Professional Documents
Culture Documents
Card ACLS
Uploaded by
Saman FirdousCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Card ACLS
Uploaded by
Saman FirdousCopyright:
Available Formats
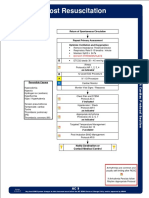
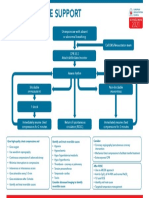
ADULT POST–CARDIAC ARREST CARE ALGORITHM ADULT BRADYCARDIA ALGORITHM ADULT TACHYCARDIA WITH A PULSE ALGORITHM
Assess appropriateness for clinical condition.
Heart rate typically ≥150/min if tachyarrhythmia.
Assess appropriateness for clinical conditions.
ROSC Obtained Heart rate typically <50/min if bradyarrhythmia.
es/Details
Dos Identify and treat underlying cause
• Maintain patent airway; assist breathing as necessary
Manage airway Identify and treat underlying causes • Oxygen (if hypoxemic)
Early placement of endotracheal tube - Maintain patent airway; assist breathing as necessary • Cardiac monitor to identify rhythm; monitor blood
Initial Stabilization Phase - Oxygen ( if hypoxemic )
• Airway management: pressure and oximetry
Manage respiratory parameters - Cardiac monitor to identify rhythm; monitor blood • IV access
Waveform capnography or
Start 10 breaths/min pressure and oximeter • 12-lead ECG, if available
capnometry to confirm and monitor
SPO2 92% to 98% endotracheal tube placement - IV access
PaCO2 35 to 45 mm Hg • Manage respiratory parameters:
- 12 lead ECG if available; don't delay therapy • Vagal maneuvers (if regular)
Titrate FIO2 for Spo2 92% to 98%; • Adenosine (if regular)
- Consider the possible hypoxic and toxicologic causes Persistent
Manage hemodynamic parameters start at 10 breaths per min; titrate to • β-Blocker or calcium channel blocker
PaCO2 of 35 to 45 mm of mercury
tachyarrhythmia causing:
Systolic blood pressure > 90 mm Hg • Consider expert consultation
• Manage hemodynamic parameters: • Hypotension?
Mean arterial pressure > 65 mm Hg
Administer crystalloid and/or • Acutely altered mental status?
Persistent NO
vasopressor or inotrope for goal • Signs of shock?
bradyarrhythmia causing:
systolic blood pressure greater than • Ischemic chest discomfort? NO Wide QRS?
Obtain 12-lead ECG 90 mm of mercury or mean arterial • Acute heart failure?
pressure greater than 65 mm of NO - Hypotension? ≥0.12 second
mercury - Acutely altered mental status? YES YES
Continued Management and - Signs of shock?
es/Details Synchronized cardioversion Consider
Dos
Consider for emergent cardiac intervention if Additional Emergent Activities - Ischemic chest discomfort?
• Consider sedation • Adenosine only if
- STEMI present These evaluations should be done - Acute heart failure? • If regular narrow complex, regular and monomorphic
- Unstable cardiogenic shock. concurrently so that decisions on consider adenosine • Antiarrhythmic infusion
targeted temperature management YES
- Mechanical circulatory support required. Monitor and Observe • Expert consultation
(TTM) receive Atropine Atropine IV dose:
high priority as cardiac interventions.
If atropine is ineffective: First dose: 1 mg bolus.
• Emergent cardiac intervention:
Early evaluation of 12-lead Repeat every 3-5 minutes.
Follows commands? - Transcutaneous pacing If refractory, consider
electrocardiogram (ECG); consider Maximum: 3 mg.
hemodynamics for decision on and/or Dopamine IV infusion: • Underlying cause
NO YES • Need to increase energy level
cardiac intervention - Dopamine infusion Usual infusion rate is
Comatose Awake • TTM: If patient is not following or 5-20 mcg/kg per minute. for next cardioversion
• TTM Other critical care commands, start TTM as soon as - Epinephrine infusion Titrate to patient response; • Addition of anti-arrhythmic drug
• Obtain brain CT management. possible; begin at 32 to 36 degrees
taper slowly. • Expert consultation
• EEG monitoring Celsius for 24
hours by using a cooling device with Epinephrine IV infusion:
• Other critical care 2-10 mcg per minute infusion.
feedback loop Consider:
management • Other critical care management Titrate to patient response.
