Professional Documents
Culture Documents
51 Disfungsi Wasting Weakness
Uploaded by
Armi ZakaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
51 Disfungsi Wasting Weakness
Uploaded by
Armi ZakaCopyright:
Available Formats
Skeletal muscle dysfunction in critical care: Wasting, weakness,
and rehabilitation strategies
Zudin Puthucheary, MRCP; Stephen Harridge, PhD; Nicholas Hart, PhD
Understanding the trajectory of skeletal muscle loss, evaluat- covery stages of critical illness is required. This could potentially
ing its relationship to the subsequent functional impairment, and lead to targeted pharmacologic and nonpharmacologic strategies
understanding the underlying mechanisms of skeletal muscle to treat, or even prevent, peripheral muscle wasting and weak-
wasting will provide goals for novel treatment strategies in the ness. (Crit Care Med 2010; 38[Suppl.]:S676 –S682)
intensive care setting. A focused approach on the effect of critical KEY WORDS: critical illness; muscle weakness; muscle protein
illness on muscle morphology, muscle protein turnover, and the turnover; muscle-signaling pathways
associated muscle-signaling pathways during the early and re-
I
ncreasing numbers of critically ill half of those discharged required some weakness (ICU-AW) is defined as bilateral
patients are admitted to the inten- form of caregiver assistance at 1 yr (2). A symmetrical limb weakness and has been
sive care unit (ICU). Although ad- study following neuromuscular abnormal- reported, at the time of wakening, in 50%
vances in medical practice and ities in survivors up to 5 yrs after critical of patients mechanically ventilated for
technology have resulted in improved illness showed ongoing disability and a ⬎7 days, and in 25% of patients 7 days
outcomes, these early survival rates are three-fold increase in mortality over this later (5). This acquired muscle weakness
poorly predictive of long-term health and period (3). The 114th World Health Orga- may be due to an axonal polyneuropathy
functional status. Following a critical ill- nization executive board focused on human (critical illness polyneuropathy), myop-
ness, impaired health status is frequently disability in its broadest terms; so, in 2004, athy (critical illness myopathy), or, more
protracted. Long-term sequelae need to it prompted its member states 1) to pro- frequently, a combination of both (criti-
be longitudinally evaluated through mea- mote early intervention and identification cal illness neuromyopathy) (6 – 8). Disuse
surements of self-reported, health-related of disability and full physical, informa- atrophy occurs in the limb muscles of
quality of life, exercise capacity, and other tional, and economic accessibility, includ- many ICU survivors, and it is not surpris-
detailed validated measurements of pe- ing rehabilitation services, in order to en- ing that muscle wasting and weakness are
ripheral muscle performance. Experience sure full participation and equality of frequent complaints (9) with evidence of
with acute respiratory distress syndrome persons with disabilities; and 2) to facilitate critical illness polyneuropathy, critical
survivors reveals that exercise capacity, access to appropriate assistive technologies illness myopathy, and critical illness neu-
assessed by using the 6-min walk test, for rehabilitation. This is wholly relevant to romyopathy persisting months to years
and health-related quality of life are patients both during and after critical ill- after hospitalization (10 –13). Depending
markedly reduced 1 yr after hospital dis- ness. Despite the overall paucity of data in on whether clinical, electrophysiologic,
charge (1). Furthermore, in an observa- this field, this statement on healthcare plus or histologic diagnostic criteria are met,
tional cohort of ⬎800 patients, more than other data has highlighted the need for a the prevalence of critical illness neuro-
concerted effort to understand critical ill-
myopathy ranges from 25% to 100% (6 –
ness-acquired muscle weakness and how
8). As regards to clinical outcome,
rehabilitation may be optimized. Indeed,
From the Lane Fox Respiratory Unit (ZP), Respira- ICU-AW and reduction in limb muscle
recent guidelines in this regard have been
tory & Critical Care Medicine (NH), Guy’s and St strength are associated with respiratory
Thomas’ Foundation Trust and Kings College, London, published by the United Kingdom National
muscle weakness and delayed weaning
UK; Centre of Human & Aerospace Physiological Sci- Institute of Clinical Excellence (4). An up-
from mechanical ventilation (14). The
ences (SH), School of Biomedical and Health Sciences, to-date PubMed search using the terms
Kings College, London, UK; National Institute of Health main risk factors for developing ICU-AW
“critical care” and “muscle weakness” re-
Research Comprehensive Biomedical Research Centre
vealed only a total of 281 articles in this are severity and duration of systemic in-
(NH), London, UK. flammatory response, length of ICU stay,
Dr. Hart has received speaker’s fees from Phillips- area. However, 30% of these were pub-
Respironics and Fisher-Paykel, and unrestricted re- lished in the last 3 years, highlighting the and duration of mechanical ventilation.
search grants from Phillips-Respironics, B&D Electro- limited previous data and an increasing in- Other factors implicated are hyperglyce-
medical, Resmed, Fisher-Paykel, and Guy’s and St terest among the critical care community. mia, hypoalbuminemia, parenteral nutri-
Thomas Charity. The remaining authors have not dis- tion, corticosteroid administration, and
closed any potential conflicts of interest.
neuromuscular-blocking agents. Inter-
For information regarding this article, E-mail: ICU-acquired weakness
nicholas.hart@gstt.nhs.uk estingly, renal replacement therapy ap-
Copyright © 2010 by the Society of Critical Care Increasingly recognized, skeletal mus- pears to be protective (5, 15). As expected,
Medicine and Lippincott Williams & Wilkins cle weakness can be commonplace in the in addition to the impact of muscle weak-
DOI: 10.1097/CCM.0b013e3181f2458d intensive care setting. ICU-acquired ness on weaning, and ICU, hospital stay,
S676 Crit Care Med 2010 Vol. 38, No. 10 (Suppl.)
and healthcare costs (14, 16, 17), recent therefore limited (12). Other measure-
studies have confirmed that both the ments have been proposed, such as man-
presence and severity of ICU-AW are in- ual muscle testing and hand grip
dependent risk factors for death (15, 18). strength, which are easier to perform, but
such volitional tests are difficult to inter-
Identification and stratification pret, especially if a borderline result is
obtained, as this could indicate weakness,
Immobilization, as occurs in all pa- poor motivation, or inability to complete
tients with critical illness, has been the task (5, 18). These limitations make
shown to alter skeletal muscle morphol- manual muscle strength testing either
ogy (19), the proportion of slow and fast unreliable or impractical, in particular,
muscle twitch fibers (20), contractility during the early stages of critical illness
(21–23), aerobic capacity (24), muscle or in patients with an impaired cognitive
protein synthesis (23, 25), subsequent state.
physical activity (24), and the electrome- As strength measurements are not al-
chanical relationship of the nerve-muscle ways feasible for assessing the severity of
interface (26). All of these factors contrib- muscle weakness, attention has more re-
ute to decreased muscle strength, power, cently focused on muscle wasting. This is
and fatigue resistance. However, in addi- a valid, rational approach, as a linear re-
tion to immobilization, other frequently lationship is present between quadriceps
encountered factors such as systemic muscle strength and rectus femoris
inflammation in critically ill patients cross-sectional area (34, 35) and fat-free
compound this loss of muscle mass and mass, which is an indicator of whole-body
function (5, 15). Identification and strat- muscle mass (36). Furthermore, ultra-
ification of the patients at risk of devel- sound measurements of the rectus femo-
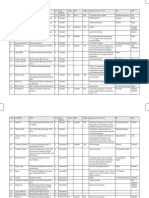
oping ICU-AW, with significant associ- ris muscle are sensitive enough to track Figure 1. a, Ultrasound measurement of rectus
ated long-term functional impairment, changes in muscle layer thickness (37, femoris cross-sectional area. b, Mean ⫾ SEM rec-
tus femoris cross-sectional area (solid line) vs.
