Professional Documents
Culture Documents
CARMABAZEPINE (Bauer)
Uploaded by
Ela chawOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CARMABAZEPINE (Bauer)
Uploaded by
Ela chawCopyright:
Available Formats
CARMABAZEPINE
INTRODUCTION
Carbamazepine is an iminostilbene derivative related to the tricyclic antidepressants that is
used in the treatment of tonic-clonic (grand mal), partial or secondarily generalized seizures (Table
11-1).1,2 Although methods have been suggested to treat acute seizures with carbamazepine, lack
of an intravenous dosage form has limited its use in this area. Thus, the drug is used primarily as
a prophylactic agent in the chronic therapy of epilepsy. Carbamazepine is also a useful agent to
treat trigeminal neuralgia and bipolar affective disorders.2,3 The antiseizure activity of
carbamazepine is related to its ability to decrease transmission in the nucleus ventralis anterior
section of the thalamus, an area of the brain thought to be involved with the generalization and
propagation of epileptic discharges.1,2 Although the exact cellular mechanism of action is unclear,
inhibition of voltage-gated sodium channels appears to be involved. Additionally, carbamazepine
depresses posttetanic potentiation and may prevent increases in cyclic adenosine monophosphate
(cAMP).
THERAPEUTIC AND TOXIC CONCENTRATIONS
The accepted therapeutic range for carbamazepine is 4–12 μg/mL when the drug is used
for the treatment of seizures. Carbamazepine plasma protein binding is quite variable among
individuals because it is bound to both albumin and α1-acid glycoprotein (AGP). In patients with
normal concentrations of these proteins, plasma protein binding is 75–80% resulting in a free
fraction of drug of 20–25%.4–6 AGP is classified as an acute phase reactant protein that is present
in lower amounts in all individuals but is secreted in large amounts in response to certain stresses
and disease states such as trauma, heart failure, and myocardial infarction. In patients with these
disease states, carbamazepine binding to AGP can be even larger resulting in an unbound fraction
as low as 10–15%. Little prospective work has been done to establish the therapeutic range for
unbound carbamazepine serum concentrations or the clinical situations where unbound
carbamazepine serum concentration measurement is useful. As an initial guide, 25% of the total
carbamazepine therapeutic range has been used to establish a preliminary desirable range for
unbound carbamazepine serum concentrations of 1–3 μg/mL. Although carbamazepine is highly
plasma protein bound, it is harder to displace this agent to the extent that a clinically important
change in protein binding takes place. Generally speaking, a doubling in unbound fraction in the
plasma is required to produce such an alteration. In comparison, phenytoin is 90% protein bound
under usual circumstances resulting in an unbound fraction in the plasma of 10%. It is relatively
easy to change the protein binding of phenytoin from 90–80%, under a variety of disease states or
conditions, which increases the unbound fraction in the plasma from 10% to 20%. However, it is
very difficult to change the protein binding of carbamazepine from 80% to 60% to achieve the
same doubling of unbound fraction in the plasma (20–40%). As a result of this, the use of unbound
carbamazepine serum concentrations are currently limited to those patients that have total
concentrations within the therapeutic range but experience adverse effects usually seen at higher
concentrations, or those patients that have total concentrations below the therapeutic range but
have a therapeutic response usually observed at higher concentrations.
Carbamazepine-10, 11-epoxide is an active metabolite of carbamazepine that contributes
to both the therapeutic and toxic effects of the drug, and can be measured in serum samples at a
limited number of epilepsy centers.7–13 The concentration of the epoxide is often related to the
presence or absence of other inhibitors or inducers of hepatic drug metabolizing enzymes. Epoxide
concentrations tend to be higher in patients taking enzyme inducers and lower in patients taking
enzyme inhibitors. The percent of epoxide to parent drug in chronically treated patients averages
about 12% for carbamazepine monotherapy, 14% when carbamazepine is taken with
phenobarbital, 18% when carbamazepine is taken with phenytoin, and about 25% when
carbamazepine is taken with both phenytoin and phenobarbital. Currently, the therapeutic range of
carbamazepine-10, 11-epoxide is not known although a suggested range of 0.4–4 μg/mL is used
by several research centers.
In the upper end of the therapeutic range (>8 μg/mL) some patients will begin to experience
the concentration-related adverse effects of carbamazepine treatment: nausea, vomiting, lethargy,
dizziness, drowsiness, headache, blurred vision, diplopia, unsteadiness, ataxia, incoordination.
