Professional Documents
Culture Documents
NWCCH Abdominal Postop
Uploaded by
Shakya WeeraratneCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NWCCH Abdominal Postop
Uploaded by
Shakya WeeraratneCopyright:
Available Formats
DISCHARGE INSTRUCTIONS AFTER LAPAROSCOPIC OR OPEN ABDOMINAL SURGERY
WHAT TO EXPECT AFTER ABDOMINAL SURGERY
You will have some discomfort in your abdomen and your physician will give you a prescription
for pain medication to help make you comfortable.
You will likely be passing flatus but you may not yet have had a bowel movement
You may have irregularity to your usual BM habits.
DIET
A soft diet should be eaten for 1 to 2 weeks.
A soft diet should avoid raw fruits and vegetables, tough meats and spicy food.
You may want to eat 6 small meals a day and drink protein shakes in place of meals when you
are initially discharged home.
o Protein shakes include Ensure, Boost, and Carnation Instant Breakfast.
If you have an ileostomy or colostomy, you will have special instructions and will likely have met
with a nutritionist prior to discharge.
Drink at least 8 glasses of liquids daily to avoid dehydration (decreased or dark urine).
BOWEL FUNCTIION
Bowel function may be erratic at first
You may have some abdominal cramping with some good days and some bad days
Your bowel function may take several months to return to a normal pattern; it takes your body
time to adjust
If you have symptoms of mild abdominal cramps, bloating, nausea, vomiting, or absence of
passing gas or stool, you may restrict your diet to liquids only. If the symptoms persist beyond
24 hours or become severe, please call your physician.
ACTIVITY
Walking is good and climbing stairs in OK.
Avoid activity which causes pain.
Avoid lifting weights greater than 15-20 pounds or straining abdominal muscles (sit ups,
pushups, and weight lifting) for approximately 6 weeks. Ask your physician at your post op visit
when it is safe to increase your exercise regimen.
ABDOMINAL WOUNDS / INFECTIIONS
You will likely have pieces of skin colored tape on your abdominal incision or incisions
You may shower with soap and water and get the tape wet; pat dry
Leave the tape in place and use gauze only if you are having any drainage; change daily if
necessary. If the tape becomes loose or hanging, it is ok to remove it.
Keep your incisions protected from clothing, rubbing, etc. to decrease the risk of infection.
If you have excessive swelling, redness, drainage or severe pain around the incision, you should
call your physician
If you have a fever greater than 101 F you should contact your physician
If you have severe abdominal discomfort, nausea and vomiting, or feeling of being unwell,
please contact your physician
DRIVING
Do not drive for at least one week after discharge
Do not drive after taking pain medication
MEDICATIONS
You will be given a prescription for pain medication
If you need refills that are not included with your original prescription, please call the office
during office hours (M-F 9am to 5pm) to request a refill. Refills will not be given on
weekends/nights by the on-call physician. Allow 24-48 hrs for a refill.
Resume any medications your primary care physician has prescribed; you will be given a
medication discharge instruction sheet.
You may be given further instructions regarding fiber, anti-diarrheal medications, antibiotics,
steroids, or other medications
OSTOMY OR STOMA (if applicable)
You will receive instruction on how to care for your stoma while you are in the hospital and you
should feel comfortable with its care at the time of discharge.
If you have difficulty with keeping a pouching system on for at least 24 hours or if there is
recurrent bleeding, severe pain, swelling around the stoma, the stoma stops functioning, or the
stoma output is >1500cc in 24 hours, please call your physician.
Bananas, peanut butter, potato salad and tapioca will thicken the stool. Metamucil or other
powdered fiber supplements will also help.
FOLLOW UP APPOINTMENTS
Appointments are usually 3-6 weeks after your discharge.
Please call 503-216-5380 to arrange your postoperative appointmen
If you have any questions, concerns, or problems please call your physician.
If you have a medical problem that requires more immediate medical attention, please present to the
Emergency Department at St. Vincent Medical Center.
