Professional Documents
Culture Documents
Hypercalcemia in Dogs Emergent Care Diagnostics and Treatments
Uploaded by
tarilubis277Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hypercalcemia in Dogs Emergent Care Diagnostics and Treatments
Uploaded by
tarilubis277Copyright:
Available Formats
FEATURES • PEER REVIEWED
Beatriz Vera/shutterstock.com
Abstract
Hypercalcemia (an elevated level of calcium in the blood) in dogs is a relatively uncommon electrolyte abnormality
that can affect multiple body systems. The most common pathologic causes of hypercalcemia are malignancy and
hyperparathyroidism. Comprehensive diagnostics must be carried out to reach a concrete diagnosis, which will allow
for appropriate treatment options to be pursued. Treatment of the underlying cause is necessary to obtain resolution
of the hypercalcemia. While waiting on diagnostic results, supportive treatments can be provided to lower calcium
levels until a long-term solution can be found. Treatment options include fluid diuresis, steroids, bisphosphonates, and
other pharmacologic compounds. Surgery and/or chemotherapy may be necessary if a neoplastic process is
discovered. By combining diagnostic results and appropriate treatment modalities, resolution of hypercalcemia can be
obtained in most cases.
56 • SUMMER 2023 • todaysveterinarynurse.com
PEER REVIEWED • FEATURES
INTERNAL MEDICINE
Hypercalcemia in Dogs:
Emergent Care,
Diagnostics, and
Treatments
Brooke Quesnell, BS, CVT, VTS (IM-Oncology)
WestVet Emergency and Specialty Center, Kuna, Idaho
H
ypercalcemia is a relatively uncommon clotting, vasodilation, vasoconstriction, and bone
electrolyte abnormality from a disease production and stability.
process or external influence leading to
excess calcium in the body. The most common There are 2 primary ways to measure calcium: total
pathologic cause of hypercalcemia in dogs is and ionized. Total reflects all calcium within the
neoplasia; 60% of dogs with hypercalcemia are body, while ionized reflects the biologically active
diagnosed with cancer.1 Abnormal calcium levels calcium levels. When only total calcium levels are
can lead to severe disturbances in normal body used, hypercalcemia can be overestimated while
functions as calcium is a key component in hypocalcemia can be underestimated. When
neuromuscular transmission, enzyme function, calcium levels in a patient are being evaluated,
Take-Home Points
z Calcium homeostasis is of vital adenocarcinoma being the most z Comprehensive and complete
importance to maintain normal common culprits. diagnostics are key to diagnosing
physiologic function of many the underlying cause of
body systems. z The extent of initial treatment is hypercalcemia.
largely based on the severity of
z HARDIONS is an acronym for clinical signs and often includes z The hypercalcemia of
remembering the most common fluid diuresis, diuretics, and malignancy panel is an important
causes of hypercalcemia. steroids. diagnostic tool in differentiating
hypercalcemia of malignancy and
z The most common pathologic z Without treating the hyperparathyroidism.
cause of hypercalcemia is underlying cause, resolution of
malignancy, with lymphoma hypercalcemia cannot occur.
and apocrine gland anal sac
todaysveterinarynurse.com • SUMMER 2023 • 57
FEATURES • PEER REVIEWED
ionized calcium is the more accurate value used to calcium level. PTH increases plasma calcium levels via
initially diagnose and monitor hypercalcemia. 3 mechanisms: utilizing bone stores of calcium via
resorption, increasing renal tubule calcium
reabsorption, and increasing the synthesis of calcitriol
NORMAL CALCIUM REGULATION in the kidneys.
Calcium regulation is maintained by 3 main substances
within the body: calcitriol, parathyroid hormone The parathyroid gland will adjust its PTH production,
(PTH), and calcitonin (FIGURE 1). with PTH and calcitriol inhibiting further secretion of
PTH. When excess calcium levels are detected by the
The body acquires much of its calcium from vitamin D parathyroid gland, calcitonin production is increased in
obtained by ultraviolet light exposure or by consuming the thyroid gland, which inhibits osteoclast activity and
foods or supplements containing vitamin D. Once bone resorption, thereby helping to stabilize calcium
vitamin D has entered the body, it is converted in the levels in normal dogs.
liver to 1,25-dihydroxyvitamin D. This precursor (an
inactive substance that is converted to an active However, in dogs with a disease process in which this
substance) is then processed by the kidney and cycle is affected or circumvented (such as cancer),
converted into calcitriol. Calcitriol is released into the excess calcium production continues regardless of the
bloodstream and helps to increase intestinal calcium normal negative feedback loop in the calcium cycle.
absorption and supports both bone and kidney calcium
reabsorption.