– Continuously monitor core Causes: Doses/Details Antiarrhythmic Infusions for Stable Wide-QRS Tachycardia
- Expert Consultation Procainamide IV dose:
temperature (esophageal, rectal, • Myocardial ischemia/
bladder) - Transvenous pacing Synchronized cardioversion: 20-50 mg/min until arrhythmia suppressed, hypotension ensues,
infarction
Evaluate and treat rapidly reversible etiologies – Maintain normoxia, normocapnia, Refer to your specific device’s QRS duration increases >50%, or max dose 17 mg/kg given.
• Drugs/toxicologic (eg, recommended Maintenance infusion: 1-4 mg/min. Avoid if prolonged QT or CHF.
Involve expert consultation for continued management euglycemia
calcium-channel blockers, energy level to max first shock success. Amiodarone IV dose:
– Provide continuous or intermittent
electroencephalogram (EEG) beta blockers, digoxin) Adenosine IV dose: First dose: 150 mg over 10 min. Repeat as needed if VT recurs.
monitoring • Hypoxia First dose: 6 mg rapid IV push; follow Follow by maintenance infusion of 1 mg/min for first 6 hours.
– Provide lung-protective ventilation • Electrolyte abnormality with NS flush. Sotalol IV dose:
H’s and T’s (eg, hyperkalemia) Second dose: 12 mg if required. 100 mg (1.5 mg/kg) over 5 min. Avoid if prolonged QT.
vers Found
ACLS
sa
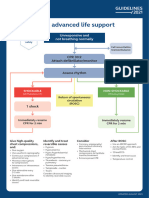
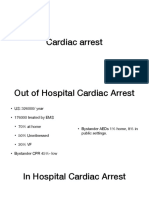
ADULT CARDIAC ARREST ALGORITHM
e
DOSES/DETALS FOR CARDIAC ARREST ALGORITHM
at
Cardiac Rhythms
Lif
ion
1 Start CPR PA N
CPR Quality KISTA
• Give oxygen • Push hard (at least 2 inches [5 cm]) and fast (100-120/min) and allow
• Attach monitor/defibrillator complete chest recoil.
• Minimize interruptions in compressions.
• Avoid excessive ventilation.
YES NO
Rhythm shockable? • Change compressor every 2 minutes, or sooner if fatigued.
• If no advanced airway, 30 to 2 compression-ventilation ratio.
9 • Quantitative waveform capnography
2
VF/pVT Asystole/PEA -If PETCO2 is low or decreasing, reassess CPR quality. Normal Sinus Rhythm
Shock Energy for Defibrillation
3 Shock Epinephrine • Biphasic: Manufacturer recommendation (eg, initial dose of 120-200
ASAP Joules); if unknown, use maximum available. Second and subsequent doses
4 should be equivalent, and higher doses may be considered.
CPR 2 minutes 10 CPR 2 minutes
• IV/IO access • IV/IO access • Monophasic: 360 Joules
• Epinephrine every 3 to 5 minutes. Drug Therapy
• Epinephrine IV/IO dose: 1 milligram every 3 to 5 minutes
Mono Morphic Ventricular Tachycardia
• Consider advanced airway,
NO capnography • Amiodarone IV/IO dose: First dose: 300 mg bolus. Second dose: 150mg.
Rhythm shockable?
OR
YES Lidocaine IV/IO dose: First dose: 1-1.5 mg per kg. Second dose: 0.5-0.75
5 Shock YES
Rhythm shockable? mg per kg.
