Professional Documents
Culture Documents
Resource Material For Emnc October 2023
Uploaded by
Jeamine Talaver PalenciaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Resource Material For Emnc October 2023
Uploaded by
Jeamine Talaver PalenciaCopyright:
Available Formats
TOPIC: ESSENTIAL MATERNAL NEWBORN CARE (EMNC)
LEARNING OBJECTIVES:
1. Perform immediate assessment of an example pregnant client shown in video in labor
2. Classify the Essential Maternal Newborn Care (EMNC)
3. Perform the proper steps in the actual delivery of newborn using the online video presentation /link
4. To deliver time-bound core intervention in the immediate period after the delivery of the newborn
5. Monitor during labor process with the use of partograph using video presentation
6. Practice how to deliver the baby and placenta correctly and aseptically using available material at home
7. Provide immediate care of the newborn using the online video and checklist
8. Perform thorough assessment of the actual postpartum client and her
newborn based on the video and checklist
9. Evaluate the outcomes of care provided to the client
The EINC practices are evidenced based standards for safe and quality care of birthing mothers and their
newborns, within the 48 hours of intrapartum period (labor and delivery) and a week of life for the newborn.
It is a package of evidenced-based practices recommended by the Department of Health (DOH),
Philippine Health Insurance Corporation (PhilHealth), and the World Health Organization (WHO) as the standard of
care in all births by skilled attendants in all government and private settings.
It is a basic component of DOH’s Maternal. Newborn and Child Health and Nutrition (MNCHN) strategy.
Essential lntrapartum and Newborn care (EINC) is the standard of care in all births by skilled attendants in all
government/private settings.
The EINC practices for newborn care constitute a series of time bound. Chronologically ordered; standard
procedures that a baby receives at birth.
At the heart of the protocol are 4 time-bound interventions:
1) immediate drying;
2) skin-to-skin contact followed by clamping of the cord after 1-3 minutes;
3) non-separation of baby from mother
4) breastfeeding initiation
Why is there a need for Essential Newborn Care Protocol?
The wide variations in newborn care practices in health facilities, both government and private, and also the
proper sequence or order of newborn care services need to be standardized based on current evidences that show
reduction in neonatal mortality and morbidity.
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
This is to achieve the United Nations Millennium Development Goal 4 of Reducing Under 5 Child Mortality
(through reduction of neonatal deaths).
Essential Maternal and Newborn Care (EMNC) Evidence-based Standard Practices .
The EMNC practices are evidenced-based standards for safe and quality care of birthing mothers and their
newborns, within the48 hours of Intrapartum period (labor and delivery) and a week of life for the newborn.
Developed and field tested by international and local experts, EMNC practices reflect current kknowledge.
EMNC distinguishes the necessary practices in the delivery and care for the newborn and the mother, from the
unnecessary. In December 2009, the Secretary of the Department of Health Francisco Duque signed Administrative
Order 2009-0025, which mandates implementation of the EMNC Protocol in both public and private hospitals.
Likewise, the Unang Yakap campaign was launched.
The EMNC practices during Intrapartum period
Continuous maternal support, by a companion of her choice, during labor and delivery
Mobility during labor – the mother is still mobile, within reason, during this stage
Position of choice during labor and delivery
Non-drug pain relief, before offering labor anesthesia
Spontaneous pushing in a semi-upright position
Episiotomy will not be done, unless necessary
Active management of third stage of labor (AMTSL)
Monitoring the progress of labor with the use of partograph
Government and international Support
Since 2010, WHO supports the DOH in changing practices for safe and quality care of mothers and newborns for all
practitioners and health facilities. It was initially implemented in 11 selected government hospitals collectively
representing about 70,000 annual live births (around 3% of all national live births). USAID also provided support
through the Joint Programme on Maternal and Neonatal Health (JPMNH).
PREPARATION:
Materials needed -in linear sequence
2 pairs of gloves
2 Dry linens
Bonnet
Oxytocin injection
Plastic clamp
Iinstrument clamp (#1 straight Kelly clamp)
Scissors
2 kidney basins
IN A SEPARATE SEQUENCE, FOR AFTER THE 1ST BREASFEED:
Eye ointment
Stethoscope
Vitamin K injection
Hepatitis B
BCG Vaccine
Cotton Balls- wet and dry
PREPARATION:
1. Prepares decontamination solution by mixing part 5% chlorine bleach to 9 parts water to make 0.5% chlorine
bleach to 9 parts water to make 0.5% chorine solution.
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
2. Change chlorine solution at the beginning of each day or whenever prior to woman’s transfer to the delivery
room
3. Ensures that mother is in her position of choice while in labor
4. Asks the mother if she wants to drink or void
5. Communicates with the mother. Inform her of the progress of labor, give assurance and
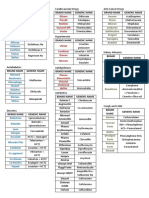
PARTOGRAPH
The partograph is a graphical presentation of the progress of labor, and of fetal and maternal condition during
labor. It is the best tool to help you detect whether labor is progressing normally or abnormally, and to warn you
as soon as possible if there are signs of fetal distress or if the mother’s vital signs deviate from the normal range.
