Professional Documents
Culture Documents
83 Full
83 Full
Uploaded by
abutalebheba95Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
83 Full
83 Full
Uploaded by
abutalebheba95Copyright:
Available Formats
Clinical Medicine 2014 Vol 14, No 1: 83–5 CME Respiratory medicine SAQs
CME Respiratory medicine SAQs (86419): self-assessment
questionnaire
Author: Laura Tanner
SAQs and answers are ONLINE for RCP fellows and (c) Type 2 respiratory failure
collegiate members (d) Metabolic acidosis
(e) Metabolic acidosis with compensation
The SAQs printed in the CME section can only be answered
online to achieve external CPD credits. Any comments should
2 A 65-year-old lady with severe chronic obstructive
be sent in via email only: clinicalmedicine@rcplondon.ac.uk
pulmonary disease (COPD) was admitted to the acute
medical unit. Her exercise capacity was reduced to 20
Format metres. She had increasing breathlessness and cough with
SAQs follow a best of five format in line with the MRCP(UK) purulent sputum. Chest radiograph showed right basal
Part 1 exam. Candidates are asked to choose the best answer consolidation.
from five possible answers.
Aterial blood gases:
The answering process pH 7.25
pCO2 9.3 kPa
1 Go to www.rcplondon.ac.uk/SAQ
pO2 10.8 kPa
2 Log on using your usual RCP username and password
sHCO3 30 mmol/l
3 Select the relevant CME question paper
aHCO3 36 mmol/l
4 Answer all 10 questions by selecting the best answer
base excess (BE) +6 mmol/l
from the options provided
5 Once you have answered all the questions, click on Submit What do these arterial blood gases show?
(a) Chronic, compensated type 2 respiratory failure
Registering your external CPD credits
(b) Acute respiratory acidosis
Carrying out this activity allows you to claim two external (c) Acute on chronic respiratory acidosis
CPD credits. These will be automatically transferred to your (d) Acute on chronic respiratory acidosis with supplemental
CPD diary, where you can review the activity and claim your oxygen
points. (e) Metabolic acidosis with supplemental oxygen
3 A 30-year-old man had a history of 48 hours of vomiting.
1 A 25-year-old intravenous drug user was admitted Blood tests reveal normal renal function but a potassium
to hospital with a heroin overdose. He was given of 2.2 mmol/l.
naloxone in the emergency department with good
Aterial blood gases:
effect and brought round to the acute medicine unit.
On review he was found unconscious. pH 7.47
pCO2 6.7 kPa
Aterial blood gases:
pO2 11.0 kPa
pH 7.25 sHCO3 33 mmol/l
pCO2 8.1 kPa aHCO3 36 mmol/l
pO2 8.7 kPa base excess (BE) +10 mmol/l
sHCO3 24 mmol/l
What do the arterial blood gases show?
aHCO3 28 mmol/l
base excess (BE) +1 mmol/l (a) Metabolic alkalosis, no lung disease
(b) Metabolic alkalosis with impaired oxygenation
What do these arterial blood gases show?
(c) Respiratory acidosis with metabolic compensation
(a) Respiratory acidosis with compensation (d) Metabolic acidosis
(b) Acute respiratory acidosis (e) Acute respiratory acidosis
© Royal College of Physicians 2014. All rights reserved. 83
CMJ1401_SAQs.indd 83 2/4/14 10:13:10 AM
CME Respiratory medicine SAQs
4 A30-year-old male presented with recurrent respiratory 7 A 75-year-old man presented with gradually progressive
infections. Sputum was repeatedly positive for dyspnoea and chronic cough. He is a smoker and had
Staphlococcus aureus and Haemophilus influenzae. Chest previously worked for 20 years in the shipyards in the
radiograph shows bronchiectasis. Genetic testing for cystic 1940s where he was a pipe lagger. On examination he is
fibrosis (CF) showed a R117H mutation of the cystic fibrosis clubbed with bibasal crackles.
gene (class IV defect).
