Professional Documents
Culture Documents
DOPS As WPBA
Uploaded by
Hafsa AamirOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
DOPS As WPBA
Uploaded by
Hafsa AamirCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/315125385
Faculty Development: DOPS as Workplace-Based Assessment
Article · June 2011
DOI: 10.5959/eimj.3.1.2011.or4
CITATIONS READS
9 753
1 author:
Shahid Hassan
International Medical University (IMU)
19 PUBLICATIONS 66 CITATIONS
SEE PROFILE
All content following this page was uploaded by Shahid Hassan on 12 August 2017.
The user has requested enhancement of the downloaded file.
Faculty Development: DOPS as Workplace-Based Assessment, Education in Medicine Journal, 2011, Vol.3 (1); e32-43
doi:10.5959/eimj.3.1.2011.or4
ORIGINAL ARTICLE
Faculty Development: DOPS as Workplace-Based Assessment
Shahid Hassan
Department of Medical Education/ORL-HNS, School of Medical Sciences, Universiti Sains Malaysia
Abstract
Background: In order to achieve the desired performance of graduates a number of traditional
evaluation exercises have been practiced to assess their competence as medical students. Many of
these assessments are done in a controlled environment and mostly reflect on tests of competence
than performance. Mini-CEX or direct observed procedural skills (DOPS) are the real performance-
based assessment of clinical skills. Increased opportunity for observation and just-in-time feedback
from the role model superiors produce a positive educational impact on students learning. This also
provides trainees with formative assessment to monitor their learning objectives. However, to
implement assessment strategies with Mini-CEX or DOPS needs to develop institution’s clear policy
for a different teaching and learning culture of workplace based assessment. It also needs to develop
user friendly rating form, checklist, elaboration of clinical competence and its attributes and
procedural guidelines for practice. A precise role of these tools in the assessment of postgraduate
program must be established before practicing them to evaluate and monitor trainee’s progress.
Objective: To determine DOPS for its acceptability and feasibility as a method of formative
assessment of clinical skills in postgraduate program of Otolaryngology and Head-Neck Surgery.
Method: A total of 25 trainees were assessed for DOPS by 8 supervisors in this 12-weeks pilot study. A
faculty development program for faculty members and trainees was run for DOPS. Trainees were
advised to undertake at least one DOPS encounter out of 42 shortlisted procedures. Assessors were
asked to mark trainees by completing a rating form using a checklist developed for each procedure.
Trainees and assessors were asked to endorse their opinion on feasibility and acceptance of DOPS for
practice of formative assessment in future. Data was analyzed to determine feasibility and
acceptability of DOPS in assessment program.
Result: Faculty development and trainees orientation in DOPS were found satisfactory for its
acceptance and feasible for its practice. Trainees were mostly assessed in outpatient clinical setting.
Majority reported higher rating of satisfaction by assessors and trainees. Among clinical skills higher
rating was received in procedural skills performed by the senior trainees.
Conclusion: DOPS was found feasible for practice of formative assessment of trainees in
postgraduate program of Otolaryngology and Head-Neck Surgery in School of Medical Sciences
(SMS) at Universiti Sains Malaysia (USM). It was well accepted by the trainees to help monitor their
quality of procedural skills as self-directed learning.
Keywords: DOPS, Faculty Development, Postgraduate, Workplace-Based Assessment,
Otorhinolaryngology, Head and Neck, Surgery
Education in Medicine Journal (ISSN 2180-1932) © www.saifulbahri.com/eimj | e32
Faculty Development: DOPS as Workplace-Based Assessment, Education in Medicine Journal, 2011, Vol.3 (1); e32-43
doi:10.5959/eimj.3.1.2011.or4
Introduction assessment is its ability to evaluate
performance in context (4)
Training in medicine traditionally follows an
apprenticeship model after the graduation Assessment is inseparable from learning and
and this has long being practiced. Formal so is the relationship between educational
supervisor and the trainee. Primary purpose
assessment in medical education mostly is
of WPBA is to promote learning and this
testing of knowledge with clinical and relationship (6). Efforts of WPBA are to
practical skills as components of those formal develop common standard and common
examinations. The assessment of clinical processes as assessment instrument
performance in medicine is important but employed at workplace. Workplace based
instrument aims at identifying areas for
challenging. Historically, assessments
improvement of formative assessment. A
have been implicit, unstandardised, and recently published guideline for the
based on holistic or subjective judgments implementation of workplace-based
in the apprenticeship model (1). Recent assessment emphasizes the importance of
using such tools as assessments for learning
reforms in postgraduate medical
rather than solely as assessments of learning
education have brought new systems for (5). WPBA as innovative assessment must be
the assessment of competence and well cleared for its purpose to both trainees
performance, workplace-based assessment and assessors. Institution need to have a clear
plan to approach and develop WPBA, which is
(WPBA) is one of these systems (2).
perceived well and acceptable to majority
Assessment of performance at workplace in faculty members. Trained and multiple
medicine has been informal, anecdotal and assessors with multiple encounters are
rarely documented. Knowledge-based needed to judge the procedures. All assessors
assessment is well established and practiced must be trained to improve the standard of
with major investment in infrastructure and WPBA delivery. Role of supervisors must be
resources of institution, either denying or well defined in term of clinical supervisor and
being less focused towards the workplace- educational supervisor (6). Training
based assessments (WPBA) in their setup. excellence must be recognized and rewarded
Performance-based training in postgraduate to encourage faculty for their positive efforts.
