Professional Documents
Culture Documents
The Full Value of Immunisation Against Respiratory Syncytial Virus For Infants Younger Tha 1 Year
Uploaded by
luis sanchezOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Full Value of Immunisation Against Respiratory Syncytial Virus For Infants Younger Tha 1 Year
Uploaded by
luis sanchezCopyright:
Available Formats
Personal View
The full value of immunisation against respiratory syncytial
virus for infants younger than 1 year: effects beyond
prevention of acute respiratory illness
Daniel R Feikin, Ruth A Karron, Samir K Saha, Erin Sparrow, Padmini Srikantiah, Daniel M Weinberger, Heather J Zar
Respiratory syncytial virus (RSV) is a leading cause of severe respiratory illness and death among children worldwide, Lancet Infect Dis 2023
particularly in children younger than 6 months and in low-income and middle-income countries. Feasible and cost- Published Online
effective interventions to prevent RSV disease are not yet widely available, although two new products aimed at November 21, 2023
https://doi.org/10.1016/
preventing RSV disease—long-acting monoclonal antibodies and maternal vaccines—have been licensed within the
S1473-3099(23)00568-6
past 2 years. The primary target of these products is reduction of the substantial burden of RSV-associated acute lower
Department of Immunization,
respiratory tract infections (LRTI) in infants younger than 1 year. However, other important public health benefits Vaccines and Biologicals, World
might also accrue with the prevention of RSV-associated LRTI during the first year of life. Mounting evidence shows Health Organization, Geneva,
that preventing RSV-associated LRTI in infants younger than 1 year could prevent secondary pneumonia caused by Switzerland (D R Feikin MD,
E Sparrow DrPH); Department
other pathogens, reduce recurrent hospitalisations due to other respiratory diseases in later childhood, decrease all-
of International Health,
cause infant mortality, ameliorate the burden of respiratory diseases on health-care systems, reduce inappropriate Bloomberg School of Public
antibiotic use, and possibly improve lung health beyond infancy. We herein review current evidence and suggest Health, Johns Hopkins
approaches to better assess the magnitude of these potential secondary effects of RSV prevention, which, if proven University, Baltimore, MD, USA
(Prof R A Karron MD); Child
substantial, are likely to be relevant to policy makers in many countries as they consider the use of these new products.
Health Research Foundation,
Dhaka, Bangladesh
Introduction RSV vaccines or monoclonal antibodies suggest that the (S K Saha PhD); Bangladesh
Acute lower respiratory tract infections (LRTI) are a number of infants (or mothers, in the case of the RSV Shishu Hospital and Institute,
Dhaka, Bangladesh (S K Saha);
leading cause of mortality in children younger than maternal vaccine) needed to be immunised to prevent
Bill & Melinda Gates
5 years worldwide.1 Respiratory syncytial virus (RSV) is one severe case of RSV disease among infants is Foundation, Seattle, WA, USA
the most common cause of LRTI and contributes approximately 50–100, which compares favourably to (P Srikantiah MD); Department
substantially to LRTI mortality. In a US surveillance that of other childhood vaccines, such as rotavirus and of Epidemiology of Microbial
Diseases, Yale School of Public
study of children with community-acquired pneumonia pneumococcal conjugate vaccines.7–9,16
Health, New Haven, CT, USA
requiring hospitalisation, RSV was the most commonly The full benefits of immunisation to prevent RSV (D M Weinberger PhD);
diagnosed pathogen, detected in 37% of children disease in infants younger than 1 year on long-term child Department of Paediatrics &
younger than 5 years.2 In a large study of severe and very health and health-care systems that can be accrued by Child Health, Red Cross War
Memorial Children’s Hospital,
severe pneumonia in seven low-income and middle- preventing RSV disease in young children are, however, Cape Town, South Africa
income countries (LMICs), RSV had the greatest likely to go beyond RSV-associated LRTI (hereafter (Prof H J Zar PhD); SA-MRC Unit
aetiological fraction (31·1%) of all pathogens.3 A referred to as RSV-LRTI). The secondary benefits from on Child & Adolescent Health,
systematic analysis of disease burden of acute lower RSV prevention are more challenging to measure and University of Cape Town,
Cape Town, South Africa
respiratory infections estimated that 101 400 deaths in might take years to become manifest, but RSV prevention (Prof H J Zar)
children younger than 5 years in 2019 were attributable might ultimately contribute substantially to public health
Correspondence to:
to RSV, representing 2·0% of all global childhood value and cost-effectiveness of RSV vaccines and Daniel Feikin, Department of
deaths; 45% of these RSV deaths occurred in children monoclonal antibodies, and be crucial to inform Immunization, Vaccines and
younger than 6 months.4 In addition, RSV was estimated decisions by countries about whether and how to Biologicals, World Health
Organization, Geneva,
to cause, in 2019, 33 million episodes of LRTI in children introduce these products in the coming years. In this
Switzerland
younger than 5 years, 3·6 million of which required Personal View, we explore the evidence and potential feikind@who.int
hospitalisation.4 magnitude of the secondary benefits of preventing RSV
After decades of slow progress in preventing RSV disease on child health and health-care systems, as well
disease in children in their first year of life, clinical as describing future research needs to better define these
trials with newer agents,5–10 such as an anti-RSV effects. RSV also causes a substantial burden of disease
monoclonal antibody with extended half-life in older adults,17 and two vaccines are already licensed for
(nirsevimab), and a bivalent RSV prefusion F vaccine this population;18,19 however, prevention of RSV disease in
(known as RSV preF) for maternal immunisation have adults is beyond the scope of this paper.
yielded encouraging efficacy results and regulatory
authorities have evaluated and licensed these products Prevention of all-cause LRTI and bacterial
on the basis of their efficacy11–14 (table 1). Moreover, as pneumonia
RSV is prevalent as a leading cause of severe respiratory The burden of LRTI caused by RSV extends beyond those
disease in children younger than 5 years worldwide, the cases in which RSV is identified. RSV-associated LRTI is
vaccine-preventable burden of LRTI attributable to RSV likely to be underdiagnosed because clinical diagnostic
disease is expected to be high.15 Clinical trial results of testing for RSV is not routinely done in most
www.thelancet.com/infection Published online November 21, 2023 https://doi.org/10.1016/S1473-3099(23)00568-6 1
Personal View
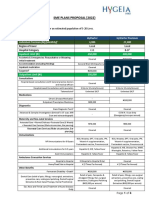
Product Product type Antigen RSV-associated LRTI Number of infants or All-cause LRTI Number of infants Regulatory
efficacy (95% CI) at mothers needed to efficacy (95% CI) at or mothers needed status
150 days immunise* to prevent 150 days to immunise* to
one RSV-associated LRTI prevent one all-
case through 150 days cause LRTI case
through 150 days
NCT02624947 RSV F protein Protein subunit RSV F protein, not For RSV MS-LRTI with For RSV MS-LRTI with For all-cause For all-cause Discontinued
(completed) nanoparticle vaccine stabilised in the severe hypoxemia†: severe hypoxemia: 167; MS-LRTI with severe MS-LRTI with severe
(Novavax) (administered to prefusion 48·3% (–1·0 to 73·5); for all RSV MS-LRTI: 111 hypoxemia: 39·0% hypoxemia: 67; for
pregnant women) conformation for all RSV (–13·0 to 57·3); for all-cause MS-LRTI:
MS-LRTI: 31·4% all-cause MS-LRTI: 44
(–1·3 to 53·6)9 20·6% (3·1 to 35·0)9
NCT04424316 RSV preF Protein subunit RSV F protein For severe RSV MA- For severe RSV-MA-LRTI: For severe all-cause For severe all-cause FDA approval
(completed) protein vaccine stabilised in the LRTI: 70·9% 89; for all RSV MA-LRTI, MA-LRTI: NA; for all- MA-LRTI: NA; for all- granted on
vaccine (administered to prefusion (44·5 to 85·9); for all 67 cause MA-LRTI: 5·2% cause MA-LRTI: 200 Aug 21, 202313
(Pfizer) pregnant women) conformation RSV MA-LRTI: 52·5% (–16·5 to 22·8%)7 and EMA
(28·7 to 68·9)7 approval
granted on
Aug 24, 202314
NCT03979313 Nirsevimab Monoclonal IgG extended half- For very severe RSV For very severe RSV MA- For very severe all- For very severe all- EMA approval
(completed) antibody life monoclonal MA-LRTI: 78·6% LRTI: 75; for LRTI requiring cause MA-LRTI: cause LRTI, NA; granted on
(administered to antibody directed (48·8 to 91·0); for hospitalisation: 65; for all NA; for all-cause for all-cause LRTI Oct 31, 202212
infant) against site 0 on F RSV-LRTI requiring RSV MA-LRTI: 24 LRTI requiring requiring and FDA
on RSV prefusion hospitalisation 76·8% hospitalisation: hospitalisation: 70; (biologics
F protein (49·4 to 89·4); for all 38·9% (6·3 to 60·2); for all-cause license)
RSV MA-LRTI: 76·4% for all-cause MA-LRTI: 19 granted on
(62·3 to 85·2)8 MA-LRTI: 38·2% July 17, 202311
(23·7 to 50·0)8
NCT04767373 Clesrovimab Monoclonal IgG extended half- Data pending Data pending Data pending Data pending Phase 2b/3
(ongoing) antibody life monoclonal trial ongoing
(administered to antibody directed
infant) against site IV on
RSV F protein10
EMA=European Medicines Agency. FDA=US Food and Drug Administration. LRTI=lower respiratory tract infections. MA-LRTI=medically attended lower respiratory infections (as defined in the clinical trial).
