Professional Documents
Culture Documents
Evaluation of Miniature Wireless Vital Signs Monitor in A Trauma
Uploaded by
Yira Tatiana Castro RomeroOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Evaluation of Miniature Wireless Vital Signs Monitor in A Trauma
Uploaded by
Yira Tatiana Castro RomeroCopyright:
Available Formats
MILITARY MEDICINE, 181, 5:199, 2016
Evaluation of Miniature Wireless Vital Signs Monitor in a Trauma
Intensive Care Unit
Jonathan P. Meizoso, MD; Casey J. Allen, MD; Juliet J. Ray, MD; Robert M. Van Haren, MD, MSPH;
Laura F. Teisch, BS; Xiomara Ruiz Baez, MD; Alan S. Livingstone, MD; Nicholas Namias, MD, MBA;
Carl I. Schulman, MD, PhD, MSPH; Kenneth G. Proctor, PhD
ABSTRACT A previous study demonstrated basic proof of principle of the value of a miniature wireless vital signs
monitor (MWVSM, MiniMedic, Athena GTX, Des Moines, Iowa) for battlefield triage However, there were unanswered
Downloaded from https://academic.oup.com/milmed/article/181/suppl_5/199/4209470 by guest on 18 April 2022
questions related to sensor reliability and uncontrolled conditions in the prehospital environment. This study deter-
mined whether MWVSM sensors track vital signs and allow for appropriate triage compared to a gold standard bed-
side monitor in trauma patients. This was a prospective study in 59 trauma intensive care unit patients. Systolic blood
pressure, temperature, heart rate (HR), skin temperature, and pulse oximetry (SpO2) were displayed on a bedside
monitor for 60 minutes. Shock index (SI) was calculated. A separate MWVSM monitor was attached to the fore-
head and finger of each patient. Data from each included pulse wave transit time (PWTT), temperature, HR, SpO2,
and a summary status termed “Murphy Factor” (MF), which ranges from 0 to 5. Patients are classified as “routine”
if MF = 0 to 1 or SI = 0 to 0.7, “priority” if MF = 2 to 3 or SI = 0.7 to 0.9, and “critical” if MF = 4 to 5 or SI ≥ 0.9.
Forehead and finger MWVSM HRs both differed from the monitor (both p < 0.001), but the few beats per minute
differences were clinically insignificant. Differences in MWVSM SpO2 (1–7%) and temperature (6–13°F) from the
monitor were site specific (all p < 0.001). Forehead PWTT (271 ± 50 ms) was less ( p < 0.001) than finger PWTT
(315 ± 42 ms); both were dissociated from systolic blood pressure (r2 < 0.05). The SI distributed patients about
equally as “routine,” “priority,” and “critical,” whereas MF overtriaged to “routine” and undertriaged to “critical”
for both sensors (all p < 0.001). Our findings suggest that MF does not accurately predict the most critical patients,
likely because erroneous PWTT values confound MF calculations. MF and the MWVSM are promising, but require fine-
tuning before deployment.
INTRODUCTION multiple casualties on the battlefield or in other austere con-
The vast majority of military trauma deaths occur prehospital ditions. This particular system contains two novel features.
and a significant proportion of in-hospital mortality occurs in First, it incorporates an injury acuity algorithm termed the
patients with no vital signs in the field.1–3 Thus, large oppor- Murphy Factor (MF), which summarizes overall patient
tunities exist for reducing trauma mortality through innovation status, and is calculated from available vital signs (whether
in the prehospital setting.4,5 measured by the sensor, input by the first responder, or calcu-
The United States Special Operations Command (SOCOM) lated by the device); additionally, it factors in the changes
and the Department of Defense designed and funded the in these vital signs over the last 30 seconds. MF includes an
development of a miniature wireless vital signs monitor adjustment to overcome data drops that are common during
(MWVSM) (MiniMedic, Athena GTX, Des Moines, Iowa) triage in chaotic environments. Second, the system is based
based on the success of its original wireless vital signs on pulse wave transit time (PWTT) rather than systolic blood
monitor.6 The new system has reduced weight and size and pressure (SBP). Various methods of PWTT measurement
addressed an unmet need to acquire vital physiologic infor- correlate well with SBP.7
mation from small surface sensors placed on up to 5 casual- A previous study suggested that a single numeric MF
ties simultaneously and then to wirelessly transmit this data from a peripheral MWVSM could predict the need for life-
to miniature monitors carried by any first responder within a saving interventions during prehospital transport.8 Although
100-m range. This would allow for appropriate monitoring, this prehospital study provided basic proof of concept, there
triage, prioritization of transport, and tracking of changes in were multiple sources of variability including patient selec-
tion, injury severity, sensor placement, transport time, and
Divisions of Trauma Surgical Critical Care and Burns, DeWitt Daughtry missing or intermittent data.