medicine needs suitable new assessment
methods as quality improvement model to As the work place based assessment in
promote excellence in practice. Postgraduate clinical skills is possible through mini clinical
medical training as apprenticeship learning evaluation exercise (Mini-CEX), the practical
has more opportunity to assess trainees in assessment of skills at workplace is also
the workplace simply because, workplace possible as direct observed procedural skills
based assessment is an “assessment of what (DOPS). DOPS is developed by Royal College
doctors actually do in practice” (3). of Physicians London (6). It is a variation on
Introducing WPBA takes time, resources and Mini-CEX to assess the practical (procedural)
requires change in culture acceptable to skills (7). Practical skills are usually assessed
faculty members. Although many forms of through log books recording the number of
assessment can be used to show a doctor’s procedures and the complication rates with
knowledge of competence, there is evidence or without the feedback provided to trainees
that competence does not reliably predict in program. DOPS is the observation of
performance in clinical practice and one clinical procedures performed by trainees,
major advantage of workplace-based which is more objective and structured
Education in Medicine Journal (ISSN 2180-1932) © www.saifulbahri.com/eimj |
e33
Faculty Development: DOPS as Workplace-Based Assessment, Education in Medicine Journal, 2011, Vol.3 (1); e32-43
doi:10.5959/eimj.3.1.2011.or4
assessment of competence. Procedure feature of DOPS however, quality of feedback
though vary with the specialty and level of directly depend on assessor’s expertise and
expertise of the trainees, each discipline time provided for feedback. Only 40% trainee
select the number of required procedures found feedback from DOPS helpful and this
essential to be performed by the trainees. reflects on lack of assessors training and time
Assessor and trainee mutually agree that available for assessment (11). DOPS as an
encounter to be assessed and the patient observation of clinical procedures performed
must be informed and consented for by trainees is more objective and structured
encounter to be assessed. Time for DOPS assessment of procedural skills. DOPS is
encounter varies with type of procedure and feasible to adopt and is reliable and valid with
normally 15 minutes are allocated for multiple observations and multiple observers
observing one procedure. Each encounter is as assessors. Institutions need to have a clear
followed by feedback to suggest plan for development of WPBA in general and
improvement and this should take 20%-30% DOPS in particular to achieve good level of
of observation time (8). Global rating of 1-9 acceptance of this approach by the faculty.
observed for primary procedural skills. However, DOPS cannot be used for complex
Associated components of clinical procedure surgical procedures due to time constraints of
also observe trainees performance in assessment. Increased opportunity for
communication skills, attitude towards observation and immediate feedback from
patient and their organizational skills as pre- the trained supervisors produces a positive
procedure analgesia and post- procedure educational impact on resident’s learning.
management. Demonstration of growth in various
procedural skills compared through scores of
DOPS is relatively new instrument and there evaluation performed periodically in training
is limited published data on utility. However, supports the validity of this method. A pilot
as a variation on the Mini-CEX study showing study on DOPS showed evidence for construct
the validity of Mini-CEX may apply to DOPS as validity as more senior trainees received
well (9). DOPS result like Mini-CEX can be higher scores (8)
generalized and considered reliable with
generalisability coefficient 0.89 provided a
trainee is observed for each procedure by
three assessors for two encounters each to Material and Methods
achieve adequate reliability (6). High face
25 trainees from the 4 classes of Master of
validity is reported due to real clinical
Surgery Program in Otolaryngology and Head
encounter while good construct validity is
and Neck Surgery undertook DOPS encounters
established through senior trainees scoring
in July 2009 for a period of 12-week. Trainees
high (8). DOPS can be used as generic
were assessed for DOPS by 8 supervisors in this
assessment tool for procedural skills and the
pilot study. Prior to this a faculty development
procedure specific form may also be
program for DOPS was carried out through
developed as check list. Items may vary from
lectures deliberating on background, concept
10-12 with a 4-9 point scale as feasible (6).
and procedure of DOPS followed by
Reliable with good constraint validity DOPS is demonstrations of DOPS in own clinical
recommended for assessment of surgical environment. Students were also exposed to
training program such as ENT (10). Individual similar settings to take up the DOPS
DOPS assessment however, should not be a encounters without any hesitation in this 12
guarantee for independent practice (6). weeks faculty development program for direct
Instrument will be more reliable with multiple observed procedural skills.
observations and multiple observers.
Feedback like in Mini-CEX is the important
Education in Medicine Journal (ISSN 2180-1932) |
© www.saifulbahri.com/eimj
e34
Faculty Development: DOPS as Workplace-Based Assessment, Education in Medicine Journal, 2011, Vol.3 (1); e32-43
doi:10.5959/eimj.3.1.2011.or4
Introducing DOPS to faculty and trainees, the encounter to be assessed.
study aimed at evaluating DOPS for its 5. Time for DOPS encounter normally set is 15
feasibility and acceptability. After the faculty minutes followed by feedback as 20% -30% of
development every trainee was advised to observation time to suggest the improvement
undertake at least one DOPS encounter out of in procedural skills required
the shortlisted procedures that was later 6. Global rating of 1-9 observed for primary
developed to comprise of 42 skills procedures procedural skill (see appendix B).
representing all 4 sub-specialties. Assessors 7. Associated components of a primary clinical
using a rating form with global rating score of procedure also observed include
1-9 and a checklist for each procedure marked communication skills, approach to patient,
the trainees for their performance, which was pre-procedure analgesia and post- procedure
declared to be component of their formative management.
assessment. Trainees were assessed both in 8. To make instrument reliable multiple
outpatient clinical setting and operation observations and multiple observers
theater. At the end of the procedure trainees essentially are ensured.
and assessors were asked to give their opinion 9. High face/construct validities make DOPS a
by direct endorsement for feasibility and reliable instrument for assessing skills is
acceptability of DOPS for the future practice of established from the literature (8).
formative assessment on a rating scale of 1-9 10. One or two peers were also allowed in
to decide on DOPS as a workplace-based each encounter as a modification to classical
measurement tool to be employed in 4 years method in order to expose the candidates to
program of Master’s of Otolaryngology and DOPS before actually undertaking the
Head-Neck Surgery. Besides, assessors were encounter.
also requested to develop checklists of
procedures shortlisted for DOPS during this 12
weeks study period. Data was analyzed to
determine supervisors and trainees willingness Result
to adopt DOPS besides, Mini-CEX as one of the
25 trainees and 8 faculty members from 4
component measurement tools in future
subspecialties of ORL-HNS discipline
formative assessment program of
participated in this study (see table 1). Faculty
postgraduate medical education in SMS, USM.
development and trainees orientation in DOPS
How do we do it? were found acceptable (see table 2) and
feasible (see table 3) by majority of the
Example below demonstrates the steps of participants for its adoption in practice of
DOPS performed as an office procedure (see formative assessment of the postgraduate
figures 1 and 2) trainees in ORL-HNS training.
