Professional Documents
Culture Documents
Muhammad Umer (Assignment 01)
Uploaded by
Umer KhanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Muhammad Umer (Assignment 01)
Uploaded by
Umer KhanCopyright:
Available Formats
ASSIGNMENT – 01 (MUHAMMAD UMER)
Q1
a) PURPOSE OF DRUG DISCOVERY:
Finding and creating new drugs or therapeutic agents that can successfully treat, cure, or
prevent a variety of illnesses and medical problems is the goal of drug discovery. This procedure
is a series of methodical, scientific methods designed to find chemicals or substances that may
interact with particular biological targets, including proteins or enzymes implicated in disease
processes.
MAIN GOAL OF DRUG DISCOVERY:
The main goal of drug discovery is to improve human health by developing new treatments for a
variety of diseases, including cancer, cardiovascular disorders, infectious diseases, neurological
disorders, and more. New drugs can relieve symptoms, slow disease progression, or even cure
some diseases.
PURPOSE OF PRE CLINICAL DEVELOPMENT :
The purpose of preclinical development in the context of drug discovery and development is to
collect the necessary data on the safety, efficacy, and pharmacokinetics of a potential drug (how
well it works in the body). possible). Preclinical studies involve a series of rigorous laboratory
and animal experiments that help researchers assess whether a drug candidate is likely to be
safe and effective in treating a particular disease. This step is critical for making an informed
decision about whether or not to promote a drug candidate in human clinical trials.
Pharmacokinetics (PK) and Pharmacodynamics (PD) Evaluation:
Researchers study how the drug is absorbed, distributed, metabolized, and excreted within the
body (PK) and how it interacts with its target and produces its effects (PD). This information
helps in predicting how the drug will behave in humans and guides dosage adjustments.
PURPOSE OF CLINICAL DEVELOPMENT:
The goal of clinical development is to rigorously and systematically evaluate the overall safety,
efficacy, and benefit risks of a new drug or therapeutic intervention in humans. Clinical
development occurs after preclinical studies and consists of a series of carefully designed and
controlled clinical trials conducted in different phases. These trials provide the necessary data
that regulators use to determine if a drug should be approved for large-scale marketing and
widespread use.
MAIN PURPOSE OF CLINICAL DEVELOPMENT:
Safety Assessment in Humans: Clinical trials assess the safety of the drug candidate in humans,
which is especially important because human physiology and responses can differ from those of
animals used in preclinical studies. Researchers closely monitor participants for adverse effects
and potential risks associated with the drug.
STEPS FOR CLINICAL DEVELOPMENT :
Clinical development involves a series of carefully planned and executed steps or phases, each
designed to gather specific types of information about a new drug's safety, efficacy, and overall
performance in humans.
Phase 0 (Exploratory) :
Phase 0 studies) are conducted early in clinical phase studies and involve limited human
exposure and have no therapeutic or diagnostic intent. Doses are subtherapeutic and patients
are monitored by the clinical researcher and involve about 10 study patients. Duration of a
patient’s participation is usually less than 1 week. Pharmacodynamics and pharmacokinetics are
studied. These trials are before the traditional dose escalation, safety, and tolerance studies.
These trials were developed to shorten the critical path for drug development, to explore
pharmacokinetic and pharmacodynamic profiles of IND’s in humans, to help in accelerating
identification of promising drugs, and to reduce development time and costs.
Phase I (First-in-Human):
Involves a small number of healthy volunteers or patients (typically 20 to 100
participants).Primary goal is to assess safety, determine safe dosage ranges, and understand the
drug's pharmacokinetics and pharmacodynamics.Usually involves escalating doses of the drug
to find the maximum tolerated dose (MTD) or the highest dose that does not cause
unacceptable side effects.
Phase II (Proof of Concept):
Phase II dose finding studies determine the most successful dose (MSD) which is the dose which
maximizes the product of the probability of seeing no toxicity together with the probability of
seeing a therapeutic response. Focuses on evaluating the drug's efficacy, optimal dosing
regimen, and further safety assessments.
Often includes a placebo or comparator group for comparison.
Helps researchers decide whether to move forward with larger-scale testing in Phase III.
Phase III (Confirmatory):;
This is the “pre-marketing phase” of clinical trials. These are often the most expensive and time-
consuming tests. Tests can be difficult to design and implement. Involves a larger and more
diverse patient population (typically several hundred to thousands of participants).
Designed to provide robust evidence of the drug's efficacy, safety, and potential side effects.
Randomized and controlled trials are common, often with multiple study sites .Collects data on
both short-term and long-term effects.