The partograph is a tool for monitoring maternal and fetal wellbeing during the active phase of labor, and a
decision-making aid when abnormalities are detected. It is designed to be used at any level of care. Its central
feature is a graph used to record the progress of cervical dilation, as determined by vaginal examination. Start the
graph at 5 cm of dilation, and 3 contractions every 10 minutes. In certain situations, e.g. induction of labor, it is
started at 4 cm of dilation. Indicators are plotted on the graph each time they are checked:
Maternal indicators:
• Vital signs (heart rate, blood pressure and temperature)
• Time of spontaneous or artificial rupture of the membranes
• Uterine contractions (number per 10 minutes and duration)
• Urine output
• Drugs administered (oxytocin, antibiotics, etc.)
Fetal indicators:
• Fetal heart rate
• Amniotic fluid (color, odor and quantity)
• Descent of the fetal head and head molding
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
WOMAN ALREADY IN THE DELIVERY ROOM
PREPARATION FOR DELIVERY
6. Checks the temperature in delivery room area to be 25-28 `C . Eliminates air draft
7. Asks woman if she is comfortable in the semi-upright position (The fault position of the delivery table)
8. Ensures the woman’s privacy
9. Removes all jewelry then wash hands thoroughly observing the WHO 1-2-3-4-5 procedures
10. Prepares a clear, clean newborn resuscitation area. Checks the equipment if clean, functional within easy
reach.
11. Arranges materials/supplies in a linear sequence:
- 2 gloves,2 dry linen, bonnet, oxytocin injection, plastic clamp, instrument clamp, scissor, 2 kidney basins
IN A SEPARATE SEQUENCE FOR AFTER THE 1ST BREASTFEED:
Eye ointment
Stethoscope
Vitamin K injection
Hepatitis vaccine
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
BCG Vaccine
Dry and wet cotton balls
12. Cleans the perineum with antiseptic solution
13.Washes hands and put on 2 pairs of sterile gloves aseptically (if same worker handles perineum and cord)
AT THE TIME OF DELIVERY
14. Encourages woman to push as desired
15. Drapes the clean, dry linen over the mother’s abdomen or arms in preparation for drying the baby
16. Applies perineal support and did controlled delivery of the head
Modified Ritgen’s maneuver is done by covering the anus with sterile
towel and exert upward and forward pressure on the fetal chin while
exerting gentle pressure with two fingers on the head to control the
emerging head. This will not only support the perineum, thus the also favor flexion so that the smallest
suboccipitobregmatic diameter of the fetal head is presented.
Ease the baby’s head out and immediately wipe the nose and mouth of secretions to establish a patent airway
(REMEMBER: the first principle in the care of the newborn is to establish and maintain a patent airway) The head
should be delivered in between contractions.
17. Calls out time of birth and sex of the baby
Take note of the exact time of delivery of the baby, proper sex identification. Allowing the mother to see the status
of the baby.
18. Informs the mother of outcome
MECHANISMS OF LABOR (CARDINAL MOVEMENTS)
Engagement
This is when the largest diameter of the fetal head descends into the maternal pelvis.
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
The term engagement is referring to the widest part of the fetal head successfully negotiating its way down deep
into the maternal pelvis. Engagement is identified by abdominal palpation, where the fetal head is 3/5th palpable
or less.
Descent
The fetus descends into the pelvis. In the primigravida this is likely to occur from 38 weeks gestation onwards, in a
multigravida woman, this may not occur until labor is established.
Descent is encouraged by:
Increased abdominal muscle tone
Braxton hicks in late stages of pregnancy
Fundal dominance of the uterine contractions during labor
Increased frequency and strength of contractions during labor
As the head descends, it moves towards the pelvic brim in either the left or right occipito-transverse position (this
means the occiput can be facing the left side or right side of the mother’s pelvis).
Flexion
As the fetus descends through the pelvis, fundal dominance of uterine contraction exerts pressure down the fetal
spine towards the occiput, forcing the occiput to come into contact with the pelvic floor. When this occurs the fetal
neck flexes (chin to chest) allowing the circumference of the fetal head to reduce to sub-occipitobregmatic
(9.5cm). In this position, the fetal skull has a smaller diameter which assists passage through the pelvis.
Internal Rotation
The pelvic floor has a gutter shape with a forward and downward slope, encouraging the fetal head to rotate
from the left or right occipito-transverse position a total of 90-degrees, to an occipital-anterior (occiput facing
forward) position, to lie under the subpubic arch.
With each maternal contraction, the fetal head pushes down on the pelvic floor. Following each contraction, a
rebound effect supports a small degree of rotation. Regular contractions eventually lead to the fetal head
completing the 90-degree turn.
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
This rotation will occur during established labor and it is commonly completed by the start of the second
stage. Further descent leads to the fetus moving into the vaginal canal and eventually, with each contraction, the
vertex becomes increasingly visible at the vulva.
Crowning
When the widest diameter of the fetal head successfully negotiates through the narrowest part of the
maternal bony pelvis, the fetal head is considered to be ‘crowning’. This is clinically evident when the head, visible
at the vulva, no longer retreats between contractions. Complete delivery of the head is now imminent and often
the woman, who has been pushing, is encouraged to pant so that the head is born with control.
Extension
Extension of the presenting part. The occiput slips beneath the suprapubic arch allowing the head to extend. The
fetal head is now born and will be facing the maternal back with its occiput anterior.