Spirometry:
How does a class IV genetic defect affect the cystic fibrosis
forced expiratory volume (FEV1) 2.23 (84% predicted)
transmembrane conductance regulator (CFTR) protein?
forced vital capacity (FVC) 2.30 (82% predicted)
(a) Cystic fibrosis transmembrane conductance regulator ratio 89%
(CFTR) reaches the apical membrane but is not activated
Computed tomography (CT) of the thorax showed bibasal,
and is non functional
peripheral fibrosis in a usual interstitial pneumonia pattern
(b) There is reduced synthesis of normal CFTR
and pleural plaques.
(c) Nonsense and frameshift mutations lead to premature
termination codons resulting in a lack of protein production What is the most likely diagnosis?
(d) The mutation results in misfolded CFTR that is then
(a) Idiopathic pulmonary fibrosis
degraded in the endoplasmic reticulum.
(b) Asbestosis
(e) The mutation results in reduced CFTR conductance at the
(c) Requires lung biopsy to secure diagnosis
cell surface
(d) Lung cancer
(e) Sarcoidosis
5 With regards to new cystic fibrosis transmembrane
conductance regulator (CFTR) ‘modulator’ therapy which 8 A 45-year-old woman presented with a 4-day history
statement is true? of leg weakness and paraesthesiae. She had a recent
(a) They have been shown to be of benefit in all class defects diarrhoeal illness. During her admission she complained of
(b) For the most common F508del mutation a ‘potentiator’ and a breathlessness on lying flat and nursing staff report she
‘corrector’ are more effective when given in combination appeared confused and drowsy in the mornings.
(c) They are not of benefit in patients whose CFTR protein is What is the best way to assess for respiratory muscle
non-functional weakness (RMW)?
(d) They are administered by inhalation
(e) They are more effective in more severe phenotypes (a) Peak expiratory flow rate morning, afternoon and evening
(b) Pulse oximetry
6 A 75-year-old man presented with breathlessness on (c) Arterial blood gas sampling
exertion. He smoked 40 cigarettes a day and had previously (d) Lying and standing spirometry with spontaneous nasal
worked in the shipyards. He had a cough productive of a inspiratory pressure (SNIP), maximal inspiratory pressure
small amount of phlegm in the mornings and no chest pain. (MIP) and maximal expiratory pressure (MEP)
Chest radiograph showed a well delineated opacity. (e) Monitor clinically looking for reduced chest expansion, weak
cough and morning headache
Spirometry:
forced expiratory volume (FEV1) 1.10 l (50% predicted) 9 In the same patient as question 8, lying and standing
forced vital capacity (FVC) 2.10 l (89% predicted) spirometry revealed a vital capacity of less than 1 l.
ratio 60% predicted She had also started to develop problems with speech,
carbon monoxide transfer factor (TLCO) 56% predicted swallowing and aspiration.
transfer coefficient (KCO) 58% predicted What should be the next step?
Computed tomography (CT) of the thorax showed bilateral, (a) Provide non-invasive ventilation on the ward
discrete, calcified pleural abnormalities with the diffuse (b) Involve the intensive treatment unit (ITU) for potential
pleural thickening. invasive ventilation
How should this patient be managed? (c) Chest radiograph to exclude aspiration pneumonia
(d) Antibiotics for treatment of aspiration pneumonia
(a) He should be followed up in chest clinic with serial CT every (e) Arrange further tests of respiratory muscle function,
3 months spontaneous nasal inspiratory pressure (SNIP), maximal
(b) He should be given smoking cessation, management inspiratory pressure (MIP) and maximal expiratory pressure
of chronice obstructive pulmonary disease (COPD) and (MEP) for first thing in the morning
reassurance with regards to pleural plaques
(c) He should be referred to the surgical team for video-assisted 10 A 72-year-old man with idiopathic pulmonary fibrosis
thoracoscopic surgery (VATS) biopsy (IPF) presented as an emergency to the admissions unit
(d) He should be advised to seek compensation from government- with progressive worsening of breathlessness. He had had
based scheme a diagnosis of idiopathic pulmonary fibrosis (IPF) for 2
(e) He should be followed up with serial chest X-ray (CXR) due years with steady decline of his lung function. Previous
to 25% risk of mesothelioma palliative care discussions have taken place and his wish
84 © Royal College of Physicians 2014. All rights reserved.
