Professional Documents
Culture Documents
Optimal Bowel Resection Margin in Colon Cancer Surgery 2023
Uploaded by
CIRUGÍA ONCOLÓGICA ABDOMENOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Optimal Bowel Resection Margin in Colon Cancer Surgery 2023
Uploaded by
CIRUGÍA ONCOLÓGICA ABDOMENCopyright:
Available Formats
Articles
Optimal bowel resection margin in colon cancer surgery:
prospective multicentre cohort study with lymph node and
feeding artery mapping
Hideki Ueno,a,∗ Kazuo Hase,a Akio Shiomi,b Manabu Shiozawa,c Masaaki Ito,d Toshihiko Sato,e Yojiro Hashiguchi,f Takaya Kusumi,g
Yusuke Kinugasa,h Hideyuki Ike,i Kenji Matsuda,j Kazutaka Yamada,k Koji Komori,l Keiichi Takahashi,m Yukihide Kanemitsu,n Heita Ozawa,o
Masayuki Ohue,p Tadahiko Masaki,q Yasumasa Takii,r Atsushi Ishibe,s Jun Watanabe,t Yuji Toiyama,u Hiromichi Sonoda,v Keiji Koda,w
Yoshito Akagi,x Michio Itabashi,y Takahiro Nakamura,z and Kenichi Sugiharaaa
a
Department of Surgery, National Defense Medical College, Saitama, Japan
b
Division of Colorectal Surgery, Shizuoka Cancer Center Hospital, Shizuoka, Japan
c
Department of Gastrointestinal Surgery, Kanagawa Cancer Center, Kanagawa, Japan
d
Colorectal and Pelvic Surgery Division, Department of Surgical Oncology, National Cancer Center Hospital East, Chiba, Japan
e
Department of Surgery, Yamagata Prefectural Central Hospital, Yamagata, Japan
f
Department of Surgery, Teikyo University School of Medicine, Tokyo, Japan
g
Department of Surgery, Keiyukai Sappro Hospital, Hokkaido, Japan
h
Department of Gastrointestinal Surgery, Tokyo Medical and Dental University, Tokyo, Japan
i
Department of Surgery, Saisei-kai Yokohama-shi Nanbu Hospital, Kanagawa, Japan
j
Second Department of Surgery, School of Medicine, Wakayama Medical University, Wakayama, Japan
k
Department of Gastroenterological Surgery, Coloproctology Center, Takano Hospital, Kumamoto, Japan
l
Department of Gastroenterological Surgery, Aichi Cancer Center Hospital, Aichi, Japan
m
Department of Surgery, Tokyo Metropolitan Cancer and Infectious Diseases Center Komagome Hospital, Tokyo, Japan
n
Department of Colorectal Surgery, National Cancer Centre Hospital, Tokyo, Japan
o
Department of Surgery, Tochigi Cancer Centre, Utsunomiya, Japan
p
Department of Gastroenterological Surgery, Osaka International Cancer Institute, Osaka, Japan
q
Department of Surgery, Kyorin University School of Medicine, Tokyo, Japan
r
Department of Surgery, Niigata Cancer Centre Hospital, Niigata, Japan
s
Department of Gastroenterological Surgery, Yokohama City University Graduate School of Medicine, Kanagawa, Japan
t
Department of Surgery, Gastroenterological Centre, Yokohama City University Medical Centre, Kanagawa, Japan
u
Department of Gastrointestinal and Pediatric Surgery, Mie University Graduate School of Medicine, Mie, Japan
v
Department of Surgery, Shiga University of Medical Science, Shiga, Japan
w
Department of Surgery, Teikyo University Chiba Medical Centre, Chiba, Japan
x
Department of Surgery, Kurume University School of Medicine, Fukuoka, Japan
y
Department of Surgery, Institute of Gastroenterology, Tokyo Women’s Medical University, Tokyo, Japan
z
Laboratory for Mathematics, National Defense Medical College, Saitama, Japan
aa
Tokyo Medical and Dental University, Tokyo, Japan
Summary The Lancet Regional
Health - Western Pacific
Background There are no standardised criteria for the ‘regional’ pericolic node in colon cancer, which represents a
2023;33: 100680
major cause of the international uncertainty regarding the optimal bowel resection margin. This study aimed to
Published Online 18
determine ‘regional’ pericolic nodes based on prospective lymph node (LN) mapping. January 2023
https://doi.org/10.
Methods According to preplanned in vivo measurements of the bowel, the anatomical distributions of the feeding 1016/j.lanwpc.2022.
artery and LNs were determined in 2996 stages I–III colon cancer patients who underwent colectomy with resection 100680
margin >10 cm at 25 institutions in Japan.
Findings The mean number of retrieved pericolic nodes was 20.9 (standard deviation, 10.8) per patient. In all patients
except seven (0.2%), the primary feeding artery was distributed within 10 cm of the primary tumour. The metastatic
pericolic node most distant from the primary tumour was within 3 cm in 837 patients, 3–5 cm in 130 patients, 5–7 cm
in 39 patients and 7–10 cm in 34 patients. Only four patients (0.1%) had pericolic lymphatic spread beyond 10 cm; all
of whom had T3/4 tumours accompanying extensive mesenteric lymphatic spread. The location of metastatic
*Corresponding author. Department of Surgery, National Defense Medical College, 3-2 Namiki, Tokorozawa, Saitama 359-8513, Japan.
E-mail address: ueno_surg1@ndmc.ac.jp (H. Ueno).
www.thelancet.com Vol 33 April, 2023 1
Articles
pericolic node did not differ by the feeding artery’s distribution. Postoperatively, none of the 2996 patients developed
recurrence in the remaining pericolic nodes.
Interpretation The pericolic nodes designated as ‘regional’ were those located within 10 cm of the primary tumours,
which should be fully considered when determining the bowel resection margin, even in the era of complete
mesocolic excision.
Funding Japanese Society for Cancer of the Colon and Rectum.
Copyright © 2022 The Author(s). Published by Elsevier Ltd. This is an open access article under the CC BY license
(http://creativecommons.org/licenses/by/4.0/).
Keywords: Colon cancer; Pericolic lymph node; Regional lymph node; Tumour-node-metastasis classification
Research in context
Evidence before this study lymphatic spread beyond 10 cm was rare (approximately
Internationally, there is a great deal of uncertainty regarding 0.1%). All exceptional cases with positive distant pericolic
the optimal resection margin of the bowel in colon cancer nodes had T3/T4 tumours with massive lymph node
surgery. A major reason for this is that there are no metastasis and experienced a high incidence of recurrence;
standardised criteria for regional pericolic nodes to be this finding indicates that such distant pericolic spread is a
resected in colon cancer surgery, and, as per the tumour– form of systemic, rather than local disease. Furthermore, in
node–metastasis classification, all pericolic nodes are treated 99.8% of patients, one or more feeding arteries were located
as ‘regional’. The conventional concept of feeding artery- in the pericolic region within 10 cm of the primary tumour.
oriented bowel resection often influences surgeons’ readiness Moreover, the distribution of the feeding artery did not
to include two or more feeding arteries in the resection significantly affect the status of the pericolic lymphatic
specimens. In addition, as a result of the recent prevalence spread, although it did affect the mesenteric lymphatic spread
toward performing complete mesocolic excision (CME), the toward the origin of the feeding artery. Finally, intraoperative
length of the resected bowel is often used as a yardstick for identification of the feeding artery was 95% accurate, but this
evaluating specimen quality, and wider resection of the bowel was reduced to 86% in patients with a BMI ≥30.
is regarded as a hallmark of high-quality colon cancer surgery.
Implications of all the available evidence
However, there is currently no robust evidence for the
Based on the actual anatomical distribution of pericolic lymph
advantage of wider resection of the bowel.
node metastasis and its prognostic implication, the 10 cm-
Added value of this study rule is a valid and practical criterion to define regional pericolic
This is the first large-scale, prospective multicentre cohort nodes. Even in the era of CME, it should be emphasized that
study to identify and assess metastatic pericolic lymph node surgical procedures intended to extend bowel resection
distribution in patients with stage I–III colon cancer. The beyond the regional pericolic area do not improve the quality
satisfactory number of pericolic lymph nodes examined and of surgery. This should be fully considered when determining
the methodology whereby intraoperative markings were used the bowel resection margin in curatively-intended surgery for
to identify the location of the lymph nodes and feeding colon cancer.
arteries ensured high-quality lymph node mapping. Pericolic
Introduction metastasis. However, there are currently no global
Lymph node (LN) metastasis is the most common mode standardised criteria for the definition of regional LNs in
of spread in colon cancer, and the oncological outcomes the pericolic region. As per the tumour-node-metastasis
of patients who undergo curative colectomy are greatly classification, all pericolic nodes are treated as regional,
influenced by the quality of surgery, specifically that of and there are no specific sub-classifications based on the
lymphadenectomy. In most patients, the pericolic risk of metastasis in individual LNs.4 This lack of clas-
nodes, i.e., the LNs located along the bowel and mar- sification has greatly contributed to the uncertainty
ginal artery, are the starting site of metastasis.1–3 The regarding the optimal resection margin of the bowel in
optimal extent of bowel resection is closely associated colon cancer.