CAUSES OF HYPERCALCEMIA
Calcium levels in the body are further regulated by the HARDIONS is an effective mnemonic device to
parathyroid gland. The parathyroid gland produces remember common causes of hypercalcemia2:
PTH, whose primary role is maintaining a homeostatic
Thyroid glands: N.Vinoth Narasingam/shutterstock.com; Bone: Alexander_P/shutterstock.com
High blood Low blood
calcium level calcium level
Thyroid Parathyroids
Calcitonin Parathyroid
hormone
Buildup of bone Breakdown of bone
by osteoblasts by osteoclasts
Bone
contains
Ca++
Blood Blood
Ca++ level Ca++ level
decreases increases
Normal blood
calcium level
FIGURE 1. Regulation of blood calcium.
Ca++ = serum calcium
58 • SUMMER 2023 • todaysveterinarynurse.com
PEER REVIEWED • FEATURES
H = hyperparathyroidism, hypercalcemia of Primary hyperparathyroidism most commonly occurs
malignancy (HM), and humoral hypercalcemia of in older dogs around 7 years of age. Sex and breed
malignancy (HHM) predilection are not statistically relevant, with the
A = Addison’s disease (hypoadrenocorticism) exception of the keeshond, which has a hereditary form
R = Renal disease/failure of the disease.4
D = Vitamin D toxicity
I = Idiopathic (cats) Clinical signs of hyperparathyroidism coincide with
O = Osteolytic (osteomyelitis, hypertrophic general hypercalcemia signs but are often less severe or
osteodystrophy, disuse osteoporosis) nonexistent at the time of diagnosis. Evidence of
N = Neoplasia primary hyperparathyroidism is often an incidental
S = Spurious finding on routine lab work in older dogs.
Other uncommon causes of hypercalcemia include
excess intestinal phosphate binders, excessive calcium Hypoadrenocorticism
supplementation, hypervitaminosis A, milk-alkali Approximately one-third of dogs diagnosed with
syndrome, thiazide diuretics, acromegaly, hypoadrenocorticism are found to have mild
thyrotoxicosis, postrenal transplantation, and hypercalcemia. Multiple factors may influence this
aluminum exposure. finding, including increased calcium citrate,
hemoconcentration, increased renal resorption of
calcium, and increased affinity of serum proteins for
Hypercalcemia of Malignancy calcium. When the hypoadrenocorticism is treated and
In dogs, HM is most often associated with T-cell stable, the hypercalcemia resolves quickly.
lymphoma and anal gland adenocarcinoma. HM can
also occur with multiple myeloma, parathyroid tumors
(often benign), thymoma, melanoma, mammary Renal Disease/Failure
tumors, and others. HM is most commonly caused by Hypercalcemia can be an attributing cause or sign of
release of PTH-related peptide (PTHrP) from tumor renal failure. The association of hypercalcemia and
cells into circulation, referred to as HHM. Other renal failure almost always accompanies a primary
growth factors and cytokines released from cancer cells comorbidity, such as neoplasia, primary
can further contribute to and synergize the role of hyperparathyroidism, or vitamin D toxicity. Severe
PTHrP in HM. PTHrP can function just as PTH does hypercalcemia can contribute to acute renal failure.
in the calcium cycle by increasing osteoclast activity, Mild to moderate hypercalcemia may be a result of
resulting in bone resorption, and increasing renal chronic renal failure.1
tubule calcium reabsorption. HM can also occur more
directly due to osteolysis from bone tumors, releasing
excess calcium into circulation.1,3 Toxicity
Hypercalcemia secondary to toxicity can occur from
ingestion of calcium or vitamin D supplements,
Hyperparathyroidism cholecalciferol (vitamin D3)-containing rodenticides,
Primary hyperparathyroidism is another potential cause calcitriol, glycoside-containing plants, and intestinal
of hypercalcemia, although its incidence is less than phosphate binders. Treatments specific to the toxin can
that of malignant causes. Hyperparathyroidism results be instituted in addition to supportive treatments for
in the parathyroid glands producing and secreting too hypercalcemia.
much PTH, leading to excessive calcium recruitment
by the bones, kidneys, and intestines. This overzealous
production of PTH is caused by a nodule or nodules Idiopathic
within the parathyroid glands. These nodules are Unlike cats, in which idiopathic hypercalcemia is a
statistically benign, although malignant nodules are common diagnosis when hypercalcemia is discovered,
possible.1 idiopathic hypercalcemia is very rare in dogs.
todaysveterinarynurse.com • SUMMER 2023 • 59
FEATURES • PEER REVIEWED
PRESENTING CLINICAL SIGNS any evidence of neoplasia. If any evidence of neoplasia
OF HYPERCALCEMIA IN DOGS is discovered, additional diagnostics such as ultrasound-
Calcium is involved in many of the daily body guided fine-needle aspiration or biopsy should be
processes. When calcium is not properly regulated, it performed.
can cause a variety of clinical signs:
● Vomiting Aberrant calcium lab values can occur due to a
● Diarrhea nonfasted sample, the physiologic growth of young
● Polyuria animals, or lab error and for spurious reasons due to
● Polydipsia lipemia or detergent contamination of the sample,
● Anorexia hemoconcentration, hyperproteinemia,
● Muscle weakness hypoadrenocorticism, and exposure to drastically cold
● Twitching (muscle tremors) temperatures during transport.
