Professional Documents
Culture Documents
Management of Neuropathic Pain in Polyneuropathy
Uploaded by
Flea CidCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Management of Neuropathic Pain in Polyneuropathy
Uploaded by
Flea CidCopyright:
Available Formats
Management of REVIEW ARTICLE
Neuropathic Pain in
C O N T I N U UM AUDIO
INTERVIEW AVAILABLE
Polyneuropathy
ONLINE
By Amanda C. Peltier, MD, MS; Derek Wood, MD
ABSTRACT
CITE AS:
PURPOSE OF REVIEW: Many polyneuropathies cause significant neuropathic CONTINUUM (MINNEAP MINN)
pain, resulting in substantial morbidity and reduced quality of life. 2020;26(5, PERIPHERAL NERVE AND
MOTOR NEURON DISORDERS):
Appropriate management is crucial for maintaining quality of life for patients 1299–1322.
with painful polyneuropathies. The US Food and Drug Administration
(FDA) has only approved one new drug for painful diabetic neuropathy in the Address correspondence to
past decade, a topical capsaicin patch that was initially approved for the Dr Amanda C. Peltier, Vanderbilt
University Medical Center,
treatment of postherpetic neuralgia in 2009. Gabapentinoids and serotonin A-0118 Medical Center North,
norepinephrine reuptake inhibitors (SNRIs) continue to have an advantage in Nashville, TN 37232, Amanda.
safety profiles and efficacy. Other antiepileptic medications remain peltier@vumc.org.
second-line agents because of fewer studies documenting efficacy. RELATIONSHIP DISCLOSURE:
Dr Peltier serves as secretary for
the International Diabetes
RECENT FINDINGS: This
article reviews recent literature on complementary Neuropathy Consortium, on the
and pharmacologic therapies for the management of painful board of directors of the
polyneuropathies. Exercise has emerged as an important therapeutic tool American Autonomic Society,
and on advisory boards for
and may also improve the underlying polyneuropathy in the setting of Akcea Therapeutics; Alnylam
obesity, metabolic syndrome, and diabetes. Pharmaceuticals, Inc; and CSL
Behring. Dr Peltier has received
personal compensation for
SUMMARY: The approach to management of painful polyneuropathies is speaking engagements from
multifactorial, using both pharmacologic and nonpharmacologic measures Akcea Therapeutics and CSL
Behring and research/grant
to improve pain severity and patient quality of life.
support from Akcea
Therapeutics; CSL Behring; and
the National Institute of
Neurological Disorders and
INTRODUCTION Stroke NeuroNEXT. Dr Wood
P
ainful polyneuropathy is one of the most common neurologic disorders reports no disclosure.
encountered by neurologists. The prevalence of polyneuropathy in the UNLABELED USE OF
general population is at least 4% and may be as high as 10% among PRODUCTS/INVESTIGATIONAL
those older than 40 years of age. A significant minority of these patients USE DISCLOSURE:
Drs Wood and Peltier discuss
have neuropathic pain, and it is estimated that up to 5% of Americans the unlabeled/investigational
have painful polyneuropathy.1–3 Diabetic polyneuropathy is the most common use of α-lipoic acid,
amitriptyline, cannabidiol oil,
cause of painful neuropathy in the world. Diabetic polyneuropathy affects 10% to
carbamazepine, nortriptyline,
50% of patients with diabetes, of which at least 20% have neuropathic pain.4 This oxcarbazepine, spinal cord
translates to more than 2.3 million affected patients in the United States alone. stimulators, valproic acid, and
venlafaxine for the treatment of
Chemotherapy-induced peripheral neuropathy, another common cause of painful neuropathic pain in
polyneuropathy, affects up to 30% of cancer survivors.5 Additional causes of polyneuropathy.
painful peripheral neuropathy include alcohol and other toxic substances,
nutritional deficiency, human immunodeficiency virus (HIV) infection, light © 2020 American Academy
chain and hereditary amyloidosis, and idiopathic (TABLE 8-1). of Neurology.
CONTINUUMJOURNAL.COM 1299
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF NEUROPATHIC PAIN IN POLYNEUROPATHY
EPIDEMIOLOGY AND IMPACT OF NEUROPATHIC PAIN
Twenty million Americans have chronic neuropathic pain.6 Causes include
painful polyneuropathies, postherpetic neuralgia, chronic back pain, spinal cord
injury, multiple sclerosis, and stroke. Postherpetic neuralgia and trigeminal
neuralgia affect 0.09% of the population. Painful diabetic polyneuropathy is
among the most common causes of neuropathic pain and is the most common
cause of painful polyneuropathy.7 Neuropathic pain more commonly affects
women than men (8% compared to 5.7%) and patients older than 50 years of
age.8 Neuropathic pain, including chemotherapy-induced peripheral
neuropathy, affects 20% to 50% of patients with cancer.9
The cost of pain in the United States is between $565 billion and $635 billion
each year, which is evenly split between medical costs and lost productivity.
Approximately $293 billion is due to direct costs of medical care, including
prescriptions, procedures, health care visits, and other health care expenditures.
Indirect costs are extrapolated from lost wages and productivity of patients with
pain and their caregivers.10 Chronic pain is associated with higher direct medical
costs than the most expensive major diagnoses, including cardiovascular disease
and cancer.10 Diabetic polyneuropathy alone is estimated to cost $11 billion to
$14 billion dollars annually.11,12 In Europe, the estimated annual costs per patient
for all neuropathic pain vary between €1939 and €3131 in direct costs and between
€7000 and €11,000 in indirect costs.13 Annual per patient costs in the United States
are $1600 to $7000 in direct costs and $6016 to $19,000 in indirect costs.14–16
Health care costs may be up to 3 times higher for patients with diabetic
polyneuropathy compared to controls and increase with opioid use.12,17 Because of
the imprecision in estimating the prevalence of chemotherapy-induced peripheral
neuropathy, it is difficult to estimate costs specific to neuropathy-related pain.
Multiple studies using a variety of assessment tools consistently indicate that
quality of life is significantly reduced for patients with neuropathic pain across all
domains.18,19 Medications used for neuropathic pain can affect cognition and
TABLE 8-1 Differential Diagnosis of Common Etiologies of Painful Neuropathies
◆ 丣Diabetic polyneuropathy
◆ 丣Monoclonal gammopathy–associated polyneuropathy
◆ 丣Chemotherapy-induced polyneuropathy (associated with taxanes, oxaliplatin, vincristine,
thalidomide, bortezomib)
◆ 丣Idiopathic small fiber polyneuropathy
◆ 丣Neuropathy associated with metabolic syndrome
◆ 丣Human immunodeficiency virus (HIV)–associated polyneuropathy
◆ 丣Hereditary sensory and autonomic neuropathies
◆ 丣Sjögren syndrome–associated polyneuropathy
◆ 丣Pyridoxine (vitamin B6) toxicity
◆ 丣Celiac neuropathy
◆ 丣Alcohol and other toxic neuropathies
◆ 丣Light chain and hereditary amyloidotic neuropathies
◆ 丣Nutritional deficiency neuropathies
1300 OCTOBER 2020
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
function. Neuropathic pain also affects sleep, mood, and other aspects of KEY POINTS
health.20,21 Neuropathic pain has a bidirectional relationship with sleep and
● Painful polyneuropathy is
mood.22 Pain leads to sleep disturbance in 60% to 80% of patients, and impaired one of the most common
sleep, in turn, leads to increased pain intensity and a higher risk of pain causes of neuropathic pain
catastrophizing (defined as magnification, rumination, and helplessness), and may affect up to 1 in 20
leading to reduced quality of life and poor overall health outcomes.23–25 Half of Americans.
patients with painful diabetic polyneuropathy have depression or anxiety, and
● Painful polyneuropathy is
one-fourth have both.26 associated with significantly
reduced quality of life and
PATHOGENESIS OF NEUROPATHIC PAIN increased health care costs,
Multiple mechanisms lead to neuropathic pain, many of which are centered as well as costs to society in
lost worker productivity.
on the dorsal root ganglion. Dorsal root ganglion cells are pseudounipolar
T-shaped cells with a bifurcated axon, one process extending into the ● Neuropathic pain leads to
periphery and the other centrally. Dorsal root ganglion neurons include those sleep disruption and vice
for myelinated Aβ and Aδ fibers and nonmyelinated C fibers, which are versa. Up to 80% of patients
with neuropathic pain have
arranged somatotopically in the ganglia. Myelinated axons terminate in sleep disturbance.
specialized receptors and C fibers in free nerve endings. Dorsal root ganglion
neurons can be cross-depolarized by excitation of neighboring dorsal root ● Half of patients with
ganglion cells within the same ganglion or cells within the substantia painful diabetic neuropathy
have depression or anxiety,
gelatinosa.27 A state of hyperexcitability and lack of inhibition by descending
and one-fourth have both.
central pathways is one of the main mechanisms of neuropathic pain arising
from polyneuropathy. Ectopic firing and central sensitization are thought ● Although the specific role
to be the main drivers of neuropathic pain.19 of SCN9A sequence variants
Evolving evidence suggests axonal and neuronal ion channels (particularly in the pathogenesis of small
fiber neuropathy is
voltage-gated sodium channels) play an important role in facilitating uncertain, voltage-gated
hyperexcitability in painful neuropathies. The role of the Nav1.7 voltage-gated sodium channels play an
sodium channel has received particular interest. Mutations in the Nav1.7 important role in
gene, SCN9A, cause both congenital insensitivity to pain and hereditary neuropathic pain, and
pharmacologic inhibition is a
erythromelalgia.28,29 Evidence is conflicting regarding the role of other SCN9A promising therapeutic
sequence variants in the etiology of small fiber neuropathy.30–32 Sodium Nav strategy.
channels 1.6, 1.8, and 1.9 have also been shown to have altered expression in
animal models of diabetic polyneuropathy, suggesting upregulation in
neuropathy leading to increased ectopic firing.33 Blocking axon potentials with
sodium channel blockers has been the putative action of multiple antiepileptic
drugs used in neuropathic pain, such as carbamazepine, oxcarbazepine,
lamotrigine, and lacosamide, and ongoing trials are exploring the utility of
sodium channel antagonists in patients with specific sodium channel
sequence variants.
The α2δ1 subunit of N-type calcium channels on C fibers in the superficial
dorsal horn of the spinal cord is the mechanistic target of gabapentinoids
(gabapentin and pregabalin). Binding of the gabapentinoids decreases
neurotransmitter release of norepinephrine, glutamate, and aspartate.34,35
Potassium channel expression is also altered in neuropathic pain, although this is
not a common pharmacologic target. While γ-aminobutyric acid (GABA) is
involved in neuropathic pain, few data support efficacy for GABA and GABA
transporter antagonists.36
PHARMACOLOGIC MANAGEMENT OF PAINFUL NEUROPATHY
Neuropathic pain is challenging to treat, and patients often need to try several
different agents alone or in combination before achieving a meaningful degree of
CONTINUUMJOURNAL.COM 1301
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF NEUROPATHIC PAIN IN POLYNEUROPATHY
pain relief. Each medication should generally be tried at the maximal tolerated
dose for 6 to 8 weeks before determining treatment failure. Particular care should
be taken during dose titration to minimize the risk of side effects. Tricyclic
antidepressants and serotonin norepinephrine reuptake inhibitors (SNRIs) may
take several weeks to titrate to an effective dose.
Therapeutic development for painful neuropathy has been challenging. The US
Food and Drug Administration (FDA) has only approved one drug for painful
diabetic polyneuropathy in the past decade. An 8% topical capsaicin patch, which
was initially approved for the treatment of postherpetic neuralgia in 2009, was
approved for the new indication of painful diabetic polyneuropathy in July 2020.
Most studies of potential neuropathic pain agents focus on postherpetic neuralgia and
painful diabetic polyneuropathy, with few addressing idiopathic painful neuropathy.
The only FDA-approved medications for treatment of painful diabetic neuropathy
are pregabalin, duloxetine, tapentadol (which is only rarely used), and the capsaicin
patch. However, other medications may be effective and are used off-label.
The first steps in managing painful polyneuropathy are to quantify pain
severity and determine treatment goals. A common error is to confuse negative
symptoms, such as numbness or a feeling of walking on rocks or stumps or
wearing tight compression socks, with neuropathic pain. Although
CASE 8-1 A 73-year-old man with a past medical history of coronary artery disease
(status post–bypass surgery), osteoarthritis, and hypertension presented
for evaluation of burning pain in his feet and imbalance. He also reported a
separate tingling sensation throughout his legs with an associated urge to
move that preceded the onset of his neuropathic pain by several years. He
only noticed this sensation when he was in a recumbent position, and it
would improve with movement.
His body mass index was 32. Neurologic examination revealed severe
vibration loss in his feet with moderate loss at the knees and mild loss at
his hands. He had a distal gradient temperature loss to the midshins and
wrists bilaterally. Achilles reflexes were absent, and he had difficulty with
tandem gait.
His hemoglobin A1c was 5.9%. His vitamin B12 level was in the low-normal
range at 286 pg/mL. Serum protein electrophoresis and immunofixation
and ferritin were normal.
He was started on gabapentin and was counseled on dietary
modifications and exercise. He was also started on oral vitamin B12
supplementation. He experienced a moderate improvement in symptoms.
