Professional Documents
Culture Documents
Causes of Open Apices
Uploaded by
kowmudimaddineniOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Causes of Open Apices
Uploaded by
kowmudimaddineniCopyright:
Available Formats
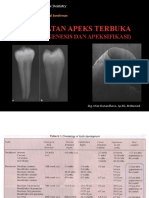
CAUSES OF OPEN APICES
1. Incomplete development The open apex typically occurs when the pulp undergoes necrosis as a result of caries or trauma, before root growth and development are complete (i.e. during stages 1-4) An open apex can also occasionally form in a mature apex (stage 5) as a result of 2. Extensive apical resorption due to orthodontic treatment, periapical pathosis or trauma 3. Root end resection during periradicular surgery 4. Over-instrumentation
Stage 1
Teeth with wide divergent apical opening and a root length estimated to less than half of the final root length.
Stage 2
Teeth with wide divergent apical opening and a root length estimated to half of the final root length.
Stage 3
Teeth with wide divergent apical opening and a root length estimated to two thirds of the final root length.
Stage 4
Teeth with wide open apical foramen and nearly completed root length.
Stage 5
Teeth with closed apical foramen and completed root development.
MANAGEMENT OF INCOMPLETELY DEVELOPED NON VITAL TEETH
_ Management
of open apices
_ Obturation without creating apical barrier3 _ Customized cone technique using - blunted tips - inverted cones - apical impression heat chemicals - rolled cone heat chemicals _ Thermoplasticized obturation _ Short fill technique Obturation after creating apical barrier _ Root end induction of calcific barrier/ apexification3,5 - induction of blood clot in the periradicular region - antibiotic pastes - calcium hydroxide mixed with various materials - collagen calcium gel
- bone morphogenic proteins - tricalcium phosphate _ Placement of artificial barriers (root-end filling materials) - amalgam - glass ionomer cement - composite - mineral trioxide aggregate6 - calcium hydroxide powder - freeze dried bone/dentin - resorbable ceramic - tricalcium phosphate - dentinal shavings This is the case of a 28-year-old male patient with a history of trauma to tooth number 8 when he was a child. As Figure 1 clearly shows, there was incomplete root formation including the absence of apical closure. There was also evidence of a periapical radiolucency. The patient came in with symptoms of abscess, including pain and periapical swelling. I placed him on antibiotics and analgesics to control the acute symptoms and we scheduled another appointment for treatment. Initially, it looked as if it would be a cut-and-dried case of obturation and immediate apicoectomy. When he returned in two weeks, the acute symptoms had abated, and I initiated treatment. I opened the access as wide as possible without compromising the crown, achieved measurement control with an apex locater, confirmed it by radiograph (Figure 2), and accomplished instrumentation with instruments as wide as a #140 reamer. I utilized large-diameter hedstrom files along the canal walls to check for tissue and debris. Now, how in blazes was I going obturate? I was able to dry the canal and then pack MTA cement to the apical measurement, using the reverse side of a coarse paper point until there was some apical resistance, thus creating a stop. Using cotton wrapped around a large diameter file, I cleaned the excess cement from the canal walls. I then placed EZ-Fill cement, using the bi-directional spiral, and thus the canal was flooded with sealer. I reversed a large gutta-percha cone, dipped it into solvent for three seconds, and placed it to measurement control. Using a spreader with no apical pressure, I laterally condensed the mass of gutta-percha, then coated a second large cone with sealer and placed it into the canal in the normal direction. Since research has shown that AH-26 based EZ-Fill sealer alone would be good enough to seal the canal, the gutta-percha core only helps to force the sealer against the MTA stop and the canal walls, leading to the final result seen in Figure 3. Immediate surgery was not necessary, and the patient walked out very happy. The dentist also felt satisfied with the result, but only time will decide the ultimate success in the case of this blunderbuss.