must be a priority of critical care physi- 38) and cross-sectional area, indicative of thigh circumference (dashed line) as percentage
cians. Patients who may benefit from muscle wasting during immobilization of baseline (day 1) value. (Adapted from reference
critical care rehabilitation and other po- (39 – 43), despite the presence of fluid re- 34.) #Significant (p ⬍ .05) change from day 1.
tential management strategies must be tention and edema observed in critically RFCSA, rectus femoris cross-sectional area; ICU,
identified, particularly as combined seda- ill patients (36, 44). We are therefore cur- intensive care unit.
tion holds and whole-body rehabilitation rently investigating this relatively novel
have been demonstrated to be safe and application of ultrasound (34, 45), which
efficacious in the early stages of critical is simple, portable, and now widely avail- flammation as likely causative factors
illness (27). This is important because the able in the ICU, to measure the quadri- (47). While these are rational explana-
patient population has marked heteroge- ceps rectus femoris cross-sectional area tions, our current knowledge of fiber-
neity. Resources need to be focused on (34) (Fig. 1). Whereas this has the poten- type morphology, changes in fiber-type
these at-risk patients, identified at the tial to be a clinically useful tool, the abil- morphology (Figs. 2 and 3), muscle atro-
earliest possible stage. However, patients ity of ultrasound to sequentially measure phy– hypertrophy-signaling pathways,
are often immobile, especially during the cross-sectional area to quantify muscle and muscle protein synthesis and prote-
early part of their admission, due to their loss and predict functional outcome re- olysis pathways are mainly based on data
life-threatening illness and the sedatives mains as yet unproven. Nevertheless, if from healthy humans and animals. It is
and opiates administered. This hinders validated, the early identification of those important to highlight differences be-
the volitional assessment of their periph- patients with low muscle mass and those tween animal models and humans and, in
eral muscles as such patients are unable with significant loss of muscle mass early particular, that the rate of protein turn-
to cooperate with the physical examina- in their critical illness will allow the over in small mammals, such as rats, is
tion. Fortunately, there are a number of stratification of patients to target thera- 2.5-fold greater than in humans (48). In
nonvolitional neurophysiologic and mus- pies to those most likely to benefit. addition, human data have shown a dis-
cle strength assessments that can be un- sociation between actual protein turn-
dertaken by using such techniques as Mechanisms contributing to over and alterations in signaling path-
electrical (10, 12) and magnetic (28 –30) ICU-AW ways purported to control protein
stimulation of peripheral nerves. These synthesis and breakdown (25, 49, 50).
have provided detailed physiologic data Although important, muscle inexcit- Furthermore, the loss of muscle mass
demonstrating reductions in peripheral ability as a cause of a loss of muscle and the fall in protein synthesis observed
and respiratory muscle strength (30 –33). performance in critically ill patients will with immobilization are not accompa-
It should be appreciated that these are not be addressed; data addressing this nied by an increase in proteolytic enzyme
primarily research tools and probably issue can be found elsewhere (46). In gene expression (51). Although there are
have limited widespread clinical utility, critically ill patients, observational data data in healthy subjects with limb immo-
in part due to the need for experienced identify risk factors associated with mus- bilization to show that the balance be-
staff and expensive equipment to perform cle weakness with immobility, disuse- tween muscle protein breakdown (MPB)
these tests; clinical outcome data are related muscle atrophy, and systemic in- and muscle protein synthesis (MPS) is
Crit Care Med 2010 Vol. 38, No. 10 (Suppl.) S677
altered mainly by a fall in MPS (23, 52), tion, response to dietary amino acids, and
there are no data in critically ill patients insulin play important roles in muscle
to define muscle loss as a consequence of protein turnover, with stress and inflam-
either impaired MPS, accelerated MPB, or mation increasing MPB (60). However,
both. MPS blunting has been reported to we need more data from critically ill pa-
occur and been termed anabolic resis- tients.
tance (48, 52–54). The mechanisms dem- In addition to the balance between
onstrated to promote these processes are MPS and MPB, we must also consider the
many of the factors encountered in crit- atrophy– hypertrophy-signaling path-
ically ill patients. In particular, these in- ways, which should have an association
clude loss of muscle mass with immobi- with muscle protein turnover although,
lization (23, 25), reduced MPS response as mentioned previously, this is a contro-
to excess dietary amino acid loading (55, versial area (49, 50). In health, the atro-
56), and insulin inhibition of MPB with phic signals are balanced by hypertrophic
no effect on MPS (56). Indeed, this may in signals, but the relative roles of each of
part add validity to the observation that these processes in critical illness are
intensive insulin therapy to control hy- poorly understood (49, 50). MPB in both
perglycemia has an association with a re- systemic disease and disuse is regulated
duction in critical illness-related neuro- by muscle-specific ubiquitin ligases or
muscular complications (57). It can be atrogenes (61, 62), with accelerated ca-
Figure 2. Twenty-four-year-old woman with postulated that this may be an effect of tabolism observed in patients with sys-
septic shock and multiorgan failure. Hematoxy- increased insulin levels facilitating inhi- temic inflammation and immobilization
lin-and-eosin stains of serial vastus lateralis bi- bition of MPB, which is already blunted (63– 67). The main atrogenes (Fig. 4),
opsy samples. Day 1 demonstrated normal mus-
cle morphology, with day 7 showing fiber in the elderly, rather than any effect me- atrogin-1, also known as muscle atrophy
atrophy, muscle necrosis, and inflammatory cel- diated by controlling serum glucose lev- F-box protein (MAFbx) and muscle ring-
lular infiltrate. (Used with permission from the els, although this needs to be studied finger-1 (MuRF-1), are dependent on the
Musculoskeletal Ultrasound Study in Critical further. In addition to the paucity of data activity of forkhead (FoxO) transcription
Care: Longitudinal Evaluation [MUSCLE] study.)
defining the relative roles of MPS and factors (68, 69). These atrogenes are ren-
MPB in critical illness, the time course of dered inactive by phosphorylation of
normalization during recovery and reha- AKT, a downstream target of insulin-like
bilitation is unknown. However, there are growth factor 1 (IGF-1) and insulin,
data to suggest that, following acute ill- which inhibits the dephosphorylation of
ness, there is a preference to increase fat forkhead (Fig. 3). Thus, IGF-1 can block
mass rather than fat-free muscle mass (1, transcriptional up-regulation of atro-
58, 59). This would suggest that there is a genes. A further requirement for the re-
fundamental modification in body com- habilitation of muscle is fatigue resis-
position after critical illness that stimu- tance, which is linked to a muscle
lates MPB and/or inhibits MPS. It is clear oxidative activity. PGC-1␣ (peroxisome
from the data generated from non- proliferator-activated receptor-␦ coacti-
critically ill patients and from healthy vator 1␣) is the master regulator of mi-
subjects that aging, exercise, immobiliza- tochondrial biogenesis (68), which is in-
Figure 3. Twenty-four-year-old man with poly-
trauma. Adenosine triphosphatase stain at pH 9.4
showing type 1 (light) and type 2 (dark) fibers.