Because carbamazepine induces its own hepatic metabolism, these adverse effects can also be seen
early during dosage titration periods soon after dosage increases are made. To improve patient
acceptance, it is important to initiate and titrate carbamazepine doses at a slow rate to minimize
side effects. Clinicians should understand that all patients with “toxic” carbamazepine serum
concentrations in the listed ranges will not exhibit signs or symptoms of carbamazepine toxicity.
Rather, carbamazepine concentrations in the ranges given increase the likelihood that an adverse
drug effect will occur.
CLINICAL MONITORING PARAMETERS
The goal of therapy with anticonvulsants is to reduce seizure frequency and maximize
quality of life with a minimum of adverse drug effects. While it is desirable to entirely abolish all
seizure episodes, it may not be possible to accomplish this in many patients. Patients should be
monitored for concentration-related side effects (nausea, vomiting, lethargy, dizziness,
drowsiness, headache, blurred vision, diplopia, unsteadiness, ataxia, incoordination).
Because carbamazepine has antidiuretic effects associated with reduced levels of
antidiuretic hormone, some patients may develop hyponatremia during chronic therapy with
carbamazepine, and serum sodium concentrations can be periodically measured.
Hematologic adverse effects can be divided into two types. The first is a leukopenia that
occurs in many patients and requires no therapeutic intervention. The typical clinical picture is an
individual with a normal white blood cell count who develops a transient decrease in this index.
In a few patients, a decreased, stable white blood cell count of 3000 cells/mm2 or less may persist
and does not appear to cause any deleterious effects. The second hematologic effect is severe and
usually requires discontinuation of the drug. Thrombocytopenia, leukopenia (trend downward in
white blood cell count with <2500 cells/mm2 or absolute neutrophil count <1000 cells/mm2), or
anemia are in this category. Rarely, aplastic anemia and agranulocytosis has been reported during
carbamazepine treatment. Drug induced hepatitis due to carbamazepine therapy has also been
reported. The severe hematologic and hepatic adverse effects tend to occur early in treatment.
Because of this, many clinicians measure a complete blood cell count and liver function tests
monthly for the first 3–6 months after a patient first begins carbamazepine treatment, and repeat
these tests every 3–6 months for the first year. Other idiosyncratic side effects include skin rash,
Stevens-Johnson syndrome, and systemic lupus-like reactions.
Carbamazepine serum concentrations should be measured in most patients. Because
epilepsy is an episodic disease state, patients do not experience seizures on a continuous basis.
Thus, during dosage titration it is difficult to tell if the patient is responding to drug therapy or
simply is not experiencing any abnormal central nervous system discharges at that time.
Carbamazepine serum concentrations are also valuable tools to avoid adverse drug effects. Patients
are more likely to accept drug therapy if adverse reactions are held to the absolute minimum.
Because carbamazepine induces its own hepatic metabolism, it is fairly easy to attain toxic
concentrations with modest increases in drug dose before maximal enzyme induction has occurred.
BASIC CLINICAL PHARMACOKINETIC PARAMETERS
Carbamazepine is primarily eliminated by hepatic metabolism (>99%) mainly via the
CYP3A4 enzyme system.14,15 Altogether 33 metabolites have been identified with
carbamazepine-10, 11-epoxide being the major species. The epoxide metabolite is active and
probably contributes to both the therapeutic and toxic side effects observed during therapy.
Carbamazepine is a potent inducer of hepatic drug metabolizing enzymes, and induces its own
metabolism, a process known as autoinduction (Figure 11-1).16–20 As a result, patients cannot
initially be placed on the dose of carbamazepine that will ultimately result in a safe and effective
outcome. At first, patients are started on 1 /4–1 /3 of the desired maintenance dose. This exposes
hepatic drug metabolizing enzymes to carbamazepine and begins the induction process. The dose
is increased by a similar amount every 2–3 weeks until the total desired daily dose is ultimately
given. This gradual exposure of carbamazepine allows liver enzyme induction and carbamazepine
clearance increases to occur over a 6- to 12-week time period. Therapeutic effect and steady-state
carbamazepine serum concentrations can be assessed 2–3 weeks after the final dosage increase.
Autoinduction continues to occur in patients who are stabilized on a carbamazepine dose but
require a dosage increase. It appears that a 2- to 3-week time period is also needed under chronic
dosing conditions for maximal autoinduction to occur after a dosage increase. The effects of
autoinduction are reversible even when doses are held for as few as 6 days.
