Professional Documents
Culture Documents
2024 VPD FormFINAL 16012024
Uploaded by
dkid9876Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2024 VPD FormFINAL 16012024
Uploaded by
dkid9876Copyright:
Available Formats
Academic Affairs
Vaccine Preventable Diseases Evidence Form 2024
General Practitioner/Nurse Practitioner Instruction for completing this form:
1. Please complete sections 2 and 3 (pages 2 to 5), for student’s to be eligible to attend placement
2. Please provide the student with the completed and signed form and any pathology results required.
Immunisation requirements:
• Vaccination Guidelines: as per current edition of the National Health and Medical Research Council Australian
Immunisation Handbook.
• Letters from medical practitioners or other vaccine service providers should be on Practice/Facility letterhead, signed by
the provider/practitioner including professional designation and service provider number.
• Hepatitis B: In accordance with the Australian Immunisation Handbook, 2022, the minimum recommended Hepatitis B
vaccination schedule is 0 month (first dose), 1 month (second dose) and 4-6 months (third dose), with serology testing
undertaken one month after the third dose. For adolescents between the ages of 11-15 Hepatitis B vaccine may be given
as a two-dose course, with the two doses 4-6 months apart. For infants a 3 dose course at 2, 4 and 6 months of age. An
accelerated Hepatitis B schedule of vaccination is not accepted as the course will not be completed until the 4th dose
at 12 months.
Documented evidence that an individual is not susceptible to Hepatitis B infection and therefore does not require
immunisation, may include serology tests indicating the presence of Hepatitis B core Antibody or a documented history
of past Hepatitis B infection. Students who are Hepatitis B antigen positive, do not have to disclose their Hepatitis B
infection status unless they perform exposure-prone procedures.
• Measles, Mumps, Rubella: Immunisation requires two doses of MMR vaccine at least one month apart. Positive IgG
indicates evidence of serological immunity, which may result from either natural infection or immunisation.
• Varicella: as for Measles, Mumps, Rubella – see note in Varicella section on form for more details (Page 3).
• Pertussis: evidence of one adult dose of dTpa within the past 10 years.
• Tuberculosis – student to provide completed QHealth TB Risk Assessment form. If they identify as at risk in Part A or Part B,
they must contact a Queensland Health TB Clinic for review or receive advise through your Practice if further testing is
required.
• Influenza: evidence that student has received a flu vaccine for the current ‘flu season’. Required annually.
Student Instructions for completing this form:
This form is to be completed in consultation with your General Practitioner (GP) or Nurse Practitioner (NP).
1. Enter your details in Section 1 page 2 of this document, and sign as authority for the University to use the information in
this form.
2. Obtain your past immunisation records eg.via council records, past GPs or by accessing mygov. If you cannot obtain your
records your Healthcare provider may request you to undergo blood testing to determine your immunity status and then
advise action as required to ensure you meet immunity requirements.
3. Arrange an appointment for your GP or NP to complete Sections 2 and 3 in full, providing initials against each item if you
are compliant. If you are not compliant, you may need to make further appointments to complete all immunisations.
You need to take your immunisation records with you for your appointment.
4. All students must read and complete Section 4 before signing and dating where indicated.
5. It is your responsibility to check that sections 2 – 3 of the form have been completed in full before you leave the
general practitioner/nurse practitioner’s office or that appointments for further immunisations are planned.
6. Read and complete Sections 4 and 5 and add your name and student number to the bottom of each page before
submitting all 5 pages of this document via InPlace.
Student Name: Student Number: 1 of 5
Reviewed 1/12/2023
Academic Affairs
Vaccine Preventable Diseases Evidence Form 2024
Section 1: Student Consent (student to complete)
I hereby request and give consent for the General Practitioner (GP)/Nurse Practitioner (NP) identified in Section 2 to complete this form
in relation to my health information. I understand that the information is being collected by the University of Southern Queensland
(UniSQ) for the purpose of administration of my admission and enrolment at UniSQ including (without limitation) for the purpose of
administration of any professional experience placements. I authorise UniSQ to disclose my personal/sensitive information to:
a) placement facilities; and
b) The Australian Health Practitioner Regulation Agency (AHPRA) - only if required under the AHPRA mandatory guidelines. I
understand that all blood tests & vaccines cost will be the responsibility of the student.
