Professional Documents
Culture Documents
Kjim 2022 266
Uploaded by
anahiguerrero1236Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Kjim 2022 266
Uploaded by
anahiguerrero1236Copyright:
Available Formats
Review
Korean J Intern Med 2023;38:282-289
https://doi.org/10.3904/kjim.2022.266
Omega-3 fatty acids and atrial fibrillation
Ji Hye Huh1 and Sang-Ho Jo2
Divisions of 1Endocrinology and 2Cardiology, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea
Although some clinical trials have demonstrated reduced incidence of cardiovascular disease with the use of omega-3 fat-
ty acids, others have found an increased risk of atrial fibrillation (AF). AF is the most common sustained cardiac arrhythmia
worldwide. It is associated with high morbidity and mortality rates and significant public health burden. Previous studies of
the effect of omega-3 fatty acids on AF occurrence have reported contradictory results. Here we reviewed the effect of ome-
ga-3 fatty acids on the risk of AF.
Keywords: Fatty acids, omega-3; Atrial fibrillation; Clinical trials; Cardiovascular diseases; Triglycerides
INTRODUCTION acids (PUFAs) from seafood reduce the development of AF,
human studies have shown conflicting results in this regard
A healthy diet requires fish intake at least twice a week. [8]. A meta-analysis of population-based cohort studies and
The popular belief that fish oil improves cardiovascular (CV) randomized controlled trials (RCTs) showed no significant
health has fueled a lucrative global market for omega-3 fat- role of n-3 fatty acids in the secondary prevention of AF
ty acid supplements. However, it is unknown whether ma- after cardioversion [9,10]. Additionally, accumulating evi-
rine-based omega-3 fatty acids, such as eicosapentaenoic dence from recent large-scale RCTs suggests that the ben-
acid (EPA) and docosahexaenoic acid (DHA), prevent cardio- efits of omega-3 fatty acid supplementation are at the ex-
vascular disease (CVD). Omega-3 fatty acid supplementa- pense of an increased risk of AF.
tion is used to prevent CVD in patients with elevated plas- Because of the contradictory results of previous studies,
ma triglyceride level [1-3]. More than 20 clinical trials have the effect of omega-3 fatty acid supplementation on the
confirmed the benefits of omega-3 fatty acid supplementa- risk of AF should be evaluated. Differences in the dose of
tion and have reported varying results. Therefore, although omega-3 fatty acids used in previous studies might account
omega-3 fatty acids have promising health benefits, certain for the apparent discrepancy in the effects on AF. Here we
issues remain unresolved. reviewed the effect of omega-3 fatty acids on the risk of
Atrial fibrillation (AF) is a common cardiac arrhythmia; AF. Given the increasing use of omega-3 fatty acids for the
its prevalence increases with age, from < 0.5% in indi- treatment of dyslipidemia and CVD prevention, a better un-
viduals in their 40s to 10% in individuals aged > 80 years derstanding of their potential association with AF is import-
[4]. Strategies to prevent AF and its complications, such as ant.
stroke, are important because of the significant morbidity,
mortality, and economic costs of AF. Previous animal stud-
ies showed that omega-3 fatty acids have anti-arrhythmic RANDOMIZED CONTROLLED TRIALS OF THE
effects [5] and treatment with n-3 fatty acids reduces the EFFECTS OF OMEGA-3 FATTY ACID SUPPLE-
AF risk in rabbit models [6]. Additionally, n-3 fatty acids MENTATION AND PLACEBO ON CARDIO-
suppress structural remodeling and atrial fibrosis in canine VASCULAR OUTCOMES
models, which reduce AF occurrence [7]. Although animal
model studies have shown that n-3 polyunsaturated fatty Omega-3 fatty acids supplementation reduces the occur-
Copyright © 2023 The Korean Association of Internal Medicine pISSN 1226-3303
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which eISSN 2005-6648
permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original work is properly cited. http://www.kjim.org
Huh JH and Jo SH. Omega-3 fatty acids and atrial fibrillation
rence of CVD and CVD-related mortality in patients at high- known atherosclerotic cardiovascular disease (ASCVD). Ad-
risk of CVD and in patients with elevated plasma triglycer- ditionally, in a 2 × 2 factorial design, the study also inves-
ide level. In the Reduction of Cardiovascular Events with tigated the effects of low-dose aspirin [14]. The study did
Icosapent Ethyl-Intervention Trial (REDUCE-IT), high-dose not show any significant association of omega-3 fatty acid
omega-3 fatty acid supplementation with highly purified supplementation with the primary outcome. Although the
icosapent ethyl (4 g) was associated with a 25% lower risk original ASCEND trial showed patient-reported adverse out-
of the primary composite CV endpoint; however, the CV comes caused by AF in the overall study participants, the
benefits were inconsistent [11]. Based on the abovemen- post hoc extensive analysis of the electronic health records
tioned findings, the 2019 dyslipidemia guidelines from the of patients with no known AF (n = 15,374; 99% of the
European Society of Cardiology and European Atheroscle- study population) showed no significant difference in AF risk
rosis Society recommend the use of 4 g of icosapent ethyl between participants in the omega-3 fatty acid and placebo
in individuals with established CVD and triglyceride levels groups (7.7% and 7.6%, respectively; rate ratio [RR], 1.02;
of 135 to 499 mg despite statin use [12]. By contrast, the 95% CI, 0.91 to 1.15). A non-fatal ventricular arrhythmia
recent Statin Residual Risk with Epanova in High Cardiovas- was also observed, with no significant difference between
cular Risk Patients with Hypertriglyceridemia (STRENGTH) the omega-3 fatty acid and placebo groups (81 and 54 cas-
trial, which used the same dose of omega-3 fatty acids but es, respectively; RR, 1.49; 95% CI, 1.06 to 2.09; p = 0.02).
used a combination of EPA and DHA, showed no significant In RP, AF events were included as a reported reason for
effect of omega-3 fatty acids on the composite CV end- CVD hospitalization [15]. In the study, AF occurred in 113
point. Moreover, certain other clinical studies demonstrated of 6,239 (1.8%) patients in the experimental arm and 92 of
that low-dose omega-3 fatty acid supplementation did not 6,266 (1.5%) patients in the placebo arm (HR, 1.22; 95%
improve CV outcomes. Furthermore, these trials also raised CI, 0.93 to 1.61; p = 0.15). The study showed that daily
concerns about the potential off-target adverse effects of supplementation with 1 g of omega-3 fatty acids did not
omega-3 fatty acids on the AF risk. Furthermore, RCTs of reduce CV mortality or morbidity in patients with multiple
the effects of omega-3 fatty acid treatment on atrial and CV risk factors.