● Seizures and cardiac arrhythmias (severe
hypercalcemia) The common diagnostics above are all appropriate
when testing for primary hyperparathyroidism. An
Commonly affected organs are the gastrointestinal additional test—an HM panel—can help differentiate
system, heart, kidneys, musculoskeletal system, and between a malignant cause and primary
central nervous system. hyperparathyroidism. The HM panel tests PTH,
ionized calcium, and PTHrP. An elevated PTH in
conjunction with hypercalcemia is indicative of
DIAGNOSTICS hyperparathyroidism. A low PTH and positive PTHrP
FOR HYPERCALCEMIA concentration is indicative of malignancy as PTHrP is
To investigate the source of hypercalcemia, a set of base not produced in measurable quantities in adult dogs,
diagnostics should be performed. A complete blood cell although a negative PTHrP can still occur with
count, comprehensive biochemical profile, and malignancy.
urinalysis should be run to evaluate for any other lab
work abnormalities, such as azotemia, that could give When hyperparathyroidism is suspected, an ultrasound
an indication of the root cause (TABLE 1).5 Given their of the thyroid and parathyroid glands is appropriate to
close connection to calcium levels, phosphorous levels evaluate for any evidence of nodules or masses. As
are an important part of lab work interpretation as well. previously mentioned, presence of a nodule is common
with primary hyperparathyroidism; these nodules are
Thoracic radiography and full abdominal most often benign.1
ultrasonography should be performed to evaluate for
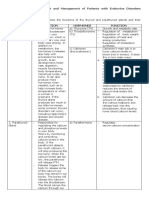
TABLE 1 Laboratory Abnormalities Commonly Associated With Causes of Hypercalcemiaa
IONIZED
DIAGNOSIS TOTAL CALCIUM PTH 1,25-DIHYDROXYVITAMIN D
CALCIUM
Primary
High High Normal to high Normal
hyperparathyroidism
Hypercalcemia of
High High Low to low-normal Low to normal
malignancy
Hypoadrenocorticism Low, normal, or high Normal Normal Normal
Chronic renal failure Low, normal, or high Normal to low Normal to high Low to normal
Low to normal;
Hypervitaminosis D High High Low to low-normal high with vitamin D 2
or D 3 toxicity
Granulomatous
High High Low to low-normal Low to normal
disease
a
Adapted from Peterson ME. Hypercalcemia in dogs and cats [professional version]. Merck Veterinary Manual. Modified October 2022. Accessed March 19,
2023. https://www.merckvetmanual.com/veterinary/endocrine-system/the-parathyroid-glands-and-disorders-of-calcium-metabolism/hypercalcemia-in-
dogs-and-cats#v54968773
PTH = parathyroid hormone; PTHrP = parathyroid hormone–related peptide
60 • SUMMER 2023 • todaysveterinarynurse.com
PEER REVIEWED • FEATURES
TREATMENT OF HYPERCALCEMIA Emergent Care
Treatment can depend on the severity of clinical signs. Emergent care for hypercalcemia may be necessary in
The most effective treatment for hypercalcemia is patients with total calcium levels >18 mg/dL and/or
addressing or removing the underlying cause. For ionized calcium levels >1.6 mmol/L in conjunction
example, in the case of HM, the tumor should be with severe clinical signs. Supportive treatment to
removed or treated with chemotherapy to alleviate the manage calcium levels will need to be started while the
hypercalcemia. Without these treatments, the root cause is diagnosed and treated.
hypercalcemia will persist unchecked. If the underlying
cause cannot be directly treated, such as tumors that are
not surgical, supportive treatments to combat the First-Line Treatments
hypercalcemia should be pursued. Fluid diuresis with 0.9% sodium chloride (NaCl) can
increase renal calcium loss. A fluid rate of 100 to
If neoplasia has been diagnosed as a probable cause of 125 mL/kg/day should improve glomerular filtration
hypercalcemia and surgery is an option, such as in the rate and sodium excretion, thereby decreasing calcium
case of apocrine gland anal sac adenocarcinoma, reabsorption. All crystalloids containing calcium should
surgical removal of the tumor is the gold standard be avoided.
treatment that will thus lower high calcium levels.