Family Department of Surgery, Ryder Trauma Center, University of Miami The present study was conducted in the controlled set-
Miller School of Medicine, 1800 NW 10th Avenue, Suite T-215 (D-40), ting of a trauma intensive care unit (TICU) for a fixed period
Miami, FL 33136. of time with a bedside monitor used as the gold standard
Presented at the Florida Committee on Trauma Meeting, Florida Chapter for paired comparison of vital signs. Furthermore, the shock
of the American College of Surgeons, Jacksonville, FL, October 17, 2014
and at the Region IV Committee on Trauma Meeting, American College of
index (SI) was used a standard to compare the MF as both
Surgeons, Orlando, FL, November 14, 2014. methods provide a single number to assess overall patient
doi: 10.7205/MILMED-D-15-00162 status. The SI, which is calculated by dividing the heart
MILITARY MEDICINE, Vol. 181, May Supplement 2016 199
Evaluation of MWVSM in a Trauma ICU
rate (HR) by the SBP, has previously been shown to cor- parisons were made between the MWVSM and conven-
relate with markers of cellular hypoxia and shock, such tional monitor measurements for HR, SpO2, and temperature.
as lactate and central venous oxygenation.9–11 It is also Correlations were made between PWTT measured by the
an indicator of patients requiring transfusion and a pre- MWVSM and SBP measured by the conventional monitor.
dictor of mortality.12 We test the hypothesis that changes SI was calculated using the conventional bedside HR
in multiple parameters obtained from the MWVSM corre- and SBP. To compare the two indices, MF was classi-
late favorably with conventional vital signs and SI in critically fied using manufacturer specifications, where “routine” is
ill trauma patients. MF = 0 to 1, “priority” is MF = 2 to 3, and “critical” is
MF = 4 to 5. Normal SI ranges from 0.5 to 0.7 and was
MATERIALS AND METHODS classified as “routine” if SI = 0 to 0.7, “priority” if SI =
0.7 to 0.9, and “critical” if SI ≥0.9. The study team deter-
Study Protocol and Patient Selection
Downloaded from https://academic.oup.com/milmed/article/181/suppl_5/199/4209470 by guest on 18 April 2022
mined values for SI a priori. Prior investigators have found
This study was conducted at the Ryder Trauma Center (Uni- that SI >0.9 is associated with injuries requiring immediate
versity of Miami/Jackson Memorial Hospital) and approved attention,10 while others have used a similar breakdown to
by the Institutional Review Board at Jackson Memorial Hos- the present study.12
pital and the University of Miami Leonard M. Miller School
of Medicine, Miami, Florida. A prospective observational
trial was performed in a convenience sample of 59 TICU Statistical Analyses
patients from October 2013 to July 2014. Eligible patients Data were analyzed using SPSS version 22.0 (IBM Corpora-
were adults (>17 years old) with an arterial catheter who were tion, Armonk, New York). Data are reported as mean ± SD
admitted to the TICU. Patients meeting inclusion criteria were if normally distributed or as median (interquartile range) if
enrolled from 8 a.m. to 5 p.m. on Mondays to Fridays during not normally distributed. Independent data were compared
the study period. with paired Student’s t test. Categorical data were compared
Data from each MWVSM were compared to data simulta- using χ2 test or Fisher’s exact test as appropriate. Significance
neously obtained with a bedside vital signs monitor (GE Solar was assessed at p < 0.05.
8000M multichannel monitor, GE Healthcare, Milwaukee,
Wisconsin) in the TICU. This monitor collected the fol-
lowing standard vital signs: HR, SBP, core body temper- RESULTS
ature as measured by Foley catheter, and pulse oximetry The study population was comprised of 59 TICU patients,
(SpO2). The test system is composed of two components: aged 47 ± 20 years with a male preponderance (80%).
a patient sensor that is affixed to either the forehead or an Mechanism of injury was blunt in 60% and penetrating in
extremity and a handheld unit. The patient sensor weighs 27%; nontraumatic cases made up 13%. These basic demo-
3.8 oz and uses two AAA alkaline batteries. The handheld graphics are similar to our usual TICU population.
monitor is 4.0 × 2.5 × 0.79 inches in size, weighs 4.2 oz, Actual SBP was 129 ± 20 mm Hg. Corresponding PWTT
and uses two AAA alkaline batteries. Communication between with the MWVSM averaged 314 ± 2 ms with the finger
MWVSM devices is achieved with Communication Zigbee sensor and 271 ± 2 ms with the forehead sensor. Forehead
(802.15.4) Wireless Protocol with a range of 100-m line PWTT (271 ± 50 ms) was significantly less ( p < 0.0001)
of sight. than peripheral PWTT (315 ± 42 ms), but this is logical
The patient sensor records physiologic variables (skin as it takes longer for the pulse wave to transmit to the
temperature, SpO2, HR, and PWTT) every second and trans- periphery. However, peripheral and forehead PWTT were
mits every 5 seconds to the monitor. Other information is dissociated from SBP. For SBP vs. peripheral PWTT the
manually input with the handheld unit, including Glasgow correlation, although weak, was statistically significant
Coma Score, medications, and fluids. In addition to record- (r2 = 0.0385, p < 0.001). There was no significant correla-
ing and storing continuous data, the sensor computes MF, tion between SBP and forehead PWTT (r2 = 0.0007, p =
which is a proprietary algorithm that incorporates changes 0.513) (Fig. 1).
in the last 30 seconds to derive a summary status alarm that Actual core temperature was 100 (3.2) °F. Correspond-
reflects injury acuity (0–5 scale). The MF requires data ing skin temperature with the MWVSM finger sensor was
from a minimum of two sources. The MF signal quality 86.8 ± 8.4°F and with the forehead sensor was 93.1 ±
is theoretically more reliable with more available data. All 4.7°F. Clearly these measures were dependent on sensor
information is wirelessly transmitted up to 100 m to a location. Paired temperature differences between core tem-
handheld monitor, which the medic can use to monitor perature and skin temperature (with both finger and fore-
up to five patients simultaneously. The software revision head sensors) were statistically significant ( p < 0.001).
was 0.0.xx2. Furthermore, the paired differences between forehead
Data from both the MWVSM and the conventional vital and finger sensors (6–13°F) were statistically significant
signs monitor were recorded every 5 minutes. Paired com- ( p < 0.001).
