnormalities of Heart Failure with reduced ejection fractions
decreased cardiac performance, renal • ACEIs and beta blockers
dysfunction, and alterations in vascular o Cornerstone of pharmacotherapy
compliance. • Attenuation of decline and improvement in cardia
o Half of these readmitted for management w/in 6 structure and function with consequent reduction in
months symptoms.
o High short-term mortality (5-8% in-hospital) • Neurohormonal Antagonism
o High long-term mortality (20% at 1 year) o 23% reduction in mortality
o The management of these patients has remained o 35% reduction in the combination endpoint of
difficult and principally revolves around volume mortality and hospitalizations for heart failure in
control and decrease of vascular impendence patients treated with ACEIs
while maintaining attention to end-organ o With beta blockers provide a further 35%
perfusion (coronary and renal) reduction in mortality on top of the benefit
• Identify and tackle known precipitants of decompensation provided by ACEIs alone.
(1st principle) • Mineralocorticoid Antagonists
o Medication nonadherence o Aldosterone antagonism – reduction in mortality
o NSAID use in all stages of symptomatic NYHA class II to IV
o Cold and flu preparations with cardiac stimulants HFrEF.
o Herbal preparations, (licorice, ginseng and ma o Elevated aldosterone promote sodium retention,
huang) electrolyte imbalance, and endothelial
• Routine use of pulmonary artery catheter is NOT dysfunction and may directly contribute to
recommended myocardial fibrosis.
• Restricted to those who respond poorly to diuresis or o Eplerenone (tested in NYHA class II and post-
experience hypotension or signs and symptoms suggestive myocardial infraction heart failure) *lesser side-
of low CO where therapeutic targets are unclear. effect than spironolactone
INTERNAL MEDICINE II Milanes, Gwapo Marquez 7 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
o Spironolactone (tested in NYHA class III and IV o Potent lipid-altering and pleiotropic effects of
heart failure) *side-effect: gynecomastia (in statins, reduce major cardiovascular events and
males), can also cause menstrual abnormalities improve survival in non-heart failure
(in females) *K+ sparring diuretics populations.
o Reduced mortality and hospitalizations, with o Once heart failure is well established, this
significant reductions in SCD. therapy may not be as beneficial and
• RAAS therapy and Neurohormonal “Escape” theoretically could even be detrimental by
o Neurohormonal “escape” has been witnessed in depleting ubiquinone in the electron transport
patients with HFrEF by finding that circulating chain.
levels of angiotensin II return to pretreatment o If statins are required to treat progressive
levels with long-term ACEI therapy coronary artery disease in the background
o ARBs blunt this phenomenon by binding setting of heart failure, then they should be
competitively to the ATI receptor. employed.
• Arteriovenous Vasodilation o However, no rationale appears to exist for
o Hydralazine + nitrates = improved survival in routine statin therapy in nonischemic heart
HFrEF failure.
o Hydralazine – reduces systemic vascular • Anticoagulation Antiplatelet
resistance and induces arterial vasodilation by o HFrEF – accompanied by a hypercoagulable state
affecting intracellular calcium kinetics and therefore a high risk of thromboembolic
o Nitrates – transformed in smooth muscle cells events, including stroke, pulmonary embolism,
into nitric oxide, which stimulates CGMP and peripheral arterial embolism.
production and consequent arterial-venous o Although long-term oral anticoagulation is
vasodilation. established in certain groups, including patients
o This combination improves survival, but not to with atrial fibrillation,
the magnitude evidenced by ACEIs or ARBs ▪ The data are insufficient to support the
• Heart Rate Modifications use of warfarin in patients in normal
o Ivabradine – and inhibitor of the If current in the sinus rhythm without a history of
sinoatrial node, slows the heart rate without a thromboembolic events or
negative inotropic effect. echocardiographic evidence of left
• Digoxin ventricular thrombus.
o Mild inotropic effect, attenuate carotid sinus ▪ High risk patients (HF with evidence of
baroreceptor activity, and are atrial fibrillation may be needed to be
sympathoinhibitory.
o Decrease serum norepinephrine levels, plasma
renin levels, and possibly aldosterone levels.
o For patients who remain profoundly
symptomatic despite optimal neurohormonal
blockade and adequate volume control
o *beneficial specially to px with reduced ejection
fraction
• Oral Diuretics
o Loop diuretic agents are often required because
of their increased potency and frequent dose
adjustments may be necessary because of
variable oral absorption and fluctuations in renal
function. given anticoagulation therapy
• Calcium Channel Antagonists “CHA2DS2-VASc scoring” can help
o Amlodipine and felodipine (second generation guide in decision making.
agents) • Fish oil
▪ safely and effectively reduce blood o Long-cahin omega-3 polyunsaturated fatty acids
pressure in HFrEF but do not affect (ω-3 PUFAs) – modestly improved clinical
morbidity, mortality, or quality of life. outcomes in patients with HFrEF. (GISSI-HF trial)
(may be given because they don’t have o Three-month treatment with ω-3 PUFAs
inotropic effect) enriched circulating eicosapentaenoic acid (EPA)
o Verapamil and diltiazem (first generation agents) and docosahexaenoic acid (DHA)
▪ May exert negative inotropic effects o Low EPA levels are inversely related to total
and destabilize previously mortality in patients with HFrEF.
asymptomatic patient. (*we don’t give • Cardiac Resynchronization Therapy (CRT)
in HFrEF because of inotropic effect) o Nonsynchronous contraction between the walls
• Statins of the left ventricle (intraventricular) or between
INTERNAL MEDICINE II Milanes, Gwapo Marquez 8 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
the ventricular chambers (interventricular)
impairs systolic function, decreases mechanical
efficiency of contraction, and adversely affects
ventricular filling
o The single most important association of extent
of dyssynchrony is a widened QRS interval on
the surface electrocardiogram, particularly in the
presence of a left bundle branch block pattern.
o With placement of a pacing lead via the coronary
sinus to the lateral wall of the ventricle, cardiac
resynchronization therapy (CRT) enables a more
synchronous ventricular contraction by aligning the
timing of activation of the opposing walls.
• Surgical Therapy in Heart Failure
o CORONARY ARTERY BYPASS GRAFTING (CABG)
is considered in patients with ischemic
cardiomyopathy with multivessel coronary heart
disease.
o Saphenous vein – grafted vein
o Note: grafts can still be blocked and are checked
via angiogram.
o The recognition that hibernating myocardium,
defined as myocardial tissue with abnormal
function but maintained cellular function, could
recover after revascularization led to the notion
that revascularization with CABG would be
useful in those with living myocardium.
o Revascularization is most robustly supported in
individuals with ongoing angina and left
ventricular failure.
o SURGICAL VENTRICULAR RESTORATION (SVR)
▪ A technique characterized by infarct
exclusion to remodel the left ventricle
by reshaping it surgically in patients
with ischemic cardiomyopathy and
dominant anterior left ventricular
dysfunction.
DISEASE MANAGEMENT AND SUPPORTIVE CARE
• Despite stellar outcomes with medical therapy, admission
rates following heart failure hospitalization remain high,
with nearly half of all patients readmitted to hospital
within 6 months of discharge.
• The key to achieving enhanced outcomes must begin with
the attention to transitional care at the index
hospitalization with facilitated discharge through
comprehensive discharge planning, patient and caregiver
education, appropriate use of visiting nurses and planned
follow-up.
• Advise the patient regarding medication, fluid intake
(usually 1.5-2L of water a day), avoid salts, and reminder
of medications.
INTERNAL MEDICINE II Milanes, Gwapo Marquez 9 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
Atrial Size Increased, may Increased; Increased;
OUTLINE also be may be related to
I. Cardiomyopathy primarily massive elevated
A. Dilated Cardiomyopathy affected filling
B. Restrictive Cardiomyopathy pressures
C. Hypertrophic Cardiomyopathy Valvular Related to Related to Related to
D. Myocarditis regurgitations annular endocardial valve-septum
dilation; mitral involvement; interaction;
appears earlier frequent mitral
I. CARDIOMYOPATHY during mitral and regurgitation
• Definition decompensatio tricuspid
o Disease of the Heart Muscle n; tricuspid regurgitation
o “a heterogenous group of diseases of the regurgitation , rarely
myocardium associated with mechanical an/or with right severe
electrical dysfunction that usually (but not ventricular
invariably) exhibit inappropriate ventricular dysfunction
hypertrophy or dilatation and are due to a Common first Exertional Exertional Exertional
variety of causes that frequently are genetic” symptoms intolerance intolerance, intolerance;
• General Clinical Presentation fluid may have
o Exertional intolerance with breathlessness and retention chest pain
fatigue early, may
o Fluid retention (shortness of breath, dyspnea or have
cough in supine) dominant
o AV valve regurgitation right-sided
o Chest pain symptoms
o Atrial and Ventricular tachyarrhythmias Congestive Left before Right often Left-sided
o Embolic events symptoms right, except dominates congestion at
right prominent rest may
A. DILATED CARDIOMYOPATHY in young adults develop late
• Enlargement of the left ventricle with decreased systolic Arrhythmias Ventricular Ventricular Ventricular
function as measured by left ventricular ejection fraction tachyarrhythmi uncommon tachyarrhyth
• 1/3 of cases may be familial a; conduction except in mias; atrial
• Acquired cardiomyopathy attributed to infection or toxin block in Chaga’s sarcoidosis, fibrillation.
exposure disease, and conduction
Toxin exposure or viral infection some families. block in
↓ Atrial sarcoidosis
Some myocytes die during initial injury, some die later by fibrillation. and
apoptosis amyloidosis.
↓ Atrial
Surviving myocytes hypertrophy fibrillation
↓
Local and circulating factors stimulate deleterious response A.1. CAUSES/ETIOLOGY
↓ • Infection (myocarditis)
Dynamic remodeling of interstitial scaffolding • Toxic – environmental and pharmacologic agents
o Alcohol is the most common
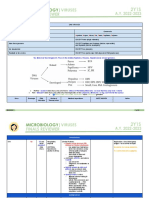
Table 254-1 Presentation with Symptomatic Cardiomyopathy o Diastolic dysfunction, mild ventricular dilation,
Dilated Restrictive Hypertrophic subclinical dilation seen before development of
Ejection Usually <30% 25-50% >60% clinical HF
fraction when o Atrial fibrillations are common
(normal symptoms are o Marked improvement can occur within 3 – 6
>55%) severe months of abstinence
Left ≥ 60 mm <60mm (may Often o Cocaine, amphetamines and related
ventricular be decreased catecholaminergic stimulants
diastolic decreased) • Chemotherapy are most common drugs implicated
dimension anthracyclines
(normal o Acute heart failure
<55mm) o Doxorubicin cardiotoxicity
Left Normal or Normal or Markedly • Trastuzumab – incidence is lower, cardiotoxicity not
Ventricular decreased increased increased always resolve
wall thickness
INTERNAL MEDICINE II Milanes, Gwapo Marquez 10 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
• Cyclophosphamide and ifosfamide – acutely and with very • Ventricle shows global ventricular dilation with basal
high doses. contraction, forming the shape of the narrow-necked jar
• Metabolic (tako-tsubo)
o Hyperthyroidism • Presentations:
o Hypothyroidism o Pulmonary edema, hypotension, and chest pain
o Pheochromocytoma with ECG changes mimicking an acute infraction.
• Nutritional deficiencies
o Beri-beri deficiency
• Hemochromatosis A.4. IDIOPATHIC DILATED CARDIOMYOPATHY (Idiopathic DCM)
• Diagnosis of exclusion
Examples of inherited defects in metabolic pathways associated with • 2/3 of dilated cardiomyopathies are still labeled as
cardiomyopathy, usually restrictive or psueudohypertrophic idiopathic
phenotype. (Table 238-4) Harrison’s 19th ed. • however, a substantial proportion of these may reflect
unrecognized genetic disease.