Diuretics can further increase renal calcium loss in
If primary hyperparathyroidism has been diagnosed, conjunction with fluid diuresis. Loop diuretics should
surgery or ethanol ablation of the parathyroid nodule(s) be used over thiazide diuretics, which are
should be pursued. Surgery is the preferred treatment; contraindicated in hypercalcemia because they decrease
however, in patients that are not good surgical renal excretion of calcium. Furosemide at 2 to 4 mg/kg
candidates or when the client is not willing to pursue or higher q8h to q12h will increase renal calcium
surgery, ablation can be an alternative treatment excretion.
option. The efficacy of ethanol ablation can vary
depending on the size of the nodule and skill/ Glucocorticoids can be very beneficial in the treatment
experience of the clinician performing the procedure of hypercalcemia when it is related to neoplasia. Their
but has been estimated at approximately 72%.6-8 use before a diagnosis of neoplasia can potentially
Complications that can occur include bark changes, inhibit obtaining a concrete diagnosis, especially in
coughing, dysphagia, hypersalivation, and laryngeal patients with probable lymphoma. Glucocorticoids
paralysis (if the laryngeal nerve is affected). When have lymphocytic properties, which can change the
treatment is successful, resolution of hypercalcemia can architecture of the lymph nodes, making cytologic or
occur within 3 days of the procedure. histopathologic diagnosis difficult. Falsely low PTHrP
concentrations can also occur secondary to steroid
administration, which can inhibit differentiating
between HM and primary hyperparathyroidism.
PHOSPHOROUS PTHrP Other agents that may be useful when first-line
treatments are suboptimal include bisphosphonates,
Normal to low Negative mithramycin, calcitonin, or calcimimetics.
Normal to low Positive (sometimes)
Normal to high Negative
Bisphosphonates
Bisphosphonates are a group of drugs used in both
High Negative
human and veterinary medicine to treat osteoporosis
and bone cancer and to mediate hypercalcemia.
Normal to high Negative
Bisphosphonates work by inhibiting osteoclast activity
in the bones by attaching to the osteoclast and
Normal to high Negative disrupting intracellular enzyme functions essential to
bone resorption. Bone resorption is the process of
breaking down bone, which leads to the release of
calcium into the bloodstream. By interrupting this
todaysveterinarynurse.com • SUMMER 2023 • 61
FEATURES • PEER REVIEWED
process, we can decrease excess calcium release while Calcitonin
also providing improved bone structure/stability and Calcitonin, a hormone produced by the thyroid gland,
pain control in patients with bone neoplasia. is an effective agent for decreasing calcium levels
rapidly. Calcitonin inhibits osteoclast activity in bone
Bisphosphonates can be administered intravenously or and renal reabsorption of calcium and phosphate,
orally. Bioavailability of oral bisphosphonates in dogs is thereby lowering calcium levels. These effects occur
poor in contrast to IV administration, but it can be a quickly but are short-lived due to resistance building
more attractive option for long-term treatment of up over 12 to 24 hours. Calcitonin is best used for
hypercalcemia in some cases. IV administration will not reducing calcium levels quickly in patients with severe
result in osteoclast inhibition for 24 to 48 hours hypercalcemia and severe clinical signs. Close
postinfusion; therefore, bisphosphonates are not an monitoring of ionized calcium levels is necessary as
initial treatment of choice in cases of acute hypocalcemia can occur. Other important values to
hypercalcemia with severe clinical signs. monitor include phosphorous, blood urea nitrogen,
creatinine, hydration status, and urine cast formation.
Bisphosphonates must be used cautiously or avoided
entirely in patients with renal disease as they can cause Calcitonin is an expensive medication and availability
nephrotoxicity. An additional side effect is mandibular can be inconsistent. Although calcitonin can decrease
osteonecrosis. Generalized skeletal pain for a few days calcium levels rapidly, it is not a sustainable decrease
after infusion is a common complaint from humans due to development of resistance; therefore, use of
receiving bisphosphonates; therefore, it is reasonable to calcitonin in veterinary medicine is limited and
surmise that dogs may experience similar effects. In the uncommon.7-9
author’s experience, some clients do report lethargy and
stiffness in their dogs for 2 to 3 days postinfusion.