From day 1 to day 7, there was a 43% mean
reduction in type 1 fiber cross-sectional area and
a 5% mean reduction in type 2 fiber cross-
sectional area. (Used with permission from the Figure 4. Muscle atrophy– hypertrophy-signaling pathways downstream of insulin-like growth fac-
Musculoskeletal Ultrasound Study in Critical tor-1 (IGF-1). PI3K, phosphoinositide 3-kinase; mTOR, mammalian target of rapamycin; foxO, fork-
Care: Longitudinal Evaluation [MUSCLE] study.) head transcription factors; PGC-1␣, peroxisome proliferator-activated receptor-␦ coactivator 1␣.
S678 Crit Care Med 2010 Vol. 38, No. 10 (Suppl.)
of muscle-specific MURF-1 and atrogin-1. growth hormone had been proposed as an
These ubiquitin ligases, which are the agent to modify the catabolic effects of
proteins that bind and mediate ubiquiti- critical illness by modifying protein turn-
nation, promote skeletal muscle atrophy over and nitrogen balance, in a multina-
and therefore are potential targets for tional, randomized controlled trial it was
drug therapy. An alternative approach shown to increase mortality (83). Myosta-
would be to develop a prohypertrophy tin, or growth factor differentiation factor
drug, such as IGF-1. IGF-1 infused di- 8, in contrast to IGF-1 and testosterone,
rectly into the tibialis anterior muscles of is a negative regulator of muscle mass
mice produced muscle hypertrophy (72). (84). Myostatin knockout animal models
However, in contrast to increased local exhibit a markedly hypertrophied pheno-
IGF-1 expression resulting from muscle type; natural inhibitors of myostatin may
overload (73), increasing circulating have therapeutic value (85). However, the
IGF-1, through growth hormone admin- efficacy of such a treatment needs further
istration, has not resulted in increased evaluation; although the animal data
MPS (74, 75). Finally, the IGF-1 receptor have shown an increase in muscle size,
is ubiquitous and could result in a sys- this hypertrophied muscle generates a
temic effect rather than being limited to lower force per unit area, which is an
skeletal muscle; therefore, targeting it for obvious weakness in any strategy to im-
Figure 5. Muscle atrophy F-box in samples from drug therapy may not provide any bene- prove long-term function.
day 1 and day 7. Data are normalized to ␣-tubulin fits to muscle protein turnover and mus- Nonpharmacologic Strategies. As we
protein expression. (Used with permission from
the Musculoskeletal Ultrasound Study in Critical
cle mass. IGF-1 acts through the phos- have described, there is compelling evi-
Care: Longitudinal Evaluation [MUSCLE] study.) phoinositide 3-kinase (PI3K)/Akt/ dence that ICU-AW exists, with strong
mammalian target of rapamycin (mTOR) supporting evidence that aging, immobi-
pathway (76), a pathway that can be acti- lization, and altered response to dietary
duced by exercise. This also has an vated independent of IGF-1 (77). In ani- amino acids, and insulin have significant
inhibitory effect on forkhead dephosphor- mal studies, activation of phosphoinosi- deleterious effects on skeletal muscle. In
ylation and highlights the complex inter- tide 3-kinase not only results in skeletal an attempt to counteract critical illness
action between different signaling path- muscle hypertrophy but also defends immobility, there has been a recent and
ways. The extent to which this complex against denervation-induced atrophy substantial focus on critical care rehabil-
regulation of signaling pathways is al- (78), whereas an absence of Akt reduces itation, both during and following ICU
tered in the muscles of critically ill pa- muscle mass and results in insulin resis- admission, and assessment of rehabilita-
tients remains to be determined (50, 66, tance (79), depending on which of the tion in terms of functional outcomes in-
70). Preliminary data are becoming avail- three identifiable forms are lacking. How- cluding health-related quality of life and
able; Figure 5 shows the down-regulation ever, human data show that resistance exercise capacity after ICU discharge (47,
of muscle atrophy F-box protein in the training reduces Akt (80). In animal stud- 86 –90). A multicenter randomized con-
quadriceps muscle in a patient following ies, activation of Akt and subsequent ac- trolled study has demonstrated the effi-
a 7-day stay in an ICU. tivation of mammalian target of rapamy- cacy of combined sedation holds and re-
cin increases hypertrophy (77, 81), habilitation in the early stages of critical
Strategies to treat and prevent whereas rapamycin inhibition of mTOR illness with improved functional outcome
muscle loss inhibited hypertrophy (77). Although at hospital discharge (27). More data are
these data provide understanding of the emerging with a number of ongoing tri-
Pharmacologic Strategies. Progress in signaling pathways in animal studies and als; however, to date, there has been little
the understanding of the muscle-signal- selected patient groups, they must be focus on the premorbid condition of the
ing pathways that mediate skeletal mus- confirmed in critically ill patients before patient that may exacerbate neuromuscu-
cle hypertrophy and atrophy allows scien- any clinical intervention trials that target lar complications of critical illness. This
tists to generate hypotheses to facilitate specific pathways are undertaken. It approach to ICU-AW has been driven, in
drug design and discovery. A rational ap- would be reasonable to focus attention in part, by the anabolic effects induced by
proach would be to develop drugs that the first instance on the activity of physical training and the enhanced exer-
either inhibit MPB pathways during skel- MURF-1 and atrogin-1 in the muscle of cise performance observed in patients
etal muscle atrophy, or stimulate MPS critically ill patients, because these mus- with chronic respiratory and cardiac dis-
pathways during hypertrophy, to develop cle-specific ubiquitin ligases are essential ease who have undergone rehabilitation
antiatrophy or prohypertrophy drugs for muscle atrophy and are potentially exercise programs (91, 92). However, the
(Fig. 4). A simple approach for an antiat- the best targets for an antiatrophy drug. common goal of rehabilitation is whole-
rophy drug would be to inhibit the ubiq- Another target for consideration is testos- body exercise which, even with the ad-
uitin proteosome pathways by using pro- terone, used by athletes to improve mus- vances in technology to allow ICU pa-
teosome inhibitors, which would reduce cle size and performance. Clinical trials tients to mobilize while receiving
the rate of proteolysis and atrophy in have shown its efficacy in promoting ventilator support (93, 94), is difficult to
skeletal muscle (71). However, blocking muscle mass (82), but its use as a thera- deliver to all patients due to the resources
these pathways could have a systemic ef- peutic agent needs to be carefully evalu- required. An alternative modality, using
fect on other tissues. This has led to an ated as it has both a prothrombotic and neuromuscular electrical stimulation,
approach to inhibit the enzymatic activity carcinogenic effect. Similarly, although could be a useful additional peripheral
Crit Care Med 2010 Vol. 38, No. 10 (Suppl.) S679
muscle training and rehabilitation tool. mechanical ventilation. Crit Care Med 2004; septic patients. Crit Care Med 2005; 33:
Neuromuscular electrical stimulation has 32:61– 69 349 –354
previously been demonstrated to amelio- 3. Niskanen M, Kari A, Halonen P: Five-year 18. Ali NA, O’Brien JM Jr, Hoffmann SP, et al:
rate the fall in MPS in immobilized mus- survival after intensive care– comparison of Acquired weakness, handgrip strength, and
12,180 patients with the general population. mortality in critically ill patients. Am J Re-
cle (95). This supports the finding from a
Finnish ICU Study Group. Crit Care Med spir Crit Care Med 2008; 178:261–268
recent randomized controlled trial that 19. Tabary JC, Tabary C, Tardieu C, et al: Phys-
1996; 24:1962–1967
neuromuscular electrical stimulation at- 4. National Institute for Health and Clinical Ex- iological and structural changes in the cat’s
tenuates the decline in quadriceps mus- cellence: Rehabilitation after critical illness. soleus muscle due to immobilization at dif-
cle mass in critically ill patients (96). NICE clinical guideline 83. Available at: http:// ferent lengths by plaster casts. J Physiol
Furthermore, neuromuscular electrical www.nice.org.uk/nicemedia/live/12137/43526/ 1972; 224:231–244
stimulation does not require active pa- 43526.pdf. Published March 2009. Accessed 20. Tomanek RJ, Lund DD: Degeneration of dif-
tient cooperation and has been shown to August 23, 2010 ferent types of skeletal muscle fibres. II. Im-
have functional benefits with an increase 5. De Jonghe B, Sharshar T, Lefaucheur JP, et mobilization. J Anat 1974; 118:531–541
in exercise performance, skeletal muscle al: Paresis acquired in the intensive care 21. Fischbach GD, Robbins N: Changes in con-
unit: A prospective multicenter study. JAMA tractile properties of disused soleus muscles.