COMMENT This patient exhibited symptoms of both a painful sensory peripheral
polyneuropathy and restless legs syndrome (RLS). RLS may be primary or
may be seen in association with other neurologic disorders, such as
peripheral neuropathy. Distinguishing the features of RLS from peripheral
neuropathy can be challenging because of similarities in symptoms. This
case highlights the importance of selecting medications that may help both
RLS and neuropathic pain.
1302 OCTOBER 2020
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
uncomfortable, negative neuropathic symptoms will not respond to neuropathic KEY POINTS
pain agents. It is also important to educate patients that medications for
● No new medications for
neuropathic pain do not alter the natural history of neuropathy progression. The neuropathic pain have been
decision to begin a neuropathic pain agent for positive symptoms, such as approved in the past
tingling, burning, or pins and needles sensations, should be based on patients’ 10 years (although the
perception of severity and an understanding of their goals for treatment. For high-dose capsaicin patch
that was approved for
example, once informed that neuropathy is slowly progressive and that it rarely
postherpetic neuralgia in
leads to requirement for assistive devices to support ambulation, many patients 2009 was recently approved
opt to hold off on symptomatic treatment. Factors suggesting treatment is for use in painful diabetic
warranted include interference with sleep and activities of daily living. polyneuropathy in July
2020). The most commonly
Differentiating painful polyneuropathy from restless legs syndrome (RLS),
used medications are the
which may coexist with painful neuropathy, is important. Most pain medications gabapentinoids, which act
(except for gabapentinoids) are ineffective for RLS, and some agents (such as on α2δ calcium channels, and
tricyclic antidepressants) may worsen it (CASE 8-1). medications that increase
Setting realistic treatment expectations is essential. Complete pain relief is norepinephrine at the
synapse.
typically not a realistic goal. Use of pain scores and visual analog scales may be
helpful in quantifying pain for follow-up visits. Gabapentinoids (gabapentin ● Each neuropathic pain
and pregabalin), tricyclic antidepressants, and SNRIs are the first-line medication should generally
treatments for painful neuropathy. The authors typically advocate using either a be tried at the maximal
tolerated dose for 6 to
gabapentinoid or an SNRI as first-line treatment, as these have the most evidence 8 weeks before concluding
available and most are now available in a generic form. Therapeutic choices it is ineffective.
should be personalized based on the patient’s pain profile, comorbid medical
conditions, and medication side effects. Identification of appropriate ● Differentiating painful
polyneuropathy from
expectations in timing of relief is also important. SNRIs typically require longer
restless legs syndrome
to take effect. Knowing when to refer a patient to a multidisciplinary pain (RLS), which may coexist
clinic is important. Referral should be considered for patients with greater pain with painful neuropathy, is
severity, those for whom first-line neuropathic agents have failed, and those important as most pain
with significant mental health comorbidities or pain catastrophizing. medications (with the
exception of the
Specific classes of neuropathic pain agents are reviewed below. Many patients gabapentinoids) are
require more than one agent to achieve meaningful pain relief. Unfortunately, ineffective for RLS, and
few head-to-head data comparing these medications are available. some agents (such as
tricyclic antidepressants)
may worsen RLS.
First-line Neuropathic Pain Agents
Clinical evidence for pharmacologic therapies for neuropathic pain is discussed ● Setting realistic treatment
in the sections that follow. TABLE 8-237 and TABLE 8-3 summarize therapies and expectations for pain
their level of evidence. The therapies discussed have high-quality clinical trial management is essential.
Complete pain relief is
data, high-level recommendations from professional societies such as the typically not a realistic goal.
American Academy of Neurology (AAN), and FDA approval providing the
rationale for their designation as first-line therapies. ● Gabapentin is absorbed in
the intestine via an
GABAPENTINOIDS. Gabapentinoids were initially developed as analogues of the active-transport mechanism
and displays nonlinear
inhibitory neurotransmitter GABA to treat epilepsy. After producing significant pharmacokinetics with
improvement in neuropathic pain, they were discovered to block the α2δ subunit saturable absorption and
of voltage-gated calcium channels in the dorsal horn of the spinal cord. decreased bioavailability at
higher doses.
GABAPENTIN. In 1994, gabapentin was approved for the treatment of epilepsy, but
today it is more widely used as a first-line treatment for neuropathic pain.
Gabapentin may be started at a daily dose of 900 mg/d divided into three doses,
although it is frequently started at a lower dose. The dose is then titrated based on
clinical response to a maximum of 3600 mg/d. Gabapentin is absorbed in the
CONTINUUMJOURNAL.COM 1303
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF NEUROPATHIC PAIN IN POLYNEUROPATHY
intestine via an active-transport mechanism and displays nonlinear
pharmacokinetics with saturable absorption and decreased bioavailability at
higher doses. Bioavailability of oral doses of gabapentin decrease as the dose
goes up, from 80% of 100 mg to 27% of 1600 mg. Peak serum concentration
occurs at 3 hours.38 Therefore, a typical dosing scheme would titrate up to doses
TABLE 8-2 First-line Medications for the Treatment of Painful Diabetic Neuropathya
American Academy
Typical Dose of Neurology Level of
Medication Range Common Side Effects Recommendation Notes
Gabapentin 300–1200 mg Sedation, weight gain, B Adjust dose in patients
3 times a day peripheral edema with renal dysfunction
Pregabalin 150–600 mg/d in Sedation, weight gain, A Adjust dose in patients
two to three peripheral edema with renal dysfunction;
divided doses Schedule V controlled
substance
Tricyclic 10–25 mg at Anticholinergic: dry B Avoid in patients with
antidepressants (eg, bedtime; titrate up mouth, constipation, history of prior suicide
amitriptyline, to maximum of orthostatic attempt; obtain ECG if
nortriptyline) 150 mg/d hypotension, urinary titrating to high doses or
retention, sedation; if on concomitant QTc
weight gain prolonging drugs; also
avoid in individuals with
specific cardiac
conductance
abnormalities
Duloxetine 30 mg/d to 60 mg Nausea, dizziness, B Avoid in patients with
2 times a day increased blood hepatic dysfunction
pressure, hyperhidrosis and in patients with a
glomerular filtration rate
lower than 30 mL/min;
60 mg 2 times a day has
not been shown to be
more effective than
60 mg/d
Venlafaxine Immediate release: Nausea, dizziness, B Extended-release
37.5 mg/d to increased blood formulation may be
225 mg/d in two to pressure, hyperhidrosis better tolerated and less
three divided likely to be associated
doses once higher with a withdrawal
than 37.5 mg/d syndrome on
discontinuation
Extended release:
37.5 mg/d;
increase in 37.5 mg
increments to total
daily dose of
225 mg/d
ECG = electrocardiogram.
a
Data from Bril V, et al, Neurology.37
1304 OCTOBER 2020
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
of 900 mg maximum per dose 3 to 4 times a day. Very little increase in efficacy KEY POINT
occurs over 3600 mg daily.
● Gabapentin and
Gabapentin acts on the α2δ subunit of presynaptic voltage-gated calcium pregabalin have similar
channels, leading to inhibition of these channels and modulation of efficacy, although patients
neurotransmitter release. The name gabapentin is a misnomer as the drug has may respond to, or tolerate,
no effect on GABA receptors. Gabapentin is non–protein bound and does not one and not the other.
Gabapentin displays
undergo hepatic metabolism. It is renally excreted unchanged with a half-life
nonlinear pharmacokinetics
of 5 to 9 hours.39 The dosage should be adjusted based on creatinine clearance. with saturable absorption
Gabapentin enacarbil is an extended-release form. It was shown to be superior to and decreased
placebo in reducing daily pain on an 11-point Likert scale.40 Gabapentin has bioavailability at higher
doses, which may favor the
a Level B recommendation from the AAN’s evidence-based guideline on the
use of pregabalin.
treatment of painful diabetic neuropathy.37
Gabapentin is generally well tolerated and is often the first medication tried for
painful neuropathy based on long-standing clinician experience, limited drug
interactions, easy titratability, good tolerability, and low cost. The most common
reason for discontinuing the medication is sedation or ineffectiveness. Other
potential adverse effects include peripheral edema and weight gain. An
encephalopathy with positive and negative myoclonus may be observed in cases of
gabapentin toxicity and typically occurs in the setting of renal dysfunction. In
response to the opioid epidemic, numerous states have enacted legislation making
gabapentin a controlled substance because of concern that gabapentin may
potentiate the effects of opioids.
PREGABALIN. Like gabapentin, pregabalin also acts on the α2δ subunit of
voltage-gated calcium channels. The FDA approved pregabalin in 2004 for the
treatment of epilepsy, postherpetic neuralgia, and painful diabetic neuropathy.
It is typically started at 150 mg/d in two to three divided doses and is titrated
based on clinical response to a maximum dose of 300 mg/d to 600 mg/d. Unlike
gabapentin, pregabalin has linear pharmacokinetics, with greater than 90%
bioavailability regardless of dose.38 Like gabapentin, it is renally excreted
unchanged, and the dose should be adjusted based on creatinine clearance.
Although pregabalin’s half-life allows for dosing 2 times a day, some patients feel
a wearing off and benefit from dosing 3 times a day.
Several Class I studies have demonstrated the superiority of pregabalin over
placebo for the treatment of painful diabetic neuropathy. A randomized
double-blind placebo-controlled study demonstrated a statistically significant
decrease in mean pain score for pregabalin 300 mg/d compared to placebo,
although 10% of patients in the pregabalin group withdrew from the study
because of adverse effects.41 In another study of patients with painful diabetic
neuropathy, pregabalin 300 mg/d did not differ from gabapentin enacarbil
(1200 mg/d to 3600 mg/d) and neither drug differed from placebo.42 Pregabalin
is the only medication to receive a Level A recommendation from the AAN’s
evidence-based guidelines on the treatment of painful diabetic neuropathy.37
Some patients for whom gabapentin has failed because of tolerability or
efficacy issues may have a better response with pregabalin or vice versa, although
medications from other classes should be tried first. The side effect profile of
pregabalin is similar to gabapentin. As of 2019, pregabalin is available as a generic
formulation, which will likely help mitigate cost issues previously associated with
the drug. Pregabalin is a Schedule V controlled substance (the lowest risk level
among the FDA drug schedules).
CONTINUUMJOURNAL.COM 1305
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF NEUROPATHIC PAIN IN POLYNEUROPATHY
TRICYCLIC ANTIDEPRESSANTS. The tricyclic antidepressants were originally
synthesized in the 1950s and act to inhibit norepinephrine and serotonin reuptake.
They also act as antagonists at histamine and muscarinic cholinergic receptors,
producing a characteristic side effect profile. The two most commonly used tricyclic
antidepressants for painful polyneuropathy are amitriptyline and nortriptyline.
These tricyclic antidepressants should be started at a low dose (10 mg to 25 mg) at
bedtime, increased by 10 mg/d to 25 mg/d every 7 to 14 days to a maximum dose of
75 mg/d to 150 mg/d, although many patients are able to achieve pain relief at lower
doses. An ECG should be obtained when titrating to higher doses or if starting a
tricyclic antidepressant in combination with other QTc-prolonging drugs.
Amitriptyline 75 mg/d was shown to be superior to placebo in patients with
diabetic and nondiabetic painful polyneuropathy, with 67% of patients on
amitriptyline having improvement.43 Tricyclic antidepressants have a Level B
recommendation from the AAN’s evidence-based guideline on the treatment of
painful diabetic neuropathy.37
The most common adverse effects of tricyclic antidepressants are sedation and
anticholinergic effects. Nortriptyline may be less sedating than amitriptyline.
Common anticholinergic effects include dry mouth, constipation, orthostatic
hypotension, urinary retention, and blurred vision. Cognitive impairment may
also be seen, particularly in individuals with underlying cognitive dysfunction.
Caution should be exercised when initiating tricyclic antidepressants in elderly
individuals or those with preexisting cognitive or autonomic dysfunction
as they may be more susceptible to anticholinergic side effects. Tricyclic
antidepressants should be avoided in patients with severe depression or
history of suicide attempt, as intentional overdose may cause a fatal cardiac
dysrhythmia. Slow upward titration can mitigate some adverse effects, especially
sedation. The authors typically increase weekly or every two weeks to
improve tolerability.
TABLE 8-3 Multimodal Options for Painful Polyneuropathy Treatment
Complementary/
Pharmacologic Therapies Nonpharmacologic Therapies Exercise
First-level therapies Pregabalin, duloxetine, α-Lipoic acid 600 mg/d Aerobic exercise 4
(clinically proven with gabapentin h/wk at 50–85%
placebo-controlled studies, FDA maximum heart
approved, Level A and B rate
evidence-based recommendations)
Second-level therapies Tricyclic antidepressants, Levomefolate/Schizochytrium/ Balance exercises
(smaller studies, prospective studies venlafaxine, valproate, pyridoxal phosphate/ to decrease fall
without placebo control, greater side lidocaine patches methylcobalamin, B vitamin risk, tai chi
effects) supplements (avoiding excess
vitamin B6), spinal cord stimulation
Third-level therapies Topiramate, lacosamide, Acupuncture Yoga
(anecdotal, case studies) oxcarbazepine,
lamotrigine, mexiletine
FDA = US Food and Drug Administration.
1306 OCTOBER 2020
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
SEROTONIN NOREPINEPHRINE REUPTAKE INHIBITORS. SNRIs block reuptake of KEY POINTS
both serotonin and norepinephrine. Their specific effects on norepinephrine
● The two most commonly
reuptake are thought to increase descending pain inhibitory pathways used tricyclic
converging on the dorsal horn in the spinal cord. Their number needed to treat antidepressants for painful
correlates with norepinephrine reuptake inhibition.44 polyneuropathy are
amitriptyline and
nortriptyline.