• Glycogen storage diseases • Continued reconsideration of etiology during chronic heart
o II- Pompe’s (alpha 1,4 glucosidase failure management often reveals specific causes later in a
o III – Forbes: de-branching enzyme (amylo 1,6 patient’s course.
glucosidase)
• Glucose metabolism (Defective PRKAG2) MAJOR CAUSES OF DILATED CARDIOMYOPATHY
o Fatty acid metabolism • Inflammatory Myocarditis (INFECTIVE)
▪ Carnitine transport defect o Viral (coxsackie, adenovirus, HIV, hepatitis C)
▪ Medium chain Acyl-CoA o Parasitic (T.cruzi – Chaga’s disease,
dehydrogenase toxoplasmosis)
▪ Long-chain Acyl-CoA dehydrogenase o Bacterial (diphtheria)
o Sphingolipidoses o Spirochetal (Borellia burdorferi – Lyme disease)
▪ Fabry’s disease (alpha galactosidase A) o Ricketsial (Q fever)
▪ Gaucher disease (beta- o Fungal (with systemic infection)
glucocerebroside) • Inflammatory Myocarditis (NON-INFECTIVE)
o Disorders of lysosomal function o Granulomatous inflammatory disease
▪ Danon’s disease – (lysosome- ▪ Sarcoidosis
associated membrane protein, LAMP2) ▪ Giant cell myocarditis
o Miscellaneous o Hypersensitivity myocarditis
▪ Hemochromatosis – Fe metabolism o Polymyositosis, dermatomyositis
▪ Familial amyloidosis – abnormal o Collagen vascular disease
transthyretin o Peripartum cardiomyopathy
▪ Barth syndrome – tafazzin defect o Transplant rejection
affecting cardiolipin • Metabolic
▪ Friedreich’s ataxia – frataxin o Nutritional deficiencies: thiamine, selenium,
carnitine
A.2. FAMILIAL DILATED CARDIOMYOPATHY o Electrolyte deficiencies: calcium, phosphate,
• Most recognizable familial syndromes are the muscular magnesium
dystrophies. o Endocrinopathy:
• Prominent family history of sudden death or ventricular ▪ Thyroid disease
tachycardia before clinical cardiomyopathy suggests ▪ Pheochromocytoma
genetic defects in the desmosomal proteins causing ▪ Diabetes
arrhythmogenic ventricular dysplasia o Obesity
o Defect in proteins of the desmosomal complex o Hemochromatosis
disrupt myocyte junction and adhesions, leading • Familial
to replacement of myocardium by deposits of o Skeletal and cardiac myopathy
fat. o Dystrophin-related dystrophy (Duchenne’s,
*There arrhythmogenic right ventricular dysplasia – due to lipid Becker’s)
deposition at the right ventricle, which causes arrythmias. o Mitochondrial myopathies (e.g. Kearns-Sayre
syndrome)
A.3. TAKO-TSUBO CARDIOMYOPATHY o Arrhythmogenic ventricular dysplasia
*broken heart syndrome o Hemochromatosis
• Apical ballooning syndrome, or stress-induced o Associated with other systemic diseases
cardiomyopathy, occurs typically in older women after o Susceptibility to immune-mediated myocarditis
sudden intense emotional or physical stress. • Toxic
o Alcohol
o Catecholamines: amphetamines, cocaine
INTERNAL MEDICINE II Milanes, Gwapo Marquez 11 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
o Chemotherapeutic agents (anthracyclines,
trastuzumab)
o Interferon
o Other therapeutic agents (hydroxychloroquine,
chloroquine)
o Drugs of misuse (emetine, anabolic steroids)
o Heavy metals: lead, mercury
o Occupational exposure: hydrocarbons, arsenicals
• Overlap with restrictive cardiomyopathy
o Minimally dilated cardiomyopathy
o Hemochromatosis
o Amyloidosis
o Hypertrophic cardiomyopathy (“burned-out”)
• “Idiopathic”
• Miscellaneous (Shared Elements of Above etiologies)
o Arrhythmogenic right ventricular dysplasia (may
also affect left ventricle)
o Left ventricular noncompaction
o Peripartum cardiomyopathy
B. RESTRICTIVE CARDIOMYOPATHY
• Dominated by abnormal diastolic function, often with
mildly decreased contractility and ejection fraction
• Both atria are enlarged, sometimes massively
• Modest left ventricular dilation can be present, end
diastolic dimension <6 cm.
• End diastolic pressure are elevated. C. HYPERTROPHIC CARDIOMYOPATHY
• Exercise intolerance is usually the first symptom
• Marked left ventricular hypertrophy in the absence of
• More of right sided symptoms
other causes such as hypertension and valve disease.
• Cardiac impulse less displaced and less dynamic
• The systolic function as measured by ejection fraction
• 4th heart sound more common more than the 3 rd heart
often supra-normal.
sound in sinus rhythm (atrial gallop)
• Hypertrophy may be asymmetric involving the septum
• JVP (Jugular Venous Pulse waves) shows rapid y descents
more than free wall of the ventricles.
• Prevalence 1:5000 adults. (Prevalence in N. America,
Africa, and Asia Is about 1:500. It is the leading cause of
sudden death in the young and is an important cause of
HF)
• Characterized hemodynamically by diastolic dysfunction,
originally attributed to the hypertrophy, fibrosis, and
intraventricular gradient when present.
C.1. EPIDEMIOLOGY
• Between 20-40 years old
• Dyspnea on exertion
• Chest pain with either an atypical or typical exertional
pattern
and may increase during inspiration • Palpitations
A-Atrial contraction (RA) • First manifestations maybe “SUDDEN CARDIAC DEATH”
X-atrial relaxation
C-Closure of tricuspid valve (bulging of tricuspid valve with C.2. DIAGNOSIS
ventricular contraction) • Harsh murmur – Left lower sternal border
V-Villing (fillng) of RA (blood from Vena cavae) • Fourth heart sound can be heard
Y-atrial emptying with opening of tricuspid valve • Palpation of the carotid pulse may reveal a bifid systolic
impulse
• Systemic fluid retention
C.3. TREATMENT
• Beta-adrenergic blocking drugs and verapamil
o Most commonly used initial therapy
INTERNAL MEDICINE II Milanes, Gwapo Marquez 12 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
• Diuretic therapy • Almost half will have major improvement in left
o If with fluid retention ventricular ejection fraction during the subsequent 6-12
• Anti coagulation months. (Check again with 2-D echo in 6-12 mos. for
• Disopyramide evaluation)
• Amiodarone – for arrhythmias
D.1.2. PARASITIC MYOCARDITIS
D. MYOCARDITIS • CHAGA’S DISEASE
• Refers to the inflammation, necrosis or myocytolysis of o Protozoan Trypanosoma cruzi
o Third most common parasitic infection in the
myocardial cells.
world and the Most common cause of
• Most commonly attributed to infectious organisms that
cardiomyopathy.
can invade the myocardium directly, produce cardiotoxins,
o Acute phase
and trigger chronic inflammatory responses.
▪ Unrecognized, with nonspecific
symptoms or occasionally with acute
D.1. INFECTIVE MYOCARDITIS
myocarditis and meningiencephalitis
• Viral Myocarditis (Most common)
o Silent stage
• Parasitic Myocarditis
▪ Progresses slowly over 10-30
• Bacterial Infections
• Manifest in the cardiac and
• Other Infections:
gastrointestinal systems in
o Spirochetes
the chronic stages.
o Fungal
▪ (>10-30 years in almost half of
o Rickettsial patients to manifest chronically in the
cardiac and gastrointestinal systems)
o Mostly in Africa
D.1.1. VIRAL MYOCARDITIS
• Features typical of Chaga’s disease:
VIRAL MYOCARDITIS
o Conduction system abnormalities
• Viral invasion and replication lead directly to myocardial
▪ Sinus node and atrioventricular (AV)
injury and lysis.
node dysfunction
• Proteases degrade the protein, dystrophin, in the myocyte ▪ Right bundle branch block
membrane complex that is genetically abnormal in some o Atrial fibrillation
muscular dystrophies. o Ventricular tachyarrhythmias
• Picornavirus, Enterovirus, Coxsackie, echovirus, poliovirus, o Small ventricular aneurysms (apex)
Influenza, mumps, respiratory syncytial virus, arboviruses o Dilated ventricles giving rise to pulmonary and
(dengue fever and yellow fever), and arenaviruses (Lassa systemic emboli.
fever) • African trypanosomiasis infection
CLINICAL PRESENTATIONS: o Tsetse fly bite
• Progressive dyspnea and weakness o West African form is caused by Trypanosoma
• Chest pain brucei gambiense and progresses silently over
• Tachyarrhythmias years.
ACUTE FULMINANT MYOCARDITIS o East African form caused by T. brucei
• Rapid progression from severe febrile respiratory rhodesiense
syndrome to cardiogenic shock from multiple organ ▪ Progress rapidly through perivascular
system failure. infiltration to myocarditis and heart
LAB TESTS: failure, with frequent arrhythmias.
• Echocardiography • TOXOPLASMOSIS
• Troponin and Creatine Kinase o May present with encephalitis or chorioretinitis,
o Mildly elevated and in the heart can cause myocarditis,
• MRI pericardial effusion, constrictive pericarditis, and
• Endomyocardial biopsy (most ideal; but limited in the heart failure.
Philippines) o Therapy:
o Lymphocytic infiltration with evidence of ▪ Pyrimethamine and sulfadiazine or
myocyte necrosis; fulminant myocarditis-marked clindamycin.
tissue edema without a cellular infiltrate • TRICHINELLOSIS
MANAGEMENT and TREATMENT o Trichinella spiralis larva ingested with
• Stabilizing the hemodynamic status and then toward undercooked meat
adjusting neurohormonal antagonists for the treatment of o Myalgias, weakness, fever, periorbital and facial
heart failure edema, and conjunctival and retinal
• Resolve spontaneously, while others progress to hemorrhage.
cardiomyopathy without other obvious cause. o May “occasionally” invade the myocardium
o Diagnosis:
INTERNAL MEDICINE II Milanes, Gwapo Marquez 13 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
▪ Specific serum antibody o Involve the myocardium directly as well as
▪ Supported by the presence of through tuberculous pericarditis
eosinophilia o Rarely does so when the disease is treated with
o Treatment: antibiotics
▪ Anthelminthic drugs and • WHIPPLE’S DISEASE
glucocorticoids. (steroids) o Caused by Tropheryma whippleii
o Usual manifestations are in the gastrointestinal
D.1.3. BACTERIAL MYOCARDITIS tract, but pericarditis, coronary arteritis, valvular
• Direct invasion and abscess formation (rare) lesions, and occasionally clinical heart failure
• Contractility is depressed globally in severe infection and may also occur.
sepsis through systemic inflammatory responses (more • OTHER INFECTIONS:
common) o Spirochetal myocarditis
▪ Lyme carditis
• DIPHTHERIA ▪ Most often presents with arthritis and
o Specifically affects the heart (in almost half of conduction system disease
the cases) and is the ▪ Resolves within 1-2 weeks of antibiotic
o Most common cause of death in patients with treatment
this infection ▪ Only rarely causing clinical heart
o Releases a toxin that impairs protein synthesis failure.
and may particularly affect the conduction o Fungal myocarditis
system. ▪ Hematogenous or direct spread
o Specific antitoxin should be administered as ▪ Aspergillosis, actinomycosis,
soon as possible, with higher priority than blastomycosis, candidiasis,
antibiotic therapy. coccidiodomycosis, cryptococcosus,
o The prevalence of vaccines has shifted the histoplasmosis, and mucormycosis.
incidence of diphtheria from children to ▪ Cardiac infection is rare.
countries without routine vaccination and older o Rickettsial infections
immunocompromised populations. ▪ Q fever, Rocky Mountain spotted
o Other systemic bacterial infections: brucellosis, fever, and scrub typhus.
Chlamydophila, legionella, meningococcus, ▪ Accompanied by ECG changes, but
mycoplasma, psittacosis, and salmonellosis most clinical manifestations relate to
• CLOSTRIDIAL INFECTIONS systemic vascular involvement.
o Cause myocardial damage from the released
toxin D.2. NON-INFECTIVE MYOCARDITIS
o “Gas bubbles” detected in the myocardium • Cardiac Transplantation Rejection
o Occasionally abscesses can form in the • The most commonly diagnosed non infective inflammation
myocardium and pericardium is granulomatous myocarditis. (Includes sarcoidosis and
• STREPTOCOCCAL INFECTION giant cell myocarditis)
o Β-hemolytic streptococci • Granulomatous myocarditis (sarcoidosis)
o Most commonly associated with acute • Giant cell myocarditis
rheumatic fever (use of Jones Criteria, look o Less common (10-20% of biopsy- positive cases
below) of myocarditis)
o Characterized by inflammation and fibrosis of • Hypersensitivity myocarditis
cardiac valves and systemic connective tissue o Antibiotics (chronic)
o Can also lead to a myocarditis with focal or o Thiazides
diffuse infiltrates of mononuclear cells o Anticonvulsants
o Indomethacin
o And methyldopa
• Polymyositosis and dermatomyositis
• Mild symptoms:
o have better prognosis; complete resolution has
been described
• Patients who have progressed to chronic myocarditis:
o Dilated cardiomyopathy
• TUBERCULOSIS
INTERNAL MEDICINE II Milanes, Gwapo Marquez 14 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
OUTLINE
I. Introduction and review
II. Mitral stenosis
III. Mitral regurgitation In patient with mitral stenosis,
In mitral regurgitation, during
IV. Aortic stenosis narerestrict yung flow ng blood
contraction, the blood goes
V. Aortic regurgitation from left atrium towards left
back to the left atrium instead
VI. Tricuspid stenosis ventricle; both side gets
of the aorta; both sides gets
VII. Tricuspid regurgitation enlarged; causes pulmonary
enlarged
VIII. Pulmonic stenosis congestion
IX. Pulmonic regurgitation Aortic stenosis – the left
ventricle and left atrium gets
Aortic regurgitation – all sides
I. INTRODUCTION AND REVIEW enlarged; can also cause
can also get enlarged
• On the right side of the heart there is tricuspid and then pulmonary congestion; even
pulmonary valve. the right side gets enlarged
• On the left side is mitral then aortic valve. Pulmonic regurgitation – right
Tricuspid stenosis – only right
• During systole, closing of mitral and tricuspid valve and ventricle and right atrium gets
atrium gets enlarged
opening of aortic and pulmonic valve. enlarged
• During diastole, closing of aortic and pulmonic valve and
opening of mitral and tricuspid valve. (Diastole more on II. MITRAL STENOSIS
ventricular filling) • Etiology:
o Rheumatic fever: leading cause
o JONES criteria (Joints, Heart, Nodules, Erythema
marginatum, Syndenham chorea)
o History of tonsilitis after 10-14 days there would be
symptoms included in the JONES criteria
o Congenital Mitral Stenosis: Parachute abnormalities;
magkadikit yung papillary muscles
o Cor Triatriatum: abnormal membrane obstructing the
mitral valve
o Mitral annular calcification: annulus is a saddle-shaped
structure that supports the leaflets of the mitral valve
o SLE – Butterfly rash, Raynaud’s, Pericarditis
o Libman-Sacks Endocarditis: valvular lesion in SLE
o Rheumatoid arthritis: lung lesions; uncommon
2D ECHO o Left atrial myxoma: usually attached at the septal side
• Transthoracic o Solitary, mobile masses that are heterogeneously
hyperechoic.