Phase IV (Post-Marketing Surveillance):
These Phase IV takes place after the drug is approved and available on the market. Phase IV
studies include “all studies (other than routine surveillance) performed after drug approval and
related to the approved indication”. These are post-marketing surveillance studies. The focus of
the trials is on how drugs work in the real world. Anyone seeking treatment from their physician
may be treated with the therapy. Their personal physician monitors the results of treatment.
Focuses on monitoring the drug's safety and effectiveness in a real-world setting and a larger
patient population. Aims to identify rare adverse events and long-term effects that may not
have been captured in earlier phases . Can lead to label updates or changes in usage guidelines
based on new information.
b) USUAL TIME FRAME INVOLVED IN THE DISCOVERY OF
DRUG :
The complexity of the disease, the nature of the drug target, the availability of resources, the
success of various stages, regulatory requirements, and unforeseen challenges that may arise
during the process are just a few of the many variables that can affect the length of time
involved in drug discovery.
The first stage is to identify and validate a suitable pharmacological target. Understanding the
biological processes and disease-related chemicals is necessary for this which may take 1 to 3
years.:Screening libraries of compounds to identify molecules that interact with the target (hits)
and further optimizing them to improve their activity which may take 1-2 years .Increasing the
potency, selectivity, pharmacokinetic characteristics, and safety of the identified molecules.So,
the total time involved in the drug discovery process from the initial identification of a target to
the completion of lead optimization, can range from approximately 2-4 years.
Usual time frame Involve in pre clinical development :
Preclinical development normally lasts 1 to 3 years, though this can vary depending on a variety
of factors such as the complexity of the drug candidate, the condition being addressed, the
extent of toxicity testing required, and regulatory considerations.
Usual time frame Involve in clinical development :
Clinical development is a multi-phase process that involves human studies to assess a novel
drug candidate's safety, effectiveness, and overall performance. The length of clinical
development can vary greatly depending on criteria such as disease complexity, patient
population size, phase success, regulatory requirements, patient recruiting, and unforeseen
hurdles. Clinical development can take anything from 6 to 7 years on average which Involves all
the phases .
USUAL TIME Frame In regulatory Approval :
The time it takes to obtain regulatory approval for a new drug is 0.5-2 years .
C)Usual sample size for drug discovery :
The sample size for drug discovery can vary significantly depending on the specific stage of drug
development and the goals of the study. The sample size range upto 5000 to 10000 compounds
Usual sample size for pre-clinical development :
In preclinical stages, sample sizes are often smaller compared to clinical trials. Which ranges
upto 250
Usual sample size for clinical development :
. Phase 1 Trials: These are usually conducted with a small number of healthy volunteers
(typically 20-100 participants)
Phase 2 Trials: These involve a larger number of participants (typically around 100-500)
Phase 3 Trials: These are large-scale trials designed to confirm the efficacy and safety of the
intervention in a larger patient population (typically 1000 to 5000 participants).
Q2
PROS of Emergency Use Approvals:
Fast Response: EUAs permit for quick arrangement of vital diagnostics, immunizations,
and medications to combat the widespread. Usually particularly critical in circumstances where
the infection is spreading quickly and causing critical hurt.
Lifesaving Potential: In crisis circumstances, speeding up get to interventions can save lives
and relieve the affect of the illness.
Public Health Advantage: Quickened endorsements can offer
assistance control transmission, ensure healthcare frameworks, and decrease the burden of
the disease on society.
Scientific Collaboration: The criticalness has cultivated exceptional collaboration
among researchers, analysts, and administrative organizations, driving to
the quick improvement of successful intercessions.
Adaptable Regulation: Administrative organizations can adjust to modern prove and informati
on rapidly, making educated choices based on rising data.
Cons of Emergency Use Approvals:
Limited Safety Data: Due to the assisted nature of EUAs, there may well be less
comprehensive safety and adequacy information accessible compared to the
standard regulatory process. This might lead to uncertainties about the long-
term impacts of interventions.
Risk of Ineffectiveness:
A few interventions that get crisis utilize approval might afterward be found to be ineffective or
have unanticipated negative consequences.
Post-Approval checking:
Thorough post-approval checking can be compromised due to the assisted handle,
which might delay distinguishing proof of potential security issues.
Potential Abuse:
In few cases, crisis utilize seem leadto abuse or abuse of interventions without legitimate prove
of their adequacy, possibly hurting patients.