6 NO Advanced Airway
CPR 2 minutes 11
• IV/IO access • Endotracheal intubation or supraglottic advanced airway. Ventricular Fibrillation
CPR 2 minutes. • Waveform capnography or capnometry to confirm and monitor ET tube
• Epinephrine every 3 to 5 minutes.
• Consider advanced airway,
• Treat reversible causes. placement.
capnography • Once advanced airway in place, give 1 breath every 6 seconds (10 breaths
per minute) with continuous chest compressions
NO Rhythm shockable?
Rhythm shockable? Return of Spontaneous Circulation (ROSC)
NO YES • Pulse and blood pressure.
YES • Abrupt sustained increase in PETCO2 (typically greater than or equal to 40 Atrial Fibrillation
7 Shock mm of mercury)
• Spontaneous arterial pressure waves with intra-arterial monitoring.
8 CPR 2 minutes
• Amiodarone or lidocaine. Reversible Causes
• Treat reversible causes. • Hypovolemia • Tension pneumothorax
• Hypoxia • Tamponade, cardiac
• Hydrogen ion (acidosis) • Toxins
12
• Hypo-/hyperkalemia Atrial Flutter
• If no signs of return of Go to 5 or 7 • Thrombosis, pulmonary
• Hypothermia • Thrombosis, coronary
spontaneous circulation
(ROSC), go to Box 10 or Box 11
• If ROSC, go to Post–Cardiac
Arrest Care
• Consider appropriateness of LIFESAVERS FOUNDATION PAKISTAN
continued resuscitation (+92-51) 8493015 lifesaversfoundation@gmail.com lifesaverspaksitan.com
Supraventricular Tachycardia
You might also like
- Guide to Canine and Feline ElectrocardiographyFrom EverandGuide to Canine and Feline ElectrocardiographyRuth WillisNo ratings yet
- AC 9 Post Resuscitation Protocol Final 2017 EditableDocument2 pagesAC 9 Post Resuscitation Protocol Final 2017 EditableLeandro NogueiraNo ratings yet
- AlgorithmACLS PCAC 200622Document1 pageAlgorithmACLS PCAC 200622Sandy XNo ratings yet
- ACLS Healthcare Provider Post-Cardiac Arrest Care Algorithm: o Co Io o CoDocument1 pageACLS Healthcare Provider Post-Cardiac Arrest Care Algorithm: o Co Io o CoAlexis HospitalNo ratings yet
- Adult Post-Cardiac Arrest Care Algorithm: o Co Io o CoDocument1 pageAdult Post-Cardiac Arrest Care Algorithm: o Co Io o CoKavya ShreeNo ratings yet
- AlgorithmACLStachycardiawithapulse PDFDocument1 pageAlgorithmACLStachycardiawithapulse PDFDendy Frannuzul RamadhanNo ratings yet
- Tachycardia With A Pulse Algorithm: Assess Appropriateness For Clinical ConditionDocument1 pageTachycardia With A Pulse Algorithm: Assess Appropriateness For Clinical ConditionDendy Frannuzul RamadhanNo ratings yet
- 7.2post Resus Algorithms 1Document1 page7.2post Resus Algorithms 1abrar risandiNo ratings yet
- 7.2post Resus Algorithms 1Document1 page7.2post Resus Algorithms 1Massimo Di BenedettoNo ratings yet
- Post Arrest CareDocument23 pagesPost Arrest CareMohamed RasoolNo ratings yet
- Atrial Fibrillation: Key TreatmentsDocument2 pagesAtrial Fibrillation: Key TreatmentschoobiNo ratings yet
- 12-Adult Post Resuscitation Care Algorithm 2021Document1 page12-Adult Post Resuscitation Care Algorithm 2021khaledNo ratings yet
- Managemen Disritmia: Dr. Rofika Hanifa, SPPDDocument20 pagesManagemen Disritmia: Dr. Rofika Hanifa, SPPDavivlabirdNo ratings yet