• PLAX view: Apex towards the base view; beside the sternum
o Prolapses during diastole
• PSAX view: Transverse cut view; beside the sternum
o Arise most commonly from the interatrial septum
• Apical 4 chamber view: Compare the 4 chambers of the heart
and have a predilection for the left atrium
• Apical 2 chamber view: Left atrium and Left ventricle only
o Infective endocarditis with large vegetations
• Apical 5 chamber view: Aorta is included
o Vegetations can attach on the atrial surface of the
• Subcostal position: allows multiple short axis views; below the mitral valve
xiphoid process
o Symptoms: intermittent fever, new murmur,
• Transesophageal Echocardiography (TEE): view of the spontaneous HF, peripheral signs (osler’s nodes,
posterior part of the heart Janeway lesions)
Congenital Mitral Stenosis
A. Major Categories of Valve Problems
1. Stenosis – valves does not open all the way for the blood
to pass through
2. Regurgitation – valve does not close all the way so blood
leaks backwards or backflow
• Pure or predominant MS
o 40% of all patients with rheumatic disease and a
history of RF
INTERNAL MEDICINE II Milanes, Gwapo Marquez 15 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
• May accompany mitral regurgitation and aortic valve disease o Advance the catheter into the RA, RV, PA, and then
• 3 valves commonly involved in RHD: mitral valve, aortic valve “wedge” it into a branch of the pulmonary artery (lung
and tricuspid valve bed)
• The wedged catheter cuts off PA flow and the end hole lumen
PATHOPHYSIOLOGY measures pressures through the capillary bed to the LA
o Valve leaflets are thickened by fibrous tissue or calcific • PCWP provides an indirect estimate of left atrial pressure
deposits (LAP) and Left ventricular end diastolic pressure (LVEDP)
o Mitral commissures fuse • It can be directly measured by placing a catheter within the
o Chordae tendineae fuse and shorten left ventricle
o Narrowing at the apex of the funnel shaped valve o It is not feasible to advance this catheter back into the
▪ fish mouth appearance left atrium
o 2D Echo: • Simultaneous PCWP and LV pressure measures if there are
▪ Mitral Stenosis Severity based on the size of the any gradient between them
valve:
Normal 4.0-6.0 cm Transvalvular pressure gradient
Mild 1.6-2.0 cm • When mitral stenosis is present, there is a diastolic pressure
Moderate 1.1-1.5 cm gradient between the PCW or LAP and LV
o LA pressure of ∼25 mmHg is required to maintain a
Severe <1.0 cm
normal cardiac output (CO)
o Moderate MS: Cardiac output (CO) is normal or almost so o To assess the severity of obstruction hemodynamically,
at rest, but rises sub normally during exertion. both the transvalvular pressure gradient and the flow
o Severe MS: particularly those in whom pulmonary vascular rate must be measured
resistance is markedly elevated, the CO is subnormal at rest • Significance: can be used for mitral valve operation; to check
and may fail to rise or may even decline during activity. whether intervention was effective
• Flow rate depends on the CO and the heart rate
• Increase in heart rate shortens diastole proportionately more
than systole and diminishes the time available for flow across
the mitral valve.
• Tachycardia and rapid AF augments transvalvular pressure
gradient → further elevates LA pressure
Note: In the presence of significant obstruction, i.e., when the orifice
area is reduced to <2 cm, blood can flow from the LA to the LV only if
propelled by an abnormally elevated left atrioventricular pressure
gradient, the hemodynamic hallmark of Mitral Stenosis.
SYMPTOMS
• Dyspnea and cough (Initial manifestations)
• Orthopnea (As the MS progress)
• Paroxysmal nocturnal dyspnea (As the MS progress)
o Due to congestion, edema and fibrous thickening of the
walls of the alveoli and pulmonary capillaries the lung
• ↑ LA pressure > enlarged LA and ↑ pulmonary venous capacity is reduced hence the patient develops the lung
pressure (pulmonary congestion or edema) > ↑ pulmonary symptoms. These changes somehow put the patient in
wedge pressure > ↑ PA pressure > ↑ pulmonary vascular high risk of recurrent pulmonary emboli and infection if
resistance > Dilated RV > hypertrophy > heart failure MS remains untreated
o Wedge pressure yung pinakadulo na naaabot ng catheter • Hemoptysis
• Pulmonary regurgitation o Rupture of pulmonary-bronchial venous connections
• Tricuspid valve dilation > Tricuspid regurgitation > secondary to pulmonary venous hypertension
• Right sided heart failure (Hepatomegaly (dilation of Glisson’s o Occurs most frequently in patients who have elevated LA
capsule), Splenomegaly) pressures without markedly elevated pulmonary
• Diastolic pressure gradient: between the pulmonary capillary vascular resistances and this is rarely fatal
wedge or left atrial pressure and the left ventricle • Permanent Atrial Fibrillation
o Formation of thrombus usually occurs in the left atrial
Pulmonary Artery Wedge Pressure (PAWP) or Pulmonary appendage (pockets)
Capillary Wedge Pressure (PCWP) o turning point in the patient’s course
• It is measured by allowing a balloon-tipped, multi-lumen o enlarged LA
catheter (Swan-Ganz catheter) by inserting into a peripheral o acceleration of the rate at which symptoms progress
vein (e.g., jugular or femoral vein) o Systemic embolization occurs more frequently in
patients with AF, >65 years of age and reduced cardiac
output
INTERNAL MEDICINE II Milanes, Gwapo Marquez 16 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
• Plum-colored malar flush (facial features) o Color flow imaging provides information about the
o Occurs when CO is low and pulmonary hypertension is direction of blood flow, its velocity, and the presence of
severe turbulence.
o rose color is because of the dilatation of malar • Chest X-ray
capillaries due to cutaneous vasodilation; o Straightening of the upper left border of the cardiac
o the bluish tinge is because of the cyanosis due to chronic silhouette
hypoxemia o Prominence of the main pulmonary arteries
o Dilation of the upper lobe pulmonary veins
• Pr o minent a wave reflects i ncreased right atrial pressure o Posterior displacement of the esophagus by an enlarged
LA
from pulmonary hypertension and right ventricular failure.
o Normal to slightly enlarged heart
• Pr o minent v wave is seen with tricuspid regurgitation. o Equalization or cephalization of pulmonary blood flow
o Small aorta
PHYSICAL FINDINGS o Kerley B lines are a sign seen on chest radiographs with
• Inspection and Palpation interstitial pulmonary edema
o Systemic arterial pressure is usually normal or slightly
low Review: Normal LAA area – flat or slightly concave
o RV tap along the left sternal
o Diastolic thrill- rarely be present at the cardiac apex
o Hepatomegaly, ankle edema, ascites, and pleural
effusion (right), may occur in patients with MS and RV
failure
• Auscultation
o Normally, mitral valve is louder in S1 than S2 at apex; sa
base S1 is softer than S2
o Accentuated S1 early in mitral stenosis
o Soft S1 in severe mitral stenosis
o P2 (pulmonic) component of the second heart sound (S2)
will be loud if severe pulmonary hypertension is due
to mitral stenosis
o Close fixed splitting of S2: both on inspiration and
expiration may splitting
▪ Kapag wide fixed splitting sa ASD na yon
o Interval between A2 and OS varies inversely with the
severity of the MS
▪ Becomes wide; Higher left atrial pressure of severe
MS causes earlier MV opening and later closure of
the MV
o Low-pitched, rumbling, diastolic murmur, heard best at
the apex with the patient in the left lateral recumbent
position, accentuated by mild exercise
• Best position for checking for MS: ask the patient to turn to a left
lateral decubitus position, or pwede ding hand lift papahawakan Figure 1.
yung daliri, or advice the patient to exhale deeply o Sub-valvular Apparatus (SVA) Pathology
Note: When cardiac output is markedly reduced in MS, the typical ▪ Degree of distortion of the sub-valvular apparatus
auscultatory findings, including the diastolic rumbling murmur, may ▪ Grade I: Mild; multiple, thickened, discrete chordae
not be detectable (Silent MS) were visible just below commissures
▪ Grade II: Moderate; thickened and fused chordae
LABORATORY EXAMINATION form two identifiable thick chords below
• ECG commissure
o P wave usually suggests LA enlargement ▪ Grade III: Severe; fused chordae appear as a single,
o P wave becomes tall and peaked in lead II thick chord below the commissure
o P wave upright in lead V 1 (severe pulmonary
hypertension or TS complicates MS) o Left Atrial Enlargement
o Right atrial (RA) enlargement
o QRS complex is usually normal
o Right-axis deviation and RV hypertrophy (severe
pulmonary hypertension)
o Color flow imaging in mitral stenosis. diastolic frame
from apical view recorded from a patient with MS
INTERNAL MEDICINE II Milanes, Gwapo Marquez 17 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
Figure 5. Posterior displacement and upliftment of left mainstem
Figure 2. Double density bronchus (walking man sign)
Figure 3. Upliftment of left mainstem bronchus and widening of o Right Ventricular Hypertrophy
carinal angle
o Right Atrial Enlargement
Figure 4. Lateral view: Prominent posterosuperior cardiac border
INTERNAL MEDICINE II Milanes, Gwapo Marquez 18 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
▪ Accentuation of pulmonary vascularity
o Favor atrial septal defect over MS
▪ Absence of LA enlargement and Kerley B lines
▪ Fixed splitting of S 2
▪ Grade 2 or 3 mid-systolic murmur at the mid to
upper left sternal border all
▪ ASD with large left-to-right shunts may result in
functional TS
Left Atrial Myxoma
o Similar in MS:
o Right Ventricular Enlargement ▪ Obstruct LA emptying
▪ Causing dyspnea
▪ Diastolic murmur
▪ Hemodynamic changes resembling those of MS
o Favor Left Atrial Myxoma
▪ Have features suggestive of a systemic disease
[weight loss, fever, anemia, systemic emboli, and
elevated serum IgG and interleukin 6 (IL-6)
concentrations]
▪ Auscultatory findings may change markedly with
body position
▪ The diagnosis can be established by the
demonstration of a characteristic echo-producing
mass in the LA with TTE.
TREATMENT
Figure 6. PA View: Rounding and upliftment of cardiac apex Coronary angiography is advisable preoperatively to identify
patients with critical coronary obstructions
o Men older than 40 years of age
o Women older than 45 years of age
o Younger patients with coronary risk factors
o Positive noninvasive stress tests for myocardial ischemia
Penicillin prophylaxis of group A -hemolytic streptococcal
infections
o Secondary prevention of rheumatic fever is important for
at-risk patients with rheumatic MS
Symptomatic patients
o Restriction of sodium intake
o Oral diuretics
o Beta blockers
o Nondihydropyridine calcium channel blockers
Figure 7. Lateral View: Retrosternal fullness (contact of anterior o Digitalis glycosides (AF)
cardiac border greater than 1/3 of the sternal length) o Warfarin (INR) of 2–3 (if with AF or a history of
thromboembolism)
DIFFERENTIAL DIAGNOSIS Mitral Valvotomy (Commissurotomy)
• Significant MR o indicated in symptomatic patients
o May also be associated with a prominent diastolic o NYHA Functional Class II–IV
murmur at the apex (antegrade transmitral flow) o isolated MS
o Diastolic murmur commences slightly later than in o < ∼1 cm 2/m 2 body surface area
patients with MS o <1.5 cm 2 in normal-sized adults
o Evidence of LV enlargement o Mitral valvotomy can be carried out by two techniques:
o Opening snap and increased P2are absent ▪ PMBV
o S 1 is soft or absent ▪ Surgical valvotomy
o Apical pansystolic murmur of at least grade III/VI Mitral Valve Replacement
intensity o MS with significant MR
o S 3 suggest significant MR o Severely distorted valve by previous procedure
o No improvement with valvotomy
Atrial Septal Defect o It is routinely performed with preservation of the chordal
o Similar in MS: attachments to optimize LV functional recovery
▪ Evidence of RV enlargement o Pulmonary hypertension and RV dysfunction are
additional risk factors for poor outcome.