Call 503-216-5380 with any questions
You might also like
- Natural Medicine - 2016 October PDFDocument100 pagesNatural Medicine - 2016 October PDFDinh Ta HoangNo ratings yet
- Iodine Clock ReactionDocument3 pagesIodine Clock Reactionsunny_415No ratings yet
- DischargeDocument4 pagesDischargePatricia Franco100% (1)
- Rec To Vaginal Fistula RepairDocument7 pagesRec To Vaginal Fistula Repairnaftalina7No ratings yet
- Discharge PlanDocument5 pagesDischarge PlanrraksNo ratings yet
- Abdominal Rectopexy Operation: Your Questions AnsweredDocument5 pagesAbdominal Rectopexy Operation: Your Questions AnsweredlakanthNo ratings yet
- Gastric Sleeve Bariatric Cookbook: A Guide To Recovery (Complete With Healthy And Delicious Recipes)From EverandGastric Sleeve Bariatric Cookbook: A Guide To Recovery (Complete With Healthy And Delicious Recipes)No ratings yet
- Nausea and VomitingDocument7 pagesNausea and VomitingLady Nadjma M. LaoNo ratings yet
- Gastric Sleeve Cookbook: 77 Delicious and Healthy Gastric Sleeve Recipes with an Easy Guide to Being on the Gastric Sleeve DietFrom EverandGastric Sleeve Cookbook: 77 Delicious and Healthy Gastric Sleeve Recipes with an Easy Guide to Being on the Gastric Sleeve DietNo ratings yet
- Nutrition For Cancer Patients During Treatment Part 2Document10 pagesNutrition For Cancer Patients During Treatment Part 2reading4chNo ratings yet
- Gastric Sleeve Cookbook: A Food Guide to Stages One and Two of Your Gastric Sleeve Surgery RecuperationFrom EverandGastric Sleeve Cookbook: A Food Guide to Stages One and Two of Your Gastric Sleeve Surgery RecuperationRating: 3.5 out of 5 stars3.5/5 (3)
- Pain Free in One DayDocument24 pagesPain Free in One DayDama FortunaNo ratings yet
- Barium MealDocument3 pagesBarium MealVithiya Chandra SagaranNo ratings yet
- Guide For Eating After Gastric Bypass SurgeryDocument42 pagesGuide For Eating After Gastric Bypass Surgerymolly brown100% (1)
- Type Test Verification SafePlus 12 24 KVDocument8 pagesType Test Verification SafePlus 12 24 KVGary FortuinNo ratings yet
- Postpartum Discharge PlanDocument2 pagesPostpartum Discharge PlanGlaizalyn Fabella Tagoon75% (12)
- Mercaptans Removal From Gases by Absorption Into Amines and CausticDocument8 pagesMercaptans Removal From Gases by Absorption Into Amines and Causticgopal100% (1)
- Biolis 24i PDFDocument43 pagesBiolis 24i PDFMohamed Ben MohamedNo ratings yet
- Post Op Management Following Surgery For Rectal ProlapseDocument2 pagesPost Op Management Following Surgery For Rectal ProlapseChris NewallNo ratings yet
- Postpartum Discharge PlanDocument2 pagesPostpartum Discharge PlanNielette R. BASAL100% (1)
- Laparoscopic Cholecystectomy: Patient InformationDocument2 pagesLaparoscopic Cholecystectomy: Patient InformationAnne Marie Angelica BilonoNo ratings yet
- 2016 08 Factsheet - MM Nature SpanishDocument2 pages2016 08 Factsheet - MM Nature SpanishHE HNo ratings yet
- Laparoscopic Heller Myotomy For AchalasiaDocument2 pagesLaparoscopic Heller Myotomy For AchalasiaJessa JessNo ratings yet
- Devona MangaDocument5 pagesDevona MangaANGEL DE JESUS GONZALEZ - OLIVASNo ratings yet
- Hemorrhoidectomy Care 8 12 - tcm75 618832Document3 pagesHemorrhoidectomy Care 8 12 - tcm75 618832Seceleanu MarianNo ratings yet
- Instr HystDocument2 pagesInstr HystRashmi BalagopalNo ratings yet
- METHODSDocument2 pagesMETHODSBtob meloNo ratings yet
- Diarrhea JPNDocument6 pagesDiarrhea JPNShawnNo ratings yet
- HysterectomyDocument3 pagesHysterectomyNari BurathiNo ratings yet
- Discharge Deck - FINAL 2020Document44 pagesDischarge Deck - FINAL 2020Zion OlmosNo ratings yet
- Anal Fissure Post OpDocument5 pagesAnal Fissure Post OpRitesh BharambeNo ratings yet