with how ‘regional’ pericolic nodes are defined, which For example, in surgical textbooks published in the
should be routinely resected due to the potential risk of United States, ‘left partial colectomy’ for tumours
2 www.thelancet.com Vol 33 April, 2023
Articles
located at the descending colon has been introduced as a (Supplemental Table S1) between June 2013 and
procedure to resect the transverse colon and sigmoid December 2017 and were in principle followed up
colon up to the middle of each, as well as all of the according to the JSCCR Guidelines8 were included.
sigmoid arteries except for the most distal.5 According to Patients with multiple colon cancers and those treated
this procedure, the resection margin of the colon should with preoperative adjuvant therapy were excluded. The
reach approximately 20 cm (or longer in some cases) on patient demographics are shown in Table 1. Because
each side of the primary tumour, although the exact tumour location is an essential factor that can affect the
value has not been specified. Meanwhile, the American distribution of positive lymph nodes, it was estimated
Society of Colon and Rectal Surgeons (ASCRS) recom- not only with the conventional categorisation (cecum,
mends that colon resection includes proximal and distal ascending colon, transverse colon, descending colon,
margins of 5–7 cm in order to ensure the adequate and sigmoid colon: categorisation 1), but with the cate-
removal of pericolic nodes at risk of metastasis.6 In gorisation of whether the tumor is located at the flexure
addition, a previous study highlighted a significant in- portion or non-flexure portion of the colon (categoriza-
ternational difference in the length of bowel resected in tion 2).
colon cancer surgery. For instance, in a leading German The incidence of recurrence associated with the
institution adopting complete mesocolic excision length of the bowel resected was investigated in these
(CME), the median length of large bowel specimens 2996 patients using surveillance information in January
resected for left-side tumours was 38 (32–43) cm, but 2020. The median follow-up period was 44 (0–76)
was only 15 (13–20) cm in Japanese institutions adopt- months. A total of 300 patients (10.0%) developed
ing D3 dissection.7 recurrent disease (local, regional, or distant recurrence),
This multicentre cohort study conducted by the and the 3-year relapse-free survival (RFS) rate was 88.5%
Japanese Society for Cancer of the Colon and Rectum as calculated by the Kaplan–Meier method.
(JSCCR) prospectively assessed metastatic LN distribu-
tion, focusing on the distance from the primary tumour
and the anatomical association with feeding artery Bowel resection and in vivo markings on the bowel
location (UMIN000030331). The main purpose of this and feeding artery
study was to determine the criteria for ‘regional’ peri- Bowel resection was performed to include all pericolic
colic nodes to facilitate the standardisation of colon LNs defined as ‘regional’ according to both the 10-cm
cancer surgery by ascertaining the optimal length of rule (Supplemental Fig. S2) and the feeding-artery-
bowel resection. oriented rule (Supplemental Fig. S3). Consequently, all
patients received colectomy with a bowel resection
margin of at least 10 cm. Patients who had no feeding
Patients and methods arteries within 10 cm of the primary tumour received a
Patients wider bowel resection to include all LNs between the
This study was conducted according to the Declaration primary tumour and 5 cm from the primary feeding
of Helsinki and comparable Japanese ethical standards. artery.
The study was approved by the Institutional Review The anatomical location of the feeding artery and
Boards of the JSCCR and each participating institution. LNs were determined based on preplanned in vivo
Written informed consent was obtained from all study measurements of the bowel. More specifically, before
participants. resecting the bowel, in the natural state with no external
This is a multicentre, prospective cohort study. The tension, points were marked respectively on the bowel
pre-determined target sample size of this study deter- (the colon or terminal ileum) by serosal sutures at 3, 5, 7
mined on the basis of the consensus of opinion among and 10 cm from the proximal and distal edges of the
the investigators in terms of the validity of sub- tumour. The distal end of the primary feeding artery
population analysis according to T stage was 3000, and was also marked with a stitch during the operation.
a total of 3102 patients were enrolled in this study to
examine the anatomical distribution of metastatic LNs
(Supplemental Fig. S1). After excluding 106 patients Back-table procedures: Identification of feeding
who were ineligible for analysis {48 patients with rectal arteries in the resected specimens
cancer, 14 patients with distant metastasis, one patient After resecting the bowel, the primary feeding artery
with benign disease, 38 patients with missing data, and (i.e., the branch of the superior or inferior mesenteric
5 patients withdrawn from the study based on the artery located closest to the primary tumour) was iden-
request from the institution due to any ineligible criteria tified in fresh surgical specimens and its anatomical
which had been found after registration}, 2996 patients location was recorded (Fig. 1). The distance between the
with histologically proven adenocarcinoma, classified as distal end of the primary feeding artery and the closest
pathological stage I, II or III colon cancer, who received edge of the primary tumour was determined according
curative surgery at 25 institutions in the JSCCR to the intraoperative marking stitches on the bowel.
www.thelancet.com Vol 33 April, 2023 3
Articles
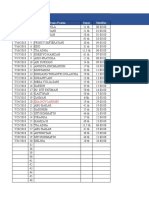
Factors
Age of patients, mean (SD) 68.8 (11.2)
Sex, number (%) Male, 1528 (51.0)
Female, 1468 (49.0)
Body mass index, mean (SD) 22.6 (3.5)
Surgical approach, number (%) Open, 889 (29.7)
Laparoscopic, 2107 (70.3)
Intraoperative marking, number (%) Under direct vision, 2903 (96.9)
Laparoscopically, 93 (3.1)
Number of LN retrieved, mean (SD) All: 30.8 (15.0)
Pericolic: 20.9 (10.8)
Intermediate: 6.3 (4.8)
Main: 3.6 (4.1)
Main LN dissection, number (%) Yes: 2436 (81.3)
No: 560 (18.7)
Pathological T stage, number (%) T1: 574 (19.2)
T2: 440 (14.7)
T3: 1443 (48.2)
T4a: 449 (15.0)
T4b: 90 (3.0)
Pathological N stage, number (%) N0: 1880 (62.8)
N1: 792 (26.4)
N2: 324 (10.8)
Lymph node positivity (%) Overall: 1116 (37.3)
Pericolic: 1044 (34.8)
Intermediate: 257 (8.6)
Main: 68 (2.8)a
Tumour differentiationb, number (%) Well: 1248 (41.7)
Mod: 1552 (51.8)
Por: 91 (3.0)
Muc: 99 (3.3)
Others: 6 (0.2)
Tumour location [categorization 1]c, number (%) C: 368 (12.3)
A: 989 (33.0)
T: 459 (15.3)
D: 215 (7.2)
S: 965 (32.2)
Tumour location [categorization 2], number (%) Hepatic flexure: 262 (8.7)
Splenic flexure: 154 (5.1)
Others: 2580 (86.1)
Proximal and distal length of bowel resected (cm) according to C: 11.7 (4.5) and 12.2 (4.4)
tumour location-1, mean (SD) A: 13.1 (5.5) and 12.2 (4.3)
T: 15.7 (7.8) and 11.6 (3.6)
D: 11.4 (4.8) and 12.2 (4.9)
S: 10.7 (2.7) and 11.4 (3.7)
Proximal and distal length of the resected bowel (cm) according to Hepatic flexure: 18.1 (8.4) and 11.4 (2.8)
tumour location [categorisation 2], mean (SD) Splenic flexure: 11.5 (4.3) and 12.6 (5.5)
Others: 11.9 (4.7) and 11.8 (4.1)
Postoperative adjuvant chemotherapyd, number (%) CAPOX: 387 (12.9) [249 (8.3)]
Capecitabine: 322 (10.7) [250 (8.3)]
UFT/leucovorin: 173 (5.8) [136 (4.5)]
FOLFOX: 53 (1.8) [38 (1.3)]
SOX: 21 (0.7) [15 (0.5)]
S-1: 15 (0.5) [11 (0.4)]
5-fluorouracil/leucovorin: 11 (0.4) [11 (0.4)] none: 2008 (67.0)
uncertain: 6 (0.2)
LN: lymph node, SD: standard deviation. aIn patients who underwent main LN dissection (n = 2436). bWel, Mod, Por, and Muc represent well differentiated
adenocarcinoma, moderately differentiated adenocarcinoma, poorly differentiated adenocarcinoma, and mucinous carcinoma, respectively. cC, A, T, D, and S represent the
cecum, ascending colon, transverse colon, descending colon, and sigmoid colon, respectively. dCAPOX: a chemotherapy combination including capecitabine and oxaliplatin;
UFT: tegafur and uracil; FOLFOX: a chemotherapy combination including 5-fluorouracil, leucovorin, and oxaliplatin; SOX: a chemotherapy combination including S-1 and
oxaliplatin; numbers in square brackets represent those of patients who completed adjuvant chemotherapy.
Table 1: Background of the 2996 colon cancer patients analysed.