200 MILITARY MEDICINE, Vol. 181, May Supplement 2016
Evaluation of MWVSM in a Trauma ICU
forehead sensor. Similar to HR, conventional and MWVSM
measurements were statistically ( p < 0.001) different, but
clinically insignificant. Paired differences between the fin-
ger and forehead sensors were also significantly different
( p < 0.001).
Table I shows the differences between HR, SpO2, and
temperature using the bedside monitor and the MWVSM.
Figure 2 compares MF and SI in all three severity cate-
gories and demonstrates inappropriate triage by both fore-
head and peripheral sensors. According to the SI, the patients
were distributed about equally in the “routine,” “priority,”
and “critical” categories; however, MF significantly overtriaged
Downloaded from https://academic.oup.com/milmed/article/181/suppl_5/199/4209470 by guest on 18 April 2022
patients to the “routine” category and undertriaged patients
to the “critical” category in both sensors (all p < 0.001).
DISCUSSION
The present study is the second from our group that eval-
uates the MWVSM for potential trauma triage. The major
new findings are that peripheral and forehead PWTT were
dissociated from SBP and that relative to SI, MF signifi-
cantly overtriaged patients to the “routine” category and
undertriaged patients to the “critical” category for either
the forehead or peripheral sensor. These observations sup-
port the conclusion that MF does not accurately predict
the most critical patients likely because erroneous PWTT
values confound the MF calculation. The concept of MF and
the MWVSM is promising, but requires further fine-tuning
before deployment.
The military WVSMs before this miniature version were
smaller than conventional monitors, but still bulky and
difficult to transport for SOCOM.6 The MWVSM offers a
(theoretical) logistic advantage for continuous monitoring
of multiple casualties on the battlefield from remote loca-
tions. We demonstrated basic proof of concept that the MF
can summarize overall patient status in the prehospital set-
ting.8 This follow-up study aimed to critically evaluate the
MWVSM in the controlled setting of a TICU to demonstrate
whether data obtained from the MWVSM correlates with the
conventional vital signs monitor. Furthermore, we aimed to
correlate MF with SI, a previously validated measure that is
FIGURE 1. (A) Peripheral sensor pulse wave transit time (PWTT) (ms) vs. able to accurately predict early mortality and need for mas-
systolic blood pressure (SBP) (mm Hg). Pearson correlation = −0.1961; sive transfusion after blunt trauma.10,13,14
r2 = 0.038; n = 604; p < 0.001. (B) Forehead sensor PWTT (ms) vs.
SBP (mm Hg). Pearson correlation = 0.0259; r2 = 0.00067; n = 640;
MWVSM HR is reasonably accurate. Although the values
p = not significant. are statistically significant, a 2 to 3 bpm difference is clini-
cally insignificant. Data from the peripheral MWVSM sensor,
but not the forehead sensor, agrees with conventional SpO2;
Actual HR was 102 ± 18 beats per minute (bpm), compared this can be expected secondary to different perfusion patterns
to 105 ± 22 bpm with the finger sensor and 104 ± 21 bpm in the forehead and periphery. However, skin temperature
with the forehead sensor. Although the differences between from either sensor differs from the actual core temperature. It
conventional and MWVSM HR were statistically significant is unclear what, if any, additional vital information is provided
( p < 0.001), a difference of only 2 bpm cannot be considered by measuring skin temperature from either site.
clinically significant. Measurements between the forehead and The most significant finding is that PWTT is poorly cor-
finger sensors were similar ( p = 0.35). related with SBP regardless of sensor placement. We believe
Finally, median SpO2 was 100 (2)%. This was compared that the inaccuracies in triaging patients using the MF are
to 100 (3)% with the finger sensor and 93 ± 8.3% with the secondary to this discrepancy in PWTT as the MF uses
MILITARY MEDICINE, Vol. 181, May Supplement 2016 201
Evaluation of MWVSM in a Trauma ICU
TABLE I. Summary of Conventional and miniature wireless vital signs monitor (MWVSM) Vital Signs
Heart Rate (bpm) Skin Temperature, Pulse Oximetry SpO2 (%) Temperature (°F)
Bedside Monitor 102 ± 18 100 (2) 100 (3)
n = 757 n = 736 n = 624
Peripheral MWVSM Sensor 105 ± 22 100 (3) 87 ± 8
n = 721 n = 568 n = 728
Paired Difference Sensor vs. Monitor p < 0.001 p < 0.001 p < 0.001
Forehead MWVSM Sensor 104 ± 21 93 ± 8.3 93 ± 5
n =721 n = 612 n = 745
Paired Difference Sensor vs. Monitor p < 0.001 p < 0.001 p < 0.001
Paired Difference Sensor vs. Sensor p = 0.350 p < 0.001 p < 0.001
Downloaded from https://academic.oup.com/milmed/article/181/suppl_5/199/4209470 by guest on 18 April 2022
PWTT in its summary status alarm algorithm. Unfortunately,
the algorithm for calculating the MF is proprietary and we
are unaware of the weight that PWTT carries in the calcula-
tion. MF derived from both sensors overtriaged patients to the
“routine” category and undertriaged patients to the “critical”
category; overall, MF inappropriately triaged approximately
50% of patients relative to SI.