MS-LRTI=medically significant lower respiratory infections (as defined in the clinical trial). NA=not available. RSV=respiratory syncytial virus. *Number needed to immunise to avert one case was calculated as the
reciprocal of the difference in risk between the intervention group and the placebo group. The number needed to immunise accounts for product efficacy and incidence in the setting where the trial took place.
†Defined as a peripheral oxygen saturation of less than 92% at sea level.
Table 1: Completed or ongoing phase 3 trials of products showing efficacy against RSV-LRTI and all-cause LRTI in infants up to 5 months of age
health-care systems. In addition, RSV can synergistically of co-infection with other pathogens might have been
interact with other pathogens to cause LRTI, but is often reduced as a consequence of lower circulation of
overlooked because RSV is no longer detectable at the respiratory pathogens resulting from widespread non-
time of testing or its presence is deemed incidental. pharmaceutical interventions (eg, use of facial masks
Randomised controlled trials of effective preventive and physical distancing).20–23 Another trial of the bivalent
products might provide an opportunity to estimate the RSV prefusion F vaccine7 given to pregnant women
true disease burden attributable to RSV by comparing showed a small, non-significant reduction in all-cause
outcome rates in all-cause LRTI (not just LRTI caused by medically attended LRTI, which might be due to the
RSV) between vaccinated and placebo groups. When unusually low attributable fraction of RSV in all-cause
looking at the rate reduction caused by vaccination, as LRTI (22%) during the trial, which was conducted during
indicated by the number needed to immunise, the study the COVID-19 pandemic.
of the RSV F protein nanoparticle maternal vaccine Disruptions related to the COVID-19 pandemic
(NCT02624947) showed more than twice as a high provided another opportunity to probe the attributable
disease prevention capacity against all-cause LRTI than burden of RSV in all-cause LRTI. RSV, along with several
against RSV-associated LRTI outcomes.9 In contrast, the other respiratory viruses, largely disappeared for over a
randomised controlled trial of nirsevimab (NCT03979313) year, starting in March, 2020, due to the extensive
showed a similar number needed to immunise for all- implementation of non-pharmaceutical interventions to
cause and RSV-associated LRTI outcomes.8 The prevent the spread of SARS-CoV-2.21 The viruses then
difference in the results from these randomised reappeared, but often during the spring and summer
controlled trials might be related to more complete rather than during the typical autumn and winter
diagnosis of RSV cases in the nirsevimab trial, and it epidemic period.24,25 In a study in Israel, an estimate
might also be due to the fact that the nirsevimab trial based on the timing and intensity of these patterns
took place during the COVID-19 pandemic, when rates suggested that 49% of radiologically confirmed alveolar
2 www.thelancet.com/infection Published online November 21, 2023 https://doi.org/10.1016/S1473-3099(23)00568-6
Personal View
pneumonia in children younger than 5 years was deaths in this age group worldwide, or 3·6% (3·0–4·4)
associated with RSV, along with 21% of other types of after exclusion of the first week of life, when birth-related
LRTI.22 In addition, 18% of cases of bacteraemic deaths predominate.4 With the more permissive and less
pneumococcal pneumonia were estimated to be linked to specific metric of RSV detection among deceased
a preceding RSV infection, whereas no association was children younger than 6 months, RSV-associated
found between RSV infection and non-pneumonia mortality in these children was estimated at 102 000 deaths
invasive pneumococcal disease.22 In France, during the (uncertainty range 88 800–118 800), which might reflect
COVID-19 pandemic, a 63% decrease in invasive the under-recognised contribution of RSV to infant
pneumococcal disease was observed among children deaths.4
younger than 15 years; modelling suggested that a The updated RSV global mortality estimates incor
decline in RSV cases probably contributed 40% (95% CI porate new data from community mortality studies in
15–65) of this decrease.23 Similar results were found in Zambia, India, Pakistan, and Argentina, where naso
Canada, where a resurgence of RSV was estimated to pharyngeal swabs were obtained from deceased infants
contribute to 77% (95% CI 33–100) of the post-pandemic within 48 hours of death to test for presence of RSV.33
rebound of invasive pneumococcal disease in late 2021.26 Those studies showed that a high proportion of mortality
In contrast, in South Africa, where hospitalisation rates in children younger than 5 years occurs in the
for both RSV and invasive pneumococcal disease community rather than in the hospital, and that deaths
approximately halved during the peak of the pandemic in the community accounted for more than 70% of all
compared with pre-pandemic rates, RSV rates rebounded deaths in the lowest income settings in Zambia and
in 2022 while invasive pneumococcal disease rates did India (although the Indian setting was a low-income
not, suggesting that the relationship between the two rural community that was not representative of most of
pathogens might be less direct and involve other factors India). The studies further uncovered a sizable,
in some settings.20 previously unmeasured presence of RSV among these
The use of pneumococcal conjugate vaccines also deaths in the community setting, accounting for 4–27%
provided an opportunity to better understand the effects of all deaths among children younger than 6 months—
of RSV co-infections on acute LRTI. In a randomised findings that supported the use of all-cause deaths,
controlled trial of a nine-valent pneumococcal conjugate rather than just respiratory deaths, as the denominator
vaccine, South African children who received a for the revised RSV global burden calculations. A
pneumococcal conjugate vaccine had a non-significant limitation of these community mortality studies was that
lower rate (22% lower [95% CI –3 to 41]) of RSV-associated a causal link between detection of RSV and its role in the
pneumonia than did those who received a placebo; child’s death was not evaluated.
among HIV-negative children, the rate was 32% lower The global mortality estimates also incorporated data
(95% CI 6 to 50)]).27 This finding is in agreement with from the Child Health and Mortality Prevention For the Child Health and
observational studies; reductions in the incidence of Surveillance (CHAMPS) platform, which assesses Mortality Prevention
Surveillance network see
hospitalisation for RSV and bronchiolitis in children multiple aetiologies among deceased children by means https://champshealth.org/
were temporally associated with the universal intro of molecular and pathological evaluation of tissue
duction of pneumococcal conjugate vaccines in children collected with minimally invasive post-mortem sampling
in several populations.28–30 For instance, RSV hospi from multiple organs, and assigns the causal chain for
talisations among children aged 3–11 months declined by each death via a standardised process. Among children
18% in the USA after the introduction of the pneumo younger than 6 months in seven high-mortality CHAMPS
coccal conjugate vaccine.31 However, another study in sites, RSV was detected in 4·0% of all deaths and was
Australia did not detect a decline in RSV after the identified in the causal chain of 1·7% deaths.34 Among
introduction of pneumococcal conjugate vaccines.32 deaths in the first week of life, RSV was rarely detected
(1·3%), and was never established to be in the causal
RSV-associated mortality chain of death. However, between the ages of 7 days and
Prevention of RSV-associated deaths is a major goal of 6 months, RSV was detected in 8·7% of deaths and
immunisation programmes in LMICs, wherein more identified in the causal chain of 4·7% of deaths. Notably,
than 97% of global RSV deaths occur.4 The updated RSV very few deaths were deemed to be caused by RSV
global mortality analysis for 2019 reported RSV- alone—as previously mentioned, RSV can increase the
attributable mortality in which RSV was in the causal risk for subsequent bacterial superinfection,27 and thus
chain of the death, and RSV-associated mortality where serve as the initial pathogenic insult that contributes to
RSV was detected in the respiratory tract but had an deaths several days or even weeks after onset of RSV
unclear causal role.4 RSV-attributable mortality in illness.35
children younger than 6 months (the target age range for
RSV vaccines and monoclonal antibodies) was estimated Respiratory illnesses subsequent to RSV-LRTI
at 45 700 deaths (uncertainty range 38 400–55 900),4 which The Drakenstein Child Health study, a South African
translates to 2·1% (uncertainty range 1·7–2·5) of all birth cohort study, reported that children with RSV-LRTI
www.thelancet.com/infection Published online November 21, 2023 https://doi.org/10.1016/S1473-3099(23)00568-6 3
Personal View
in the first 2 years of life had a three-times higher risk of epidemiological study over five RSV seasons showed a
subsequent recurrent LRTI due to non-RSV pathogens.36 30% increase in subsequent asthma risk depending on
The incidence of recurrent LRTI was highest following birth timing, with the highest risk in those born 13 weeks
severe RSV-LRTI requiring hospitalisation, but even before the RSV peak.47 Furthermore, a US birth cohort
ambulatory RSV-LRTI was associated with a significantly that measured RSV infection (which should be
higher risk of recurrent LRTI compared with ambulatory distributed more randomly and less influenced by
non-RSV LRTI. A previous study in Gambian children genetic susceptibility than severe RSV disease) reported
with RSV-LRTI requiring hospitalisation and age- a 26% lower risk of asthma at the age of 5 years (adjusted
matched controls also reported an increased incidence of OR 0·74 [95% CI 0·58–0·94]) in children not infected
LRTI after hospitalisation for RSV-LRTI,37 as did a study with RSV during infancy than in children infected with
in Tennessee, USA.38 Despite the association shown in RSV during infancy (ie, the first year of life); the reduction