CMJ1401_SAQs.indd 84 2/4/14 10:13:10 AM
CME Respiratory medicine SAQs
was to be at home during the end stage of his disease.
He has been treated with oral prednisolone but had CME Cardiology SAQs
continued to deteriorate and required 10 l of oxygen
via CPAP to maintain saturations of 90%. He is now is Answers to the CME SAQs published in
comatose.
Clinical Medicine December 2013
What is the next step in this man’s care?
Q1 Q2 Q3 Q4 Q5 Q6 Q7 Q8 Q9 Q10
(a) Refer patient to the intensive treatment unit (ITU) for (c) (e) (a) (d) (a) (c) (d) (b) (b) (c)
intubation and invasive ventilation
(b) Continue continuous positive airway pressure (CPAP)
Please note, the answer for Q3 should be ‘(a) Digoxin
indefinitely
(c) Remove CPAP and give morphine and midazolam for monotherapy would be reasonable for rate control’,
symptoms not beta blocker as printed.
(d) Transfer home immediately
(e) Chest physiotherapy
© Royal College of Physicians 2014. All rights reserved. 85
CMJ1401_SAQs.indd 85 2/4/14 10:13:10 AM
You might also like
- Acid BaseDocument89 pagesAcid BaseEdouinaNo ratings yet
- Residency: Called - To.See - Patient V1.1Document111 pagesResidency: Called - To.See - Patient V1.1Glen OngNo ratings yet
- Ruppels Manual of Pulmonary Function Testing 10th Edition Mottram Test BankDocument13 pagesRuppels Manual of Pulmonary Function Testing 10th Edition Mottram Test Bankkhuyentryphenakj1100% (32)
- Criteria For Diagnosing Personality DisordersDocument43 pagesCriteria For Diagnosing Personality DisordersKhrycys Olairez RNNo ratings yet
- Approach To Acid-Base Disorders: Quran 5:32Document34 pagesApproach To Acid-Base Disorders: Quran 5:32Hina BatoolNo ratings yet
- Arterial Blood Gas Analysis - making it easyFrom EverandArterial Blood Gas Analysis - making it easyRating: 4.5 out of 5 stars4.5/5 (4)
- Coconut CookbookDocument23 pagesCoconut CookbookNatalia Stone100% (1)
- Arterial Blood GasesDocument10 pagesArterial Blood GasesSoumya BhattacharyaNo ratings yet
- ABG Lecture DR Lenora FernandezDocument60 pagesABG Lecture DR Lenora Fernandezapi-19431894No ratings yet
- ABG Arterial Blood Gas: Interpretation .. Simplified ApproachDocument62 pagesABG Arterial Blood Gas: Interpretation .. Simplified ApproachPrasanna Kumar100% (1)
- SarcoidosisDocument95 pagesSarcoidosisvnybhagat100% (2)
- UNIT: PH and Blood GasesDocument14 pagesUNIT: PH and Blood Gasesbiddyusmc100% (2)
- Arterial Blood Gas - ppt1Document53 pagesArterial Blood Gas - ppt1Madhuri100% (2)
- Metabolism Lippincott's Q&ADocument86 pagesMetabolism Lippincott's Q&Alina amjadNo ratings yet
- Abg Analysis ReviewerDocument21 pagesAbg Analysis ReviewerAyiessa_AJNo ratings yet
- Solar Return ReportDocument5 pagesSolar Return ReportJOYYANo ratings yet
- E RDocument10 pagesE Rroy_linaoNo ratings yet
- Acid-Base Disorders and The ABGDocument28 pagesAcid-Base Disorders and The ABGPaul KelnerNo ratings yet
- Eating Disorders: by Group A1: Marwa Alsaleh, Zahra Almousa, Maha Alshrywi, Israa AlagnamDocument28 pagesEating Disorders: by Group A1: Marwa Alsaleh, Zahra Almousa, Maha Alshrywi, Israa AlagnamYuki HimeNo ratings yet