1. A number of required core procedures Among clinical skill procedures higher rating
essential to be performed by trainees are was reported in procedural skills performed by
selected (see appendix A) the senior trainees compared to their junior
2. A procedure specific rating form (see colleagues (see table 2). Faculty development
appendix B) and checklist (see appendix C) for for DOPS resulted in organization of additional
the observers are prepared. 21 checklists of finally 42 shortlisted DOPS
3. Assessor and trainee mutually agree for core procedural skills in various sub-specialties
encounter to be assessed. of Otolaryngology and Head-Neck Surgery.
4. Patient is informed and consented for
Education in Medicine Journal (ISSN 2180-1932) |
© www.saifulbahri.com/eimj
e35
Faculty Development: DOPS as Workplace-Based Assessment, Education in Medicine Journal, 2011, Vol.3 (1); e32-43
doi:10.5959/eimj.3.1.2011.or4
Figure 1: Illustrating the real steps of DOPS performed as an office procedure in a surgical
skill of taking biopsy from the nose and observed by a checklist and marked by a rating
form by an assessor. Note a peer observing the procedure.
Figure 2: Illustrating the further steps of DOPS observed by a checklist to provide feedback on
performance by demonstration of one of the steps and after procedure assurance of
reexamination of site of biopsy.
Education in Medicine Journal (ISSN 2180-1932) |
© www.saifulbahri.com/eimj
e36
Faculty Development: DOPS as Workplace-Based Assessment, Education in Medicine Journal, 2011, Vol.3 (1); e32-43
doi:10.5959/eimj.3.1.2011.or4
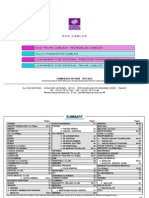
Table 1: Number of trainees versus supervisors and their sub-specialty developed for DOPS
Trainees trained with No of Subspecialties Supervisors trained with DOPS
DOPS (Total No 25) (Total = 4) (Total No 12)
Year Numbers No Sub-specialty Sub-specialty Numbers
I 7 1 Otology Otology 1
II 5 2 Rhinology Rhinology 2
III 5 3 HNS HNS 4
IV 2 4 Pediatric ORL Pediatric. ORL 1
Table 2: Supervisor’s versus trainee’s level of satisfaction and the trainees reported mean
score
No Sub-Specialty Supervisor’s level Trainee’s level of Year of training
of satisfaction satisfaction Vs. mean scores
1 Pediatric ORL Range 6 -9 Range 6-8 Year I - 6.5
2 H & N Surgery Range 8-9 Range 8-9 Year II- 7.2
3 Otology Range 7-9 Range 7-9 Year III- 7.5
4 Rhinology Range 8-9 Range 8-9 Year IV- 8.5
Table 3: Range of supervisor’s versus trainee’s feasibility scores and the number prepared
checklists as per sub-specialty.
No Sub-Specialty Supervisor’s Trainee’s Checklists
feasibility score feasibility score Developed
1 Pediatric ORL Range 7 -9 Range 6-7 2
2 H & N Surgery Range 8-9 Range 7-8 10
3 Otology Range 6-7 Range 7-9 5
4 Rhinology Range 8-9 Range 6-9 4
Education in Medicine Journal (ISSN 2180-1932) © www.saifulbahri.com/eimj|
e37
Faculty Development: DOPS as Workplace-Based Assessment, Education in Medicine Journal, 2011, Vol.3 (1); e32-43
doi:10.5959/eimj.3.1.2011.or4
Discussion emergency or routine operation theater setting
is the preferably chosen task for work place
Most of the traditional assessments e.g. OSCE, based assessment. More complex time
long and short cases with simulated or consuming surgical procedures are not feasible
standardized patients or for that matter real for evaluation through WPBA as a time-bar
patients are all done in a controlled procedures. Other alternate methods for
environment (12). A workplace-based assessment of complex surgical procedures
assessment (WPBA) as direct observed should be explored. Protocol to develop DOPS
procedural skills (DOPS) is within the scope of must follow the general principles of any WPBA
practice for formative assessment however, its as under.
implementation necessarily needs consent and
consensus of faculty, educators and hierarchy of A DOPS rating form should be established with
the institution. Assessment should move from consensus of clinical faculty, educators and
use of numerical value to standard-expected in hierarchy of the institution (13). Educational
procedural skills to gathering of qualitative and the clinical supervisor’s role as teacher
information in decision-making. However, the development in program must clearly be
WPBA instrument designed must be reliable, defined (6). Process of DOPS as a WPBA should
valid and feasible within the resources available intend to be trainee-led and trainees should
in clinical practice (4). Instrument must be rather be allowed to fix the time of undertaking
consistent with training program and attributes DOPS. ORL-HNS Discipline practices DOPS with
of different specialties. DOPS is performed in a this freedom for trainees who are advised to
real clinical situation. Increased opportunity for practice the procedure several times before
observation and just-in-time feedback from the approaching the clinical supervisor to assess
supervising role models in DOPS produces them. Adequate observation time must be
positive educational impact on student’s allowed to complete the assessment effectively
learning. This also provides trainees with and quality feedback process must be ensured
formative assessment to monitor their learning with each DOPS to stimulate a change in
objectives (4). However, to implement practice.