You might also like
- Pulpo, Pulpec, Apex, Injuries 1Document6 pagesPulpo, Pulpec, Apex, Injuries 1Cyril Almario Cunanan100% (1)
- Management of Blunderbuss CanalsDocument11 pagesManagement of Blunderbuss CanalsNitesh PatilNo ratings yet
- Apexogenesis of A Symptomatic MolarDocument5 pagesApexogenesis of A Symptomatic MolarFoysal SirazeeNo ratings yet
- Endodontics Final ReviewerDocument16 pagesEndodontics Final ReviewerMehdi Moshaveri100% (3)
- Procedural Errors in Root Canal Treatment: Sheet #5Document8 pagesProcedural Errors in Root Canal Treatment: Sheet #5Popescu MihaelaNo ratings yet
- UNIT4 Endodontics - Best PPDocument37 pagesUNIT4 Endodontics - Best PPAnna PruteanuNo ratings yet
- Clinical Management of Severe External Root Resorption: T C K Y A C C P LDocument6 pagesClinical Management of Severe External Root Resorption: T C K Y A C C P LNevena SaulicNo ratings yet
- Apexification ApexogenesisDocument68 pagesApexification ApexogenesisSarath MohanNo ratings yet
- 13.endodontic Treatment FR YounPermanent TeethDocument31 pages13.endodontic Treatment FR YounPermanent TeethKhan MustafaNo ratings yet
- International Journal of Research in Dentistry: Single Sitting Apexification Treatment With Mta Apical Plugs: A CaseDocument4 pagesInternational Journal of Research in Dentistry: Single Sitting Apexification Treatment With Mta Apical Plugs: A CaseirfanaNo ratings yet
- DhaDocument175 pagesDhaSOMVIR KUMARNo ratings yet
- Regenerative EndodonticsDocument46 pagesRegenerative EndodonticsShameena KnNo ratings yet
- Pulp Therapy of Non-Vital Teeth (Pulpectomy)Document27 pagesPulp Therapy of Non-Vital Teeth (Pulpectomy)Mahmoud A. ZoghborNo ratings yet
- Intro To EndoDocument18 pagesIntro To EndoGareth DoodyNo ratings yet
- En Do Don TicsDocument5 pagesEn Do Don TicsAbhinav TalekarNo ratings yet
- Coanal AtresiaDocument4 pagesCoanal AtresiaBkas GrgNo ratings yet
- Palatal and Facial Veneers To TreatDocument11 pagesPalatal and Facial Veneers To TreatSabrina Antonella Zeballos ClarosNo ratings yet
- Endo Pre FinalsDocument18 pagesEndo Pre FinalsRayne Gelle100% (2)
- Makalah Skenario 3 Blok 6Document45 pagesMakalah Skenario 3 Blok 6Hanaria Putri S EffriantoNo ratings yet
- Endodontic SurgeryDocument8 pagesEndodontic SurgeryjoseNo ratings yet
- L3. Apexogenesis - ApexificationDocument44 pagesL3. Apexogenesis - ApexificationAGENG RAHMA HIJAHANIS ILMASTITI 1No ratings yet
- Dha LastDocument197 pagesDha LastCarlos Vidal Tudela89% (27)
- 4 - 10) Pulp Therapy For The Young Permanent DentitionDocument15 pages4 - 10) Pulp Therapy For The Young Permanent Dentitionبراءة أحمد السلاماتNo ratings yet
- Vital Pulp TherapyDocument56 pagesVital Pulp Therapyapi-37103310% (1)
- Eur J Esthet Dent 2008 VailatiF-1Document0 pagesEur J Esthet Dent 2008 VailatiF-1Dentist HereNo ratings yet
- Large Lesion Management - Roots0112Document4 pagesLarge Lesion Management - Roots0112nuriacampoNo ratings yet
- Revascularization of Immature Permanent Incisors After Severe Extrusive Luxation InjuryDocument10 pagesRevascularization of Immature Permanent Incisors After Severe Extrusive Luxation InjuryEduardo CarrielNo ratings yet
- Endodontics First Lecture: Dental TraumaDocument10 pagesEndodontics First Lecture: Dental Traumaasop06No ratings yet
- Management of Open ApexDocument28 pagesManagement of Open Apexdiksha sinha100% (4)
- 5 Working Length Dr. SarahDocument6 pages5 Working Length Dr. SarahFatimah ZahraaNo ratings yet
- Endodontics Final ReviewerDocument27 pagesEndodontics Final ReviewerRosette Go100% (5)
- Pulp Therapy For The Young Permanent Dentition: ApexogenesisDocument15 pagesPulp Therapy For The Young Permanent Dentition: Apexogenesisapi-3855312No ratings yet