ventricular arrhythmias have revealed inconsistent results. In In Omega-3 Fatty Acids in Elderly With Myocardial In-
the past 10 years, several RCTs have evaluated the AF risk farction (OMEMI) trial, 1,027 elderly patients with a recent
with omega-3 fatty acid supplementation (Table 1). Low- myocardial infarction were randomized to treatment with
dose omega-3 fatty acid supplementation (≤ 1 g/day) has intermediate dose omega-3 fatty acids (combination of EPA
been evaluated in the Vitamin D and Omega-3 Trial (VITAL) and DHA; 1.8 g/day) or corn oil. After 2 years, there was no
Rhythm study, A Study of Cardiovascular Events in Diabetes significant difference in the primary composite CV endpoint
(ASCEND), and Risk and Prevention Study (RP). between the two groups; however, 7.2% of patients treat-
In the VITAL Rhythm study, 12,542 participants were ed with omega-3 fatty acids developed AF compared to 4%
randomized to receive standard-dose omega-3 fatty acids of patients treated with corn oil (HR, 1.84; 95% CI, 0.98 to
(840 mg/day), containing EPA and DHA, and 12,557 were 3.45; p = 0 .06) [16].
randomized to receive placebo. Cases of incident AF were In the STRENGTH trial, 13,078 patients at high-risk of
identified through self-reported diagnoses and claims data CVD were randomized to treatment with high-dose carbox-
from the Centers for Medicare and Medicaid Services. After ylic acid formulation of omega-3 fatty acids (combination of
a median of 5.3 years, the incidence of AF in individuls re- EPA and DHA; 4 g/day) or corn oil. At a median follow-up
ceiving omega-3 fatty acids and placebo was 7.2 per 1,000 of 42 months, the major composite CV endpoint showed
person-years and 6.6 per 1,000 person-years, respectively no significant difference between the two groups; however,
(hazard ratio [HR], 1.09; 95% confidence interval [CI], 0.96 the risk of AF was higher in the omega-3 fatty acid group
to 1.24; p = 0.19) [13]. compared to the corn oil group (2.2% and 1.3%, respec-
ASCEND, a large-scale mail-based RCT, examined the ef- tively; HR, 1.69; 95% CI, 1.29 to 2.21; p < 0.001) [17].
fects of daily intake of 0.84 g of omega-3 fatty acids (com- In the REDUCE-IT trial, 8,179 participants were ran-
prising EPA and DHA) on the incidence of life-threatening domized to treatment with high-dose omega-3 fatty acids
CV events in individuals with diabetes mellitus but without (4 g/day; similar to that used in the STRENGTH trial), con-
https://doi.org/10.3904/kjim.2022.266 www.kjim.org 283
The Korean Journal of Internal Medicine Vol. 38, No. 3, May 2023
sisting of purified EPA (icosapent ethyl), or mineral oil. In A recent meta-analysis of six RCTs showed that omega-3
line with the STRENGTH trial, there was a significant in- fatty acids were associated with a higher risk of incident AF
crease in the AF risk after treatment with omega-3 fatty ac- compared to placebo (incidence rate ratio [IRR], 1.29; 95%
ids compared to mineral oil (5.3% and 3.9%, respectively; CI, 1.13 to 1.48; p = 0.0002; random effects model) [18].
p = 0.003). After a median follow-up of 4.9 years, icosapent The meta-analysis showed that individuals at high-risk of or
ethyl reduced the primary composite CV outcome by 25% with established CVD and elevated plasma triglyceride levels
compared to mineral oil. were at a higher risk of incident AF with omega-3 fatty acid
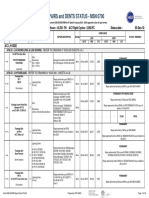
Table 1. Major clinical trials of the risk of atrial fibrillation with omega-3 fatty acid supplementation
Median AF at baseline Total AF
Compar-
Trial Number follow-up, included in Study drug events, Types of AF event Risk of AF
ator
yr the analysis %/yr
VITAL 25,119 5.3 No 1 g/day of ɷ-3 fatty Olive oil 900 New-onset AF Hazard ratio was
(2020) acids (460 mg (0.7) 1.09 (95% CI,
EPA and 380 mg 0.96–1.24;
DHA) p = 0.19)
ASCENDa 15,480 7.4 Yes 1 g/day of ɷ-3 fatty Olive oil 301 Main article: Main article:
(2018) acids (460 mg (0.3) patient-reported Rate ratio was
EPA and 380 mg AF (without 1.23 (95% CI,
DHA) excluding pre- 0.98–1.54).
existing AF); Research letter:
research letter: 1.02 (95% CI,
new-onset AF 0.91–1.15)
Risk and 12,505 5 Yes 1 g/day of ɷ-3 fatty Olive oil 205 Hospitalization Hazard ratio was
Prevention acids (EPA and (0.3) for AF (without 1.23 (95% CI,
study (RP) DHA < 85% in excluding preex- 0.94–1.62;
(2013) ratio from 0.9:1 to isting AF) p = 0.15)
1.5:1)
OMEMI 1,014 2b No 1.8 g/day of ɷ-3 Corn oil 43 (2.1) New-onset AF Hazard ratio was
(2020) fatty acids (930 1.84 (95% CI,
mg EPA and 660 0.98–3.45;
mg DHA) p = 0.06)
STRENGTH 13,078 3.5 Yes 4 g/day of ɷ-3 fatty Corn oil 230 New-onset AF Hazard ratio was
(2020) acids (EPA and (0.5) 1.67 (95% CI,
DHA) 1.28–2.18;
p < 0.001)
REDUCE-IT 8,179 4.9 Yes 4g/day of icosapent Mineral 374 (0.9) New-onset or The calculated
(2019) ethyl (ethyl ester oil worsening AF risk ratio was
of EPA) events (without 1.35 (95% CI,
excluding 1.11–1.65;
preexisting AF) p = 0.003)
AF, atrial fibrillation; VITAL, Vitamin D and Omega-3 Trial; EPA, eicosapentaenoic acid; DHA, docosahexaenoic acid; CI, confidence
interval; ASCEND, A Study of Cardiovascular Events in Diabetes; OMEMI, Omega-3 Fatty Acids in Elderly With Myocardial Infarc-
tion; STRENGTH, Statin Residual Risk with Epanova in High Cardiovascular Risk Patients with Hypertriglyceridemia; REDUCE-IT, Re-
duction of Cardiovascular Events With Icosapent Ethyl-Intervention Trial.
a
The original ASCEND trial publication was used to extract patient-reported AF adverse events. The sensitivity analysis was based
on a post hoc research letter reporting a more comprehensive assessment of AF (n = 1,177) based on electronic health records.
b
The trial’s total sample size was 1,014, but only 759 were included in the AF analysis after excluding those with prevalent AF. Only
the total length of the trial was reported.