An injectable form of carbamazepine is not available. For oral use, the drug is available as
immediate-release tablets (chewable: 100 mg, regular: 100 mg, 200 mg, 300 mg), sustained-release
tablets (100 mg, 200 mg, 400 mg), sustained-release capsules (100, 200, 300 mg), and suspension
(100 mg/5 mL). The rapid release dosage forms are erratically absorbed from the gastrointestinal
tract resulting in peak concentrations between 2–24 hours after a single dose of tablets (average 6
hours). During multiple dose studies after maximal autoinduction has taken place, peak
concentrations occur about 3 hours after tablet administration. Peak concentrations after multiple
doses of the sustained-release dosage forms are observed 3–12 hours after administration. Rectal
administration of an extemporaneously compounded carbamazepine retention enema results in
similar serum concentrations as that produced by a comparable immediate-release tablet.
The absolute oral bioavailability of carbamazepine is not known because no intravenous
form of the drug is available for comparison. Based on the best estimates available, carbamazepine
bioavailability is good and averages about 85–90%. The relative bioavailability of other dosage
forms (chewable tablet, suspension, sustained-release tablets and sustainedrelease capsules)
compared to the immediate-release tablet approaches 100%. If a patient is receiving a stable dose
of carbamazepine on one dosage form, the same total daily dose of another dosage form can
typically be substituted without adjustment. However, some bioequivalence problems have been
reported for generic carbamazepine products.
Usual initial maintenance doses are 10–20 mg/kg/d for children under 6 years of age, 200
mg/d for children 6–12 years old and 400 mg/d for adults. Twice daily dosing is initially used until
autoinduction takes place. Dosage increases to allow for autoinduction are made every 2–3 weeks
depending on response and adverse effects. Most adults will require 800–1200 mg/d of
carbamazepine while older children will require 400–800 mg/d. Although some minor side effects
occur, single loading doses of 8 mg/kg have been given to adults as suspension or immediate-
release tablets in order to achieve therapeutic concentrations within 2–4 hours after administration.
USE OF CARBAMAZEPINE SERUM CONCENTRATIONS TO ALTER DOSES
Because of the large amount of pharmacokinetic variability among patients, it is likely that
doses computed using patient population characteristics will not always produce carbamazepine
serum concentrations that are expected or desirable. Because of pharmacokinetic variability, the
autoinduction pharmacokinetics followed by the drug, the narrow therapeutic index of
carbamazepine and the desire to avoid adverse side effects of carbamazepine, measurement of
carbamazepine serum concentrations is conducted for almost all patients to ensure that therapeutic,
nontoxic levels are present. In addition to carbamazepine serum concentrations, important patient
parameters (seizure frequency, potential carbamazepine side effects, etc.) should be followed to
confirm that the patient is responding to treatment and not developing adverse drug reactions.
When carbamazepine serum concentrations are measured in patients and a dosage change is
necessary, clinicians should seek to use the simplest, most straightforward method available to
determine a dose that will provide safe and effective treatment.
Pseudolinear Pharmacokinetics Method
A simple, easy way to approximate new total serum concentrations after a dosage
adjustment with carbamazepine is to temporarily assume linear pharmacokinetics, then subtract
10–20% for a dosage increase or add 10–20% for a dosage decrease to account for autoinduction
pharmacokinetics: Cssnew = (Dnew / Dold)Cssold, where Cssnew is the expected steady-state
concentration from the new carbamazepine dose in μg/mL, Cssold is the measured steady-state
concentration from the old carbamazepine dose in μg/mL, Dnew is the new carbamazepine dose
to be prescribed in mg/d, and Dold is the currently prescribed carbamazepine dose in mg/d. Note:
This method is only intended to provide a rough approximation of the resulting carbamazepine
steady-state concentration after an appropriate dosage adjustment, such as 100–200 mg/d, has been
made. The pseudolinear pharmacokinetics method should never be used to compute a new dose
based on measured and desired carbamazepine concentrations.