INTERNAL MEDICINE II Milanes, Gwapo Marquez 19 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
oEndocardial cushions (atrioventricular cushion
III. MITRAL REGURGITATION defects most commonly)
• Abnormality or disease process that affects any one or more o Primum atrial septal defect (cleft anterior mitral valve
of the five functional components of the mitral valve leaflet)
apparatus • Rheumatic MR
o Annulus o Rigidity
▪ Constitutes the anatomical junction between the o Deformity
ventricle and the left atrium, and serves an insertion o Retraction of the valve cusps
site for the leaflet tissue. o Commissural fusion
▪ The normal motion and contraction of the mitral o Shortening, contraction, and fusion of the chordae
annulus also contributes to tendineae
maintaining valve competence Note: It is considered non-ischemic forms of dilated cardiomyopathy
o Chordae tendineae once the left ventricular end-diastolic dimension reaches 6 cm
o Papillary muscles
o Subjacent myocardium • "mitral regurgitation begets mitral regurgitation “
o Leaflets o MR is often progressive
o enlargement of the LA places tension on the posterior
A. Etiologies mitral leaflet → pulling it away from the mitral orifice
Acute → aggravating the valvular dysfunction
o Infective Endocarditis: bacterial vegetations first o LV dilation → increases the regurgitation → enlarges
appear along “contact line” of mitral valve but spread the LA and LV → chordal rupture → vicious circle
to involve atria and chordae tendineae with
subsequent rupture and shrinkage of the latter B. Types
o Papillary Muscle rupture (Post MI) • Type I: Normal leaflet motion
▪ Acute myocardial infarction (MI) with papillary o Ischemic cardiomyopathy
muscle rupture o Dilated cardiomyopathy
▪ Posteromedial papillary muscle is involved much o Endocarditis
more frequently than the anterolateral papillary o Congenital
muscle because of its singular blood supply • Type II: Increased leaflet motion (leaflet prolapse)
o Chordal rupture/leaflet (MVP, MI): thickening and o Degenerative Diseases
erosion of mitral valve with stumps of ruptured o Fibroelastic deficiency
chordae tendineae resulting in valvular incompetence, o Marfan syndrome
regurgitation and atrial enlargement o Forme fruste Barlow
o Blunt trauma o Barlow Disease
Chronic
o Primary (affecting leaflets, chordae) • Type IIIA: Restricted leaflet motion (restricted opening)
▪ Myxomatous (MVP, Barlow’s) o Rheumatic disease
▪ Rheumatic fever o Carcinoid disease
▪ IE (healed) o Radiation
▪ Congenital (Cleft, AV Canal) o Lupus erythematosus
▪ Radiation o Ergotamine use
o Secondary (leaflets, chordae are “innocent o Hypereosinophilic syndrome
bystanders”) o Mucopolysaccharidosis
▪ Ischemic cardiomyopathy • Type IIIB: Restricted leaflet motion (restricted closure)
▪ Dilated Cardiomyopathy o Ischemic cardiomyopathy
▪ HOCM (with SAM) o Dilated cardiomyopathy
▪ Chronic AF with LA enlargement and annular
dilatation PATHOPHYSIOLOGY
o Mitral annular calcification • Resistance to LV emptying (LV afterload) is reduced
• MVP and HOCM is usually dynamic in nature • LV is decompressed into the LA during ejection → reduction
o Anterior papillary muscle displacement in LV size during systole → rapid decline in LV tension
o Systolic anterior motion of the anterior mitral valve • Initial compensation to MR is more complete LV emptying.
leaflet into the narrowed LV outflow tract • LV volume increases progressively with time → reduced
• Annular calcification prevalent in: forward CO
o Advanced renal disease • LV compliance is often increased → LV diastolic pressure
o Women >65 years of age does not increase until late in the course
o Hypertension • Since ejection fraction (EF) rises in severe MR in the presence
o Diabetes of normal LV function, even a modest reduction in this
• MR may occur as a congenital anomaly parameter (<60%) reflects significant dysfunction.
• Severe nonischemic MR
INTERNAL MEDICINE II Milanes, Gwapo Marquez 20 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
o Regurgitant volume 60 mL/beat ▪ May be followed by a short, rumbling, mid-diastolic
o Regurgitant fraction (RF) 50% murmur, even in the absence of structural MS
o Effective regurgitant orifice area 0.40 cm 2 o S4; acute severe MR who are in sinus rhythm
• Severe ischemic MR: effective regurgitant orifice area of >0.3
cm 2 LABORATORY EXAMINATION
• Acute severe MR A. ECG
o Acute pulmonary edema is common in patients with • Sinus rhythm
acute severe MR • Evidence of LA enlargement
o Regurgitant volume is delivered into a normal-sized LA • RA enlargement (severe pulmonary hypertension)
having normal or reduced compliance • AF (Chronic severe MR)
o LA pressures rise markedly for any increase in LA volume • eccentric LV hypertrophy
o The v wave in the LA pressure pulse is usually prominent
o LA and pulmonary venous pressures are markedly B. Chest x-ray
elevated
• Sinus The LA and LV are the dominant chambers in chronic
o Pulmonary edema is common
MR
o Murmur of acute MR is early in timing and decrescendo
• LA may be massively enlarged and forms the right border of
in configuration ending well before S 2
o Arterial pressure may be reduced the cardiac silhouette.
• Pulmonary venous congestion, interstitial edema, and
o Narrow pulse pressure
o Jugular venous pressure and wave forms may be normal Kerley B lines are sometimes noted.
or increased and exaggerated • Marked calcification of the mitral leaflets (combined
o Apical impulse is not displaced rheumatic MR and MS)
o Signs of pulmonary congestion are prominent • Calcification of the mitral annulus
• Chronic severe MR • Acute severe MR may have asymmetric pulmonary edema
o Increased LA compliance o Regurgitant jet is directed predominantly to the orifice
o Little if any increase in LA and pulmonary venous of an upper lobe pulmonary vein
pressures
o LA v wave is relatively less prominent C. Echocardiogram (TTE)
o Holosystolic in timing and plateau in configuration • Assess the mechanism of the MR and its hemodynamic
o AF is almost invariably present severity
o Arterial pressure is usually normal • LV function (LV end-diastolic and end-systolic volumes and
o Carotid arterial pulse may show a sharp upstroke EF)
o Systolic thrill is often palpable at the cardiac apex • Leaflet structure and function
o LV is hyperdynamic with a brisk systolic impulse • Chordal integrity
o Palpable rapid-filling wave (S 3) • LA and LV size
o Apex beat is often displaced laterally • Annular calcification
• Regional and global LV systolic function
• Width or area of the color flow MR jet within the LA
• Intensity of the continuous wave Doppler signal
• Follow the course of patients with chronic MR
• Provide rapid assessment for any clinical change
SYMPTOMS
• Chronic severe MR D. Left Ventriculography
o Fatigue
• Involves injecting contrast media into the heart's ventricle
o exertional dyspnea
to measure the volume of blood pumped
o Orthopnea
o Palpitations (onset of AF)
• Right-sided heart failure
o Painful hepatic congestion
o Ankle edema
o Distended neck veins
o Ascites
o Secondary TR
• Auscultation
o S1; generally absent, soft, or buried
o S2; the aortic valve may close prematurely
▪ wide but physiologic splitting of S 2
o S3; A low-pitched Figure 8. The left atrium is opacified on the right but not on the left
▪ Occurring 0.12–0.17 s after the aortic valve closure indicative of mitral regurgitation. The arrow represents blood flow.
sound With a competent mitral valve, all of the blood ejected by the left
INTERNAL MEDICINE II Milanes, Gwapo Marquez 21 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
ventricle goes into the aorta. In patients with mitral regurgitation, a • AS in adults is due to degenerative calcification of the aortic
portion of left ventricular stroke volume goes into the left atrium cusps and occurs most commonly on a substrate
o Congenital disease (bicuspid aortic valve)
TREATMENT o Chronic (trileaflet) deterioration, or
• Warfarin o Previous rheumatic inflammation
o If AF intervenes • Pathologic study of specimens removed at the time of aortic
o target INR of 2–3 valve replacement
• Heart failure treatment o 53% were bicuspid
o Diuretics o 4% unicuspid
o Beta blockers • Genetic polymorphisms
o Angiotensin-converting enzyme (ACE) inhibitors o Vitamin D receptor
o Digitalis o Estrogen receptor in postmenopausal women
o biventricular pacing (cardiac resynchronization therapy o Interleukin 10
[CRT] o Apolipoprotein E4
• Exercise
o Should avoid isometric forms of exercise (severe MR)
• Surgical Repair
o Consists of valve reconstruction using a variety of
valvuloplasty techniques and insertion of an annuloplasty
ring
o Spares the patient the long-term adverse consequences
of valve replacement (thromboembolic and
hemorrhagic complications)
o Maintain LV function to a relatively greater degree
o Currently most commonly applied surgical approaches to
posterior leaflet prolapse.
A. Triangular resection;
B. Quadrangular resection and sliding leaflet plasty
C. Neochordoplasty with polytetrafluoroethylene
sutures
• Indications for early consideration of mitral valve repair
o Recent-onset AF
o Pulmonary hypertension(PA pressure 50 mmHg at rest or
60 mmHg with exercise)
• Surgical treatment of chronic, nonischemic severe MR is Figure 9. Causes of aortic stenosis. A, in a parasternal midsystolic
indicated for asymptomatic patients short-axis view, calcific aortic stenosis is characterized by
o LV dysfunction is progressive fibrocalcific masses on the aortic side of the leaflet that result in
o LVEF falling below 60% increased leaflet stiffness without commissural fusion. Calcific
o End-systolic dimension increasing beyond 40 mm shadowing and reverberations limit image quality. B, with a
• Percutaneous Mitral Valve Repair congenital bicuspid valve, the two leaflets (with a raphe in the
o Clip used to grasp the free edges of the anterior and anterior leaflet) open widely in systole. C, the diagnostic features of
posterior leaflets in their midsections during rheumatic stenosis are commissural fusion and mitral valve
transcatheter repair of selected patients with mitral involvement, with the characteristic triangular aortic valve opening
regurgitation in systole. D, the unicuspid valve has only one point of attachment
(at the 6 o’clock position) with a funnel-shaped valve opening.
IV. AORTIC STENOSIS
• Narrowing of the aortic valve opening
• Restricts the blood flow from the left ventricle to the aorta
• Epidemiology
o Occurs in about one-fourth of all patients with chronic
valvular heart disease
o ~80% of adult patients with symptomatic, valvular AS are
male
Etiology
INTERNAL MEDICINE II Milanes, Gwapo Marquez 22 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
Figure 10. Radiation-induced aortic and mitral stenosis. High-dose Mediastinal radiation → late scarring, fibrosis and
radiation to the chest induces severe fibrosis and calcification of the calcification of the leaflets with AS
aortic and mitral valves. A characteristic finding is heavy calcification
along the aorto-mitral curtain (arrow). Risk factors
Pathogenesis of Calcific Aortic Stenosis
• Shares many features with vascular atherosclerosis
o Endothelial dysfunction
o Lipid accumulation Figure 12. Schematic working model of the interplay between risk
o Inflammatory cell activation factors for fibrocalcific aortic valve disease and the dysfunctional
o Cytokine release “response to injury” that can increase propensity for development
o Upregulation of several signaling pathways of valvular stenosis. Note that both valvular calcification and fibrosis
• Traditional atherosclerotic risk factors associated with the are likely to play major roles in the development of
development and progression of calcific AS hemodynamically significant aortic valve dysfunction
o Low-density lipoprotein (LDL)-cholesterol
o Lipoprotein a [Lp(a)] BICUSPID AORTIC VALVE DISEASE
o Diabetes mellitus • Most common congenital heart valve defect
o Smoking • Incidence of 0.5–1.4% of the population
o Chronic kidney disease • 2–4:1 male to female predominance
o Metabolic syndrome • Autosomal dominant with incomplete penetrance
• Some believe X-linked component
• Mutation in the NOTCH1 gene
• Aortic coarctation or medial degeneration with ascending
aortic aneurysm formation occurs commonly among patients
with BAV disease
• Patients with BAV disease have larger aortas than patients
with comparable tricuspid aortic valve disease
• Aortopathy develops independent of the hemodynamic
severity of the valve lesion and is a risk factor for aneurysm
formation and/or dissection.