assessment strategies in DOPS, institution needs
to develop clear policy for a different teaching A list to identify core procedural skills is the
and learning culture of workplace based next requirement to be done by the faculty for
assessment. It also needs to develop user DOPS evaluation of postgraduate trainees and
friendly rating form and the checklist, this was achieved in Master’s of Surgery
elaboration of clinical competence and its Program of Otorhinolaryngology and Head-
attributes (see appendices A, B and C), Neck Surgery (see appendix A). Most of these
procedural guidelines for practice and the procedures are the one that can be performed
precise role of these tools in assessment of the as an office procedure. Some minor to medium
postgraduate program practiced to evaluate and operative procedures are also included (see
monitor trainee’s progress (13). Evidence-based appendix A), however in view of the patient’s
aspect of this study on faculty development for safety those procedures are ensured close
DOPS is the 21 checklists of various procedural supervision with just-on time information and
skills developed out of 42 core clinical support as instructional feedback. A rating form
procedures (see appendix A) identified by the modified form one practiced in Royal College of
teaching faculty of Department of Medicine U.K. and a checklist for each
Otolaryngology and Head-Neck Surgery . procedure has been developed keeping in view
the indigenous socio-cultural values (see
DOPS as a WPBA is time constraint evaluation appendices B and C). All such procedures to be
of trainee’s performance designed to assess done by a trainee must also conform to his level
some minor to medium practical skills often of training (see the footnote in appendix A). In
those performed as office procedures. Less a subsequent practice of DOPS trainees were
complex surgical procedures in clinic, ward, asked to pick up a minimum 7 procedures per
Education in Medicine Journal (ISSN 2180-1932) © www.saifulbahri.com/eimj | e38
Faculty Development: DOPS as Workplace-Based Assessment, Education in Medicine Journal, 2011, Vol.3 (1); e32-43
doi:10.5959/eimj.3.1.2011.or4
year out of 42 core procedural skills to patient’s opinion) while procedure was
complete 28 DOPS encounters in 4 years of performed. We found patient’s feedback as
Master of Surgery Program in ORL-HNS. authentic, realistic and relevant to judge
Procedures were allowed to be repeated with trainee’s organizational efficiency, humanistic
the previous or a new supervisor if more qualities and professionalism gauging his
feedback or feedback with a different assessor overall competence.
is desired. The core procedural skills are
distributed over five subspecialties and general Fourth modification was to allow the
otolaryngology (see appendix A). demonstration of competence by trainees in
DOPS rather, using simulation techniques in
DOPS practiced in ORL-HNS Discipline were special situations where performance based
subjected to certain modifications to optimize techniques with real patients were less likely to
learning from this assessment, experienced as be achieved on time however, and such
part of educational strategy. However, these assessments were performed in workplace. This
adjustments were in keeping with principles of is to compensate for real WPBA of some of
learning and teaching. These modifications those procedural skills difficult to achieve in
were brought to enhance the educational postgraduate training in practice. Learning and
impact of postgraduate learning environment in assessing through simulated and standardized
School of Medical Sciences at Universiti Sains patients (SP) helps a trainee in building his
Malaysia. confidence for subsequent handling of real
patients. Training with SP is not only relaxing
First modification practiced is the mandatory but it also allows mistakes and repetition of
probing questions to be asked on skills skills as many times as it may occur. It adds to
encompassing indications, anatomy, trainee’s experience prior to a real encounter.
pathophysiology and complications of However, we must not forget the fact that
procedure as a test of theoretical knowledge DOPS is the assessment of performance in a
and its application to help assess the overall real life clinical situation.
performance of the trainee in a particular
practical skill. Second modification was to allow
one or two peers to attend the encounter of
DOPS. Presence of a second trainee in Conclusion
encounter helps to inculcate the culture of peer
DOPS was found acceptable and feasible for
learning among the students by observing the
formative assessment of postgraduate training
peer’s performance and giving feedback to each
in ORL-HNS. Practice of DOPS provided the
other at their mutual convenience. We found
means to supervisors and to incentives to
that learning through mutual observation is
trainees to monitor their self-directed learning
relaxing, promptly acceptable and friendly
objectives and to improve quality of procedural
among peers and it also provides opportunities
skills acquired during their on-job
for feedback. Third modification was to invite
(apprenticeship) learning in clinical education.
patient’s feedback immediately after the
DOPS to be effective as an assessment tool
encounter in which patient’s trained for this
needs regular appraisal, clear learning goals and
role were available. However to do that one
supervisor’s dual role as teacher and assessors.
must ensure that patient is adequately
High rating of satisfaction by assessors and the
educated and can easily be trained for a quick
trainees reported in this study suggest faculty
feedback on trainee’s communication skills
and trainee’s readiness to adapt DOPS as WPBA
(introducing himself to patient and taking his or
in formative assessment. However, looking
her consent for the procedure), patient’s
forward to DOPS as a method in summative
comfort (care taken to avoid pain or distress
assessment remains challenging. Nevertheless
during the procedure) and trainee’s confidence
it can be considered a step forward to building
(organization and adequate clinical skill in
up program for assessment with triangulation
Education in Medicine Journal (ISSN 2180-1932) © www.saifulbahri.com/eimj | e39
Faculty Development: DOPS as Workplace-Based Assessment, Education in Medicine Journal, 2011, Vol.3 (1); e32-43
doi:10.5959/eimj.3.1.2011.or4
of measurement tools in a standard – setting www.aomrc.org.uk/Improving Assessment.
strategy that values qualitative information in
decision-making of postgraduate medical 7. Wragg A, Wade W, Fuller G, Cowan G, Mills P.
education assessment. Assessing the performance of specialist registrars.
Clinical Medicine 2003; 3(2): 131-134.