- Postpartum Discharge Instructions - Howard County General Hospital, Johns Hopkins MedicineDocument7 pagesPostpartum Discharge Instructions - Howard County General Hospital, Johns Hopkins MedicineA.No ratings yet
- General Advice Following Hepatobiliary and Pancreatic SurgeryDocument8 pagesGeneral Advice Following Hepatobiliary and Pancreatic SurgeryiweNo ratings yet
- Bowel Prep ProtocolDocument9 pagesBowel Prep ProtocolGillìan KìrbyNo ratings yet
- Discharge Instructions For Laparoscopic AppendectomyDocument1 pageDischarge Instructions For Laparoscopic AppendectomyNguyễn Mạnh CườngNo ratings yet
- Nursing ManagementDocument2 pagesNursing ManagementCindy MamalangkasNo ratings yet
- Scenario Flow and ScriptDocument6 pagesScenario Flow and ScriptJhoneric Vencer EscultorNo ratings yet
- Alliance Obgyn Prenatal Obstetrical CareDocument7 pagesAlliance Obgyn Prenatal Obstetrical CareArnette LingatNo ratings yet
- Discharge Plan 3Document3 pagesDischarge Plan 3minjungNo ratings yet
- Discharge Instructions For Hemorrhoid Surgery: Home CareDocument2 pagesDischarge Instructions For Hemorrhoid Surgery: Home CareKath ReignNo ratings yet
- Post-Operative Instructions: Laparoscopic CholecystectomyDocument2 pagesPost-Operative Instructions: Laparoscopic Cholecystectomyrizwan234No ratings yet
- What Is A Total Abdominal Hysterectomy?Document8 pagesWhat Is A Total Abdominal Hysterectomy?Iuthisam HassanNo ratings yet
- Discharge Planning FDocument2 pagesDischarge Planning FJameseu KimNo ratings yet
- Laparoscopic Cholecystectomy 8-12 - tcm75-618838Document4 pagesLaparoscopic Cholecystectomy 8-12 - tcm75-618838zaid maythamNo ratings yet
- Nursing ManagementDocument6 pagesNursing ManagementLoraine CastilloNo ratings yet
- Lap CholeDocument1 pageLap Cholerizwan234No ratings yet
- Nutrition Education 1-1Document1 pageNutrition Education 1-1api-254031084No ratings yet
- XELOX Chemotherapy Guide: For Patients With Colorectal CancerDocument32 pagesXELOX Chemotherapy Guide: For Patients With Colorectal CancerBeatrice FiranNo ratings yet
- TurbtDocument3 pagesTurbtAl-nazer Azer AlNo ratings yet
- Mater Health Preparing For Your Colonoscopy A5 Booklet Mar2021 V5 WEBDocument12 pagesMater Health Preparing For Your Colonoscopy A5 Booklet Mar2021 V5 WEB25hdf89v57No ratings yet
- Ureteral Reimplant Surgery Home Care FactsheetDocument3 pagesUreteral Reimplant Surgery Home Care FactsheetEmilia AndreiNo ratings yet
- Discharge Instructions After FistulotomyDocument3 pagesDischarge Instructions After FistulotomyUsername374100% (1)
- GIE Colonscopy Prep and Diet GuideDocument4 pagesGIE Colonscopy Prep and Diet GuideNiar MarhaliNo ratings yet
- Caregiver Guide - Constipation ProblemsDocument11 pagesCaregiver Guide - Constipation ProblemsHayuta WatamotoNo ratings yet
- After Your Caesarean SectionDocument8 pagesAfter Your Caesarean SectionAmy PainterNo ratings yet
- Discharge Instructions For Laparoscopic AppendectomyDocument1 pageDischarge Instructions For Laparoscopic AppendectomyLokesh PutturNo ratings yet
- Minor Ailments:: (Morning Sickness)Document14 pagesMinor Ailments:: (Morning Sickness)Blackcat KememeyNo ratings yet
- Instructions Post Operative Care Following Hysterectomy Abdominal SurgeryDocument4 pagesInstructions Post Operative Care Following Hysterectomy Abdominal SurgerysujanNo ratings yet
- PIN0638 Female Incontinence v1Document5 pagesPIN0638 Female Incontinence v1Shamsuddin HasnaniNo ratings yet
- Information and Advice Following Rectal/anal Surgery: Oxford University HospitalsDocument4 pagesInformation and Advice Following Rectal/anal Surgery: Oxford University HospitalsChitra nanjappaNo ratings yet