The MWVSM was developed for use in chaotic military
mass casualty environments when triage and transport deci-
sions are difficult. MF is an overall summary status alarm
that would theoretically aid the combat medic to make life
and death decisions. The MWVSM will never replace a
well-trained medic, but it can provide useful information
under times of stress. Woodford et al15 have also previously
demonstrated the benefit of an automated continuous vital
signs analysis system with decision support capabilities in
prehospital care. Furthermore, a significant amount of work
regarding WVSM and machine learning has been done
by the U.S. Army Institute of Surgical Research. Liu and
Holcomb studied the WVSM, which is the predecessor to
the MWVSM, in 305 patients and found that the WVSM
improved accuracy in identifying patients requiring lifesav-
ing intervention.6 The same group has used automated sys-
tems incorporating nonstandard vital signs, including HR
variability (HRV) and HR complexity (HRC), and found
that these improve the prediction of mortality and lifesaving
interventions in trauma patients.16,17
Several other noninvasive strategies have been pro-
posed to triage trauma patients.6,15,16,18–21 King et al18 pro-
spectively analyzed 75 trauma patients requiring prehospital
helicopter transport and found that HRV predicted base
excess and the requirement of lifesaving interventions; HRV
more accurately identified critical patients than trauma center
criteria or prehospital vital signs. Indeed, the current “stan-
dard” vital signs measures used to identify patients in shock
have been questioned; Eastridge used the Joint Theater
Trauma Registry to study 7,180 military combat casualties
and found that SBP ≤ 100 mm Hg is a better indicator
of true hypotension and hypoperfusion in military trauma
than the traditional 90 mm Hg.22 Ryan et al19 found HRV
FIGURE 2. (A) Percentage of patients with peripheral sensor Murphy
Factor (MF) vs. Shock Index (SI) in each acuity category. (B) Percentage of to be a predictor of morbidity and mortality in the hemo-
patients with forehead sensor MF vs. SI in each acuity category. dynamically stable trauma patient. HRC also analyzes HR
202 MILITARY MEDICINE, Vol. 181, May Supplement 2016
Evaluation of MWVSM in a Trauma ICU
time sequences and has been found by several groups to revision of the manuscript, figures, and tables. KGP had overall responsi-
correlate with the need for lifesaving interventions in the bility for the study, including conception and experimental design; analy-
sis and interpretation of the data; drafting and revision of the manuscript,
prehospital setting.16,21 Continuous near-infrared spectroscopy figures, and tables; statistical expertise and evaluation; obtaining funding
can predict the need for transfusion in patients deemed for this project; and supervision.
hemodynamically stable with an SBP >90 mm Hg and may
prove to be an excellent adjunct to physiologic monitoring
REFERENCES
in the future.20
1. Champion HR, Bellamy RF, Roberts CP, Leppaniemi A: A profile of
Limitations to this study include the use of a conve-
combat injury. J Trauma 2003; 54(5 Suppl): S13–9.
nience sample, which is not randomized and thus subject 2. Bellamy RF: The causes of death in conventional land warfare: impli-
to bias. No interventions were performed based on results cations for combat casualty care research. Mil Med 1984; 149(2):
from the MWVSM. Furthermore, we do not have data 55–62.
Downloaded from https://academic.oup.com/milmed/article/181/suppl_5/199/4209470 by guest on 18 April 2022
regarding whether any of these patients required blood prod- 3. Eastridge BJ, Mabry RL, Seguin P, et al: Death on the battlefield
(2001-2011): implications for the future of combat casualty care.
uct transfusion or other interventions. The MF depends on
J Trauma Acute Care Surg 2012; 73(6 Suppl 5): S431–7.
the reliability of input signals and these are sometimes lost 4. Blackbourne LH, Czarnik J, Mabry R, et al: Decreasing killed in action
when patients are in extremis; in this present study, some and died of wounds rates in combat wounded. J Trauma 2010; 69(Suppl 1):
data were lost even when patients were not in extremis. S1–4.
If the overall purpose of the MWVSM is to identify those 5. Gerhardt RT: Prehospital and emergency care research at the U.S.
Army Institute of Surgical Research: enabling the next great leap
patients who are in shock (i.e., cold, clammy, hypotensive,
in combat casualty survival. U.S. Army Med Dep April–June 2011:
and tachycardic) then the device needs further fine-tuning to 82–6.
avoid data drops. Additionally, the MWVSM is designed to 6. Liu NT, Holcomb JB, Wade CE, et al: Development and validation of a
collect continuous data however the data analyzed included machine learning algorithm and hybrid system to predict the need for
only snapshots at every 5 minutes compared to the con- life-saving interventions in trauma patients. Med Biol Eng Comput 2014;
ventional monitor. Our previous study demonstrated that a 52(2): 193–203.