4 www.thelancet.com Vol 33 April, 2023
Articles
A B
Fig. 1: Identification of the primary feeding artery and lymph nodes, and their categorisation in the resected surgical specimens. The
resected fresh surgical specimens were pinned on corkboard in a fan shape, with the feeding artery stump and both sides of the bowel stumps
stretched out, and the mesocolic fascia was peeled off using surgical scissors (IA). The mesenteric fatty tissues were removed piecemeal with
scissors to visually identify the feeding/marginal arteries and lymph nodes (IB). The distance between the distal end of the primary feeding
artery and the closest edge of the primary tumour (double-headed arrow) was recorded according to the intraoperative marking stitches on the
bowel (II). The lymph nodes were classified into pericolic, intermediate and main lymph nodes according to the Japanese Classification of Cancer
of the Colon and Rectum (Supplemental Fig. S4). Pericolic lymph nodes were collected by groups, according to the intraoperative serosal sutures
made at 3, 5, 7 and 10 cm from the primary tumour (i.e., primary tumour region, 0 < D ≤ 3 [proximal/distal], 3 < D ≤ 5 [proximal/distal],
5 < D ≤ 7 [proximal/distal], 7 < D ≤ 10 [proximal/distal] and D > 10 [proximal/distal] groups) and were separately submitted to pathological
examination. The abovementioned processes were performed by surgeons. D: Distance from the closer primary tumour edge (cm).
Back-table procedures: LN retrieval and Japanese Classification of Colorectal Carcinoma issued by
categorisation the JSCCR (Supplemental Fig. S4).9,10 The pericolic
LNs were retrieved from the resected surgical speci- nodes were subcategorised according to the distance
mens and categorised as pericolic, intermediate, or from the primary tumour (D) determined by the intra-
main LNs based on the LN grouping system of the operative marking stitches on the bowel (Fig. 1) as
www.thelancet.com Vol 33 April, 2023 5
Articles
follows: (1) primary tumour region, (2) 0 < D ≤ 3 cm assess differences in the number of LNs retrieved/
(proximal/distal sides), (3) 3 < D ≤ 5 cm (proximal/distal involved, feeding artery distribution, accuracy of intra-
sides), (4) 5 < D ≤ 7 cm (proximal/distal sides), (5) operative identification of the feeding artery and recur-
7 < D ≤ 10 cm (proximal/distal sides) and (6) D > 10 cm rence rates. Test of Spearman’s rank correlation
(proximal/distal sides). coefficient and Cochran-Armitage trend test were used
The procedures that were performed to identify the to assess associations between the location of the pri-
feeding/marginal arteries and to retrieve LNs were mary feeding artery and pericolic tumour spread or
exclusively performed by surgeons. LNs were patholog- tumour spread along supplying arteries. The RFS (time
ically examined in routine diagnostic practice at each from surgery to the first recurrence or death) was esti-
institution with the conventional method with hema- mated using the Kaplan–Meier method. Alive patients,
toxylin and eosin staining for a representative section of including those who were lost to follow-up, were
the LN. Tumor nodules with no pathological evidence of censored at their last follow-up date. All statistical
LN structure are considered as LN metastases, irre- analyses were performed using R version 3.6.1
spective of their size and contour morphology. (R Foundation, Vienna, Austria) by an experienced
mathematical statistician (TN).
Statistical analyses
The study endpoints were to determine the anatomical
distribution of metastatic LNs, and the incidence of Role of the funding source
recurrence associated with insufficient lengths of bowel This study was supported by the Fund of the Japanese
resection (https://upload.umin.ac.jp/cgi-open-bin/ctr_ Society for Cancer of the Colon and Rectum (JSCCR).
e/ctr_view.cgi?recptno=R000034640). No pharmaceutical company nor other agency were
The analysis of variance (ANOVA) and t-test were involved in this study and this research received no
used for continuous variables and the chi-square test or specific grant funding with no role of the funding
Fisher’s exact test was used for categorical variables to source in this work.
Intraoperative marking stitch
Pericolic lymph nodes
Distal Proximal
tumour tumour
10 cm 7 cm 5 cm 3 cm edge edge 3 cm 5 cm 7 cm 10 cm
Distal Marginal artery Proximal
Primary feeding artery
Mean number of lymph nodes harvested (SD)
0·4 (1·5) 1·3 (1·6) 1·5 (1·6) 1·9 (1·9) 2·6 (2·4) 5·1 (4·6) 2·5 (2·4) 1·9 (2·2) 1·6 (2·0) 1·5 (2·1) 0·7 (2·4)
Number of patients with lymph node metastasis (%)
3 (0·1) 19 (0·6) 22 (0·7) 74 (2·5) 231 (7·7) 814 (27·2) 245 (8·2) 103 (3·4) 29 (1·0) 19 (0·6) 1 (0·0)
Location of the primary feeding artery: number of patients (%)
3 (0·1) 17 (0·6) 18 (0·6) 84 (2·8) 333 (11·1) 1828 (61·0) 494 (16·5) 162 (5·4) 29 (1·0) 24 (0·8) 4 (0·1)
Fig. 2: Actual status of the distribution of pericolic lymph nodes and the primary feeding artery. The number of lymph nodes, incidence of
lymph node metastasis and location of the primary feeding artery are shown according to the segments determined by in vivo marking stiches
made at 3, 5, 7 and 10 cm from the primary tumour. SD: Standard deviation.
6 www.thelancet.com Vol 33 April, 2023
Articles
T-stage Overall P-value Pericolic segments subdivided by the distance from the primary tumour (cm)a
Primary tumour 0<D≤3 3<D≤5 5<D≤7 7 < D ≤ 10 D > 10
region
Mean and SD of the number of T1 (n = 574) 17.7 (9.8) <0.0001b 3.3 (3.4) 4.7 (3.4) 3.6 (2.9) 3.0 (2.8) 2.5 (2.6) 0.8 (2.3)
retrieved lymph nodes per patient T2 (n = 440) 20.7 (10.8) 4.6 (4.3) 5.1 (3.7) 3.9 (3.1) 3.1 (2.9) 2.9 (3.6) 1.0 (2.8)
T3 (n = 1443) 21.1 (10.1) 5.4 (4.6) 5.1 (3.5) 3.7 (2.9) 3.1 (2.6) 2.7 (2.7) 1.1 (2.6)
T4a (n = 449) 23.9 (13.0) 6.6 (5.2) 5.4 (3.6) 4.1 (3.1) 3.5 (2.8) 3.0 (2.9) 1.4 (5.3)
T4b (n = 90) 25.1 (10.6) 7.5 (5.6) 5.8 (3.7) 4.3 (3.1) 3.0 (2.6) 3.2 (3.0) 1.2 (2.8)
All (n = 2996) 20.9 (10.8) 5.1 (4.6) 5.1 (3.5) 3.8 (3.0) 3.2 (2.7) 2.7 (2.9) 1.1 (3.1)
The number of patients with metastatic T1 (n = 574) 68 (11.8) <0.0001c 38 (6.6) 23 (4.0) 15 (2.6) 3 (0.5) 1 (0.2) 0
pericolic lymph nodes (%) T2 (n = 440) 111 (25.2) 75 (17.0) 47 (10.7) 17 (3.9) 5 (1.1) 6 (1.4) 0
T3 (n = 1443) 534 (37.0) 418 (29.0) 204 (14.1) 83 (5.8) 22 (1.5) 19 (1.3) 2 (0.1)
T4a (n = 449) 277 (61.7) 235 (52.3) 114 (25.4) 42 (9.4) 16 (3.6) 8 (1.8) 2 (0.4)
T4b (n = 90) 54 (60.0) 48 (53.3) 18 (20.0) 7 (7.8) 3 (3.3) 1 (1.1) 0
All (n = 2996) 1044 (34.8) 814 (27.2) 406 (13.6) 164 (5.5) 49 (1.6) 35 (1.2) 4 (0.1)
D: distance from the closer primary tumour edge (cm), SD: standard deviation. aSum of the number of lymph node (upper row) and patient (lower row) both proximal and distal to the primary tumour.
b
ANOVA. cChi-square test.
Table 2: Pericolic lymph nodal status according to pathological T stage.
Results patients (0.1%) had LN involvement within >10 cm of
Pericolic nodal status according to the distance the primary tumour.
from the primary tumour Four cases with pericolic LN involvement >10 cm
The anatomical distribution of the pericolic LNs is from the primary tumour were reported from different
shown in Fig. 2. The primary tumour region had the institutions. All had extensive LN metastasis, defined as
largest number of LNs {mean, 5.1; standard deviation the involvement of ≥10 LNs and/or main LN involve-
(SD), 4.6}, and the number decreased according to the ment (Supplemental Table S2).
distance from the primary tumour. The total number of Although the anatomical distribution of positive LNs
retrieved pericolic nodes was 20.9 (SD, 10.8) per patient, was associated with the T stage, only 2 (0.1%) of 1443
and the number was significantly associated with the T- patients with T3 tumours and 2 (0.4%) of 449 patients
stage, ranging from 17.7 (SD, 9.8) for T1 to 25.1 (SD, with T4a tumours had positive pericolic nodes located
10.6) for T4b (Table 2). >10 cm from the primary tumour (Fig. 3). Similarly, the
Overall, 1044 (34.8%) out of 2996 patients had incidence of patients with pericolic positive nodes
pericolic LN metastasis. Among the 11 pericolic seg- located >5 cm from the primary tumour was <1% in T1
ments made according to the in vivo marking stiches at tumours. The anatomical distribution of positive LNs in
3, 5, 7 and 10 cm from the primary tumour, the inci- the pericolic region did not differ significantly depend-
dence of LN metastasis was highest in the primary ing on the location of the primary tumour (Table 3).
tumour region (27.2%) and decreased with increasing
distance from the primary tumour (Fig. 2). There was
no significant difference in the anatomical distribution Anatomical distribution of the feeding arteries and
of the positive pericolic nodes between the proximal their association with the location of the
and distal sides (P = 0.41). The incidence of metastasis metastatic LNs
in LNs located ≥7 cm from the primary tumour was Among 2996 patients, a feeding artery flowed into the
<1% both proximal and distal to the primary tumour. pericolic region within 10 cm of the primary tumour in
The incidence according to the T-stage is shown in 2989 (99.8%), and 1828 patients (61.0%) had a feeding
Table 2. artery that flowed into the primary tumour region
The metastatic LNs were confined within the pri- (Fig. 2). In four of the seven cases with no feeding artery
mary tumour region in 528 patients (17.6%) (Fig. 3). within 10 cm of the primary tumour, the primary
The most distant metastatic LNs were distributed tumour was located at the splenic flexure (Supplemental
outside the primary tumour region in 516 patients Table S3).