DULOXETINE. Duloxetine acts to inhibit the reuptake of serotonin and
norepinephrine. It was the first drug approved by the FDA for the treatment of ● Caution should be
diabetic peripheral neuropathy in 2004. The standard dose is 60 mg once a day, exercised when initiating
although it may be initiated at 30 mg/d for the first week if tolerability is a tricyclic antidepressants in
concern. Although it can be dosed up to 120 mg/d in two divided doses, doses elderly individuals or those
with preexisting cognitive or
higher than 60 mg/d are not thought to confer additional benefit and are autonomic dysfunction as
associated with increased side effects.45 Duloxetine should be avoided in patients they may be more
with hepatic impairment and in patients with impaired renal function susceptible to
(glomerular filtration rate lower than 30 mL/min). anticholinergic side effects,
and their use should be
A multicenter double-blind randomized placebo-controlled trial in patients with avoided in patients with
painful diabetic neuropathy compared duloxetine at 60 mg/d and 60 mg 2 times severe depression or history
a day with placebo.46 The primary end point was mean change from baseline on of suicide attempt because
a 24-hour average pain score. Duloxetine at 60 mg/d and 60 mg 2 times a day of the risk of intentional
overdose.
was associated with a statistically significant improvement compared to placebo.
Of patients in the duloxetine 60 mg 2 times a day group, 12.1% discontinued ● Duloxetine may be a
treatment because of adverse effects compared to only 4.3% in the 60 mg/d particularly good agent for
group and 2.6% in the placebo group. Nausea is the most common adverse effect. patients with painful
diabetic neuropathy with
Fatigue, increased sweating, decreased libido, and hypertension are other possible
comorbid depression,
side effects. A risk of serotonin syndrome exists if used in combination with other anxiety, or fibromyalgia.
serotonergic medications (eg, tricyclic antidepressants, selective serotonin
reuptake inhibitors [SSRIs], tramadol). Duloxetine may be a particularly good
choice for patients who also have depression/anxiety or fibromyalgia.
VENLAFAXINE. Venlafaxine is another drug within the SNRI class that has been
shown to be beneficial for the treatment of neuropathic pain. It is available in
both an immediate-release and an extended-release formulation. The
immediate-release formulation is started at 37.5 mg/d to 75 mg/d and can
be titrated to 225 mg/d. Doses greater than 37.5 mg/d should be given in two
or three divided doses. The extended-release formulation is given as a
once-daily dose and can be started at 37.5 mg/d to 75 mg/d and increased by
37.5 mg every 1 to 2 weeks if needed. The extended-release formulation is
often preferred because of ease of use, less severe discontinuation syndrome
on stopping the drug, and less dizziness and nausea at initiation of therapy. In
patients with renal or hepatic impairment, the daily dose should be reduced
accordingly.
Venlafaxine extended-release formulation has shown benefit in the treatment
of painful diabetic neuropathy compared to placebo, with a 32% reduction
(75 mg) and 50% reduction (150 mg to 225 mg) on a visual analog pain intensity
scale compared to 27% in the placebo group.47 Like duloxetine, venlafaxine has
a Level B recommendation from the AAN’s evidence-based guideline on the
treatment of painful diabetic neuropathy.37
The side effect profile of venlafaxine is similar to duloxetine. Patients taking
the immediate-release formulation should be advised against stopping the drug
abruptly because of the risk of precipitating a withdrawal syndrome.
CONTINUUMJOURNAL.COM 1307
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF NEUROPATHIC PAIN IN POLYNEUROPATHY
Second-line Neuropathic Pain Agents
Many patients with painful polyneuropathy do not adequately respond to first-line
agents. Evidence supports the utility of a number of other treatments that may be
used as second-line agents.
ANTIEPILEPTIC DRUGS. Valproic acid was shown to have efficacy in the management
of painful diabetic neuropathy compared to placebo48,49; however, limited studies
involved a small number of patients and were done at the same single center. Valproic
acid has many side effects, including weight gain, thrombocytopenia, pancreatitis,
tremor, sedation, and hair loss, and thus it is less likely to be used when considering a
second-line agent for neuropathy. Reports are conflicting regarding the efficacy of
oxcarbazepine for the treatment of painful diabetic polyneuropathy. Although several
studies have failed to show benefit, patients in one study of oxcarbazepine initiated at
300 mg/d and titrated to a maximum of 1800 mg/d had a significantly larger decrease
in the mean change on a visual analog scale pain score compared to placebo.50
Hyponatremia is a well-known adverse effect. Carbamazepine has also been used for
chronic pain but has not been shown to be effective over placebo. It can also cause
hyponatremia and significant bone marrow depression.51
Topiramate has also been investigated for use in painful diabetic
polyneuropathy. Topiramate titrated up to 400 mg/d or the maximum tolerated
dose was shown to be modestly superior to placebo in pain reduction on a visual
analog scale score over 12 weeks.52 Topiramate has several adverse effects,
including fatigue, cognitive dysfunction, and extremity paresthesia; it may also
trigger depressive episodes in some individuals. It should be avoided in patients
with a history of nephrolithiasis. Weight loss is a well-known side effect of
topiramate, and its use as a treatment for neuropathic pain in patients with
metabolic syndrome is actively being investigated. An ongoing multicenter
clinical trial of topiramate as a potential disease-modifying agent for neuropathy
associated with metabolic syndrome based on its effects on weight and
insulin sensitivity is ongoing using the NeuroNEXT trial network.53
Several studies have failed to demonstrate a benefit for use of lamotrigine in
the treatment of painful diabetic polyneuropathy. However, post hoc analysis in
one study of patients who reached a dose of 400 mg/d demonstrated a
statistically significant mean reduction in pain intensity score from baseline to
19 weeks compared to placebo.54–56
MEXILETINE. Mexiletine is a sodium channel blocker that has also been studied
for the treatment of neuropathic pain. It is typically prescribed for myotonia and
arrhythmias. In a placebo-controlled study, it did not provide pain relief greater
than placebo.57
TOPICAL LIDOCAINE AND CAPSAICIN. Topical agents may add symptomatic relief
and have the advantage of minimal side effects.58 Topical lidocaine is available
in both an ointment and patch form. Lidocaine can be a useful adjunctive therapy
in patients whose pain is well localized to the distal extremities.59,60 It has been
best studied in postherpetic neuralgia as the pain is in a more localized area. As the
neuropathy progresses and becomes more proximal, topical lidocaine becomes less
useful because of more area needing coverage. One strategy is to apply lidocaine
patches at night before bed as patients with neuropathic pain tend to notice their
pain more at night. Lidocaine patches should be used for a maximum of 12 hours
1308 OCTOBER 2020
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
on, followed by 12 hours off, and up to three patches may be used at a time. KEY POINTS
Lidocaine has been shown to be more useful as an add-on therapy.
● Despite a lower
Topical capsaicin has also been studied in postherpetic neuralgia and diabetic efficacy compared to
neuropathic pain and has Level B evidence.37 Capsaicin is a transient receptor gabapentinoids and
potential cation channel subfamily V member 1 (TRPV1) agonist. At low doses and serotonin norepinephrine
with brief exposure, it causes a burning sensation (capsaicin is the active ingredient in reuptake inhibitors,
antiepileptic drugs and
hot peppers). With a high dose or repeated exposure, it causes epidermal axonal mexiletine may still be worth
degeneration, which is the putative mechanism of action. The new capsaicin a trial in some patients with
patch approved by the FDA has a higher concentration of capsaicin (8%), and up refractory pain.
to four patches can be applied at a time, which will last for up to 3 months.61
● Topical agents (such as
Application must take place in the clinic in a well-ventilated area. The provider
lidocaine patches or cream)
applying the patch should wear nitrile gloves to prevent skin exposure. During are of modest efficacy but
the clinical trials, participants had lidocaine cream applied before putting on may add symptomatic relief
patches to minimize pain and discomfort from the patches. When using in selected patients with
neuropathic pain and have
low-dose topical capsaicin cream for neuropathic pain, patients must be warned
the advantage of minimal
that they will experience a period of burning discomfort with initiation of side effects.
therapy and that gloves should be worn during administration to avoid
inadvertent exposure to sensitive areas (eg, eyes). Previously, most experts used ● Opioid analgesics,
topical capsaicin sparingly and mainly for patients with tactile allodynia in a including tramadol, should
not be used as first- or
localized region. It is unclear how effective the new patch will be in clinic. second-line medications for
neuropathic pain and should
OPIOID ANALGESICS. Opioid analgesics (including tramadol) should not be used only be considered in severe
as first- or second-line medications for neuropathic pain and should only be and refractory cases when
considered in severe and refractory cases when all other options have failed. all other options have failed.
In general, referral to a pain
Oxycontin was shown to be effective in a placebo-controlled study and in clinic is recommended if
subsequent studies.62,63 Morphine was shown to have efficacy in combination opioid therapy is being
with other medications, such as gabapentin and pregabalin, in additional considered.
studies.64,65 Other opioids have not been as well studied but presumably have
similar benefits. Given the long-term safety and medicolegal implications of
prescribing opioid analgesics and that they are not recommended as first- or
second-line agents, it is advisable to refer these patients to a pain clinic for
initiation and management of opioid therapy because of the complexities
involved.66
Tramadol has a mixed mechanism of action. Tramadol is both a μ-opioid receptor
agonist and an SNRI. Tramadol has been studied in several trials, including trials for
pain in diabetic polyneuropathy and postherpetic neuralgia, and was found to be
effective compared to placebo.67,68 Tramadol is dosed starting at 25 mg and can be
increased to 50 mg administered up to every 6 hours, with a maximum of 400 mg/d.
Long-acting tramadol should not be increased to higher than 300 mg/d.
Tapentadol has a similar mechanism to tramadol in that it not only has weak
μ-opioid receptor agonism but also has norepinephrine reuptake inhibitor
activity. Initial studies of tapentadol showed minimal efficacy over placebo.69
However, studies with extended-release tapentadol showed a greater than 30%
decrease in pain in the majority of patients with painful diabetic peripheral
neuropathy.70,71 It was also studied in cancer pain in an open-label study and
chronic low back pain.72,73 Its weak efficacy makes it a third-line option. It is
dosed starting at 50 mg, increasing to 100 mg up to every 4 to 6 hours with a
maximum of 1600 mg/d.
Opioid-induced hyperalgesia is a significant phenomenon that is thought to be
caused by neuroplastic changes and sensitization to μ-opioid receptors and
CONTINUUMJOURNAL.COM 1309
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF NEUROPATHIC PAIN IN POLYNEUROPATHY
nociceptor toll-like receptor 4 (TLR4), which may arise from opioid activation
of mast cells, microglia, and other cells in the peripheral and central nervous
systems.74–76 It was first described in 1945 and is different from tolerance, which
occurs over time and requires gradually escalating dosages to maintain the
same level of analgesia. Opioid-induced hyperalgesia causes patients to have
increased pain and diffuse allodynia that is often different than their initial pain
manifestation.74 Although opioid-induced hyperalgesia may be more common with
higher-potency opioids, tramadol has also been reported to cause opioid-induced
hyperalgesia, making it a concern for lower-potency opioids as well.77 The treatment
is to recognize opioid-induced hyperalgesia when it occurs, taper opioids, and then
determine whether it is safe to restart opioid treatment (CASE 8-2).
Other medicines studied for neuropathic pain include dihydroergotamine
(a treatment for migraine), which is a 5-HT1 receptor agonist that may improve
pain in rat models,78 and memantine, an anti–N-methyl-D-aspartate (NMDA)
receptor antagonist used for dementia. Memantine has been studied in seven
CASE 8-2 A 67-year-old woman with type 2 diabetes presented with a 20-year
history of painful neuropathy symptoms. She was taking pregabalin,
oxcarbazepine, metaxalone, paroxetine, and tramadol and had been on
opioids for years, which were recently transitioned to fentanyl patches.
She had subjectively good pain control, and her hemoglobin A1c had been
maintained at 6.1%. Her main symptoms were memory issues and
dizziness.
At her appointment, she was slow to respond and had small pupils. She
had severe sensory loss to above the knees to both pin and vibration and
distal weakness of toe extensors and finger abductors. Deep tendon
reflexes were absent in the legs.
The decision was made to start tapering and weaning off her
medications because of concern for polypharmacy as she was exhibiting
poor balance, confusion, and sedation. She was weaned off
oxcarbazepine and metaxalone first because of the suspicion that they
were most likely related to side effects. At the next visit, discussion
about her opioid use was productive and she agreed to wean off opioids
given concern regarding the risk of opioid-induced hyperalgesia and
multiple side effects. She was slowly tapered off fentanyl over the next
several months with good results and fewer memory issues.
COMMENT Recognition of medication side effects and stepwise elimination or
decrease in dosage of medicines to avoid side effects is important.
Recognition of opioid tolerance and opioid-induced hyperalgesia is crucial,
although management of this situation is often difficult in practice and
avoidance of opioids is recommended. Many patients with refractory pain
are reluctant to reduce dosages, and education on this issue may take more
than one visit. For this reason, if a patient’s pain is refractory to multiple
medications, consideration of the use of opioids is best referred to an
experienced pain specialist and avoided as much as possible.