7. Patzak A, Mendoza Y, Gesche H, Konermann M: Continuous blood
MF >3 in the prehospital setting was associated with the pressure measurement using the pulse transit time: comparison to intra-
need for lifesaving intervention upon arrival to the trauma arterial measurement. Blood Press 2015; 24(4): 217–21.
center. The current findings suggest that MF is not a reli- 8. Van Haren RM, Thorson CM, Valle EJ, et al: Novel prehospital
able indicator of shock because it undertriages a propor- monitor with injury acuity alarm to identify trauma patients who
tion of the most severely injured patients. Together, this require lifesaving intervention. J Trauma Acute Care Surg 2014; 76(3):
743–9.
suggests that a significant number of patients could be mis- 9. Rady MY: The role of central venous oximetry, lactic acid concentra-
classified by MF. tion and shock index in the evaluation of clinical shock: a review.
In summary, in a TICU population at an urban level I Resuscitation 1992; 24(1): 55–60.
trauma center, the MWVSM demonstrated poor correlation 10. Rady MY, Smithline HA, Blake H, Nowak R, Rivers E: A comparison
between PWTT and SBP. We believe this was responsible of the shock index and conventional vital signs to identify acute, critical
illness in the emergency department. Ann Emerg Med 1994; 24(4):
for the inaccurate triage using the MF when compared to the
685–90.
previously validated SI. Improvements in measuring PWTT 11. Rady MY, Nightingale P, Little RA, Edwards JD: Shock index: a
are required to obtain more accurate MF values. The use of re-evaluation in acute circulatory failure. Resuscitation 1992; 23(3):
noninvasive blood pressure rather than PWTT may provide 227–34.
another option for improved identification of patients in 12. Mutschler M, Nienaber U, Munzberg M, et al: The Shock Index
revisited—a fast guide to transfusion requirement? A retrospective
shock using the MWVSM. Newer modalities such as HRV,
analysis on 21,853 patients derived from the TraumaRegister DGU. Crit
HRC, and near-infrared spectroscopy will likely be benefi- Care 2013; 17(4): R172.
cial in future wireless vital signs devices for more accurate 13. Vandromme MJ, Griffin RL, Kerby JD, McGwin G Jr, Rue LW 3rd,
and timely diagnosis and treatment of combat casualties. Weinberg JA: Identifying risk for massive transfusion in the relatively
Further work is required to validate the MWVSM for use by normotensive patient: utility of the prehospital shock index. J Trauma
SOCOM in the battlefield. 2011; 70(2): 384–8; discussion 388–90.
14. Zarzaur BL, Croce MA, Fischer PE, Magnotti LJ, Fabian TC: New
vitals after injury: shock index for the young and age x shock index for
the old. J Surg Res 2008; 147(2): 229–36.
ACKNOWLEDGMENTS 15. Woodford MR, Mackenzie CF, DuBose J, et al: Continuously recorded
This work was supported in part by the Office of Naval Research (Grant oxygen saturation and heart rate during prehospital transport outperform
No. N140610670) and the U.S. Army Medical Research & Materiel Com- initial measurement in prediction of mortality after trauma. J Trauma Acute
mand (Grant No. 09078015). Care Surg 2012; 72(4): 1006–11.
JPM was directly responsible for all aspects of this study. He partici- 16. Liu NT, Holcomb JB, Wade CE, Darrah MI, Salinas J: Utility of vital
pated in the collection, analysis, and interpretation of data, and drafting signs, heart rate variability and complexity, and machine learning for
and revision of the manuscript, figures, and tables. CJA, JJR, RMVH, LFT, identifying the need for lifesaving interventions in trauma patients. Shock
and XRB participated in the experimental design, collection of data, and 2014; 42(2): 108–14.
revision of the manuscript, figures, and tables. ASL, NN, and CIS were 17. Liu NT, Holcomb JB, Wade CE, Salinas J: Improving the prediction of
medically responsible for the patients and participated in the review and mortality and the need for life-saving interventions in trauma patients
MILITARY MEDICINE, Vol. 181, May Supplement 2016 203
Evaluation of MWVSM in a Trauma ICU
using standard vital signs with heart-rate variability and complexity. 20. Beekley AC, Martin MJ, Nelson T, et al: Continuous noninvasive tissue
Shock 2015; 43(6): 549–55. oximetry in the early evaluation of the combat casualty: a prospective
18. King DR, Ogilvie MP, Pereira BM, et al: Heart rate variability as a tri- study. J Trauma 2010; 69(Suppl 1): S14–25.
age tool in patients with trauma during prehospital helicopter transport. 21. Cancio LC, Batchinsky AI, Salinas J, et al: Heart-rate complexity for
J Trauma 2009; 67(3): 436–40. prediction of prehospital lifesaving interventions in trauma patients.
19. Ryan ML, Ogilvie MP, Pereira BM, et al: Heart rate variability is an J Trauma 2008; 65(4): 813–9.
independent predictor of morbidity and mortality in hemodynamically 22. Eastridge BJ, Salinas J, Wade CE, Blackbourne LH: Hypotension is
stable trauma patients. J Trauma 2011; 70(6): 1371–80. 100 mm Hg on the battlefield. Am J Surg 2011; 202(4): 404–8.