- Labor Case Digests 7Document7 pagesLabor Case Digests 7Ezra Joy Angagan CanosaNo ratings yet
- Acidosis Alkalosis BiochemistryDocument31 pagesAcidosis Alkalosis BiochemistryliyaNo ratings yet
- ABG Made Simple: DR Satish Deopujari Founder National Chairman (India) PICC 1998Document19 pagesABG Made Simple: DR Satish Deopujari Founder National Chairman (India) PICC 1998Bimantoko Hadi Sriyono100% (1)
- Clinical Chemistry II ELECTROLYTESDocument2 pagesClinical Chemistry II ELECTROLYTESEden MaeNo ratings yet
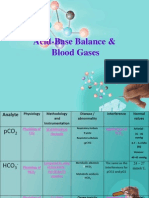
- Acid-Base Balance & Blood GasesDocument39 pagesAcid-Base Balance & Blood GasesSulaiman TahsinNo ratings yet
- StudentDocument2 pagesStudentAnonymous hF5zAdvwCCNo ratings yet
- Acid BaseDocument6 pagesAcid BasejyayNo ratings yet
- Internal Medicine - Phase 3: Important Legal InformationDocument19 pagesInternal Medicine - Phase 3: Important Legal InformationClaire YabaNo ratings yet
- Spirometry and ABG AnalysisDocument23 pagesSpirometry and ABG AnalysisRaihanShaheedNo ratings yet
- Arterial Blood Gas: Interpretation and Clinical ImplicationsDocument112 pagesArterial Blood Gas: Interpretation and Clinical ImplicationsmatrixtrinityNo ratings yet
- Arterial Blood Gases: Laboratory InsightsDocument9 pagesArterial Blood Gases: Laboratory InsightsYusuf NugrohoNo ratings yet
- Abg AnalysisDocument65 pagesAbg AnalysisSyed Farooque AliNo ratings yet
- Arterial Blood Gas Analysis: BY-Shivam Sachan (JR Ii) Moderator - Dr. R.K YADAV (M.D)Document52 pagesArterial Blood Gas Analysis: BY-Shivam Sachan (JR Ii) Moderator - Dr. R.K YADAV (M.D)imranqazi11No ratings yet
- Acid Base and Electrolyte BalanceDocument6 pagesAcid Base and Electrolyte BalanceMuhammad Hamza AlviNo ratings yet
- MCQs of AHN Unit-2 Fluid, Electrolytes & Acid Base ImbalanceDocument7 pagesMCQs of AHN Unit-2 Fluid, Electrolytes & Acid Base Imbalanceloferk44No ratings yet
- ABG - Acidbase Disorders Elmenya University Hospital EGYPTDocument127 pagesABG - Acidbase Disorders Elmenya University Hospital EGYPTkhaledNo ratings yet
- Blood Gas AnalysisDocument5 pagesBlood Gas AnalysisLucy BrittainNo ratings yet
- Blood Gases (Abgs) Interpretation Dr/Baha Eldin Hassan Ahmed Fellow Paediatric Critical CareDocument48 pagesBlood Gases (Abgs) Interpretation Dr/Baha Eldin Hassan Ahmed Fellow Paediatric Critical Carehagir alhajNo ratings yet
- Blood Gases and Acid-Base Disorders: Dr. Wan Nedra Sp. A Pediatricts Departement University of YARSIDocument39 pagesBlood Gases and Acid-Base Disorders: Dr. Wan Nedra Sp. A Pediatricts Departement University of YARSIIQBAL HAKKIKINo ratings yet
- Arterial Blood Gas InterpretationDocument74 pagesArterial Blood Gas InterpretationSarina AsuncionNo ratings yet
- AGD 16 JAN 23. Dr. HERIDocument35 pagesAGD 16 JAN 23. Dr. HERImutiara firdausyNo ratings yet
- Michael Chansky Acid Base Made Easy Handout PDFDocument18 pagesMichael Chansky Acid Base Made Easy Handout PDFAustine OsaweNo ratings yet