- Advanced Cardiac Life SupportDocument37 pagesAdvanced Cardiac Life SupportRoy Acosta GumbanNo ratings yet
- Screenshot 2565-05-03 at 10.34.19Document39 pagesScreenshot 2565-05-03 at 10.34.19Sugus PichayaNo ratings yet
- Aha Acls GuideDocument11 pagesAha Acls GuideIrene PimentelNo ratings yet
- 8-Adult Advanced Life Support Algorithm 2021Document1 page8-Adult Advanced Life Support Algorithm 2021khaledNo ratings yet
- Acls Study Guide 2016Document2 pagesAcls Study Guide 2016Caridad RodasNo ratings yet
- Critical Event ChecklistsDocument25 pagesCritical Event ChecklistsarisyiNo ratings yet
- Acls Study Guide 2016Document2 pagesAcls Study Guide 2016nova939100% (2)
- Er FinalsDocument63 pagesEr FinalsNaren RaviNo ratings yet
- 2020 Acls Megacode Testing Scenarios - 2Document13 pages2020 Acls Megacode Testing Scenarios - 2Dr. Saqib RazaNo ratings yet
- Post Cardiac ArrestDocument2 pagesPost Cardiac ArrestAlthea AlcalaNo ratings yet
- Adult Cardiac Arrest Circular Algorithm: Monitor CPR QualityDocument1 pageAdult Cardiac Arrest Circular Algorithm: Monitor CPR QualityAlexis HospitalNo ratings yet
- Adult Cardiac Arrest Circular Algorithm: Monitor CPR QualityDocument1 pageAdult Cardiac Arrest Circular Algorithm: Monitor CPR QualityChris LeeNo ratings yet
- Syok KardiogenikDocument31 pagesSyok KardiogenikcantikarevieraNo ratings yet
- Cardiology Exam 2 - Lecture Notes: Treating Adult BradycardiaDocument5 pagesCardiology Exam 2 - Lecture Notes: Treating Adult BradycardiaAddieNo ratings yet
- Onlinemeded Notes CardioDocument1 pageOnlinemeded Notes CardioCourtney HolbrookNo ratings yet
- Cardiac Arrest Circular Algorithm: Start CPR 2 M IN UT ESDocument1 pageCardiac Arrest Circular Algorithm: Start CPR 2 M IN UT ESjohndoe1995No ratings yet
- Monitoring Intra Operatif: Mindi Widayani NRP 122.022.1115 FK UPN "Veteran" JakartaDocument21 pagesMonitoring Intra Operatif: Mindi Widayani NRP 122.022.1115 FK UPN "Veteran" Jakartaputri wulandariNo ratings yet
- Adenosine 8-28-22Document1 pageAdenosine 8-28-22ladawskiNo ratings yet
- NRNP 6566 Week 4 Knowledge CheckDocument7 pagesNRNP 6566 Week 4 Knowledge Checkmary011danielNo ratings yet
- Adult Advanced Life Support Algorithm 2021 Aug 2023Document1 pageAdult Advanced Life Support Algorithm 2021 Aug 2023cknihilnewNo ratings yet
- CardiologyDocument8 pagesCardiologyMa. Kristina Cazandra IbañezNo ratings yet
- NCP CardioDocument10 pagesNCP CardioCharles LigonNo ratings yet
- 11 Post Resus Care OkDocument25 pages11 Post Resus Care OkdocgilbertNo ratings yet
- Angiography (Cardiac Catherization) : Patient Teaching/preparationDocument2 pagesAngiography (Cardiac Catherization) : Patient Teaching/preparationpsyNo ratings yet
- Algo Bradycardia DikonversiDocument5 pagesAlgo Bradycardia DikonversiDaniel SitungkirNo ratings yet
- Algorithms of AHA 2020Document23 pagesAlgorithms of AHA 2020Emirhan llkhanNo ratings yet
- 2021 ACLS Study GuideDocument20 pages2021 ACLS Study GuideShane Brown83% (12)
- ACLS Megacode Testing ScenariosDocument12 pagesACLS Megacode Testing Scenariosealm10100% (2)