Downloaded from https://academic.oup.com/milmed/article/181/suppl_5/199/4209470 by guest on 18 April 2022
204 MILITARY MEDICINE, Vol. 181, May Supplement 2016
You might also like
- TERAPIA COMBINADA - Solaris 708 Service Manual 02-07 - 14 PDFDocument172 pagesTERAPIA COMBINADA - Solaris 708 Service Manual 02-07 - 14 PDFkevin alegreNo ratings yet
- Removable Partial DenturesDocument34 pagesRemovable Partial DenturesZaraNo ratings yet
- Hseplan 200615062050Document169 pagesHseplan 200615062050Mohammad AshpakNo ratings yet
- Perioperative Risk Stratification and ModificationDocument23 pagesPerioperative Risk Stratification and ModificationDianita P Ñáñez VaronaNo ratings yet
- Manual of Practice Management for Ambulatory Surgery Centers: An Evidence-Based GuideFrom EverandManual of Practice Management for Ambulatory Surgery Centers: An Evidence-Based GuideNiraja RajanNo ratings yet
- Accupuncture Needle DepthDocument21 pagesAccupuncture Needle DepthStephen T LeNo ratings yet
- PH Eur 1433 Herbal DrugsDocument2 pagesPH Eur 1433 Herbal DrugsLuisSanabriaSaavedra0% (1)
- Pi Is 0741521416001579Document8 pagesPi Is 0741521416001579Dr-Rabia AlmamalookNo ratings yet
- Jurnal Bedside MonitorDocument4 pagesJurnal Bedside MonitorAnonymous eCgTp1No ratings yet
- Standardized Outcome Measures in Stroke Rehabilitation and Falls After Discharge - A Cohort StudyDocument9 pagesStandardized Outcome Measures in Stroke Rehabilitation and Falls After Discharge - A Cohort StudyMiguelySusy Ramos-RojasNo ratings yet
- Trauma Score PDFDocument10 pagesTrauma Score PDFNdHy_Windhy_3403No ratings yet
- Seymour 2016Document13 pagesSeymour 2016Yadira SantosNo ratings yet
- Epidemiological Profile and Outcome Analysis With Prism Iii Score of Patients Admitted To A Pediatric Intensive Care Unit in A Tertiary Care CenterDocument27 pagesEpidemiological Profile and Outcome Analysis With Prism Iii Score of Patients Admitted To A Pediatric Intensive Care Unit in A Tertiary Care CenterIJAR JOURNALNo ratings yet
- Thursday, October 10, 2013 4:10 - 5:10 Concurrent Session: TraumaDocument2 pagesThursday, October 10, 2013 4:10 - 5:10 Concurrent Session: TraumaPeko PekoNo ratings yet
- Sharshar 2009 Debil y EstadiaDocument7 pagesSharshar 2009 Debil y EstadiaStefania Anahi MartelNo ratings yet
- Morse 2001Document5 pagesMorse 2001Anonymous EAPbx6No ratings yet
- Independent Risk Factor ShiveringDocument9 pagesIndependent Risk Factor ShiveringAnonymous r2nNdvvweNo ratings yet
- Injury Journal - Effective TriageDocument5 pagesInjury Journal - Effective TriagemediclassroomNo ratings yet
- A Machine Learning Algorithm To Identify Patients With Tibial Shaft Fractures at Risk For Infection After Operative TreatmentDocument9 pagesA Machine Learning Algorithm To Identify Patients With Tibial Shaft Fractures at Risk For Infection After Operative TreatmentarchchayaNo ratings yet
- (19330693 - Journal of Neurosurgery) Decompressive Hemicraniectomy - Predictors of Functional Outcome in Patients With Ischemic StrokeDocument7 pages(19330693 - Journal of Neurosurgery) Decompressive Hemicraniectomy - Predictors of Functional Outcome in Patients With Ischemic StrokeRandy Reina RiveroNo ratings yet
- RamachandranDocument9 pagesRamachandranjojobaggins100% (1)
- Preoperative Assessment of The Risk For Multiple Complications After SurgeryDocument10 pagesPreoperative Assessment of The Risk For Multiple Complications After SurgerylaisNo ratings yet
- Accepted Manuscript: Journal of Cardiothoracic and Vascular AnesthesiaDocument27 pagesAccepted Manuscript: Journal of Cardiothoracic and Vascular AnesthesiaRian AprizaNo ratings yet
- Continuous Monitoring of Vital Signs Using Wearable Devices On The General Ward: Pilot StudyDocument15 pagesContinuous Monitoring of Vital Signs Using Wearable Devices On The General Ward: Pilot Studymariana.bragaNo ratings yet
- Penetrating Abdominal Trauma in The Era of Selective Conservatism: A Prospective Cohort Study in A Level 1 Trauma CenterDocument9 pagesPenetrating Abdominal Trauma in The Era of Selective Conservatism: A Prospective Cohort Study in A Level 1 Trauma CenterDewi HenssaNo ratings yet
- Ewss PDFDocument6 pagesEwss PDFChintia Meliana Kathy SiraitNo ratings yet
- Contemporary Clinical Trials: ArticleinfoDocument8 pagesContemporary Clinical Trials: ArticleinfoDavy JonesNo ratings yet
- 708 FullDocument8 pages708 FullHidayadNo ratings yet
- AR6TIFICIALDocument9 pagesAR6TIFICIALutip25No ratings yet