1310 OCTOBER 2020
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
trials, with only two showing benefit over placebo.79 Ketamine and amantadine KEY POINT
have also been studied, with mixed results.79 Ketamine, an anesthetic NMDA
● Opioid-induced
receptor antagonist, is commonly added to topical compounded creams for hyperalgesia causes
neuropathic pain but has not shown any clinical efficacy in topical form.80 patients to have increased
pain and diffuse allodynia
SUPPLEMENTS AND OTHER ALTERNATIVE TREATMENTS FOR that is often different than
their initial pain
NEUROPATHIC PAIN
manifestation.
Patients often seek complementary and alternative treatments for neuropathic
pain in polyneuropathy for multiple reasons. Some patients are fearful or
suspicious of pharmacologic therapies, and some may have had significant side
effects or incomplete efficacy. Some therapies have been advertised with
minimal clinical data. α-Lipoic acid is the best studied supplement, but other
commonly used supplements with some clinical studies are also discussed below.
α-Lipoic Acid
α-Lipoic acid is an antioxidant that has shown symptomatic benefit for patients
with painful diabetic polyneuropathy.81 It is most commonly used as an
adjunctive therapy or as a second-line agent. It may also be suggested to patients
who are averse to conventional pharmacotherapeutics and prefer a nutraceutical
option. α-Lipoic acid has been studied in several large studies with conflicting
evidence. The ALADIN III (Treatment of Symptomatic Diabetic Polyneuropathy
With the Antioxidant Alpha-Lipoic Acid: A 7-month Multicenter Randomized
Controlled Trial) study showed an improvement in Neuropathy Impairment
Score but not in Total Symptom Score.82 The SYDNEY 2 (Assessment of Efficacy
and Safety of Thioctic Acid in the Oral Treatment of Symptomatic Diabetic
Neuropathy) trial compared orally administered α-lipoic acid (600 mg/d,
1200 mg/d, or 1800 mg/d) to placebo. The primary outcome measure was change
in baseline Total Symptom Score. All three doses were found to be superior to
placebo in pain relief and Neuropathy Symptoms and Change Score, although
mean Total Symptom Score did not differ between treatment groups.81,83 The
NATHAN 1 (Assessment of Efficacy and Safety of Thioctic Acid in the Oral
Treatment of Diabetic Polyneuropathy [Stage 1 or 2]) study suggested that
patients with fewer comorbidities (eg, hypertension, cardiovascular disease, and
obesity) were more likely to improve in Neuropathy Impairment Score-Lower
Limbs.84,85 The most common adverse effects are acid reflux and nausea, but in
the authors’ experience, α-lipoic acid tends to be discontinued more often
because of ineffectiveness than because of tolerability issues.
Cannabidiol and Cannabis-derived Treatments
Cannabinoids have become a popular pharmacotherapy in many neurologic
disorders, such as multiple sclerosis, epilepsy, and Parkinson disease.
Cannabinoids bind to cannabinoid receptors, predominantly CB1 in the brain but
also TRPV1, peroxisome proliferator-activated receptor γ (PPARγ), GABA
receptors, and calcium channels.86 Many patients report anecdotal improvement
with the use of cannabidiol, whether taken orally or used as an ointment.2
A Cochrane Review evaluated 16 placebo-controlled studies of cannabinoid
products, including cannabidiol oil, tetrahydrocannabinol (THC) and
cannabidiol oronasal spray, nabilone (synthetic mimic of THC), inhaler herbal
cannabis, and plant-derived THC. The number needed to benefit was calculated
to be 20 because of small differences between placebo and cannabis products to
CONTINUUMJOURNAL.COM 1311
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF NEUROPATHIC PAIN IN POLYNEUROPATHY
decrease pain by a significant amount (28% in the cannabis group reported a
meaningful decrease in pain compared to 22% in the placebo group).87 Most
studies were of low quality with possible bias and small numbers.87 The side
effects of cannabis products include dizziness, sedation, hypotension, and ataxia.
Adverse effects may be worse in the elderly because of slower metabolism and
increased fat percentage.88 In addition, cannabis interacts with other commonly
used medications for neuropathic pain, such as valproic acid.89 Because of
current legal and regulatory concerns as well as insufficient data regarding its
efficacy in the treatment of painful diabetic polyneuropathy, the use of cannabis
cannot currently be recommended outside of an investigational setting. When
counseling patients about cannabidiol products, clinicians should emphasize that
well-designed clinical trials are lacking and that potentially significant side
effects may occur.
Other Supplements
Deficiencies of multiple B vitamins (most notably vitamins B1, B6, and B12) are
known to cause polyneuropathy.90,91 Metformin, a hypoglycemic agent
commonly used in diabetes, is also known to decrease vitamin B12 absorption,
potentially exacerbating existing diabetic polyneuropathy. A branded multi–B
vitamin supplement (levomefolate/Schizochytrium/pyridoxal phosphate/
methylcobalamin) has shown some efficacy in diabetic polyneuropathy.92,93
However, it is simply folate, vitamin B6, and B12, and costs up to $136 for
30 capsules, which is substantially more expensive compared to buying similar
supplements over the counter. In addition, the vitamin B6 component may
also increase risk for hypervitaminosis B6–associated toxicity, leading to
worsening sensory neuropathy/ganglionopathy. In the authors’ opinion, other
multivitamins that are marketed specifically to patients with neuropathy are also
expensive and provide no value beyond that of inexpensive over-the-counter
alternatives.
Additional supplements that have been advertised as potentially helpful
include acetyl-L-carnitine, a supplement thought to enhance mitochondrial
activity, which has been shown to improve diabetic polyneuropathy in animal
models.94 Curcumin has been anecdotally shown to improve neuropathy and
neuropathic pain, with some evidence in animal studies,95–97 and nutmeg and
St. John’s wort have also been shown to have some improvement in neuropathic
pain.98 Lion’s mane (Hericium erinaceus) may improve neuroregeneration and
increase nerve growth factor, with some nociceptive activity.99,100 Fish oil, which
contains omega-3 fatty acids,101,102 has also been touted for neuropathic pain
based on a study in rats.101 Clinical trial data are lacking, and the efficacy of fish
oil has not been established.
PSYCHIATRIC TREATMENT FOR REFRACTORY NEUROPATHIC PAIN
Specific studies of antidepressants not affecting norepinephrine reuptake, such
as SSRIs, have shown they are not specifically efficacious in the treatment of
neuropathic pain. However, they are still useful for underlying major depression,
which may exacerbate neuropathic pain.103 In addition, individualized treatment
of depression is important, and cognitive therapy can be a useful tool in
multidisciplinary pain clinics.104 Evaluation of the risk of suicide is important in
patients with refractory neuropathic pain as many treatments have a possible
effect of increased suicidality. Patients on opioid therapy are especially at risk for
1312 OCTOBER 2020
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
overdose, and increased monitoring is necessary to avoid it. Anecdotally, KEY POINTS
neuropathic pain that is refractory to multiple agents may be an indication of
● High-quality clinical trial
coexistent depression; screening for depression may lead to improved pain data supporting the use of
management. The use of SNRIs can be especially helpful with coexistent cannabinoids for
depression neuropathic pain are
lacking, and side effects are
common. Their use outside
NONPHARMACOLOGIC TREATMENT OF NEUROPATHIC PAIN
of clinical trials is
Many patients inquire about or try alternative treatments for neuropathic pain discouraged.
when pharmacologic treatments are insufficient or not tolerated or if they are
interested in complementary medicine. The literature on exercise and other ● Recognition and
nonpharmacologic therapies is summarized below. Most of these therapies individualized treatment of
depression is important,
have the same drawbacks of limited or absence of placebo-controlled rigorous and cognitive therapy can
clinical trials as do many of the pharmacologic treatments and supplements be a useful tool in
summarized. multidisciplinary pain
clinics.
Exercise ● Given the multiple health
Exercise is a largely overlooked treatment modality, but growing literature benefits of exercise and
documenting its efficacy in improving chronic neuropathic pain and improvement in other
potentially improving some etiologies of neuropathic pain make it a promising parameters of health,
exercise should be highly
therapeutic option for both neuropathic and non-neuropathic pain.105 It has
encouraged in all
been primarily studied in diabetic polyneuropathy and neuropathy associated patients with painful
with metabolic syndrome and prediabetes.106,107 Animal exercise studies polyneuropathy.
show that exercise increases dorsal root ganglion production of multiple
neurotrophic factors, including brain-derived neurotrophic factor and nerve
growth factors, and decreases proinflammatory cytokines such as tumor necrosis
factor-α and IL-1β.108,109 In addition to improving pain, exercise may improve
the underlying neuropathy among patients with metabolic syndrome,110 likely
by improving insulin sensitivity and multiple metabolic factors, including
dyslipidemia.110,111
The specific type and amount of exercise necessary to result in improved pain
and neuropathy is uncertain, as is the relative importance of associated dietary
counseling. Moderate aerobic exercise in addition to strength training has been
studied in supervised and unsupervised settings and has shown improvement in
pain and objective parameters of neuropathy.112,113 Tai chi and other balance
exercises may improve fall risk, but outcome measures have not included pain, so
it is undetermined whether they also improve pain control.114 Yoga may help
with chronic pain but has not been studied specifically in neuropathic pain
populations.115 Given the multiple health benefits of exercise, including
improvement in other parameters of health, exercise should be highly
encouraged in all patients with painful polyneuropathy. The authors typically
recommend 30 minutes of moderate-intensity exercise daily, using whatever
modality the patient most enjoys and can sustainably tolerate.
Spinal Cord Stimulation
The premise of spinal cord stimulation is that electrical stimulation of nerve roots
or dorsal columns via a surgically placed electrode in the epidural space would act
as a gate and block pain perception without ablation. Electrical stimulation is
produced by a radio-controlled device to modulate anesthesia. Two trials of
spinal cord stimulation have shown at least short-term benefits in painful
diabetic polyneuropathy,116,117 with some patients experiencing durable
CONTINUUMJOURNAL.COM 1313
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF NEUROPATHIC PAIN IN POLYNEUROPATHY
improvement.118 Long-term cost-effectiveness is unclear compared to
pharmacologic treatments as the short-term cost is relatively high and not all
patients benefit long term.119,120 Significant risk exists, and complications are
possible, including infection, damage to the nerve roots or cord during surgical
placement, and hardware failures. In addition, patients are unable to get future
MRIs after placement, and pain relief decreases over time. This treatment
modality may be an option in patients with refractory pain or in those who are
intolerant to multiple medications, but only in the hands of experienced
surgeons and well-trained personnel. In general, spinal cord stimulation should
only be recommended following a thorough evaluation in a multidisciplinary
pain clinic.
Acupuncture
Acupuncture is an established treatment for pain in China and other Asian
countries, but placebo-controlled studies are limited. Acupuncture’s mechanism
of action is not well established, although it has been theorized to either affect
descending pain control pathways or to decrease neuroinflammation.121 In one
study, acupuncture was shown to be associated with improved glycemic
control.122 A Cochrane Review found insufficient evidence to support or refute
acupuncture’s efficacy for neuropathic pain.123 Although most studies were
small and many had significant methodologic limitations, several suggest some
benefit in diabetic polyneuropathy and chemotherapy-induced peripheral
neuropathy.123–126 In the United States, access to acupuncture is limited in many
nonurban settings. The authors offer acupuncture as an option for patients with
pain that is refractory to multiple medications and those who are interested in
alternative therapies. Not all insurance plans cover acupuncture, so a discussion
regarding cost is important. However, this has changed significantly in the past
10 years, and Medicare and other private insurers may now cover to a limited
number of visits.
AN ALGORITHMIC APPROACH TO NEUROPATHIC PAIN MANAGEMENT
Most patients with painful polyneuropathy should be started on either a
gabapentinoid or an SNRI as a first-line agent, although the choice of agent
should be based on patient comorbidities. Patients with associated RLS may
benefit from the dual action of gabapentinoids, whereas a patient with symptoms
of associated depression may benefit more from an SNRI such as duloxetine or
venlafaxine. After appropriate titration to a maximally tolerated dose, the patient
should be reevaluated in 6 to 8 weeks for efficacy and consideration of a second
or alternative agent or treatment approach (TABLE 8-2 and TABLE 8-3). Many
patients require more than one agent for effective treatment.65 Typically, if a
gabapentinoid is started first, a tricyclic antidepressant or SNRI would be added
second and vice versa. Tricyclic antidepressants are typically not started as
first-line agents because of significant side effects in the elderly, but they may be
reasonable first-line agents in younger patients (eg, in a younger patient with
significant insomnia) (CASE 8-3).
All patients should be counseled regarding the positive effects of exercise.
Many patients with painful polyneuropathy are resistant to exercise and worry it
will make pain worse. Also, many patients with diabetic polyneuropathy may
be sedentary, morbidly obese, and have joint symptoms that may limit exercise
choices. Working with patients on finding affordable and realistic goals of
1314 OCTOBER 2020
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
exercise and access to exercise equipment can be a challenge. However, if they
exercise, many patients will see that it improves pain and overall quality of life.
If combination therapy is not helpful and patients have tolerated appropriate
dose escalation without improvement, complementary agents (such as α-lipoic
acid) and other second-line agents or nonpharmacologic treatments (such as
acupuncture) should be considered. If pain continues to be refractory and trials
of even third-line agents are unsuccessful, referral to a multidisciplinary pain
clinic is helpful. A multidisciplinary pain clinic can evaluate for possible
treatment using spinal cord stimulation, opioids, or other treatments beyond the
scope of this review (TABLE 8-3).