- Maimun Zulhaidah A Tinny R Indra Clinical Pathology DeptDocument47 pagesMaimun Zulhaidah A Tinny R Indra Clinical Pathology DeptSunny AghniNo ratings yet
- Clinical Scenario 01Document480 pagesClinical Scenario 01Emon FaizNo ratings yet
- Blood Gases, PH, & Buffer SystemsDocument51 pagesBlood Gases, PH, & Buffer SystemsDiether LanderoNo ratings yet
- Thursday 15 1-30 Jonathan TaliercioDocument74 pagesThursday 15 1-30 Jonathan TaliercioCroitoru CosminNo ratings yet
- ABG Lecture PDFDocument11 pagesABG Lecture PDFbianca maaliwNo ratings yet
- Biochem Acid Base Electrolytes ABGDocument12 pagesBiochem Acid Base Electrolytes ABGNaser Hamdi ZalloumNo ratings yet
- Abg SakshiDocument59 pagesAbg SakshiSakshi GuptaNo ratings yet
- Acid-Base Balance + Arterial Blood GasesDocument30 pagesAcid-Base Balance + Arterial Blood GasesQusai IbraheemNo ratings yet
- Arterial Blood Gas Analysis: DR - Rakesh Chandra Chaurasia PGT 3 Ims, Bhu Moderator: DR - Manjaree Mishra Asset - ProfDocument64 pagesArterial Blood Gas Analysis: DR - Rakesh Chandra Chaurasia PGT 3 Ims, Bhu Moderator: DR - Manjaree Mishra Asset - ProfArmaanjeet SinghNo ratings yet
- 4 5969878728963002643Document21 pages4 5969878728963002643peternady202No ratings yet
- Acid-Base Imbalances: Dr. Emmanuel Sandy Department of Chemical Pathology Comahs-UslDocument49 pagesAcid-Base Imbalances: Dr. Emmanuel Sandy Department of Chemical Pathology Comahs-UslVivian KamaraNo ratings yet
- ABGAnalysis Resident LectureDocument71 pagesABGAnalysis Resident LecturePutu AdhekNo ratings yet
- Metabolic AcidosisDocument102 pagesMetabolic AcidosisShajahan SideequeNo ratings yet
- Arterial Blood Gas Interpretation: Associate Professor Dr. Samah ShehataDocument44 pagesArterial Blood Gas Interpretation: Associate Professor Dr. Samah Shehataraed faisalNo ratings yet
- Computer-Based Scenario Biochemistry: How To Read Bloods?Document66 pagesComputer-Based Scenario Biochemistry: How To Read Bloods?Haytham KhalifaNo ratings yet
- Cases Acid BaseDocument3 pagesCases Acid BaseSa MoNo ratings yet
- Blood Gas Analysis: Respiratory DisordersDocument15 pagesBlood Gas Analysis: Respiratory DisordersYogeshRavalNo ratings yet
- 9.3 Bedside Rules For Acid-Base DisordersDocument4 pages9.3 Bedside Rules For Acid-Base DisordersmahchusNo ratings yet
- PeterLloyd On AcidbaseDocument12 pagesPeterLloyd On AcidbaseThatikala AbhilashNo ratings yet
- 2016 Acid Base DisordersDocument48 pages2016 Acid Base DisordersbellabelbonNo ratings yet
- กรณีศึกษา (case study) อ.เพ็ญนภาDocument8 pagesกรณีศึกษา (case study) อ.เพ็ญนภาKanisthita ChutikittidechapatNo ratings yet
- AbgDocument38 pagesAbgroopaNo ratings yet
- Acid - Base BalanceDocument37 pagesAcid - Base BalanceSittie RamosNo ratings yet
- Arterial Blood Gas AnalysisDocument6 pagesArterial Blood Gas AnalysisMaribee Tagayun EspirituNo ratings yet
- Blood GasesDocument3 pagesBlood GasesFaithNo ratings yet