• Can be a component of more complex congenital heart
disease with or without other left heart obstructing lesions, as
in Shone’s complex
Figure 11. Lipid and inflammatory cell infiltration occurs across
damaged endothelium. A cascade of events follows that leads
eventually to formation of disorganized collagen (fibrosis) and
calcium hydroxyapatite (bone) deposition. Valvular interstitial cells
(VIC) are critical participants in this active process.
Rheumatic Disease of the Aortic Leaflet
Commissural fusion → bicuspid-appearing valve →
leaflets more susceptible to trauma → fibrosis,
calcification, further narrowing Figure 13. CMR of ascending aortic aneurysm in patient with
bicuspid aortic valve and unrepaired mild CoA who died suddenly
Rheumatic AS is almost always associated with involvement from an aortic wall rupture.
of the mitral valve and with AR
INTERNAL MEDICINE II Milanes, Gwapo Marquez 23 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
Figure 14. Bicuspid aortic valves may have a visible raphe—the
fusion ridge of two aortic leaflets.
• The obstruction to LV outflow produces a systolic pressure
gradient between the LV and aorta.
• Severe obstruction (acute) → LV responds by dilation and
reduction of stroke volume.
• severe obstruction (chronic) → LV contractile performance is
Figure 15. Bicuspid aortic valve during diastole (A) and systole (B) in maintained by the presence of concentric LV hypertrophy
parasternal short-axis (PSAX) view. Note horizontal commissure
• A large transaortic valve pressure gradient may exist for many
(arrow) in diastole and “fish mouth” appearance during systole
years without a reduction in CO or LV dilation
• Excessive hypertrophy becomes maladaptive, LV systolic
OTHER FORMS OF OBSTRUCTION TO LEFT VENTRICULAR OUTFLOW
function declines, abnormalities of diastolic function progress,
In addition to valvular AS, three other lesions may be
and irreversible myocardial fibrosis develops
responsible for obstruction to LV outflow:
• Severe obstruction to LV outflow
o Hypertrophic obstructive cardiomyopathy
o A mean systolic pressure gradient >40 mmHg with a
o Discrete fibromuscular/membranous subaortic stenosis
normal CO
o Supravalvular AS
o Effective aortic orifice area <∼ 1 cm2
• The causes of left ventricular outflow obstruction can be
o ∼ <0.6 cm2/m2 body surface area in a normal-sized
differentiated on the basis of the cardiac examination and
• Diminished compliance of the hypertrophied LV
Doppler echocardiographic findings.
o Elevated LV end-diastolic pressure
o Preserved EF
o CO at rest is within normal limits in most patients with
severe AS, it usually fails to rise normally during exercise
• Late in the course, contractile function deteriorates because
of afterload excess
o CO and LV–aortic pressure gradient decline
o Mean LA, PA, and RV pressures rise
• LV performance can be further compromised by
superimposed CAD
PATHOPHYSIOLOGY
SYMPTOMS
• Three cardinal symptoms
o Exertional dyspnea: elevation of the pulmonary capillary
pressure caused by elevations of LV diastolic pressures
o Angina pectoris: imbalance between the augmented
myocardial oxygen requirements and reduced oxygen
availability
o Syncope
▪ Decline in arterial pressure caused by vasodilation in
the exercising muscles and inadequate
vasoconstriction
▪ Sudden fall in CO produced by an arrhythmia
• Advanced stages of the disease
o Marked fatigability
o Weakness
INTERNAL MEDICINE II Milanes, Gwapo Marquez 24 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
o Peripheral cyanosis
o Cachexia
o Orthopnea
o Paroxysmal nocturnal dyspnea
o Pulmonary edema
• Severe pulmonary hypertension
• Murmur of AS
o Systemic venous hypertension
o Ejection (mid) systolic
o Hepatomegaly
o Commences shortly after the S 1
o AF
o Increases in intensity to reach a peak toward the middle
of ejection
PHYSICAL FINDINGS
o Ends just before aortic valve closure
Rhythm is generally regular until late in the course
o Low-pitched, rough and rasping in character
AF should suggest the possibility of associated mitral valve
o Loudest at the base of the heart
disease
o Most common in second right intercostal space
Systemic arterial pressure usually within normal limits
o Transmitted upward along the carotid arteries
Late stages: stroke volume declines → systolic pressure may
o Occasionally transmitted downward and to the apex,
fall → pulse pressure narrow
where it may be confused with the systolic murmur of
Pulsus parvus et tardus
MR (Gallavardin effect)
o Thrill or anacrotic "shudder“
o Palpable over the carotid arteries, more commonly the
left
• a wave in the jugular venous pulse is accentuated
o Diminished distensibility of the RV cavity
The LV impulse is usually displaced laterally
A double apical impulse (with a palpable S 4) may be
recognized, particularly with the patient in the left lateral
recumbent position
A systolic thrill may be present at the base of the heart to the
right of the sternum when leaning forward or in the
suprasternal notch.
Auscultation
Early systolic ejection sound is frequently audible in children,
adolescents, and young adults with congenital BAV disease
Paradoxical splitting of S 2
The sound of aortic valve closure can be heard most Figure 16. Harsh, loud systolic, crescendo-decrescendo murmur in
frequently in patients with AS who have pliable valves, and aortic area – 4th sound; paradoxical splitting of S 2
calcification diminishes the intensity of this sound.
S 4 is audible at the apex and reflects the presence of LV LABORATORY EXAMINATION
hypertrophy and an elevated LV end-diastolic pressure A. ECG
S 3 generally occurs late in the course, when the LV dilates and • Severe AS → LV hypertrophy
its systolic function becomes severely compromised • Advanced cases → ST-segment depression and T-wave
inversion (LV "strain") in standard leads I and aVL and in the
left precordial leads
• No close correlation between the ECG and the
hemodynamic severity of obstruction
• Absence of ECG signs of LV hypertrophy does not exclude
severe obstruction
INTERNAL MEDICINE II Milanes, Gwapo Marquez 25 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
Figure 17. Calcific (“senile”) degeneration of aortic valve showing
“echo-bright” reflection (arrows). Commissural fusion can occur, but
is not a hallmark of this disease process. Commissural fusion is a
B. Echocardiogram hallmark feature of rheumatic valvular heart disease.
• Thickening and calcification
• Reduced systolic opening of the valve leaflets
• LV hypertrophy
• Eccentric closure of the aortic valve cusps is characteristic
of congenitally bicuspid valves.
• TEE imaging usually displays the obstructed orifice
extremely well, but it is not routinely required for accurate
characterization.
• Dobutamine stress echocardiography is useful for the
evaluation of patients with AS and severe LV systolic
dysfunction (EF <0.35), in whom the severity of the AS can
often be difficult to judge
Figure 18. Aortic stenosis showing restricted leaflet opening (arrow)
C. Chest x-ray during systole (parasternal long-axis view [PLAX]).
• Rounding of the cardiac apex
• Dilated proximal ascending aorta
• Aortic valve calcification (lateral view)
• LV enlargement
• Pulmonary congestion
• Enlargement of the LA, PA, and right heart chambers
Figure 19. (L) Normal aortic valve (R) Degenerative calcific AS
D. Catheterization
• Catheterization is also useful in three distinct categories of
patients
o Patients with multivalvular disease, in whom the role
played by each valvular deformity should be defined to
aid in the planning of operative treatment
o Young, asymptomatic patients with noncalcific
congenital AS, to define the severity of obstruction to
LV outflow
o Patients in whom it is suspected that the obstruction to
LV outflow may not be at the level of the aortic valve
but rather at the sub- or supravalvular level.
Severe AS valve area <1 cm2
Moderate AS valve area of 1–1.5 cm2
Mild AS valve area of 1.5–2 cm2
Aortic valve jet velocity of less than 2.5 meters/s (peak
sclerosis gradient <25 mmHg)
INTERNAL MEDICINE II Milanes, Gwapo Marquez 26 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
• In patients with AR due to primary valvular disease, dilation of
NATURAL HISTORY the aortic annulus may occur secondarily and lead to
Death in patients with severe AS occurs most commonly in the worsening regurgitation.
seventh and eighth decades Primary Aortic Root Disease
Average time to death after the onset of various symptoms Cystic medial degeneration of the ascending aorta
was as follows: Idiopathic dilation of the aorta
o Angina pectoris, 3 years Annuloaortic ectasia
o Syncope, 3 years Osteogenesis imperfecta
o Dyspnea, 2 years Severe hypertension
o Congestive heart failure, 1.5–2 years Syphilis and Ankylosing spondylitis
Sudden death as the first manifestation of severe AS is very
uncommon (<1% per year) in asymptomatic adult patients
Calcific AS is a progressive disease
o Annual reduction in valve area averaging 0.1 cm2
o Annual increases in the peak jet velocity and mean valve
gradient averaging 0.3 meters/s and 7 mmHg
TREATMENT
Medical Treatment
o Severe AS (valve area <1 cm 2)
o Avoid strenuous physical activity and competitive sports
o Avoid dehydration and hypovolemia
o Medications used for the treatment of hypertension or
CAD
▪ Beta blockers
▪ ACE inhibitors
▪ HMG-CoA reductase inhibitors ("statins") exhibit
slower progression of leaflet calcification
Surgical Treatment
o Indications PATHOPHYSIOLOGY
▪ Severe AS (valve area <1 cm2 or 0.6 cm2/m2 body
surface area)
▪ Symptomatic
▪ LV dysfunction (EF <50%)
▪ BAV disease and an aneurysmal or expanding aortic
root (maximal dimension >4.5 cm or annual increase
in size >0.5 cm/year), even if they are asymptomatic
▪ Patients with asymptomatic moderate or severe AS
who are referred for CABG surgery should also have
AVR
• Percutaneous balloon aortic valvuloplasty
o Preferable for operation:
▪ Children
▪ Young adults with congenital
▪ Noncalcific AS
o Not commonly use in adults with severe calcific AS
▪ Very high restenosis rate (80% within 1 year)
▪ High risk of procedural complications
▪ "bridge to operation"
• The total stroke volume ejected by the LV is increased in
V. AORTIC REGURGITATION patients with AR
Primary Valve Disease • In patients with severe AR, the volume of regurgitant flow may
• Rheumatic origin is much less common in patients with equal the effective forward stroke volume
isolated AR who do not have associated rheumatic mitral valve • In AR the entire LV stroke volume is ejected into a high-
disease pressure zone, the aorta
• Patients with congenital BAV disease may develop • Increase in the LV end-diastolic volume (increased preload)
predominant AR, and approximately 20% of patients will
constitutes the major hemodynamic compensation for AR
require aortic valve surgery
• Chronic AR
• AR may result from infective endocarditis
o LV preload and afterload are both increased
INTERNAL MEDICINE II Milanes, Gwapo Marquez 27 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
o Deterioration of LV function often precedes the
development of symptoms C. Auscultation
o Considerable thickening of the LV • Severe AR
o Autopsy the hearts of these patients may be among the o Aortic valve closure sound (A 2) is usually absent
largest encountered, sometimes weighing >1000 g. • BAV disease
o Systolic ejection sound
HISTORY o Occasionally an S 4 also may be heard
Three-fourths of patients with pure or predominant valvular • Chronic AR
AR are men o High-pitched
Women predominate among patients with primary valvular o Blowing
AR who have associated rheumatic mitral valve disease o Decrescendo diastolic murmur
Acute severe AR o Heard best in the third intercostal space along the left
o Infective endocarditis sternal border
o Aortic dissection • Mild AR
o Trauma o Murmur is brief, but as the severity increases, it
o LV cannot dilate sufficiently to maintain stroke volume generally becomes louder and longer, indeed
o LV diastolic pressure rises rapidly with associated marked holodiastolic
elevations of LA and PA wedge pressures • Mid-systolic ejection murmur is frequently audible in
• Chronic severe AR isolated AR.
o Long latent period • Heard best at the base of the heart
o Remain relatively asymptomatic for as long as 10–15 • Austin Flint murmur: soft, low-pitched, rumbling mid-to-
years
late diastolic murmur
o It is probably produced by the diastolic displacement
PHYSICAL FINDINGS of the anterior leaflet of the mitral valve by the AR
Jarring of the entire body stream
Bobbing motion of the head with each systole can be o Not associated with hemodynamically significant
appreciated
mitral obstruction
Abrupt distention and collapse of the larger arteries are easily
visible LABORATORY EXAMINATION
Examination should be directed toward the detection of
conditions predisposing to AR A. ECG
o Bicuspid valve
Chronic severe AR: ECG signs of LV hypertrophy
o Endocarditis
LV strain
o Marfan's syndrome
o ST-segment depression
o Ankylosing spondylitis
o T-wave inversion in leads I, aVL, V 5, and V6
• Diffuse myocardial disease
A. Arterial pulse
o Left-axis deviation
Corrigan's pulse: rapidly rising “water-hammer” pulse,
o QRS prolongation denote diffuse myocardial disease
which collapses suddenly as arterial pressure falls rapidly
during late systole and diastole
Quincke’s pulse: capillary pulsations, an alternate flushing
and paling of the skin at the root of the nail while pressure
is applied to the tip of the nail
Traube’s sign: booming “pistol-shot” sound can be heard
over the femoral arteries
Duroziez’s sign: to-and-fro murmur is audible if the femoral
artery is lightly compressed with a stethoscope
Arterial pulse pressure is widened as a result of both
systolic hypertension and a lowering of the diastolic
pressure
B. Palpation
LV impulse is heaving and displaced laterally and inferiorly
diastolic thrill may be palpable along the left sternal border
in thin-chested individuals
prominent systolic thrill may be palpable in the
suprasternal notch and transmitted upward along the
carotid arteries
In many patients with pure AR or with combined AS and AR,
the carotid arterial pulse is bisferiens
INTERNAL MEDICINE II Milanes, Gwapo Marquez 28 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
o Cardiac arrhythmias and systemic infections are poorly
B. Chest x-ray tolerated in patients with severe AR and must be treated
• Chronic severe AR promptly and vigorously.
o Apex is displaced downward and to the left in the o Although nitroglycerin and long-acting nitrates are not as
frontal projection helpful in relieving anginal pain as they are in patients
o In the left anterior oblique and lateral projections, the with ischemic heart disease, they are worth a trial.