284 www.kjim.org https://doi.org/10.3904/kjim.2022.266
Huh JH and Jo SH. Omega-3 fatty acids and atrial fibrillation
supplementation than with placebo treatment. Another creased risk of AF, particularly in trials that used high-dose
meta-analysis of six RCTs also found significantly increased omega-3 fatty acids, as the AF risk is higher at doses > 1 g/day.
risk of AF with omega-3 fatty acid supplementation (IRR, Large-scale trials have shown that omega-3 fatty acid sup-
1.31; 95% CI, 1.13 to 1.51; p = 0.04; random effects mod- plementation may have a dose-dependent protective ef-
el) [19]. Similarly, a recent meta-analysis of seven RCTs and fect against coronary events. Therefore, patients who take
81,210 patients found a 25% increase in AF risk in patients omega-3 fatty acids, particularly at high doses, should be
treated with omega-3 fatty acids compared to those treated informed about the AF risk and monitored for possible de-
with placebo [20]. velopment of this common and dangerous arrhythmia.
Therefore, although previous studies have shown incon-
sistent positive effects of omega-3 fatty acid supplementa-
tion on the composite CV endpoints, most trials have found TYPE AND FORMULATION OF OMEGA-3
an increased risk of AF. FATTY ACIDS AND AF
The U.S. Food and Drug Administration has approved sever-
DOSE OF OMEGA-3 FATTY ACIDS AND AF al prescription omega-3 fatty acid agents for the treatment
of extremely high triglyceride levels [1]. The typical daily
Recent clinical trials suggest, but do not prove, a dose-re- dose of the 1-g omega-3 fatty acid capules is 4 g, which
lated risk of AF with omega-3 fatty acid supplementation. provides > 3 g/day of EPA + DHA. The U.S. Food and Drug
Curfman [21] found that treatment with 4.0 g/day of ome- Administration has approved the n-3 fatty acid products
ga-3 fatty acid was associated with an almost 2-fold in- Lovaza (n-3 acid-ethyl esters [O3AEE]; 0.465 g of EPA and
creased risk of AF, whereas treatment with an intermediate 0.375 g of DHA per capsule; GlaxoSmithKline, Brentford,
dose of 1.8 g/day was not associated with an increased risk UK), Omtryg (similar to O3AEE but not available for clinical
of AF (HR, 1.84). Similarly, there was no apparent increase use; Beckloff Associates, Overland Park, KS, USA), and Vas-
in AF risk at a standard daily dose of 840 mg/day in VITAL cepa (ethyl ester product consisting of EPA without DHA,
Rhythm study [21]. Therefore, the occurrence of AF appears chemically known as icosapent ethyl; Amarin Corp., Dublin,
to be independent of clinical outcomes, with increased in-
cidence of AF in trials that did (e.g., REDUCE-IT) and did
Study HR (95% CI) Weight (%)
not (e.g., STRENGTH) demonstrate significant reductions in
ASCVD occurrence. VITAL 1.09 (0.96-1.24) 21.85
ASCEND 1.23 (0.98-1.54) 14.22
A recent meta-analysis of seven RCTs found that the in-
STRENGTH 1.69 (1.29-2.21) 11.70
cremental risk of AF associated with omega-3 fatty acids
RP 1.22 (0.93-1.61) 11.43
was greater in trials that used > 1 g/day of omega-3 fatty
REDUCE-IT 1.35 (1.11-1.65) 16.13
acid supplementation [22]. The AF risk increases with ome- GISSI-HF 1.10 (0.96-1.26) 21.50
ga-3 fatty acid dose, with HR of 1.12 (95% CI, 1.03 to 1.22; OMEMI 1.84 (0.98-3.45) 3.18
p = 0.024) for doses ≤ 1 g/day to 1.49 (95% CI, 1.04 to Overall 1.25 (1.07-1.46)
2.15; p = 0.042) for doses > 1 g/day. In a meta-regression 0.5 1 2 4
model of the linear association between omega-3 fatty acid HR (95% CI)
dose and risk of AF, the HR for AF increased by 1.11 (95% Heterogeneity: τ2 = 0.01, I2 = 54.57%, H2 = 2.20
CI, 1.06 to 1.15; p = 0.001) for every 1 g increase in the dose Figure 1. Effects of omega-3 fatty acid supplementation on the
of omega-3 fatty acids (residual heterogeneity, I2 = 0.00%; risk of atrial fibrillation. HR, hazard ratio; CI, confidence interval;
VITAL, Vitamin D and Omega-3 Trial; ASCEND, A Study of Car-
p = 0.54) over a dose of 1 to 4 g/day. Sensitivity analysis with
diovascular Events in Diabetes; STRENGTH, Statin Residual Risk
the constant term showed similar results (HR, 1.09; 95% CI, with Epanova in High Cardiovascular Risk Patients with Hypertri-
1.01 to 1.18; p = 0.030 per 1 g increase of omega-3 fatty glyceridemia; RP, Risk and Prevention Study; REDUCE-IT, Reduc-
acid dose) (Fig. 1) [22]. tion of Cardiovascular Events With Icosapent Ethyl-Intervention
Trial; GISSI-HF, Gruppo Italiano per lo Studio della Sopravvivenza
The large-scale RCTs of CV outcomes showed that ome- nell’Insufficienza Cardiaca-Heart Failure; OMEMI, Omega-3 Fatty
ga-3 fatty acid supplementation was associated with in- Acids in Elderly With Myocardial Infarction.