Student Name:
Student Number: Mobile phone number:
Date of Birth:
Course of Study:
Student Signature: Date of Signature:
Important Student Note: Students enrolled in Bachelor of Nursing/Bachelor of Midwifery may undertake exposure prone procedures
(EPP) throughout the course of their study and are required to Complete Section 4 Exposure Prone Procedures at the commencement
of the program.
Section 2: Completing General Practitioner/Nurse Practitioner Details
General/Nurse Practitioner’s Name (PRINT):
Practice Stamp or Facility name &
Address
Provider Number:
General/Nurse Practitioner’s Signature:
Date:
Student Name: Student Number: 2 of 5
Reviewed 1/12/2023
Academic Affairs
Vaccine Preventable Diseases Evidence Form 2024
Section 3: Immunisations
Health Practitioner ONLY to complete this section – please ensure all immunisation dates and/or serology
results are added
Evidence of vaccination General Practitioner/Nurse
Disease
(Please select ONE option for each) Practitioner
3.1 Measles, Two documented doses of MMR vaccine at least one month apart GP/NP to initial when
Mumps and Date of doses 1: ____/____/_____ 2: ____/____/_____ compliant:
Rubella (MMR) OR
Documented evidence of positive IgG for MMR Initial: __________
Date of serology: ____/____/_____
Booster dose if required: ____/____/_____
OR
Birth date before 1966
* Please note if responsive to measles, mumps or rubella only 1 booster dose
advised.
3.2 Pertussis Documented evidence of one adult dose of dTpa within the past GP/NP to initial when
(Whooping Cough) ten years compliant:
or dTpa Date of dose: ____/____/_____
(Diphtheria,
*Please note that Exercise Physiology Students do not require dTpa Initial: __________
Tetanus and
Pertussis)
3.3 Varicella Two documented doses of Varicella vaccine at least one month GP/NP to initial when
apart compliant:
(Chicken Pox)
Date of doses 1: ____/____/_____ 2: ____/____/_____
OR
Initial: __________
Documented evidence of positive IgG for Varicella
Date of serology: ____/____/_____
Booster dose if required: ____/____/_____
OR
History of chickenpox or documentation of physician-diagnosed
shingles
If student has a negative history of Varicella infection and no documented history of age-appropriate
vaccination, it is suggested to have serology testing done first as a majority of those with a negative history
are immune, and thus may not require vaccination. Testing to check for seroconversion after varicella
vaccination is not recommended.
3.4 Annual Evidence of Influenza vaccination yearly during annual ‘Flu Season’ GP/NP to initial when
Seasonal – must be completed every year compliant:
Influenza Date of dose 1st year: ___/___/____
Vaccination *After first year, evidence to be provided separately via InPlace every 12
months Initial: __________
Student Name: Student Number: 3 of 5
Reviewed 1/12/2023
Academic Affairs
Vaccine Preventable Diseases Evidence Form 2024
3: Immunisations
Health Practitioner ONLY to complete this section
General Practitioner/Nurse
Evidence of vaccination
Disease Practitioner Clinical
(Please select ONE option for each) Assessment
3.5(a) Hepatitis B Three documented doses of Hepatitis B vaccines given over 4 to 6 Dose 2 due:
months
Please note: __________________
Dose 1 (0 months): ____/____/_____
Accelerated Dose 3 due:
courses are not Dose 2 (1 month): ____/____/______
__________________
accepted Dose 3 (4-6 months): ____/____/_____
OR - serology after 2 doses is not accepted
Hepatitis B Serology (titre level >10mIU/ml at least 4 to 8 weeks
Fully Compliant
after completion of primary course) GP/NP to Initial when fully
Titre level: ________ Date of serology: ____/____/_____ compliant:
AND - if negative serology after first series of 3 vaccines
One booster dose of Hepatitis B vaccines for non-responder to Initial:_____________
primary course of 3 vaccines (anti-HBs titre <10mIU/ml at least 4 -
8 weeks after completed primary course)
Dose 4 (0 months): ____/____/_____ Non-responder
Hepatitis B Serology (4 weeks post dose 4) _________ Please complete section below
only if student has completed
Date: _____/____/_____If anti- HBs still <10 mIU per mL then the 6 vaccinations here and still
has negative serology 1 month
Dose 5 (1 month): ____/____/______
after the second series. All 6
Dose 6 (2 months): ____/____/_____ doses and serologies must be
documented here.