- Objective Data Diagnosis Goals Interventions EvaluationDocument2 pagesObjective Data Diagnosis Goals Interventions EvaluationHira Akram Hira AkramNo ratings yet
- Cardiac ArrestDocument15 pagesCardiac ArrestJim Rohn100% (1)
- Tams NCP and DrugDocument5 pagesTams NCP and DrugNicholas Xavier VenturaNo ratings yet
- Transoperative 812217287Document27 pagesTransoperative 812217287Pepe PeñaNo ratings yet
- 2010 Emergency Nursing Cases Updates - CDH - 10-06-10Document2 pages2010 Emergency Nursing Cases Updates - CDH - 10-06-10shalomNo ratings yet
- Algorithm-ACLS ACS 200806 1Document1 pageAlgorithm-ACLS ACS 200806 1Kavya Shree100% (1)
- ACLS Pocket CardDocument6 pagesACLS Pocket Cardno_spam_mang80% (5)
- EKG Nclex High YieldDocument13 pagesEKG Nclex High Yieldnene lewis100% (1)
- Cardiac/Cardiogenic Shock: Clinical Practice GuidelinesDocument3 pagesCardiac/Cardiogenic Shock: Clinical Practice GuidelinesAnonymous Yo0mStNo ratings yet
- Bradycardia and TachycardiaDocument66 pagesBradycardia and TachycardiaKarissaNo ratings yet
- NCM 118 - Lesson 11 (Arrhythmia)Document5 pagesNCM 118 - Lesson 11 (Arrhythmia)Bobby Christian DuronNo ratings yet
- Types of DysrhythmiasDocument15 pagesTypes of DysrhythmiasKevin VillaranteNo ratings yet
- Post-Cardiac Arrest Care Algorithm: Return of Spontaneous Circulation (ROSC)Document1 pagePost-Cardiac Arrest Care Algorithm: Return of Spontaneous Circulation (ROSC)johndoe1995No ratings yet
- Sinus Bradycardia: o No TX If AsymptomaticDocument3 pagesSinus Bradycardia: o No TX If Asymptomaticelle50% (2)
- Socul CardiogenDocument30 pagesSocul Cardiogencretu mihaiNo ratings yet
- Post Operative Management After TAPVC RepairDocument36 pagesPost Operative Management After TAPVC RepairsreedeviNo ratings yet
- 9 - Role of Non InvasiveDocument46 pages9 - Role of Non InvasiveHavara Kausar AkbarNo ratings yet
- Case StudyDocument16 pagesCase StudyArmand Bong Santiago100% (1)
- LINEE GUIDA ERC 2021 - Capitolo 7 - Terapia Post RianimazioneDocument114 pagesLINEE GUIDA ERC 2021 - Capitolo 7 - Terapia Post Rianimazionegiuseppe.tancredi.scarioNo ratings yet
- Texbook of Emergency CardiologyDocument445 pagesTexbook of Emergency CardiologyArtur TarsaNo ratings yet
- Fang Impact of Emergency Medical Technician Configurations On Outcomes of Patients in Cardiac ArrestDocument12 pagesFang Impact of Emergency Medical Technician Configurations On Outcomes of Patients in Cardiac ArrestJamison ParfittNo ratings yet
- 8-Adult Advanced Life Support Algorithm 2021Document1 page8-Adult Advanced Life Support Algorithm 2021khaledNo ratings yet
- (2014) Capnography During Cardiopulmonary Resuscitation - Current Evidence and Future DirectionsDocument10 pages(2014) Capnography During Cardiopulmonary Resuscitation - Current Evidence and Future DirectionsDominik Chirito PastorNo ratings yet
- Adult Cardiac Arrest Algorithm: VF/PVT Asystole/PEADocument1 pageAdult Cardiac Arrest Algorithm: VF/PVT Asystole/PEAAlexis HospitalNo ratings yet
- GREY BOOK August 2022 75th EditionDocument155 pagesGREY BOOK August 2022 75th EditionMohamed AbdelmoniemNo ratings yet