https://doi.org/10.3904/kjim.2022.266 www.kjim.org 285
The Korean Journal of Internal Medicine Vol. 38, No. 3, May 2023
Ireland). The concentrations and ratios of EPA and DHA vary discrepancy between the results of previous studies, the as-
between the preparations. EPA and DHA are present in the sociation between types of prescription omega-3 fatty acids
form of ethyl esters rather than free fatty acids in the ethyl and AF risk should be further evaluated.
ester agents (O3AEE and icosapent ethyl). Notably, the bio-
availability of EPA and DHA also varies between the chem-
ical forms, as products containing ethyl esters have lower OTHER FACTORS RELATED TO THE ASSO-
bioavailability than the free fatty acid forms. Omega-3 fatty CIATION BETWEEN OMEGA-3 FATTY ACIDS
acid supplements have varying effects on CVDs depend- AND AF
ing on the type of omega-3 fatty acid formulation [1], as
EPA and DHA may have variable effects on lipids and lipo- The risk-benefit ratio of omega-3 fatty acids for AF varies ac-
proteins or other metabolic parameters [23]. Based on the cording to its dose and formulation as well as patient char-
results of the REDUCE-IT and Japan EPA Lipid Intervention acteristics. The OMEMI trial showed that individuals aged
Study (JELIS) trials, EPA-alone formulations are increasingly ≥ 75 years had the highest absolute risk difference (> 3%)
being used to reduce the risk of ASCVD [11,24]. Therefore, for developing AF in the omega-3 fatty acid supplement
the AF risk of AF would may vary according to the formula- group. The OMEMI trial investigators used a monitor to
tion of omega-3 fatty acids. record AF occurrences, which may have led to the great-
A recent meta-analysis of RCTs showed increased AF risk er identification of asymptomatic subclinical cases [16]. A
with omega-3 fatty acid treatment when the results of RE- known history of AF may also be a risk factor for AF re-
DUCE-IT trial, which tested only EPA, were excluded [22]. currence after omega-3 fatty acid supplementation. Some
However, it is possible that certain omega-3 fatty acid for- previous studies have reported a higher risk of postopera-
mulations used in the included trials may have different ef- tive AF in patients with elevated omega-3 fatty acid level.
fects on the AF risk. In the OMEMI trial, greater increase However, sensitivity analysis of clinical trials that excluded
in serum phospholipid EPAs was independently associated patients with AF at baseline showed no difference in results
with a lower risk of incident major adverse CV events and a compared to studies that did not exclude patients with AF at
higher risk of new-onset AF [25]. A greater increase in EPA baseline, as well as no significant interaction [22].
was associated with a higher probability of developing AF Because most clinical trials of omega-3 fatty acids were
(adjusted HR, 1.36; 95% CI, 1.07 to 1.72; p = 0.011), with conducted on Western populations, ethnic differences in
a linear relationship [16]. Similarly, the serum phospholipid the association between omega-3 fatty acids and AF should
EPA level was associated with new-onset AF (adjusted HR, be considered. Notably, few studies have investigated the
1.36; 95% CI, 1.07 to 1.72; p = 0.011). By contrast, chang- effects of omega-3 fatty acids supplementation on ventric-
es in the DHA level were not significantly associated with ular arrhythmias in the Asian population. In the JELIS trial,
incident AF after treatment with 1.8 g/day of EPA/DHA (ad- 18,645 Japanese patients with a history of coronary artery
justed HR, 1.29; 95% CI, 0.91 to 1.83; p = 0.16). Similarly, disease and hypercholesterolemia were randomly assigned
no associations were observed between the achieved DHA to 1.8 g/day of EPA plus statin or statin-only groups; sig-
level and AF risk (adjusted HR, 1.29; 95% CI, 0.91 to 1.83; nificantly fewer major coronary events were noted in the
p = 0.15). The ratio of change in EPA level was associated EPA plus statin group compared to the statin-only group.
with incident AF after treatment with 1.8 g/day of EPA/DHA However, AF outcomes related to omega-3 fatty acids were
(HR, 1.35; 95% CI, 1.06 to 1.72; p = 0.01); by contrast, not evaluated as a pre-specified endpoint of the trial. Con-
change in the DHA level was not significantly associated sidering the probable benefit of omega-3 fatty acids on AS-
with the incident AF risk. There was no significant correla- CVD in the Asian population, the AF risk associated with
tion of changes in EPA and DHA levels with incident AF in omega-3 fatty acid supplementation should be investigated
patients randomized to the placebo group (corn oil). in more detail.
A recent study found a consistent inverse association To date, few reports have investigated the effects of ome-
between the EPA content in adipose tissues and AF risk in ga-3 fatty acid supplementation on the AF risk according
both men and women [26]. The DHA content was inversely to the patient-level characteristics. Therefore, to understand
related to the AF risk in women, but not in men. Given the more fully the risk-benefit ratio of omega-3 fatty acids in
286 www.kjim.org https://doi.org/10.3904/kjim.2022.266
Huh JH and Jo SH. Omega-3 fatty acids and atrial fibrillation
high-risk individuals (e.g., older and patients with CV comor- covered to date, with over 2,500 amino acids arranged in
bidities), future trials should include systematic, pre-speci- 38 transmembrane helices. These proteins form homotri-
fied ascertainment and adjudication of AF outcomes assist- meric dome-shaped structures with three upward curved
ed by electrocardiogram monitoring via new smart devices propeller-like blades and a central pore during assembly.
and adjudication by independent clinicians. The blades flatten due to increased mechanical force, which
causes the central pore to open, leading to non-selective
influx of positively charged ions, such as calcium (Fig. 2).
POSSIBLE MECHANISMS UNDERLYING THE Lipids in the cell membranes regulate the conformational
ASSOCIATION BETWEEN OMEGA-3 FATTY changes that result in the opening and closing of the PIEZO
ACIDS AND AF channel. Dietary omega-3 fatty acids are incorporated into
the cardiomyocyte surface membranes, making them thin-
It is unclear how omega-3 fatty acids increase the AF risk. ner and more compliant [29]. The impact of these chang-
Omega-3 fatty acids stabilize the cardiac membrane and es varies according to the type of omega-3 fatty acid used.