Calcimimetics
Pamidronate was previously the most commonly used Calcimimetics are a newer class of drugs that reduce the
intravenous bisphosphonate for many years, but secretion of PTH and can suppress circulating PTH.
zoledronate has taken over due to its drastically Calcimimetics increase the sensitivity of calcium-
increased antiresorption properties and effectiveness, sensing receptors within the parathyroid gland, leading
along with a shorter administration time. Zoledronate to a decrease in PTH and total calcium levels. This can
is dosed at 0.1 to 0.2 mg/kg (not to exceed 4 mg/dog), be an effective treatment option for primary
diluted in 0.9% NaCl over 15 minutes.7 A shorter or hyperparathyroidism and to reduce calcium levels in
longer administration time can increase the risk of renal failure patients.
nephrotoxicity; therefore, it is vital to calculate the
administration rate to provide the full dose in exactly
15 minutes.6-8 SUMMARY
Calcium homeostasis in the body is of paramount
importance given the significant effects aberrations can
Mithramycin cause. Hypercalcemia in dogs can be caused by a variety
Mithramycin, an antibiotic with antineoplastic of disease processes influencing its severity and
properties and calcium-lowering activity, can be used as treatment options, including HM, primary
an emergent treatment choice to attempt to lower hyperparathyroidism, hypoadrenocorticism, renal
calcium levels quickly. Mithramycin has great potential failure, and toxicity. Use the acronym HARDIONS to
for hepatotoxicity, bone marrow toxicity, and renal remember the common causes. Careful consideration
toxicity based on its dosing; therefore, it should be used of diagnostic results in conjunction with severity of
judiciously and only after serum biochemical values clinical signs can guide short- and long-term treatment
have been evaluated. The calcium-lowering activity of options. It is important to always remember that
mithramycin is short-lived, making it useful for quickly treatment of the underlying disease process causing
lowering calcium levels, but not for maintaining hypercalcemia must be instituted to achieve resolution
normal calcium values over the long term. of clinical signs. TVN
62 • SUMMER 2023 • todaysveterinarynurse.com
References
1. Bailey DB. Paraneoplastic syndromes. In: Vail DM, Thamm DH, Liptak J,
eds. Withrow and MacEwen’s Small Animal Oncology. 6th ed. Elsevier;
2019:83-97.
2. Chew D. Hypercalcemia in dogs: approach to diagnosis and treatment.
Proceedings presented at: World Small Animal Veterinary Association
World Congress; August 8-11, 2001; Vancouver, British Columbia,
Canada. Accessed April 9, 2023. https://www.vin.com/apputil/
content/defaultadv1.aspx?id=3843801&pid=8708
3. Gröne A, Weckmann MT, Blomme EAG, Capen CC, Rosol TJ.
Dependence of humoral hypercalcemia of malignancy on parathyroid
hormone-related protein expression in the canine anal sac apocrine
gland adenocarcinoma (CAC-8) nude mouse model. Vet Pathol.
1998;35(5):344-351. doi:10.1177/030098589803500503
4. Goldstein RE, Atwater DZ, Cazolli DM, Goldstein O, Wade CM,
Lindblad-Toh K. Inheritance, mode of inheritance, and candidate genes
for primary hyperparathyroidism in Keeshonden. J Vet Intern Med.
2007;21(1):199-203. doi:10.1892/0891-6640(2007)21[199:imoiac]2.0. INTRODUCING AN ALL-NEW
co;2
VETFOLIO CERTIFICATE
5. Peterson ME. Hypercalcemia in dogs and cats [professional version].
Merck Veterinary Manual. Modified October 2022. Accessed March FOR MANAGERS
19, 2023. https://www.merckvetmanual.com/veterinary/endocrine-
system/the-parathyroid-glands-and-disorders-of-calcium-metabolism/
hypercalcemia-in-dogs-and-cats#v54968773
6. Rasor L, Pollard R, Feldman EC. Retrospective evaluation of three LEAD LIKE
A UNICORN
treatment methods for primary hyperparathyroidism in dogs. JAAHA.
2007;43(2):70-77. doi:10.5326/0430070
7. Supportive care for the cancer patient. In: Vail DM, Thamm DH, Liptak
J, eds. Withrow and MacEwen’s Small Animal Oncology. 6th ed.
Elsevier; 2019:286-319.
8. Berenson J, Hirschberg R. Safety and convenience of a 15-minute
infusion of zoledronic acid. The Oncologist. 2004;9(3):319-329. Are you a new manager?
doi:10.1634/theoncologist.9-3-319
Or do you aspire to be?
9. Daniels E, Sakakeeny C. Hypercalcemia: pathophysiology, clinical signs,
and emergent treatment. JAAHA. 2015;51(5):291-299. doi:10.5326/ This course is for you!
jaaha-ms-6297
Brooke Quesnell
Brooke has been a certified veterinary
technician for more than 13 years and a
veterinary technician specialist in oncology
for more than 5 years. She currently
works as the clinical education specialist COURSE LEADER: Amy Newfield
for WestVet Emergency and Specialty
Center (parent corporation, MedVet).
Brooke is passionate about educating
fellow veterinary nurses and clinical
Sign up for just $199 or get it free
team members, with a special interest in with a VetFolio subscription!
oncology and specialized procedures such
as electrochemotherapy and compassionate
client care. She regularly presents
continuing education courses on local
and national levels for various companies
and conferences, contributes to textbooks
relating to oncology, and writes articles for
veterinary journals.