observational studies, recurrent LRTI has not been in risk was confined to non-atopic asthma subtypes.48
evaluated in randomised controlled trials of RSV The authors estimated that prevention of RSV infection
prevention, which would provide more definitive during infancy could potentially reduce cases of asthma
evidence of the association. at the age of 5 years by 15%; however, current RSV
Several studies and meta-analyses have reported a vaccines and monoclonal antibodies are unlikely to
significant association between RSV-LRTI in the first provide sterilising immunity and prevent all RSV
year of life (especially severe or RSV-LRTI requiring infections.49 Furthermore, potential mechanisms for the
hospitalisation) and recurrent wheezing or asthma in association of RSV-LRTI with subsequent recurrent
childhood.39–41 In a meta-analysis published in 2020, wheezing or asthma have now been shown in several in
children who had RSV-LRTI had 3·4-times (95% CI vitro and animal experiments (eg, RSV can affect
2·7–4·2) higher odds of subsequent wheezing, and a inflammatory pathways and airway epithelial develop
2·6-times (95% CI 1·7–4·0) higher odds of asthma at the ment).50 Early-life RSV-LRTI in South African children
age of 6 years or older.39 Almost all studies were was also associated with development of a recurrent
from high-income country settings; however, in the wheezing phenotype with increased airway resistance at
Drakenstein Child Health Study in South Africa, early 5 years, independent of baseline function.42
life RSV-LRTI was also strongly associated with all The long-term impact of early-life RSV-LRTI might
wheezing phenotypes (early, late, or recurrent) up to the extend beyond childhood and into chronic respiratory
age of 5 years.42 illness in adults. Asthma in young adults in Norway was
Despite the strong association between RSV-LRTI and almost twice as probable in those who had bronchiolitis
subsequent recurrent wheezing or asthma seen in during infancy than in demographically matched
observational studies, whether RSV is part of a causal individuals who did not.51 A study of a longitudinal cohort
pathway or RSV-LRTI, recurrent wheezing, and asthma recruited at birth in 1946 in the UK found that respiratory
reflect a common underlying genetic or physiological infection in infancy was associated with both obstructive
susceptibility to respiratory illness is unclear.39,43 A and restrictive lung function patterns in adulthood, but
randomised controlled trial of the monoclonal antibody only among smokers.52 A later analysis of the same birth
palivizumab in preterm infants (born at 32–35 weeks of cohort found a 93% increased risk of early adult
gestation) reported a significant 10% reduction in respiratory mortality, particularly from chronic obstruc
parental report of mild wheezy illness at 1 year and tive pulmonary disease, among those who had a LRTI
6 years of age; however, no difference was detected in episode before the age of 2 years, after adjustment for
physician-diagnosed wheezing or asthma or lung childhood socioeconomic factors and adult smoking.53
function as measured by spirometry at the age of 6 years.44 However, these associations between early-life LRTI and
Another randomised controlled trial of motavizumab, an adult respiratory disease are not specific to RSV and,
effective monoclonal antibody that was never licensed, importantly, are unable to adjust for an underlying
showed no difference in recurrent wheezing in full-term genetic predisposition for severe respiratory disease.
Native American children up to the age of 3 years.45
Additional evidence refuting a causal association comes RSV burden on health-care systems
from genetic studies. The association between RSV-LRTI RSV can have a substantial burden on health-care
with subsequent recurrent wheezing or asthma is systems. In temperate climates, the peak RSV season
reduced when partly controlling for genetic susceptibility: usually occurs over several months in autumn and
the adjusted odds ratio (OR) for the association decreases winter. Even in subtropical climates, approximately
from 4·2 (95% CI 2·4–7·4) to 2·5 (1·2–4·9).39 A small three-quarters of countries have seasonal RSV
study of monozygotic twins with discordant RSV-LRTI circulation.54 These seasonal spikes in RSV disease can
status showed no association with subsequent recurrent overwhelm hospitals by consuming much of the bed
wheezing or asthma.46 capacity in paediatric units and placing stress on staffing
In contrast, several birth-timing studies are more requirements. In the USA, discharge data from 2009–19
suggestive of a causal role of RSV. One large showed that RSV bronchiolitis was the overall leading
4 www.thelancet.com/infection Published online November 21, 2023 https://doi.org/10.1016/S1473-3099(23)00568-6
Personal View
cause of infant hospitalisation in every year, accounting (1·3–23·1) reduction in all antimicrobial prescriptions
for approximately 9·5% of all hospitalisations; during through to the age of 90 days compared with infants in
the RSV season, RSV accounted for approximately the placebo group, equating to 4·8 (95% CI 0·5–8·6)
16–18% of all hospitalisations among infants.55 In some antimicrobial courses averted per 100 infants.61 In the
high-incidence years, such as the recent 2022–23 season, nirsevimab trial, antibiotic use in children up to the age
the impact of RSV on the health-care system is even of 5 months in the intervention group was reduced by
greater.56 23·6% (3·8–39·3), resulting in 8·2 antibiotic courses
RSV’s burden on the health-care system is not confined averted per 100 infants.60 The reduction in antibiotic use
to high-income countries, but occurs also in LMICs, might extend beyond prevention of RSV-LRTI—for
where overall rates of RSV-LRTI are generally higher.57 In example, RSV has been implicated as an important cause
the Pneumonia Etiology Research for Child Health of acute otitis media, which drives a large proportion of
(PERCH) study of severe and very severe pneumonia, paediatric antibiotic use.62–64 One study found that
RSV was found to be the leading cause overall and in RSV-LRTI in the first 6 months of life was associated
each of the seven participating countries.3 Moreover, in with an increased incidence of otitis media and antibiotic
four PERCH countries with available data (The Gambia, prescriptions in the second half of infancy (6–11 months
Mali, Kenya, and South Africa), RSV accounted for of age).38 However, whether RSV prevention in the first
7·5–13·6% of all-cause hospitalisations in children aged 6 months of life can reduce the incidence of acute otitis
1–59 months.3 In the Drakenstein Child Health Study in media is unclear. Although a small randomised
South Africa,35 RSV-associated disease accounted for controlled trial of intravenous RSV immunoglobulin
15·3% of all-cause hospitalisations (excluding birth given to children younger than 2 years at high risk of
hospitalizations) in the first 2 years, and 22·0% in the severe RSV disease showed a reduction in the incidence
first 6 months of life.58 of the otitis media (27% vs 43%; p<0·01),65 a larger
In LMICs, where paediatric bed shortages tend to be randomised controlled trial of palivizumab, a monoclonal
more acute, the high burden of RSV admissions in antibody that more specifically targets RSV, found no
paediatric units can have secondary effects on hospital difference in otitis media rates between palivizumab and
systems’ ability to deliver care to children affected by placebo recipients (42% vs 40%; p=0·51).66
other health conditions. A study in the largest paediatric Given its high global incidence, RSV also incurs a
hospital in Bangladesh evaluated nearly 20 000 admitted substantial financial burden on health-care systems. One
children younger than 5 years in 2019. During this time, meta-analysis estimated that, in 2017, the global cost of
RSV-positive cases accounted for 6% of all admissions RSV-LRTI management (including both inpatient and
and 20–30% of all admissions during the peak RSV outpatient costs) was €4·82 billion (95% CI 3·47–7·93);
season; the average length of stay for RSV-positive while the cost per RSV episode was several-times higher
patients was 5 days.59 65% percent of RSV cases occurred in high-income countries than in LMICs, LMICs
within the first 6 months of life, which is the age range accounted for 65% of the global cost.67 This analysis did
for which current RSV products are likely to offer not take into account household expenditures. In
protection. In the same study, approximately 20% of Finland, 52% of parents of children younger than 3 years
children requiring hospitalisation were refused with an RSV-associated illness missed at least 1 day of
admission due to the unavailability of inpatient beds, and work, with a mean duration of absenteeism of 2·6 days
30-day mortality was higher among children who were (SD 1·5).64 Studies in Kenya and South Africa show that,
refused admission, mostly with perinatal complications although direct health-care expenses account for most
and neonatal diseases, than among those admitted. The costs related to RSV disease in those settings, a
researchers modelled that 15% of hospital bed-day substantial financial burden is placed on households
occupancy would be averted by an effective maternal through out-of-pocket expenses and indirect costs.68,69 A
RSV vaccine, resulting in a 2% reduction in mortality detailed review of the financial costs of RSV disease is
among children who need to be admitted to hospital, beyond the scope of this paper; cost-effectiveness
mostly due to fewer children being turned away for lack analyses of RSV prevention, including in LMICs, have
of bed availability. been published elsewhere.70,71
In the randomised controlled trial of nirsevimab
that took place mostly in high-income settings, Future research to define secondary effects of
hospitalisations for respiratory illness of any cause were RSV disease prevention
reduced by 38·9% (95% CI 6·3–60·2) and outpatient As countries introduce new maternal RSV vaccines and
visits for LRTI decreased by 41·9% (25·7–54·6) in infants monoclonal antibodies, how might these ripple effects of
receiving nirsevimab.8,60 Beyond its effects on health-care prevention best be measured, and over what timeframes?