(17.2%): 0 < D ≤ 3 cm segment in 309 patients (10.3%), The distance of the primary feeding artery from the
3 < D ≤ 5 cm segment in 130 patients (4.3%), primary tumour differed significantly depending on
5 < D ≤ 7 cm segment in 39 patients (1.3%) and the location of the primary tumour (Table 4). The
7 < D ≤ 10 cm segment in 34 patients (1.1%). Only four feeding artery distributed most closely to the primary
www.thelancet.com Vol 33 April, 2023 7
Articles
Intraoperative marking stitch
Metastatic pericolic node
Most distant metastatic pericolic node
Proximal/distal
tumour edge 3 cm 5 cm 7 cm 10 cm
Overall 528 309 130 39 34 4
n = 2,996 (17·6) (10·3) (4·3) (1·3) (1·1) (0·1)
Subgroups according to the pathological T-stage
T1, n = 574 32 (5·6) 20 (3·5) 12 (2·1) 3 (0·5) 1 (0·2) 0
T2, n = 440 48 (10·9) 39 (8·9) 14 (3·2) 4 (0·9) 6 (1·4) 0
T3, n = 1,443 277 (19·2) 155 (10·7) 65 (4·5) 17 (1·2) 18 (1·2) 2 (0·1)
T4a, n = 449 138 (30·7) 84 (18·7) 33 (7·3) 12 (2·7) 8 (1·8) 2 (0·4)
T4b, n = 90 33 (36·7) 11 (12·2) 6 (6·7) 3 (3·3) 1 (1·1) 0
Pericolic lymphatic 17·2 [15·9–18·6]
spread to the outside Tumour
edge 6·9 [6·0–7·8]
of the primary tumour 3 cm
region (%) 2·6 [2·0–3·1]
5 cm
1·3 [0·9–1·7]
7 cm
0·1 [0·0–0·3]
10 cm
Fig. 3: Location of the most distant metastatic pericolic lymph node. The pericolic region was divided into six segments according to the
in vivo marking stiches made at 3, 5, 7 and 10 cm from the primary tumour. The figures demonstrate the number (%) of patients whose most
distant metastatic pericolic lymph node was located in each segment, irrespective of being distal and proximal to the primary tumour. Note that
the primary tumour region was the most common segment to harbour the most distant pericolic lymph node involvement, and the incidence
decreased as the distance from the primary tumour increased. The values in the brackets indicate 95% confidence intervals.
tumour in patients with cecum cancer, followed by Accuracy of intraoperative identification of the
those with sigmoid colon cancer. In patients with feeding arteries
ascending, transverse or descending colon cancers, the Postoperative examination of the resected surgical
primary feeding artery was more distant from the pri- specimens showed that the intraoperative marking for
mary tumour as compared with in those with cecum or the feeding arteries was judged as correct in 2853 of the
sigmoid colon cancers. In patients with tumours 2996 patients (95.2%). The accuracy of the intra-
located at the splenic flexure, the proportion of patients operative identification of the feeding arteries was
with a feeding artery >5 cm from the primary tumour significantly associated with BMI (P < 0.0001) (Table 5).
was higher, and the mean distance of the primary
feeding artery from the primary tumour was greater
than that in patients with tumours located at other Postoperative oncological events according to
colon segments. pericolic LN status
Despite a significant difference in the distribution of None of the included patients experienced recurrence in
the primary feeding artery according to the location of the pericolic LN, although we did observe anastomotic
the primary tumour, the anatomical distribution of the recurrence, likely due to tumour implantation at the
positive pericolic LNs was not significantly affected by anastomotic site, in six patients (0.2%) during the
the location of the primary feeding artery (Table 3). In observation period. The recurrence-free survival at 3
contrast, metastasis in intermediate and/or main LNs years was calculated according to the location of the
was observed significantly more frequently in patients most distant metastatic pericolic node as 80.4%, 79.1%,
whose feeding artery was distributed within the primary 76.2%, 62.7%, and 69.7% for patients with the most
tumour as compared with those in which it was more distant metastatic pericolic node within the primary
distant from the primary tumour (Table 3). tumour, within 3 cm of the primary tumour, within
8 www.thelancet.com Vol 33 April, 2023
Articles
Location of the primary Total number No metastasis Pericolic tumour spread (location of the most distant metastatic pericolic LN) Tumour spread along
tumour and primary of patients (%) in pericolic LNs supplying arteriesa
feeding artery
Primary 0 < D ≤ 3 3 < D ≤ 5 5 < D ≤ 7 7 < D ≤ 10 D > 10 P-value Incidence P-value
tumour
region
Tumour location [categorization 1]
Cecum 137 (12.3) 9 (6.6) 72 (52.6) 37 (27.0) 15 (10.9) 2 (1.5) 1 (0.7) 1 (0.7) 0.27b 37 (27.0) 0.0055e
Ascending colon 369 (33.1) 15 (4.1) 165 (44.7) 109 (29.5) 50 (13.6) 16 (4.3) 12 (3.3) 2 (0.5) 80 (21.7)
Transverse colon 148 (13.3) 20 (13.5) 62 (41.9) 39 (26.4) 19 (12.8) 5 (3.4) 3 (2.0) 0 53 (35.8)
Descending colon 78 (7.0) 3 (3.8) 36 (46.2) 28 (35.9) 8 (10.3) 1 (1.3) 2 (2.6) 0 13 (16.7)
Sigmoid colon 384 (34.4) 25 (6.5) 193 (50.3) 96 (25.0) 38 (9.9) 15 (3.9) 16 (4.2) 1 (0.3) 101 (26.3)
Tumour location [categorization 2]
Non-flexure site 974 (87.3) 53 (5.4) 470 (48.3) 272 (27.9) 108 (11.1) 36 (3.7) 32 (3.3) 3 (0.3) 0.19c 242 (24.8) 0.00062e
Hepatic flexure 91 (8.2) 18 (19.8) 38 (41.8) 19 (20.9) 13 (14.3) 0 2 (2.2) 1 (1.1) 36 (39.6)
Splenic flexure 51 (4.6) 1 (2.0) 20 (39.2) 18 (35.3) 9 (17.6) 3 (5.9) 0 0 6 (11.8)
Location of the primary feeding artery
Primary tumour region 709 (63.5) 48 (6.8) 322 (45.4) 209 (29.5) 79 (11.1) 23 (3.2) 25 (3.5) 3 (0.4) 0.31d 199 (28.1) <0.0001f
≤5 cm from the primary tumour 377 (33.8) 23 (6.1) 195 (51.7) 89 (23.6) 46 (12.2) 16 (4.2) 7 (1.9) 1 (0.3) 82 (21.8)
5–10 cm from the primary tumour 28 (2.5) 1 (3.6) 10 (35.7) 11 (39.3) 4 (14.3) 0 2 (7.1) 0 3 (10.7)
>10 cm from the primary tumour 2 (0.2) 0 1 (50.0) 0 1 (50.0) 0 0 0 0
D: distance from the closest primary tumour edge (cm), LN: lymph node. aMetastasis in intermediate and/or main LNs. bP-value obtained by chi-square test is shown for 1044 patients with positive
pericolic LNs, in which groups of ‘5< D ≤ 7’, ‘7< D ≤ 10’ and ‘D > 10’ are combined. cP-value obtained by chi-square test is shown for 1044 patients with positive pericolic LNs, in which groups
of ‘5 < D ≤ 7’, ‘7 < D ≤ 10’ and ‘D > 10’, and groups ‘hepatic flexure’ and ‘splenic flexure’ are combined, respectively. dTest of Spearman’s rank correlation coefficient. eChi-square test. fCochran-Armitage
trend test.
Table 3: Anatomical distribution of metastatic lymph nodes according to the location of the primary tumour and primary feeding artery in 1116 patients with lymph node
involvement.