- A Tactile Method For Canal Length Determination in EndodonticsDocument3 pagesA Tactile Method For Canal Length Determination in EndodonticsdrtoothNo ratings yet
- Department of Conservative Dentistry: Presented By: Nikita GoyalDocument27 pagesDepartment of Conservative Dentistry: Presented By: Nikita GoyalAnkita GoyalNo ratings yet
- Dr. Muneera GhaithanDocument44 pagesDr. Muneera GhaithanAli MezaalNo ratings yet
- Microsoft Word - Vital Pulp TherapyDocument11 pagesMicrosoft Word - Vital Pulp TherapyZeinab Mohamed MorsyNo ratings yet
- Apex o GenesisDocument54 pagesApex o GenesisbrahmannaNo ratings yet
- Modified Oral ScreenDocument5 pagesModified Oral ScreenJovia Chitrayanti0% (1)
- Dominguez Reyes 2005Document5 pagesDominguez Reyes 2005Ábilson FabianiNo ratings yet
- Intracanal MedicationDocument34 pagesIntracanal MedicationdentistdentistdentisNo ratings yet
- Cvek Pulpotomy: Report of A Case With Five-YearDocument4 pagesCvek Pulpotomy: Report of A Case With Five-YearKaren SandovalNo ratings yet
- Pulpectomy & ApexificationDocument72 pagesPulpectomy & ApexificationSimrah AjmalNo ratings yet
- Treatment Planning Seminar IDocument23 pagesTreatment Planning Seminar Ialsakar26No ratings yet
- Maxillary ObturatorDocument79 pagesMaxillary ObturatorAmit KhattakNo ratings yet
- 1 Three Years Follow Up of Combined Perio EndoDocument3 pages1 Three Years Follow Up of Combined Perio EndohanNo ratings yet
- Cons5-Sheet 5Document29 pagesCons5-Sheet 5Yomna NimerNo ratings yet
- Apexification 07.03.22Document10 pagesApexification 07.03.22Shreya KediaNo ratings yet
- Dentj 38 4 09Document4 pagesDentj 38 4 09ilmayudNo ratings yet
- Pedodontic Lect 19Document4 pagesPedodontic Lect 19Mustafa AmmarNo ratings yet
- Endo SurgeryDocument5 pagesEndo Surgeryahmed muhammadNo ratings yet
- Bioabsorbable Root Analogue For Closure of Oroanatral Communication - Thoma Et Al - BIBL 36Document7 pagesBioabsorbable Root Analogue For Closure of Oroanatral Communication - Thoma Et Al - BIBL 36stoia_sebiNo ratings yet
- GoldenDocument308 pagesGoldenammarkochiNo ratings yet
- 79-87 BGDDDRDocument9 pages79-87 BGDDDRaftinaaNo ratings yet
- انو محاضرة ثانية اسنان ذي قارDocument12 pagesانو محاضرة ثانية اسنان ذي قارhaider yahyaNo ratings yet
- Bioabsorbable Root Analogue For Closure of Oroantral Comm After Tooth ExtractionDocument0 pagesBioabsorbable Root Analogue For Closure of Oroantral Comm After Tooth ExtractionTrinhTaNo ratings yet
- Clinical Cases in Restorative and Reconstructive DentistryFrom EverandClinical Cases in Restorative and Reconstructive DentistryRating: 5 out of 5 stars5/5 (1)
- Adhesive Restoration of Endodontically Treated TeethFrom EverandAdhesive Restoration of Endodontically Treated TeethRating: 3 out of 5 stars3/5 (2)
- Minimally Invasive Approaches in Endodontic PracticeFrom EverandMinimally Invasive Approaches in Endodontic PracticeGianluca PlotinoNo ratings yet
- OHNS--Otolaryngology; Head and Neck surgery: pocket field guideFrom EverandOHNS--Otolaryngology; Head and Neck surgery: pocket field guideNo ratings yet
- Reaearch Article Annals and Essences of DentistryDocument6 pagesReaearch Article Annals and Essences of DentistrykowmudimaddineniNo ratings yet
- Diet and Its Relation To Endodontic InflammationDocument4 pagesDiet and Its Relation To Endodontic InflammationkowmudimaddineniNo ratings yet
- Bonding AgentsDocument4 pagesBonding Agentskowmudimaddineni100% (1)
- Caries Excavation: Created By: T. Dammaschke Category: Preserving Dentistry Table of ContentDocument6 pagesCaries Excavation: Created By: T. Dammaschke Category: Preserving Dentistry Table of ContentkowmudimaddineniNo ratings yet
- Root Canal Sealers - SeminarDocument49 pagesRoot Canal Sealers - Seminarkowmudimaddineni100% (2)