visits, RSV prevention is also likely to result in decreased Some of these outcomes, such as effects on all-cause
antimicrobial use. In the RSV F protein nanoparticle LRTI or on health-care system use, might be discernible
maternal vaccine trial (NCT02624947), despite moderate in the short term through planned or post-hoc analyses
efficacy, infants in the vaccine group had a 12·9% of the ongoing randomised controlled trials of RSV
www.thelancet.com/infection Published online November 21, 2023 https://doi.org/10.1016/S1473-3099(23)00568-6 5
Personal View
Level of pre-licensure evidence Certainty of effect Rapidity of effect demonstration after
implementation
Severe RSV-LRTI High (efficacy shown for all High (shown for all products in RCTs) Rapid (due to high incidence and high product
products in RCTs) effectiveness)
All-cause LRTI (including bacterial Medium (efficacy shown as Medium (depends on aetiologic fraction of RSV among Rapid (with high aetiologic fraction of RSV among LRTI
pneumonia) secondary outcome in some RCTs) LRTI cases) cases in settings with seasonal epidemics)
RSV disease-associated mortality Low (not shown in RCTs) Medium (preventing severe RSV-LRTI should prevent Medium (will require large post-introduction
RSV mortality in settings with poor access to care) populations to document because mortality is rare
outcome)
All-cause child mortality Low (not measured in RCTs) Low overall (because RSV contributes to small Medium (will require large post-introduction
proportion of child mortality); medium in the populations in high-mortality settings to document)
1–5 months age group (in which RSV contributes more
to mortality)
Long-term respiratory illness and lung Low to medium (mixed evidence Low to medium (mixed evidence of the causal role of Slow (many years of follow-up after widescale
function of the causal role of RSV; RCTs RSV) introduction needed to show impact on lung health
generally have not shown an outcomes)
effect)
Health-care system capacity Medium (reduction in Medium (among children aged 1–5 months during RSV Medium to rapid (in case of large RSV aetiological
hospitalisations and outpatient season); higher in settings of good access to health care fraction during RSV seasonal epidemics); quicker in
visits for all-cause LRTI shown in (ie, in high-income countries more than in lower- settings of good access to health care
some trials) income and middle-income countries)
Health-care system cost Low (no direct evidence that RSV Medium (should be documentable if reductions in Medium (would probably need several RSV seasons to
prevention lowers costs) health-care use occur) document effect on costs)
Reductions in antibiotic use High (effects shown in several Medium (depends on local antibiotic prescribing Medium to rapid (depends on antibiotic prescribing
RCTs) practices; less likely in low-income and middle-income practice and incidence of RSV)
countries, where antibiotic use is lower)
LRTI=lower respiratory tract infections. RCTs=randomised controlled trials. RSV=respiratory syncytial virus.
Table 2: Outcomes of RSV disease prevention on key outcomes after widespread introduction of RSV vaccines and monoclonal antibodies
vaccines and monoclonal antibodies (table 2, figure).72 A variety of study designs could be considered. In
However, relatively few participants from LMICs were areas where a prevention strategy has not yet been
enrolled in the randomised controlled trials; secondary introduced, randomised introduction of a product might
effects on child health and health-care system outcomes be initiated, such as step-wedge designs in which a
will also need to be measured in LMICs, where both product is introduced in a staggered manner in different
specific outcomes and magnitude of outcomes might geographical units (eg, subdistrict, district). Randomised
differ substantially from those in high-income countries.9 introduction of RSV vaccines and monoclonal anti
Assessment of many of these secondary outcomes will bodies, however, is unlikely to be feasible in many real-
require evaluations to be done after widespread world settings and would probably be done only in
introduction of RSV vaccines or monoclonal antibodies. special studies. As such, post-introduction evaluations
Measurements of the impact of RSV prevention is likely can also evaluate effects by means of quasi-experimental
to be more efficient in settings with clearly defined RSV designs, such as an interrupted time series, to estimate
seasons, when the aetiologic fraction of RSV among reductions in burden of vaccine-preventable disease
LRTI is high. Assessment would ideally occur over at once widespread vaccine introduction has occurred.77,78
least two RSV seasons because the severity of RSV Such evaluations require reliable pre-introduction and
epidemics might vary from year to year.73 Moreover, some post-introduction data regarding the outcome of interest,
countries show a biennial pattern of alternating severe as well as adjustment for other secular changes that
and less severe RSV epidemics, which might create the might affect surveillance. Synthetic controls analyses,
need for longer follow-ups to capture the full range of which use a weighted average of multiple comparison
effects of RSV prevention.74 Post-introduction effect groups (eg, similar countries who did not introduce RSV
studies could be used not only to define the impact on vaccines and monoclonal antibodies), might avoid some
biological outcomes, such as all-cause LRTI, severe LRTI, of the potential temporal confounders in other
and otitis media, but also health-care systems outcomes, approaches.79
such as hospital bed-days used and antibiotic courses In addition to post-introduction evaluations of the
prescribed.75 Moreover, post-introduction studies are positive secondary effects of RSV prevention, monitoring
probably the only feasible way to have a large enough for population-based adverse effects after widespread
population and a long enough follow-up time to define roll-out of these products must also occur. Some potential
effects on rare outcomes (eg, LRTI mortality) or outcomes risks of these products that will need to be evaluated are
that require a long time to manifest (eg, asthma).76 the emergence of viruses with escape mutations to the
6 www.thelancet.com/infection Published online November 21, 2023 https://doi.org/10.1016/S1473-3099(23)00568-6
Personal View
More than 5 years
Between 6 months and 5 years
Up to 6 months
Reduced incidence Improved lung
of wheezing health
episodes
Reduced all-cause LRTI
Reduced antibiotic use
Improved availability of
hospital beds
Reduced V LR
RSV-LRTI
all-cause deaths
RIP
Potential Potential
reduced reduced
incidence of incidence of
Reduced RSV
asthma COPD
disease deaths
Reduced
recurrent LRTI
Figure: Potential effects of preventing RSV-LRTI in infants younger than 1 year, by duration of impact
Figure created with BioRender.com. COPD=chronic obstructive pulmonary disease. LRTI=lower respiratory tract infections. RSV=respiratory syncytial virus.
epitopes targeted by monoclonal antibodies and pregnancy salient public health gains that can be achieved both in
outcomes after maternal vaccination.7,80,81 Descriptions of the short term and later in life. More evidence of the
approaches to monitoring post-introduction safety are secondary effects of RSV prevention should be gathered
beyond the scope of this paper. in clinical trials and post-introduction studies. Such
evidence will be crucial for decision makers to assess
Conclusion the full public health value of RSV prevention in their
RSV disease is poised to be the next clinically significant settings. It is this type of evidence on the full value of
infectious disease of infants to become preventable by these products that led WHO’s Strategic Advisory
immunisation. After decades of development, two Group of Experts on Immunization to call for a large-
classes of preventive products, RSV maternal vaccines scale RSV impact study in LMICs, where many
and long-acting monoclonal antibodies for infants, are competing immunisation and health priorities are
now licensed in the USA and European Union and pressing.82 The next few years will be a decisive period to
might soon be widely available. The primary focus of better define how these new preventive products can
the trials of these products, as well as their use case, is reduce the burden of RSV-LRTI, and to assess the ripple
the prevention of RSV-associated LRTI in infants effects of prevention on other important public health
younger than 1 year. The effects of preventing RSV measures.
disease, however, are likely to go beyond this important Contributors
outcome. We described how preventing RSV disease in DRF conceptualised the paper. All authors contributed to the original
infants younger than 1 year can lead to several other draft and revised the final paper. ES and DRF produced the figure.
www.thelancet.com/infection Published online November 21, 2023 https://doi.org/10.1016/S1473-3099(23)00568-6 7
Personal View
Declaration of interests 17 Shi T, Denouel A, Tietjen AK, et al. Global Disease Burden
DMW reports grants or contracts, paid to institution and unrelated to estimates of respiratory syncytial virus-associated acute respiratory
the subject of this work, from the US National Institutes of Health, infection in older adults in 2015: a systematic review and meta-
Bill & Melinda Gates Foundation, US Veterans Affairs Department, analysis. J Infect Dis 2020; 222 (suppl 7): S577–83.
Pfizer, and Merck; consulting fees from Merck, Pfizer, and 18 US Food and Drug Administration. FDA approved first respiratory
GSK/Affinivax; and payment or honoraria for lectures, presentations, syncytial virus (RSV) vaccine. https://fda.gov/news-events/press-
participation in speakers’ bureaus, manuscript writing, or educational announcements/fda-approves-first-respiratory-syncytial-virus-rsv-
vaccine (accessed Aug 28, 2023).
events from Pfizer and Merck. HJZ reports funding paid to institution
from the Gates Foundation, US National Institutes of Health, Pfizer, 19 US Food and Drug Administration. Abrysvo. https://www.fda.gov/
vaccines-blood-biologics/abrysvo (accessed Aug 28, 2023).