3–5 cm, within 5–7 cm, and within 7–10 cm from the specimens than pathologists, meticulously retrieved the
primary tumour, respectively (Supplemental Fig. S5). Of LNs from unfixed surgical specimens. We are aware that
the four patents with distant pericolic nodal metastasis these are not common practice in Europe but we believe
located >10 cm from the primary tumour, three devel- that these achieved a satisfactory number of retrieved
oped recurrence in distant organs or non-mesenteric LNs in this study.15 Additionally, we assessed the
LNs postoperatively (Supplemental Table S2). anatomical distribution of the primary feeding artery
and the paracolic nodes based on in vivo measurement
of the bowel given that there is a remarkable difference
Discussion in the length of colorectal segments between in vivo and
This is the first multicenter cohort study that prospec- in vitro. In deed, Goldstein et al.16 reported that bowel
tively assessed LN distribution in terms of the distance segments shrink by 40% of their original in vivo length
from the primary tumor and the anatomical association following removal from the patient and after being left
with feeding artery location according to the preplanned in an unfixed state for 10–20 min, and by up to 57%
protocol with in vivo measurement. Based on the actual after fixation. In previous LN mapping studies,17,18 the
anatomical distribution of pericolic LN metastasis and distance of the pericolic nodes from the primary tumour
its prognostic implication, we concluded that the 10 cm- was measured in resected surgical specimens, and no
rule is a valid and practical criterion to define ‘regional’ information was obtained regarding the association with
pericolic nodes. the feeding artery location. We believe that the large
The mean number of retrieved LNs was 30.8 per number of pericolic nodes evaluated and the method-
patient, which was much higher than figures reported ology used to assess their anatomical location ensured
by previous studies, which ranged from 11 to 14 in the quality of the LN mapping and clinical applicability
studies with large cohorts of stage II and III colorectal of the results obtained in the present study.
cancer patients.11–14 This may have been due to the Both the number of the pericolic nodes retrieved and
methodology adopted to retrieve the LNs in this study, the number of involved nodes decreased as the distance
that is not being used in clinical practice but allows us to from the primary tumour increased. Notably, only
provide most accurate and useful information for sur- approximately 1% or less metastatic foci were patho-
geons that can be used intraoperatively. In detail, sur- logically identified in pericolic nodes located >10 cm
geons, who are better trained in handling fresh from the primary tumour, irrespective of the T-stage.
www.thelancet.com Vol 33 April, 2023 9
Articles
Primary tumour location Total number Location of the distal end of the primary feeding P-valuea Distance between the primary P-valuec
of patients (%) artery, number (%) feeding artery and the primary
tumour, mean (SD)b
Primary tumour ≤5 cm from the >5 cm from the
region primary tumour primary tumour
Categorisation 1 Cecum 368 (12.3) 310 (84.2) 58 (15.8) 0 (0.0) <0.0001 2.0 (0.9) cm <0.0001
Ascending colon 989 (33.0) 541 (54.7) 417 (42.2) 31 (3.1) 3.2 (1.8) cm
Transverse colon 459 (15.3) 231 (50.3) 196 (42.7) 32 (7.0) 3.6 (2.4) cm
Descending colon 215 (7.2) 123 (57.2) 76 (35.3) 16 (7.4) 3.8 (2.2) cm
Sigmoid colon 965 (32.2) 623 (64.6) 326 (33.8) 16 (1.7) 2.8 (1.7) cm
Categorisation 2 Non-flexure site 2580 (86.1) 1626 (63.0) 895 (34.7) 59 (2.3) 3.0 (1.8) cm
Hepatic flexure 262 (8.7) 131 (50.0) 115 (43.9) 16 (6.1) <0.0001d 3.4 (2.2) cm 0.081d
Splenic flexure 154 (5.1) 71 (46.1) 63 (40.9) 20 (13.0) <0.0001e 4.1 (2.9) cm 0.0011e
SD: standard deviation. aChi-square test and Fisher’s exact test. bIn patients in whom the primary feeding artery is distributed outside the primary tumour region (n = 1168). cANOVA and t-test. dP-values
are shown for the difference between the ‘Non-flexure site’ and ‘Hepatic flexure” groups. eP-values are shown for the difference between the ‘Non-flexure site’ and ‘Splenic flexure’ groups.
Table 4: Location of the primary feeding artery according to the location of the primary tumour.
Some previous studies in the late 1900s using the estimated value of the incidence of pericolic lymphatic
clearing technique reported cases of distant pericolic spread beyond 10 cm was 0.13%, and the upper limit of
nodal metastasis, e.g., 37 cm from the primary tumour the 95% confidence interval remained low (0.26%).
in Grinnel’s study19 and 23 cm from the primary tumour Moreover, we found no LN recurrence in the remnant
in Morikawa et al.’s research20; however, no clear pericolic region within our observation period of 44
distinction between curative and palliative cases was months. In addition, all exceptional four cases with
made in these studies. In previous studies that only pericolic lymphatic spread beyond 10 cm had extensive
investigated patients who underwent curatively- mesenteric LN metastasis. Postoperatively, three of
intended surgery, the incidence of metastasis in peri- these patients developed recurrence in distant organs,
colic nodes >10 cm from the primary tumour was rare, indicating that such distant pericolic lymphatic spread is
with 0% reported in Hida et al.’s study21 and 0.2% re- a form of systemic, rather than local disease. Based on
ported in Yamaoka et al.’s.18 In the present study, the these results, we concluded that pericolic LNs located
Parameters Categories Intraoperative identification of the P-value
anatomical distribution of the
feeding artery
Accurate Inaccurate
Sex, number (%) Male 1442 (94.4) 86 (5.6) 0.031a
Female 1411 (96.1) 57 (3.9)
Age, mean (SD) 68.8 (11.2) 67.5 (11.4) 0.16b
BMI, mean (SD) 22.5 (3.5) 23.9 (3.6) <0.0001b
BMI, number (%) <20 655 (97.2) 19 (2.8)
20 ≤ BMI < 25 1561 (95.8) 69 (4.2)
25 ≤ BMI < 30 568 (92.8) 44 (7.2)
≥30 69 (86.3) 11 (13.8)
Intraoperative detection, number (%) Under direct vision 2760 (95.1) 143 (4.9) 0.022c
Laparoscopically 93 (100) 0 (0.0)
Tumour location [categorisation 1], number (%) Cecum 360 (97.8) 8 (2.2) 0.12d
Ascending colon 938 (94.8) 51 (5.2)
Transverse colon 432 (94.1) 27 (5.9)
Descending colon 203 (94.4) 12 (5.6)
Sigmoid colon 920 (95.3) 45 (4.7)
Tumour location [categorisation 2], number (%) Hepatic flexure 242 (92.4) 20 (7.6) 0.071d
Splenic flexure 148 (96.1) 6 (3.9)
Others 2463 (95.5) 117 (4.5)
BMI: Body mass index, SD: standard deviation. aChi-square test with Yates’ continuity correction. bt-test. cFisher’s exact test. dChi-square test.
Table 5: Accuracy of intraoperative identification of the feeding artery.
10 www.thelancet.com Vol 33 April, 2023
Articles
within 10 cm of the primary tumour can be exclusively feeding-artery-oriented rule (Supplemental Fig. S3),
defined as ‘regional’, and should be resected as a routine which is still used in Japan.10,27 This revision of the
surgical procedure. Current ASCRS guidelines recom- definition of regional pericolic node was based on theory
mend resection margins of 5–7 cm, but surgeons concerning the estimated lymphatic flow from the per-
should be aware of the potential risk of pericolic nodal icolic towards the feeding artery region. Similarly, in the
recurrence according to the resection margin; e.g., recent ASCRS guidelines, the grade of recommendation
approximately 5% for a 5-cm margin and 2% for a 7-cm is ‘strong’ for the statement that the extent of resection
margin in patients with T4 tumor. of the colon should correspond to the lymphovascular
In Western countries, the length of bowel resection drainage of the colon cancer site.6 However, there is no
is thought to depend on the removal of the colon’s high-quality evidence to support its validity of feeding-
arterial supply,6,22 and surgeons generally intend to artery-oriented bowel resection in clinical practice.
resect the vascular arcade next to the primary feeding The present study shows that the distribution of the
artery.7 Consequently, wide bowel resection is routinely feeding artery differs depending on the location of the
employed in routine colon cancer surgery.5,7 In addition, primary tumour. In general, the arcade of feeding ar-
due to the recent prevalence of CME, the length of the teries is wide in the transverse and descending colon,
resected bowel is sometimes used as a standard to especially the splenic flexure site, as compared with the
evaluate specimen quality, and wider resection of the cecum and sigmoid colon.19 However, our results
bowel is regarded as a hallmark of high-quality colon showed that the distribution of positive pericolic nodes
cancer surgery.23 However, based on the results of the did not differ according to the location of the primary
present study, surgical procedures that intend to extend tumour. Moreover, the location of the primary feeding
bowel resection beyond the regional pericolic region do artery did not significantly affect the anatomical distri-
not contribute to improving the quality of surgery. There bution of positive pericolic nodes. These results indicate
are well-ordered, orthodromic lymphatic frow from the that the feeding-artery-oriented definition of regional
pericolic lymphatic vessels to lymph nodes around pericolic nodes is not fully supported within a practical
feeding vessels, indicating the importance of under- framework.
standing the area of pericolic area potentially harboring In addition, intraoperative identification of the
cancer cells with lymphatic spread in determining the feeding artery is not always accurate, especially in obese
optimal resection extent of mesentery. The concept of patients. According to our results, in over one in ten
‘regional’-LN-oriented bowel resection, not that of ‘the patients with a BMI ≥30, surgeons were unable to
wider, the better’ is useful to achieve the optimal sur- accurately identify the feeding artery location intra-
gical procedure without excess or deficiency, and does operatively. This also indicates that the bowel resection
not conflict with the concept of the CME technique. This policy based on the feeding-artery-oriented criteria for
is because the goal of CME is en bloc removal of the regional pericolic nodes may be suboptimal when
mesocolon harbouring metastatic LNs, with sharp standardising colon cancer surgery, and it may be even
anatomic dissection along the embryologic planes and more so when it comes to the Caucasian European/
preservation of the intact visceral fascia of the meso- American population with high BMI.