References 8. Wilkinson JR, Crossley JGM, Wragg A, Mills P, Cowan
G, Wade W. Implementing workplace-based
1. Van der Vleuten CPM. The assessment of assessment across the medical specialties in the
professional competence: development, United Kingdom. Med Educ 2008; 42(4):364-373.
research and practical implications. Adv Health
Sci Educ 1996; 1:41-67. 9. Goff BA, Lentz GM, Lee D, Houmard B, Mandel LS.
Development of an objective structured assessment of
2. Scheele F, Teunissen P, Van Luijk S, technical skills for obstetric and gynecology residents.
Heineman E, Fluit L, Mulder H, et al. Introducing acogjnl 2000; 96(1): 146-150.
competency based postgraduate medical
education in the Netherlands. Med Teach 2008; 10. Roberson DW, Kentala E, Forbes P. Development
30:248-53. and validation of an objective instrument to measure
surgical performance at tonsillectomy. Laryngoscope
3. Swanwick T, Chana N. Workplace-based 2005; 115(12): 2127-2137.
assessment. Br J Hosp Med (Lond) 2009;
70:290-3. 11. Smith D, Riley S, Kazmierczak A, Aitken M, Paice E,
Le Rolland P. National Survey of Trainees 2007.
4. Miller A, Archer J., Impact of workplace Postgraduate Medical Education and Training Board
based assessment on doctors’ education and 2008 Available on line: URL:http:
performance: a systematic review. BMJ 2010; //www.pmetb.org.uk/fileadmin/user/QA/Trainee_Surv
341: c5064 doi: 10.1136/bmj.c5064 ey/National_Survey_of_Trainees_2007_ Summary.
Report_20080723-Final.pdf.
5. General Medical Council, Academy of
Medical Royal Colleges. Workplace based 12. Rennie SC, Mossey PA, Crosby JR. Structured
assessment: a guide for implementation. 2010. clinical operative tests: assessing invasive practical
702-14. www.gmc- procedures. Med Educ 2001; 35: 1066–1090.
uk.org/Workplace_Based_Assessment.
13. Hassan S. Clinical skills authentic learning with
6. General Medical Council, Academy of Royal workplace-based assessments. Kota Bharu: SARANA
Medical Colleges. Improving Assessment in Publishing, 2009.
Clinical and Procedural Skills: Direct
Observation of Procedural Skills: 2009; 26-27.
Corresponding Author: Associate Professor Dr Shahid Hassan, Medical Education/
Otorhinolaryngology Department, School of Medical Sciences, Universiti Sains Malaysia, Kubang
Kerian, 16150 Kota Bharu, Kelantan, Malaysia.
Email: shahid@kb.usm.my, gorshahi@yahoo.com
Accepted: June 2011 Published: June 2011
Education in Medicine Journal (ISSN 2180-1932) © www.saifulbahri.com/eimj | e40
Faculty Development: DOPS as Workplace-Based Assessment, Education in Medicine Journal, 2011, Vol.3 (1); e32-e43
Appendix A: Core procedural skills identified by ORL-HNS faculty for the DOPS evaluation of
postgraduates in Master’s of Surgery in Otolaryngology-Head & Neck Surgery. Out of these a checklist
of 21 procedures were developed during the 12 weeks faculty development program in DOPS.
NO PROCEDURAL SKILLS NO PROCEDURAL SKILLS
1 Tuning fork test 22 Incision drainage quinsy
2 Aural toilet by syringing 23 Incision drainage abscess neck
3 Mastoid dressing 24 Lymph node excision biopsy
4 Myringotomy/insertion of grummet 25 Incision biopsy of a neck mass
5 Removal foreign body ear 26 Post nasal space biopsy for NPC
6 Pure tone audiometry 27 Excision thyroglossal duct cyst
7 Impedance audiometry 28 Esophagoscopy
8 Removal foreign body nose 29 Indirect laryngoscopy (IDL)
9 Posterior rhinoscopy 30 Rigid endoscopic examination of larynx
10 Nasopharyngoscopy 31 Stroboscopy
11 Intranasal biopsy of mass nose 32 Direct laryngoscopy (DL) / biopsy
12 Sub-mucous diathermy of turbinate 33 Bronchoscopy
13 Anterior nasal packing 34 Insertion of nasogastric tube
14 Posterior nasal packing 35 E. T. Intubation/extubation
15 Antrum washout 36 Tracheostomy as elective procedure
16 Intra nasal pollectomy 37 Fine needle aspiration cytology
17 Reducing fracture nasal bone 38 Tissue for frozen section microscopy
18 Nasal smear cytology 39 Drawing venous blood
19 Skin allergy test 40 Drawing arterial blood
20 Adenoidectomy 41 Applying surgical knots
21 Tonsillectomy on one side 42 Interrupted, mattress sutures
Note: Keeping patient’s safety in view procedures are labeled for performance of trainees for level of
their training in postgraduate program of Master’s of Surgery in Otolaryngology-Head & Neck Surgery
as follows: 1. For year III and IV trainees only, 2. For year II and above only, 3. For any level of
training.
Education in Medicine Journal (ISSN 2180-1932) © www.saifulbahri.com/eimj | e41
Faculty Development: DOPS as Workplace-Based Assessment, Education in Medicine Journal, 2011, Vol.3 (1); e32-e43
Appendix B: Direct observation of procedural skills (DOPS) rating form developed for the assessment
of ORL-HNS practical skills, modified from GMC ST Version used in Anaesthesia.