Titre level (4 to 8 weeks after Dose 6): ____/____/_____
3.5(b): Non-Responder to Hepatitis B Vaccine Acknowledgement – ONLY COMPLETE 3.5(b) if all 6
vaccinations + negative serology results after each series are completed & documented above. Health Practitioner to complete
this section ONLY if student meets the below guidelines.
• The Student has completed both a primary and secondary course of Hepatitis B vaccines and does not have
adequate post-vaccination Hepatitis B antibodies detected following completion of the secondary course and the
student and I have discussed risk and prevention required whilst on clinical placement.
• The student is aware of the recommended management in the event of a potential exposure to Hepatitis B,
including the recommendations for administration of Hepatitis B immunoglobulin (HBIG).
• The student is aware that if they undertake exposure prone procedures throughout the course of their study
that they have a responsibility to have Hepatitis B screening at least annually, and after any blood or body fluid
exposure.
Student Name (PRINT) Student Signature Date
GP/NP Name (PRINT) GP/NP Signature Date
Student Name: Student Number: 4 of 5
Reviewed 1/12/2023
Academic Affairs
Vaccine Preventable Diseases Evidence Form 2024
Immunisations - For Students residing outside of Queensland ONLY (complete relevant sections)
Health Practitioner ONLY to complete this section
General
Evidence of vaccination Practitioner/Nurse
State Disease
(Please select ONE option for each) Practitioner Clinical
Assessment
Western Tuberculosis
Have you worked or been a patient in a hospital outside Western GP/NP to initial when
Australia Australia, or overseas, in the past 12 months? compliant:
Screening
NO YES (go to next section) Initial: __________
If YES and you have not had an MRSA screen result since that time
GP/NP to initial when
you are required to have an MRSA screening.
compliant:
Date____/____/_____ Result:____________ Initial: __________
Northern Hepatitis A Evidence of two doses of Hepatitis A vaccine at least 6 GP/NP to initial when
Territory months apart compliant:
and Dose 1: ____/____/_____ Dose 2: ____/____/_____
Victoria
OR Initial: __________
Serology Titre level: ____________
Tasmania HIV Antibody GP/NP to initial when
Test Date: ____/____/_____ Result:__________________ compliant:
Initial: __________
Hepatitis C GP/NP to initial when
Antibody Test Date: ____/____/_____ Result:___________________ compliant:
Initial: __________
Section 4: Exposure Prone Procedures (all students to complete, please read document attached)
The current Communicable Diseases Network Australia (CDNA) guidelines define an Exposure Prone Procedure as one
where there is a risk of injury to the healthcare worker resulting in exposure of the patient’s open tissue to the blood of the
worker. These procedures include those where the hands of the worker (whether gloved or not) may come into contact
with sharp instruments, needle tips, or sharp tissue (spicules of bone or teeth) inside a patient’s open body cavity, wound or
confined anatomical space where the hands or fingertips may not be completely visible at all times.
While there is not a requirement to provide evidence of such, students must be aware of their infectious disease
status.
This student is aware of their infectious status with regards to HIV and HCV, and any consequent implications.
Student Name (PRINT) Student Signature Date
Section 5: Student Declaration
I declare that the information provided on this form is true and correct.