performance, and health-related quality
2002; 288:2859 –2867 J Physiol 1969; 201:305–320
of life (97–99) in patients with chronic 22. Duchateau J, Hainaut K: Electrical and me-
obstructive pulmonary disease. These 6. Latronico N, Shehu I, Seghelini E: Neuro-
muscular sequelae of critical illness. Curr chanical changes in immobilized human
outcomes need to be evaluated in criti- muscle. J Appl Physiol 1987; 62:2168 –2173
Opin Crit Care 2005; 11:381–390
cally ill patients. 7. Latronico N, Peli E, Botteri M: Critical illness 23. Kortebein P, Ferrando A, Lombeida J, et al:
myopathy and neuropathy. Curr Opin Crit Effect of 10 days of bed rest on skeletal mus-
CONCLUSION Care 2005; 11:126 –132 cle in healthy older adults. JAMA 2007; 297:
8. De Jonghe B, Sharshar T, Hopkinson N, et al: 1772–1774
We consider the next challenge to be Paresis following mechanical ventilation. 24. Kortebein P, Symons TB, Ferrando A, et al:
the development of simple tools to iden- Curr Opin Crit Care 2004; 10:47–52 Functional impact of 10 days of bed rest in
tify patients early in the course of their 9. Griffiths RD, Jones C: Recovery from inten- healthy older adults. J Gerontol A Biol Sci
critical illness. A direct focus on the sive care. BMJ 1999; 319:427– 429 Med Sci 2008; 63:1076 –1081
25. Gibson JN, Halliday D, Morrison WL, et al:
pathophysiologic processes occurring 10. Coakley JH, Nagendran K, Yarwood GD, et al:
Decrease in human quadriceps muscle pro-
within the muscle, in particular muscle Patterns of neurophysiological abnormality
tein turnover consequent upon leg immobi-
morphology, protein turnover, and its re- in prolonged critical illness. Intensive Care
lization. Clin Sci (Lond) 1987; 72:503–509
lationship to the muscle-signaling path- Med 1998; 24:801– 807
26. Seki K, Taniguchi Y, Narusawa M: Alter-
ways, is required. With this approach, we 11. Fletcher SN, Kennedy DD, Ghosh IR, et al:
ations in contractile properties of human
will be able not only to potentially target Persistent neuromuscular and neurophysio-
skeletal muscle induced by joint immobiliza-
logic abnormalities in long-term survivors of
particular pathways with antiatrophy or tion. J Physiol 2001; 530:521–532
prolonged critical illness. Crit Care Med
prohypertrophy drugs but also to use 2003; 31:1012–1016
27. Schweickert WD, Pohlman MC, Pohlman AS,
techniques such as neuromuscular stim- et al: Early physical and occupational therapy
12. Guarneri B, Bertolini G, Latronico N: Long-
ulation to train the quadriceps muscle in in mechanically ventilated, critically ill pa-
term outcome in patients with critical illness
both the early and recovery stages of crit- tients: A randomised controlled trial. Lancet
myopathy or neuropathy: The Italian multi-
2009; 373:1874 –1882
ical illness. All of these interventions, in- centre CRIMYNE study. J Neurol Neurosurg
28. Polkey MI, Kyroussis D, Hamnegard CH, et
cluding studies of the effects of rehabili- Psychiatry 2008; 79:838 – 841 al: Quadriceps strength and fatigue assessed
tation in patients with skeletal muscle 13. de Sèze M, Petit H, Wiart L, et al: Critical by magnetic stimulation of the femoral nerve
weakness during and after critical illness, illness polyneuropathy. A 2-year follow-up in man. Muscle Nerve 1996; 19:549 –555
will need to be correlated with short- and study in 19 severe cases. Eur Neurol 2000; 29. Swallow EB, Gosker HR, Ward KA, et al: A
long-term functional and health-related 43:61– 69 novel technique for nonvolitional assessment
quality of life outcomes. 14. De Jonghe B, Bastuji-Garin S, Durand MC, et of quadriceps muscle endurance in humans.
al: Respiratory weakness is associated with J Appl Physiol 2007; 103:739 –746
limb weakness and delayed weaning in criti- 30. Harris ML, Luo YM, Watson AC, et al: Adduc-
ACKNOWLEDGMENTS cal illness. Crit Care Med 2007; 39: tor pollicis twitch tension assessed by mag-
2007–2015 netic stimulation of the ulnar nerve. Am J
We acknowledge Professor Michael
15. Sharshar T, Bastuji-Garin S, Stevens RD, et Respir Crit Care Med 2000; 162:240 –245
Rennie (University of Nottingham) for his al: Presence and severity of intensive care 31. Harris ML, Moxham J: Measuring respiratory
expert advice and guidance in this work, unit-acquired paresis at time of awakening and limb muscle strength using magnetic
Dr. Anthea Rowlerson for assistance in are associated with increased intensive care stimulation: Measuring respiratory and limb
processing the samples shown in Figures unit and hospital mortality. Crit Care Med muscle strength using magnetic stimulation.
2 and 3, and Chibeza Agley for the West- 2009; 37:3047–3053 Br J Int Care 1998; 8:21–28
ern blot data shown in Figure 5. 16. Garnacho-Montero J, Madrazo-Osuna J, 32. Mills GH, Ponte J, Hamnegard CH, et al:
García-Garmendia JL, et al: Critical illness Tracheal tube pressure change during mag-
polyneuropathy: Risk factors and clinical netic stimulation of the phrenic nerves as an
REFERENCES
consequences. A cohort study in septic pa- indicator of diaphragm strength on the in-
1. Herridge MS, Cheung AM, Tansey CM, et al: tients. Intensive Care Med 2001; 27: tensive care unit. Br J Anaesth 2001; 87:
One-year outcomes in survivors of the acute 1288 –1296 876 – 884
respiratory distress syndrome. N Engl J Med 17. Garnacho-Montero J, Amaya-Villar R, García- 33. Pickles JKS, Harris ML, et al: Medium to
2003; 348:683– 693 Garmendía JL, et al: Effect of critical illness long-term outcomes of critical illness hand
2. Chelluri L, Im KA, Belle SH, et al: Long-term polyneuropathy on the withdrawal from me- muscle weakness. Abstract. Am J Respir Crit
mortality and quality of life after prolonged chanical ventilation and the length of stay in Care Med 2004; 169:783
S680 Crit Care Med 2010 Vol. 38, No. 10 (Suppl.)