LV is displaced posteriorly and encroaches on the o Patients with syphilitic aortitis should receive a full
spine. course of penicillin therapy.
o Aorta may fill the retrosternal space in the lateral view o Beta blockers and the angiotensin receptor blocker (ARB)
(aneurysmal dilation of the aorta) losartan may be useful to retard the rate of aortic root
enlargement in young patients with Marfan syndrome
C. Echocardiogram and aortic root dilation.
LV size is increased in chronic AR
systolic function is normal or even supernormal until • Surgical Treatment
o In deciding on the advisability and proper timing of
myocardial contractility declines
surgical treatment, two points should be kept in mind:
Characteristic finding
o Rapid ▪ Patients with chronic severe AR usually do not
become symptomatic until after the development of
o High-frequency diastolic fluttering of the anterior
myocardial dysfunction;
mitral leaflet
o Produced by the impact of the regurgitant jet ▪ When delayed too long (defined as >1 year from
onset of symptoms or LV dysfunction), surgical
• Severe AR
treatment often does not restore normal LV size and
o Central jet width exceeds 65% of the left ventricular
function.
outflow tract
o Operation can be deferred as long as the patient both
o Regurgitant volume is 60 mL/beat
remains asymptomatic and retains normal LV function
o Regurgitant fraction is 50%
without severe or progressive chamber dilation.
o Diastolic flow reversal in the proximal descending
o Aortic valve replacement (AVR) is indicated for the
thoracic aorta
treatment of severe AR in symptomatic patients
irrespective of LV function.
TREATMENT
o In general, the operation should be carried out in
• For Acute AR
asymptomatic patients with severe AR and progressive
o Patients with acute severe AR may respond to
LV dysfunction defined by an LVEF <50%, an LV end-
intravenous diuretics and vasodilators (such as sodium systolic dimension >50 mm, or an LV diastolic dimension
nitroprusside), but stabilization is usually short-lived and
>65 mm.
operation is indicated urgently.
o Intraaortic balloon counter-pulsation is contraindicated. VI. TRICUSPID STENOSIS
o Beta blockers are also best avoided so as not to reduce
• Less prevalent than MS
the CO further or slow the heart rate, thus allowing more
• Generally rheumatic in origin
time for diastolic filling of the LV.
• M<F
o Surgery is the treatment of choice and is usually
• Does not occur as an isolated lesion
necessary within 24 h of diagnosis.
• Usually associated with MS
• For Chronic AR
o Early symptoms of dyspnea and effort intolerance • Hemodynamically significant TS
respond to treatment with diuretics; vasodilators o Occurs in 5–10% of patients with severe MS
(Angiotensin converting enzyme [ACE] inhibitors, o Rheumatic TS is commonly associated with some degree
dihydropyridine calcium channel blockers, or of TR
hydralazine) may be useful as well. o Non-rheumatic causes of TS are rare
o Surgery can then be performed in a more controlled
setting.
o The use of vasodilators to extend the compensated
phase of chronic severe AR before the onset of symptoms
or the development of LV dysfunction is more
controversial and less well established.
o Systolic blood pressure should be controlled (goal <140 PATHOPHYSIOLOGY
mmHg) in patients with chronic AR, and vasodilators are • Diastolic pressure gradient between the RA and RV defines
an excellent first choice as antihypertensive agents.
TS
o It is often difficult to achieve adequate control because
• Augmented when the transvalvular blood flow increases
of the increased stroke volume that accompanies severe
during inspiration and declines during expiration
AR.
INTERNAL MEDICINE II Milanes, Gwapo Marquez 29 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
• Mean diastolic pressure gradient of 4 mmHg is usually
sufficient to elevate the mean RA pressure to levels that result PHYSICAL FINDINGS
in systemic venous congestion. • TS usually occurs in the presence of other obvious valvular
• In patients with sinus rhythm disease
o RA a wave may be extremely tall and may even approach • Diagnosis may be missed unless it is considered
the level of the RV systolic pressure • Severe TS
o y descent is prolonged o Marked hepatic congestion → cirrhosis, jaundice
• Cardiac output o Serious malnutrition
o At rest is usually depressed o Anasarca
o Fails to rise during exercise o Ascites
o Low CO is responsible for the normal or only slightly o Congestive hepatomegaly
elevated LA, PA, and RV systolic pressures despite the o Jugular veins are distended
presence of MS o Giant a waves
• The presence of TS can mask the hemodynamic and clinical o v waves are less conspicuous
features of any associated MS. o Because tricuspid obstruction impedes RA emptying
during diastole
SYMPTOMS o Slow y descent
• Development of MS generally precedes that of TS • OS of the tricuspid valve may rarely be heard approximately
o Pulmonary congestion 0.06 s after pulmonic valve closure
o Fatigue • The diastolic murmur of TS has many of the qualities of the
• Severe TS complain diastolic murmur of MS, and because TS almost always occurs
o Little dyspnea in the presence of MS, it may be missed
o Hepatomegaly • Tricuspid murmur
o Ascites o Heard best along the left lower sternal border
o Edema o Over the xiphoid process
o Fatigue o Prominent during presystole (sinus rhythm)
• TS may be suspected for the first time when symptoms of o Augmented during inspiration
right-sided failure persist after an adequate mitral valvotomy. o Reduced during expiration and particularly during the
strain phase of the Valsalva maneuver
Table 1. Clinical and laboratory features of TS
LABORATORY EXAMINATION
• ECG
o Features of RA enlargement
▪ Tall, peaked P waves in lead II
▪ Prominent, upright P waves in lead V1.
o The absence of ECG evidence of RV hypertrophy (RVH) in
a patient with right-sided heart failure who is believed to
have MS should suggest associated tricuspid valve
disease.
o Tricuspid valve is usually thickened and domes in
diastole
o Severe TS
▪ Valve area ≤1 cm 2 or
▪ Pressure half-time of ≥190 MS
o RA and inferior vena cava (IVC) are enlarged
o Transthoracic echocardiography (TTE)
▪ Additional information regarding the severity of any
associated TR, mitral valve structure and function,
left ventricle (LV) and RV size and function, and PA
pressure.
• Chest x-ray in patients with combined TS and MS
o Prominence of the RA and superior vena cava without
much enlargement of the PA
o With less evidence of pulmonary vascular congestion
• Cardiac catheterization is not routinely necessary for
assessment of TS.
TS RHD VS TS CARCINOID
More on right-sided heart failure symptoms
INTERNAL MEDICINE II Milanes, Gwapo Marquez 30 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
TREATMENT
• Medical
Carcinoid Tricuspid Rheumatic Tricuspid o Marked systemic venous congestion
Valvulopathy Valvulopathy ▪ Salt restriction
‘Drumstick leaflets’ are Leaflets are thickened, with ▪ Bed rest
thickened, retracted and commissural fusion, chordal ▪ Diuretic therapy
relatively fixed thickening, diastolic doming • Surgery
o At the time of surgical mitral valvotomy or mitral valve
NO MV involvement WITH MV involvement replacement (MVR) for mitral valve disease
o Moderate or severe TS
o Mean diastolic pressure gradients exceeding ~4 mmHg
and tricuspid orifice areas <1.5–2 cm 2
• Mechanical valves in the tricuspid position are more prone to
thromboembolic complications than in other positions
• Percutaneous tricuspid balloon valvuloplasty for isolated
severe TS without significant TR is very rarely performed
VII. TRICUSPID REGURGITATION
• TR secondary to marked dilation of the tricuspid annulus
from RV enlargement due to PA hypertension accounts for
80% of cases
• Functional TR may complicate RV enlargement of any cause
• Commonly seen in the late stages of heart failure due to
rheumatic or congenital heart disease with severe PA
hypertension as well as in ischemic and idiopathic dilated
cardiomyopathies.
• Rheumatic fever may produce primary (organic) TR, often
associated with TS
• Causes
o Infarction of RV papillary muscles
o Tricuspid valve prolapse
o Carcinoid heart disease
o Endomyocardial fibrosis
o Radiation
o Infective endocarditis
o Leaflet trauma
INTERNAL MEDICINE II Milanes, Gwapo Marquez 31 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
• TR is more often diagnosed by examination of the neck veins
Table 2. Causes of TR than by auscultation of the heart sounds.
• Marked hepatomegaly
• Systolic pulsations
• Ascites
• Pleural effusions
• Edema
• Positive hepatojugular reflex
• Prominent RV pulsation along the left parasternal region
• May sometimes be confused with that of MR unless
attention is paid to its variation during the respiratory cycle
and the extent of RV enlargement
• Atrial fibrillation (AF) is usually present in the chronic phase of
the disease
Carvallo’s Sign of Tricuspid Regurgitation
o Pansystolic murmur produced by functional TR, audible
PATHOPHYSIOLOGY along the left sternal border, louder during inspiration,
• The incompetent tricuspid valve allows blood to flow diminishes during forced expiration or the strain phase
of the Valsalva maneuver
backward from the RV into the RA
o Blowing
• The severity and physical signs of TR can vary as a function of
o Holosystolic murmur
o PA systolic pressure (in the absence of RV outflowtract
o Lower left sternal margin
stenosis)
o Intensified during inspiration
o Dimension of the tricuspid valve annulus
o Respiratory cycle
LABORATORY EXAMINATION
• RV filling is increased during inspiration
• ECG
• Significant degrees of TR will lead to
o Inferior Q-wave MI ( prior RV MI,RVH)
o RA enlargement
o Bizarre right bundle branch block type pattern with
o Elevation of the RA
preexcitation ( Ebstein’s anomaly)
o Elevation of jugular venous pressures
o ECG signs of RA enlargement
o Prominent c-v waves in the pulse tracings
o AF is frequently noted
• Progressive TR can lead to “ventricularization” of the RA wave
• Chest x-ray
form
• Severe TR is also characterized by
o RV dilation (RV volume overload)
o Systolic dysfunction
o PA hypertension
o Myocardial fibrosis from previous injury.
SYMPTOMS
• Mild or moderate degrees
o Usually well tolerated in the absence of other
hemodynamic disturbances
o TR most often coexists with left-sided valve lesions
• Fatigue and exertional dyspnea
o Reduced forward CO
• Disease progresses and RV function declines Figure 20. RA and RV enlargement in TR
o Cervical pulsations
o Abdominal fullness • TTE: definitive with demonstration of RA dilation and RV
o Bloating volume overload and prolapsing, flail, scarred, or
o Diminished appetite displaced/tethered tricuspid leaflets
o Muscle wasting • Diagnosis and assessment of TR can be made by color flow
o Progressive weight gain Doppler imaging
o Painful swelling of the lower extremities • Severe TR is accompanied by hepatic vein systolic flow
reversal
PHYSICAL FINDINGS • Continuous wave Doppler of the TR velocity profile is useful in
• The neck veins in patients with severe TR estimating PA systolic pressure
• Distended with prominent c-v waves and rapid y descents (in
the absence of TS).
INTERNAL MEDICINE II Milanes, Gwapo Marquez 32 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
PATHOPHYSIOLOGY
• Defined hemodynamically by a systolic pressure gradient
between the RV and main PA
• RV hypertrophy develops as a consequence of sustained
obstruction to RV outflow, and systolic ejection is prolonged.