Student Name (PRINT) Student Signature Date
Student Name: Student Number: 5 of 5
Reviewed 1/12/2023
You might also like
- Immunization Report PDFDocument2 pagesImmunization Report PDFJag UnathNo ratings yet
- PSW6 - PPHFDocument16 pagesPSW6 - PPHFanishthNo ratings yet
- Univ of Florida ImmunisationDocument2 pagesUniv of Florida ImmunisationPavan Kumar MangipudiNo ratings yet
- Pre-Registration Nursing Information For Prospective StudentsDocument4 pagesPre-Registration Nursing Information For Prospective StudentsbthangarajNo ratings yet
- Immunizations Page Effective Spring 2010 Guidelines For Completing Immunization InformationDocument7 pagesImmunizations Page Effective Spring 2010 Guidelines For Completing Immunization InformationShubham TrivediNo ratings yet
- Form B - Other Jobs - High - V High Risk TBDocument8 pagesForm B - Other Jobs - High - V High Risk TBMorshed HumayunNo ratings yet
- Immunization Requirement Form - UpdateDocument2 pagesImmunization Requirement Form - UpdateManojkumar ANo ratings yet
- Immunisation Compliance Certificate 1Document2 pagesImmunisation Compliance Certificate 1api-687735091No ratings yet
- Undertaking Declaration PD2022 - 030Document2 pagesUndertaking Declaration PD2022 - 030MejoNo ratings yet
- Memorandum: Faculty of DentistryDocument3 pagesMemorandum: Faculty of Dentistryabhinav guptaNo ratings yet
- Pre-Placement Assessment Form - Jan 2023Document4 pagesPre-Placement Assessment Form - Jan 2023Nicole KhouryNo ratings yet
- Immunization Record PART I: To Be Completed by The Student. Please Print or TypeDocument3 pagesImmunization Record PART I: To Be Completed by The Student. Please Print or Typeruhayl khanNo ratings yet
- Immunisation Compliance Form 1 2018 Version 5 FinalDocument2 pagesImmunisation Compliance Form 1 2018 Version 5 FinalAnthony Farquhar WuNo ratings yet
- Medical Record FormDocument4 pagesMedical Record FormДария КоваленкоNo ratings yet
- AMOpportunities Certificate of ImmunizationDocument1 pageAMOpportunities Certificate of ImmunizationАида АрзуманянNo ratings yet
- Immunization Letter NB FORM RevisedDocument6 pagesImmunization Letter NB FORM RevisedUddhavendra Pal SinghNo ratings yet
- An Important FormDocument3 pagesAn Important FormRachel ColeNo ratings yet
- Immunization Record: Form Is Due at OrientationDocument3 pagesImmunization Record: Form Is Due at OrientationCasey JonesNo ratings yet
- Appendix 6 Undertaking - Declaration FormDocument1 pageAppendix 6 Undertaking - Declaration FormAr AsifNo ratings yet
- Dd/Mm/Yyyy Dd/Mm/Yyyy Dd/Mm/YyyyDocument6 pagesDd/Mm/Yyyy Dd/Mm/Yyyy Dd/Mm/YyyyJohn50% (2)
- Immuz FormDocument2 pagesImmuz Formapi-250919827No ratings yet
- Good Health in the Tropics: Advice to Travellers and SettlersFrom EverandGood Health in the Tropics: Advice to Travellers and SettlersNo ratings yet
- VSLO Immunization Form 22-23Document6 pagesVSLO Immunization Form 22-23Will HNo ratings yet
- Immun RecordDocument2 pagesImmun RecordNonofYaNo ratings yet
- Infectious Disease Screening Immunisation Policyincluding BBVV 4Document13 pagesInfectious Disease Screening Immunisation Policyincluding BBVV 4aqeelNo ratings yet
- Immreq15 16Document2 pagesImmreq15 16api-234991765No ratings yet
- Phase II To III - 324 Pregnant Women - Randomized Placebo-Controlled Observer-Blind Study of BNT162b2 or Placebo. Start Feb 2021 and End Aug 2022Document11 pagesPhase II To III - 324 Pregnant Women - Randomized Placebo-Controlled Observer-Blind Study of BNT162b2 or Placebo. Start Feb 2021 and End Aug 2022Mary-Jane StevensNo ratings yet
- FIU Immunization Documentation FormDocument2 pagesFIU Immunization Documentation FormMO MONo ratings yet
- Rhodes Immunization RecordDocument5 pagesRhodes Immunization RecordDr.P.S.N RajuNo ratings yet
- University of Minnesota Academic Health Center Student Tuberculosis & Immunization FormDocument2 pagesUniversity of Minnesota Academic Health Center Student Tuberculosis & Immunization Formmikey pNo ratings yet