- Acute Medicine Surgery - 2019 - Shibahashi - Can The Shock Index Be A Reliable Predictor of Early Mortality After TraumaDocument7 pagesAcute Medicine Surgery - 2019 - Shibahashi - Can The Shock Index Be A Reliable Predictor of Early Mortality After TraumaFidencio ParraNo ratings yet
- Fenotipos Sepsis 3Document5 pagesFenotipos Sepsis 3Gerardo LermaNo ratings yet
- Utility of Vital Signs in Mass CasualtyDocument4 pagesUtility of Vital Signs in Mass CasualtyYves BurckelNo ratings yet
- Format Review Article Title Article: Nama Mahasiswa: Cornel Anggara Url: NIM: 2017 1030009 Section PurposeDocument3 pagesFormat Review Article Title Article: Nama Mahasiswa: Cornel Anggara Url: NIM: 2017 1030009 Section PurposeM. Ibnu HabibNo ratings yet
- (10920684 - Neurosurgical Focus) Impact of Preoperative Endovascular Embolization On Immediate Meningioma Resection OutcomesDocument7 pages(10920684 - Neurosurgical Focus) Impact of Preoperative Endovascular Embolization On Immediate Meningioma Resection OutcomesBedussa NuritNo ratings yet
- UC Irvine: Western Journal of Emergency Medicine: Integrating Emergency Care With Population HealthDocument13 pagesUC Irvine: Western Journal of Emergency Medicine: Integrating Emergency Care With Population HealthARINANo ratings yet
- American Heart Journal Plus: Cardiology Research and PracticeDocument6 pagesAmerican Heart Journal Plus: Cardiology Research and Practice18ME045No ratings yet
- 5 SheetDocument12 pages5 SheetLaraib KanwalNo ratings yet
- Luan2019 PDFDocument12 pagesLuan2019 PDFrifki irsyadNo ratings yet
- Perioperative Pulmonary Outcomes With OsaDocument9 pagesPerioperative Pulmonary Outcomes With OsawandapandabebeNo ratings yet
- Articulo Hombro. Expectativas Del Pte Con Inestabilidad.Document9 pagesArticulo Hombro. Expectativas Del Pte Con Inestabilidad.ambarquiroga17No ratings yet
- Prediction of Adverse Cardiac Outcomes in High-Risk Mexican Patients With Chest Pain in The Emergency DepartmentDocument6 pagesPrediction of Adverse Cardiac Outcomes in High-Risk Mexican Patients With Chest Pain in The Emergency Departmentluis sanchezNo ratings yet
- 1 s2.0 S0300957218309092 Main PDFDocument7 pages1 s2.0 S0300957218309092 Main PDFBirhanu MuletaNo ratings yet
- Apache IvDocument14 pagesApache IvLUISNo ratings yet
- Original Article: Surgical Infections Volume 18, Number 00, 2017 Mary Ann Liebert, Inc. DOI: 10.1089/sur.2016.029Document4 pagesOriginal Article: Surgical Infections Volume 18, Number 00, 2017 Mary Ann Liebert, Inc. DOI: 10.1089/sur.2016.029MishellDominguezNo ratings yet
- Readmission and Other Adverse Events After Transsphenoidal Surgery: Prevalence, Timing, and Predictive FactorsDocument9 pagesReadmission and Other Adverse Events After Transsphenoidal Surgery: Prevalence, Timing, and Predictive FactorsbobNo ratings yet
- Predisposing Factors For Early Infection in Patients With Open Fractures and Proposal For A Risk ScoreDocument7 pagesPredisposing Factors For Early Infection in Patients With Open Fractures and Proposal For A Risk ScoremoaraNo ratings yet
- Application of Different Scoring Systems and Their Value in Pediatric Intensive Care UnitDocument6 pagesApplication of Different Scoring Systems and Their Value in Pediatric Intensive Care UnitPreksha AdeNo ratings yet
- ICMLWSDocument10 pagesICMLWSAhmed AlaaNo ratings yet
- Early Warning ScoreDocument7 pagesEarly Warning ScoreDaniello RahanrNo ratings yet
- Zoltie N, Et Al., 1993Document4 pagesZoltie N, Et Al., 1993Hendry SusantoNo ratings yet
- Development and Validation of A Preoperative Scoring System To Predict 30 Day Mortality in Patients Undergoing Hip Fracture SurgeryDocument7 pagesDevelopment and Validation of A Preoperative Scoring System To Predict 30 Day Mortality in Patients Undergoing Hip Fracture Surgeryuhs888No ratings yet
- Scoring TENDocument5 pagesScoring TENreyhanrrNo ratings yet
- Simplified Frailty Index As A Predictor of Adverse Outcomes in Total Hip and Knee ArthroplastyDocument6 pagesSimplified Frailty Index As A Predictor of Adverse Outcomes in Total Hip and Knee ArthroplastyJohn SmithNo ratings yet
- Marshall1991 The Outcome of Severe Closed Head InjuryDocument9 pagesMarshall1991 The Outcome of Severe Closed Head InjuryJulieta PereyraNo ratings yet
- Risk Factors For Post Induction Hypotension in Children Presenting For SurgeryDocument6 pagesRisk Factors For Post Induction Hypotension in Children Presenting For SurgeryasfwegereNo ratings yet