AstraZeneca, and MSD. RAK reports grants paid to institution from the
20 Izu A, Nunes MC, Solomon F, et al. All-cause and pathogen-
US National Institutes of Health and Sanofi Pasteur; and is the chair of
specific lower respiratory tract infection hospital admissions in
the WHO Product Development for Vaccines Advisory Committee.
children younger than 5 years during the COVID-19 pandemic
DRF and ES report funding paid to institution from the Gates (2020–22) compared with the pre-pandemic period (2015–19) in
Foundation for respiratory syncytial virus-related activities. SKS and South Africa: an observational study. Lancet Infect Dis 2023;
PS declare no competing interests. 23: 1031–41.
References 21 Avolio M, Venturini S, De Rosa R, Crapis M, Basaglia G.
1 Perin J, Mulick A, Yeung D, et al. Global, regional, and national Epidemiology of respiratory virus before and during COVID-19
causes of under-5 mortality in 2000–19: an updated systematic pandemic. Infez Med 2022; 30: 104–08.
analysis with implications for the Sustainable Development Goals. 22 Dagan R, van der Beek BA, Ben-Shimol S, et al. The COVID-19
Lancet Child Adolesc Health 2022; 6: 106–15. pandemic as an opportunity for unravelling the causative
2 Jain S, Williams DJ, Arnold SR, et al. Community-acquired association between respiratory viruses and pneumococcus-
pneumonia requiring hospitalization among US children. associated disease in young children: a prospective study.
N Engl J Med 2015; 372: 835–45. EBioMedicine 2023; 90: 104493.
3 O’Brien KL, Baggett HC, Brooks WA, et al. Causes of severe 23 Rybak A, Levy C, Angoulvant F, et al. Association of
pneumonia requiring hospital admission in children without HIV nonpharmaceutical interventions during the COVID-19 pandemic
infection from Africa and Asia: the PERCH multi-country case- with invasive pneumococcal disease, pneumococcal carriage, and
control study. Lancet 2019; 394: 757–79. respiratory viral infections among children in France.
JAMA Netw Open 2022; 5: e2218959.
4 Li Y, Wang X, Blau DM, et al. Global, regional, and national disease
burden estimates of acute lower respiratory infections due to 24 Billard MN, van de Ven PM, Baraldi B, Kragten-Tabatabaie L,
respiratory syncytial virus in children younger than 5 years in 2019: Bont LJ, Wildenbeest JG. International changes in respiratory
a systematic analysis. Lancet 2022; 399: 2047–64. syncytial virus (RSV) epidemiology during the COVID-19 pandemic:
association with school closures. Influenza Other Respir Viruses
5 Hammitt LL, Dagan R, Yuan Y, et al. Nirsevimab for prevention of
2022; 16: 926–36.
RSV in healthy late-preterm and term infants. N Engl J Med 2022;
386: 837–46. 25 Li Y, Wang X, Cong B, Deng S, Feikin DR, Nair H. Understanding
the potential drivers for respiratory syncytial virus rebound during
6 Simões EAF, Center KJ, Tita ATN, et al. Prefusion F protein-based
the coronavirus disease 2019 pandemic. J Infect Dis 2022;
respiratory syncytial virus immunization in pregnancy.
225: 957–64.
N Engl J Med 2022; 386: 1615–26.
26 Ouldali N, Deceuninck G, Lefebvre B, et al. Increase of invasive
7 Kampmann B, Madhi SA, Munjal I, et al. Bivalent prefusion F
pneumococcal disease in children temporally associated with RSV
vaccine in pregnancy to prevent RSV illness in infants. N Engl J Med
outbreak in Quebec: a time-series analysis. Lancet Reg Health Am
2023; 388: 1451–64.
2023; 19: 100448.
8 Muller WJ, Madhi SA, Seoane Nuñez B, et al. Nirsevimab for
27 Madhi SA, Klugman KP, Group VT. A role for Streptococcus
prevention of RSV in term and late-preterm infants. N Engl J Med
pneumoniae in virus-associated pneumonia. Nat Med 2004;
2023; 388: 1533–34.
10: 811–13.
9 Madhi SA, Polack FP, Piedra PA, et al. Respiratory syncytial virus
28 Foote EM, Singleton RJ, Holman RC, et al. Lower respiratory tract
vaccination during pregnancy and effects in infants. N Engl J Med
infection hospitalizations among American Indian/Alaska Native
2020; 383: 426–39.
children and the general United States child population.
10 Tang A, Chen Z, Cox KS, et al. A potent broadly neutralizing Int J Circumpolar Health 2015; 74: 29256.
human RSV antibody targets conserved site IV of the fusion
29 Fathima P, Blyth CC, Lehmann D, et al. The impact of
glycoprotein. Nat Commun 2019; 10: 4153.
pneumococcal vaccination on bacterial and viral pneumonia in
11 US Food and Drug Administration. FDA approves new drug to Western Australian children: record linkage cohort study of
prevent RSV in babies and toddlers. July 17, 2023. https://www.fda. 469 589 births, 1996–2012. Clin Infect Dis 2018; 66: 1075–85.
gov/news-events/press-announcements/fda-approves-new-drug-
30 Le H, Gidding H, Blyth CC, Richmond P, Moore HC.
prevent-rsv-babies-and-toddlers (accessed Aug 14, 2023).
Pneumococcal conjugate vaccines are protective against respiratory
12 European Medicines Agency. Beyfortus. https://www.ema.europa. syncytial virus hospitalizations in infants: a population-based
eu/en/medicines/human/EPAR/beyfortus (accessed observational study. Open Forum Infect Dis 2023; 10: ofad199.
Jan 27, 2023).
31 Weinberger DM, Klugman KP, Steiner CA, Simonsen L, Viboud C.
13 US Food and Drug Administration. FDA approves first vaccine for Association between respiratory syncytial virus activity and
pregnant individuals to prevent RSV in infants. Aug 21, 2023. pneumococcal disease in infants: a time series analysis of US
https://fda.gov/news-events/press-announcements/fda-approves- hospitalization data. PLoS Med 2015; 12: e1001776.
first-vaccine-pregnant-individuals-prevent-rsv-infants (accessed
32 Binks MJ, Beissbarth J, Oguoma VM, et al. Acute lower respiratory
Aug 28, 2023).
infections in Indigenous infants in Australia’s Northern Territory
14 Pfizer. European Commission approves Pfizer’s ABRYSVO™ to across three eras of pneumococcal conjugate vaccine use (2006–15):
help protect infants through maternal immunization and older a population-based cohort study. Lancet Child Adolesc Health 2020;
adults from RSV. Aug 24, 2023. https://www.pfizer.com/news/ 4: 425–34.
press-release/press-release-detail/european-commission-approves-
33 Srikantiah P, Vora P, Klugman KP. Assessing the full burden of
pfizers-abrysvotm-help-protect (accessed Aug 31, 2023).
respiratory syncytial virus in young infants in low- and middle-
15 Gessner BD, Feikin DR. Vaccine preventable disease incidence as a income countries: the importance of community mortality studies.
complement to vaccine efficacy for setting vaccine policy. Vaccine Clin Infect Dis 2021; 73 (suppl 3): S177–79.
2014; 32: 3133–38.
34 Blau DM, Baillie VL, Els T, et al. Deaths attributed to respiratory
16 Gessner BD, Wilder-Smith A. Estimating the public health syncytial virus in young children in high-mortality rate settings:
importance of the CYD-tetravalent dengue vaccine: vaccine report from child health and mortality prevention surveillance
preventable disease incidence and numbers needed to vaccinate. (CHAMPS). Clin Infect Dis 2021; 73 (suppl 3): S218–28.
Vaccine 2016; 34: 2397–401.
8 www.thelancet.com/infection Published online November 21, 2023 https://doi.org/10.1016/S1473-3099(23)00568-6
Personal View
35 Li Y, Campbell H, Nair H, Investigators R. Unveiling the risk period 54 Li Y, Hodgson D, Wang X, Atkins KE, Feikin DR, Nair H.
for death after respiratory syncytial virus illness in young children Respiratory syncytial virus seasonality and prevention strategy
using a self-controlled case series design. J Infect Dis 2020; planning for passive immunisation of infants in low-income and
222 (suppl 7): S634–39. middle-income countries: a modelling study. Lancet Infect Dis 2021;
36 Zar HJ, Nduru P, Stadler JAM, et al. Early-life respiratory syncytial 21: 1303–12.
virus lower respiratory tract infection in a South African birth 55 Suh M, Movva N, Jiang X, et al. respiratory syncytial virus is the
cohort: epidemiology and effect on lung health. Lancet Glob Health leading cause of United States infant hospitalizations, 2009-2019:
2020; 8: e1316–25. a study of the national (nationwide) inpatient sample. J Infect Dis
37 Weber MW, Milligan P, Giadom B, et al. Respiratory illness after 2022; 226 (suppl 2): S154–63.
severe respiratory syncytial virus disease in infancy in The Gambia. 56 Abu-Raya B, Viñeta Paramo M, Reicherz F, Lavoie PM. Why has the
J Pediatr 1999; 135: 683–88. epidemiology of RSV changed during the COVID-19 pandemic?