You might also like
- Fast Facts: Ottimizzazione del trattamento delle fluttuazioni motorie nella malattia di ParkinsonFrom EverandFast Facts: Ottimizzazione del trattamento delle fluttuazioni motorie nella malattia di ParkinsonNo ratings yet
- Lec - No.12 (Carbamazipine)Document13 pagesLec - No.12 (Carbamazipine)phd0780No ratings yet
- Pharmacology of CNS: Prajogo Wibowo Faculty of Medicine Hang Tuah UniversityDocument37 pagesPharmacology of CNS: Prajogo Wibowo Faculty of Medicine Hang Tuah UniversityIda Bagus Putu SwabawaNo ratings yet
- TDM CarbazipineDocument4 pagesTDM CarbazipineMounika16 PedamalluNo ratings yet
- Clinical Use Utilizarea ClinicăDocument4 pagesClinical Use Utilizarea Clinicăsherylin4uNo ratings yet
- MEFENAMIC-ACID-mefenamic Acid Caps Ule Sciele Pharma IncDocument14 pagesMEFENAMIC-ACID-mefenamic Acid Caps Ule Sciele Pharma IncIrma DamayantiNo ratings yet
- Ramipril ProspectDocument18 pagesRamipril ProspectStefan Codrin CriclevitzNo ratings yet
- Analgesic: Mefenamic AcidDocument5 pagesAnalgesic: Mefenamic Acidmegazhang94No ratings yet
- Omeprazole: Losec 40 MG Powder and Solvent For Solution For Injection CompositionDocument11 pagesOmeprazole: Losec 40 MG Powder and Solvent For Solution For Injection CompositionNadia AfifahNo ratings yet
- Lamivudine: in Vitro Studies Indicate That Zidovudine-Resistant Virus Isolates Can Become ZidovudineDocument7 pagesLamivudine: in Vitro Studies Indicate That Zidovudine-Resistant Virus Isolates Can Become ZidovudineKirtikrushna Suresh Prasad OjhaNo ratings yet
- HW3 PharmacologyDocument8 pagesHW3 PharmacologyMICHAEL GABRIEL JIMENEZNo ratings yet
- S 025 LBLDocument16 pagesS 025 LBLarmanNo ratings yet
- Summary of Product Characteristics: For A Full List of Excipients, See Section 6.1Document17 pagesSummary of Product Characteristics: For A Full List of Excipients, See Section 6.1umarn1582No ratings yet
- Farmako PDFDocument16 pagesFarmako PDFIsney HanindyaNo ratings yet
- Mefenamic Acid Capsules, USP 250 MG RX Only: Reference ID: 3928117Document20 pagesMefenamic Acid Capsules, USP 250 MG RX Only: Reference ID: 3928117Riska AuliahNo ratings yet
- 15 NG - PPH Algorithm-Aug08Document8 pages15 NG - PPH Algorithm-Aug08Nurkholis AminNo ratings yet
- CarbamazepinaDocument15 pagesCarbamazepinaNataliaPalacínBernalNo ratings yet
- Pharmacokinetic Variability of Newer Antiepileptic Drugs: When Is Monitoring Needed?Document16 pagesPharmacokinetic Variability of Newer Antiepileptic Drugs: When Is Monitoring Needed?cvetinovic_vNo ratings yet
- SPC Pramipexole 0.7 MGDocument14 pagesSPC Pramipexole 0.7 MGJehan SarahdiniNo ratings yet
- Notes 1Document24 pagesNotes 1coosa liquorsNo ratings yet
- Anticonvulsant: Class A Group 6Document37 pagesAnticonvulsant: Class A Group 6Syahril TaminNo ratings yet
- Avelumab 800 MGDocument9 pagesAvelumab 800 MGVlad CroitoruNo ratings yet
- Clinical Pharmacokinetics - Lect9 - AnticonvulsantDocument20 pagesClinical Pharmacokinetics - Lect9 - AnticonvulsantLaylaNo ratings yet
- AEDand LiverdiseaseDocument22 pagesAEDand LiverdiseaseEmir SmailbegovićNo ratings yet
- New Zealand Datasheet Details Omeprazole InjectionDocument9 pagesNew Zealand Datasheet Details Omeprazole InjectionYuzark GumintangNo ratings yet
- Antikonvulsan OkeDocument77 pagesAntikonvulsan OkeAci LusianaNo ratings yet
- Carbamazepine NotesDocument2 pagesCarbamazepine Notesammaramaryam6463No ratings yet