34. Seymour JM, Ward K, Sidhu PS, et al: Ultra- involvement of the ubiquitin proteasome sys- Identification of ubiquitin ligases required
sound measurement of rectus femoris cross- tem in human skeletal muscle remodelling for skeletal muscle atrophy. Science 2001;
sectional area and the relationship to quad- and atrophy. Biochim Biophys Acta 2008; 294:1704 –1708
riceps strength in COPD. Thorax 2009; 64: 1782:730 –743 66. Lecker SH, Solomon V, Mitch WE, et al:
418 – 423 51. de Boer MD, Selby A, Atherton P, et al: The Muscle protein breakdown and the critical
35. Narici MV, Landoni L, Minetti AE: Assess- temporal responses of protein synthesis, role of the ubiquitin-proteasome pathway in
ment of human knee extensor muscles stress gene expression and cell signalling in human normal and disease states. J Nutr 1999;
from in vivo physiological cross-sectional quadriceps muscle and patellar tendon to 129(Suppl 1S):227S–237S
area and strength measurements. Eur J Appl disuse. J Physiol 2007; 585:241–251 67. Lecker SH, Jagoe RT, Gilbert A, et al: Multi-
Physiol Occup Physiol 1992; 65:438 – 444 52. Paddon-Jones D, Sheffield-Moore M, Cree ple types of skeletal muscle atrophy involve a
36. Campbell IT, Watt T, Withers D, et al: Muscle MG, et al: Atrophy and impaired muscle pro- common program of changes in gene expres-
thickness, measured with ultrasound, may be tein synthesis during prolonged inactivity sion. FASEB J 2004; 18:39 –51
an indicator of lean tissue wasting in multi- and stress. J Clin Endocrinol Metab 2006; 68. Sandri M, Lin J, Handschin C, et al: PGC-
ple organ failure in the presence of edema. 91:4836 – 4841 1alpha protects skeletal muscle from atrophy
Am J Clin Nutr 1995; 62:533–539 53. Rennie MJ: Muscle protein turnover and the by suppressing FoxO3 action and atrophy-
37. Chi-Fishman G, Hicks JE, Cintas HM, et al: wasting due to injury and disease. Br Med specific gene transcription. Proc Natl Acad
Ultrasound imaging distinguishes between Bull 1985; 41:257–264 Sci USA 2006; 103:16260 –16265
normal and weak muscle. Arch Phys Med 54. Glover EI, Phillips SM, Oates BR, et al: Im- 69. Sacheck JM, Hyatt JP, Raffaello A, et al: Rapid
Rehabil 2004; 85:980 –986 mobilization induces anabolic resistance in disuse and denervation atrophy involve tran-
38. Freilich RJ, Kirsner RL, Byrne E: Isometric human myofibrillar protein synthesis with scriptional changes similar to those of muscle
strength and thickness relationships in hu- low and high dose amino acid infusion. wasting during systemic diseases. FASEB J
man quadriceps muscle. Neuromuscul Dis- J Physiol 2008; 586:6049 – 6061 2007; 21:140 –155
ord 1995; 5:415– 422 55. Volpi E, Mittendorfer B, Rasmussen BB, et al: 70. Kimball SR, O’Malley JP, Anthony JC, et al:
39. Abe T, Kawakami Y, Suzuki Y, et al: Effects of The response of muscle protein anabolism to Assessment of biomarkers of protein anabo-
20 days bed rest on muscle morphology. combined hyperaminoacidemia and glucose- lism in skeletal muscle during the life span
J Gravit Physiol 1997; 4:S10 –S14 induced hyperinsulinemia is impaired in the of the rat: Sarcopenia despite elevated pro-
40. Bleakney R, Maffulli N: Ultrasound changes elderly. J Clin Endocrinol Metab 2000; 85: tein synthesis. Am J Physiol 2004; 287:
to intramuscular architecture of the quadri- 4481– 4490 E772–E780
ceps following intramedullary nailing. 56. Cuthbertson D, Smith K, Babraj J, et al: 71. Tawa NE Jr, Odessey R, Goldberg AL: Inhib-
J Sports Med Phys Fitness 2002; 42:120 –125 Anabolic signaling deficits underlie amino itors of the proteasome reduce the acceler-
41. Ellis S, Kirby LC, Greenleaf JE: Lower ex- acid resistance of wasting, aging muscle. ated proteolysis in atrophying rat skeletal
tremity muscle thickness during 30-day 6 FASEB J 2005; 19:422– 424 muscles. J Clin Invest 1997; 100:197–203
degrees head-down bed rest with isotonic 57. Hermans G, Wilmer A, Meersseman W, et al: 72. Adams GR, McCue SA: Localized infusion of
and isokinetic exercise training. Aviat Space Impact of intensive insulin therapy on neu- IGF-I results in skeletal muscle hypertrophy
Environ Med 1993; 64:1011–1015 romuscular complications and ventilator de- in rats. J Appl Physiol 1998; 84:1716 –1722
42. Akima H, Kawakami Y, Kubo K, et al: Effect pendency in the medical intensive care unit. 73. Hameed M, Orrell RW, Cobbold M, et al:
of short-duration spaceflight on thigh and Am J Respir Crit Care Med 2007; 175: Expression of IGF-I splice variants in young
leg muscle volume. Med Sci Sports Exerc 480 – 489 and old human skeletal muscle after high
2000; 32:1743–1747 58. Dulloo AG, Girardier L: Adaptive changes in resistance exercise. J Physiol 2003; 547:
43. Uremovic M, Pasic MB, Seric V, et al: Ultra- energy expenditure during refeeding follow- 247–254
sound measurement of the volume of mus- ing low-calorie intake: Evidence for a specific 74. Yarasheski KE, Zachwieja JJ, Campbell JA,
culus quadriceps after knee joint injury. Coll metabolic component favoring fat storage. et al: Effect of growth hormone and resis-
Antropol 2004; 28(Suppl 2):227–233 Am J Clin Nutr 1990; 52:415– 420 tance exercise on muscle growth and
44. Reid CL, Campbell IT, Little RA: Muscle 59. Reid CL, Murgatroyd PR, Wright A, et al: strength in older men. Am J Physiol 1995;
wasting and energy balance in critical illness. Quantification of lean and fat tissue repletion 268:E268 –E276
Clin Nutr 2004; 23:273–280 following critical illness: A case report. Crit 75. DeVol DL, Rotwein P, Sadow JL, et al: Acti-
45. Gruther W, Benesch T, Zorn C et al: Muscle Care 2008; 12:R79 vation of insulin-like growth factor gene ex-
wasting in intensive care patients: Ultra- 60. Wolfe RR: Regulation of skeletal muscle pro- pression during work-induced skeletal mus-