colon,24 rather than extensive removal of the mesocolon. Unlike the situation in pericolic tumour spread, the
In Japan, the 10-cm rule had been used as the cri- location of the feeding artery impacted the incidence of
terion to classify pericolic nodes since the first edition of central lymphatic spread along the supplying arteries.
the Japanese staging manual for colorectal cancer Specifically, incidences of tumour spread along the
(General Rules for Clinical and Pathological Studies on supplying arteries were significantly higher in patients
Cancer of the Colon, Rectum and Anus) was published in with a primary feeding artery distributing in the peri-
September 1977.25 Under this rule, pericolic nodes colic region of the primary tumour. In addition, the
located within 10 cm of the closest edge of the primary incidence was lower in patients with a tumour located at
tumour were regarded as regional LNs (Supplemental the splenic flexure, where feeding arteries are sparsely
Fig. S2) and they were classified as either Group 1 located, than those with tumours at other sites. Namely,
(pericolic nodes ≤5 cm from the primary tumour) or when there is a feeding artery in close proximity to the
Group 2 (pericolic nodes 5–10 cm from the primary tumour, tumour cells may easily travel to the main LNs
tumour).9 As an exception, in patients with no feeding via the network of lymphatic vessels around the feeding
arteries distributing within 10 cm of the primary artery, indicating the requirement for central vascular
tumour, all LNs located between the primary tumour ligation achievement.
and the primary feeding artery were treated as regional We identified seven exceptional cases with no
nodes.9 feeding arteries located within 10 cm of the primary
In contrast, the General Rules for Clinical and Patho- tumour. None of them had LN involvement in the per-
logical Studies on Cancer of the Colon, Rectum and Anus icolic nodes >10 cm from the primary tumour, inter-
(7th edition) published on March 200626 adopted alter- mediate LNs or main LNs. These results suggest that
native criteria to define regional pericolic nodes—the segmental resection of the colon with a 10-cm resection
www.thelancet.com Vol 33 April, 2023 11
Articles
margin (D1 resection10,27) is as sufficient as curatively- Acknowledgements/Funding
intended surgery for such cases. However, as of now, This study was only funded by the Japanese Society for Cancer of the
Colon and Rectum and had no specific sponsor companies.
considering the limited number of cases analyzed and
the potential inaccuracy of intraoperative identification
of the feeding artery, the conventional 10-cm rule9,25—
Appendix A. Supplementary data
the regional area extends to include pericolic LNs at the Supplementary data related to this article can be found at https://doi.
periphery of the primary feeding artery in cases having org/10.1016/j.lanwpc.2022.100680.
no feeding artery within 10 cm of the primary tumor—
is more realistic from a practical point of view. References
In conclusion, the distribution of the feeding artery 1 Pusztaszeri M, Matter M, Kuonen A, Bourzourene H. Nodal stag-
did not impact the status of pericolic lymphatic spread, ing in colorectal cancer: should distant lymph nodes be recovered
in surgical specimens? Hum Pathol. 2009;40:552–557.
although it might affect that of central lymphatic spread 2 Tan KY, Kawamura YJ, Mizokami K, et al. Distribution of the first
along the supplying arteries that independently impairs metastatic lymph node in colon cancer and its clinical significance.
Colorectal Dis. 2010;12:44–47.
survival outcomes.28 According to the actual anatomical 3 Kim NK, Kim YW, Han YD, et al. Complete mesocolic excision and
distribution of pericolic LN metastasis and its prognostic central vascular ligation for colon cancer: principle anatomy, sur-
implication, the 10-cm rule is a valid and practical crite- gical technique, and outcomes. Surg Oncol. 2016;25:252–262.
4 Union for International Cancer Control. TNM classification of ma-
rion to define the ‘regional’ pericolic region, and this lignant tumours (8th edition). West Sussex (UK): John Wiley & Sons,
should be fully considered when determining the bowel Ltd; 2017.
5 Corman ML, ed. Corman’s colon and rectal surgery (six edition). New
resection margin. Our study has limitations. First, we did York: Lippincott Williams & Wilkins; 2013.
not examine micro-metastasis in the pericolic LN based 6 Vogel JD, Eskicioglu C, Weiser MR, Feingold DL, Steele SR. The
on serial sectioning29 or immunohistochemical staining.30 American Society of Colon and Rectal Surgeons Clinical Practice
Guidelines for the treatment of colon cancer. Dis Colon Rectum.
However, given that we observed no LN recurrence in the 2017;60:999–1017.
remnant pericolic region even in patients with segmental 7 West NP, Kobayashi H, Takahashi K, et al. Understanding optimal
resection of the colon with a 10-cm resection margin, colonic cancer surgery: comparison of Japanese D3 resection and
European complete mesocolic excision with central vascular liga-
micro-metastasis of clinical significance outside a 10-cm tion. J Clin Oncol. 2012;30:1763–1769.
resection margin would be highly unlikely. Second, our 8 Watanabe T, Itabashi M, Shimada Y, et al. Japanese Society for
findings are based on a Japanese population only. We are Cancer of the Colon and Rectum (JSCCR) guidelines 2010 for the
treatment of colorectal cancer. Int J Clin Oncol. 2012;17:1–29.
currently conducting an international prospective obser- 9 Japanese Society for Cancer of the Colon and Rectum. Japanese
vational cohort study for optimal bowel resection extent classification of colorectal carcinoma (First English edition). Tokyo:
Kanehara & Co., Ltd.; 1997.
and central radicality for colon cancer (T-REX study), 10 Japanese Society for Cancer of the Colon and Rectum. Japanese
which involves multiple institutions in seven countries classification of colorectal carcinoma (Second English edition). Tokyo:
(ClincalTrials.gov NCT02938481) and will allow us to Kanehara & Co., Ltd.; 2009.
11 Tekkis P, Smith J, Heriot A, Darzi A, Thompson M, Stamatakis J.
determine whether the above findings are ubiquitously A national study on lymph node retrieval in resectional surgery for
observed and can be generalised in patients with colon colorectal cancer. Dis Colon Rectum. 2006;49:1673–1683.
12 Mannen J, James L, Molloy M, Williams A, Wray C, Sussman J.
cancer in other countries.31 The relationship of lymph node dissection and colon cancer sur-
vival in the Veterans Affairs Central Cancer Registry. Am J Surg.
2007;194:349–354.
Contributors 13 Vather R, Sammour T, Kahokehr A, Connolly A, Hill A.
H.U., K.H., and K.S. devised the initial concept and design of the study. Lymph node evaluation and long-term survival in stage II and stage
A.S., M.S., Ma.I., H.U., T.S., Y.H., T.K., Yus.K., H.I., K.M., K.Y., Ko.K,. III colon cancer: a national study. Ann Surg Oncol. 2009;16:
K.T., Yuk.K., H.O., M.O., T.M., Ya.T., A.I., J.W., Yu.T., H.S., Ke.K., Y.A., 585–593.
and Mi.I. were responsible for data curation and verification of the raw 14 Chou J, Row D, Gonen M, Liu Y-H, Schrag D, Weiser M. Clinical
and pathologic factors that predict lymph node yield from surgical
data. T.N. analysed the data. All authours were involved in data inter-
specimens in colorectal cancer. A population-based study. Cancer.
pretation and validation. H.U. wrote the original draft of the paper and 2010;116:2560–2570.
produced the figures and tables of the manuscript. K.S., K.H., A.S., 15 Ueno H, Hase K, Hashiguchi Y, et al. Potential causes of stage
M.S., Ma.I., T.S., Y.H., T.K., Yus.K., H.I., K.M., K.Y., Ko.K., K.T., migration and their prognostic implications in colon cancer: a
Yuk.K., H.O., M.O., T.M., Ya.T., A.I., J.W., Yu.T., H.S., Ke.K., Y.A., Mi.I. nationwide survey of specialist institutions in Japan. Jpn J Clin
and T.N. were involved in reviewing and editing drafts of the paper and Oncol. 2014;44:547–555.
approving the manuscript. H.U. was involved in the project adminis- 16 Goldstein NS, Soman A, Sacksner J. Disparate surgical margin
tration and KS played a role in the funding acquisition, supervision, and lengths of colorectal resection specimens between in vivo and
in vitro measurements. Am J Clin Pathol. 1999;111:349–351.
decision to submit the manuscript for publication.
17 Hashiguchi Y, Hase K, Ueno H, Mochizuki H, Shinto E,
Yamamoto J. Optimal margins and lymphadenectomy in colonic
cancer surgery. Br J Surg. 2011;98:1171–1178.
Data sharing statement 18 Yamaoka Y, Kinugasa Y, Shiomi A, et al. The distribution of lymph
The data contains personal information, and the study participants have node metastases and their size in colon cancer. Langenbecks Arch
not consented to public data sharing. Data access requires permission Surg. 2017;402:1213–1221.
from the Japanese Society for Cancer of the Colon and Rectum. 19 Grinnell RS. Lymphatic block with atypical and retrograde
lymphatic metastasis and spread in carcinoma of the colon and
rectum. Ann Surg. 1966;163:272–280.
20 Morikawa E, Yasutomi M, Shindou K, et al. Distribution of meta-
Declaration of interests static lymph nodes in colorectal cancer by the modified clearing
All authors declare no competing interests. method. Dis Colon Rectum. 1994;37:219–223.