protect against arrhythmias, including ventricular arrhyth- DHA slows down the inactivation of PIEZO1 while EPA
mias, through both direct electrophysiologic actions and speeds it up. Therefore, the DHA:EPA ratio might determine
positive effects on biological processes involved in atrial re- the overall effect. A DHA-predominant effect would result
modeling. However, omega-3 fatty acids have direct effects in PIEZO1 activation and increased influx of calcium and
on the activity of cardiac calcium, sodium, and potassium other cations (Fig. 2). Finally, these changes would prolong
ionic currents, which can alter the duration of the ventricu- the action potential, increase the likelihood of delayed af-
lar action potential [27]. Therefore, omega-3 fatty acids may ter-depolarizations and consequently AF, and promote cal-
promote re-entrant arrhythmias, despite being anti-arrhyth- cium-dependent signaling. Other atrial cell types, such as
mic in therapeutic conditions. Several previous studies have fibroblasts, may also express mechanical stress-related sig-
evaluated the electrical characteristics of the ventricular naling through the PIEZO1 channels. Atrial fibroblasts from
wall; few studies have evaluated how omega-3 fatty acids patients with AF have higher PIEZO1 expression levels and
influence the atria. activity than those from patients with sinus rhythm, indicat-
Recently, some studies have found that PIEZO proteins ing that PIEZO1 may promote atrial structural remodeling
mediate the effect of omega-3 fatty acids on AF [28]. The [30]. A pro-arrhythmic environment may result from chang-
PIEZO1/2 proteins are two of the largest ion channels dis- es in voltage-gated ion channels, ionic pumps, cell surface
receptors, and extracellular matrix-cytoskeletal interactions.
In addition, PIEZO1 channels, which are one of several cell
Omega-3 fatty acids membrane characteristics altered by omega-3 fatty acid in-
gestion, also create a pro-arrhythmic environment.
Further mechanistic clinical trials are required to under-
Ca2+ K+ stand the processes by which omega-3 fatty acid supple-
Ext.
mentation increases the AF risk and alters the electrophysi-
1
STRETCH STRETCH
Ca
Piezo
ologic characteristics of the myocardium. This is particularly
BK
Int.
important because of the clinical use of omega-3 fatty acids
Human atrial fibroblasts for the treatment of hypertriglyceridemia and prevention of
ASCVD. Furthermore, additional research is required to un-
Arrhythmic trigger derstand the role of active metabolites with unique charac-
Atrial structural remodeling teristics produced by omega-3 fatty acid consumption.
CONCLUSIONS
Risk of atrial fibrillation ↑
Figure 2. Possible mechanisms underlying the association be-
tween omega-3 fatty acid supplementation and atrial fibrillation. Omega-3 fatty acids supplementation is associated with
https://doi.org/10.3904/kjim.2022.266 www.kjim.org 287
The Korean Journal of Internal Medicine Vol. 38, No. 3, May 2023
increased AF risk, particularly in trials that used high dos- Efficacy and safety of prescription omega-3 fatty acids for the
es. Therefore, several factors should be considered before prevention of recurrent symptomatic atrial fibrillation: a ran-
prescribing omega-3 fatty acids, including their dose, type, domized controlled trial. JAMA 2010;304:2363-2372.
and formulation (fish, dietary fish oil supplements, and puri- 10. Cao H, Wang X, Huang H, et al. Omega-3 fatty acids in the
fied fatty acids), as well as patient-related factors and atrial prevention of atrial fibrillation recurrences after cardioversion:
mechanical milieu. Because the benefits of omega-3 fatty a meta-analysis of randomized controlled trials. Intern Med
acids are dose-dependent, the associated AF risk should be 2012;51:2503-2508.
balanced against the benefit for ASCVD. Patients who take 11. Bhatt DL, Steg PG, Miller M, et al. Cardiovascular risk reduc-
omega-3 fatty acids, particularly at high doses, should be tion with icosapent ethyl for hypertriglyceridemia. N Engl J
informed of the risk of AF and followed up for the possible Med 2019;380:11-22.
development of this common and potentially hazardous ar- 12. Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS guide-
rhythmia. lines for the management of dyslipidaemias: lipid modification
to reduce cardiovascular risk. Eur Heart J 2020;41:111-188.
13. Albert CM, Cook NR, Pester J, et al. Effect of marine omega-3
REFERENCES fatty acid and vitamin D supplementation on incident atrial
fibrillation: a randomized clinical trial. JAMA 2021;325:1061-
1. Skulas-Ray AC, Wilson PW, Harris WS, et al. Omega-3 fatty ac- 1073.
ids for the management of hypertriglyceridemia: a science ad- 14. ASCEND Study Collaborative Group, Bowman L, Mafham M,
visory from the American Heart Association. Circulation 2019; et al. Effects of n-3 fatty acid supplements in diabetes melli-
140:e673-e691. tus. N Engl J Med 2018;379:1540-1550.
2. Hu Y, Hu FB, Manson JE. Marine omega-3 supplementation 15. Risk and Prevention Study Collaborative Group, Roncaglioni
and cardiovascular disease: an updated meta-analysis of 13 MC, Tombesi M, et al. n-3 fatty acids in patients with multiple
randomized controlled trials involving 127 477 participants. J cardiovascular risk factors. N Engl J Med 2013;368:1800-
Am Heart Assoc 2019;8:e013543. 1808.
3. Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto 16. Kalstad AA, Myhre PL, Laake K, et al. Effects of n-3 fatty acid
miocardico. Dietary supplementation with n-3 polyunsaturat- supplements in elderly patients after myocardial infarction: a
ed fatty acids and vitamin E after myocardial infarction: results randomized, controlled trial. Circulation 2021;143:528-539.
of the GISSI-Prevenzione trial. Lancet 1999;354:447-455. 17. Nicholls SJ, Lincoff AM, Garcia M, et al. Effect of high-dose
4. Patel NJ, Deshmukh A, Pant S, et al. Contemporary trends of omega-3 fatty acids vs corn oil on major adverse cardio-
hospitalization for atrial fibrillation in the United States, 2000 vascular events in patients at high cardiovascular risk: the
through 2010: implications for healthcare planning. Circula- STRENGTH randomized clinical trial. JAMA 2020;324:2268-
tion 2014;129:2371-2379. 2280.