A 52-year-old woman presented with a 3-year history of burning pain and CASE 8-3
tingling in her feet associated with a severe pruritic sensation. She had a
past medical history of hypertension, hypertriglyceridemia, obstructive
sleep apnea, and anxiety. She reported that she had been taking vitamin B
supplements for years.
Physical examination revealed a blood pressure of 136/85 mm Hg and a
body mass index of 32.2 (class 1 obesity). Excoriations on the feet were
observed related to intense scratching, and she had a distal gradient
temperature loss to the ankles and wrists bilaterally. Distal vibratory
sensation and deep tendon reflexes were intact.
Her laboratory workup revealed a vitamin B6 level elevated to 4 times
the upper limit of normal (20 nmol/L to 125.0 nmol/L).
All extraneous sources of vitamin B6, including supplements, were
discontinued. She was started on gabapentin but was unable to tolerate it
because of daytime sleepiness and cognitive fog. She was then switched
to duloxetine, which helped somewhat, but she was unable to tolerate
doses higher than 30 mg/d because of hyperhidrosis. Low-dose
pregabalin was later added and cautiously titrated up given her prior
sensitivity to gabapentin. She tolerated this regimen well.
This case illustrates several important points, including the importance of COMMENT
trialing different medications within the same class (eg, gabapentin and
pregabalin) as well as selecting medications to target underlying
comorbidities. In this case, a serotonin norepinephrine reuptake inhibitor
(SNRI) was used to target comorbid anxiety. Additionally, the patient had
reported pruritus, which highlights an often-overlooked symptom. Pruritus
can be neuropathic in nature and seen in the setting of small fiber
neuropathy. Her examination findings of distal temperature loss with intact
vibratory sensation and reflexes is suggestive of a predominately small
fiber process. Finally, it is not uncommon for patients with painful
polyneuropathy to have multiple different risk factors or causes. This
patient had metabolic syndrome and an elevated pyridoxine (vitamin B6)
level, each of which can cause a painful small fiber neuropathy. Patients
with an established cause for polyneuropathy, including diabetes, should
also be carefully evaluated for other potential etiologies.
CONTINUUMJOURNAL.COM 1315
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF NEUROPATHIC PAIN IN POLYNEUROPATHY
KEY POINT It is very important to explore sleep disturbances, depression, and anxiety
with every patient. Those with comorbid depression may benefit from an
● An algorithmic approach
that integrates
SNRI, and independent therapy for associated sleep and mood disorders may
pharmacologic and be necessary.
nonpharmacologic therapy Analysis of failure of neuropathic pain treatment is important. Failure is
with specific attention to commonly due to lack of appropriate dose escalation (without adverse side effects),
comorbid sleep and mood
inadequate treatment duration (ie, less than 6 weeks), or side effects related to the
disorders is the most
effective approach to specific agent used. Sometimes, patients discontinue a medication due to symptoms
neuropathic pain that may not be related to the agent. Retrial at a lower dose with slower titration can
management. be helpful, especially in patients for whom multiple agents have failed. Screening for
coexistent conditions such as depression, RLS, and other conditions that may
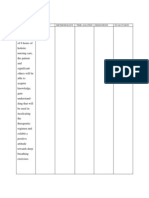
impede success is helpful (FIGURE 8-1127).128,129
CONCLUSION
Management of painful polyneuropathies is challenging and often requires
multiple strategies. An urgent need exists for additional therapeutic
development, including clinical trials that enroll patients with idiopathic and
other forms of painful neuropathy such as chemotherapy-induced peripheral
neuropathy. The largest contribution in recent literature has been the
demonstration of exercise as a therapeutic strategy for neuropathic pain. Further
FIGURE 8-1
An algorithmic approach to neuropathic pain management.
ALA = α-lipoic acid; Rx = prescription; SNRIs = serotonin norepinephrine reuptake inhibitors;
TCAs = tricyclic antidepressants.
Modified with permission from Bates D, et al, Pain Med.127 © 2019 Oxford University Press.
1316 OCTOBER 2020
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
work needs to be done in demonstrating the optimal type and dose of exercise.
An algorithmic approach that integrates pharmacologic and nonpharmacologic
therapy with specific attention to comorbid sleep and mood disorders is the most
effective approach to neuropathic pain management. Patients with severe or
refractory neuropathic pain may benefit from a referral to a multidisciplinary
pain clinic.
REFERENCES
1 Gregg EW, Sorlie P, Paulose-Ram R, et al. 11 Gordois A, Scuffham P, Shearer A, et al. The
Prevalence of lower-extremity disease in the US health care costs of diabetic peripheral
adult population >=40 years of age with and neuropathy in the US. Diabetes Care 2003;26(6):
without diabetes: 1999–2000 national health and 1790–1795. doi:10.2337/diacare.26.6.1790.
nutrition examination survey. Diabetes Care
12 Kiyani M, Yang Z, Charalambous LT, et al. Painful
2004;27(7):1591–1597. doi:10.2337/
diabetic peripheral neuropathy: health care
diacare.27.7.1591.
costs and complications from 2010 to 2015.
2 Diabetes Control and Complications Trial Neurol Clin Pract 2020;10(1):47–57. doi:10.1212/
Research Group, Nathan DM, Genuth S, et al. CPJ.0000000000000671.
The effect of intensive treatment of diabetes on
13 Liedgens H, Obradovic M, De Courcy J, et al. A
the development and progression of long-term
burden of illness study for neuropathic pain in
complications in insulin-dependent diabetes
Europe. Clinicoecon Outcomes Res 2016;8:
mellitus. N Engl J Med 1993;329(14):977–986.
113–126. doi:10.2147/CEOR.S81396.
doi:10.1056/NEJM199309303291401.
14 Dworkin RH, Malone DC, Panarites CJ, et al.
3 Hanewinckel R, Drenthen J, van Oijen M, et al.
Impact of postherpetic neuralgia and painful
Prevalence of polyneuropathy in the general
diabetic peripheral neuropathy on health care
middle-aged and elderly population. Neurology
costs. J Pain 2010;11(4):360–368. doi:10.1016/j.
2016;87(18):1892–1898. doi:10.1212/
jpain.2009.08.005.
WNL.0000000000003293.
15 Schaefer C, Mann R, Sadosky A, et al. Burden
4 Hicks CW, Selvin E. Epidemiology of peripheral
of illness associated with peripheral and
neuropathy and lower extremity disease in
central neuropathic pain among adults seeking
diabetes. Curr Diab Rep 2019;19(10):86. doi:10.
treatment in the United States: a patient-
1007/s11892-019-1212-8.
centered evaluation. Pain Med 2014;15(12):
5 Seretny M, Currie GL, Sena ES, et al. Incidence, 2105–2119. doi:10.1111/pme.12502.
prevalence, and predictors of chemotherapy-
16 Schaefer C, Sadosky A, Mann R, et al. Pain
induced peripheral neuropathy: a systematic
severity and the economic burden of
review and meta-analysis. Pain 2014;155(12):
neuropathic pain in the United States: BEAT
2461–2470. doi:10.1016/j.pain.2014.09.020.
Neuropathic Pain Observational Study.
6 Nickel FT, Seifert F, Lanz S, Maihöfner C. Clinicoecon Outcomes Res 2014;6:483–496.
Mechanisms of neuropathic pain. doi:10.2147/CEOR.S63323.
Eur Neuropsychopharmacol 2012;22(2):81–91.
17 Dworkin RH, Panarites CJ, Armstrong EP, et al.
doi:10.1016/j.euroneuro.2011.05.005.
Healthcare utilization in people with
7 van Hecke O, Austin SK, Khan RA, et al. postherpetic neuralgia and painful diabetic
Neuropathic pain in the general population: a peripheral neuropathy. J Am Geriatr Soc 2011;
systematic review of epidemiological studies. 59(5):827–836. doi:10.1111/j.1532-5415.2011.03403.x.
Pain 2014;155(4):654–662. doi:10.1016/j.pain.2013.
18 Boyd A, Casselini C, Vinik E, Vinik A. Quality of life
11.013.
and objective measures of diabetic neuropathy
8 Bouhassira D, Lantéri-Minet M, Attal N, et al. in a prospective placebo-controlled trial of
Prevalence of chronic pain with neuropathic ruboxistaurin and topiramate. J Diabetes Sci
characteristics in the general population. Pain Technol 2011;5(3):714–722.
2008;136(3):380–387. doi:10.1016/j.pain.2007.08.013. doi:10.1177/193229681100500326.
9 Tofthagen CS, McMillan SC. Pain, neuropathic 19 Colloca L, Ludman T, Bouhassira D, et al.
symptoms, and physical and mental well-being in Neuropathic pain. Nat Rev Dis Primers 2017;3:
persons with cancer. Cancer Nurs 2010;33(6): 17002. doi:10.1038/nrdp.2017.2.
436–444. doi:10.1097/NCC.0b013e3181e212b4.
20 Galer BS, Gianas A, Jensen MP. Painful diabetic
10 Gaskin DJ, Richard P. The economic costs of pain polyneuropathy: epidemiology, pain description,
in the United States. J Pain 2012;13(8):715–724. and quality of life. Diabetes Res Clin Pract 2000;
doi:10.1016/j.jpain.2012.03.009. 47(2):123–128. doi:10.1016/s0168-8227(99)00112-6.
CONTINUUMJOURNAL.COM 1317
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF NEUROPATHIC PAIN IN POLYNEUROPATHY
21 Poliakov I, Toth C. The impact of pain in patients 34 Patel R, Dickenson AH. Mechanisms of the
with polyneuropathy. Eur J Pain 2011;15(10): gabapentinoids and α 2 δ-1 calcium channel
1015–1022. doi:10.1016/j.ejpain.2011.04.013. subunit in neuropathic pain. Pharmacol Res
Perspect 2016;4(2):e00205. doi:10.1002/
22 McMillan SC, Tofthagen C, Morgan MA.
prp2.205.
Relationships among pain, sleep disturbances,
and depressive symptoms in outpatients from 35 Fink K, Meder W, Dooley DJ, Göthert M. Inhibition
a comprehensive cancer center. Oncol Nurs of neuronal Ca (2+) influx by gabapentin and
Forum 2008;35(4):603–611. doi:10.1188/08. subsequent reduction of neurotransmitter
ONF.603-611. release from rat neocortical slices. Br J
Pharmacol 2000;130(4):900–906. doi:10.1038/sj.
23 Cheatle MD, Foster S, Pinkett A, et al. Assessing
bjp.0703380.
and managing sleep disturbance in patients with
chronic pain. Sleep Med Clin 2016;11(4):531–541. 36 Li C, Lei Y, Tian Y, et al. The etiological
doi:10.1016/j.jsmc.2016.08.004. contribution of GABAergic plasticity to the
pathogenesis of neuropathic pain. Mol Pain 2019;
24 Ferini-Strambi L. Neuropathic pain and sleep: a
15:1744806919847366. doi:10.1177/
review. Pain Ther 2017;6(suppl 1):19–23.
1744806919847366.
doi:10.1007/s40122-017-0089-y.
37 Bril V, England J, Franklin GM, et al. Evidence-
25 Mehta N, Bucior I, Bujanover S, et al. Relationship
based guideline: treatment of painful diabetic
between pain relief, reduction in pain-associated
neuropathy: report of the American Academy
sleep interference, and overall impression of
of Neurology, the American Association of
improvement in patients with postherpetic
Neuromuscular and Electrodiagnostic Medicine,
neuralgia treated with extended-release
and the American Academy of Physical Medicine
gabapentin. Health Qual Life Outcomes 2016;
and Rehabilitation. Neurology 2011;76(20):
14:54. doi:10.1186/s12955-016-0456-0.
1758–1765. doi:10.1212/WNL.0b013e3182166ebe.
26 Selvarajah D, Cash T, Sankar A, et al. The
38 Bockbrader HN, Wesche D, Miller R, et al. A
contributors of emotional distress in painful
comparison of the pharmacokinetics and
diabetic neuropathy. Diab Vasc Dis Res 2014;11(4):
pharmacodynamics of pregabalin and
218–225. doi:10.1177/1479164114522135.
gabapentin. Clin Pharmacokinet 2010;49(10):
27 Esposito MF, Malayil R, Hanes M, Deer T. 661–669. doi:10.2165/11536200-000000000-00000.
Unique characteristics of the dorsal root
39 McLean MJ. Clinical pharmacokinetics of
ganglion as a target for neuromodulation. Pain
gabapentin. Neurology 1994;44(6 suppl 5):
Med 2019;20(suppl 1):S23–S30. doi:10.1093/
S17–S22; discussion S31–S32.
pm/pnz012.
40 Backonja M, Beydoun A, Edwards KR, et al.
28 Estacion M, Han C, Choi JS, et al. Intra- and
Gabapentin for the symptomatic treatment of
interfamily phenotypic diversity in pain
painful neuropathy in patients with diabetes
syndromes associated with a gain-of-function
mellitus: a randomized controlled trial. JAMA
variant of NaV1.7. Mol Pain 2011;7:92.
1998;280(21):1831–1836. doi:10.1001/
doi:10.1186/1744-8069-7-92.
jama.280.21.1831.