- Valproic AcidDocument15 pagesValproic AcidNadya PrafitaNo ratings yet
- Bipolar Disorders and Carbamazepine PharmacokinetiDocument5 pagesBipolar Disorders and Carbamazepine PharmacokinetiAgr YuroNo ratings yet
- MEFTAL P Suspension PIDocument10 pagesMEFTAL P Suspension PIpiyush patelNo ratings yet
- 10-Valproic AcidDocument49 pages10-Valproic AcidAli AmerNo ratings yet
- Chapter 2Document34 pagesChapter 2zaidhusam100% (2)
- Tishk International University: ApixabanDocument4 pagesTishk International University: ApixabanDyar MzafarNo ratings yet
- Trileptal: DescriptionDocument33 pagesTrileptal: DescriptionAdanies GonzalezNo ratings yet
- Iavt 03 I 2 PDocument3 pagesIavt 03 I 2 PAnastasia Lilian SuryajayaNo ratings yet
- Epi LepsiDocument29 pagesEpi LepsiGita SerafikaNo ratings yet
- L AsparaginaseDocument2 pagesL AsparaginaseBigBoostingNo ratings yet
- Drugs That Lower The Seizure Threshold: Andrew W HitchingsDocument10 pagesDrugs That Lower The Seizure Threshold: Andrew W HitchingsesraaNo ratings yet
- 3 s2.0 B9780123864543007053 MainDocument3 pages3 s2.0 B9780123864543007053 MainPeem PrinNo ratings yet
- EPIRUBICIN Ferron PharmaceuticalsDocument7 pagesEPIRUBICIN Ferron PharmaceuticalsHep PutNo ratings yet
- Candesartan RBX PIDocument14 pagesCandesartan RBX PIshadab0123No ratings yet
- Therapeutic Drug MonitoringDocument6 pagesTherapeutic Drug MonitoringEdi Uchiha SutarmantoNo ratings yet
- Anti ParkinsonismsDocument7 pagesAnti ParkinsonismsArslan SaeedNo ratings yet
- Bioavailability and Bioequivalence. Therapeutic Drug MonitoringDocument3 pagesBioavailability and Bioequivalence. Therapeutic Drug MonitoringJoel MathewNo ratings yet
- LercanidipineDocument8 pagesLercanidipineddandan_2No ratings yet
- PIIS1053077018310437Document5 pagesPIIS1053077018310437andi rahmatNo ratings yet
- PharmacologyDocument116 pagesPharmacologyvargheseNo ratings yet
- Bipolar Disorders and Carbamazepine PharmacokinetiDocument6 pagesBipolar Disorders and Carbamazepine PharmacokinetiluthfiahNo ratings yet
- Normopresan Product Characteristics SummaryDocument7 pagesNormopresan Product Characteristics SummaryasdwasdNo ratings yet
- 29880020: Antiepileptic Drugs in Critically Ill PatientsDocument12 pages29880020: Antiepileptic Drugs in Critically Ill PatientsEward Rod SalNo ratings yet
- Antihypertensive Drug InteractionsDocument8 pagesAntihypertensive Drug InteractionsNur AzimahNo ratings yet
- Regulatory Document2 EngDocument201 pagesRegulatory Document2 EngDomenico LombardiniNo ratings yet
- Levetiracetam Therapy for Seizures: Mechanism, Uses, MonitoringDocument5 pagesLevetiracetam Therapy for Seizures: Mechanism, Uses, MonitoringChrisNo ratings yet
- DI Query - 3Document5 pagesDI Query - 3uneesolutionsNo ratings yet
- Amlodipine-10mg TabletDocument7 pagesAmlodipine-10mg TabletMd. Abdur RahmanNo ratings yet
- Zebinix Epar Product Information - enDocument169 pagesZebinix Epar Product Information - enAlobrixinvestigaçom InvestigaçomNo ratings yet
- Vesanoid (Tretinoin) Capsules R Only Warnings 1. Experienced Physician and InstitutionDocument14 pagesVesanoid (Tretinoin) Capsules R Only Warnings 1. Experienced Physician and InstitutionArun GargNo ratings yet
- Epilepsy Drug Classification and New Drugs in DevelopmentDocument10 pagesEpilepsy Drug Classification and New Drugs in DevelopmentSeshadri Sekhar ChatterjeeNo ratings yet