- Information and Advice Following Rectal/anal Surgery: Oxford University HospitalsDocument4 pagesInformation and Advice Following Rectal/anal Surgery: Oxford University HospitalsChitra nanjappaNo ratings yet
- Analsurgery PDFDocument4 pagesAnalsurgery PDFChitra nanjappaNo ratings yet
- Joe Y.B. Lee, MD: Preoperative, Postoperative and Home Recovery InstructionsDocument5 pagesJoe Y.B. Lee, MD: Preoperative, Postoperative and Home Recovery InstructionsLinda SugiartoNo ratings yet
- Nasogastric Tube Feeding ML4763 PDFDocument7 pagesNasogastric Tube Feeding ML4763 PDFStereo PodNo ratings yet
- Ileoscopy Prep 12.2019Document2 pagesIleoscopy Prep 12.2019Ahmed GhanimNo ratings yet
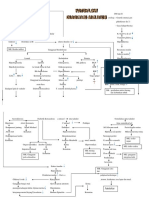
- Patoflow DMDocument2 pagesPatoflow DMAngel da CostaNo ratings yet
- Master of International HealthDocument5 pagesMaster of International HealthJesper Domincil BayauaNo ratings yet
- Access To JusticeDocument9 pagesAccess To JusticeprimeNo ratings yet
- Siklus Biogeokimia - Retensi NutrienDocument24 pagesSiklus Biogeokimia - Retensi NutrienPutri Nur Fadhilah YasharNo ratings yet
- Lab 2 - Capacitive ReactanceDocument4 pagesLab 2 - Capacitive Reactanceali basitNo ratings yet
- The Internet Test 9th Grade A2b1 Tests 105573Document5 pagesThe Internet Test 9th Grade A2b1 Tests 105573Daniil CozmicNo ratings yet
- SAVULESCU, Julian - A Simple Solution To The Puzzles of End of LifeDocument5 pagesSAVULESCU, Julian - A Simple Solution To The Puzzles of End of Lifediradosta_1992No ratings yet
- 94 175 1 SM PDFDocument8 pages94 175 1 SM PDFikaNo ratings yet
- Arrival Guide To MalaysiaDocument2 pagesArrival Guide To Malaysiaamanu092No ratings yet
- Comparative Study of Different Varieties of Rice For Making Homemade Instant CoffeeDocument9 pagesComparative Study of Different Varieties of Rice For Making Homemade Instant CoffeeJhon Kyle RoblesNo ratings yet
- MAPEH Assignment For Mr. Felicilda (Only)Document6 pagesMAPEH Assignment For Mr. Felicilda (Only)Jericho Green Gerona100% (1)
- Spoilage of Frozen Chicken Nuggets by Toxigenic Psycrophilic FungiDocument16 pagesSpoilage of Frozen Chicken Nuggets by Toxigenic Psycrophilic FungiNIDHI BARINo ratings yet
- Manual Fritadeira PDFDocument136 pagesManual Fritadeira PDFtherasiaNo ratings yet
- ADPKDDocument75 pagesADPKDVenkataramanan KrishnamoorthyNo ratings yet
- Electrochemistry NotesDocument4 pagesElectrochemistry NotesAyush RorNo ratings yet
- Cable Test Bridge KMK 7Document2 pagesCable Test Bridge KMK 7zaki3speedNo ratings yet
- NURS FPX 6410 Assessment 2 Executive Summary To AdministrationDocument7 pagesNURS FPX 6410 Assessment 2 Executive Summary To Administrationzadem5266No ratings yet
- Cord Care Evaluation ToolDocument1 pageCord Care Evaluation ToolCherry AnnNo ratings yet
- Shabeer Et Al-2018-Journal of PerinatologyDocument8 pagesShabeer Et Al-2018-Journal of PerinatologyrenataNo ratings yet
- Volume Booster: YT-300 / YT-310 / YT-305 / YT-315 / YT-320Document1 pageVolume Booster: YT-300 / YT-310 / YT-305 / YT-315 / YT-320SeikatsukaiNo ratings yet
- Substation Off Line and Hot Line CommissioningDocument3 pagesSubstation Off Line and Hot Line CommissioningMohammad JawadNo ratings yet
- 150.66-RP4 YcalDocument92 pages150.66-RP4 YcalJosé RamosNo ratings yet
- Ucrete SpecsDocument10 pagesUcrete SpecspsrikanthanNo ratings yet
- Formulating A Dental Treatment Plan: DR Tashnim BagusDocument33 pagesFormulating A Dental Treatment Plan: DR Tashnim BagustarekrabiNo ratings yet
- Effects of Career Plateau On Job Satisfaction and MotivationDocument105 pagesEffects of Career Plateau On Job Satisfaction and Motivationalanwil100% (1)