External Rotation/Restitution
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
Because the shoulders at the point of the head being delivered are only just reaching the pelvic floor they are often
still negotiating the pelvic outlet and the fetus may naturally align its head with the shoulders. This is called
restitution and visually you may see the head externally rotate to face the right or left medial thigh of the mother.
Expulsion
Downward traction by the healthcare professional will assist the delivery of the anterior shoulder below the
suprapubic arch. This is followed by upward traction assisting the delivery of the posterior shoulder. The fetal body
will be delivered by the contractions, the health professional’s role is only to assist safe negotiation of this last
stage.
As the head rotates, deliver the anterior shoulder by exerting a gentle downward push and then slowly give an
upward lift to deliver the posterior shoulder. While supporting the head and the neck, deliver the rest of the body.
The infant is grasped around the back with the left hand, and the right hand is placed, near the vagina under the
baby’s buttocks, supporting the infant’s body.
Immediately after the delivery of the newborn should be held below the level of the mother’s vulva for a few
minutes to encourage flow of blood from the placenta to the baby.
The infant held with his head in a dependent position (head lower than the rest of the body) to allow for drainage
of secretions.
REMEMBER: Never stimulate a baby to cry unless you have drained him out of his secretions first.
Mechanism of Labor
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
FIRST 30 SECONDS
19.Thoroughly dries the baby for at least 30 seconds, starting from the face and the head, going down to the trunk
and extremities while performing a quick check for breathing.
1-3 MINUTES
20. Removes the wet cloth
21.Place the baby in skin to skin contact on the mother’s abdomen or chest
22.Covers baby with the dry cloth and the baby’s head with a bonnet .This prevents hypothermia, infection, and
hypoglycemia
23. Excludes a second baby by palpating the abdomen in preparation for giving oxytocin
24. Uses wet cloth to wipe the soiled gloves. Gives oxytocin within one minute of baby’s birth. Disposes of wet
cloth properly
25. Removes ist gloves and decontaminate them properly (in 0.5% chlorine solution for at least 10 minutes)
26. Palpates umbilical cord to check for pulsations
Do not milk the cord towards the baby– After the 1st clamp, you may“ strip ” the cord– After the 1st clamp , you
may “strip” the cord of blood before applying the 2nd clamp– Cut the cord close to the plastic clamp so that there
is no need for a 2nd “trim”– Do not apply any substance onto the cord
27. After pulsation stopped, clamps cord using the plastic clamp or cord or tie 2 cm. From the base. Prevents
anemia and protects against brain hemorrhage in premature newborn.
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
28. Place the instrument clamp 5 cm. From the base
29. Cuts near plastic clamp (midways)
30. Performs the remaining steps of the AMTSL (Active management of the third stage of labor)
Waits for strong uterine contractions then applies controlled cord traction and counter traction on the uterus,
continuing until placenta is delivered
-Massages the uterus until firm and contracted
PLACENTAL DELIVERY
The third stage of labor refers to the period following the completed delivery of the newborn until the completed
delivery of the placenta. Relatively little thought or teaching seems to be devoted to the third stage of labor
compared with that given to the first and second stages. The placenta is a unique organ of pregnancy that
nourishes your baby. Typically, it attaches to the top or side of the uterus. The baby is attached to the placenta via
the umbilical cord. After your baby is delivered, the placenta follows. This is the case in most births. But there are
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
some exceptions. Delivery of the placenta is also known as the third stage of labor. Delivery of the entire placenta
is vital to a woman’s health after giving birth. Retained placenta can cause bleeding and other unwanted side
effects. For this reason, a doctor will examine the placenta after delivery to ensure that it is intact. If a piece of
placenta is left in the uterus, or the placenta doesn’t deliver, there are other steps a doctor can take.
The following 3 classic signs indicate that the placenta has separated from the uterus :
A. The uterus contracts and rises.
B. The umbilical cord suddenly lengthens.
C. A gush of blood occurs.
Two types of placental separation:
A. Duncan’s Method
B. Shultz Method
Schultz Method- Shiny side
- Placenta separates in the center and folds in on itself as it descends into the lower part of uterus
(80%). Fetal surface appears at vulva with membranes trailing behind
- Minimal visible blood loss as retroplacental clot contained within membranes (inverted sac)
Duncan Method - Dirty side
- It is the separation starts at the lower edge of placenta lateral border separates (20%).
- maternal surface appears first at vulva. Usually accompanied by more bleeding
from placental site due to slower separation and no retro placental clot.
Tract the cord slowly, winding it around the clamp until placenta spontaneously comes out,
rotating it slowly so that no membranes are left inside the uterus, a method called Brandt
Andrews Maneuver.
31. Inspects the lower vagina and perineum for lacerations/ tears and repaired lacerations /tears as necessary
32. Examines the placenta for completeness and abnormalities
Active management:
Involves an injection of a drug called syntocinon or ergometrine in your thigh soon after your
baby’s born.
It speeds up the delivery of the placenta – it usually happens within 30 minutes of having your
baby. Your midwife will push on your uterus and pull the placenta out by the umbilical cord.
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
You’ll have the umbilical cord cut between one and five minutes after you give birth.