- Clexane and Clexane Forte : Name of The MedicineDocument20 pagesClexane and Clexane Forte : Name of The MedicineMarin MarianNo ratings yet
- Alkeran®: (Melphalan) TabletsDocument8 pagesAlkeran®: (Melphalan) Tabletskaren rodriguezNo ratings yet
- SMF Update Barang 03 Oktober 2022Document52 pagesSMF Update Barang 03 Oktober 2022Apotek Ibnu RusydNo ratings yet
- Daftar Harga 2021 FahrenheitDocument5 pagesDaftar Harga 2021 FahrenheitIrsan SyarifuddinNo ratings yet
- Inventv 2022Document21 pagesInventv 2022Din DinNo ratings yet
- Presentation CYP450 by Snehasis JanaDocument13 pagesPresentation CYP450 by Snehasis JanaSnehasis JanaNo ratings yet
- Slow Fast Moving ItemsDocument34 pagesSlow Fast Moving Itemshirairfan990No ratings yet
- Acceptable Prescribing Terms and Abbreviations PosterDocument1 pageAcceptable Prescribing Terms and Abbreviations PosterAdelNo ratings yet
- Autocoids 1Document9 pagesAutocoids 1Rutwik YNo ratings yet
- Diabetesmeds AcceptablecombDocument2 pagesDiabetesmeds AcceptablecombCotton LogicNo ratings yet
- ProductsDocument106 pagesProductsbochieng404No ratings yet
- Annex 1 SM and BS With Refs ListsDocument5 pagesAnnex 1 SM and BS With Refs ListsAjmal SeemabNo ratings yet
- Wesleyan Nursing Drug StudyDocument3 pagesWesleyan Nursing Drug StudyIrish SupanNo ratings yet
- OBAT YANG MENDEKATI EXPIRE DATE 2021Document2 pagesOBAT YANG MENDEKATI EXPIRE DATE 2021vicki yugasworoNo ratings yet
- Adult Parenteral Guidelines 2020Document57 pagesAdult Parenteral Guidelines 2020Sara Aly YoussefNo ratings yet
- Daftar Obat High Alert Dan Lasa PKM Sendang AgungDocument3 pagesDaftar Obat High Alert Dan Lasa PKM Sendang AgungDian PutraNo ratings yet
- Borang CP3Document2 pagesBorang CP3farmasi.ketengahjayaNo ratings yet
- CNS Stimulant 2022 - Stu.Document39 pagesCNS Stimulant 2022 - Stu.Eltaib Mohamad 2427No ratings yet
- Label Box ObatDocument145 pagesLabel Box ObatIrwandi SuhermanNo ratings yet
- Exel So Desember 2021 10 Januari 2022Document279 pagesExel So Desember 2021 10 Januari 2022Ani Nur RohmaNo ratings yet
- Form 3 DDD 2022Document16 pagesForm 3 DDD 2022Miranti SastraningrumNo ratings yet
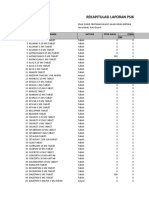
- Rekapitulasi Laporan Psikotropika: NO Nama Satuan Stok Awal Pemasukan PBFDocument9 pagesRekapitulasi Laporan Psikotropika: NO Nama Satuan Stok Awal Pemasukan PBFlarasNo ratings yet
- KetamineDocument5 pagesKetamineapi-142637023No ratings yet
- WWW Globalrph Com Narcotic HTMDocument5 pagesWWW Globalrph Com Narcotic HTMroooNo ratings yet
- Drug StudyDocument3 pagesDrug StudyMary rose PidoNo ratings yet
- Dosage: 50 MG Order: PRN q6h Route: IV (Case Scenario Based)Document3 pagesDosage: 50 MG Order: PRN q6h Route: IV (Case Scenario Based)Edward Luis EsguerraNo ratings yet
- TRAMADOLDocument4 pagesTRAMADOLRudie Lee PascualNo ratings yet
- Multiple Choice Question - Pharmacotherapy of EpilepsyDocument2 pagesMultiple Choice Question - Pharmacotherapy of EpilepsyChaitanya MungaseNo ratings yet
- NCLEX PharmacologyDocument51 pagesNCLEX PharmacologyJan Mitchelle100% (2)
- Is Doa 10 Cup TestDocument1 pageIs Doa 10 Cup TestUqi.No ratings yet
- DRUG 6 CognexDocument4 pagesDRUG 6 CognexMora MokhlesNo ratings yet
- Top 5 Anadrol Cycles For Huge Muscle GainsDocument1 pageTop 5 Anadrol Cycles For Huge Muscle GainsKinan KholandiNo ratings yet