Bypassing Approval for Emergency Use :
The decision to bypass the standard approval process for emergency use of vaccines or any
medical intervention is a complex and contentious one. It involves balancing the urgent need to
address a public health crisis with ensuring the safety and efficacy of the intervention. So in
such particular case for COVID , bypassing was the only way to control that rapidly spreading
and life-threatening situation, there might be a need to expedite the availability of
interventions to save lives and prevent further harm .But on the other hand If this by passing
wouldn’t happened this disaster could cause more devastating situation and then we had to
bypass much bigger decree .
You might also like
- Purpose of Drug DiscoveryDocument6 pagesPurpose of Drug DiscoveryUmer KhanNo ratings yet
- 10 - Drug DevelopmentDocument5 pages10 - Drug DevelopmentLaura SaglietiNo ratings yet
- DRUG TESTING AND MEDICATION (By Anashe Magorimbo)Document2 pagesDRUG TESTING AND MEDICATION (By Anashe Magorimbo)Leon MzarabaniNo ratings yet
- ENGLISH AssignmentDocument15 pagesENGLISH AssignmentManahil SardarNo ratings yet
- Clinical Research: Presented By: Deepali KhetmalisDocument16 pagesClinical Research: Presented By: Deepali KhetmalisAmol KokaneNo ratings yet
- Exploring The Drug Development ProcessDocument9 pagesExploring The Drug Development Processs adhikariNo ratings yet
- 2ahandout ENG 2020 ElearningDocument5 pages2ahandout ENG 2020 ElearningNupura AjeshNo ratings yet
- Clinical Research NotesDocument98 pagesClinical Research NotesToha Afreen100% (1)
- The Drug Development ProcessDocument7 pagesThe Drug Development ProcessSACHIN BHASKAR NARKHEDE100% (1)
- Clinical - Trial - Phases 4th OneDocument11 pagesClinical - Trial - Phases 4th OneSrikant SinghNo ratings yet
- Drug Development Process-1Document12 pagesDrug Development Process-1Ima AnNo ratings yet
- Clinical Trial PhasesDocument4 pagesClinical Trial PhasesManish SarasvatiNo ratings yet
- Research 101: Sponsored byDocument34 pagesResearch 101: Sponsored byMohammed HammedNo ratings yet
- 2.2 Clinical Trails Phases - Clinical Research - Pharma DostDocument9 pages2.2 Clinical Trails Phases - Clinical Research - Pharma DostjhancyNo ratings yet
- Clinical TrialsDocument73 pagesClinical TrialsSunilNo ratings yet
- Lesson-2 Clinical TrailsDocument2 pagesLesson-2 Clinical Trailsmnvaibhav75No ratings yet
- Assignment On Drug DiscoveryDocument3 pagesAssignment On Drug DiscoveryMuhad KabeerNo ratings yet
- Drug Discovery ProcessDocument22 pagesDrug Discovery ProcessEAC School of Pharmacy ManilaNo ratings yet
- Final Project LevofloxacinDocument102 pagesFinal Project LevofloxacinJalwaz TihamiNo ratings yet
- Types of Studies - NRC Research Institute (FDA)Document3 pagesTypes of Studies - NRC Research Institute (FDA)Muhammad ReyhanNo ratings yet
- BT Sec Final Paper Answer Sem4Document3 pagesBT Sec Final Paper Answer Sem4Ankit AthreyaNo ratings yet
- Clinical ResearchDocument5 pagesClinical ResearchDeepti ShrivasNo ratings yet
- Clinical Trials: FDA ApprovalDocument3 pagesClinical Trials: FDA Approvalthamizh555No ratings yet
- Clinical Trials in IndiaDocument44 pagesClinical Trials in IndiaRounak VirmaniNo ratings yet
- Phases of Clinical TrialDocument10 pagesPhases of Clinical TrialUmardin SaifyNo ratings yet
- Drug Development: New Chemical Entity DevelopmentDocument6 pagesDrug Development: New Chemical Entity DevelopmentDeenNo ratings yet
- Clinical TrialDocument9 pagesClinical TrialAyanNo ratings yet
- Clinical Studies in New Drug DevelopmentDocument14 pagesClinical Studies in New Drug DevelopmentDWALE AUBADENo ratings yet
- Practicals (Pharmaceutical Technology)Document24 pagesPracticals (Pharmaceutical Technology)Kustian Kohat100% (1)
- Overview of PharmacovigilanceDocument12 pagesOverview of PharmacovigilanceEditor IJTSRDNo ratings yet