You might also like
- Calcium Metabolism & Calcium Metabolism DisordersDocument45 pagesCalcium Metabolism & Calcium Metabolism Disorderstrisya arthaputriNo ratings yet
- 287 FullDocument4 pages287 FullRye CalderonNo ratings yet
- Hipercalcemia BJMDocument4 pagesHipercalcemia BJMPedroUribeNo ratings yet
- PTH Regulation and Hyperparathyroidism GuideDocument39 pagesPTH Regulation and Hyperparathyroidism GuideAris josuaNo ratings yet
- Hypercalcemia (F&e)Document3 pagesHypercalcemia (F&e)Sarah Grace CajucomNo ratings yet
- HypercalcemiaDocument12 pagesHypercalcemiaAnam MirNo ratings yet
- Hyperparathyroid Case Report: A Self TestingDocument16 pagesHyperparathyroid Case Report: A Self Testinghusna fauziahNo ratings yet
- Parathyroid DiseaseDocument10 pagesParathyroid Diseasemohammedghassan53No ratings yet
- Parathyroid Glands: Anatomy, Function and DisordersDocument28 pagesParathyroid Glands: Anatomy, Function and DisordersOmar Alruwaili100% (1)
- Groman 2012Document5 pagesGroman 2012EFRAIN CARDENAS MENDOZANo ratings yet
- Hormon Parathyroid: Dr. Nanang Miftah F, SPPDDocument13 pagesHormon Parathyroid: Dr. Nanang Miftah F, SPPDFitri Nur DiniNo ratings yet
- Parathyroid HormoneDocument120 pagesParathyroid HormoneLaura TapiaNo ratings yet
- Hypercalcemic Crisis: Reinhard ZieglerDocument7 pagesHypercalcemic Crisis: Reinhard ZieglerRo KohnNo ratings yet
- Bachelor of Science in Medical Laboratory Science: Clinical Chemistry 2Document8 pagesBachelor of Science in Medical Laboratory Science: Clinical Chemistry 2Rafael SaldivarNo ratings yet
- MacroMinerals: Calcium, Phosphorus, Potassium, Sodium, Chloride, and MagnesiumDocument9 pagesMacroMinerals: Calcium, Phosphorus, Potassium, Sodium, Chloride, and MagnesiumDerek AtienzaNo ratings yet
- Hypercalcemia Diet: A Beginner's 3-Week Guide to Managing High Calcium Disease through Nutrition, With Sample Recipes and a Meal PlanFrom EverandHypercalcemia Diet: A Beginner's 3-Week Guide to Managing High Calcium Disease through Nutrition, With Sample Recipes and a Meal PlanNo ratings yet
- Hypocalcemia: Dept of Nephrology PsriDocument40 pagesHypocalcemia: Dept of Nephrology Psriind78No ratings yet
- Calcium, Phosphate and Vitamin D MetabolismDocument25 pagesCalcium, Phosphate and Vitamin D MetabolismRendy LectusNo ratings yet
- Quizlet Hypercalcemia PDFDocument2 pagesQuizlet Hypercalcemia PDFmaangelamangampo.aringoNo ratings yet
- Share Market Report 6Document13 pagesShare Market Report 6Nithish DevadigaNo ratings yet
- Pediatric Endocrinology Part 2: Pediatrics 2Document8 pagesPediatric Endocrinology Part 2: Pediatrics 2sarguss14No ratings yet
- Parathormone, CalcitoninDocument14 pagesParathormone, CalcitoninIbrahimNo ratings yet
- Assessment and Management of Patients With Endocrine DisordersDocument8 pagesAssessment and Management of Patients With Endocrine DisordersaliNo ratings yet
- Parathyroid Hormone PDFDocument120 pagesParathyroid Hormone PDFLaura TapiaNo ratings yet
- Calcium Homeostasis HormonesDocument31 pagesCalcium Homeostasis HormonesNoval FebriNo ratings yet
- Parathyroid Gland: Clinical Chemistry - 3Document16 pagesParathyroid Gland: Clinical Chemistry - 3Mary Rose BarrigaNo ratings yet
- CalciumDocument77 pagesCalciumRhaffy RapaconNo ratings yet
- HypercalcemiaDocument2 pagesHypercalcemiaJulieNo ratings yet
- LEC 3 Parathyroid Gland DisordersDocument39 pagesLEC 3 Parathyroid Gland Disordersalhusien.abd2000No ratings yet
- Hypoparathyroidism: DR Ranganath N Professor Department of OrthopaedicsDocument33 pagesHypoparathyroidism: DR Ranganath N Professor Department of Orthopaedicsnandhana s nairNo ratings yet