Early cord clamping reduces the amount of blood your baby gets from you at birth by about
20%. But this also makes it less likely they’ll get neonatal jaundice that needs treatment.
It lowers the risk of heavy blood loss.
It might make you feel sick or vomit, and can increase your risk of high blood pressure.
33. Cleans the mother, flushes perineum and applies perineal pad/ napkin/ cloth
34. Checks baby’s color and breathing checks that mother is comfortable, uterus contracted and firm
35. Disposes of the placenta in a leak proof container or plastic
36. Decontaminates (soaked in 5% chlorine solution) (instruments before cleaning decontaminates 2nd pair of
gloves before disposal, starting that decontamination lasts for at least 10 minutes.
37. Advices mother to maintain skin to skin contact. Baby should be in prone position on mother’s chest in
between the breasts with head turned to one side.
Continues non-separation of newborn and mother for early breastfeeding protects infants from drying from
infection.
15 TO 90 MINUTES
38. Advices mother to observe for feeding cues and cited examples of feeding cues
Look for signs of good attachment and suckling:
− Mouth wide open
− Lower lip turned outward
− Baby’s chin touching breast
− Suckling is slow, deep with some pauses
− If the attachment or suckling is not good, try again and reassess.
39. Supports mother, instructs her on positioning and attachment
40. Wait for full breastfeed to be completed. The first feed provides colostrum.
41. After a complete breastfeed, administer eye ointment (first do thorough physical examination , then give
vitamin K and Hepatitis and BCG injection)
Eye ointment application
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
Vitamin K injection
Hepatitis B vaccine injection
42. Advises (optional delayed) bathing of baby.
43. Advices breastfeeding per demand
44. In the first hour, check the baby’s breathing and color, and check mother’s vital signs and massages the uterus
every 15 minutes and document
45. In the second hour, checks mother - baby dyad every 30 minutes to I hour
Mother-baby dyad care, including skin-to-skin contact of healthy infants and mothers, is an important component
of maternal-newborn care. Beginning at birth, mothers and newborns should be viewed as a unit with no
disruption of the parent-infant relationship.
46.Documents and completes all records
POSTPARTUM PERIOD
Immediately after delivery of a baby, the mother is monitored for at least 1 hour. If an
anesthetic was used during delivery or if there were any problems during delivery, she may be
monitored for several hours after delivery, usually in a well-equipped recovery room with access
to oxygen, intravenous fluids, and resuscitation equipment.
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
Staff members check the mother’s pulse rate and temperature. Normally, within the first 24
hours, the mother’s pulse rate (which increased during pregnancy) begins to decline toward
normal and her temperature may increase slightly, usually returning to normal during the first
few days. After the first 24 hours, recovery is rapid. They make every effort to minimize the new
mother’s pain and the risk of bleeding and infection.
Bleeding
Minimizing bleeding is the first priority. After delivery of the placenta (afterbirth), a nurse may
periodically massage the mother’s abdomen to help the uterus contract and remain contracted,
thus preventing excessive bleeding.
If needed, oxytocin is given to stimulate contraction of the uterus. The drug is injected into a muscle or
given intravenously as a continuous infusion until the uterus is contracted.
If women lose a lot of blood during and after delivery, a complete blood count is done to check
for anemia before they are discharged.
Urination
Urine production often increases greatly, but temporarily, after delivery. Because bladder
sensation may be decreased after delivery, hospital staff members encourage a new mother to
try to urinate regularly, at least every 4 hours. Doing so avoids overfilling the bladder and helps
prevent bladder infections. Staff members may gently press on the mother’s abdomen to check
the bladder and determine whether it is being emptied.
Occasionally, if the new mother cannot urinate on her own, a catheter must be inserted
temporarily into the bladder to empty the urine. Hospital staff members try to avoid using an
indwelling catheter (a catheter that is left in the bladder for a period of time). This type of
catheter increases the risk of bladder and kidney infections.
Defecation
The new mother is also encouraged to defecate before leaving the hospital. But because
hospital stays are so short, this expectation may not be practical. Doctors may recommend that
if she has not defecated within 3 days, she take laxatives to avoid constipation, which can cause
or worsen hemorrhoids. If the rectum or muscles around the anus were torn during delivery,
doctors may prescribe stool softeners.
Opioids, which are occasionally given after cesarean delivery to relieve severe pain, can worsen
constipation. So if an opioid is needed, the lowest effective dose of such drugs is used.
Diet and exercise
A new mother can have a regular diet as soon as she wants it, sometimes shortly after delivery.
She should get up and walk as soon as possible. A new mother can start exercises to strengthen
abdominal muscles, often after 1 day if delivery was vaginal and later if it was cesarean. Curl-ups
with bent knees, done in bed, are effective. However, most women are too tired to start
exercising so soon after delivery.
Before discharge
Before a new mother leaves the hospital, she is examined. If mother and baby are healthy, they
commonly leave the hospital within 24 to 48 hours after vaginal delivery and within 96 hours
after a cesarean delivery. Sometimes discharge is as early as 6 hours if no general anesthetic was
used and no problems occurred. The mother is given information about changes to expect in her
body and measures to take as her body recovers from having a baby. Regular follow-up visits are
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
scheduled, usually starting at 6 weeks after delivery. If delivery was cesarean or if problems
occurred, the first visit may be scheduled sooner.