38 Abreo A, Wu P, Donovan BM, et al. Infant respiratory syncytial eClinicalMedicine 2023; 61: 102089.
virus bronchiolitis and subsequent risk of pneumonia, otitis media, 57 Langley JM, Bianco V, Domachowske JB, et al. Incidence of
and antibiotic utilization. Clin Infect Dis 2020; 71: 211–14. respiratory syncytial virus lower respiratory tract infections during
39 Brunwasser SM, Snyder BM, Driscoll AJ, et al. Assessing the the first 2 years of life: a prospective study across diverse global
strength of evidence for a causal effect of respiratory syncytial virus settings. J Infect Dis 2022; 226: 374–85.
lower respiratory tract infections on subsequent wheezing illness: 58 Wedderburn CJ, Bondar J, Lake MT, et al. Risk and rates of
a systematic review and meta-analysis. Lancet Respir Med 2020; hospitalisation in young children: a prospective study of a
8: 795–806. South African birth cohort. medRxiv 2023; published online
40 Régnier SA, Huels J. Association between respiratory syncytial June 12. https://doi.org/10.1101/2023.06.08.23289961 (preprint).
virus hospitalizations in infants and respiratory sequelae: 59 Saha S. 2013, Impact of RSV infections on the health system.
systematic review and meta-analysis. Pediatr Infect Dis J 2013; ReSViNET Conference, Feb 22–24, 2023. https://www.youtube.
32: 820–26. com/watch?app=desktop&v=PceXTnuDNrw&t=8290s (accessed
41 Shi T, Ooi Y, Zaw EM, et al. Association between respiratory Aug 28, 2023).
syncytial virus-associated acute lower respiratory infection in early 60 Simões EAF, Madhi SA, Muller WJ, et al. Efficacy of nirsevimab
life and recurrent wheeze and asthma in later childhood. J Infect Dis against respiratory syncytial virus lower respiratory tract infections
2020; 222 (suppl 7): S628–33. in preterm and term infants, and pharmacokinetic extrapolation to
42 McCready C, Haider S, Little F, et al. Early childhood wheezing infants with congenital heart disease and chronic lung disease:
phenotypes and determinants in a South African birth cohort: a pooled analysis of randomised controlled trials.
longitudinal analysis of the Drakenstein Child Health Study. Lancet Child Adolesc Health 2023; 7: 180–89.
Lancet Child Adolesc Health 2023; 7: 127–35. 61 Lewnard JA, Fries LF, Cho I, Chen J, Laxminarayan R. Prevention
43 Driscoll AJ, Arshad SH, Bont L, et al. Does respiratory syncytial of antimicrobial prescribing among infants following maternal
virus lower respiratory illness in early life cause recurrent wheeze vaccination against respiratory syncytial virus.
of early childhood and asthma? Critical review of the evidence and Proc Natl Acad Sci USA 2022; 119: e2112410119.
guidance for future studies from a World Health Organization- 62 Phillips M, Finelli L, Saiman L, Wang C, Choi Y, Patel J. Respiratory
sponsored meeting. Vaccine 2020; 38: 2435–48. syncytial virus-associated acute otitis media in infants and children.
44 Scheltema NM, Nibbelke EE, Pouw J, et al. Respiratory syncytial J Pediatric Infect Dis Soc 2020; 9: 544–50.
virus prevention and asthma in healthy preterm infants: 63 Papan C, Willersinn M, Weiß C, Karremann M, Schroten H,
a randomised controlled trial. Lancet Respir Med 2018; 6: 257–64. Tenenbaum T. Antibiotic utilization in hospitalized children under
45 O’Brien KL, Chandran A, Weatherholtz R, et al. Efficacy of 2 years of age with influenza or respiratory syncytial virus
motavizumab for the prevention of respiratory syncytial virus infection—a comparative, retrospective analysis. BMC Infect Dis
disease in healthy Native American infants: a phase 3 randomised 2020; 20: 606.
double-blind placebo-controlled trial. Lancet Infect Dis 2015; 64 Heikkinen T, Ojala E, Waris M. Clinical and socioeconomic burden
15: 1398–408. of respiratory syncytial virus infection in children. J Infect Dis 2017;
46 Poorisrisak P, Halkjaer LB, Thomsen SF, et al. Causal direction 215: 17–23.
between respiratory syncytial virus bronchiolitis and asthma studied 65 The PREVENT Study Group. Reduction of respiratory syncytial
in monozygotic twins. Chest 2010; 138: 338–44. virus hospitalization among premature infants and infants with
47 Wu P, Dupont WD, Griffin MR, et al. Evidence of a causal role of bronchopulmonary dysplasia using respiratory syncytial virus
winter virus infection during infancy in early childhood asthma. immune globulin prophylaxis. Pediatrics 1997; 99: 93–99.
Am J Respir Crit Care Med 2008; 178: 1123–29. 66 The IMpact-RSV Study Group. Palivizumab, a humanized
48 Rosas-Salazar C, Chirkova T, Gebretsadik T, et al. Respiratory respiratory syncytial virus monoclonal antibody, reduces
syncytial virus infection during infancy and asthma during hospitalization from respiratory syncytial virus infection in high-
childhood in the USA (INSPIRE): a population-based, prospective risk infants. The IMpact-RSV Study Group. Pediatrics 1998;
birth cohort study. Lancet 2023; 401: 1669–80. 102: 531–37.
49 Wilkins D, Yuan Y, Chang Y, et al. Durability of neutralizing RSV 67 Zhang S, Akmar LZ, Bailey F, et al. Cost of respiratory syncytial
antibodies following nirsevimab administration and elicitation of virus-associated acute lower respiratory infection management in
the natural immune response to RSV infection in infants. Nat Med young children at the regional and global level: a systematic review
2023; 29: 1172–79. and meta-analysis. J Infect Dis 2020; 222 (suppl 7): S680–87.
50 Binns E, Tuckerman J, Licciardi PV, Wurzel D. Respiratory syncytial 68 Moyes J, Tempia S, Walaza S, et al. The economic burden of RSV-
virus, recurrent wheeze and asthma: a narrative review of associated illness in children aged <5 years, South Africa 2011–2016.
pathophysiology, prevention and future directions. BMC Med 2023; 21: 146.
J Paediatr Child Health 2022; 58: 1741–46. 69 Koltai M, Moyes J, Nyawanda B, et al. Estimating the cost-
51 Sørensen KG, Øymar K, Dalen I, Halvorsen T, Mikalsen IB. effectiveness of maternal vaccination and monoclonal antibodies for
Asthma, atopy and lung function in young adults after respiratory syncytial virus in Kenya and South Africa. BMC Med
hospitalisation for bronchiolitis in infancy: impact of virus and sex. 2023; 21: 120.
BMJ Open Respir Res 2022; 9: e001095. 70 Baral R, Higgins D, Regan K, Pecenka C. Impact and cost-
52 Allinson JP, Hardy R, Donaldson GC, Shaheen SO, Kuh D, effectiveness of potential interventions against infant respiratory
Wedzicha JA. Combined impact of smoking and early-life exposures syncytial virus (RSV) in 131 low-income and middle-income
on adult lung function trajectories. Am J Respir Crit Care Med 2017; countries using a static cohort model. BMJ Open 2021; 11: e046563.
196: 1021–30. 71 Li X, Willem L, Antillon M, Bilcke J, Jit M, Beutels P. Health and
53 Allinson JP, Chaturvedi N, Wong A, et al. Early childhood lower economic burden of respiratory syncytial virus (RSV) disease and
respiratory tract infection and premature adult death from the cost-effectiveness of potential interventions against RSV among
respiratory disease in Great Britain: a national birth cohort study. children under 5 years in 72 Gavi-eligible countries. BMC Med 2020;
Lancet 2023; 401: 1183–93. 18: 82.
www.thelancet.com/infection Published online November 21, 2023 https://doi.org/10.1016/S1473-3099(23)00568-6 9
Personal View
72 Karron RA, Zar HJ. Determining the outcomes of interventions to 78 Lopez Bernal JA, Andrews N, Amirthalingam G. The use of quasi-
prevent respiratory syncytial virus disease in children: what to experimental designs for vaccine evaluation. Clin Infect Dis 2019;
measure? Lancet Respir Med 2018; 6: 65–74. 68: 1769–76.
73 Billard MN, Wildenbeest J, Bont LJ, et al. Year-to-year variation in 79 Bruhn CA, Hetterich S, Schuck-Paim C, et al. Estimating the
attack rates could result in underpowered respiratory syncytial virus population-level impact of vaccines using synthetic controls.
vaccine efficacy trials. J Clin Epidemiol 2022; 147: 11–20. Proc Natl Acad Sci USA 2017; 114: 1524–29.