- Comparativeanalysisofsofavs - Saps-Iiscore in Assessing Mortality in Polytrauma Patients For Quality ManagementDocument9 pagesComparativeanalysisofsofavs - Saps-Iiscore in Assessing Mortality in Polytrauma Patients For Quality ManagementIJAR JOURNALNo ratings yet
- Use of A Modified Early Warning Score System To Reduce The Rate of In-Hospital Cardiac ArrestDocument6 pagesUse of A Modified Early Warning Score System To Reduce The Rate of In-Hospital Cardiac ArrestPuspa AmandatyNo ratings yet
- Sofa ScoreDocument6 pagesSofa ScoreNadiah Umniati SyarifahNo ratings yet
- 2020 Journal WatchDocument140 pages2020 Journal WatchMarcoNo ratings yet
- Clinical Profile and Outcome of Shock in MechanicaDocument6 pagesClinical Profile and Outcome of Shock in MechanicaUlfa Sari Al-BahmiNo ratings yet
- Relationship Between The in Ammation/immune Indexes and Deep Venous Thrombosis (DVT) Following Tibial Plateau FracturesDocument14 pagesRelationship Between The in Ammation/immune Indexes and Deep Venous Thrombosis (DVT) Following Tibial Plateau FracturesEKO SANDY SINAGANo ratings yet
- Impact of Frailty On Outcomes in Surgical Patients - A Systematic Review and Meta-Analysis AM JOURNAL 20119 Nihms-1515850Document20 pagesImpact of Frailty On Outcomes in Surgical Patients - A Systematic Review and Meta-Analysis AM JOURNAL 20119 Nihms-1515850SANDRA MILENA GUTIERREZ CAÑASNo ratings yet
- Damage Control Resuscitation: Identification and Treatment of Life-Threatening HemorrhageFrom EverandDamage Control Resuscitation: Identification and Treatment of Life-Threatening HemorrhagePhilip C. SpinellaNo ratings yet
- Adult Critical Care Medicine: A Clinical CasebookFrom EverandAdult Critical Care Medicine: A Clinical CasebookJennifer A. LaRosaNo ratings yet
- Icu Drugs 1Document19 pagesIcu Drugs 1Ahmad SaleemNo ratings yet
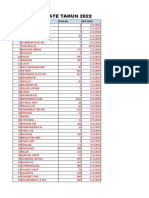
- Expired Date Tahun 2023Document10 pagesExpired Date Tahun 2023Lala PoNo ratings yet
- Ethnobotanical, Phytochemical, and Pharmacological Properties of Nepenthes Species: A ReviewDocument4 pagesEthnobotanical, Phytochemical, and Pharmacological Properties of Nepenthes Species: A ReviewRisamy RuzNo ratings yet
- Zambia Study Dec 2019Document9 pagesZambia Study Dec 2019AbiodunOlaiyaPaulNo ratings yet
- ClaimFormDocument9 pagesClaimFormVirat Vipul ChaudharyNo ratings yet
- GENERALDocument12 pagesGENERALAirg AlesantNo ratings yet
- Dokumen - Tips CTD Module 1Document29 pagesDokumen - Tips CTD Module 1Cosmiin DascaluNo ratings yet
- MN Senate Only HHS Offer 4Document12 pagesMN Senate Only HHS Offer 4FluenceMediaNo ratings yet
- Seizure-NcpDocument2 pagesSeizure-NcpRomuel PaparonNo ratings yet
- Phase 1 IntroDocument7 pagesPhase 1 Intro22024552 Hà Đăng LongNo ratings yet
- Dasar Pengelolaan Penderita Gawat Darurat: Dept. Anestesiologi & Terapi Intensif FK-USU/RSUP H.Adam Malik-MedanDocument47 pagesDasar Pengelolaan Penderita Gawat Darurat: Dept. Anestesiologi & Terapi Intensif FK-USU/RSUP H.Adam Malik-Medanfibri fameliaNo ratings yet
- Covid19 India Dashboard - All India Corona Status3Document4 pagesCovid19 India Dashboard - All India Corona Status3SRINIVASARAO JONNALANo ratings yet
- ABL9Document4 pagesABL9TW RHKLNo ratings yet
- Presentasi Haemodialisa TEKNISIDocument53 pagesPresentasi Haemodialisa TEKNISIMUSARONGAHNo ratings yet
- Giann Pascual: Associate Degree NursingDocument1 pageGiann Pascual: Associate Degree NursingGiann PascualNo ratings yet
- Brosur Savina 300Document8 pagesBrosur Savina 300Rumah Sakit Lancang KuningNo ratings yet
- ELECTROCUTIONDocument27 pagesELECTROCUTIONalyssaNo ratings yet
- Voicesofvisn 6Document11 pagesVoicesofvisn 6Kyle HoodNo ratings yet
- Alpha Blood Root Paste ResultsDocument5 pagesAlpha Blood Root Paste ResultsJeNo ratings yet
- Chapter 4 - Wrist BlockDocument6 pagesChapter 4 - Wrist BlockmikayNo ratings yet
- Reduction of Implant Loading Using A Modified Centric Occlusal AnatomyDocument16 pagesReduction of Implant Loading Using A Modified Centric Occlusal AnatomyPablo Gutiérrez Da VeneziaNo ratings yet
- ISAPS NL Vol4 N2 PDFDocument17 pagesISAPS NL Vol4 N2 PDFhuyenthanh1807No ratings yet
- MARS Appliance - Clements1982Document11 pagesMARS Appliance - Clements1982rohitNo ratings yet
- IHI Patient Safety Leadership Walk Rounds ToolDocument5 pagesIHI Patient Safety Leadership Walk Rounds ToolAhmad ZaatariNo ratings yet
- Jasmin 1Document22 pagesJasmin 1angel angelNo ratings yet