29 Dib-Hajj SD, Waxman SG. Sodium channels in
41 Rosenstock J, Tuchman M, LaMoreaux L,
human pain disorders: genetics and
Sharma U. Pregabalin for the treatment of painful
pharmacogenomics. Annu Rev Neurosci 2019;
diabetic peripheral neuropathy: a double-blind,
42:87–106. doi:10.1146/annurev-neuro-070918-
placebo-controlled trial. Pain 2004;110(3):
050144.
628–638. doi:10.1016/j.pain.2004.05.001.
30 Wadhawan S, Pant S, Golhar R, et al. NaV channel
42 Rauck R, Makumi CW, Schwartz S, et al.
variants in patients with painful and nonpainful
A randomized, controlled trial of gabapentin
peripheral neuropathy. Neurol Genet 2017;3(6):
enacarbil in subjects with neuropathic pain
e207. doi:10.1212/NXG.0000000000000207.
associated with diabetic peripheral neuropathy.
31 Hoeijmakers JG, Faber CG, Merkies IS, Waxman Pain Pract 2013;13(6):485–496. doi:10.1111/
SG. Painful peripheral neuropathy and sodium papr.12014.
channel mutations. Neurosci Lett 2015;596:51–59.
43 Vrethem M, Boivie J, Arnqvist H, et al. A
doi:10.1016/j.neulet.2014.12.056.
comparison of amitriptyline and maprotiline
32 Waxman SG, Merkies ISJ, Gerrits MM, et al. in the treatment of painful polyneuropathy in
Sodium channel genes in pain-related diabetics and nondiabetics. Clin J Pain 1997;13(4):
disorders: phenotype-genotype associations 313–323. doi:10.1097/00002508-199712000-00009.
and recommendations for clinical use. Lancet
44 Obata H. Analgesic mechanisms of
Neurol 2014;13(11):1152–1160. doi:10.1016/
antidepressants for neuropathic pain. Int J Mol
S1474-4422(14)70150-4.
Sci 2017;18(11). pii:E2483. doi:10.3390/ijms18112483.
33 Bennett DL, Clark AJ, Huang J, et al. The role of
45 Ormseth MJ, Scholz BA, Boomershine CS.
voltage-gated sodium channels in pain signaling.
Duloxetine in the management of diabetic
Physiol Rev 2019;99(2):1079–1151. doi:10.1152/
peripheral neuropathic pain. Patient Prefer
physrev.00052.2017.
Adherence 2011;5:343–356. doi:10.2147/PPA.S16358.
1318 OCTOBER 2020
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
46 Raskin J, Pritchett YL, Wang F, et al. A double- 58 Sommer C, Cruccu G. Topical treatment of
blind, randomized multicenter trial comparing peripheral neuropathic pain: applying the
duloxetine with placebo in the management of evidence. J Pain Symptom Manage 2017;53(3):
diabetic peripheral neuropathic pain. Pain Med 614–629. doi:10.1016/j.jpainsymman.2016.09.015.
2005;6(5):346–356. doi:10.1111/j.1526-4637.2005.
59 Wolff RF, Bala MM, Westwood M, et al. 5%
00061.x.
lidocaine-medicated plaster vs other relevant
47 Rowbotham MC, Goli V, Kunz NR, Lei D. interventions and placebo for post-herpetic
Venlafaxine extended release in the treatment of neuralgia (PHN): a systematic review. Acta Neurol
painful diabetic neuropathy: a double-blind, Scand 2011;123(5):295–309. doi:10.1111/j.1600-
placebo-controlled study. Pain 2004;110(3): 0404.2010.01433.x.
697–706. doi:10.1016/j.pain.2004.05.010.
60 Martini A, Del Balzo G, Schweiger V, et al.
48 Kochar DK, Jain N, Agarwal RP, et al. Sodium Efficacy of lidocaine 5% medicated plaster
valproate in the management of painful (VERSATIS®) in patients with localized
neuropathy in type 2 diabetes - a randomized neuropathic pain poorly responsive to
placebo controlled study. Acta Neurol Scand pharmacological therapy. Minerva Med
2002;106(5):248–252. doi:10.1034/j.1600-0404. 2018;109(5):344–351. doi:10.23736/S0026-
2002.01229.x. 4806.18.05690-2.
49 Kochar DK, Rawat N, Agrawal RP, et al. Sodium 61 Baranidhran G, Das S, Bhaskar A. A review of the
valproate for painful diabetic neuropathy: a high-concentration capsaicin patch and
randomized double-blind placebo-controlled experience in its use in the management of
study. QJM 2004;97(1):33–38. doi:10.1093/qjmed/ neuropathic pain. Ther Adv Neurol Disord 2013;
hch007. 6(5):287–297. doi:10.1177/1756285613496862.
50 Dogra S, Beydoun S, Mazzola J, et al. 62 Portenoy RK, Farrar JT, Backonja MM, et al.
Oxcarbazepine in painful diabetic neuropathy: a Long-term use of controlled-release oxycodone
randomized, placebo-controlled study. Eur J Pain for noncancer pain: results of a 3-year registry
2005;9(5):543–554. doi:10.1016/j.ejpain.2004.11.006. study. Clin J Pain 2007;23(4):287–299.
doi:10.1097/AJP.0b013e31802b582f.
51 Wiffen PJ, Derry S, Moore RA, Kalso EA.
Carbamazepine for chronic neuropathic pain and 63 Watson CP, Moulin D, Watt-Watson J, et al.
fibromyalgia in adults. Cochrane Database Syst Controlled-release oxycodone relieves
Rev 2014(4):CD005451 doi:10.1002/14651858. neuropathic pain: a randomized controlled trial in
CD005451.pub3. painful diabetic neuropathy. Pain 2003;105(1–2):
71–78. doi:10.1016/s0304-3959(03)00160-x.
52 Raskin P, Donofrio PD, Rosenthal NR, et al.
Topiramate vs placebo in painful diabetic 64 Gilron I, Bailey JM, Tu D, et al. Morphine,
neuropathy: analgesic and metabolic effects. gabapentin, or their combination for neuropathic
Neurology 2004;63(5):865–873. doi:10.1212/01. pain. N Engl J Med 2005;352(13):1324–1334.
wnl.0000137341.89781.14. doi:10.1056/NEJMoa042580.
53 ClinicalTrials.gov. Topiramate for Cryptogenic 65 Chaparro LE, Wiffen PJ, Moore RA, Gilron I.
Sensory Peripheral Neuropathy in Metabolic Combination pharmacotherapy for the
Syndrome (CSPN) (TopCSPN). clinicaltrials.gov/ treatment of neuropathic pain in adults.
ct2/show/NCT02878798?recrs=ad&cond= Cochrane Database Syst Rev 2012(7):CD008943.
topiramate&draw=2&rank=5. Accessed doi:10.1002/14651858.CD008943.pub2.
August 4, 2020.
66 Finnerup NB, Otto M, McQuay HJ, et al. Algorithm
54 Vinik AI, Tuchman M, Safirstein B, et al. for neuropathic pain treatment: an evidence
Lamotrigine for treatment of pain associated based proposal. Pain 2005;118(3):289–305.
with diabetic neuropathy: results of two doi:10.1016/j.pain.2005.08.013.
randomized, double-blind, placebo-controlled
67 Harati Y, Gooch C, Swenson M, et al. Double-
studies. Pain 2007;128(1–2):169–179. doi:10.1016/
blind randomized trial of tramadol for the
j.pain.2006.09.040.
treatment of the pain of diabetic neuropathy.
55 Dick IE, Brochu RM, Purohit Y, et al. Sodium Neurology 1998;50(6):1842–1846. doi:10.1212/
channel blockade may contribute to the wnl.50.6.1842.
analgesic efficacy of antidepressants. J Pain
68 Boureau F, Legallicier P, Kabir-Ahmadi M.
2007;8(4):315–324. doi:10.1016/j.jpain.2006.10.001.
Tramadol in post-herpetic neuralgia: a
56 Wiffen PJ, Derry S, Moore RA. Lamotrigine for randomized, double-blind, placebo-controlled
chronic neuropathic pain and fibromyalgia in trial. Pain 2003;104(1–2):323–331. doi:10.1016/
adults. Cochrane Database Syst Rev 2013(12): s0304-3959(03)00020-4.
CD006044. doi:10.1002/14651858.CD006044.
69 Tominaga Y, Koga H, Uchida N, et al.
pub4.
Methodological issues in conducting pilot trials
57 Wallace MS, Magnuson S, Ridgeway B. Efficacy in chronic pain as randomized, double-blind,
of oral mexiletine for neuropathic pain with placebo-controlled studies. Drug Res (Stuttg)
allodynia: a double-blind, placebo-controlled, 2016;66(7):363–370. doi:10.1055/s-0042-107669.
crossover study. Reg Anesth Pain Med 2000;
25(5):459–467. doi:10.1053/rapm.2000.8583.
CONTINUUMJOURNAL.COM 1319
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF NEUROPATHIC PAIN IN POLYNEUROPATHY
70 Schwartz S, Etropolski M, Shapiro DY, et al. 82 Ziegler D, Hanefeld M, Ruhnau KJ, et al.
Safety and efficacy of tapentadol ER in patients Treatment of symptomatic diabetic
with painful diabetic peripheral neuropathy: polyneuropathy with the antioxidant alpha-lipoic
results of a randomized-withdrawal, placebo- acid: a 7-month multicenter randomized
controlled trial. Curr Med Res Opin 2011;27(1): controlled trial (ALADIN III Study). ALADIN III
151–162. doi:10.1185/03007995.2010.537589. Study Group. Alpha-Lipoic Acid in Diabetic
Neuropathy. Diabetes Care 1999;22(8):1296–1301.
71 Schwartz S, Etropolski MS, Shapiro DY, et al. A
doi:10.2337/diacare.22.8.1296.
pooled analysis evaluating the efficacy and
tolerability of tapentadol extended release for 83 Foster TS. Efficacy and safety of alpha-lipoic
chronic, painful diabetic peripheral neuropathy. acid supplementation in the treatment of
Clin Drug Investig 2015;35(2):95–108. doi:10.1007/ symptomatic diabetic neuropathy. Diabetes
s40261-014-0249-3. Educ 2007;33(1):111–117. doi:10.1177/0145721706297450.
72 Galie E, Villani V, Terrenato I, Pace A. 84 Ziegler D, Low PA, Freeman R, et al. Predictors of
Tapentadol in neuropathic pain cancer patients: improvement and progression of diabetic
a prospective open label study. Neurol Sci 2017; polyneuropathy following treatment with
38(10):1747–1752. doi:10.1007/s10072-017-3035-1. α-lipoic acid for 4 years in the NATHAN 1 trial.
J Diabetes Complications 2016;30(2):350–356.
73 Freo U, Romualdi P, Kress HG. Tapentadol for
doi:10.1016/j.jdiacomp.2015.10.018.
neuropathic pain: a review of clinical studies. J Pain
Res 2019;12:1537–1551. doi:10.2147/JPR.S190162. 85 Ziegler D, Low PA, Litchy WJ, et al. Efficacy and
safety of antioxidant treatment with α-lipoic acid
74 Chu LF, Angst MS, Clark D. Opioid-induced
over 4 years in diabetic polyneuropathy: the
hyperalgesia in humans: molecular mechanisms
NATHAN 1 trial. Diabetes Care 2011;34(9):
and clinical considerations. Clin J Pain 2008;24(6):
2054–2060. doi:10.2337/dc11-0503.
479–496. doi:10.1097/AJP.0b013e31816b2f43.
86 Cristino L, Bisogno T, Di Marzo V. Cannabinoids
75 Araldi D, Bogen O, Green PG, Levine JD.
and the expanded endocannabinoid system in
Role of nociceptor toll-like receptor 4 (TLR4) in
neurological disorders. Nat Rev Neurol 2020;16(1):
opioid-induced hyperalgesia and hyperalgesic
9–29. doi:10.1038/s41582-019-0284-z.
priming. J Neurosci 2019;39(33):6414–6424.
doi:10.1523/JNEUROSCI.0966-19.2019. 87 Mucke M, Phillips T, Radbruch L, et al. Cannabis-
based medicines for chronic neuropathic pain in
76 Varrassi G, Fusco M, Skaper SD, et al. A
adults. Cochrane Database Syst Rev 2018;3:
pharmacological rationale to reduce the
CD012182. doi:10.1002/14651858.CD012182.pub2.
incidence of opioid induced tolerance and
hyperalgesia: a review. Pain Ther 2018;7(1):59–75. 88 Kamrul R, Bunka D, Crawley A, et al. Navigating
doi:10.1007/s40122-018-0094-9. cannabinoid choices for chronic neuropathic
pain in older adults: potholes and highlights.
77 Lee SH, Cho SY, Lee HG, et al. Tramadol induced
Can Fam Physician 2019;65(11):807–811.
paradoxical hyperalgesia. Pain Physician 2013;
16(1):41–44. 89 Foster BC, Abramovici H, Harris CS. Cannabis and
cannabinoids: kinetics and interactions. Am J
78 Kayser V, Aubel B, Hamon M, Bourgoin S. The
Med 2019;132(11):1266–1270. doi:10.1016/j.amjmed.
antimigraine 5-HT 1B/1D receptor agonists,
2019.05.017.
sumatriptan, zolmitriptan and dihydroergotamine,
attenuated pain-related behaviour in a rat model 90 Alvarez M, Sierra OR, Saavedra G, Moreno S.
of trigeminal neuropathic pain. Br J Pharmacol Vitamin B12 deficiency and diabetic neuropathy
2002;137(8):1287–1297. doi:10.1038/sj. in patients taking metformin: a cross-sectional
bjp.0704979. study. Endocr Connect 2019;8(10):1324–1329.
doi:10.1530/EC-19-0382.