- Phases of Clin TrialDocument26 pagesPhases of Clin TrialPraneeth Sanjeev ReddyNo ratings yet
- FDA Approval Process EbookDocument15 pagesFDA Approval Process EbookCarlos Alberto Salazar DuqueNo ratings yet
- Phases of Clinical TrialsDocument30 pagesPhases of Clinical TrialsMahum SohailNo ratings yet
- Basic Clinical Trial TerminologyDocument2 pagesBasic Clinical Trial Terminologysatty1979No ratings yet
- MPHR - 129 (Clinical Trial Managment)Document42 pagesMPHR - 129 (Clinical Trial Managment)Dr-Harikesh MauryaNo ratings yet
- Drug Development Process StagesDocument7 pagesDrug Development Process Stagesvipinkv99No ratings yet
- Step 3 - FDA Clinical Research - DrugsDocument6 pagesStep 3 - FDA Clinical Research - DrugsMuhammad ReyhanNo ratings yet
- Drug DevelopmentDocument5 pagesDrug Developmentnevelle4667No ratings yet
- unit2_clinical-trialsDocument12 pagesunit2_clinical-trialsDevangNo ratings yet
- Pharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceFrom EverandPharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceRating: 3 out of 5 stars3/5 (1)
- Clinical Trials:Overview and OpportunitiesDocument23 pagesClinical Trials:Overview and OpportunitiesSasidhar RlcNo ratings yet
- Clinical Research MethodologyDocument11 pagesClinical Research MethodologymisganaNo ratings yet
- An Introduction To Clinical TrialsDocument9 pagesAn Introduction To Clinical TrialsIrfan AhmadNo ratings yet
- Project About Clinical Drug Development: BY Bharatwajan M Student From Presidency College, ChennaiDocument19 pagesProject About Clinical Drug Development: BY Bharatwajan M Student From Presidency College, ChennaiDineshNo ratings yet
- Drug Development StagesDocument4 pagesDrug Development Stagespeter mwangiNo ratings yet
- Phases: ResearchDocument9 pagesPhases: ResearchMuskan AhujaNo ratings yet
- Brief Review On Clinical TrialsDocument23 pagesBrief Review On Clinical TrialssallurajNo ratings yet
- Clinical Trails GlossaryDocument68 pagesClinical Trails Glossaryapi-3810976100% (1)
- Drug Development and EvaluationDocument25 pagesDrug Development and EvaluationArlises SinagaNo ratings yet
- Drug Design and DevelopmentDocument5 pagesDrug Design and DevelopmentMark Russel Sean LealNo ratings yet
- Clinical Trials Lecture 4 (1)Document17 pagesClinical Trials Lecture 4 (1)tyleree3No ratings yet
- Clinical TrialsDocument51 pagesClinical TrialsRajan JattNo ratings yet
- Different phases of clinical trialsDocument5 pagesDifferent phases of clinical trialsAshwan KumarNo ratings yet
- Desain Study Halaman 31 40Document5 pagesDesain Study Halaman 31 40capita doankNo ratings yet
- Drug Discovery and DevelopmentDocument17 pagesDrug Discovery and DevelopmentMarchelino Devan WibisonoNo ratings yet
- Drug Development ProcessapolloDocument19 pagesDrug Development Processapollotamara_0021No ratings yet
- Pharmacoepidemiology and Pharmacovigilance: Synergistic Tools to Better Investigate Drug SafetyFrom EverandPharmacoepidemiology and Pharmacovigilance: Synergistic Tools to Better Investigate Drug SafetyRating: 4.5 out of 5 stars4.5/5 (3)
- Clinical Trial Phases ExplainedDocument5 pagesClinical Trial Phases ExplainedDavid ThaiNo ratings yet
- 3_-5_The_Drug_Development_ProcessDocument10 pages3_-5_The_Drug_Development_Processaghanafissa5No ratings yet
- U.S. Food & Drug: Administration 10903 New Hampshire Avenue Silver Spring, MD 20993Document14 pagesU.S. Food & Drug: Administration 10903 New Hampshire Avenue Silver Spring, MD 20993jonathan panganibanNo ratings yet
- Mount Kenya UniversityDocument3 pagesMount Kenya UniversityAnonymous DGxdAOlNo ratings yet
- M. Preterm and Postterm - NewDocument92 pagesM. Preterm and Postterm - NewTry Ariditya UtomoNo ratings yet
- Werner & Ingbar’s The Thyroid 8th EditionDocument10 pagesWerner & Ingbar’s The Thyroid 8th Editionbyrock66No ratings yet