• RV dysfunction from afterload mismatch occurs earlier in the
course of PS and at lower peak systolic pressures, because the
RV adapts less well to this type of hemodynamic burden →
noncompliant and hypertrophied RV → RA a wave elevates
o Prominent RA v wave signifies functional TR from RV
and annular dilation
• Severe PS: peak systolic gradient across the pulmonic valve
of >50 mmHg
• Moderate PS: peak gradient of 30–50 mmHg
TREATMENT
• PS rarely progresses in patients with peak gradients <30
• Diuretics
mmHg, but may worsen in those with moderate disease due to
• Aldosterone antagonist
valve thickening and calcification with age.
• Tricuspid valve surgery is recommended
• CO is maintained until late in the course of the disease
o Severe TR who are undergoing left-sided valve surgery
o Tricuspid annular dilation (>40 mm)
SYMPTOMS
o History of right heart failure, or PA hypertension
• Mild to moderate PS: asymptomatic
Please see Appendix for the management of TR
• Severe PS
o Exertional dyspnea
VIII. PULMONIC STENOSIS
o Early-onset fatigue
• Essentially a congenital disorder
o Anginal chest pain (d/t RV oxygen supply-demand
• Isolated PS: valve is typically domed
mismatch)*
• Noonan’s syndrome: with dysplastic pulmonic valves,
o Syncope*
chromosome 12 (mutations in PTPN1 gene) * Occur with very severe forms of obstruction or in the presence of a
• Less common etiologies: destabilizing trigger (e.g. atrial fibrillation, fever, infection, anemia or
o Carcinoid pregnancy)
o Obstructing tumors PHYSICAL FINDINGS
o Bulky vegetations • Murmur of mild or moderate PS
• The pulmonic valve is only very rarely affected by the o Mid-systolic in timing
rheumatic process.
o Crescendo-decrescendo in configuration
o Heard best in the left second interspace
o Introduced by an ejection sound (click) in younger adults
▪ Ejection sound is the only right-sided acoustic event
that decreases in intensity with inspiration.
▪ Reflects the premature opening of the pulmonic
valve by the elevated RV end-diastolic (postatrial a
wave) pressure
• Severe PS
o Ejection sound moves closer to the first heart sound and
eventually becomes inaudible
o Right-sided fourth heart sound may emerge
o Systolic murmur peaks later and may persist through the
aortic component of the second heart sound (A2)
o Pulmonic valve closure is delayed
o Pulmonic component of the second heart sound (P2) is
reduced or absent.
• Prominent a wave: indicative of higher atrial pressure
necessary to fill the noncompliant RV (seen in jugular venous
pulse)
• Signs of right heart failure (may appear very late in the
Figure 21. Classification of the abnormal pulmonic valve. The disease)
abnormal pulmonic valve may be classified as (A) acommisural with o Hepatomegaly
prominent systolic doming of the valve cusps and an eccentric o Ascites
orifice, (B) unicommissural, (C) bicuspid with fused commissures, or o Edema
(D) dysplastic with severely thickened and deformed valve cusps.
LABORATORY EXAMINATION
INTERNAL MEDICINE II Milanes, Gwapo Marquez 33 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
• ECG: right axis deviation, RVH, RA enlargement Color flow Doppler evaluation shows flow acceleration and
• Chest x-ray turbulence across the stenotic pulmonary valve.
o Poststenotic dilation of the main PA (frontal plane
projection)
o Filling of the retrosternal airspace due to RV enlargement
(lateral film)
o Cardiac apex appears to be lifted off the left
hemidiaphragm
o RA may also be enlarged
TREATMENT
• Diuretics can be used to treat symptoms and signs of right
heart failure
• Percutaneous pulmonic balloon valvotomy is recommended
for
o Symptomatic patients
▪ Domed valve and a peak gradient >50 mmHg
▪ Mean gradient >30 mmHg
o Asymptomatic patients
▪ Peak gradient >60 mmHg
▪ Mean gradient >40 mmHg
• Surgery may be required when the valve is dysplastic
Figure 22. Right atrial and ventricular enlargement, dilation of the
pulmonary artery (arrow), and diminished vascular markings.
• Transthoracic Echocardiography (TTE)
o Allows definitive diagnosis and characterization in most
cases with depiction of the valve and assessment of the
gradient, RV function, PA pressures
• Transesophageal echocardiography (TEE)
o May be useful in some patients for improved delineation
Figure 24. Cardiac catheterization images from pulmonic balloon
of the RV outflow tract (RVOT) and assessment of
valvotomy. A, Right ventricular anteroposterior angiogram
infundibular hypertrophy
demonstrates systolic doming (arrow) of a stenotic pulmonic valve
• Cardiac catheterization
(PV) due to severe valve stenosis. Dynamic subvalvular obstruction
o Not usually necessary for diagnosis
can also be seen below the valve. Post-stenotic dilation of the
o If performed: pressures should be obtained from just
pulmonary artery (PA) is present. RV, Right ventricle. B, pulmonic
below and above the pulmonic valve
balloon valvotomy resulted in marked reduction in the
• Correlation between doppler assessment of peak
transpulmonic gradient.
instantaneous gradient and catheterization-measured peak-
to-peak gradient is weak
IX. PULMONIC REGURGITATION
• Etiology
o Consequence of primary valve pathology, annular
enlargement or their combination
o After surgical treatment of RVOT obstruction in children
(e.g. Tetralogy of Fallot)
o After percutaneous pulmonic balloon valvotomy
• Carcinoid → mixed pulmonic valve disease with PR and PS
• Long-standing severe PA hypertension → dilation of the
pulmonic valve ring and PR
Figure 23. The pulmonic valve cusps of the patient with the carcinoid
syndrome (A), were thickened, retracted, and fixed with a stenotic
pulmonary valve orifice (left panel, parasternal short-axis view).
INTERNAL MEDICINE II Milanes, Gwapo Marquez 34 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
• Tricuspid valve systolic jet velocity: estimation of PA pressures
• Cardiac magnetic resonance (CMR): provides greater
anatomic detail
• Cardiac catheterization is not routinely necessary but would
be performed as part of a planned transcatheter procedure.
TREATMENT
• Pharmacologic
o Vasodilator
o Diuretics: used to treat manifestations of RSHF
PATHOPHYSIOLOGY
• Surgical/interventional strategies
• Results in RV chamber enlargement and eccentric
o Surgical valve replacement for primary, severe, pulmonic
hypertrophy
valve disease (rare)
• State of increased preload and afterload o Transcatheter pulmonic valve replacement has been
• Reverse pressure gradient from the PA to the RV successfully performed in many patients with severe PR
PROGRESSIVELY DECREASES throughout diastole → after childhood repair of tetralogy of Fallot or pulmonic
decrescendo nature of the diastolic murmur valve stenosis or atresia
• ↑ RV diastolic pressure, murmur becomes SHORTER in
duration REFERENCES
• Reduction in RV ejection fraction may be an early indicator of 1. 2022 Trans
hemodynamic compromise 2. Lecture PPT
• Significant enlargement of the RV and RA with marked 3. Lecture Recordings
elevation of the jugular venous pressure 4. Harrison’s Priniciples of Internal Medicine 20th Ed
SYMPTOMS
• Mild or moderate degrees: do not by themselves result in
symptoms
• PA hypertension
• With progressively severe PR and RV dysfunction
o Fatigue
o Exertional dyspnea
o Abdominal fullness/bloating
o Lower extremity swelling
PHYSICAL FINDINGS
• Graham Steell murmur
o Hallmark of PR
o High-pitched, diastolic, decrescendo blowing murmor
o Along the left sternal border
o Indistinguishable from the AR murmur
o ↑ intensity with inspiration and is accompanied by a loud
and often palpable P2
o Results from dilation of the pulmonary valve ring
o Occurs in patients with mitral valve disease and severe
pulmonary hypertension.
• Survivors of childhood surgery for tetralogy of Fallot/PS
pulmonary atresia
o Have ab RV-PA conduit that is freely regurgitant because
it has no valve
o PA pressures NOT ELEVATED
o Diastolic murmur is LOW PITCHED and of SHORT
DURATION
LABORATORY EXAMINATION
• ECG may show findings of RVH and RA enlargement
• Chest x-ray: RV and RA may be enlarged
• Transthoracic Doppler echocardiography: pulmonic valve
morphology and function can
APPENDIX
Appendix A. Wilkins Scoring System for Mitral Valvuloplasty
INTERNAL MEDICINE II Milanes, Gwapo Marquez 35 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
If the score is 8 or less, then a favorable outcome is likely with PBMV
Highly mobile, "doming" anterior (AML) and posterior
(PML) mitral valve with slightly thickened leaflet tips.
Diastolic doming of tkhe thickened AML (“hockey stick”
appearance) is indicative of restricted anterior leaflet
motion. There is no evidence of sub-valvular thickening.
The echo score is 4.
The mitral leaflets are thickened and this thickening (SVTh)
extends below the leaflet tips into the subvalvar
apparatus. The echo score is 11.
Appendix B. Management of Mitral Stenosis
INTERNAL MEDICINE II Milanes, Gwapo Marquez 36 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
Appendix C. Mitral Stenosis Severity
Appendix D. Mitral Regurgitation Severity
Appendix E. Management of Mitral Regurgitation
INTERNAL MEDICINE II Milanes, Gwapo Marquez 37 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
Appendix F. Assessment of AS
Appendix G. Management strategy for patients with aortic stenosis
Appendix H. AR severity
INTERNAL MEDICINE II Milanes, Gwapo Marquez 38 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
Appendix I. Management of Aortic Regurgitation
Appendix J. Management of Tricuspid Regurgitation
Appendix K. Assessment of TR Severity
Appendix L. Abnormal CFD PR
INTERNAL MEDICINE II Milanes, Gwapo Marquez 39 of 40
INTERNAL MEDICINE II
(1 SEMESTER) |Heart Series #3 | August 24, 2021 |Dr. Eleazar Daet
ST
Heart Failure + Cardiomyopathy + Valvular Disease
Appendix M. Abnormal CWD PR
APPENDIX N. Murmurs
INTERNAL MEDICINE II Milanes, Gwapo Marquez 40 of 40
You might also like
- Congestive Heart FailureDocument13 pagesCongestive Heart FailureAgeng BudianantiNo ratings yet
- Echo Heart FailureDocument82 pagesEcho Heart FailureJing CruzNo ratings yet
- Heart Failure: Dr. Dr. Teuku Heriansyah, SP - JP (K) - FIHADocument42 pagesHeart Failure: Dr. Dr. Teuku Heriansyah, SP - JP (K) - FIHARudy LusmiandaNo ratings yet
- Heart Failure in Sub-Saharan Africa: A Clinical Approach: ReviewDocument9 pagesHeart Failure in Sub-Saharan Africa: A Clinical Approach: ReviewrizkaNo ratings yet
- Week9-10 VistalDocument6 pagesWeek9-10 VistalKier Elizalde VistalNo ratings yet
- CHF & CardiomyopathiesDocument25 pagesCHF & CardiomyopathiesDan HoNo ratings yet
- Pa 02 CardioDocument45 pagesPa 02 CardioElly NuñezNo ratings yet
- AnnCardAnaesth10119-300904 082130 PDFDocument8 pagesAnnCardAnaesth10119-300904 082130 PDFFirah Triple'sNo ratings yet
- Systolic Vs Diastolic Heart FailureDocument57 pagesSystolic Vs Diastolic Heart FailureRashiden MadjalesNo ratings yet
- Ongenital Eart Iseases: Iman Sulaiman Al-Hatmi 85569Document63 pagesOngenital Eart Iseases: Iman Sulaiman Al-Hatmi 85569Anişoara FrunzeNo ratings yet
- Board HF ManagementDocument48 pagesBoard HF ManagementNaufal BinseffNo ratings yet