12 www.thelancet.com Vol 33 April, 2023
Articles
21 Hida J, Yasutomi M, Maruyama T, Fujimoto K, Uchida T, anus (7th Japanese edition). Tokyo: Kanehara & Co., Ltd.; 2006
Okuno K. The extent of lymph node dissection for colon carcinoma. [in Japanese].
The potential impact on laparoscopic surgery. Cancer. 1997;80: 27 Japanese Society for Cancer of the Colon and Rectum. Japanese
188–192. classification of colorectal, appendiceal, and anal carcinoma (Third
22 Nelson H, Petrelli N, Carlin A, et al. Guideline 2000 for colon and English edition). Tokyo: Kanehara & Co., Ltd.; 2019.
rectal cancer surgery. J Natl Cancer Inst. 2001;93:583–596. 28 Shinto E, Ike H, Hida J, et al. Proposal of a modified subclas-
23 Wang C, Gao Z, Shen K, et al. Safety, quality and effect of complete sification system for stage III colorectal cancer: a multi-
mesocolic excision vs non-complete mesocolic excision in patients institutional retrospective analysis. Ann Gastroenterol Surg.
with colon cancer: a systemic review and meta-analysis. Colorectal 2020;4:667–675.
Dis. 2017;19:962–972. 29 Ueno H, Yamauchi C, Hase K, Ichikura T, Mochizuki H. Clini-
24 Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S. copathological study of intrapelvic cancer spread to the iliac area in
Standardized surgery for colonic cancer: complete mesocolic exci- lower rectal adenocarcinoma by serial sectioning. Br J Surg.
sion and central ligation-technical notes and outcome. Colorectal 1999;86:1532–1537.
Dis. 2009;11:354–364. 30 Ueno H, Mochizuki H, Hashiguchi Y, et al. Risk factors for an
25 Japanese Society for Cancer of the Colon and Rectum. General rules adverse outcome in early invasive colorectal carcinoma. Gastroen-
for clinical and pathological studies on cancer of the colon, rectum and terology. 2004;127:385–394.
anus (1st Japanese edition). Tokyo: Kanehara & Co., Ltd.; 1977 31 Shiozawa M, Ueno H, Shiomi A, et al. Study protocol for an in-
[in Japanese]. ternational prospective observational cohort study for optimal
26 Japanese Society for Cancer of the Colon and Rectum. General rules bowel resection extent and central radicality for colon cancer
for clinical and pathological studies on cancer of the colon, rectum and (T-REX study). Jpn J Clin Oncol. 2021;51:145–155.
www.thelancet.com Vol 33 April, 2023 13
You might also like
- Endoscopic Management of Colorectal T1(SM) CarcinomaFrom EverandEndoscopic Management of Colorectal T1(SM) CarcinomaShinji TanakaNo ratings yet
- 1 s2.0 S1015958417305833 MainDocument7 pages1 s2.0 S1015958417305833 Mainyerich septaNo ratings yet
- IkjjjkjDocument7 pagesIkjjjkjMohammad AjiNo ratings yet
- Clinicopathological Features and Treatment OutcomeDocument9 pagesClinicopathological Features and Treatment Outcomesyfs92ctpvNo ratings yet
- JurnalDocument35 pagesJurnalAndi MujtahidaNo ratings yet
- Presentasi KARYA AKHIRDocument37 pagesPresentasi KARYA AKHIRZuhan ArifNo ratings yet
- 2017 Surgical Evolution of Rectal CancerDocument8 pages2017 Surgical Evolution of Rectal CancerDr Juan Antonio Villanueva (Coloproctologia)No ratings yet
- Actualizacion de Reporte de CA Colorectal 2019Document14 pagesActualizacion de Reporte de CA Colorectal 2019Jairo Lino BNo ratings yet
- Annals of Medicine and SurgeryDocument7 pagesAnnals of Medicine and SurgeryInggitaDarmawanNo ratings yet
- Expert Consensus Contouring Guidelines For Intensity Modulated Radiation Therapy in Esophageal and Gastroesophageal Junction CancerDocument10 pagesExpert Consensus Contouring Guidelines For Intensity Modulated Radiation Therapy in Esophageal and Gastroesophageal Junction CancermarrajoanaNo ratings yet
- Research Article: Characteristics of Patients With Colonic Polyps Requiring Segmental ResectionDocument7 pagesResearch Article: Characteristics of Patients With Colonic Polyps Requiring Segmental ResectionAkiko Syawalidhany TahirNo ratings yet
- Soria 2019Document7 pagesSoria 2019Dr. Alexandre SatoNo ratings yet
- Retroperitoneal Nodal Metastases From Colorectal Cancer: Curable Metastases With Radical Retroperitoneal Lymphadenectomy in Selected PatientsDocument8 pagesRetroperitoneal Nodal Metastases From Colorectal Cancer: Curable Metastases With Radical Retroperitoneal Lymphadenectomy in Selected PatientsSchiopu VictorNo ratings yet
- Ac 30 165Document10 pagesAc 30 165Zest IanNo ratings yet
- Current Trends in Extended Lymph Node Dissection For Esophageal CarcinomaDocument6 pagesCurrent Trends in Extended Lymph Node Dissection For Esophageal CarcinomaYacine Tarik AizelNo ratings yet
- Radical Surgery For Cancer of The Pancreas: Kothaj PDocument3 pagesRadical Surgery For Cancer of The Pancreas: Kothaj Pyacine26No ratings yet
- Full TextDocument6 pagesFull Textpqp2303No ratings yet
- Localized Resection For Colon Cancer: R.A. Cahill, J. Leroy, J. MarescauxDocument9 pagesLocalized Resection For Colon Cancer: R.A. Cahill, J. Leroy, J. MarescauxIliasa IliasNo ratings yet
- EAU Guidelines Update on Non-Muscle Invasive Bladder CancerDocument15 pagesEAU Guidelines Update on Non-Muscle Invasive Bladder CancerMuhammad FaisalNo ratings yet
- SMJ 60 247Document6 pagesSMJ 60 247Chee Yung NgNo ratings yet
- Article - Laparoscopic Versus Open Surgery For Rectal Cancer (COLOR II) - Short-Term Outcomes of A Randomised, Phase 3 Trial - 2013Document9 pagesArticle - Laparoscopic Versus Open Surgery For Rectal Cancer (COLOR II) - Short-Term Outcomes of A Randomised, Phase 3 Trial - 2013Trí Cương NguyễnNo ratings yet
- European Association of Urology Guidelines On Muscle-Invasive and Metastatic Bladder Cancer: of The 2020 GuidelinesDocument23 pagesEuropean Association of Urology Guidelines On Muscle-Invasive and Metastatic Bladder Cancer: of The 2020 GuidelinesBalqist Asyawa Andra PutriNo ratings yet
- Heidenreich Et Al. - Anatomic Extent of Pelvic Lymphadenectomy in Bladder CancerDocument5 pagesHeidenreich Et Al. - Anatomic Extent of Pelvic Lymphadenectomy in Bladder CanceryuenkeithNo ratings yet
- Tugas Bahasa Inggris Temu 2: A12-B Kelompok 3Document12 pagesTugas Bahasa Inggris Temu 2: A12-B Kelompok 3Wisnu 12No ratings yet
- RJX 102Document3 pagesRJX 102FachryNo ratings yet
- Adjuvant Therapy. Most Studies HaveDocument9 pagesAdjuvant Therapy. Most Studies HaveAnonymous UTUWFODCEYNo ratings yet
- The Surgical Treatment of Esophageal Cancer Indications Comparative Analysis of Surgical TechniquesDocument19 pagesThe Surgical Treatment of Esophageal Cancer Indications Comparative Analysis of Surgical Techniquesalinutza_childNo ratings yet
- s13048 018 0461 5rtyDocument5 pagess13048 018 0461 5rtyAni triyantiNo ratings yet
- Impact of Surgical Margins On Overall Survival After Gastrectomy For Gastric Cancer: A Validation of Japanese Gastric Cancer Association Guidelines On A Western SeriesDocument13 pagesImpact of Surgical Margins On Overall Survival After Gastrectomy For Gastric Cancer: A Validation of Japanese Gastric Cancer Association Guidelines On A Western SeriesХулан ХүрэлбаатарNo ratings yet
- Laparoscopic Low Anterior Resection With Two PlannDocument6 pagesLaparoscopic Low Anterior Resection With Two PlannRoman ShyyanNo ratings yet
- Clinical Outcomes of Laparoscopic Surgery For Transverse and Descending Colon Cancers in A Community SettingDocument6 pagesClinical Outcomes of Laparoscopic Surgery For Transverse and Descending Colon Cancers in A Community SettingpingusNo ratings yet
- Mesenterico PDFDocument7 pagesMesenterico PDFTay SalinasNo ratings yet
- Long-Term Outcomes of Primary Endoscopic Resection Vs Surgery For T1Document16 pagesLong-Term Outcomes of Primary Endoscopic Resection Vs Surgery For T1ellya zalfaNo ratings yet