79 Aiyer R, Mehta N, Gungor S, Gulati A. A
systematic review of NMDA receptor 91 Gwathmey KG, Grogan J. Nutritional neuropathies.
antagonists for treatment of neuropathic pain in Muscle Nerve 2019. doi:10.1002/mus.26783.
clinical practice. Clin J Pain 2018;34(5):450–467.
92 Fonseca VA, Lavery LA, Thethi TK, et al. Metanx in
doi:10.1097/AJP.0000000000000547.
type 2 diabetes with peripheral neuropathy: a
80 Yang XD, Fang PF, Xiang DX, Yang YY. Topical randomized trial. Am J Med 2013;126(2):141–149.
treatments for diabetic neuropathic pain. doi:10.1016/j.amjmed.2012.06.022.
Exp Ther Med 2019;17(3):1963–1976. doi:10.3892/
93 Shevalye H, Watcho P, Stavniichuk R, et al.
etm.2019.7173.
Metanx alleviates multiple manifestations of
81 Ziegler D, Ametov A, Barinov A, et al. Oral peripheral neuropathy and increases
treatment with alpha-lipoic acid improves intraepidermal nerve fiber density in Zucker
symptomatic diabetic polyneuropathy: the diabetic fatty rats. Diabetes 2012;61(8):2126–2133.
SYDNEY 2 trial. Diabetes Care 2006;29(11): doi:10.2337/db11-1524.
2365–2370. doi:10.2337/dc06-1216.
94 Sima AA, Ristic H, Merry A, et al. Primary
preventive and secondary interventionary
effects of acetyl-L-carnitine on diabetic
neuropathy in the bio-breeding Worcester rat.
J Clin Invest 1996;97(8):1900–1907. doi:10.1172/
JCI118621.
1320 OCTOBER 2020
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
95 Zhang DW, Fu M, Gao SH, Liu JL. Curcumin and 106 Diabetes Prevention Program Research Group,
diabetes: a systematic review. Evid Based Knowler WC, Fowler SE, et al. 10-year follow-up
Complement Alternat Med 2013;2013:636053. of diabetes incidence and weight loss in the
doi:10.1155/2013/636053. Diabetes Prevention Program Outcomes Study.
Lancet 2009;374(9702):1677–1686. doi:10.1016/
96 Zhang X, Guan Z, Wang X, et al. Curcumin
S0140-6736(09)61457-4.
alleviates oxaliplatin-induced peripheral
neuropathic pain through inhibiting oxidative 107 Smith AG, Russell J, Feldman EL, et al. Lifestyle
stress-mediated activation of NF-κB and intervention for pre-diabetic neuropathy.
mitigating inflammation. Biol Pharm Bull 2020; Diabetes Care 2006;29(6):1294–1299. doi:10.2337/
43(2):348–355. doi:10.1248/bpb.b19-00862. dc06-0224.
97 Pastrana-Quintos T, Salgado-Mareno G, 108 Cooper MA, Kluding PM, Wright DE. Emerging
Pérez-Ramos J, et al. Anti-allodynic effect relationships between exercise, sensory nerves,
induced by curcumin in neuropathic rat is and neuropathic pain. Front Neurosci 2016;10:
mediated through the NO-cyclic-GMP-ATP 372. doi:10.3389/fnins.2016.00372. eCollection
sensitive K+ channels pathway. BMC 2016.
Complement Med Ther 2020;20(1):83.
109 Kluding PM, Pasnoor M, Singh R, et al. The effect
doi:10.1186/s12906-020-2867-z.
of exercise on neuropathic symptoms, nerve
98 Boyd A, Bleakley C, Hurley DA, et al. Herbal function, and cutaneous innervation in people
medicinal products or preparations for with diabetic peripheral neuropathy. J Diabetes
neuropathic pain. Cochrane Database Syst Rev Complications 2012;26(5):424–429. doi:10.1016/j.
2019;4:CD010528. doi:10.1002/14651858. jdiacomp.2012.05.007.
CD010528.pub4.
110 Singleton JR, Marcus RL, Lessard MK, et al.
99 Lai PL, Naidu M, Sabaratnam V, et al. Supervised exercise improves cutaneous
Neurotrophic properties of the lion’s mane reinnervation capacity in metabolic syndrome
medicinal mushroom, Hericium erinaceus (higher patients. Ann Neurol 2015;77(1):146–153.
Basidiomycetes) from Malaysia. Int J Med doi:10.1002/ana.24310.
Mushrooms 2013;15(6):539–554. doi:10.1615/
111 Singleton JR, Smith AG, Marcus RL. Exercise as
intjmedmushr.v15.i6.30.
therapy for diabetic and prediabetic neuropathy.
100 Liu PS, Chueh SH, Chen CC, et al. Lion’s mane Curr Diab Rep 2015;15(12):120. doi:10.1007/s11892-
medicinal mushroom Hericium erinaceus 015-0682-6.
(Agaricomycetes), modulates purinoceptor-
112 Kluding PM, Bareiss SK, Hastings M, et al. Physical
coupled calcium signaling and murine
training and activity in people with diabetic
nociceptive behavior. Int J Med Mushrooms
peripheral neuropathy: paradigm shift. Phys
2017;19(6):499–507. doi:10.1615/
Ther 2017;97(1):31–43. doi:10.2522/ptj.20160124.
IntJMedMushrooms.v19.i6.20.
113 Balducci S, Iacobellis G, Parisi L, et al. Exercise
101 Unda SR, Villegas EA, Toledo ME, et al. Beneficial
training can modify the natural history of
effects of fish oil enriched in omega-3 fatty
diabetic peripheral neuropathy. J Diabetes
acids on the development and maintenance of
Complications 2006;20(4):216–223. doi:10.1016/
neuropathic pain. J Pharm Pharmacol 2020;72(3):
j.jdiacomp.2005.07.005.
437–447. doi:10.1111/jphp.13213.
114 Alsubiheen A, Petrofsky J, Daher N, et al. Effect
102 Yorek MA. Is fish oil a potential treatment for
of Tai Chi exercise combined with mental
diabetic peripheral neuropathy? Curr Diabetes
imagery theory in improving balance in a diabetic
Rev 2018;14(4):339–349. doi:10.2174/
and elderly population. Med Sci Monit 2015;21:
1573399813666170522155327.
3054–3061. doi:10.12659/MSM.894243.
103 Hooten WM. Chronic pain and mental health
115 Mooventhan A, Nivethitha L. Evidence based
disorders: shared neural mechanisms,
effects of yoga in neurological disorders. J Clin
epidemiology, and treatment. Mayo Clin Proc
Neurosci 2017;43:61–67. doi:10.1016/j.
2016;91(7):955–970. doi:10.1016/j.mayocp.2016.
jocn.2017.05.012.
04.029.
116 de Vos CC, Meier K, Zaalberg PB, et al. Spinal
104 Townsend CO, Bruce BK, Hooten WM, Rome JD.
cord stimulation in patients with painful diabetic
The role of mental health professionals in
neuropathy: a multicentre randomized clinical
multidisciplinary pain rehabilitation programs.
trial. Pain 2014;155(11):2426–2431. doi:10.1016/j.
J Clin Psychol 2006;62(11):1433–1443. doi:10.1002/
pain.2014.08.031.
jclp.20322.
117 Slangen R, Schaper NC, Faber CG, et al. Spinal
105 Ambrose KR, Golightly YM. Physical exercise as
cord stimulation and pain relief in painful
non-pharmacological treatment of chronic pain:
diabetic peripheral neuropathy: a prospective
why and when. Best Pract Res Clin Rheumatol
two-center randomized controlled trial.
2015;29(1):120–130. doi:10.1016/j.berh.2015.04.022.
Diabetes Care 2014;37(11):3016–3024.
doi:10.2337/dc14-0684.
CONTINUUMJOURNAL.COM 1321
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MANAGEMENT OF NEUROPATHIC PAIN IN POLYNEUROPATHY
118 van Beek M, Slangen R, Schaper NC, et al. 124 Lu Z, Moody J, Marx BL, Hammerstrom T.
Sustained treatment effect of spinal cord Treatment of chemotherapy-induced
stimulation in painful diabetic peripheral peripheral neuropathy in integrative oncology: a
neuropathy: 24-month follow-up of a survey of acupuncture and oriental medicine
prospective two-center randomized practitioners. J Altern Complement Med 2017;
controlled trial. Diabetes Care 2015;38(9): 23(12):964–970. doi:10.1089/acm.2017.0052.
e132–e134. doi:10.2337/dc15-0740.
125 Rowin J. Integrative neuromuscular medicine:
119 Slangen R, Faber CG, Schaper NC, et al. A trial- neuropathy and neuropathic pain: consider the
based economic evaluation comparing spinal alternatives. Muscle Nerve 2019;60(2):124–136.
cord stimulation with best medical treatment in doi:10.1002/mus.26510.
painful diabetic peripheral neuropathy. J Pain
126 Baute V, Zelnik D, Curtis J, Sadeghifar F.
2017;18(4):405–414. doi:10.1016/j.jpain.2016.11.014.
Complementary and alternative medicine for
120 Mekhail N, Visnjevac O, Azer G, et al. Spinal cord painful peripheral neuropathy. Curr Treat
stimulation 50 years later: clinical outcomes of Options Neurol 2019;21(9):44. doi:10.1007/
spinal cord stimulation based on randomized s11940-019-0584-z.
clinical trials-a systematic review. Reg Anesth
127 Bates D, Schultheis BC, Hanes MC, et al. A
Pain Med 2018;43(4):391–406. doi:10.1097/
comprehensive algorithm for management of
AAP.0000000000000744.
neuropathic pain. Pain Med 2019;20(suppl 1):
121 Lai HC, Lin YW, Hsieh CL. Acupuncture- S2–S12. doi:10.1093/pm/pnz075.
analgesia-mediated alleviation of central
128 Akın S, Bölük C, Türk Börü Ü, et al. Restless legs
sensitization. Evid Based Complement Alternat
syndrome in type 2 diabetes mellitus. Prim
Med 2019;2019:6173412. doi:10.1155/2019/6173412.
Care Diabetes 2019;13(1):87–91. doi:10.1016/j.
122 Kumar R, Mooventhan A, Manjunath NK. pcd.2018.08.006.
Immediate effect of needling at CV-12
129 Bastia JK, Bhoi SK, Kalita J, Misra UK. Neuropathy
(Zhongwan) acupuncture point on blood
in a cohort of restless leg syndrome patients.
glucose level in patients with type 2 diabetes
J Clin Neurosci 2015;22(8):1314–1318. doi:10.1016/
mellitus: a pilot randomized placebo-controlled
j.jocn.2015.01.032.
trial. J Acupunct Meridian Stud 2017;10(4):
240–244. doi:10.1016/j.jams.2017.06.003.
123 Ju ZY, Wang K, Cui HS, et al. Acupuncture for
neuropathic pain in adults. Cochrane Database
Syst Rev 2017;12:CD012057. doi:10.1002/
14651858.CD012057.pub2.