- Congenital Heart DiseasesDocument52 pagesCongenital Heart DiseasesCristina Maria100% (1)
- Pathophysiology of Congenital Heart Diseases PDFDocument8 pagesPathophysiology of Congenital Heart Diseases PDFdramitjainNo ratings yet
- Pathophysiology of Congenital Heart Diseases PDFDocument8 pagesPathophysiology of Congenital Heart Diseases PDFkishanNo ratings yet
- Congenital Heart Diseases Practical Approach in Children With Heart MurmurDocument51 pagesCongenital Heart Diseases Practical Approach in Children With Heart Murmurdennyyy175No ratings yet
- Acut Heart FailureDocument20 pagesAcut Heart FailureCatherine MorrisNo ratings yet
- Overview Heart Failure: (Hfref, Hfpef)Document37 pagesOverview Heart Failure: (Hfref, Hfpef)Zaras Yudisthira SagaNo ratings yet
- Acute & Chronic Heart Failure: Dr. Nurkhalis, SPJP, FihaDocument98 pagesAcute & Chronic Heart Failure: Dr. Nurkhalis, SPJP, FihablackcatNo ratings yet
- Cardio Notes 2Document11 pagesCardio Notes 2AngieNo ratings yet
- Planning: Determine Patient's Clinical StatusDocument17 pagesPlanning: Determine Patient's Clinical StatusAsti DwiningsihNo ratings yet
- Congenital Heart Disease NotesDocument7 pagesCongenital Heart Disease NotesFarisa Jane BanggoNo ratings yet
- The Spectrum of Cardiac Manifestations in Coronavirus Disease 2019 (COVID-19) - A Systematic Echocardiographic StudDocument31 pagesThe Spectrum of Cardiac Manifestations in Coronavirus Disease 2019 (COVID-19) - A Systematic Echocardiographic StudsamuelNo ratings yet
- Congenital Heart DiseaseDocument12 pagesCongenital Heart DiseaseNinna Isabel VictorioNo ratings yet
- HeartFailure Nursing FIK 2014Document101 pagesHeartFailure Nursing FIK 2014Putri NurlaeliNo ratings yet
- World's Largest Science, Technology & Medicine Open Access Book PublisherDocument44 pagesWorld's Largest Science, Technology & Medicine Open Access Book PublisherireneaureliaNo ratings yet
- Clinical Assessment in Acute Heart Failure: Review ArticleDocument17 pagesClinical Assessment in Acute Heart Failure: Review ArticleAnonymous NeRC5JYiSNo ratings yet
- 1 CHFDocument62 pages1 CHFFalmeta EliyasNo ratings yet
- Heart FailureDocument48 pagesHeart Failurecoollist33100% (1)
- Cardiac DiseasesDocument8 pagesCardiac DiseasesTJ NgNo ratings yet
- A Mistake That Has Hurt No One: Sinus MistakusDocument4 pagesA Mistake That Has Hurt No One: Sinus MistakusasclepiuspdfsNo ratings yet
- Heart FailureDocument6 pagesHeart FailureNinna Isabel VictorioNo ratings yet
- The Spectrum of Cardiac Manifestations in Coronavirus Disease 2019 (COVID-19) - A Systematic Echocardiographic StudyDocument31 pagesThe Spectrum of Cardiac Manifestations in Coronavirus Disease 2019 (COVID-19) - A Systematic Echocardiographic Studyre septian IlhamsyahNo ratings yet
- AnticoagulantDocument38 pagesAnticoagulantyan salviantoNo ratings yet
- Surgery II: Congenital Heart DiseaseDocument10 pagesSurgery II: Congenital Heart DiseaseRea Dominique CabanillaNo ratings yet
- Complete Cardiac DiagnosisDocument2 pagesComplete Cardiac DiagnosisAria Jean MostajoNo ratings yet
- Heart Failure With Preserved Ejection Fraction HF PEF A Mini ReviewDocument3 pagesHeart Failure With Preserved Ejection Fraction HF PEF A Mini ReviewPaul HartingNo ratings yet
- Heart FailureDocument16 pagesHeart FailureAmalia CajesNo ratings yet
- Atrial Fibrillation 2021 - YCDocument24 pagesAtrial Fibrillation 2021 - YCHamza AldiriNo ratings yet
- Approach To A Patient With Congenital Heart DiseaseDocument164 pagesApproach To A Patient With Congenital Heart DiseaseCloudySkyNo ratings yet
- Congenital Heart Disease2Document126 pagesCongenital Heart Disease2api-19916399No ratings yet
- HHD 1Document10 pagesHHD 1Ardan RajasaNo ratings yet
- Cases of Cardiac Arrhythmia and Cardiac Failure: ForewordDocument16 pagesCases of Cardiac Arrhythmia and Cardiac Failure: Forewordpeter911x2134No ratings yet
- Lec 4Document9 pagesLec 4fbbqbcht6yNo ratings yet
- Diastolic Dysfunction Heart FailureDocument46 pagesDiastolic Dysfunction Heart FailureChadi Alraies100% (4)
- Drugs Used in Heart FailureDocument33 pagesDrugs Used in Heart FailureLynx Kee Bayating100% (1)
- Acyanotic Congenital Heart DiseaseDocument48 pagesAcyanotic Congenital Heart DiseasenabillagusrinaNo ratings yet
- Kelompok 15 Skenario 3Document24 pagesKelompok 15 Skenario 3Rachmad SammuliaNo ratings yet
- Congenital Heart DiseaseDocument5 pagesCongenital Heart Diseasesarguss14100% (1)
- Advances in Management of Heart Failure 0n 16.10.19Document50 pagesAdvances in Management of Heart Failure 0n 16.10.19Vijendra patleNo ratings yet
- Heart-Failure OConnor 11 1Document8 pagesHeart-Failure OConnor 11 1Muhammad Iqbal Al-islamyNo ratings yet
- Cardiac MurmursDocument3 pagesCardiac MurmursDanielleNo ratings yet
- Congenital Heart DefectsDocument9 pagesCongenital Heart DefectsSHAMAE FAITH FARRENNo ratings yet
- Heart Failure Lily ModifiedDocument57 pagesHeart Failure Lily ModifiedSabila FatimahNo ratings yet
- Chronic Congestive Heart Failure: Dr. Irwan, SPJPDocument115 pagesChronic Congestive Heart Failure: Dr. Irwan, SPJPMuhammad Arief Budiman YSNo ratings yet
- InPractice 2012 FelineCardiomyopathyDocument11 pagesInPractice 2012 FelineCardiomyopathyAngel ValdiviaNo ratings yet
- Brahmbhatt 2018Document7 pagesBrahmbhatt 2018Jr SparkNo ratings yet
- OB - Cardiovascular Disorders (LRA)Document6 pagesOB - Cardiovascular Disorders (LRA)Anonymous ANo ratings yet
- Module 2 ABC-CardioDocument7 pagesModule 2 ABC-Cardiomelba040510No ratings yet
- Congenital Heart Diseases (CHD) VoiceoverDocument50 pagesCongenital Heart Diseases (CHD) VoiceoverAmmar AlnajjarNo ratings yet
- Neurology Multiple Choice Questions With Explanations: Volume IIFrom EverandNeurology Multiple Choice Questions With Explanations: Volume IIRating: 5 out of 5 stars5/5 (2)
- Management of Anxiety and Other Non PsychoticDocument4 pagesManagement of Anxiety and Other Non PsychoticCRUZ Jill EraNo ratings yet
- Management of Mood Disorders - AnnotatedDocument6 pagesManagement of Mood Disorders - AnnotatedCRUZ Jill EraNo ratings yet
- Management of PD and Psychiatric - EmergenciesDocument8 pagesManagement of PD and Psychiatric - EmergenciesCRUZ Jill EraNo ratings yet
- 2.04 OBSTETRICS I Physiology of Labor Normal Labor and Abnormal LaborDocument14 pages2.04 OBSTETRICS I Physiology of Labor Normal Labor and Abnormal LaborCRUZ Jill EraNo ratings yet
- Rad2 - Group 4Document8 pagesRad2 - Group 4CRUZ Jill EraNo ratings yet
- 2016 - Observational Research Methods. Research Design II Cohort, Cross Sectional, and Case-Control StudiesDocument8 pages2016 - Observational Research Methods. Research Design II Cohort, Cross Sectional, and Case-Control StudiesamarillonoexpectaNo ratings yet
- Basic Biostatistics For Post-Graduate Students: Educational ForumDocument9 pagesBasic Biostatistics For Post-Graduate Students: Educational ForumSuryaprakash Reddy ChappidiNo ratings yet
- 1 Z5 Vya Lit 8 WR MC YAj 1 LPZDa QG 6 XM 8 V HGyDocument3 pages1 Z5 Vya Lit 8 WR MC YAj 1 LPZDa QG 6 XM 8 V HGyCRUZ Jill EraNo ratings yet
- Martinez Mesa 2016 Sampling How To Select ParticipantsDocument5 pagesMartinez Mesa 2016 Sampling How To Select Participantsdanilo alejandro garcia orjuelaNo ratings yet
- Head & Neck Rebyuwer - Lec & LabDocument41 pagesHead & Neck Rebyuwer - Lec & LabCRUZ Jill EraNo ratings yet
- PFCM - Screening TestsDocument7 pagesPFCM - Screening TestsCRUZ Jill EraNo ratings yet
- Medicine IM Platinum-1Document357 pagesMedicine IM Platinum-1Bom Tna67% (3)
- (MICROBIO) Viruses Reviewer (Edited Ver)Document33 pages(MICROBIO) Viruses Reviewer (Edited Ver)CRUZ Jill EraNo ratings yet
- (MICROBIO) Mycoses ReviewerDocument4 pages(MICROBIO) Mycoses ReviewerCRUZ Jill EraNo ratings yet
- The PARAGON-HF Trial: The Sacubitril/valsartan in Heart Failure With Preserved Ejection FractionDocument5 pagesThe PARAGON-HF Trial: The Sacubitril/valsartan in Heart Failure With Preserved Ejection FractionsumaNo ratings yet
- Cardio My OpathiesDocument61 pagesCardio My OpathiesIrina Cabac-PogoreviciNo ratings yet
- The ESC Textbook of Heart F - (Z-Library)Document1,038 pagesThe ESC Textbook of Heart F - (Z-Library)danielkevin19141No ratings yet
- Diastolic Heart Failure PDFDocument344 pagesDiastolic Heart Failure PDFOscar GasconNo ratings yet
- The ESC Handbook of Cardiovascular Rehabilitation 2020Document225 pagesThe ESC Handbook of Cardiovascular Rehabilitation 2020Daboin ZambranoNo ratings yet
- Challenging Cases in Neonatology 2018Document388 pagesChallenging Cases in Neonatology 2018Sabera Kapasi100% (1)
- Cardiovascular Physiology Case 9Document50 pagesCardiovascular Physiology Case 9Kim AcostaNo ratings yet
- Understanding Cardiac OutputDocument3 pagesUnderstanding Cardiac OutputAlexandra HerreraNo ratings yet
- PF Pathfath EquipoDocument6 pagesPF Pathfath EquipoWilliams Alejandro Choroco VillegasNo ratings yet
- Case Study 29Document2 pagesCase Study 29Edna MooreNo ratings yet
- Geriatric Assessment FormaDocument12 pagesGeriatric Assessment FormaAparna AbyNo ratings yet
- Total Summerized EMPA STUDIES 2Document51 pagesTotal Summerized EMPA STUDIES 2EslamNo ratings yet
- NCP - Decreased Cardiac Output Related To Altered Heart RateDocument2 pagesNCP - Decreased Cardiac Output Related To Altered Heart RateKian Herrera100% (1)
- Pulmonary Arterial Hypertension Pathogenesis and Clinical ManagementDocument27 pagesPulmonary Arterial Hypertension Pathogenesis and Clinical ManagementMr. LNo ratings yet
- Adriamycin (Doxorubicin) : Cardiotoxicity: A ReviewDocument5 pagesAdriamycin (Doxorubicin) : Cardiotoxicity: A ReviewnandaNo ratings yet
- Case Study Fnes 366Document6 pagesCase Study Fnes 366api-347761303No ratings yet
- Angadi, 2015Document6 pagesAngadi, 2015Prana JagannathaNo ratings yet
- Permanent Pacemaker Implantation / Box Change - A Guide To The ProcedureDocument5 pagesPermanent Pacemaker Implantation / Box Change - A Guide To The ProcedureSapna thakurNo ratings yet
- Test 3Document9 pagesTest 3jec9229No ratings yet
- SL Penyakit Jantung Pulmonal & HipertensiDocument24 pagesSL Penyakit Jantung Pulmonal & HipertensiReni MelindaNo ratings yet
- B.inggris KtiDocument61 pagesB.inggris KtiDimasNo ratings yet
- Gnaps EmedicineDocument13 pagesGnaps Emedicineharyanti lupitaNo ratings yet
- ST - WaterDocument7 pagesST - WaterlalitrajindoliaNo ratings yet
- Acute Coronary Syndrome, MI & ADHF-1Document28 pagesAcute Coronary Syndrome, MI & ADHF-1Hank WangNo ratings yet
- Case 3Document4 pagesCase 3Vien Marie Palaubsanon SilawanNo ratings yet
- Ati Pharmacology Study GuideetsyDocument49 pagesAti Pharmacology Study GuideetsyKarima Jones100% (4)
- Revised EMS Run SheetDocument2 pagesRevised EMS Run Sheetanon-939227100% (2)
- Medical and Cardiac Risk Stratification and Exercise Prescription in Persons With CancerDocument7 pagesMedical and Cardiac Risk Stratification and Exercise Prescription in Persons With CancermarciarigaudNo ratings yet
- Diabetes and Cardiovascular DiseaseDocument119 pagesDiabetes and Cardiovascular DiseaseAlina PopaNo ratings yet
- Heart Failure Pelatihan Dokter KeluargaDocument55 pagesHeart Failure Pelatihan Dokter KeluargaDelia NingrumNo ratings yet