References:
Department of Health. (2009, December 1). Unang Yakap: Essential Newborn Care [Video]. Government
Website.https://www.doh.gov.ph/unang-yakap
Greek Medics (June 2018). Mechanism of Labor and Fetal Position- OSCE GUIDE [Video]. YouTube.
https://www.youtube.com/watch?v=ruIa1bC4tsw
Medical Aid Films - Films for Life. (2013, September 11). How to use a partograph to assess women in labor
[Video].YouTube.https://www.youtube.com/watch?v=hTh5MJFzgPY
Pilliteri, A. (2009). Maternal & Child Health Nursing: Care of the Childbearing & Childrearing Family (Maternal and
Child Health Nursing). LWW; Sixth, North American edition.
Tan, T. (2015). Performance Evaluation Tool/Manual Procedure.
University of Nottingham Division of Midwery (2010). Mechanism of labor [Video]. You
tube.https://www.youtube.com/watch?v=2kM35XMMiPk
World Health Organization (2009). Newborn Care Until the First Week of life. [File].Government
Website.http://caro.doh.gov.ph/wp-content/uploads/2014/09/EINC.pdf.
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
Immediate Care of the Newborn in the Delivery room
Learning Objectives:
Understand about the care of newborn (i.e. immediate and routine care)
Discuss about warmth, care of skin, eyes, and care of cord etc.
Discuss about immunization and breast feeding.
Explain about the follow up care and general observation of the newborn.
Use relevant data and information to develop appropriate essential newborn recommendations.
A. Principle No. 1:
Establish and maintain a patent airway.
1. The newborn’s position should be one which promotes the drainage of secretion (head lower than the rest of
the body), except when there are signs of increasing intracranial pressure.
(e.g. shrill, high-pitched cry; vomiting; tense, bulging anterior fontanelle; abnormally large head) in which case, the
head should be positioned higher than the rest of the body.
2. Suction the newborn properly.
a. Turn the baby’s head to one side
b. Suction gently and quickly – prolonged and deep suctioning of the nasopharynx during the first 5-10 minutes
after birth will stimulate the vagus nerve (located in the esophagus, and cause bradycardia.
c. Suction the mouth first before the nose – suctioning the nose causes reflex inhalation of the pharyngeal
secretions into the trachea and bronchi, thus causing aspiration. Suction mouth first so as to remove the
pharyngeal secretions.
d. To test for patency of the airway, occlude one nostril at a time. (Remember: Newborns are nasal breathers.) If
the newborn struggles when a nostril is occluded, additional suctioning is indicated.
B. Principle No. 2:
Maintain appropriate body temperature.
Newborn suffers large losses of heat because he is wet at birth, the Delivery Room is cold, and he does not have
enough subcutaneous tissues to keep him warm and he does not know how to shiver. (Heat production is
accomplished primarily by non-shivering thermogenesis, the major energy source for heat is his brown fat.
Measures to maintain appropriate body heat:
Effects of cold stress:
a. Metabolic acidosis – one of the ways by which heat is produced is by increasing metabolism. When this occurs,
fatty acids accumulate because of the breakdown of brown fat (seen only in term newborn, preemies have less)
b. Hypoglycemia – due to the use of sugar stored as glycogen.
Dry immediately and wrap warmly
Put under a droplight or as in a Kraisselman radiant warmer
C. Principle No. 3:
Assess the newborn carefully:
1. Apgar score – standardized evaluation of the newborn. It is done at one minute after birth to determine his
general condition at birth and then at five minutes to determine how well the newborn is adjusting to extrauterine
life discovered by Virginia Apgar.
Apgar Scoring
The most critical observation is the heart rate.
The general attitude of the newborn at birth is that of flexion.
Body pink, extremities blue (called acrocyanosis) is normal during the first 24 hours of life
Interpretation:
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
0 – 3: the baby is in serious danger and needs immediate resuscitation
4 – 6: the baby’s condition is guarded and needs more extensive clearing of the airway
7 – 10: the baby is at his best possible health
2. Silverman-Anderson scale – index of respiratory distress (score of 0 is an indication of good respiratory function)
Grunting sound of air pushing past partially closed glottis, heard during inspiration
Retractions: sternal and intercostals; due to use of accessory muscles to aid in breathing.
Flaring nares: due to newborn’s efforts to lessen resistance in narrow nasal passages.
Seesaw respirations: Flattening of chest with inspiration and bulging of abdomen, caused by the
utilization of abdominal muscles during prolonged, forced respiration.
D. Principle No. 4
Identify the newborn
Identification of the neonate should be done in the delivery room before transferring to the nursery.
Footprints are said to be the best form, although identical ID bands for both baby and mother will suffice.
Anthropometric measurements:
- Weight- lower limit for expected birthweights for all NB is -2.5(5.5 lb) to 3.4 kg. (7.7 lb).