sound observation of the M. quadriceps fem- tein metabolism in catabolic states. Curr cle growth. Am J Physiol 1990; 259:E89 –E95
oris muscle layer. J Rehabil Med 2008; 40: Opin Clin Nutr Metab Care 2005; 8:61– 65 76. Rommel C, Bodine SC, Clarke BA, et al: Me-
185–189 61. Kandarian SC, Jackman RW: Intracellular diation of IGF-1-induced skeletal myotube
46. Khan J, Harrison TB, Rich MM: Mechanisms signaling during skeletal muscle atrophy. hypertrophy by PI(3)K/Akt/mTOR and
of neuromuscular dysfunction in critical ill- Muscle Nerve 2006; 33:155–165 PI(3)K/Akt/GSK3 pathways. Nat Cell Biol
ness. Crit Care Clin 2008; 24:165–177, x 62. Jackman RW, Kandarian SC: The molecular 2001; 3:1009 –1013
47. Truong AD, Fan E, Brower RG, et al: Bench- basis of skeletal muscle atrophy. Am J 77. Bodine SC, Stitt TN, Gonzalez M, et al: Akt/
to-bedside review: Mobilizing patients in the Physiol 2004; 287:C834 –C843 mTOR pathway is a crucial regulator of skel-
intensive care unit–from pathophysiology to 63. Tiao G, Hobler S, Wang JJ, et al: Sepsis is etal muscle hypertrophy and can prevent
clinical trials. Crit Care 2009; 13:216 associated with increased mRNAs of the muscle atrophy in vivo. Nat Cell Biol 2001;
48. Phillips SM, Glover EI, Rennie MJ: Alter- ubiquitin-proteasome proteolytic pathway in 3:1014 –1019
ations of protein turnover underlying disuse human skeletal muscle. J Clin Invest 1997; 78. Murgia M, Serrano AL, Calabria E, et al: Ras
atrophy in human skeletal muscle. J Appl 99:163–168 is involved in nerve-activity-dependent regu-
Physiol 2009; 107:645– 654 64. Léger B, Senese R, Al-Khodairy AW, et al: lation of muscle genes. Nat Cell Biol 2000;
49. Greenhaff PL, Karagounis LG, Peirce N, et al: Atrogin-1, MuRF1, and FoXO, as well as 2:142–147
Disassociation between the effects of amino phosphorylated GSK-3beta and 4E-BP1 are 79. Chen WS, Xu PZ, Gottlob K, et al: Growth
acids and insulin on signaling, ubiquitin li- reduced in skeletal muscle of chronic spinal retardation and increased apoptosis in mice
gases, and protein turnover in human mus- cord-injured patients. Muscle Nerve 2009; with homozygous disruption of the Akt1
cle. Am J Physiol 2008; 295:E595–E604 40:69 –78 gene. Genes Dev 2001; 15:2203–2208
50. Murton AJ, Constantin D, Greenhaff PL: The 65. Bodine SC, Latres E, Baumhueter S, et al: 80. Deldicque L, Atherton P, Patel R, et al: De-
Crit Care Med 2010 Vol. 38, No. 10 (Suppl.) S681
crease in Akt/PKB signalling in human skel- 88. Zanni JM, Korupolu R, Fan E, et al: Rehabil- tensive care unit: Improving neuromuscular
etal muscle by resistance exercise. Eur J Appl itation therapy and outcomes in acute respi- weakness and physical function. JAMA 2008;
Physiol 2008; 104:57– 65 ratory failure: An observational pilot project. 300:1685–1690
81. Reynolds TH 4th, Bodine SC, Lawrence JC Jr: J Crit Care 2009; 25:254 –262 95. Gibson JN, Smith K, Rennie MJ: Prevention
Control of Ser2448 phosphorylation in the 89. Burtin C, Clerckx B, Robbeets C, et al: Early of disuse muscle atrophy by means of elec-
mammalian target of rapamycin by insulin exercise in critically ill patients enhances trical stimulation: Maintenance of protein
and skeletal muscle load. J Biol Chem 2002; short-term functional recovery. Crit Care synthesis. Lancet 1988; 2:767–770
277:17657–17662 Med 2009; 37:2499 –2505 96. Gerovasili V, Stefanidis K, Vitzilaios K, et al:
82. Bhasin S, Storer TW, Berman N, et al: The 90. Cuthbertson BH, Rattray J, Campbell MK, et Electrical muscle stimulation preserves the
effects of supraphysiologic doses of testoster- al: The PRaCTICaL study of nurse led, inten- muscle mass of critically ill patients: A ran-
one on muscle size and strength in normal sive care follow-up programmes for improv- domized study. Crit Care 2009; 13:R161
men. N Engl J Med 1996; 335:1–7 ing long term outcomes from critical illness:
97. Neder JA, Sword D, Ward SA, et al: Home
83. Takala J, Ruokonen E, Webster NR: In- A pragmatic randomised controlled trial.
based neuromuscular electrical stimulation
creased mortality associated with growth BMJ 2009; 339:b3723
as a new rehabilitative strategy for severely
hormone treatment in critically ill adults. 91. Mador MJ, Kufel TJ, Pineda LA, et al: Effect of
disabled patients with chronic obstructive
N Engl J Med 1999; 341:785–792 pulmonary rehabilitation on quadriceps fa-
pulmonary disease (COPD). Thorax 2002; 57:
84. Otto A, Patel K: Signalling and the control of tiguability during exercise. Am J Respir Crit
skeletal muscle size. Exp Cell Res 2010 Apr Care Med 2001; 163:930 –935 333–337
18. [Epub ahead of print] 92. Kumar V, Selby A, Rankin D, et al: Age- 98. Zanotti E, Felicetti G, Maini M, et al: Periph-
85. Glass DJ. Signaling pathways perturbing related differences in the dose-response rela- eral muscle strength training in bed-bound
muscle mass. Curr Opin Clin Nutr Metab tionship of muscle protein synthesis to resis- patients with COPD receiving mechanical
Care 2010; 13:225–229 tance exercise in young and old men. ventilation: effect of electrical stimulation.
86. Stevens RD, Hart N, de Jonghe B, et al: J Physiol 2009; 587:211–217 Chest 2003; 124:292–296
Weakness in the ICU: A call to action. Crit 93. Morris PE, Goad A, Thompson C, et al: Early 99. Vivodtzev I, Pépin JL, Vottero G, et al: Improve-
Care 2009; 13:1002 intensive care unit mobility therapy in the ment in quadriceps strength and dyspnea in
87. Puthucheary Z, Hart N: Intensive care unit treatment of acute respiratory failure. Crit daily tasks after 1 month of electrical stimula-
acquired muscle weakness: When should we Care Med 2008; 36:2238 –2243 tion in severely deconditioned and malnour-
consider rehabilitation? Crit Care 2009; 13:167 94. Needham DM: Mobilizing patients in the in- ished COPD. Chest 2006; 129:1540 –1548
S682 Crit Care Med 2010 Vol. 38, No. 10 (Suppl.)