- Adult Early Warning Score Observation Chart For Cardiothoracic UnitDocument1 pageAdult Early Warning Score Observation Chart For Cardiothoracic UnitalexipsNo ratings yet
- Pregnancy Induced Hypertension (PIH)Document15 pagesPregnancy Induced Hypertension (PIH)Aiman ArifinNo ratings yet
- Plural of Medical Terms UsmpDocument2 pagesPlural of Medical Terms UsmpUSMP FN ARCHIVOSNo ratings yet
- Adobe Scan Jul 28, 2023Document6 pagesAdobe Scan Jul 28, 2023Krishna ChaurasiyaNo ratings yet
- A Sonographic Sign of Moderate ToDocument5 pagesA Sonographic Sign of Moderate ToDivisi FER MalangNo ratings yet
- Malawi Clinical HIV Guidelines 2019 Addendumversion 8.1Document28 pagesMalawi Clinical HIV Guidelines 2019 Addendumversion 8.1INNOCENT KHULIWANo ratings yet
- Upper Gastrointestinal BleedingDocument41 pagesUpper Gastrointestinal BleedingAnusha VergheseNo ratings yet
- LP MAPEH 9 (Health)Document4 pagesLP MAPEH 9 (Health)Delima Ninian100% (2)
- ETT IntubationDocument27 pagesETT IntubationGilbert Sterling Octavius100% (1)
- Protokol KemoterapiDocument147 pagesProtokol KemoterapiDala VW100% (1)
- Quiz 632 General Science For SSC ExaminationsDocument4 pagesQuiz 632 General Science For SSC ExaminationsDibyendu SahuNo ratings yet
- CHCCCS023 Support Independence and WellbeingDocument22 pagesCHCCCS023 Support Independence and WellbeingSushma karkiNo ratings yet
- Acid Base Disorders JAPIDocument5 pagesAcid Base Disorders JAPIVitrag_Shah_1067No ratings yet
- Why Jaggery? Is Jaggery Healthy? What Is Better: Jaggery or Sugar? Can Jaggery Cure Ailments?Document5 pagesWhy Jaggery? Is Jaggery Healthy? What Is Better: Jaggery or Sugar? Can Jaggery Cure Ailments?satheb319429No ratings yet
- Five Elements Chart TableDocument7 pagesFive Elements Chart TablePawanNo ratings yet
- Bahasa InggrisDocument6 pagesBahasa InggrisSofi SusantoNo ratings yet
- Algorithm: Essential Newborn Care: Is The Baby Gasping or Not Breathing?Document1 pageAlgorithm: Essential Newborn Care: Is The Baby Gasping or Not Breathing?Dela cruz KimberlyNo ratings yet
- Unilever Lifebuoy in India Implementing The Sustainability PlanDocument14 pagesUnilever Lifebuoy in India Implementing The Sustainability PlanMira Sesaria50% (2)
- Satyug Darshan Vidalaya1Document30 pagesSatyug Darshan Vidalaya1Naina GuptaNo ratings yet
- Amazing Facts About Our BrainDocument4 pagesAmazing Facts About Our BrainUmarul FarooqueNo ratings yet
- Pathophysiology of Intrauterine Growth Restriction (IUGR) - The... Download Scientific DiagramDocument1 pagePathophysiology of Intrauterine Growth Restriction (IUGR) - The... Download Scientific DiagramNajla As'ariNo ratings yet
- Formulation and Evaluation of Herbal Lip Rouge.: Research ArticleDocument5 pagesFormulation and Evaluation of Herbal Lip Rouge.: Research ArticleTynNo ratings yet
- Human Body Systems: Study GuideDocument11 pagesHuman Body Systems: Study Guideapi-242114183No ratings yet
- International Rice Research Notes Vol.18 No.1Document69 pagesInternational Rice Research Notes Vol.18 No.1ccquintosNo ratings yet
- CHN - 1Document23 pagesCHN - 1Raagul SaravanaKumarNo ratings yet
- Week 6 Nursing Care of The Family With Reproductive DisordersDocument27 pagesWeek 6 Nursing Care of The Family With Reproductive DisordersStefhanie Mae LazaroNo ratings yet
- The Effect of Tobacco Smoking Among Third Year Student Nurse in The University of LuzonDocument6 pagesThe Effect of Tobacco Smoking Among Third Year Student Nurse in The University of LuzonNeil Christian TadzNo ratings yet
- IMTX PatentDocument76 pagesIMTX PatentCharles GrossNo ratings yet
- Histopathology of Dental CariesDocument7 pagesHistopathology of Dental CariesJOHN HAROLD CABRADILLANo ratings yet
- Nail Disorder and DiseasesDocument33 pagesNail Disorder and Diseasesleny90941No ratings yet