5. Kumar S, Kassotis JT. Do omega-3 polyunsaturated fatty acids 18. Lombardi M, Carbone S, Del Buono MG, et al. Omega-3 fatty
prevent atrial fibrillation? Cardiology 2014;127:220-222. acids supplementation and risk of atrial fibrillation: an updat-
6. Ninio DM, Murphy KJ, Howe PR, Saint DA. Dietary fish oil pro- ed meta-analysis of randomized controlled trials. Eur Heart J
tects against stretch-induced vulnerability to atrial fibrillation Cardiovasc Pharmacother 2021;7:e69-e70.
in a rabbit model. J Cardiovasc Electrophysiol 2005;16:1189- 19. Kow CS, Doi SAR, Hasan SS. The coincidence of increased risk
1194. of atrial fibrillation in randomized control trials of omega-3
7. Sakabe M, Shiroshita-Takeshita A, Maguy A, et al. Omega-3 fatty acids: a meta-analysis. Expert Rev Clin Pharmacol 2021;
polyunsaturated fatty acids prevent atrial fibrillation associ- 14:773-775.
ated with heart failure but not atrial tachycardia remodeling. 20. Okereke OI, Vyas CM, Mischoulon D, et al. Effect of long-
Circulation 2007;116:2101-2109. term supplementation with marine omega-3 fatty acids vs
8. Rix TA, Mortensen LM, Schmidt EB. Fish, marine n-3 fatty placebo on risk of depression or clinically relevant depressive
acids, and atrial fibrillation: experimental data and clinical ef- symptoms and on change in mood scores: a randomized clini-
fects. Front Physiol 2012;3:152. cal trial. JAMA 2021;326:2385-2394.
9. Kowey PR, Reiffel JA, Ellenbogen KA, Naccarelli GV, Pratt CM. 21. Curfman G. Omega-3 fatty acids and atrial fibrillation. JAMA
288 www.kjim.org https://doi.org/10.3904/kjim.2022.266
Huh JH and Jo SH. Omega-3 fatty acids and atrial fibrillation
2021;325:1063. 2022;145:1037-1039.
22. Gencer B, Djousse L, Al-Ramady OT, Cook NR, Manson JE, 29. Romero LO, Massey AE, Mata-Daboin AD, et al. Dietary fatty
Albert CM. Effect of long-term marine ɷ-3 fatty acids supple- acids fine-tune Piezo1 mechanical response. Nat Commun
mentation on the risk of atrial fibrillation in randomized con- 2019;10:1200.
trolled trials of cardiovascular outcomes: a systematic review 30. Jakob D, Klesen A, Allegrini B, et al. Piezo1 and BKCa channels
and meta-analysis. Circulation 2021;144:1981-1990. in human atrial fibroblasts: Interplay and remodelling in atrial
23. Mozaffarian D, Wu JH. (n-3) fatty acids and cardiovascular fibrillation. J Mol Cell Cardiol 2021;158:49-62.
health: are effects of EPA and DHA shared or complementary?
J Nutr 2012;142:614S-625S.
Received : August 11, 2022
24. Yokoyama M, Origasa H, Matsuzaki M, et al. Effects of eicos-
Accepted : November 21, 2022
apentaenoic acid on major coronary events in hypercholes-
terolaemic patients (JELIS): a randomised open-label, blinded Correspondence to Sang-Ho Jo, M.D.
Division of Cardiology, Department of Internal Medicine, Hallym Uni-
endpoint analysis. Lancet 2007;369:1090-1098. versity Sacred Heart Hospital, 22 Gwanpyeong-ro 170beon-gil, Don-
25. Myhre PL, Kalstad AA, Tveit SH, et al. Changes in eicosapen- gan-gu, Anyang 14068, Korea
taenoic acid and docosahexaenoic acid and risk of cardiovas- Tel: +82-31-380-3722, Fax: +82-31-386-2269
E-mail: sophi5neo@gmail.com
cular events and atrial fibrillation: a secondary analysis of the https://orcid.org/0000-0002-2063-1542
OMEMI trial. J Intern Med 2022;291:637-647.
CRedit authorship contributions
26. Rix TA, Dinesen P, Lundbye-Christensen S, et al. Omega-3
Ji Hye Huh: data curation, formal analysis, methodology, visualization,
fatty acids in adipose tissue and risk of atrial fibrillation. Eur J writing - original draft; Sang-Ho Jo: conceptualization, funding acqui-
Clin Invest 2022;52:e13649. sition, methodology, writing - review & editing
27. Den Ruijter HM, Berecki G, Opthof T, Verkerk AO, Zock PL, Conflicts of interest
Coronel R. Pro- and antiarrhythmic properties of a diet rich in The authors disclose no conflicts.
fish oil. Cardiovasc Res 2007;73:316-325.
Funding
28. Fatkin D, Cox CD, Martinac B. Fishing for links between This work was supported by grants from Hallym University research
omega-3 fatty acids and atrial fibrillation. Circulation fund 2020 (HURF-2020-12) and the Ministry of SMEs and Startups of
Korea (no. S2722143).