You might also like
- The Osteoporotic Syndrome: Detection, Prevention, and TreatmentFrom EverandThe Osteoporotic Syndrome: Detection, Prevention, and TreatmentNo ratings yet
- Arthritis and Society: The Impact of Musculoskeletal DiseasesFrom EverandArthritis and Society: The Impact of Musculoskeletal DiseasesNo ratings yet
- Early Rehab in ICU May Prevent WeaknessDocument10 pagesEarly Rehab in ICU May Prevent WeaknessCarolina CamposNo ratings yet
- NIH Public Access: Author ManuscriptDocument15 pagesNIH Public Access: Author ManuscriptJ Roberto Meza OntiverosNo ratings yet
- Surgical ICU-AWDocument28 pagesSurgical ICU-AWArmi ZakaNo ratings yet
- Debilidad Neuromuscular Adquirida y Movilizacion Temprana en UTIDocument14 pagesDebilidad Neuromuscular Adquirida y Movilizacion Temprana en UTILucho FelicevichNo ratings yet
- The Impact of Extended Bed Rest On The Musculoskeletal System in The Critical Care EnvironmentDocument8 pagesThe Impact of Extended Bed Rest On The Musculoskeletal System in The Critical Care EnvironmentDavid SugiartoNo ratings yet
- 30 Mekanisme WastingDocument61 pages30 Mekanisme WastingArmi ZakaNo ratings yet
- ICU-acquired Weakness: Narrative ReviewDocument17 pagesICU-acquired Weakness: Narrative ReviewRevista Science and FitnessNo ratings yet
- Timing of Rehabilitation On Length of Stay and Cost in Patients With Hip or Knee Joint Arthroplasty: A Systematic Review With Meta-AnalysisDocument22 pagesTiming of Rehabilitation On Length of Stay and Cost in Patients With Hip or Knee Joint Arthroplasty: A Systematic Review With Meta-AnalysisskNo ratings yet
- Muscular Weakness and Muscle Wasting in The Critically IllDocument14 pagesMuscular Weakness and Muscle Wasting in The Critically IllpamelaNo ratings yet
- Pathophysiology and Management of Critical Illness Polyneuropathy and MyopathyDocument11 pagesPathophysiology and Management of Critical Illness Polyneuropathy and MyopathyWenNo ratings yet
- 262 FullDocument10 pages262 FullDaniel IturriagaNo ratings yet
- Kizilarslanoglu 2016Document7 pagesKizilarslanoglu 2016EviNo ratings yet
- ICU-acquired Weakness: What Is Preventing Its Rehabilitation in Critically Ill Patients?Document4 pagesICU-acquired Weakness: What Is Preventing Its Rehabilitation in Critically Ill Patients?EviNo ratings yet
- Myokine ICU Vanhorebbek 2023Document13 pagesMyokine ICU Vanhorebbek 2023ediNo ratings yet
- Role of Physiotherapy in The Mobilization of PatieDocument9 pagesRole of Physiotherapy in The Mobilization of PatieroblesguzmanmelisaNo ratings yet
- Early Mobilization and Rehabilitation in The ICU Moving Back To The FutureDocument9 pagesEarly Mobilization and Rehabilitation in The ICU Moving Back To The FutureRodrigoSachiFreitasNo ratings yet
- Sharshar 2009 Debil y EstadiaDocument7 pagesSharshar 2009 Debil y EstadiaStefania Anahi MartelNo ratings yet
- Caring Stroke Patients With Musculoskeletal Problem: A Narrative ReviewDocument6 pagesCaring Stroke Patients With Musculoskeletal Problem: A Narrative ReviewIndri Hana EzauwNo ratings yet
- Art 3Document17 pagesArt 3ALEJANDRA GARZÓN CUELLAR.No ratings yet
- 4-1Document9 pages4-1Elahe SadeqiNo ratings yet
- RCCM 200908-1203ocDocument6 pagesRCCM 200908-1203oclsales1986oliNo ratings yet
- Intensive Care Unit-Acquired Weakness in Patients With Acute Kidney Injury A Contemporary ReviewDocument16 pagesIntensive Care Unit-Acquired Weakness in Patients With Acute Kidney Injury A Contemporary ReviewMajooCalderonNo ratings yet
- Physical Therapy Protocols To Attenuate Skeletal Muscle Atrophy in Critically Ill Patients Narrative ReviewDocument11 pagesPhysical Therapy Protocols To Attenuate Skeletal Muscle Atrophy in Critically Ill Patients Narrative ReviewVladimir AlvarezNo ratings yet
- Batt 2013 - ICU-AW - Clinical Phenotypes and Molecular MechanismsDocument9 pagesBatt 2013 - ICU-AW - Clinical Phenotypes and Molecular MechanismsSebastián Caimanque CortésNo ratings yet
- Acute Spinal Cord Injury: Pathophysiology and Pharmacological Intervention (Review)Document18 pagesAcute Spinal Cord Injury: Pathophysiology and Pharmacological Intervention (Review)Jasper CubiasNo ratings yet
- Jurnal Frozen ShoulderDocument21 pagesJurnal Frozen ShoulderMega Mulya Dwi FitriyaniNo ratings yet
- Spondylysis in Young AthletesDocument15 pagesSpondylysis in Young AthletesFer NandoNo ratings yet
- Physiotherapeutic Intervention in A Patient With Spinal Cord Injury (SCI) .Document7 pagesPhysiotherapeutic Intervention in A Patient With Spinal Cord Injury (SCI) .eka aningNo ratings yet
- Functional Limitations Post-COVID-19Document2 pagesFunctional Limitations Post-COVID-19Xavier ChahuillcoNo ratings yet
- Critical Care PDFDocument9 pagesCritical Care PDFAnonymous 3VkEwIsXRNo ratings yet
- BMC Musculoskeletal DisordersDocument12 pagesBMC Musculoskeletal DisordersTeresaNo ratings yet
- JURNAL 18 GordonDocument17 pagesJURNAL 18 GordonResky Ika Sah PutriNo ratings yet
- Clinical ResearcheffectsDocument7 pagesClinical ResearcheffectsJackielyn C. AportaderaNo ratings yet
- Jurnal GerontikDocument8 pagesJurnal GerontikLIZBETH FEMMIL SAPUTRINo ratings yet
- Rober Son 2018Document9 pagesRober Son 2018MeisaNo ratings yet
- 1 s2.0 S0753332220309148 MainDocument7 pages1 s2.0 S0753332220309148 Mainyayu latifahNo ratings yet
- WJC 3 248Document8 pagesWJC 3 248RIAN NUGRAHANo ratings yet
- MO S04 LecturaDocument10 pagesMO S04 LecturaCynthia Ramirez QuintanaNo ratings yet
- Achilles Tendinopathy Evaluation, Rehabilitation,.9Document8 pagesAchilles Tendinopathy Evaluation, Rehabilitation,.9toce auNo ratings yet
- ICU Acquired Weakness: A Review of Epidemiology and PathophysiologyDocument35 pagesICU Acquired Weakness: A Review of Epidemiology and PathophysiologyEviNo ratings yet
- Aichner 2002Document15 pagesAichner 2002cah bagusNo ratings yet
- Intensive-Care-Unit-Acquired Muscle Weakness: Steven Deem MDDocument12 pagesIntensive-Care-Unit-Acquired Muscle Weakness: Steven Deem MDMackarena Pacheco FaundezNo ratings yet
- InterDocument17 pagesInterNita YulindaNo ratings yet
- T Huret 2006Document16 pagesT Huret 2006Tomi Cannel CoalNo ratings yet
- The Rate and Assessment of Muscular Wasting During Critical IllnesDocument26 pagesThe Rate and Assessment of Muscular Wasting During Critical IllnesAdiel OjedaNo ratings yet
- Recovery and Regeneration After Spinal Cord Injury: A Review and Summary of Recent LiteratureDocument9 pagesRecovery and Regeneration After Spinal Cord Injury: A Review and Summary of Recent LiteratureHutsDMNo ratings yet
- This Item Is The Archived Peer-Reviewed Author-Version ofDocument12 pagesThis Item Is The Archived Peer-Reviewed Author-Version ofK scuddsNo ratings yet
- Moore 2019Document5 pagesMoore 2019Tania salais obregonNo ratings yet
- oooDocument10 pagesoooaner cristobal alonso alonsoNo ratings yet