- GW Hospital MOU & Observer Health Information FormDocument2 pagesGW Hospital MOU & Observer Health Information Formengel0321hotmail.comNo ratings yet
- Immunization FormsDocument8 pagesImmunization FormsJobin JosephNo ratings yet
- MD Occupational Health ProtocolDocument6 pagesMD Occupational Health ProtocolGareth GrechNo ratings yet
- Vaccination Requirements of IFMSA Exchange Progam in Israel-9.15Document2 pagesVaccination Requirements of IFMSA Exchange Progam in Israel-9.15Niko DobrilovicNo ratings yet
- COVID 19 Consent FormDocument2 pagesCOVID 19 Consent FormfvdssfdNo ratings yet
- Kindergarten WorksheetDocument2 pagesKindergarten WorksheetJayRAjNo ratings yet
- Screenshot 2022-08-09 at 1.33.29 PMDocument6 pagesScreenshot 2022-08-09 at 1.33.29 PMsivapraveenaNo ratings yet
- Health Information FormDocument13 pagesHealth Information FormArtero-Cavallaro PabloNo ratings yet
- 2014-2015 Texas Minimum State Vaccine Requirements For Students Grades K-12Document4 pages2014-2015 Texas Minimum State Vaccine Requirements For Students Grades K-12James AllenNo ratings yet
- Immunization Requirement - Student Health Center - The University of UtahDocument2 pagesImmunization Requirement - Student Health Center - The University of Utahmithun916No ratings yet
- Examinee's Guide FOE 2022-10 (Pandemic Edition) ADocument22 pagesExaminee's Guide FOE 2022-10 (Pandemic Edition) ASam DeeNo ratings yet
- Instruction For Medical Examination - eDocument2 pagesInstruction For Medical Examination - emanueltsibiaNo ratings yet
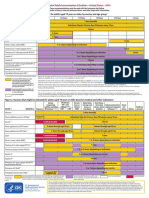
- Figure 1. Recommended Immunization Schedule For Adults Aged 19 Years or Older, by Vaccine and Age GroupDocument2 pagesFigure 1. Recommended Immunization Schedule For Adults Aged 19 Years or Older, by Vaccine and Age GroupmsarasNo ratings yet
- Vaccination Requirement International Students 022019Document2 pagesVaccination Requirement International Students 022019KryzNo ratings yet
- Dear Healthcare Provider 2014Document1 pageDear Healthcare Provider 2014TanuNo ratings yet
- PSW Clinical Requirements Package Fall 2023 InternationalDocument16 pagesPSW Clinical Requirements Package Fall 2023 InternationalAnish KumarNo ratings yet
- Occupational Health QuestionnaireDocument13 pagesOccupational Health QuestionnaireMohamed HafezNo ratings yet
- CUB - Immunisation FormDocument2 pagesCUB - Immunisation FormArcane BeingNo ratings yet
- Ocfs-Medical Statement of Child in ChildcareDocument2 pagesOcfs-Medical Statement of Child in ChildcareNikki NievesNo ratings yet
- 2021 Immunisations FormDocument3 pages2021 Immunisations Formmilksheikh2004No ratings yet
- Health Immunization Clearance Form: Section A: ImmunizationsDocument3 pagesHealth Immunization Clearance Form: Section A: ImmunizationsFaith SetikNo ratings yet
- Adult ScheduleDocument3 pagesAdult ScheduledrmanojvimalNo ratings yet
- ImmunizationCertificate PDFDocument2 pagesImmunizationCertificate PDFAnonymous kq5iEDxxhrNo ratings yet
- Immunization FormsDocument6 pagesImmunization FormsNadya IrsalinaNo ratings yet
- Reading VaccineImmunizationDocument13 pagesReading VaccineImmunizationelztly4694No ratings yet
- ScheduleDocument2 pagesScheduleapi-286634335No ratings yet
- 2019 - 2020 - Boston Immunization - Hult Immunization FormDocument4 pages2019 - 2020 - Boston Immunization - Hult Immunization FormOscar RomainvilleNo ratings yet
- Influenza vaccination: What does the scientific proof say?: Could it be more harmful than useful to vaccinate indiscriminately elderly people, pregnant women, children and health workers?From EverandInfluenza vaccination: What does the scientific proof say?: Could it be more harmful than useful to vaccinate indiscriminately elderly people, pregnant women, children and health workers?No ratings yet
- USMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsFrom EverandUSMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsRating: 5 out of 5 stars5/5 (9)
- BAMBOO U - 5 Ways To Process BambooDocument11 pagesBAMBOO U - 5 Ways To Process BambooeShappy HomeNo ratings yet
- GBC Module 1Document69 pagesGBC Module 1MOHAMED82% (129)
- Vaccum FilterationDocument6 pagesVaccum FilterationAkshay bhuranNo ratings yet
- Kali Kaula A Manual of Tantric Magick HardbackDocument3 pagesKali Kaula A Manual of Tantric Magick Hardbackalintuta20% (1)
- The Revenge of The SerpentDocument2 pagesThe Revenge of The SerpentMiyamoto MusashiNo ratings yet
- USEFUL TIPS For Repairing LAPTOPDocument17 pagesUSEFUL TIPS For Repairing LAPTOPGeronJosephusLofrancoManaiz100% (1)
- Revised EstimateDocument2 pagesRevised EstimateMd. Abdul HaiNo ratings yet
- Health Benefits of Financial Inclusion A Literature ReviewDocument7 pagesHealth Benefits of Financial Inclusion A Literature Reviewl1wot1j1fon3No ratings yet
- 118CP Selection of CP Systems For Reinforced Concrete StructuresDocument15 pages118CP Selection of CP Systems For Reinforced Concrete StructuresWill NashNo ratings yet
- What Is Splunk - (Easy Guide With Pictures) - Cyber Security KingsDocument9 pagesWhat Is Splunk - (Easy Guide With Pictures) - Cyber Security Kingsrokoman kungNo ratings yet
- Thesis Statement, Topic Sentence, and Supporting Details: Paul Christian Reforsado AbadDocument29 pagesThesis Statement, Topic Sentence, and Supporting Details: Paul Christian Reforsado AbadMicole BrodethNo ratings yet
- Valley Line LRT Preliminary DesignDocument26 pagesValley Line LRT Preliminary DesigncaleyramsayNo ratings yet
- Safety StockDocument8 pagesSafety StockIwan NovaNo ratings yet
- Synthesis of Sufanilic AcidDocument4 pagesSynthesis of Sufanilic AcidWinston Jake Gerolaga0% (1)
- Human Resource ManagementDocument86 pagesHuman Resource ManagementK V S PRASD REDDYNo ratings yet
- Study of Steam Generation Units With Their Accessories and MountingsDocument64 pagesStudy of Steam Generation Units With Their Accessories and MountingsMasudur RahmanNo ratings yet
- .50 BMG - Wikipedia PDFDocument13 pages.50 BMG - Wikipedia PDFAce ActionNo ratings yet
- Goat Fattening Rs. 0.85 MillionDocument18 pagesGoat Fattening Rs. 0.85 MillionZakir Ali100% (1)
- Lenovo Ideapad V110-15AST - LV114A (15270-1 08A03)Document64 pagesLenovo Ideapad V110-15AST - LV114A (15270-1 08A03)Mahmut KaralarNo ratings yet
- Adenosine Deaminase: Quantitative Determination of Adenosine Deaminase (ADA) in Serum and Plasma SamplesDocument1 pageAdenosine Deaminase: Quantitative Determination of Adenosine Deaminase (ADA) in Serum and Plasma Samplesmark.zac1990No ratings yet
- How To ApplyDocument129 pagesHow To ApplySasa KasaNo ratings yet
- STEP English (1-18) All Worksheets 2020Document134 pagesSTEP English (1-18) All Worksheets 2020Shema ZulfiqarNo ratings yet
- Modules in Grade 12: Quarter 1 - Week 3 Academic Track - StemDocument23 pagesModules in Grade 12: Quarter 1 - Week 3 Academic Track - StemZenarose MirandaNo ratings yet
- Energy Sector Capacity Building Diagnostic and Needs Assessment StudyDocument150 pagesEnergy Sector Capacity Building Diagnostic and Needs Assessment StudyAyoub EnergieNo ratings yet
- Special Theory of RelativityDocument16 pagesSpecial Theory of RelativityBrigita SteffyNo ratings yet
- Azam in 30 DuaDocument3 pagesAzam in 30 DuafaizaninNo ratings yet
- NCERT Exemplar Class 8 Maths Solutions Chapter 3 Square-Square Root & Cube-Cube RootDocument77 pagesNCERT Exemplar Class 8 Maths Solutions Chapter 3 Square-Square Root & Cube-Cube Rootdeep34No ratings yet
- First Quarter Examination in PracticalDocument2 pagesFirst Quarter Examination in PracticalMark Anthony B. AquinoNo ratings yet
- Data Mining ToolsDocument9 pagesData Mining Toolspuneet0303No ratings yet
- English Language Unit 1 May 2011Document3 pagesEnglish Language Unit 1 May 2011Kieran RichardsNo ratings yet