https://doi.org/10.3904/kjim.2022.266 www.kjim.org 289
You might also like
- Mini Project 1 - 1Document9 pagesMini Project 1 - 1Sameer BaraNo ratings yet
- 39ED3050CT - RT49S - AP Service ManualDocument31 pages39ED3050CT - RT49S - AP Service Manualبوند بوند100% (1)
- Omega-3 Fatty Acids For CardioprotectionDocument10 pagesOmega-3 Fatty Acids For Cardioprotectionbalderchow100% (1)
- Jamacardiology Aung 2018 Oi 170076Document10 pagesJamacardiology Aung 2018 Oi 170076jimmyneutron1337No ratings yet
- Aplicações Óleo de Peixe Nos Cuidados Saúde PrimáriaDocument9 pagesAplicações Óleo de Peixe Nos Cuidados Saúde PrimáriaVanessa Gama GalassoNo ratings yet
- Achieving Optimal N 3 Fatty Acid Status The V 2014 The American Journal ofDocument4 pagesAchieving Optimal N 3 Fatty Acid Status The V 2014 The American Journal ofmadhuramfoods.chiralaNo ratings yet
- Omega Fatty Acids and Their Role in Cardiovascular DiseasesDocument13 pagesOmega Fatty Acids and Their Role in Cardiovascular DiseasesSana IqbalNo ratings yet
- Effects of Omega-3 Fatty Acids On Markers of Inflammation in Patients With Chronic Kidney DiseaseDocument9 pagesEffects of Omega-3 Fatty Acids On Markers of Inflammation in Patients With Chronic Kidney DiseaseStefanie SuwitaNo ratings yet
- Introduction Literature Review DoneDocument8 pagesIntroduction Literature Review DoneRahatNo ratings yet
- Acidos Grasos EsencialesDocument5 pagesAcidos Grasos EsencialesEstefanyOrdoñezNo ratings yet
- Do Vegetarians Have To Eat Fish For Optimal Cardiovascular ProtectionDocument5 pagesDo Vegetarians Have To Eat Fish For Optimal Cardiovascular ProtectionRejane RodriguesNo ratings yet
- Omega-3 Supplements and Cardiovascular Diseases: TanaffosDocument9 pagesOmega-3 Supplements and Cardiovascular Diseases: TanaffosNatalia LeeNo ratings yet
- Important Bioactive Properties of Omega-3 Fatty Acids: ReviewDocument7 pagesImportant Bioactive Properties of Omega-3 Fatty Acids: ReviewBao Chi Nguyen NgocNo ratings yet
- Cardiovascular Benefits of Omega-3 Fatty Acids: Clemens Von Schacky, William S. HarrisDocument6 pagesCardiovascular Benefits of Omega-3 Fatty Acids: Clemens Von Schacky, William S. HarrisJuanokNo ratings yet
- Omega 3 FunctionsDocument30 pagesOmega 3 FunctionsFilipos ConstantinNo ratings yet
- OmegaDocument3 pagesOmegadeyaNo ratings yet
- Prostaglandins, Leukotrienes and Essential Fatty AcidsDocument12 pagesProstaglandins, Leukotrienes and Essential Fatty AcidsNatália LopesNo ratings yet
- Nutrients: An Update On Omega-3 Polyunsaturated Fatty Acids and Cardiovascular HealthDocument12 pagesNutrients: An Update On Omega-3 Polyunsaturated Fatty Acids and Cardiovascular HealthIgor BaltaNo ratings yet
- Omega-3 Supplements An IntroductionDocument6 pagesOmega-3 Supplements An IntroductionMeg MelliganNo ratings yet
- Essential Fatty Acids v2Document8 pagesEssential Fatty Acids v2SyamsulNo ratings yet
- Omega 3 1Document6 pagesOmega 3 1Maria Leidy Figueroa AnaconaNo ratings yet
- O3fa CVDDocument10 pagesO3fa CVDSrinivas PingaliNo ratings yet
- Are Diets High in Omega-6 Polyunsaturated Fatty Acids Unhealthy?Document5 pagesAre Diets High in Omega-6 Polyunsaturated Fatty Acids Unhealthy?Julio ToribioNo ratings yet
- Alpha-Linolenic Acid: Heart DiseaseDocument9 pagesAlpha-Linolenic Acid: Heart DiseaseDila DiasuarminNo ratings yet
- Am J Cardiol Deha EpaDocument10 pagesAm J Cardiol Deha EpajoremeNo ratings yet
- Understanding Omega3Document7 pagesUnderstanding Omega3kikevasquezNo ratings yet
- Implementing AHRQ Effective Health Care Reviews: Omega-3 Fatty Acids and Cardiovascular DiseaseDocument3 pagesImplementing AHRQ Effective Health Care Reviews: Omega-3 Fatty Acids and Cardiovascular DiseaseAreej ErhimaNo ratings yet
- Aspirin To Prevent Future CVDDocument10 pagesAspirin To Prevent Future CVDAngelo DestaNo ratings yet
- Omega 3 RCTDocument8 pagesOmega 3 RCTtoooqaaa21No ratings yet
- Fish Oil Supplements Linked With Heart Rhythm DisorderDocument3 pagesFish Oil Supplements Linked With Heart Rhythm DisorderReman AlingasaNo ratings yet
- Omega 3 Fatty Acids 1Document16 pagesOmega 3 Fatty Acids 1sarav dhanuNo ratings yet
- MAY 05-23-Omega-3-Omega-6-Ratio PDFDocument10 pagesMAY 05-23-Omega-3-Omega-6-Ratio PDFJONATHAN KAPLANNo ratings yet
- Omega3 Report PDFDocument25 pagesOmega3 Report PDF4444alisaNo ratings yet
- Fish Consumption Could Protect Your EyesightDocument2 pagesFish Consumption Could Protect Your EyesightandreaNo ratings yet
- Microalgae BetterDocument5 pagesMicroalgae BetteryuwonoyaoNo ratings yet
- Omega 3Document8 pagesOmega 3Mireya AlejandraNo ratings yet
- Mancinelli Omega Balance Table CourseDocument19 pagesMancinelli Omega Balance Table Coursemorasaki003No ratings yet
- Jurnal 3Document8 pagesJurnal 3Fryza SatriaNo ratings yet
- Journal Pre-Proofs: Journal of Advanced ResearchDocument28 pagesJournal Pre-Proofs: Journal of Advanced ResearchAyantika DeyNo ratings yet
- Interaksi Obat 2Document5 pagesInteraksi Obat 2h2blockersNo ratings yet
- For The Prevention of Recurrent Symptomatic Atrial Efficacy and Safety of Prescription Omega-3 Fatty AcidsDocument11 pagesFor The Prevention of Recurrent Symptomatic Atrial Efficacy and Safety of Prescription Omega-3 Fatty AcidsLili VillanuevaNo ratings yet
- Omega 3 Fatty Acids Research PapersDocument8 pagesOmega 3 Fatty Acids Research Papersvevuf1zad1w2100% (1)
- Omega 3Document10 pagesOmega 3RakeshKumarNo ratings yet
- CVD ArticleDocument2 pagesCVD ArticleiacubaNo ratings yet
- OmegaDocument11 pagesOmegaHaninii Suhaila HKNo ratings yet
- March 23rd Article - J Am Heart AssocDocument18 pagesMarch 23rd Article - J Am Heart AssocDylis-Judith Fafa MensahNo ratings yet