Average birth weight for mature female NB is 3.4 kg (7.5 lb) & mature male is 3.5 kg. (7.7
lb).Macrosomic - 4.7 kg (10 lb) is unusual.
th
- Length – average birth length of a mature 50 percentile female neonate -49 cm. (19.2 in.),
mature males- 50cm (19.6 in.). The lower limit – birth length- 46(18 in.). Rare cases- 57.5 cm (24
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
in.). Head circumference- mature NB- 34 to 35 cm (13.5-14 in.).Greater than 37cm. (14.8 in.) or
less than 33cm. (13.2 in.) should be carefully check for neurological involvement.HC is measured
with a tape measure drawn across the center of the forehead and around the most prominent
potion of the posterior head(occiput).
- Chest Circumference- 2 cm. (0.75 to 1 in.) less than the head circumference- measured at the
level of the nipples – Normal 32 to 33 cm.
Vital Signs:
- Temperature – 99 ⁰F (37.2 ⁰ C) at birth.
- Temperature of the delivery / birthing rooms 68 ⁰F to 72 ⁰ F (21 ⁰C to 22 ⁰C).
Newborns lose heat by 4 separate mechanisms:
Convection
Conduction
Radiation
Evaporation
- Pulse – heart rate inside the utero averages 110 to 160 beats per min. Immediately after birth
HR may be rapid as 180beats pm. An hour after birth as the NB settles down to sleep, HR
stabilizes to an average of 120 to 140 bpm.Respiration-first few minutes of life maybe as high as
90 breaths /m. As respiratory activity is established & maintained, average is 30 to 60breaths/m.
watching the abdomen
th
- Blood pressure- approximately 80/46 mm Hg at birth. 10 day rises to 100/50mm hg. BP of NB
is somewhat inaccurate so it is not routinely measured unless cardiac anomaly is suspected.
- Doppler method may be used to take BP.
Medications:
Crede’s Prophylaxis- apply tetracycline 1% or erythromycin 0.5% ophthalmic ointment at the
conjunctival sac to prevent OphthalmiaNeonatorum (neonatal conjunctivitis) when the mother
has gonorrhea or chlamydial infection.
Vitamin K – 1.0 mg (0.1ml) for weight more than 1500gms. IM at left vastuslateralis – for
premature- 0.5 mg (0.05ml) less than 1500grams, given to help blood clots or prevent bleeding.
Hepatitis B Vaccine- IM at right vastuslateralis- upper outer portion of the thigh 0.5 ml. BCG
vaccine – 0.05 ml. intradermal, right deltoid region of the arm.
END OF THE LECTURE… MMSANTOS 2022
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
References:
Gardner, S., & Snell, B. (2016). Care of the Well Newborn. Jones & Bartlett Publishers.
NursingSOS (2018, June 6). APGAR Score: Newborn Nursing Assessment [Video].
Youtube.https://youtu.be/X48lqTNUTQk
Identify the newborn.
Identification of the neonate should be done in the delivery room before transferring to the nursery. Footprints a
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
PREPARED BY: MARILYN M. SANTOS,PhD. MAN.,RN.1ST SEMESTER 2023/OCTOBER
You might also like
- On Autumn's Wing, A Story of Birth Trauma, Brain Injury and Miracles.From EverandOn Autumn's Wing, A Story of Birth Trauma, Brain Injury and Miracles.No ratings yet
- Essential Intrapartum and Newborn Care (EINC) PracticesDocument26 pagesEssential Intrapartum and Newborn Care (EINC) PracticesDaryl Adrian RecaidoNo ratings yet
- Essential Newborn Care Checklist Ateneo College NursingDocument7 pagesEssential Newborn Care Checklist Ateneo College NursingNur Fatima SanaaniNo ratings yet
- EINC Essential Intrapartim NC ChecklistDocument7 pagesEINC Essential Intrapartim NC Checklisthey aadarshaNo ratings yet
- Essential Newborn and Mother Care StandardsDocument3 pagesEssential Newborn and Mother Care StandardsMasterclass40% (5)
- Einc G5Document24 pagesEinc G5JAMIL MANALNo ratings yet
- Delivery Room Technique GuideDocument8 pagesDelivery Room Technique GuideChristine Joy MolinaNo ratings yet
- DR Technique Checklist101Document8 pagesDR Technique Checklist101Christine Joy MolinaNo ratings yet
- Intrapartum: Delivery Room Technique PurposeDocument8 pagesIntrapartum: Delivery Room Technique PurposeRoshin TejeroNo ratings yet
- DR Technique ChecklistDocument8 pagesDR Technique ChecklistChristine Joy MolinaNo ratings yet
- MCN Lab WRDocument101 pagesMCN Lab WRMaui TabuzoNo ratings yet
- Care of Normal Newborn BabiesDocument439 pagesCare of Normal Newborn BabiesSebastian Spatariu100% (2)
- Delivery Room Technique GuideDocument8 pagesDelivery Room Technique GuidePATRICIA JULIANNE CASTAÑETO RIVERANo ratings yet