Personal Data Date: Pleas complete the questions using sign
Trainee’s Name
Matric Number Year of training Year / Phase
Assessor’s Name
Assessor’s training Face to face Read guidelines Course Web/CD
Assessor’s Position Professor Associate Professor Senior Lecturer
Procedure Taking a biopsy from the nose as an office procedure
Clinical Setting O.P. Clinic A&E Ward Theater Skills Center
Case Category Scheduled Urgent Emergency Simulated
Number of times DOPS observed by assessor 0 1 2-5 5-10
Number of times procedure performed by trainee 0 1-4 5-9 >9
Please grade the Unsatisfactory Borderline Satisfactory Superior Excellent
following areas of 1 2 3 4 5 6 7 8 9
performance
1. Has knowledge of
indications and
relevant anatomy
2. Takes the informed
consent
3. Demonstrates the
preoperative
measures
4. Observe the
aseptic measures
5. Hass awareness
about the situation
6. Demonstrates
technical skill
7. Seeks the help
where appropriate
8. Demonstrate post
procedure
9. Communication
skills
10. Demonstrates
patient care
11. Over all ability to
perform procedure
Education in Medicine Journal (ISSN 2180-1932) © www.saifulbahri.com/eimj | e42
Faculty Development: DOPS as Workplace-Based Assessment, Education in Medicine Journal, 2011, Vol.3 (1); e32-e43
Appendix C: Checklist developed for individual procedure is essential for standardized rating of
DOPS. Space provided in this form to record strengths and weaknesses can also be used separate
than the checklist here.
Time taken for observation _____ minutes Time taken for feedback ______ minutes
Trainee’s satisfaction with DOPS Not at all High
1 2 3 4 5 6 7 8 9 10
Assessor’s satisfaction with DOPS Not at all High
1 2 3 4 5 6 7 8 9 10
Assessor’s signature Trainee’s
signature
Please record areas of strengths and weaknesses as well as suggestions to improve
No Checklist of procedure stated in rating form to assess trainee’s performance
1 Introducing yourself to patient, giving the information about the procedure and taking
consent to obtain the biopsy from nose under local anesthesia
2 Wearing on the gloves, examining the nose alternatively with 00 and 300 rigid endoscope
for any anatomical variation and nature of lesion. Possible site for biopsy is also decided
at this point.
3 Placing the cotton wicks soaked in cocain in middle meatus around the lesion after
explaining the step to patient and waiting for 3-5 minutes before taking the biopsy
4 Introducing a sterile punched forceps along with 00 endoscope the site on lesion earlier
selected for biopsy is reached and held with the punched forceps and pulled the tissue
with a jerk and immediately placed in a bottle containing formalin solution. One more
attempt after reassuring the patient made to obtain another bite with sufficient tissue
for histopathology. Cover place over the bottle immediately and labeled before sending
to lab.
5 Patient is informed once again about the completion of procedure and inquiring for any
pain before taking permission to reexamine the nose and the site of biopsy for possibility
of any bleeding.
6 Asking the patient to wait for another 10-15 minutes followed by re-examination before
allowing him to go home after ensuring no pain and post nasal bleeding
Education in Medicine Journal (ISSN 2180-1932) © www.saifulbahri.com/eimj | e43
View publication stats
You might also like
- Introducing Objective Structured Practical Examination As A Formative Assessment Tool For Phase I Medical Professionals in PhysiologyDocument6 pagesIntroducing Objective Structured Practical Examination As A Formative Assessment Tool For Phase I Medical Professionals in PhysiologyPramod JaliNo ratings yet
- Specific Program For EvaluationDocument9 pagesSpecific Program For EvaluationLOGESWARRY K.VESUPATHYNo ratings yet
- Workplace Based Assessment - Tools To Assess Competencies in A CliDocument6 pagesWorkplace Based Assessment - Tools To Assess Competencies in A CliDME LUMHSNo ratings yet
- A Survey On The Clinical Performance Evaluation of Operating Room Interns From The Perspective ofDocument6 pagesA Survey On The Clinical Performance Evaluation of Operating Room Interns From The Perspective ofAbigail GarciaNo ratings yet
- Work Base Assessment in Anesthesia For Postgraduate ResidentsDocument4 pagesWork Base Assessment in Anesthesia For Postgraduate ResidentsMJSPNo ratings yet
- 6.+61863 47-56Document10 pages6.+61863 47-56Dwi NopriyantoNo ratings yet
- Estudio Cualitativo Del Portafolio Que Explora Las Recomendaciones de Los Funcionarios ResponsablesDocument9 pagesEstudio Cualitativo Del Portafolio Que Explora Las Recomendaciones de Los Funcionarios ResponsablesFalconSerfinNo ratings yet
- Utility of Work Based Assessment Among Surgical Residents: A Systematic Literature ReviewDocument8 pagesUtility of Work Based Assessment Among Surgical Residents: A Systematic Literature ReviewUsama AzizNo ratings yet
- ojsadmin,+4Document6 pagesojsadmin,+4Suhad HasanNo ratings yet
- Core Principles of Assessment in Competency Based Medical EducationDocument9 pagesCore Principles of Assessment in Competency Based Medical EducationJasmik SinghNo ratings yet
- Procedure-Based Assessments in Trauma and Orthopaedic Training - The Trainees' PerspectiveDocument6 pagesProcedure-Based Assessments in Trauma and Orthopaedic Training - The Trainees' PerspectiveSaleh MuzaniNo ratings yet