- Ezolvin Syrup Patient Information Leaflet PDFDocument1 pageEzolvin Syrup Patient Information Leaflet PDFSameer SamouaNo ratings yet
- PMLS1 Lesson 3Document8 pagesPMLS1 Lesson 3John Daniel AriasNo ratings yet
- Live music reduces pediatric distressDocument5 pagesLive music reduces pediatric distressandreaNo ratings yet
- Sample: Pediatric Hernia Inguinal and Femoral RepairDocument8 pagesSample: Pediatric Hernia Inguinal and Femoral RepairSamuel Sebastian SirapanjiNo ratings yet
- Potassium Chloride - Uses, Dosage & Side EffectsDocument4 pagesPotassium Chloride - Uses, Dosage & Side EffectsKenneth Mark B. TevesNo ratings yet
- Knowledge of Chemotherapy and Occupational Safety Measures Among Nurses in Oncology UnitsDocument7 pagesKnowledge of Chemotherapy and Occupational Safety Measures Among Nurses in Oncology UnitsIOM BNSNo ratings yet
- India's National Diabetes ProgrammeDocument9 pagesIndia's National Diabetes ProgrammeNaveenNo ratings yet
- Oppenheim J.J., Feldmann M. - Introduction To The Role of Cytokines in Innate Host Defense and Adaptive Immunity (2000) PDFDocument18 pagesOppenheim J.J., Feldmann M. - Introduction To The Role of Cytokines in Innate Host Defense and Adaptive Immunity (2000) PDFHesbon MomanyiNo ratings yet
- Country Presentation MaldivesDocument11 pagesCountry Presentation MaldivesEndah PutriNo ratings yet
- Respiratory MedicationsDocument18 pagesRespiratory Medicationsapi-338095748No ratings yet
- Care of The Older Adult Handouts PrelimsDocument7 pagesCare of The Older Adult Handouts PrelimsAmanda Joy TuizaNo ratings yet
- Three Treasures Correspondences BrochureDocument4 pagesThree Treasures Correspondences Brochure292293709No ratings yet
- Posted: Mon Jun 21, 2010 4:02 PM Post Subject: DENTAL MCQS: Previous Year PaperDocument16 pagesPosted: Mon Jun 21, 2010 4:02 PM Post Subject: DENTAL MCQS: Previous Year PaperMadhul Singhal100% (1)
- Healthcare EnvironmentDocument24 pagesHealthcare EnvironmentJOHN VINCENT BJORN GRAGEDA100% (1)
- O Lightening Probably Occurs Early in Primiparas Because of Tight Abdominal Muscles. inDocument2 pagesO Lightening Probably Occurs Early in Primiparas Because of Tight Abdominal Muscles. inMarie Ashley CasiaNo ratings yet
- OSCDDocument331 pagesOSCDmanselsap100% (1)
- Tata Laksana Perawatan Gigi Pada Pasien Kelainan Jantung Yang Ditanamkan Icd Dan Mengonsumsi WarfarinDocument17 pagesTata Laksana Perawatan Gigi Pada Pasien Kelainan Jantung Yang Ditanamkan Icd Dan Mengonsumsi WarfarinEka ApriantiNo ratings yet
- Rapid HIV Test Detects Antibodies in BloodDocument4 pagesRapid HIV Test Detects Antibodies in Bloodkbl27No ratings yet
- Case Presentation DengueDocument3 pagesCase Presentation DengueLindel Assley Turqueza100% (1)
- PCOS PathophysiologyDocument2 pagesPCOS PathophysiologyMegaNo ratings yet
- Simulation in Health Care Education: Perspectives in Biology and Medicine February 2008Document6 pagesSimulation in Health Care Education: Perspectives in Biology and Medicine February 2008Birendra MahatNo ratings yet
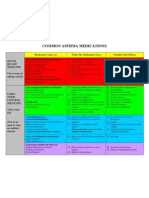
- Common Asthma MedicationsDocument1 pageCommon Asthma MedicationsHeart of the Valley, Pediatric CardiologyNo ratings yet
- International Journal of Pharmaceutical Science Invention (IJPSI)Document6 pagesInternational Journal of Pharmaceutical Science Invention (IJPSI)inventionjournalsNo ratings yet
- SJT Practice Paper Large Print PDFDocument83 pagesSJT Practice Paper Large Print PDFRumaisha Nuha ZNo ratings yet
- Pharmacist Interview QuestionsDocument5 pagesPharmacist Interview Questionsmohdshadan87399No ratings yet
- Minimally Invasive Face-Lifting: S-Lift and S-Plus Lift RhytidectomiesDocument11 pagesMinimally Invasive Face-Lifting: S-Lift and S-Plus Lift RhytidectomiesAditi SharmaNo ratings yet