- Farmacology Del Paro CardiacoDocument14 pagesFarmacology Del Paro CardiacoNicoSwtifNo ratings yet
- Intro To Critical Care NursingDocument4 pagesIntro To Critical Care NursingHain YoloNo ratings yet
- Anaesthetic Crisis ManualDocument63 pagesAnaesthetic Crisis ManualkushishaNo ratings yet
- SLCEP ALS e Book PDFDocument74 pagesSLCEP ALS e Book PDFgnanasegaram vithursanNo ratings yet
- 2020 Focused Transesophageal Echocardiography During Cardiac Arrest ResuscitationDocument10 pages2020 Focused Transesophageal Echocardiography During Cardiac Arrest Resuscitationbogeg74816No ratings yet
- Advanced Life Support-RESSU CouncilDocument30 pagesAdvanced Life Support-RESSU CouncilGigel DumitruNo ratings yet
- Adult Cardiac Arrest Algorithm: VF/PVT Asystole/PEADocument8 pagesAdult Cardiac Arrest Algorithm: VF/PVT Asystole/PEAVitor Hugo100% (2)
- Postarrest Steroid Use May Improve Outcomes of Cardiac Arrest SurvivorsDocument9 pagesPostarrest Steroid Use May Improve Outcomes of Cardiac Arrest Survivorsmonica trifitrianaNo ratings yet
- WHATs New in CPCRDocument4 pagesWHATs New in CPCRJessicaHernandezNo ratings yet
- Emergency Viva (Full)Document48 pagesEmergency Viva (Full)ashokarathnasingheNo ratings yet
- Advanced Life Support EMS ScenariosDocument147 pagesAdvanced Life Support EMS Scenariosfidelurtecho4881No ratings yet
- Resuscitation Guide Lines 2005: Aries PerdanaDocument36 pagesResuscitation Guide Lines 2005: Aries PerdanaLa Ode RinaldiNo ratings yet
- Pra & Intra Hospital Cardiac Arrest Management-MAHESA Agustus 2021Document65 pagesPra & Intra Hospital Cardiac Arrest Management-MAHESA Agustus 2021Menggy 31No ratings yet
- Obstetrics AclsDocument6 pagesObstetrics AclsPedro BurgosNo ratings yet
- Pals CardDocument12 pagesPals CardSara KhanNo ratings yet
- Pediatric Cardiac Arrest AlgorithmDocument27 pagesPediatric Cardiac Arrest AlgorithmLinna AndrianiNo ratings yet
- Design of Cardiopulmonary Resuscitation MachineDocument6 pagesDesign of Cardiopulmonary Resuscitation MachineShiferaw TesfayeNo ratings yet
- 16 Cardiopulmonary - Resuscitation - in - The - Prone.1Document8 pages16 Cardiopulmonary - Resuscitation - in - The - Prone.1LelyNo ratings yet
- Technique For Chest Compressions in Adult CPRDocument5 pagesTechnique For Chest Compressions in Adult CPRZara Yupita AzraNo ratings yet
- Arc Guideline 11 1 Introduction To and Principles of in Hospital Resuscitation Feb 2019Document22 pagesArc Guideline 11 1 Introduction To and Principles of in Hospital Resuscitation Feb 2019hernandez2812No ratings yet
- 3.ALS Algorithms Advanced Life SupportDocument1 page3.ALS Algorithms Advanced Life SupportLucian Alin DinuNo ratings yet
- ALS AlgorithmDocument22 pagesALS AlgorithmBookwormNo ratings yet
- Double Sequential External Defibrillation For Refractory Ventricular Fibrillation (Dose VF) : Study Protocol For A Randomized Controlled TrialDocument11 pagesDouble Sequential External Defibrillation For Refractory Ventricular Fibrillation (Dose VF) : Study Protocol For A Randomized Controlled TrialRurgenciasNo ratings yet