- Neonatal NursingDocument53 pagesNeonatal Nursingkrishnasree100% (1)
- Intrapartum Delivery TechniquesDocument10 pagesIntrapartum Delivery TechniquesOmar James Abdulgani LimNo ratings yet
- Intrapartum: Delivery Room Technique PurposeDocument7 pagesIntrapartum: Delivery Room Technique Purposesharmena harunNo ratings yet
- 9 Labor and DeliveryDocument6 pages9 Labor and DeliveryUri Perez MontedeRamosNo ratings yet
- Care of Normal NewbornDocument13 pagesCare of Normal NewbornTanu BhatiaNo ratings yet
- Case Assignment On The Newborn Care Using EENCDocument5 pagesCase Assignment On The Newborn Care Using EENClily machanNo ratings yet
- Intrapartum DR TechniqueDocument10 pagesIntrapartum DR TechniqueAl-waleed JulkanainNo ratings yet
- Delivery Room Technique GuideDocument10 pagesDelivery Room Technique GuideAl-waleed JulkanainNo ratings yet
- Kangaroo Mother Care Rooming in UpdatedDocument44 pagesKangaroo Mother Care Rooming in UpdatedStar DustNo ratings yet
- Outline For Reporting CHNDocument6 pagesOutline For Reporting CHNKyla FernandezNo ratings yet
- EINCDocument16 pagesEINCLea Mee CastroverdeNo ratings yet
- Essential prenatal and newborn care guideDocument33 pagesEssential prenatal and newborn care guideCharlotte Monique CapuaNo ratings yet
- Pregnancy Diagnosis and Fetal AssessmentDocument41 pagesPregnancy Diagnosis and Fetal AssessmentKrystel Anne MilanNo ratings yet
- Stages of LaborDocument15 pagesStages of LaborJune DumdumayaNo ratings yet
- Transes 1 (PEDIATRICS-LAB)Document2 pagesTranses 1 (PEDIATRICS-LAB)Ashley Judd EmpaynadoNo ratings yet
- Delivery Room (Functions and Responsibilities)Document12 pagesDelivery Room (Functions and Responsibilities)Louis Gabriel AdayaNo ratings yet
- Essential Newborn CareDocument8 pagesEssential Newborn CareAbeer AguamNo ratings yet
- Activity #1 Nupc110-CmcrpDocument4 pagesActivity #1 Nupc110-CmcrpMelody BoadoNo ratings yet
- BEMONCDocument7 pagesBEMONCKriziah Grace VillavertNo ratings yet
- Newborn Care ChecklistDocument5 pagesNewborn Care ChecklistAda Gay Olandia SerencioNo ratings yet
- 5 EincDocument4 pages5 EincJirah DawalNo ratings yet
- EINCDocument2 pagesEINCmayeNo ratings yet
- Essential Intrapartum AND Newborn Care By: Heidi C. Cabanatan, RNDocument20 pagesEssential Intrapartum AND Newborn Care By: Heidi C. Cabanatan, RNThrecia RotaNo ratings yet
- Individual Case Study Delivery Room Exposure: (Agusan Del Norte Provincial Hospital, Butuan City)Document13 pagesIndividual Case Study Delivery Room Exposure: (Agusan Del Norte Provincial Hospital, Butuan City)pius troy macapazNo ratings yet
- Delivery Room: (Institution/ Area)Document8 pagesDelivery Room: (Institution/ Area)Nickaela CalalangNo ratings yet
- Essential Intrapartum & Newborn Care: Joanne Marie S. Garcia, RN, ManDocument35 pagesEssential Intrapartum & Newborn Care: Joanne Marie S. Garcia, RN, ManknotstmNo ratings yet
- Modul Normal Delivery 2016Document8 pagesModul Normal Delivery 2016Alvin FarhanNo ratings yet
- NCM 104 Lec Reviewer FinalsDocument11 pagesNCM 104 Lec Reviewer FinalsFERNANDEZ, RELLY ANDREWNo ratings yet
- CHN1 Lec Session #19 SASDocument9 pagesCHN1 Lec Session #19 SASMark Raymunstine TamposNo ratings yet
- C-Section (Suparna & Aanchal)Document16 pagesC-Section (Suparna & Aanchal)bhaveshchaudhary4343No ratings yet
- Best Practices in Maternity CareDocument32 pagesBest Practices in Maternity CareFev BanataoNo ratings yet
- Conducting Normal DeliveryDocument8 pagesConducting Normal DeliveryA HNo ratings yet
- DIESTRO - EINC Reaction PaperDocument2 pagesDIESTRO - EINC Reaction PaperAngela Mae DiestroNo ratings yet
- Management Guideline NICU Updated 2018 - PediMedicineDocument213 pagesManagement Guideline NICU Updated 2018 - PediMedicinenishan chakma100% (1)
- RD Manual Med and BathingDocument5 pagesRD Manual Med and Bathingapple m.No ratings yet
- EINCDocument9 pagesEINCFLORENCE RIVA MAQUILING GUIMARYNo ratings yet
- Antenatal ExaminationDocument18 pagesAntenatal ExaminationAnonymous 0C4OZmR100% (1)
- ESSENTIAL INTRAPARTUM NEWBORN CARE (Assisting and Handling Delivery)Document4 pagesESSENTIAL INTRAPARTUM NEWBORN CARE (Assisting and Handling Delivery)Hannah Angelu CabadingNo ratings yet
- Health Policies For Essential Intrapartum and Newborn CareDocument2 pagesHealth Policies For Essential Intrapartum and Newborn CareNielette R. BASALNo ratings yet