- Medical Students' Competency MilestonesDocument12 pagesMedical Students' Competency MilestonesWordtreader PtNo ratings yet
- Online 83300003Document11 pagesOnline 83300003Anonymous dRAu54No ratings yet
- Using Portfolios To Assess Professional CompetenceDocument3 pagesUsing Portfolios To Assess Professional CompetenceJunaid AhmadNo ratings yet
- Objective Structured Practical Examination/objective Structured Clinical Examination As Assessment Tool: Faculty PerceptionDocument4 pagesObjective Structured Practical Examination/objective Structured Clinical Examination As Assessment Tool: Faculty PerceptionHarshita arora100% (1)
- Impact and Effectiveness of A Mandatory Competency-Based Simulation Program For Pediatric Emergency Medicine FacultyDocument10 pagesImpact and Effectiveness of A Mandatory Competency-Based Simulation Program For Pediatric Emergency Medicine FacultyTushar RameshNo ratings yet
- Evaluate The Effectiveness of Mini-CEX Towards Clinical Competency Achievement in Neurological Examination of Clinical Practice Nursing Students at General Hospital MedanDocument11 pagesEvaluate The Effectiveness of Mini-CEX Towards Clinical Competency Achievement in Neurological Examination of Clinical Practice Nursing Students at General Hospital MedanLasma Rina SinuratNo ratings yet
- PNSG Table - LDocument17 pagesPNSG Table - Lapi-457773521No ratings yet
- Clinical Performance Assessment Tools in Physiotherapy Practice Education: A Systematic ReviewDocument8 pagesClinical Performance Assessment Tools in Physiotherapy Practice Education: A Systematic Reviewdan iacobNo ratings yet
- Best Practices in Summative AssessmentDocument10 pagesBest Practices in Summative AssessmentJoshuaNo ratings yet
- Work Based Assessment A Practical GuideDocument38 pagesWork Based Assessment A Practical GuideShajita DNo ratings yet
- The Role of Assessment in Competency-Based Medical EducationDocument8 pagesThe Role of Assessment in Competency-Based Medical EducationMaria PalaciosNo ratings yet
- Clinical PortDocument72 pagesClinical PortKetheesaran LingamNo ratings yet
- Lurie 2716Document9 pagesLurie 2716Ferdy LainsamputtyNo ratings yet
- PrinciplesofassesmentDocument10 pagesPrinciplesofassesmentLesa MalNo ratings yet
- IJBGM - Evaluation of Training Effectiveness Based On Reaction A Case StudyDocument12 pagesIJBGM - Evaluation of Training Effectiveness Based On Reaction A Case Studyiaset123No ratings yet
- Hallas 2012Document10 pagesHallas 2012Florsie MirandaNo ratings yet
- Development of A Systematic Career Coaching PrograDocument10 pagesDevelopment of A Systematic Career Coaching PrograCamille de La CruzNo ratings yet
- Hennessy-Hicks Training Needs Analysis Questionnaire and ManualDocument59 pagesHennessy-Hicks Training Needs Analysis Questionnaire and Manualhikmat pramajatiNo ratings yet
- Sebok Syer 2018 Considering The Interdependence ofDocument11 pagesSebok Syer 2018 Considering The Interdependence ofYoliset RomeroNo ratings yet
- Practice Portfolio Ps PaDocument15 pagesPractice Portfolio Ps PasehrNo ratings yet
- NCMB 419 Week 11 CU10Document23 pagesNCMB 419 Week 11 CU10GERALDINE GONZALESNo ratings yet
- Peer Observation of Teaching As A Faculty Development Tool: Researcharticle Open AccessDocument6 pagesPeer Observation of Teaching As A Faculty Development Tool: Researcharticle Open AccessNgọc Quỳnh NguyễnNo ratings yet
- Coaching As A Developmental Intervention in OrganiDocument41 pagesCoaching As A Developmental Intervention in OrganiCaroline HollandNo ratings yet
- Project Summary TemplateDocument5 pagesProject Summary TemplateDan CasiñoNo ratings yet
- ECOE Guia AMEE 21 - 11 - 2019 - The ObjectDocument11 pagesECOE Guia AMEE 21 - 11 - 2019 - The ObjectAlberto CasasNo ratings yet
- Pharmacy 04 00004Document10 pagesPharmacy 04 00004Rosen AnthonyNo ratings yet
- Twelve Tips For Embedding Assessment For and As Learning Practices in A Programmatic Assessment SystemDocument8 pagesTwelve Tips For Embedding Assessment For and As Learning Practices in A Programmatic Assessment SystemClaudia HenaoNo ratings yet
- The Best and Worst Things Staff Report About Behavioral Training WorkshopsDocument13 pagesThe Best and Worst Things Staff Report About Behavioral Training WorkshopsANDRESA NERES DO NASCIMENTO DE CAMARGONo ratings yet
- A Sistematic Frameworks - Progress TestDocument15 pagesA Sistematic Frameworks - Progress TestResti Rahmadika AkbarNo ratings yet
- The Relationship Between Competence and PerformanceDocument10 pagesThe Relationship Between Competence and PerformancemzulkarnainNo ratings yet
- The Effects of A Coaching Project in Nursing On The Coaches' Training Motivation, Training Outcomes, and Job Performance: An Experimental StudyDocument9 pagesThe Effects of A Coaching Project in Nursing On The Coaches' Training Motivation, Training Outcomes, and Job Performance: An Experimental StudyCANDYPANo ratings yet
- Research ProposalDocument8 pagesResearch ProposalJahid HasanNo ratings yet
- Education and Training of Clinical and Translational Study Investigators and Research Coordinators A Competency-Based Approach.Document10 pagesEducation and Training of Clinical and Translational Study Investigators and Research Coordinators A Competency-Based Approach.Luis FelipeNo ratings yet