- Keseimbangan Omega 3 Dan 6 Terhadap DislipidemiaDocument4 pagesKeseimbangan Omega 3 Dan 6 Terhadap DislipidemiaAhmad YassirNo ratings yet
- The Omega-3 Index: A New Risk Factor For Death From Coronary Heart Disease?Document9 pagesThe Omega-3 Index: A New Risk Factor For Death From Coronary Heart Disease?Igor KhedeNo ratings yet
- Jurnal Nutri3Document11 pagesJurnal Nutri3Winda SariNo ratings yet
- Fish Oil in Rheumatic Diseases.Document8 pagesFish Oil in Rheumatic Diseases.José Isaac Lamas GarcíaNo ratings yet
- Fish Oil and ArrhythmiaDocument7 pagesFish Oil and ArrhythmiaRonald D. KankaNo ratings yet
- Effects of Oleic Acid: Review Article Doi: 10.17546/msd.25609Document8 pagesEffects of Oleic Acid: Review Article Doi: 10.17546/msd.25609Radwan AjoNo ratings yet
- Research Summaries: Benefits of Fish Oil With Footnotes: Alzheimer's Disease, DementiaDocument5 pagesResearch Summaries: Benefits of Fish Oil With Footnotes: Alzheimer's Disease, DementiaPankaj SinghNo ratings yet
- Research Digest: Exclusive Sneak PeekDocument9 pagesResearch Digest: Exclusive Sneak PeekStashaNo ratings yet
- Fish Oil Won't Accelerate Weight LossDocument4 pagesFish Oil Won't Accelerate Weight LossAlfie CahilogNo ratings yet
- Dầu cá cho bệnh tim mạch: một bước ngoặt mới- Báo khoa họcDocument22 pagesDầu cá cho bệnh tim mạch: một bước ngoặt mới- Báo khoa họcNam NguyenHoangNo ratings yet
- Omega-3 and Breast CancerDocument19 pagesOmega-3 and Breast CancerGilmara12No ratings yet
- Fotuhi 2009Document13 pagesFotuhi 2009peri umardianaNo ratings yet
- ScreenshotDocument5 pagesScreenshotAluNo ratings yet
- Omega-3 Oils: Applications in Functional FoodsFrom EverandOmega-3 Oils: Applications in Functional FoodsErnesto HernandezRating: 3.5 out of 5 stars3.5/5 (3)
- A Presentation On-: Dr. Nikhil Oza Intern BvdumcDocument43 pagesA Presentation On-: Dr. Nikhil Oza Intern BvdumcMaheboob GanjalNo ratings yet
- 10th ORLIAC Scientific Program As of 26 Jan 2018Document6 pages10th ORLIAC Scientific Program As of 26 Jan 2018AyuAnatrieraNo ratings yet
- AD1 Elements of Architectural Composition For Placemaking PDFDocument4 pagesAD1 Elements of Architectural Composition For Placemaking PDFAndre Yap100% (1)
- Binder 3 of 4 Dec-2018Document1,169 pagesBinder 3 of 4 Dec-2018Anonymous OEmUQuNo ratings yet
- Science Involved in Floating Paper Clip Science Experiment GuidelinesDocument4 pagesScience Involved in Floating Paper Clip Science Experiment GuidelinesSHIELA RUBIONo ratings yet
- Manual 35S EnglishDocument41 pagesManual 35S EnglishgugiNo ratings yet
- Bahir Dar University BIT: Faculity of Mechanical and Industrial EngineeringDocument13 pagesBahir Dar University BIT: Faculity of Mechanical and Industrial Engineeringfraol girmaNo ratings yet
- 1ST SUMMATIVE TEST FOR G10finalDocument2 pages1ST SUMMATIVE TEST FOR G10finalcherish austriaNo ratings yet
- Chapter 10 - The Mature ErythrocyteDocument55 pagesChapter 10 - The Mature ErythrocyteSultan AlexandruNo ratings yet
- Dialog Bahasa InggirsDocument2 pagesDialog Bahasa InggirsKeRtha NeghaRaNo ratings yet
- Communication Guide: For Vita 62 Compliant VPX Power SuppliesDocument8 pagesCommunication Guide: For Vita 62 Compliant VPX Power Suppliesk.saikumarNo ratings yet
- The Joy Luck Club Book 1Document12 pagesThe Joy Luck Club Book 1loronalicelNo ratings yet
- Tsel Manual ThermoselDocument25 pagesTsel Manual ThermoselPedro AlvelaisNo ratings yet
- Ecotopia Remixed II-FormattedDocument54 pagesEcotopia Remixed II-FormattedthisisdarrenNo ratings yet
- Typical Section SC 10: Kerajaan MalaysiaDocument1 pageTypical Section SC 10: Kerajaan MalaysiaAisyah Atiqah KhalidNo ratings yet
- Chemistry Notes: SUBJECT: Leaving Cert Chemistry Level: TEACHER: Tara LyonsDocument5 pagesChemistry Notes: SUBJECT: Leaving Cert Chemistry Level: TEACHER: Tara LyonsSevinc NuriyevaNo ratings yet
- IPC's 2 Edition of Guidance Manual For Herbs and Herbal Products Monographs ReleasedDocument1 pageIPC's 2 Edition of Guidance Manual For Herbs and Herbal Products Monographs ReleasedRakshaNo ratings yet
- L2 Biostatistics ProbabilityDocument84 pagesL2 Biostatistics ProbabilityAaron CiudadNo ratings yet
- Efficient Rice Based Cropping SystemDocument24 pagesEfficient Rice Based Cropping Systemsenthilnathan100% (1)
- Accuity: High Speed Automated 2D & 3D Optical Gauging Single Click Setup and InspectionDocument4 pagesAccuity: High Speed Automated 2D & 3D Optical Gauging Single Click Setup and InspectionAPPLENo ratings yet
- Frontinus - Water Management of RomeDocument68 pagesFrontinus - Water Management of RomezElfmanNo ratings yet
- Mathematical Modeling of Mechanical Systems and Electrical SystemsDocument49 pagesMathematical Modeling of Mechanical Systems and Electrical SystemsMary DunhamNo ratings yet
- YellowstoneDocument1 pageYellowstoneOana GalbenuNo ratings yet
- ANS: (2.59807m/s2 Horizontal) (1.5m/s2 Vertical) (12.93725 Degree Angle That The Water Surface Makes With The Horizontal)Document5 pagesANS: (2.59807m/s2 Horizontal) (1.5m/s2 Vertical) (12.93725 Degree Angle That The Water Surface Makes With The Horizontal)Lolly UmaliNo ratings yet
- Conformational Analysis: Carey & Sundberg: Part A Chapter 3Document53 pagesConformational Analysis: Carey & Sundberg: Part A Chapter 3Dr-Dinesh Kumar100% (1)
- Biologically Active Compounds From Hops and Prospects For Their Use - Karabín 2016Document26 pagesBiologically Active Compounds From Hops and Prospects For Their Use - Karabín 2016Micheli Legemann MonteNo ratings yet
- Quarter 4 English As Grade 4Document28 pagesQuarter 4 English As Grade 4rubyneil cabuangNo ratings yet