- Essential Newborn and Maternal CareDocument69 pagesEssential Newborn and Maternal CareIvan BibonNo ratings yet
- EINC-checklistDocument3 pagesEINC-checklistSteph VistalNo ratings yet
- NCM 107 RLE Checklists To Send 2023Document3 pagesNCM 107 RLE Checklists To Send 2023Keltian LaurenteNo ratings yet
- Care of Normal Neonates-2019Document14 pagesCare of Normal Neonates-2019Essam HassanNo ratings yet
- Handle Technique: Instruments and AccessoriesDocument3 pagesHandle Technique: Instruments and AccessoriesMonette Guden CuaNo ratings yet
- Essential Intrapartum Care: Practices Recommended During DeliveryDocument9 pagesEssential Intrapartum Care: Practices Recommended During DeliveryKristil ChavezNo ratings yet
- Essential Intrapartum and Newborn CareDocument5 pagesEssential Intrapartum and Newborn Careanjie kamidNo ratings yet
- Neurorehabilitation in Neuro-Oncology 2019 E-BookDocument254 pagesNeurorehabilitation in Neuro-Oncology 2019 E-BookWoffe SoloNo ratings yet
- Chapter 04: Patient Records, Medication Orders, and Medication Labels Mulholland: The Nurse, The Math, The Meds, 3rd EditionDocument5 pagesChapter 04: Patient Records, Medication Orders, and Medication Labels Mulholland: The Nurse, The Math, The Meds, 3rd EditionadenNo ratings yet
- FORM I-601 Waiver Application USDocument9 pagesFORM I-601 Waiver Application USChaudhry WathraNo ratings yet
- GMAT Crititcal Reasoning (Practice)Document11 pagesGMAT Crititcal Reasoning (Practice)Hương HuỳnhNo ratings yet
- Diabetic Retinopathy Disease Classification Using Deep Neural Network and Retina ImagesDocument13 pagesDiabetic Retinopathy Disease Classification Using Deep Neural Network and Retina ImagesIJRASETPublicationsNo ratings yet
- Genetics Problem Key Biol 121Document13 pagesGenetics Problem Key Biol 121S0% (1)
- Psychological Trauma: Theory, Research, Practice, and PolicyDocument4 pagesPsychological Trauma: Theory, Research, Practice, and PolicyPerla MontellanoNo ratings yet
- COVID Toes, Rashes: How The Coronavirus Can Affect Your SkinDocument6 pagesCOVID Toes, Rashes: How The Coronavirus Can Affect Your SkinlittlemisseeeNo ratings yet
- Z-03 Digest Part EVDocument50 pagesZ-03 Digest Part EVXaveer AzadNo ratings yet
- Ts 410 420 Product Instruction ManualDocument112 pagesTs 410 420 Product Instruction ManualRosario GonzalesNo ratings yet
- Problems faced by construction workers in Tamil NaduDocument3 pagesProblems faced by construction workers in Tamil NaduYamini HarshaNo ratings yet
- Sukie BCHDocument16 pagesSukie BCHapi-309519730No ratings yet
- Dispensing DrugsDocument1 pageDispensing DrugsIan CalalangNo ratings yet
- Colds and Their BenefitsDocument105 pagesColds and Their BenefitsAlmiranteAckbarNo ratings yet
- Bennett2007 PDFDocument8 pagesBennett2007 PDFMirza RisqaNo ratings yet
- Plasticity of Macrophage 2019 ReviewDocument9 pagesPlasticity of Macrophage 2019 ReviewKudelko MatNo ratings yet
- Melio Ebook DKDocument429 pagesMelio Ebook DKStaporn Kasemsripitak100% (1)
- Growel Dairy Farming ManualDocument52 pagesGrowel Dairy Farming ManualGrowel Agrovet Private Limited.No ratings yet
- Health and Privacy PDFDocument40 pagesHealth and Privacy PDFMonika NegiNo ratings yet
- GallstonesDocument17 pagesGallstonesع ب و دNo ratings yet
- BT-740 OP Manual (740-ENG-OPM-EUR-R02) PDFDocument50 pagesBT-740 OP Manual (740-ENG-OPM-EUR-R02) PDFJaneth Pariona SedanNo ratings yet
- ClavusDocument4 pagesClavusargie3333No ratings yet
- NCP - LeprosyDocument3 pagesNCP - LeprosyKevin DareNo ratings yet
- Fundamentals of NursingDocument16 pagesFundamentals of Nursingsorilla_franceschelNo ratings yet
- Echocardiographic Anatomy in The FetusDocument14 pagesEchocardiographic Anatomy in The FetusAnonymous hOHi6TZTnNo ratings yet
- Scoliosis Clinical & ExerciseDocument14 pagesScoliosis Clinical & ExercisePurohit_RNo ratings yet
- PDFDocument1,029 pagesPDFCk CkNo ratings yet
- A0204 Vaginal HifuDocument14 pagesA0204 Vaginal HifuleanferoNo ratings yet
- Manu Et Al-2015-Acta Psychiatrica ScandinavicaDocument12 pagesManu Et Al-2015-Acta Psychiatrica ScandinavicamerianaNo ratings yet
- Vidya Vikas Institute of Engineering & Technology: #127 - 128, Mysuru Bannur Road, Alanahally Post Mysuru - 570028Document5 pagesVidya Vikas Institute of Engineering & Technology: #127 - 128, Mysuru Bannur Road, Alanahally Post Mysuru - 570028MonishaNo ratings yet