- Objective Structured Clinical Examination (OSCE) With Immediate Feedback in Early (Preclinical) Stages of The Dental CurriculumDocument9 pagesObjective Structured Clinical Examination (OSCE) With Immediate Feedback in Early (Preclinical) Stages of The Dental CurriculumamiNo ratings yet
- Intellectual Property Rights: Open AccessDocument6 pagesIntellectual Property Rights: Open AccessAyu SumitaNo ratings yet
- Thesis Pin Aka Final Ye HeyDocument50 pagesThesis Pin Aka Final Ye HeyKaith Budomo LocadingNo ratings yet
- Health Coaching Quality FrameworkDocument22 pagesHealth Coaching Quality FrameworkGONDHES CHANNELNo ratings yet
- Self-Assessment in Medical PracticeDocument3 pagesSelf-Assessment in Medical PracticeBhakti PurnamasariNo ratings yet
- Assessment of Pharmacy Students' Clinical Skills Using Objective Structured Clinical Examination - A Literature ReviewDocument6 pagesAssessment of Pharmacy Students' Clinical Skills Using Objective Structured Clinical Examination - A Literature ReviewJordan FadhillaNo ratings yet
- Teamstepps Part of Dod Training For Improved Patient SafetyDocument6 pagesTeamstepps Part of Dod Training For Improved Patient Safetyd40sithuiNo ratings yet
- Study of Performance Appraisal System For Faculty Members in Management Institutes Affiliated To Shivaji University KolhapurDocument13 pagesStudy of Performance Appraisal System For Faculty Members in Management Institutes Affiliated To Shivaji University KolhapurelayayoungkingNo ratings yet
- Giving Feedback Effectively in The Clinical EnvironmentDocument5 pagesGiving Feedback Effectively in The Clinical EnvironmentMAurcioNo ratings yet
- Black Et Al-2007-International Journal of Pharmacy Practice PDFDocument7 pagesBlack Et Al-2007-International Journal of Pharmacy Practice PDFfaignacioNo ratings yet
- Jurnal IpeDocument11 pagesJurnal IpemusaffaNo ratings yet
- Mini-CEX y DOPSDocument15 pagesMini-CEX y DOPSAldito GlasgowNo ratings yet
- Competency Based Education:: IntroductionDocument6 pagesCompetency Based Education:: IntroductionrobinjbhattiNo ratings yet
- Qsen CurriculumDocument5 pagesQsen Curriculumapi-280981631No ratings yet
- Course Design for Public Health: A Competency Based ApproachFrom EverandCourse Design for Public Health: A Competency Based ApproachNo ratings yet
- A Trainer’S Guide for Preclinical Courses in Medicine: Series I Introduction to MedicineFrom EverandA Trainer’S Guide for Preclinical Courses in Medicine: Series I Introduction to MedicineNo ratings yet
- SNHD Protocol ManualDocument128 pagesSNHD Protocol ManualMedic03431100% (6)
- Amputações - Knee Disarticulation and Above Knee amputation-OpTechGenSurg2005Document6 pagesAmputações - Knee Disarticulation and Above Knee amputation-OpTechGenSurg2005Lorena AlmeidaNo ratings yet
- Malleolar Fractures - Handout PDFDocument14 pagesMalleolar Fractures - Handout PDFAlin Bratu100% (2)
- The Child With A URIDocument41 pagesThe Child With A URIAnaesNo ratings yet
- Ocular Prosthesis BhavanDocument58 pagesOcular Prosthesis BhavanDrkvpratheep Pratheep100% (1)
- Endodontic SurgeryDocument16 pagesEndodontic SurgeryauntymayaNo ratings yet
- Acute Coronary SyndromeDocument32 pagesAcute Coronary SyndromeCzarina jane MendozaNo ratings yet
- Blood PressureDocument5 pagesBlood PressureAndersonNo ratings yet
- Uro-Final MCQDocument45 pagesUro-Final MCQع كيف كيفك Dhaif-saeedNo ratings yet
- Daftar Obat High Alert Dan High Risk: Instalasi Farmasi Rumah Sakit Baptis BatuDocument2 pagesDaftar Obat High Alert Dan High Risk: Instalasi Farmasi Rumah Sakit Baptis BatudindaNo ratings yet
- Midwifery Short NotesDocument552 pagesMidwifery Short NotesChika JonesNo ratings yet
- Basic Life SupportDocument31 pagesBasic Life SupportNHUXUANNo ratings yet
- NCMB316 Lec PrelimDocument25 pagesNCMB316 Lec PrelimErickson V. LibutNo ratings yet
- The Necessary Steps For: Endophthalmitis ProphylaxisDocument3 pagesThe Necessary Steps For: Endophthalmitis ProphylaxisSurendar KesavanNo ratings yet
- Teeth Number 85Document16 pagesTeeth Number 85rarasNo ratings yet
- ForearmDocument8 pagesForearmNur Ashriawati BurhanNo ratings yet
- Cardiac Surgery Post-Op Care PDFDocument12 pagesCardiac Surgery Post-Op Care PDFHazel100% (1)
- TAVR Low RiskDocument5 pagesTAVR Low RiskTom BiusoNo ratings yet
- CIMSC 2019 Programme DetailsDocument6 pagesCIMSC 2019 Programme DetailsAndreea PodeanuNo ratings yet
- CPC BozDocument31 pagesCPC BozJamesNo ratings yet
- List Ruangan Ok Stok BHP NO Nama Qty SO Februari EDDocument102 pagesList Ruangan Ok Stok BHP NO Nama Qty SO Februari EDnitaNo ratings yet
- Guia de Bologna-2013Document14 pagesGuia de Bologna-2013andreigustvNo ratings yet
- Alveolar OstitisDocument8 pagesAlveolar OstitisAamir BidiwalaNo ratings yet
- Radially Expanding Cervical DilatorDocument19 pagesRadially Expanding Cervical DilatorCrescent FangNo ratings yet
- POCUS 101 Ocular Ultrasound Pocket CardDocument1 pagePOCUS 101 Ocular Ultrasound Pocket CardEduardoNo ratings yet
- Hemodynamic MonitoringDocument37 pagesHemodynamic MonitoringStephy Sojan50% (2)
- 2-Surgery 1.10Document224 pages2-Surgery 1.10reema.saleh123No ratings yet
- Brosur Carl Zeiss Visumax Corneal Surgery Mel 90Document21 pagesBrosur Carl Zeiss Visumax Corneal Surgery Mel 90khairul ihsanNo ratings yet
- Surgical InstrumentsDocument22 pagesSurgical InstrumentsDemiar Madlansacay Quinto100% (1)
- Ecg NestoDocument85 pagesEcg NestoAna ObradovicNo ratings yet