- Article 4Document10 pagesArticle 4umair muqriNo ratings yet
- Fried Frailty Pred Surg Outcomes AmCSurg 10Document8 pagesFried Frailty Pred Surg Outcomes AmCSurg 10edos838No ratings yet
- 1 s2.0 S1530891X20481868 MainDocument9 pages1 s2.0 S1530891X20481868 MainSaugi HudaNo ratings yet
- Prevention of Muscle Atrophy in ICUDocument10 pagesPrevention of Muscle Atrophy in ICUCamilo OsorioNo ratings yet
- NRR 15 1397Document11 pagesNRR 15 1397Nakarit SangsirinawinNo ratings yet
- JurnalDocument8 pagesJurnalAlifia RizqiNo ratings yet
- Fisioterapi Pada ICCUDocument10 pagesFisioterapi Pada ICCUZubaydatul UlumNo ratings yet
- Early MobilizationDocument8 pagesEarly MobilizationMari PaoNo ratings yet
- The Role of Cancer RehabilitationDocument22 pagesThe Role of Cancer RehabilitationLizeth ArceNo ratings yet
- 984 PDFDocument7 pages984 PDFJuan IgnacioNo ratings yet
- Mobilisasi MV ICUDocument12 pagesMobilisasi MV ICUArmi ZakaNo ratings yet
- MV WeaknessDocument25 pagesMV WeaknessArmi ZakaNo ratings yet
- Definisi MVDocument7 pagesDefinisi MVArmi ZakaNo ratings yet
- Female - ICU-AWDocument14 pagesFemale - ICU-AWArmi ZakaNo ratings yet
- Syok Septik - ICU-AWDocument12 pagesSyok Septik - ICU-AWArmi ZakaNo ratings yet
- Comparison of Analgesic Efficacy of Oxycodone And.46Document6 pagesComparison of Analgesic Efficacy of Oxycodone And.46Armi ZakaNo ratings yet
- Epworth Sleepiness Scale in Medical ResidentsDocument9 pagesEpworth Sleepiness Scale in Medical ResidentsArmi ZakaNo ratings yet
- MRC Escala para Evaluar Debilidad Muscular Por Grupos MuscularesDocument1 pageMRC Escala para Evaluar Debilidad Muscular Por Grupos MuscularesMileniNo ratings yet
- Effect of Preoperative Intravenous Oxycodone After Transurethral Resection of Prostate Under General AnesthesiaDocument5 pagesEffect of Preoperative Intravenous Oxycodone After Transurethral Resection of Prostate Under General AnesthesiaArmi ZakaNo ratings yet
- Oral Oxycodone For Acute Postoperative PainDocument20 pagesOral Oxycodone For Acute Postoperative PainArmi ZakaNo ratings yet
- Analgesic Effects of Oxycodone Relative To Those.15Document5 pagesAnalgesic Effects of Oxycodone Relative To Those.15Armi ZakaNo ratings yet
- 2017 Update On Pediatric Sepsis - A ReviewDocument12 pages2017 Update On Pediatric Sepsis - A ReviewYudit ArenitaNo ratings yet
- Effect of Oxycodone Hydrochloride Injection Preemptive Analgesia On SerumDocument4 pagesEffect of Oxycodone Hydrochloride Injection Preemptive Analgesia On SerumArmi ZakaNo ratings yet
- Jurnal TAP BlockDocument12 pagesJurnal TAP BlockArmi ZakaNo ratings yet
- Treatment of Dental Caries in The Young PermanentDocument39 pagesTreatment of Dental Caries in The Young PermanentShahid HameedNo ratings yet
- Cervical Cancer: The Silent KillerDocument19 pagesCervical Cancer: The Silent KillerDennis CosmodNo ratings yet
- NeuropsychiatricDocument18 pagesNeuropsychiatricSamuel JohnsonNo ratings yet
- Inhalation InjuriesDocument4 pagesInhalation InjuriesMohammadAwitNo ratings yet
- Weekly Epi Update 79Document19 pagesWeekly Epi Update 79Lee Ji EunNo ratings yet
- Master Techniques in Orthopaedic Surgery Knee11Document1,137 pagesMaster Techniques in Orthopaedic Surgery Knee11Ameer Ali100% (5)
- Suprarenal GlandDocument19 pagesSuprarenal GlandKay BristolNo ratings yet
- Drug Interactions: Digvijaya Lecturer School of Medical & Allied Sciences GD Goenka UniversityDocument28 pagesDrug Interactions: Digvijaya Lecturer School of Medical & Allied Sciences GD Goenka UniversityDigvijayaNo ratings yet
- Analisis Kesesuaian Penggunaan Antiinfeksi Pada Infeksi Oportunistik Pasien Hiv/Aids Rawat Inap Di Rsup Dr. Sardjito YogyakartaDocument7 pagesAnalisis Kesesuaian Penggunaan Antiinfeksi Pada Infeksi Oportunistik Pasien Hiv/Aids Rawat Inap Di Rsup Dr. Sardjito YogyakartaindahNo ratings yet
- ICRJ-Validation of Cornell Product As A Method of Assessing Left Ventricular HypertrophyDocument5 pagesICRJ-Validation of Cornell Product As A Method of Assessing Left Ventricular Hypertrophysamir raflaNo ratings yet
- Social Treatment in PsychiatryDocument17 pagesSocial Treatment in PsychiatryLawal Sikirat OpeyemiNo ratings yet
- Flower EsscencesDocument2 pagesFlower EsscencesDivyajyoti DevaNo ratings yet
- Anesthesiology GuideDocument4 pagesAnesthesiology GuideGeorge Wang100% (1)
- Psychedelics in Psychiatry-Keeping The Renaissance From Going Off The RailsDocument3 pagesPsychedelics in Psychiatry-Keeping The Renaissance From Going Off The RailsPaloma David VelasquezNo ratings yet
- DM Foot 81Document20 pagesDM Foot 81Zar Ni OoNo ratings yet
- Types of Medications Used After SurgeryDocument9 pagesTypes of Medications Used After SurgeryRegine VillanuevaNo ratings yet
- The Liver Is An Incredibly Hard Working Organ. Every Day, It Performs Hundreds of Critical Functions That Keep Your Body HealthyDocument27 pagesThe Liver Is An Incredibly Hard Working Organ. Every Day, It Performs Hundreds of Critical Functions That Keep Your Body HealthyHafiz Mat JizatNo ratings yet
- TM's Pathology Q BankDocument22 pagesTM's Pathology Q BankChanukya GvNo ratings yet
- Exam 3 lv4Document4 pagesExam 3 lv4Omph IcuNo ratings yet
- Untitled 5 PDFDocument6 pagesUntitled 5 PDFDeepak saxenaNo ratings yet
- D.Pharma 1st Year Health Education and Community Pharmacy Ebook (Udit Pharmacy) by Udit Narayan VishwakarmaDocument82 pagesD.Pharma 1st Year Health Education and Community Pharmacy Ebook (Udit Pharmacy) by Udit Narayan Vishwakarmajaswinder singhNo ratings yet
- Regional Sales Manager Medical Devices in Dallas FT Worth TX Resume James MooreDocument2 pagesRegional Sales Manager Medical Devices in Dallas FT Worth TX Resume James MooreJamesMoore2No ratings yet
- D.R. Form Actual Delivery Form: Brgy. 16-S Quiling Sur, Batac City (077) 670-1920Document8 pagesD.R. Form Actual Delivery Form: Brgy. 16-S Quiling Sur, Batac City (077) 670-1920Fleo GardivoNo ratings yet
- Microorganisms and Their Respective Place in The Living WorldDocument22 pagesMicroorganisms and Their Respective Place in The Living WorldAyesha MasoodNo ratings yet
- Budi Altgpt - Doc NewDocument3 pagesBudi Altgpt - Doc NewIrvanda ENVIOUSNo ratings yet
- Infertility Questionnaire A. General InformationDocument4 pagesInfertility Questionnaire A. General InformationYogita DansenaNo ratings yet
- Domestic Accident: Group 7 Muhammad Afil Rooban Sumitha SanchiaDocument22 pagesDomestic Accident: Group 7 Muhammad Afil Rooban Sumitha SanchiaMuhmd shiyas.HNo ratings yet
- Oxygen Delivery SystemsDocument9 pagesOxygen Delivery Systemsanon_784834955No ratings yet
- AMEBIASISDocument19 pagesAMEBIASISDika Herza Pratama100% (1)
- BUCCAL FAT PAD FLAP REPAIRS SMALL ORAL DEFECTSDocument4 pagesBUCCAL FAT PAD FLAP REPAIRS SMALL ORAL DEFECTSAlex OprisanNo ratings yet