74 Reeves RM, van Wijhe M, Tong S, et al. Respiratory syncytial virus- 80 Langedijk AC, Bont LJ. Respiratory syncytial virus infection and
associated hospital admissions in children younger than 5 years in novel interventions. Nat Rev Microbiol 2023; 21: 734–49.
7 European countries using routinely collected datasets. J Infect Dis 81 Simões EAF, Forleo-Neto E, Geba GP, et al. Suptavumab for the
2020; 222 (suppl 7): S599–605. prevention of medically attended respiratory syncytial virus
75 Feikin DR, Scott JA, Gessner BD. Use of vaccines as probes to infection in preterm infants. Clin Infect Dis 2021; 73: e4400–08.
define disease burden. Lancet 2014; 383: 1762–70. 82 WHO. Meeting of the Strategic Advisory Group of Experts on
76 Riddell CA, Bhat N, Bont LJ, et al. Informing randomized clinical Immunization, October 2022: conclusions and recommendations.
trials of respiratory syncytial virus vaccination during pregnancy to Geneva: World Health Organization, 2023. https://apps.who.int/
prevent recurrent childhood wheezing: a sample size analysis. iris/handle/10665/365500 (accessed Feb 8, 2023).
Vaccine 2018; 36: 8100–09.
77 Grijalva CG, Nuorti JP, Arbogast PG, Martin SW, Edwards KM, Copyright © 2023 Elsevier Ltd. All rights reserved.
Griffin MR. Decline in pneumonia admissions after routine
childhood immunisation with pneumococcal conjugate vaccine in
the USA: a time-series analysis. Lancet 2007; 369: 1179–86.
10 www.thelancet.com/infection Published online November 21, 2023 https://doi.org/10.1016/S1473-3099(23)00568-6
You might also like
- nsg-436 BenchmarkDocument6 pagesnsg-436 Benchmarkapi-509646698No ratings yet
- JNB 2 222Document13 pagesJNB 2 222Lars JayhawkNo ratings yet
- Neonatal Infections PerspectiveDocument13 pagesNeonatal Infections PerspectiveYUDY LORENA GIRALDO ALFONSONo ratings yet
- Community-Acquired Pneumonia in Children: Myths and FactsDocument4 pagesCommunity-Acquired Pneumonia in Children: Myths and FactsFranciscoDelgadoNo ratings yet
- Respiratory Syncytial Virus Infection and Bronchiolitis: Practice GapsDocument14 pagesRespiratory Syncytial Virus Infection and Bronchiolitis: Practice GapsAnge CerónNo ratings yet
- Etm 20 6 9350 PDFDocument8 pagesEtm 20 6 9350 PDFJessica Asitimbay ZuritaNo ratings yet
- ClinicalCharacteristicsandRiskfactorsofSevereRespiratorySyncytialVirus associatedAcuteLowerRespiratoryTractInfectionsinHospitalizedInfantsDocument6 pagesClinicalCharacteristicsandRiskfactorsofSevereRespiratorySyncytialVirus associatedAcuteLowerRespiratoryTractInfectionsinHospitalizedInfantsRachata HantulaNo ratings yet
- ECPE-03-SI-0012 Covid 19Document3 pagesECPE-03-SI-0012 Covid 19ijklmnopqurstNo ratings yet
- Management of The Febrile Young Infant: Cme R ADocument6 pagesManagement of The Febrile Young Infant: Cme R AsarabisimonaNo ratings yet
- Prevalence and Associated Risk Factors of Sepsis Among Neonates Admitted Into Neonatal Intensive Care Units of Public Hospitals in DhakaDocument12 pagesPrevalence and Associated Risk Factors of Sepsis Among Neonates Admitted Into Neonatal Intensive Care Units of Public Hospitals in DhakaAnonymous SMLzNANo ratings yet
- International Journal of Infectious Diseases: Ben J. MaraisDocument4 pagesInternational Journal of Infectious Diseases: Ben J. MaraisMiftahurrahmah GmsNo ratings yet
- International Journal of Pediatric Research Ijpr 9 112Document12 pagesInternational Journal of Pediatric Research Ijpr 9 112VsbshNo ratings yet
- A Vaccine For MalariaDocument2 pagesA Vaccine For MalariaArcciPradessatamaNo ratings yet
- Jurnal OkeDocument8 pagesJurnal OkeAuliaRahmanNo ratings yet
- Detection of Respiratory Syncytial Virus and Rhinovirus in Healthy InfantsDocument5 pagesDetection of Respiratory Syncytial Virus and Rhinovirus in Healthy Infants8502474No ratings yet
- Trend and Outcome of Sepsis in ChildrenDocument8 pagesTrend and Outcome of Sepsis in ChildrenGunduz AgaNo ratings yet
- Impact of Rhesus Disease On The Global Problem of Bilirubin-Induced Neurologic DysfunctionDocument4 pagesImpact of Rhesus Disease On The Global Problem of Bilirubin-Induced Neurologic DysfunctionRahmayani IsmaNo ratings yet
- NIH Public Access: Author ManuscriptDocument17 pagesNIH Public Access: Author ManuscriptAndika ZuldiansyahNo ratings yet
- Influenza Resp Viruses - 2023 - Colosia - Systematic Literature Review of The Signs and Symptoms of Respiratory Syncytial-1Document12 pagesInfluenza Resp Viruses - 2023 - Colosia - Systematic Literature Review of The Signs and Symptoms of Respiratory Syncytial-1AGUS DE COLSANo ratings yet
- Asmainf AmamDocument10 pagesAsmainf AmamgabibarbozaNo ratings yet
- Revisión Sistematica - TuberculosisDocument9 pagesRevisión Sistematica - TuberculosisKaren Reichell MedinaNo ratings yet
- Pilot Comparative Study On The Health of Vaccinated and Unvaccinated 6 - To 12-Year-Old U.S. Children - 2017Document12 pagesPilot Comparative Study On The Health of Vaccinated and Unvaccinated 6 - To 12-Year-Old U.S. Children - 2017breakingthesilence100% (1)
- Impact of Tetanus ToxoidDocument6 pagesImpact of Tetanus Toxoidanes noerNo ratings yet
- Wynn 2016 Defining Neonatal SepsisDocument11 pagesWynn 2016 Defining Neonatal SepsisEllya Latifah IlyasNo ratings yet
- Neonatal SepsisDocument12 pagesNeonatal Sepsissandra bullaNo ratings yet
- Nihms 737709Document19 pagesNihms 737709Net FlixNo ratings yet
- Effect of Pneumococcal Conjugate Vaccine Introduction On Childhood Pneumonia Mortality in Brazil: A Retrospective Observational StudyDocument8 pagesEffect of Pneumococcal Conjugate Vaccine Introduction On Childhood Pneumonia Mortality in Brazil: A Retrospective Observational StudyDiego AndradeNo ratings yet
- Epidemiol Rev 2006 Robinson 81 7Document7 pagesEpidemiol Rev 2006 Robinson 81 7chie_8866No ratings yet
- Der Kay 2018Document5 pagesDer Kay 2018Giovanni HenryNo ratings yet
- Fuchs 2018Document14 pagesFuchs 2018Miguel Angel CayojaNo ratings yet
- RSV Is Surging Among Kids - Here's What You Need To KnowDocument5 pagesRSV Is Surging Among Kids - Here's What You Need To KnowAbdo MohamedNo ratings yet
- Epidemiology of Invasive Early Onset Neonatal SepsisDocument11 pagesEpidemiology of Invasive Early Onset Neonatal SepsisLucas SalgadoNo ratings yet
- Lowerrespiratory Tractinfections: Anne B. Chang,, Christina C. Chang,, K. O'Grady,, P.J. TorzilloDocument19 pagesLowerrespiratory Tractinfections: Anne B. Chang,, Christina C. Chang,, K. O'Grady,, P.J. Torzilloshrey keyalNo ratings yet
- Paediatric Sepsis: ReviewDocument8 pagesPaediatric Sepsis: ReviewMuhamad RockystankiNo ratings yet
- Acute Respiratory Distress Syndrome Among Premature Neonates: Prevalence, Mortality Rate and Risk Factors of MortalityDocument5 pagesAcute Respiratory Distress Syndrome Among Premature Neonates: Prevalence, Mortality Rate and Risk Factors of MortalityInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Piis258953702200061x PDFDocument11 pagesPiis258953702200061x PDFRong LiuNo ratings yet
- PLOTKINDocument6 pagesPLOTKINElPaisUyNo ratings yet
- Perez Velez 2012Document14 pagesPerez Velez 2012Abby OliivasNo ratings yet
- TP 08 03 212Document15 pagesTP 08 03 212Hendro SihalohoNo ratings yet
- Art 2Document14 pagesArt 2linda margaritaNo ratings yet
- Ershad2019 Article NeonatalSepsisDocument8 pagesErshad2019 Article NeonatalSepsislucya simbiakNo ratings yet
- Tuberculosis in Infants and ChildrenDocument29 pagesTuberculosis in Infants and ChildrenAnisah TifaniNo ratings yet
- Neonatal SepsisDocument11 pagesNeonatal SepsisrezkadehaNo ratings yet