1322 OCTOBER 2020
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
You might also like
- Field Guide To Functional NutritionDocument71 pagesField Guide To Functional NutritionMeri100% (3)
- Referral Letter To Specialist From Admitted PatientDocument52 pagesReferral Letter To Specialist From Admitted PatientyazzNo ratings yet
- The Metamorphica RevisedDocument270 pagesThe Metamorphica RevisedStewart WyattNo ratings yet
- Resolving Attachment Injuries in Couples Using Emotionally Focused Therapy: A Three-Year Follow-UpDocument18 pagesResolving Attachment Injuries in Couples Using Emotionally Focused Therapy: A Three-Year Follow-UpEFTcouplesNo ratings yet
- Pain Management in Infants - Children - AdolescentsDocument9 pagesPain Management in Infants - Children - AdolescentsOxana Turcu100% (1)
- Management of Chronic Pain in The Elderly 2018Document8 pagesManagement of Chronic Pain in The Elderly 2018Dara Agusti MaulidyaNo ratings yet
- Differentiating Trigeminal Neuropathy From Trigeminal NeuralgiaDocument11 pagesDifferentiating Trigeminal Neuropathy From Trigeminal NeuralgiaGarryNo ratings yet
- The Alexander Technique For Musicians (Judith Kleinman, Peter Buckoke) PDFDocument284 pagesThe Alexander Technique For Musicians (Judith Kleinman, Peter Buckoke) PDFKamo MarabaNo ratings yet
- Traction - Active Care Physiotherapy Clinic PDFDocument13 pagesTraction - Active Care Physiotherapy Clinic PDFMuhammad ZaibNo ratings yet
- p2018b3 SampleDocument21 pagesp2018b3 SampleAhmad FahroziNo ratings yet
- The Primary Care of Seizure Disorders: A Practical Guide to the Evaluation and Comprehensive Management of Seizure DisordersFrom EverandThe Primary Care of Seizure Disorders: A Practical Guide to the Evaluation and Comprehensive Management of Seizure DisordersNo ratings yet
- Treatment of PatientsWith PsychogenicDocument2 pagesTreatment of PatientsWith PsychogenicSergio MouraNo ratings yet
- Peripheral NeuropathyDocument14 pagesPeripheral Neuropathygeofrey burtonNo ratings yet
- Acupuncture: Halos, Heredia, Herejias, HicarteDocument45 pagesAcupuncture: Halos, Heredia, Herejias, Hicarteshelbyheredia0% (1)
- Drug-Induced Peripheral Neuropathy, A Narrative ReviewDocument11 pagesDrug-Induced Peripheral Neuropathy, A Narrative ReviewMaksum Muh MaksumNo ratings yet
- Assessment of Neuropathic Pain in Primary Care: Supplement IssueDocument9 pagesAssessment of Neuropathic Pain in Primary Care: Supplement IssueRodrigo JimenezNo ratings yet
- HeritageDocument116 pagesHeritageVarshaNo ratings yet
- Neurostimulation For Neuropathic Pain: Outcomes and New ParadigmsDocument8 pagesNeurostimulation For Neuropathic Pain: Outcomes and New Paradigmssenad becarevicNo ratings yet
- Perfect Tens ManualDocument17 pagesPerfect Tens ManualBea100% (1)
- Neuropathic PainDocument19 pagesNeuropathic PainBush HsiehNo ratings yet
- Diabetic Neuropathies. 2023Document17 pagesDiabetic Neuropathies. 2023Arbey Aponte PuertoNo ratings yet
- Perineural Adjuncts For Peripheral Nerve BlockDocument7 pagesPerineural Adjuncts For Peripheral Nerve BlockpitriaNo ratings yet
- Ultramicronized Palmitoylethanolamide in Spinal Cord Injury Neuropathic Pain A Randomized Double-Blind Placebo-Conttolled TrialDocument7 pagesUltramicronized Palmitoylethanolamide in Spinal Cord Injury Neuropathic Pain A Randomized Double-Blind Placebo-Conttolled TrialKershaun MathewNo ratings yet
- Neuropatia DiabeticaDocument9 pagesNeuropatia DiabeticalucianaNo ratings yet
- Treatment of Neuropathic Pain An Overview of RecentDocument11 pagesTreatment of Neuropathic Pain An Overview of RecentIvette Silva FigueroaNo ratings yet
- Introduction: Recommendations For The Diagnosis, Assessment, and Treatment of Neuropathic PainDocument2 pagesIntroduction: Recommendations For The Diagnosis, Assessment, and Treatment of Neuropathic PainFran WermannNo ratings yet
- NIH Public Access: Effect of Sedation On Pain PerceptionDocument21 pagesNIH Public Access: Effect of Sedation On Pain PerceptionAgustina ZairidaNo ratings yet
- Advances in Neuropathic Pain: Diagnosis, Mechanisms, and Treatment RecommendationsDocument11 pagesAdvances in Neuropathic Pain: Diagnosis, Mechanisms, and Treatment Recommendationsgamesh waran gantaNo ratings yet
- AnnIMedUpdate in Palliative Med Jan2008Document7 pagesAnnIMedUpdate in Palliative Med Jan2008vabcunhaNo ratings yet
- NMSPostgrad Med J 2008 Jackson 121 6Document7 pagesNMSPostgrad Med J 2008 Jackson 121 6afeda_886608No ratings yet
- Peripheral NeuropathyDocument36 pagesPeripheral NeuropathySantiago HerreraNo ratings yet
- Evidence-Based Guideline: Treatment of Painful Diabetic NeuropathyDocument11 pagesEvidence-Based Guideline: Treatment of Painful Diabetic NeuropathyTriNo ratings yet
- Diabetic Peripheral NeuropathyDocument15 pagesDiabetic Peripheral NeuropathyValerie hongNo ratings yet
- Nonopioid, Multimodal Analgesia As First-Line Therapy After Otolaryngology Operations: Primer On Nonsteroidal Anti-Inflammatory Drugs (Nsaids)Document8 pagesNonopioid, Multimodal Analgesia As First-Line Therapy After Otolaryngology Operations: Primer On Nonsteroidal Anti-Inflammatory Drugs (Nsaids)MUHAMMAD ANWARNo ratings yet
- NCCN Task Force Report: Management of Neuropathy in Cancer: Key WordsDocument26 pagesNCCN Task Force Report: Management of Neuropathy in Cancer: Key WordsJIMENA GUADALUPE PADILLA BONILLANo ratings yet
- Opioid-Free Anaesthesia - Atow-461-00 - BDocument6 pagesOpioid-Free Anaesthesia - Atow-461-00 - BEugenio Martinez HurtadoNo ratings yet
- Diabetic Neuropathy: What Does The Future Hold?Document7 pagesDiabetic Neuropathy: What Does The Future Hold?O. floriceNo ratings yet
- An Option Overview: Neuropathic PainDocument3 pagesAn Option Overview: Neuropathic PainAndi Tri SutrisnoNo ratings yet
- Anti Nyeri Saraf The Pharmacological TherapyDocument12 pagesAnti Nyeri Saraf The Pharmacological TherapyTiara Renita LestariNo ratings yet
- Santos 2020Document9 pagesSantos 2020Riko RIKNo ratings yet
- Understanding Peripheral Neuropathic Pain in Primary Care: Diagnosis and ManagementDocument7 pagesUnderstanding Peripheral Neuropathic Pain in Primary Care: Diagnosis and ManagementInês Beatriz Clemente CasinhasNo ratings yet
- 234 Neuropathic PainDocument10 pages234 Neuropathic PainDr. Anish GolchhaNo ratings yet
- Epilepsy 2Document12 pagesEpilepsy 2cacaNo ratings yet
- Town JournalDocument1 pageTown JournalDr. MazNo ratings yet
- Cannabis Based Medicines and Medical Cannabis For Chronic Neuropathic PainDocument14 pagesCannabis Based Medicines and Medical Cannabis For Chronic Neuropathic PainRocio BeteluNo ratings yet
- MDZ e DispnéiaDocument10 pagesMDZ e DispnéiaThaísa NogueiraNo ratings yet
- Schembri2019 Article AreOpioidsEffectiveInRelievingDocument17 pagesSchembri2019 Article AreOpioidsEffectiveInRelievingSheila ZivanaNo ratings yet
- 15-Kip Aaanalgesia Under AnaesthesiaDocument13 pages15-Kip Aaanalgesia Under AnaesthesiagospelcorpNo ratings yet
- Investigatory Project On AnalgesicsDocument30 pagesInvestigatory Project On AnalgesicsAnurag Singh100% (1)
- MR - Hellp SyndromDocument21 pagesMR - Hellp SyndromDara Agusti MaulidyaNo ratings yet
- Neuropathic Pain ThesisDocument7 pagesNeuropathic Pain Thesisafcnomlaq100% (2)
- Anestesia 1Document22 pagesAnestesia 1Carlos MNo ratings yet
- A Step Closer in The Management of Uncontrolled Neuropathic Pain: Gabapentin-Nortriptyline CombinationDocument6 pagesA Step Closer in The Management of Uncontrolled Neuropathic Pain: Gabapentin-Nortriptyline CombinationM AbhiNo ratings yet
- Millimeter Wave Treatment of Diabetic Sensorymotor Polyneuropathy1Document6 pagesMillimeter Wave Treatment of Diabetic Sensorymotor Polyneuropathy1olgaremonNo ratings yet
- Pain Management in ChildrenDocument9 pagesPain Management in ChildrenNASLY YERALDINE ZAPATA CATAÑONo ratings yet
- Nyeri NeuropatikDocument7 pagesNyeri NeuropatikStephanie AureliaNo ratings yet
- Usos de La Amitriptilina y Gabapantina en Neuropatia DiabeticaDocument15 pagesUsos de La Amitriptilina y Gabapantina en Neuropatia Diabeticaberenice laraNo ratings yet
- ChoosePT - Electrotherapy, Effective Alternative For Opioid Reduction? (PDFDrive)Document118 pagesChoosePT - Electrotherapy, Effective Alternative For Opioid Reduction? (PDFDrive)kk2483697No ratings yet
- Neuropathy-In-Diabetes 2015 MedicineDocument7 pagesNeuropathy-In-Diabetes 2015 MedicineKaterinee Masielly Flores BlandónNo ratings yet
- Acupuncture - MeniereDocument4 pagesAcupuncture - MeniereTinnitus Man IndonesiaNo ratings yet
- Pain MNG in KidneyDocument8 pagesPain MNG in KidneyWaqar GhoryNo ratings yet
- Neuropathies: Essential Oils Show Promising Results in The Fight Against SymptomsDocument17 pagesNeuropathies: Essential Oils Show Promising Results in The Fight Against Symptomskcc2012No ratings yet
- End of Life Care: Presented by Pankaj Nurse Practitioner 2 Yr Moderator Dr. Sushant Khanduri Associate ProfessorDocument43 pagesEnd of Life Care: Presented by Pankaj Nurse Practitioner 2 Yr Moderator Dr. Sushant Khanduri Associate ProfessorQudrat Un NissaNo ratings yet
- Neuropathic Low Back Pain in Clinical PracticeDocument13 pagesNeuropathic Low Back Pain in Clinical PracticeGrace Febryanti TodingNo ratings yet
- Mechanisms of Acupuncture-Electroacupuncture On Persistent PainDocument38 pagesMechanisms of Acupuncture-Electroacupuncture On Persistent PainPaulo SantosNo ratings yet
- Guidelines in The Management of Diabetic Nerve Pain Clinical Utility of PregabalinDocument22 pagesGuidelines in The Management of Diabetic Nerve Pain Clinical Utility of PregabalinSuryana Marjuki0% (1)
- Parkinsonism Caused by Adverse Drug Reactions: A Case SeriesDocument3 pagesParkinsonism Caused by Adverse Drug Reactions: A Case SeriesFendi ManopeNo ratings yet
- Small Fiber Neuropathy and Related Syndromes: Pain and NeurodegenerationFrom EverandSmall Fiber Neuropathy and Related Syndromes: Pain and NeurodegenerationSung-Tsang HsiehNo ratings yet
- Peripheral Receptor Targets for Analgesia: Novel Approaches to Pain ManagementFrom EverandPeripheral Receptor Targets for Analgesia: Novel Approaches to Pain ManagementNo ratings yet
- Clinical Trial of Nitrosense® Patch For The Treatment of Patients With Painful Diabetic NeuropathyDocument6 pagesClinical Trial of Nitrosense® Patch For The Treatment of Patients With Painful Diabetic NeuropathyNayan ChaudhariNo ratings yet
- Protocol AkashDocument37 pagesProtocol AkashAkash KanojiaNo ratings yet
- Post-Op Instructions - Implant PlacementDocument2 pagesPost-Op Instructions - Implant PlacementPande NandaNo ratings yet
- NCP Pain - OBDocument5 pagesNCP Pain - OBSandra Guimaray50% (2)
- Table of ContentsDocument8 pagesTable of ContentsEmmanuel BeresoNo ratings yet
- Fulltext 1 To 33Document135 pagesFulltext 1 To 33RAY RAMIREZNo ratings yet
- Ahad PSY101 Lab ReportDocument10 pagesAhad PSY101 Lab ReportAbdullah Al AhadNo ratings yet
- Cruelty's Rewards - The Gratifications of Perpetrators and Spectators Victor NellDocument48 pagesCruelty's Rewards - The Gratifications of Perpetrators and Spectators Victor NellTernassNo ratings yet
- Nursing Care Plan: Jovel E. Cortez 2 Year Olfu Val 11BDocument9 pagesNursing Care Plan: Jovel E. Cortez 2 Year Olfu Val 11BJovel CortezNo ratings yet
- Presentation Lower Back PainDocument86 pagesPresentation Lower Back PainSten SchaperNo ratings yet
- Shouder InjuryDocument120 pagesShouder Injuryfairus_fz821575No ratings yet
- Axinerve NP MonographDocument12 pagesAxinerve NP MonographShama Safiana100% (1)
- Clinical and Diagnostic Imaging Findings in Police Working Dogs Referred For Hip OsteoarthritisDocument11 pagesClinical and Diagnostic Imaging Findings in Police Working Dogs Referred For Hip OsteoarthritisEquilibrium EduardoNo ratings yet
- MorphineDocument3 pagesMorphineAizat KamalNo ratings yet
- Stress Management: Presented by:-RISHI SHAH B.Tech CS 2 Year B244Document8 pagesStress Management: Presented by:-RISHI SHAH B.Tech CS 2 Year B244Rishi ShahNo ratings yet
- CHCCCS023 Support Independence and Wellbeing: Learner WorkbookDocument48 pagesCHCCCS023 Support Independence and Wellbeing: Learner WorkbookZafirah BukshNo ratings yet
- Bioptron Pro 1Document2 pagesBioptron Pro 1sabboubehNo ratings yet
- Weekly Patient Care Worksheet0Document4 pagesWeekly Patient Care Worksheet0mitchelltaiwo007No ratings yet
- Transcutaneous Electrical Nerve Stimulation: Mechanisms, Clinical Application and EvidenceDocument5 pagesTranscutaneous Electrical Nerve Stimulation: Mechanisms, Clinical Application and EvidenceLuis Alvarez MoralesNo ratings yet
- Assessmen T Nursing Diagnosi S Nursing Goal Nursing Intervention Rationale Subjective Cues: Independent IndependentDocument3 pagesAssessmen T Nursing Diagnosi S Nursing Goal Nursing Intervention Rationale Subjective Cues: Independent IndependentKim Glaidyl BontuyanNo ratings yet