- Parathyroid Gland: Clinical Chemistry - 3Document12 pagesParathyroid Gland: Clinical Chemistry - 3Vincent ReyesNo ratings yet
- HypercalcemiaDocument39 pagesHypercalcemiaPrajina KansakarNo ratings yet
- Calcium Salts Calcitonin and CA RegulatorsDocument40 pagesCalcium Salts Calcitonin and CA RegulatorsSudhakar LakavathNo ratings yet
- HypoparathyroidismDocument28 pagesHypoparathyroidismRon Opulencia100% (2)
- Biochem 11Document5 pagesBiochem 11Abdullah RaufNo ratings yet
- Clinical Review: The Diagnosis and Management of HypercalcaemiaDocument9 pagesClinical Review: The Diagnosis and Management of HypercalcaemiaivanilhskyNo ratings yet
- CA A Cancer J Clinicians - 2018 - Zagzag - Hypercalcemia and Cancer Differential Diagnosis and TreatmentDocument10 pagesCA A Cancer J Clinicians - 2018 - Zagzag - Hypercalcemia and Cancer Differential Diagnosis and TreatmentWilliam Perero RodríguezNo ratings yet
- Calcium-Phosphate Disorders ExplainedDocument52 pagesCalcium-Phosphate Disorders ExplainedAnish JoshiNo ratings yet
- Paratiroid Dan KalsiumDocument80 pagesParatiroid Dan KalsiumFebrina EvaNo ratings yet
- Deficiencia de Calcio en Perros y Gatos II (Ingles)Document19 pagesDeficiencia de Calcio en Perros y Gatos II (Ingles)Domenica ChoezNo ratings yet
- Activity 2 MetabsDocument10 pagesActivity 2 MetabsCalvin Keith YadaoNo ratings yet
- عرض تقديمي-3 1Document9 pagesعرض تقديمي-3 1ema22m0156No ratings yet
- Parathyroid DisordersDocument37 pagesParathyroid DisordersMannat ZaidiNo ratings yet
- A Simple Guide to Hyperparathyroidism, Treatment and Related DiseasesFrom EverandA Simple Guide to Hyperparathyroidism, Treatment and Related DiseasesNo ratings yet
- Men1, Gi Endo Cam304 2019 J.burgessDocument27 pagesMen1, Gi Endo Cam304 2019 J.burgessJeffrey XieNo ratings yet
- Calcium Homeostasis INFOODocument2 pagesCalcium Homeostasis INFOOMika Sophia GonzagaNo ratings yet
- Primary Hyperparathyroidism: Pathophysiology and Impact On BoneDocument4 pagesPrimary Hyperparathyroidism: Pathophysiology and Impact On BoneBilal HaddadaNo ratings yet
- Anaesthesia in Parathyroid Gland Disorders and Calcium MetabolismDocument25 pagesAnaesthesia in Parathyroid Gland Disorders and Calcium MetabolismAshiyan IrfanNo ratings yet
- Oncologic Emergencies Classification and TreatmentDocument41 pagesOncologic Emergencies Classification and Treatmentomad pendaftaranPPDS100% (2)
- Parathyroid: Calcium and Vitamin DDocument135 pagesParathyroid: Calcium and Vitamin DPhysiology by Dr RaghuveerNo ratings yet
- Hypercalcaemia in Primary CareDocument2 pagesHypercalcaemia in Primary CareShazwani KKTSNo ratings yet
- Hyperparathyroidism and HypoparathyroidismDocument44 pagesHyperparathyroidism and Hypoparathyroidismshweta singhNo ratings yet
- Calcium and Phosphate MetabolismDocument70 pagesCalcium and Phosphate MetabolismHariprasad L0% (1)
- 8 Endocrine Metabolic and Lipid Disorders - 2012 - Small Animal Clinical Diagnosis by Laboratory Methods Fifth EditionDocument35 pages8 Endocrine Metabolic and Lipid Disorders - 2012 - Small Animal Clinical Diagnosis by Laboratory Methods Fifth EditionNarvarte Hospital Veterinario de EspecialidadesNo ratings yet
- Calcium MetabolismDocument29 pagesCalcium MetabolismsnehaNo ratings yet
- Hypercalcemia Diagnosis and TreatmentDocument5 pagesHypercalcemia Diagnosis and Treatmentandrei_groza_2No ratings yet
- Calcium and PhosphorusDocument34 pagesCalcium and Phosphorus075 Keerthighaa SNo ratings yet
- HypocalcemiaDocument4 pagesHypocalcemiaJezreel BonaNo ratings yet
- Medical AbbreviationsDocument5 pagesMedical AbbreviationsReuelHengNo ratings yet
- Pakya ECG BasicsDocument5 pagesPakya ECG BasicsFrederick CokroNo ratings yet