- Selected Constants: Oxidation–Reduction Potentials of Inorganic Substances in Aqueous SolutionFrom EverandSelected Constants: Oxidation–Reduction Potentials of Inorganic Substances in Aqueous SolutionNo ratings yet
- Chemistry and Biochemistry of Oxygen Therapeutics: From Transfusion to Artificial BloodFrom EverandChemistry and Biochemistry of Oxygen Therapeutics: From Transfusion to Artificial BloodAndrea MozzarelliNo ratings yet
- PlasmidsDocument53 pagesPlasmidsPrerana SikarwarNo ratings yet
- Human Body Systems ProjectDocument9 pagesHuman Body Systems ProjectmrdornNo ratings yet
- Current Affairs Concept Notes For Class 6 To 8.Document2 pagesCurrent Affairs Concept Notes For Class 6 To 8.Learning 360No ratings yet
- Procedure On Knee Orthroscopy-2Document15 pagesProcedure On Knee Orthroscopy-2pslokesha84No ratings yet
- Prescription For Addiction: UpdateDocument8 pagesPrescription For Addiction: Updateoptions1No ratings yet
- Obesity Cultural and Biocultural Perspectives by Alexandra A. BrewisDocument231 pagesObesity Cultural and Biocultural Perspectives by Alexandra A. BrewisDiana Fernanda Espinosa SerranoNo ratings yet
- Acquired Hypopigmentation Disorders Other Than Vitiligo - UpToDateDocument23 pagesAcquired Hypopigmentation Disorders Other Than Vitiligo - UpToDateBhargav YagnikNo ratings yet
- S7A - Guideline - Safety Pharmacology Studies For Human PharmaceuticalsDocument13 pagesS7A - Guideline - Safety Pharmacology Studies For Human Pharmaceuticalsmogmo TsaiNo ratings yet
- English Project: AcknowledgementDocument11 pagesEnglish Project: AcknowledgementAbhishek ChauhanNo ratings yet
- Anemia AplasicaDocument9 pagesAnemia AplasicaCARLOS ALBERTO TORRES SALASNo ratings yet
- Five Myths On Fathers and FamilyDocument42 pagesFive Myths On Fathers and FamilyJOEMAFLAGENo ratings yet
- Initial Data Base To Priority Setting NotesDocument4 pagesInitial Data Base To Priority Setting NotesTangonan DarrelNo ratings yet
- 5 Do We Need Economics in MedicineDocument24 pages5 Do We Need Economics in MedicineHanan AhmedNo ratings yet
- Family Nursing Analysis LatestDocument143 pagesFamily Nursing Analysis LatestLyca Mae AurelioNo ratings yet
- Sas 1-3Document3 pagesSas 1-3Lyons SchimttNo ratings yet
- Hematopoiesis: Part 2: Erythropoiesis and LeukopoiesisDocument62 pagesHematopoiesis: Part 2: Erythropoiesis and LeukopoiesisJohn Marie IdavaNo ratings yet
- By:Dr Herbert Sihite Spog: Divisi Feto Maternal FK Usu /rs HamDocument26 pagesBy:Dr Herbert Sihite Spog: Divisi Feto Maternal FK Usu /rs HamDyn AdrianiNo ratings yet
- ICSE Board Class X Geography Board Paper - 2013: Time: 2 Hrs Total Marks: 80 General InstructionsDocument5 pagesICSE Board Class X Geography Board Paper - 2013: Time: 2 Hrs Total Marks: 80 General InstructionsAmanNo ratings yet
- Shiatsu - Case Study - Diseases - Problems Helped by ShiatsuDocument1 pageShiatsu - Case Study - Diseases - Problems Helped by ShiatsunaveenNo ratings yet
- CattleHandbookApril 2008Document70 pagesCattleHandbookApril 2008majdirossrossNo ratings yet
- Carbon TetrachlorideDocument5 pagesCarbon Tetrachloridesummi64No ratings yet