- Multidrug-Resistant Healthcare-Associated Infections in Neonates With Severe Respiratory Failure and The Impacts of Inappropriate Initial AntibioticDocument12 pagesMultidrug-Resistant Healthcare-Associated Infections in Neonates With Severe Respiratory Failure and The Impacts of Inappropriate Initial AntibioticbenNo ratings yet
- Prospects For A Safe COVID-19 Vaccine: CoronavirusDocument17 pagesProspects For A Safe COVID-19 Vaccine: CoronavirusRade ArtoritoNo ratings yet
- Special Issue ARTICLE Less Is More: Evidence-Based Management of BronchiolitisDocument11 pagesSpecial Issue ARTICLE Less Is More: Evidence-Based Management of BronchiolitisyundaNo ratings yet
- 2017 Article 71Document8 pages2017 Article 71Sahil DhamijaNo ratings yet
- BronchiolitisDocument4 pagesBronchiolitisFlavia RochmanNo ratings yet
- Impact of Earlier Combination Antiretroviral Therapy On Outcomes in ChildrenDocument6 pagesImpact of Earlier Combination Antiretroviral Therapy On Outcomes in ChildrenLUIS ALFREDO SALGADO FLORESNo ratings yet
- MacGinty Et Al-2018-Pediatric PulmonologyDocument14 pagesMacGinty Et Al-2018-Pediatric Pulmonologywawa chenNo ratings yet
- Artikel Rotaviruses FinalDocument30 pagesArtikel Rotaviruses Finalsemangat pagiNo ratings yet
- Neumonia Por InfluenzaDocument19 pagesNeumonia Por InfluenzaEdgar GavilanesNo ratings yet
- Pediatrics 2012 780 92Document15 pagesPediatrics 2012 780 92ERICKNo ratings yet
- 2023 Kumar - Childhood PneumoniaDocument7 pages2023 Kumar - Childhood PneumoniagariascospNo ratings yet
- NEonatal Sepsis PDFDocument11 pagesNEonatal Sepsis PDFMarielaTessyGonzalesParedesNo ratings yet
- Childhood Pneumonia in New ZealandDocument6 pagesChildhood Pneumonia in New ZealandEri YunianNo ratings yet
- en Measles Immunization and Vitamin A For PDocument6 pagesen Measles Immunization and Vitamin A For PM Iqbal TriansyahNo ratings yet
- Dengue LancetDocument16 pagesDengue LancetJorge Ricardo Uchuya GómezNo ratings yet
- Key Clinical Research Priorities For The Pediatric Community During The COVID-19 PandemicDocument3 pagesKey Clinical Research Priorities For The Pediatric Community During The COVID-19 PandemicnpidasNo ratings yet
- Influenza vaccination: What does the scientific proof say?: Could it be more harmful than useful to vaccinate indiscriminately elderly people, pregnant women, children and health workers?From EverandInfluenza vaccination: What does the scientific proof say?: Could it be more harmful than useful to vaccinate indiscriminately elderly people, pregnant women, children and health workers?No ratings yet
- The Vaccine Handbook: A Practical Guide for Clinicians, Twelfth EditionFrom EverandThe Vaccine Handbook: A Practical Guide for Clinicians, Twelfth EditionNo ratings yet
- Carbapenem-Resistant Acinetobacter Baumannii in Latin AmericaDocument21 pagesCarbapenem-Resistant Acinetobacter Baumannii in Latin Americaluis sanchezNo ratings yet
- Association Between Children's Caregivers Time Preferences and Childhood Overweight and Obesity in MexicoDocument20 pagesAssociation Between Children's Caregivers Time Preferences and Childhood Overweight and Obesity in Mexicoluis sanchezNo ratings yet
- 2023 Focused Update ESC Guidelines For The DX and TX of A&CHFDocument13 pages2023 Focused Update ESC Guidelines For The DX and TX of A&CHFluis sanchezNo ratings yet
- Worldwide Trends in Underweight and Obesity From 1990 To 2022Document24 pagesWorldwide Trends in Underweight and Obesity From 1990 To 2022luis sanchezNo ratings yet
- Global, Regional, and National Age-Specific Progress Towards The 2020 MilestonesDocument28 pagesGlobal, Regional, and National Age-Specific Progress Towards The 2020 Milestonesluis sanchezNo ratings yet
- Associations of Socioeconomic Status and Healthy Lifestyle With Incident Early-Onset and Late-Onset DementiaDocument10 pagesAssociations of Socioeconomic Status and Healthy Lifestyle With Incident Early-Onset and Late-Onset Dementialuis sanchezNo ratings yet
- Here's What To Know About Cardiovascular-Kidney-Metabolic Syndrome, Newly Defined by The AHADocument2 pagesHere's What To Know About Cardiovascular-Kidney-Metabolic Syndrome, Newly Defined by The AHAluis sanchezNo ratings yet
- Practice Managers Book 08Document57 pagesPractice Managers Book 08SamiYousifNo ratings yet
- FebruariDocument985 pagesFebruaririniNo ratings yet
- National Immunization ProgramDocument67 pagesNational Immunization ProgrameezahNo ratings yet
- Research and Development Center For Vaccine and ImmunizationDocument22 pagesResearch and Development Center For Vaccine and ImmunizationAaron Ezekiel OngNo ratings yet
- Covid Vaccine Diplomacy Across The Globe: A Study of The Global SouthDocument6 pagesCovid Vaccine Diplomacy Across The Globe: A Study of The Global SouthIJAR JOURNALNo ratings yet
- Austin Journal of Vaccines & ImmunotherapeuticsDocument6 pagesAustin Journal of Vaccines & ImmunotherapeuticsAustin Publishing GroupNo ratings yet
- Community Medicine Term 1 QBankDocument9 pagesCommunity Medicine Term 1 QBankFaiza TasneemNo ratings yet
- Jonah Vaccine ProgramDocument40 pagesJonah Vaccine ProgramEdwin MagnoNo ratings yet
- School Based Immunization-FinalDocument22 pagesSchool Based Immunization-FinalMohammed T. Abdul Razak100% (2)
- Hygeia HMO SME Plans Proposal - 2022 - FinalDocument4 pagesHygeia HMO SME Plans Proposal - 2022 - FinalBanks C. GeorgeNo ratings yet
- Achmad Rafli - Increasing Immunization Coverage PDFDocument40 pagesAchmad Rafli - Increasing Immunization Coverage PDFKaze GifNo ratings yet
- Epidemiology PPTDocument342 pagesEpidemiology PPTTazee Jiituu Tazee JiituuNo ratings yet
- Intensified Pulse Polio ImmunisationDocument30 pagesIntensified Pulse Polio ImmunisationAdrishyaNo ratings yet
- Newer & Emerging Vaccine SynopsisDocument13 pagesNewer & Emerging Vaccine SynopsisShikhar SinghNo ratings yet
- Conversation P17310193032Document4 pagesConversation P17310193032Dhea DewiNo ratings yet
- National Immunization Program: Ray Anthony A. Camaliga, M.D Level 1 Resident DFCMDocument39 pagesNational Immunization Program: Ray Anthony A. Camaliga, M.D Level 1 Resident DFCMAnthony AbulNo ratings yet
- HP8865 Using Paracetamol or IbuprofenDocument7 pagesHP8865 Using Paracetamol or IbuprofenRoti Toti100% (1)
- Bahasa Inggris Uraian Tugas PoliklinikDocument7 pagesBahasa Inggris Uraian Tugas PoliklinikngurahadiNo ratings yet
- Thời gian: 150 phút (không kể thời gian giao đề) : (Đề thi gồm 12 trangDocument13 pagesThời gian: 150 phút (không kể thời gian giao đề) : (Đề thi gồm 12 trangNguyễn Thanh MỹNo ratings yet
- l3 Immunization & Cold ChainDocument53 pagesl3 Immunization & Cold ChainNur AinaaNo ratings yet
- ENGERIX B Hepatitis B Vaccine RecombinantDocument16 pagesENGERIX B Hepatitis B Vaccine RecombinantAngela MotoscaNo ratings yet
- Module 7 - DOH ProgramDocument32 pagesModule 7 - DOH Programmirai desuNo ratings yet
- REPUBLIC ACT No 10152Document5 pagesREPUBLIC ACT No 10152dteroseNo ratings yet
- ESIDocument84 pagesESIssatish_kumar33% (3)
- EO Supporting The Immunization Activities - EditedDocument2 pagesEO Supporting The Immunization Activities - EditedDem SalazarNo ratings yet
- CHCECE016 Student Assessment v2.0Document27 pagesCHCECE016 Student Assessment v2.0Shane COCNo ratings yet
- Mandatory Infants and Children Health Immunization Act of 2011Document13 pagesMandatory Infants and Children Health Immunization Act of 2011Divine MacaibaNo ratings yet
- Kenya National Immunization Policy Guidelines Version SignedDocument100 pagesKenya National Immunization Policy Guidelines Version SignedHarriet Temba100% (1)
- Eng101 BookletDocument84 pagesEng101 BookletZeynep SakaNo ratings yet