- FMUSP Exchange Program Offers Global Clinical ExperienceDocument36 pagesFMUSP Exchange Program Offers Global Clinical ExperienceRBarrosoNo ratings yet
- Journal Reading Muhamad Fakhri PPDS JantungDocument24 pagesJournal Reading Muhamad Fakhri PPDS JantungLycka AkaishaNo ratings yet
- Pedia Notes Print2Document5 pagesPedia Notes Print2John Christopher LucesNo ratings yet
- Nursing Care Plan For MIDocument6 pagesNursing Care Plan For MIlouie roderosNo ratings yet
- Endovascular Treatment of Duplicated Inferior Vena Cava Compression From Retroperitoneal FibrosisDocument4 pagesEndovascular Treatment of Duplicated Inferior Vena Cava Compression From Retroperitoneal FibrosisNonaNo ratings yet
- Muscle and MovementDocument5 pagesMuscle and MovementRabiaNo ratings yet
- Drugs Acting On Blood and Blood Forming AgentsDocument29 pagesDrugs Acting On Blood and Blood Forming AgentsSri RamNo ratings yet
- Medicina 58 01115 v2Document21 pagesMedicina 58 01115 v2silmanuryanzila2705No ratings yet
- Atropine Injection, 2 MGDocument14 pagesAtropine Injection, 2 MGJake DavisNo ratings yet
- Modifiable and Non-Modifiable Risk Factors for Aortic AneurysmDocument5 pagesModifiable and Non-Modifiable Risk Factors for Aortic AneurysmJanine Gerunda100% (1)
- Approach To The Patient With AnemiaDocument37 pagesApproach To The Patient With AnemiaSumeet PratapNo ratings yet
- Chapter 22 Assessment of Cardiovascualr SysteamDocument36 pagesChapter 22 Assessment of Cardiovascualr Systeamسلطان محمد فوزي سلمانNo ratings yet
- Speaker: Maj YS Swapna Sudha Chair Person: Maj Swapna Dharmaji Moderator: Col S.SenguptaDocument33 pagesSpeaker: Maj YS Swapna Sudha Chair Person: Maj Swapna Dharmaji Moderator: Col S.SenguptaSudha Kiran100% (1)
- Chronicpankreatitis CopieDocument18 pagesChronicpankreatitis Copieomarelbihi8No ratings yet
- BIO2701 2023 Transport SystemDocument13 pagesBIO2701 2023 Transport SystemDorothy MayakaNo ratings yet
- RetinaDocument76 pagesRetinaSarahNo ratings yet
- Cholesterol CPDocument6 pagesCholesterol CPAstri AmaliaNo ratings yet
- The Cardiovascular System: Gerard Mark C. SantosDocument31 pagesThe Cardiovascular System: Gerard Mark C. SantosRamon T. De Vera100% (1)
- Budd Chiari Syndrome: by DR - Jino JustinDocument29 pagesBudd Chiari Syndrome: by DR - Jino JustinAjeet LohanaNo ratings yet
- Echocardiography for Pregnant Woman with Shortness of BreathDocument21 pagesEchocardiography for Pregnant Woman with Shortness of BreathChynthea ParamithaNo ratings yet
- Pivotmed Webinar - Dyspnea in Adult - Approach and Early Management by Dr. Irandi Putra P, PHD, SPP (K), FAPSRDocument36 pagesPivotmed Webinar - Dyspnea in Adult - Approach and Early Management by Dr. Irandi Putra P, PHD, SPP (K), FAPSRMochamad Fadel AuliaNo ratings yet
- Drugs Affecting Renin-Angiotensin SystemDocument36 pagesDrugs Affecting Renin-Angiotensin SystempradeephdNo ratings yet
- Outcomes and Strategies For Utilization of Brachial Acc - 2022 - Seminars in VasDocument10 pagesOutcomes and Strategies For Utilization of Brachial Acc - 2022 - Seminars in VasDiego RodriguesNo ratings yet
- Neurologic Disorders Associated With Mitral Valve ProlapseDocument6 pagesNeurologic Disorders Associated With Mitral Valve Prolapsegeorgiana_884431330No ratings yet
- MANNITOL Drug StudyDocument5 pagesMANNITOL Drug StudyAngela ReyesNo ratings yet
- Liu 2019Document5 pagesLiu 2019Amelia Kristin SimanjuntakNo ratings yet
- Med Surg Report Sheet Night Shift FINAL2Document2 pagesMed Surg Report Sheet Night Shift FINAL2Cindy Ann100% (1)
- Hypotension, Shock, Hemorrhage and IV Fluid ResuscitationDocument65 pagesHypotension, Shock, Hemorrhage and IV Fluid ResuscitationRidwan Hadinata SalimNo ratings yet