- Linfadenectomy in Pancreatic Adenoca Definition Isgps 2014Document10 pagesLinfadenectomy in Pancreatic Adenoca Definition Isgps 2014CIRUGÍA ONCOLÓGICA ABDOMENNo ratings yet
- Wiitm 8 20500Document4 pagesWiitm 8 20500farahNo ratings yet
- Lee2017 PDFDocument12 pagesLee2017 PDFian3yeung-2No ratings yet
- ATAR O Ocampo 2014 PJSSDocument11 pagesATAR O Ocampo 2014 PJSSPrince VallejosNo ratings yet
- Low Anterior Resection TechniquesDocument15 pagesLow Anterior Resection Techniquesdrneeraj168No ratings yet
- Dynamic CT Findings of A Polypoid Gastric - ChrisnaDocument4 pagesDynamic CT Findings of A Polypoid Gastric - ChrisnaferonicaNo ratings yet
- New Technique For Magnetic Compression Anastomosis Without Incision For Gastrointestinal ObstructionDocument10 pagesNew Technique For Magnetic Compression Anastomosis Without Incision For Gastrointestinal ObstructionChairunnisa MNo ratings yet
- Klatskin Tumor Diagnosis & Surgical ResectionDocument9 pagesKlatskin Tumor Diagnosis & Surgical ResectionFlorian JeffNo ratings yet
- EAU Guideline 2021Document20 pagesEAU Guideline 2021G WNo ratings yet
- Abe Et Al. - 2000 - Value of Laparoscopic Microwave Coagulation Therapy For Hepatocellular Carcinoma in Relation To Tumor Size and LocatDocument6 pagesAbe Et Al. - 2000 - Value of Laparoscopic Microwave Coagulation Therapy For Hepatocellular Carcinoma in Relation To Tumor Size and Locatsushmakumari009No ratings yet
- Colorectal CA CME-CVLDocument32 pagesColorectal CA CME-CVLAbu ZidaneNo ratings yet
- 167 FTPDocument8 pages167 FTPboroumandNo ratings yet
- Transanal Endoscopic Microsurgery A ReviewDocument13 pagesTransanal Endoscopic Microsurgery A ReviewYusuf riskaNo ratings yet
- Role of Surgery in Multimodal Cancer Therapy For Small AnimalsDocument16 pagesRole of Surgery in Multimodal Cancer Therapy For Small AnimalsAlexandra PradaNo ratings yet
- E041797 FullDocument11 pagesE041797 FullDewi Purnama SariNo ratings yet
- Complete Mesocolic Excision and Extent of Lymphadenectomy For The Treatment of Colon CancerDocument14 pagesComplete Mesocolic Excision and Extent of Lymphadenectomy For The Treatment of Colon CancerashentaxpayeeNo ratings yet
- Proceedings 2006Document567 pagesProceedings 2006Sheshi ShrivastavaNo ratings yet
- Shimodate 2020Document9 pagesShimodate 2020Drzizo AwadNo ratings yet
- Perkutana AblacijaDocument7 pagesPerkutana AblacijaNenad DjokicNo ratings yet
- 016 - The-Evolving-Landscape-of-Neuroendocr - 2023 - Surgical-Oncology-Clinics-of-NortDocument14 pages016 - The-Evolving-Landscape-of-Neuroendocr - 2023 - Surgical-Oncology-Clinics-of-NortDr-Mohammad Ali-Fayiz Al TamimiNo ratings yet
- Sci 43Document18 pagesSci 43Stella Putri WandaNo ratings yet
- Endoscopic Submucosal Dissection For Early Gastric Cancer: Are Expanded Resection Criteria Safe For Western Patients?Document11 pagesEndoscopic Submucosal Dissection For Early Gastric Cancer: Are Expanded Resection Criteria Safe For Western Patients?Mayra Camila PerezNo ratings yet
- Management of Primary Testicular Tumor: Alireza Ghoreifi,, Hooman DjaladatDocument7 pagesManagement of Primary Testicular Tumor: Alireza Ghoreifi,, Hooman DjaladatfelipeNo ratings yet
- 1 s2.0 S1051044322011903 MainDocument30 pages1 s2.0 S1051044322011903 MainEsmaeel Jafargholi RangrazNo ratings yet
- Review Article: Intersphincteric Resection and Coloanal Anastomosis in Treatment of Distal Rectal CancerDocument10 pagesReview Article: Intersphincteric Resection and Coloanal Anastomosis in Treatment of Distal Rectal CancerJaysonGarabilesEspejoNo ratings yet
- Journal 1 - Multidetector Computed Tomography in The Evaluation of Gastric Malignancy A Multicenteric StudyDocument6 pagesJournal 1 - Multidetector Computed Tomography in The Evaluation of Gastric Malignancy A Multicenteric StudypasyaNo ratings yet
- Assessment of Tumor Parameters As Factors of Aggressiveness in Colon Cancer 1584 9341 10 4 6Document5 pagesAssessment of Tumor Parameters As Factors of Aggressiveness in Colon Cancer 1584 9341 10 4 6Panuta AndrianNo ratings yet
- Colace (Docusate Sodium)Document1 pageColace (Docusate Sodium)E100% (1)
- Laparoscopic Anatomy of the Abdominal CavityDocument14 pagesLaparoscopic Anatomy of the Abdominal CavityUffie-Isabela GheNo ratings yet
- Common Surgical Problems in Paediatrics Review PDFDocument15 pagesCommon Surgical Problems in Paediatrics Review PDF1031 Muhammad zaryabNo ratings yet
- Daftar Diit PasienDocument5 pagesDaftar Diit PasiennovilusiyanaNo ratings yet
- Frog Dissection (Remote)Document21 pagesFrog Dissection (Remote)Mohammad NiyaifarNo ratings yet
- Gallstone Ileus 3Document7 pagesGallstone Ileus 3andisibaNo ratings yet
- LAB EXAM Systems ReviewerDocument5 pagesLAB EXAM Systems ReviewerAlexandra Danielle LimjocoNo ratings yet
- MCLD 2020 - Poster Board NumberDocument3 pagesMCLD 2020 - Poster Board NumberArdianto SucintaNo ratings yet
- CholecytitisDocument28 pagesCholecytitisواحة الأمل100% (1)
- Digestive System of Fish & ShellfishDocument19 pagesDigestive System of Fish & ShellfishGrace Angel50% (4)
- Boala CeliacaDocument4 pagesBoala CeliacaCristina TudorNo ratings yet
- IIIDocument13 pagesIIIapi-3828211No ratings yet
- 2021 Article 2922Document4 pages2021 Article 2922AnirisulNo ratings yet
- What Are H2 Blockers?Document3 pagesWhat Are H2 Blockers?Alexandra FeherNo ratings yet
- Register Igd 2018Document73 pagesRegister Igd 2018roniNo ratings yet
- Diagnosing Abdominal Hernias with ImagingDocument15 pagesDiagnosing Abdominal Hernias with ImagingSpecialNameNo ratings yet
- Intestinal Obstruction: Dr. Mohammad Jamil AlhashlamonDocument19 pagesIntestinal Obstruction: Dr. Mohammad Jamil AlhashlamonBheru LalNo ratings yet
- Muntah Pada Anak PDFDocument21 pagesMuntah Pada Anak PDFAndika SiswantaNo ratings yet
- UK Patient Proton Pump Inhibitor Medication LeafletDocument4 pagesUK Patient Proton Pump Inhibitor Medication Leafletmarisa apriliaNo ratings yet
- Presentation DiarrheaDocument23 pagesPresentation DiarrheaVenkatesh KS 233No ratings yet
- Routine Fecalysis Stool Analysis: Is A Series of Tests Done On A Stool Sample To Help Diagnose Certain ConditionsDocument3 pagesRoutine Fecalysis Stool Analysis: Is A Series of Tests Done On A Stool Sample To Help Diagnose Certain ConditionsSheila GarciaNo ratings yet
- CH16 Patho D&R AgamDocument29 pagesCH16 Patho D&R AgamBio CheNo ratings yet
- Nursing Diagnosis For Gerd: Lifestyle ChangesDocument3 pagesNursing Diagnosis For Gerd: Lifestyle ChangesSharmaine MadlaNo ratings yet
- Case Presentation: Ascariasis: Mrs. Lailanie Evangelista DotimasDocument10 pagesCase Presentation: Ascariasis: Mrs. Lailanie Evangelista DotimasRodelen MarañoNo ratings yet
- Jurnal Tentang Intervensi Keperawatan: Pedoman Penyusunan Laporan Presentasi JurnalDocument2 pagesJurnal Tentang Intervensi Keperawatan: Pedoman Penyusunan Laporan Presentasi JurnalDesilvaNo ratings yet
- Digestive System Review - Key Processes and OrgansDocument8 pagesDigestive System Review - Key Processes and OrgansJohn NinoNo ratings yet
- Gastroenterology Certification Examination Blueprint - ABIMDocument4 pagesGastroenterology Certification Examination Blueprint - ABIMabimorgNo ratings yet
- Lee2004 - High Hilar Dissection - New Technique To Reduce Biliary Complication in Living Donor Liver Transplantation (SK Lee)Document5 pagesLee2004 - High Hilar Dissection - New Technique To Reduce Biliary Complication in Living Donor Liver Transplantation (SK Lee)hoangducnamNo ratings yet
- Laparoscopic Appendictomy DictationDocument3 pagesLaparoscopic Appendictomy DictationHassanNo ratings yet
- The Portal Venous SystemDocument21 pagesThe Portal Venous SystemAhmed DsoukiNo ratings yet